Abstract
The study was performed to determine age, gender, and time-dependent changes in aortic wall thickness (AWT), and to evaluate cross-sectional associations between AWT and arterial stiffness in older adults. Three hundred seventy-one (371) longitudinal and 426 cross-sectional measurements of AWT from cardiovascular magnetic resonance (CMR) imaging studies conducted within the Multi-Ethnic Study of Atherosclerosis (MESA) were analyzed at two points in time: in 2000-2002 and then again from follow-up examinations in 2010-2012. Aortic wall thickness was determined from a double inversion recovery black-blood fast spin-echo sequence, and aortic stiffness was measured from a phase-contrast cine gradient echo sequence. The thickness of the mid-thoracic descending aortic wall was measured and correlated to distensibility of the ascending aorta (AAD) and aortic pulse wave velocity (PWV). The average rate of AWT change was 0.032mm per year. The increase in AWT was greater for those aged 45 to 54 years relative to individuals older than age 55 years (p-trend<0.001). Ascending aortic distensibility was lower (p<0.001) and PWV was higher (p=0.012) for hypertensive subjects. After adjustment for traditional risk factors, AAD was significantly related to AWT in participants without hypertension. Hypertension was associated with increased aortic stiffness independent of aortic wall thickness.
Keywords: MR imaging, aortic wall thickness, longitudinal changes, arterial stiffness, hypertension
Introduction
Arterial wall thickening is an early sign of atherosclerosis,1,2 and is associated with the prevalence and incidence of cardiovascular disease.3 There are reports of age-related increases of arterial wall thickness (AWT) in several cross-sectional community-based studies;4,5 however, rates of change in AWT among middle-aged and older adults have not been defined. Moreover, the relationship between AWT and aortic stiffness after accounting for cardiovascular risk factors has not been defined.
In a subset of individuals from the Multi-Ethnic Study of Atherosclerosis (MESA), we measured AWT and aortic distensibility using cardiac magnetic resonance (CMR) imaging as well as demographic and clinical variables. The purpose of this study was two-fold. First, we sought to characterize the age, demographic, and gender-specific distributions along with the yearly rates of change of AWT in adults aged > 45 years without symptomatic arteriosclerotic disease. Second, we desired to evaluate associations between AWT and arterial stiffness (measured by aortic distensibility and pulse wave velocity [PWV]) in these same individuals.
Methods
Study population
The first CMR exam from the MESA was initiated by the National Heart, Lung, and Blood Institute (Bethesda, MD) in 2000. This exam was performed to obtain a baseline from which future longitudinal studies could be performed to further understanding of the pathogenesis of atherosclerosis and other cardiovascular diseases in individuals whom were otherwise without evidence of symptomatic arteriosclerotic disease.6 In the longitudinal follow-up of the fifth examination (MESA5), each subject in the MESA study underwent CMR from April 2010 to February 2012. Institutional review boards at each center approved the study protocol. Of these, only one clinical site (Wake Forest University, Winston Salem, NC) had AWT images acquired in both the baseline and the follow-up CMR studies. Researchers analyzed 371 participants at baseline and 423 participants in the follow-up sessions. We excluded participants with myocardial scarring (based on the CMR late gadolinium enhancement studies) from the analysis.
MR aortic wall thickness and stiffness imaging
Baseline CMR was performed using 1.5-T whole-body MRI systems: Signa CV/i or Signa LX (GE Medical Systems, Waukesha, Wisconsin). A double-inversion recovery black-blood fast spin-echo sequence with ECG gating was used to obtain the AWT images. We acquired axial images of the descending thoracic aorta at the level of the right pulmonary artery. Imaging parameters were TR=2 R-R intervals; TE=42ms; field of view=36×36 cm; slice thickness=6 mm; echo-train length=32; and matrix size=512×256. In the follow-up examinations, CMR was performed using a 1.5T Siemens scanner (Avanto, Siemens Medical Systems, Erlangen, Germany). The imaging sequence and plane were similar to those used in the baseline, but employed a different protocol: TR=2 R-R intervals; TE=66ms; field of view =36×30 cm; slice thickness=10 mm; echo-train length=17; and matrix size=256×216. Aortic wall thickness was measured by a single observer using the same method and software as described in the MESA AWT study.7 The thickness of the midthoracic descending aortic wall was measured using electronic calipers at 4 standard positions: 12, 3, 6, and 9 o'clock (QMASS 7.2, Medis, Leiden, The Netherlands). We calculated AWT as the average value of these 4 measurements. Phase contrast cine gradient echo sequence was also obtained to evaluate aortic stiffness in the follow-up study. An aortic sagittal oblique plane with a black-blood sequence was acquired to position the aortic phase-contrast imaging, and also allowed for the measurement of the path- length between the ascending and descending aorta. Imaging parameters were as follows: temporal resolution=35 ms; field of view=36×27 cm; slice thickness=10 mm; matrix size=128 × 96; 1 signal average; velocity encoding gradient=100 cm/s.
