Abstract
To describe the signalment, clinicopathological findings and outcome in dogs presenting with acute kidney injury (AKI) and skin lesions between November 2012 and March 2014, in whom cutaneous and renal glomerular vasculopathy (CRGV) was suspected and renal thrombotic microangiopathy (TMA) was histopathologically confirmed. The medical records of dogs with skin lesions and AKI, with histopathologically confirmed renal TMA, were retrospectively reviewed. Thirty dogs from across the UK were identified with clinicopathological findings compatible with CRGV. These findings included the following: skin lesions, predominantly affecting the distal extremities; AKI; and variably, anaemia, thrombocytopaenia and hyperbilirubinaemia. Known causes of AKI were excluded. The major renal histopathogical finding was TMA. All thirty dogs died or were euthanised. Shiga toxin was not identified in the kidneys of affected dogs. Escherichia coli genes encoding shiga toxin were not identified in faeces from affected dogs. CRGV has previously been reported in greyhounds in the USA, a greyhound in the UK, without renal involvement, and a Great Dane in Germany. This is the first report of a series of non-greyhound dogs with CRGV and AKI in the UK. CRGV is a disease of unknown aetiology carrying a poor prognosis when azotaemia develops.
Keywords: Renal disease, Skin, Histopathology, Kidneys, Internal medicine, Dermatopathology
Introduction
Cutaneous and renal glomerular vasculopathy (CRGV) is a disease of unknown aetiology, reported to cause ulceration of the distal extremities in dogs. It is variably associated with clinically relevant acute kidney injury (AKI). CRGV has been reported in greyhounds in the USA (Carpenter and others 1988), a Great Dane in Germany (Rotermund and others 2002) and a greyhound in the UK (Hendricks 2000).
The major renal histopathological lesion reported in CRGV is thrombotic microangiopathy (TMA). Thrombotic microangiopathies are characterised by inflammation and damage to vascular endothelium, leading to widespread formation of microthrombi and resultant consumptive thrombocytopaenia, microangiopathic haemolytic anaemia and multiorgan dysfunction (Noris and others 2012). CRGV is the only canine disease previously reported to cause vasculopathy preferentially affecting the small vessels of the kidney and skin.
AKI can result from pre-renal (Waikar and others 2008), renal (Rentko and others 1992, Vaden and others 1997, Eubig and others 2005) and post-renal events (Fischer and others 2009). Skin lesions are not commonly associated with AKI in dogs, unless the AKI has resulted from immune-mediated disease (Fournel and others 1992), certain neoplasms (Moore and others 1994), infectious diseases (Ferrer and others 1988) or vascular events, such as vasculopathy (Goldfarb and Adler 2001).
The purpose of this report is to summarise the signalment, clinicopathological findings and outcome in 30 dogs presenting between November 2012 and March 2014, in which CRGV was suspected clinically and TMA was identified histopathologically.
Materials and methods
Cases were identified by comprehensive search of computerised record systems (using keywords) at two referral practices. Case records were searched for the diagnosis of AKI, with subsequent review of clinical case files and renal/dermal histopathology in order to identify cases compatible with CRGV. Further case submissions came from two other referral practices and 49 first opinion practices. Practices became aware of CRGV through a combination of: a letter in the veterinary literature (Walker and McMahon 2013), media reports and information on a specialist practice website. Records from suspected cases were thus selected by the additional 51 practices both prospectively and retrospectively (from memory rather than via computerised record system searches) and were subsequently reviewed by two of the authors (LPH, DJW). Dogs were included if they presented between November 1, 2012 and March 31, 2014 with skin lesions and AKI with no known identifiable cause, and with renal histopathological evidence of TMA. Animals were defined as having AKI if they had historical and laboratory evidence of kidney injury with or without clinical oligoanuria (International Renal Interest Society; www.iris-kidney.com, 2013). Clinicopathological data are reported as median and range.
Histopathology
Representative sections from skin, kidney and other organs, where possible, were paraffin embedded. Sections of 3–4 μm were prepared from each of the tissues via microtome and affixed to lysine-charged glass slides. These were stained by standard technique with haematoxylin and eosin. In addition, sections of the kidney were also stained with Warthin-Starry silver stain and Periodic Acid Schiff. Kidneys from three dogs were also stained with Masson's trichrome and Jones Methenamine silver method.
All of the renal histopathology was reviewed by a single veterinary pathologist (IH). Renal samples from three dogs were also submitted to a second veterinary pathologist (RC).
PCR for pathogenic Leptospira spp.i was carried out on sections of kidney and liver using an amplification mixture as previously described (Bourhy and others 2011). DNA was amplified and detected on a Stratagene Mx3005P qPCR system, using a program of 95°C for 10 minutes followed by 50 cycles of 95°C for 30 seconds and 57°C for 60 seconds.
Fluorescence in situ hybridisation (FISH) for pathogenic bacteriai was performed on de-waxed tissue sections (kidney and liver) using fluorescently labelled probes. Eubacteria were detected using a mixture of three probes: GCTGCCTCCCG TAGGAGT, GCAGCCACCCGTAGGTGT and GCTGCCACCCG TAGGTGT. Leptospira were detected using probe CGGGTGCT CCCCACTCAG. Escherichia coli were detected using probe GCAAAGGTATTAACTTTACTCCC.