Using validated automated software (ARTFUN. INSERM U678),8 the study recorded distensibility of the ascending aorta (AAD) and PWV. The study calculated distensibility as: AAD (mmHg−1) = [(maximum area ascending aorta – minimum area ascending aorta)] / [PP × minimum area ascending aorta] × 1,000, where PP is the brachial pulse pressure measured from the systolic and diastolic pressure during CMR aortic acquisition. Pulse wave velocity was measured as: PWV (m/s) = distance (mm) / transit time between ascending to descending aorta (ms). As previously described, the transit time was calculated as the average time difference using the least squares estimate between all data points on the systolic upslopes of the ascending and descending aortic flow curves after peak flow normalization.9
Statistical Analysis
We performed statistical analysis using SPSS (Chicago, Illinois). All continuous data were expressed as mean ± 1 standard deviation. Only those participants with aortic wall imaging at both time points were included in the longitudinal data analysis. For categorical variables, we used a Chi-square test. An unpaired student's t-test was utilized to compare the continuous variables between groups. To detect determinants of AWT changes over 10 years, multivariate linear regression analysis was performed that adjusted for the baseline age, gender, body mass index (BMI), race/ethnicity, smoking status, pack-year, low-density lipoprotein (LDL), high-density lipoprotein (HDL), systolic and diastolic blood pressure, diabetes, and hypertension status.
For the cross-sectional analysis in the follow-up exam, we first determined the relationship between AWT and the risk factors using the same model described above. To examine the association between AAD and PWV with AWT, we stratified populations by hypertensive status. Ascending aorta distensibility and PWV were continuous variables to determine their associations to AWT. Linear regressions with multivariable adjustments for demographic characteristics and risk factors were performed. Model 1 reflected adjustments for age, sex, BMI, and race/ethnicity, and model 2 demonstrated adjustments for variables in model 1 as well as systolic and diastolic blood pressure, diabetes mellitus, LDL, HDL, current smoking status, and smoking pack years. A two-tailed p-value of <0.05 was considered statistically significant.
Results
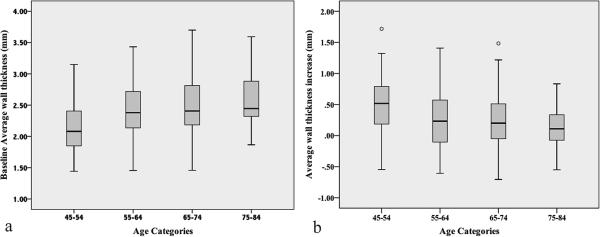
Table 1 lists demographics and aortic measurements in the latter (MESA5, 2010-2012) exams, and changes of AWT over ten years. The study cohort consisted of 61% non-Hispanic white and 39% African American subjects. Aortic wall thickness was significantly different between men and women. Men had thicker aortic walls than women (for men the baseline measure was 2.40±0.44mm, and during the MESA5 exam it was 2.75±0.26mm for men, and baseline: 2.32±0.43mm, MESA5: 2.61±0.26mm for women), but aortic stiffness measures (i.e. AAD and PWV) were similar. The change of AWT over ten years was 0.35±0.48 mm for men and 0.30±0.44 mm for women (p=0.26). The average AWT change was 0.32±0.46 mm in ten years. Figure 1 displays the average AWT at the baseline and AWT increase over ten years by age categories (at the baseline age). Aortic wall thickness increased more for those with a baseline age of 45-54 years, and reached a plateau as age increased (p-trend < 0.001).
Table 1.
Mean characteristics of the MESA5 participants
| At MESA5 (2010-2012), mean±SD | Global (N=423) | Women (N=244) | Men (N=179) | p-value |
|---|---|---|---|---|
| Age (years) | 70.8±8.7 | 70.9±8.9 | 70.5±8.5 | 0.7 |
| Race (N of white/African-American) | 259/164 | 144/100 | 115/64 | 0.29 |
| Body mass index (kg/m2) | 28.7±5.3 | 28.7±5.9 | 28.3±5.3 | 0.72 |
| Systolic blood pressure (mmHg) | 125±21 | 125±21 | 124±21 | 0.65 |
| Diastolic blood pressure (mmHg) | 68±10 | 65±10 | 71±10 | < 0.001 |
| Low-density lipoprotein (mg/dl) | 106±34 | 110±36 | 101±30 | 0.008 |
| High-density lipoprotein (mg/dl) | 56±16 | 61±17 | 50±13 | <0.001 |
| Metabolic Syndrome, (%)* | 34.3 | 39.5 | 28.1 | 0.014 |
| Aortic wall thickness (mm) | 2.67±0.27 | 2.61±0.26 | 2.75±0.26 | < 0.001 |
| Aortic wall thickness at baseline (mm) | 2.36±0.44 | 2.32±0.43 | 2.40±0.44 | 0.074 |
| AWT difference in ten years (mm) | 0.32±0.46 | 0.30±0.44 | 0.35±0.48 | 0.26 |
| Distensibility of ascending aorta (mmhg−1) | 2.04±1.4 | 2.04±1.4 | 2.04±1.5 | 0.97 |
| Pulse wave velocity (m/s) | 9.12±3.82 | 9.03±3.48 | 9.29±4.32 | 0.54 |
Metabolic Syndrome was defined by NCEP guidelines.
Figure 1.
(a) Aortic wall thickness at the baseline study by age categories. (b) Average aortic wall thickness increase in ten years by age categories (in the baseline age).
In the fully adjusted models, the baseline age, race, and BMI were the major predictors for the rate of change in AWT. Age was inversely correlated with greater rate of change in AWT (B= -0.013 mm/year, p<0.001, consistent with Figure 1), while higher BMI was related to increased AWT. (B=0.018 mm/kg/m2, p=0.001). White race was also positively associated with greater AWT increase when compared to African-Americans (p=0.03). Blood pressures at baseline were not related to the AWT change.
Among the risk factors examined, AWT in MESA5 was mainly related to older age (B= 0.007 mm/year, p<0.001), higher BMI (B=0.009 mm/kg/m2, p=0.001), higher diastolic blood pressure (B=0.005 mm/mmHg, p=0.005), and lower HDL cholesterol (B=-0.002mm/mg/dl, p=0.02).
To study the correlations between aortic morphology and function, Table 2 lists basic demographics, AWT, AAD and PWV stratified by hypertension status in the latter exam (2010-2012). When comparing these two groups, we found that AWT was not different (p=0.35) but distensibility was lower (p<0.001) and PWV was higher (p=0.012) in those with hypertension. Multivariable linear regression analyses (Table 3) demonstrated that distensibility was significantly correlated to AWT in the cohort without hypertension. Aortic wall thickness predicted PWV in the first model (Model 1, Table 3) in those with hypertension, but this correlation diminished after adjusting for more variables (Model 2, Table 3).
Table 2.
Mean characteristics of the MESA participants stratified by hypertension status
| At MESA5 (2010-2012), mean±SD | With hypertension (N=264) | W/O hypertension (N=159) | p-value |
|---|---|---|---|
| Age (years) | 72±8.5 | 69±8.6 | < 0.001 |
| Race (% of white/black) | 51/49 | 77/23 | < 0.001 |
| Body mass index (kg/m2) | 29.3±5.3 | 27.7±5.1 | 0.002 |
| Men (%) | 38 | 49 | 0.03 |
| Systolic blood pressure (mmHg) | 131±22 | 114±13 | < 0.001 |
| Diastolic blood pressure (mmHg) | 69±11 | 66±10 | 0.012 |
| Low-density lipoprotein (mg/dl) | 102±33 | 113±35 | 0.002 |
| High-density lipoprotein (mg/dl) | 56±16 | 57±17 | 0.49 |
| Metabolic Syndrome, (%)* | 45 | 17 | < 0.001 |
| Aortic wall thickness (mm) | 2.68±0.27 | 2.66±0.26 | 0.35 |
| Ascending aortic distensibility (mmHg−1) | 0.18±0.11 | 0.25±0.18 | < 0.001 |
| Pulse wave velocity (m/s) | 9.5±4.4 | 8.5±2.8 | 0.012 |
Table 3.
Regression analysis for association of distensibility and PWV with AWT (Regression coefficients B/P).
| Stiffness Measures | With hypertension (N=264) | W/O hypertension (N=159) | |||
|---|---|---|---|---|---|
| B | p | B | p | ||
| Ascending aortic distensibility (mmHg−1) | Model 1* | −0.09 | 0.54 | 0.38 | 0.003 |
| Model 2† | −0.10 | 0.55 | 0.43 | 0.003 | |
| Pulse Wave Velocity (m/s) | Model 1 | 0.008 | 0.046 | 0.005 | 0.6 |
| Model 2 | 0.006 | 0.15 | 0.005 | 0.58 | |
Model 1: multivariable analysis accounting for age, sex, race, and BMI.
Model 2: adjusted for variables in model 1 in addition to systolic and diastolic blood pressure, diabetes mellitus, LDL, HDL, current smoking status, and smoking pack years.
Discussion
Using CMR, we analyzed the change of aortic stiffening (distensibility and pulse wave velocity), thoracic AWT, and the relationship of these changes to traditional cardiovascular risk factors in an older (55 to 85 years aged) population that was free of established cardiovascular disease. Change in AWT using the same MRI methods has been previously evaluated in a cross-sectional study of 198 younger individuals.7 Compared to the 0.07 mm AWT increase in five years reported by the prior study in younger participants, our findings reveal a greater increment of change in older individuals free of symptomatic atherosclerotic disease: 0.16 mm in five years longitudinally.
After multivariable adjustment, the primary factors related to change in AWT were age, race, and BMI. While older age was associated with increased AWT, the rate of increase peaked in those 45-55 years in age and then plateaued with advancing age. This is an interesting finding, but we cannot rule out survival bias. Body mass index remained a significant factor associated with an increased AWT. Our results concerning differences in gender were consistent with previous studies:7,10 men had greater AWT than women, but AWT increase over 10 years was similar between genders.
In the longitudinal studies reported by Lam et al. from the Framingham Heart Study,9 morphological changes measured by the aortic root diameters were greater in men and women with obesity and/or hypertension over wide ranges of age. Brandts et al.11 compared 15 patients with hypertension and 15 age- and sex-matched healthy volunteers (mean age 49 years). Aortic wall thickness and PWV were all significantly higher in patients with hypertension. However, in the cross-sectional part of the present study, hypertension was more directly associated with functional impairments (stiffer aorta) than AWT.
The trend of increased arterial wall thickness with atherosclerosis and cardiovascular disease was observed in most subjects.2,3,12 Atherosclerosis and plaque deposition can increase AWT, which, combined with alterations in blood pressure, may lead to progressive increases in stiffness. While higher diastolic blood pressure was related to increased AWT and aortic stiffness was associated with hypertension, there were no overt cardiovascular symptoms in our study population.
Arterial stiffness is accepted as a major determinant of increased systolic and pulse pressure with aging and, therefore, is a major determinant of stroke13 and myocardial infarction. Aside from age and hypertension, arterial stiffness has been associated with numerous conditions, including heart failure14 and ischemic heart disease.13,15 Distensibility measures local stiffness, while PWV is considered to be an integrated marker of arterial stiffness when predicting fatal and non-fatal cardiovascular events. Those with hypertension in our study demonstrated greater aortic stiffness by reduced distensibility and increased PWV than those without hypertension. In subjects without hypertension, AWT was associated more strongly with distensibility than with PWV. Pulse wave velocity was not related to AWT in both groups in the fully adjusted model. This might suggest that AWT has greater impact on local stiffness in late adulthood. Although this finding contrasts with the study by Brandts et al.,11 in which AWT was significantly related to PWV regardless of hypertension status, our participants were 20 years older and PWV was higher than those in the Brandts, et al. study.
We recognize several limitations in our study. Current analyses included only non-Hispanic white and African-American subjects from a single site in the MESA study. Generalization to the entire MESA cohort, which includes Hispanic and Chinese participants, is therefore not possible. We only acquired AWT on a single cross-section of the descending aorta, and compared to the distensibility of the ascending aorta. Pulse wave velocity was also limited to the aortic arch. These standardized sampling sites were for both cross-sectional and longitudinal comparisons without increasing the scanning burden. Because of the heterogeneity in the vascular remodeling process and atherosclerotic changes across the arterial tree, the local measurement is not able to reflect the plaque burden as a systemic disease, particularly in the abdominal aorta.
Perspectives
In conclusion, using standardized MRI methods, we demonstrated longitudinally from the Multiethnic Study of Atherosclerosis that during mid to late adulthood, thoracic aortic wall thickens in a yearly rate of 0.032mm. While men demonstrated thicker walls than women, there was difference between genders in the rate of change in thickening. This change in aortic wall thickness over time has particular importance while considering risk factors for atherosclerosis in longitudinal research studies. Increase in AWT beyond this nominal change may identify individuals at higher risk for atherosclerosis. The data presented herein suggests aortic structural change is primarily related to age, race, and BMI. In those with hypertension, the aorta stiffens without necessarily impacting aortic wall thickness.
Novelty and Significance.
-
1)
What Is New: Using standardized MRI methods, we demonstrated longitudinally from the Multiethnic Study of Atherosclerosis that during mid to late adulthood, the thoracic aortic wall thickens in a yearly rate of 0.032mm over.
-
2)
What Is Relevant: This change has particular importance while considering risk factors for atherosclerosis in longitudinal research studies. The data presented herein suggest aortic structural change is primarily related to age, race, and BMI. In those with hypertension, the aorta stiffens without necessarily impacting aortic wall thickness.
-
3)
Summary: The increase in AWT was greater for those aged 45 to 54 years relative to individuals older than age 55 years. Ascending aortic distensibility was lower and PWV was higher for hypertensive subjects. Hypertension was associated with increased aortic stiffness independent of aortic wall thickness.
Acknowledgements
This research was supported by contracts N01-HC-95165, N01-HC-95168, from the National Heart, Lung, and Blood Institute and by grants R01 HL076438. The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org. We would also like to express our appreciation to Amy Gardin for reviewing and editing this manuscript.
Sources of Funding
N01-HC-95165, N01-HC-95168, R01 HL076438
Footnotes
Conflict-of-interest/disclosure
None
References
- 1.Ludwig M, von Petzinger-Kruthoff A, von Buquoy M, Stumpe KO. [intima media thickness of the carotid arteries: Early pointer to arteriosclerosis and therapeutic endpoint]. Ultraschall Med. 2003;24:162–174. doi: 10.1055/s-2003-40058. [DOI] [PubMed] [Google Scholar]
- 2.Nakashima Y, Wight TN, Sueishi K. Early atherosclerosis in humans: Role of diffuse intimal thickening and extracellular matrix proteoglycans. Cardiovasc Res. 2008;79:14–23. doi: 10.1093/cvr/cvn099. [DOI] [PubMed] [Google Scholar]
- 3.Burke GL, Evans GW, Riley WA, Sharrett AR, Howard G, Barnes RW, Rosamond W, Crow RS, Rautaharju PM, Heiss G. Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults. The atherosclerosis risk in communities (aric) study. Stroke. 1995;26:386–391. doi: 10.1161/01.str.26.3.386. [DOI] [PubMed] [Google Scholar]
- 4.Rosero EB, Peshock RM, Khera A, Clagett P, Lo H, Timaran CH. Sex, race, and age distributions of mean aortic wall thickness in a multiethnic population-based sample. J Vasc Surg. 2011;53:950–957. doi: 10.1016/j.jvs.2010.10.073. [DOI] [PubMed] [Google Scholar]
- 5.Stein JH, Douglas PS, Srinivasan SR, Bond MG, Tang R, Li S, Chen W, Berenson GS. Distribution and cross-sectional age-related increases of carotid artery intima-media thickness in young adults: The bogalusa heart study. Stroke. 2004;35:2782–2787. doi: 10.1161/01.STR.0000147719.27237.14. [DOI] [PubMed] [Google Scholar]
- 6.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr., Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: Objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 7.Li AE, Kamel I, Rando F, Anderson M, Kumbasar B, Lima JA, Bluemke DA. Using mri to assess aortic wall thickness in the multiethnic study of atherosclerosis: Distribution by race, sex, and age. AJR Am J Roentgenol. 2004;182:593–597. doi: 10.2214/ajr.182.3.1820593. [DOI] [PubMed] [Google Scholar]
- 8.Herment A, Kachenoura N, Lefort M, Bensalah M, Dogui A, Frouin F, Mousseaux E, De Cesare A. Automated segmentation of the aorta from phase contrast mr images: Validation against expert tracing in healthy volunteers and in patients with a dilated aorta. J Magn Reson Imaging. 2010;31:881–888. doi: 10.1002/jmri.22124. [DOI] [PubMed] [Google Scholar]
- 9.Lam CS, Xanthakis V, Sullivan LM, Lieb W, Aragam J, Redfield MM, Mitchell GF, Benjamin EJ, Vasan RS. Aortic root remodeling over the adult life course: Longitudinal data from the framingham heart study. Circulation. 2010;122:884–890. doi: 10.1161/CIRCULATIONAHA.110.937839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malayeri AA, Natori S, Bahrami H, Bertoni AG, Kronmal R, Lima JA, Bluemke DA. Relation of aortic wall thickness and distensibility to cardiovascular risk factors (from the multi-ethnic study of atherosclerosis [mesa]). Am J Cardiol. 2008;102:491–496. doi: 10.1016/j.amjcard.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brandts A, Westenberg JJ, van Elderen SG, Kroft LJ, Roes SD, Tamsma JT, van der Geest RJ, Lamb HJ, Doornbos J, Putter H, Stuber M, de Roos A. Site-specific coupling between vascular wall thickness and function: An observational mri study of vessel wall thickening and stiffening in hypertension. Invest Radiol. 2013;48:86–91. doi: 10.1097/RLI.0b013e31827f6410. [DOI] [PubMed] [Google Scholar]
- 12.Bonithon-Kopp C, Touboul PJ, Berr C, Leroux C, Mainard F, Courbon D, Ducimetiere P. Relation of intima-media thickness to atherosclerotic plaques in carotid arteries. The vascular aging (eva) study. Arterioscler Thromb Vasc Biol. 1996;16:310–316. doi: 10.1161/01.atv.16.2.310. [DOI] [PubMed] [Google Scholar]
- 13.Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, Asmar R, Reneman RS, Hoeks AP, Breteler MM, Witteman JC. Arterial stiffness and risk of coronary heart disease and stroke: The rotterdam study. Circulation. 2006;113:657–663. doi: 10.1161/CIRCULATIONAHA.105.555235. [DOI] [PubMed] [Google Scholar]
- 14.Giannattasio C, Achilli F, Failla M, Capra A, Vincenzi A, Valagussa F, Mancia G. Radial, carotid and aortic distensibility in congestive heart failure: Effects of high-dose angiotensin-converting enzyme inhibitor or low-dose association with angiotensin type 1 receptor blockade. J Am Coll Cardiol. 2002;39:1275–1282. doi: 10.1016/s0735-1097(02)01755-2. [DOI] [PubMed] [Google Scholar]
- 15.Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37:1236–1241. doi: 10.1161/01.hyp.37.5.1236. [DOI] [PubMed] [Google Scholar]