Viral metagenomicsii was performed on fresh kidney tissue, liver and lymph node by random nucleic acid amplification after enrichment for viral particles, followed by DNA sequencing and similarity searches (Illumina MiSeq library) for sequences related to those of known viruses (Victoria and others 2009).
PCR for Dog Circovirus was performed on splenic tissueii (paraffin embedded samples and fresh frozen tissue) as previously described (Li and others 2013).
FISH for Dog Circovirusi was performed on kidney tissue using probe CTCAGACAGAGACACCGTTGCTATG as previously described (Li and others 2013). Identification of bacteria was made against both unstained and organism-negative controls.
FISH for Shiga toxin:i mouse anti-Shiga toxin antibody (diluted 1/100) was incubated overnight at 4°C on renal tissue sections, which were then washed three times and incubated with goat anti-mouse G1 FITC-conjugated secondary antibody. Slides were viewed using a fluorescence microscope.
PCR for Shiga toxin on renal tissue:iii DNA was extracted from paraffin-embedded samples using the QIAamp®DNA FFPE Tissue Kit (Qiagen, Hilden, Germany). PCR for verotoxin 1 and 2 was then performed as previously described (Burnens and others 1995).
PCR for E. coli virulence genes on faeces:iv DNA was extracted from colonies of E. coli cultured from faeces (Wizard Miniprep DNA purification System, Promega). Multiplex PCRs for eaeA, stx 1 and 2, LT1 and ST1 and 2 genes were performed, as previously described (Pass and others 2000).
Results
Seventy-one cases of AKI with skin lesions were identified within the defined time period for which there was clinical suspicion of CRGV. Of these, 41 cases were excluded due to limited investigation and/or incomplete medical records. Thirty cases met the inclusion criteria as affected cases with confirmed TMA on renal histopathology.
Signalment, history and clinical signs
Breeds represented were English springer spaniel (n=5), crossbreed above 20 kg (n=4), flat coated retriever (n=4), whippet (n=3), border collie (n=2), Jack Russell terrier (n=2), Doberman (n=2) and one each of, Labrador retriever, cocker spaniel, Staffordshire bull terrier, Hungarian vizsla, Weimaraner, Dalmatian, Tibetan terrier and crossbreed below 20 kg. Median age was 4.90 years (1.00–11.75 years). Ten were male neutered, seven were female neutered, six were male entire and seven were female entire. Median weight was 23.2 kg (7.3–40.4 kg, n=28).
Affected cases were identified from multiple areas of northern and southern England (Fig 1). Ten dogs had been in the New Forest National Park shortly (four hours to 14 days) before developing skin lesions and/or becoming unwell.
FIG 1:
Map to show distribution of where confirmed cases lived. (Zoomed in view shows distribution of cases in the South of England as there were proportionally more cases from this area)
Over the first 12 months of the study period (November 1, 2012–October 31, 2013), confirmed cases presented in November (n=2), December (n=2), February (n=4), March (n=1) and May (n=1). The remaining 20 confirmed cases presented between November 1, 2013 and March 31, 2014.
Twenty dogs were vaccinated within the past year (vaccines used included distemper, D; hepatitis, H; leptospirosis, L; parvovirus, P; and parainfluenza, Pi: DHLPPi n=10; DHPPi n=1; LP n=1; DHLP n=2; L n=3; LPi n=2; type not recorded n=1), eight were unvaccinated and vaccinal status was unknown in two dogs.
Skin lesions commonly appeared before signs of systemic illness (lethargy, malaise, anorexia, vomiting, pyrexia; n=19). Median time from development of skin lesions to diagnosis of AKI was four days (1–9 days). Nine dogs had systemic signs concurrent with skin lesions and two dogs were systemically ill before developing skin lesions. The management of skin lesions before the development of AKI was variable: no medication (n=7), NSAIDs alone (n=3), antibiotic alone (amoxicillin-clavulanate n=4; marbofloxacin n=1) or a combination of NSAIDs or dexamethasone, and antibiotic (n=12). Information regarding previous medications was unavailable for three cases. With the exception of NSAIDs, none of the dogs had known access to nephrotoxins before initial presentation.
Distribution of skin lesions was: distal limbs (n=28), ventrum (n=9) and oral cavity/muzzle (n=10). Sixteen dogs had more than one lesion. Fourteen had lesions in multiple locations. The appearance of the skin lesions was highly variable, ranging from superficial erosion through to full thickness ulceration, with erythema, oedema and exudation (Fig 2). Early lesions were often erythematous and focal; they occasionally appeared vesicular, with ulceration and necrosis developing subsequently. The skin lesions were often attributed to wounds, bites, stings or focal dermatitis. Lesion size ranged from 0.5 to 5 cm in diameter. Six dogs developed new limb and/or oral lesions while hospitalised. Lesions were typically painful on palpation and digital lesions often caused lameness. Oral lesions were variable but were most often focal erosions or ulcers (Fig 3).
FIG 2:

All images are photographs of lesions affecting confirmed cases. (a) Superficial ulcer affecting medial thigh. (b) Deep ulceration, erythema and exudation on a digit. (c) Erosion to carpal pad, before cleaning. (d) The same lesion after clipping and cleaning
FIG 3:
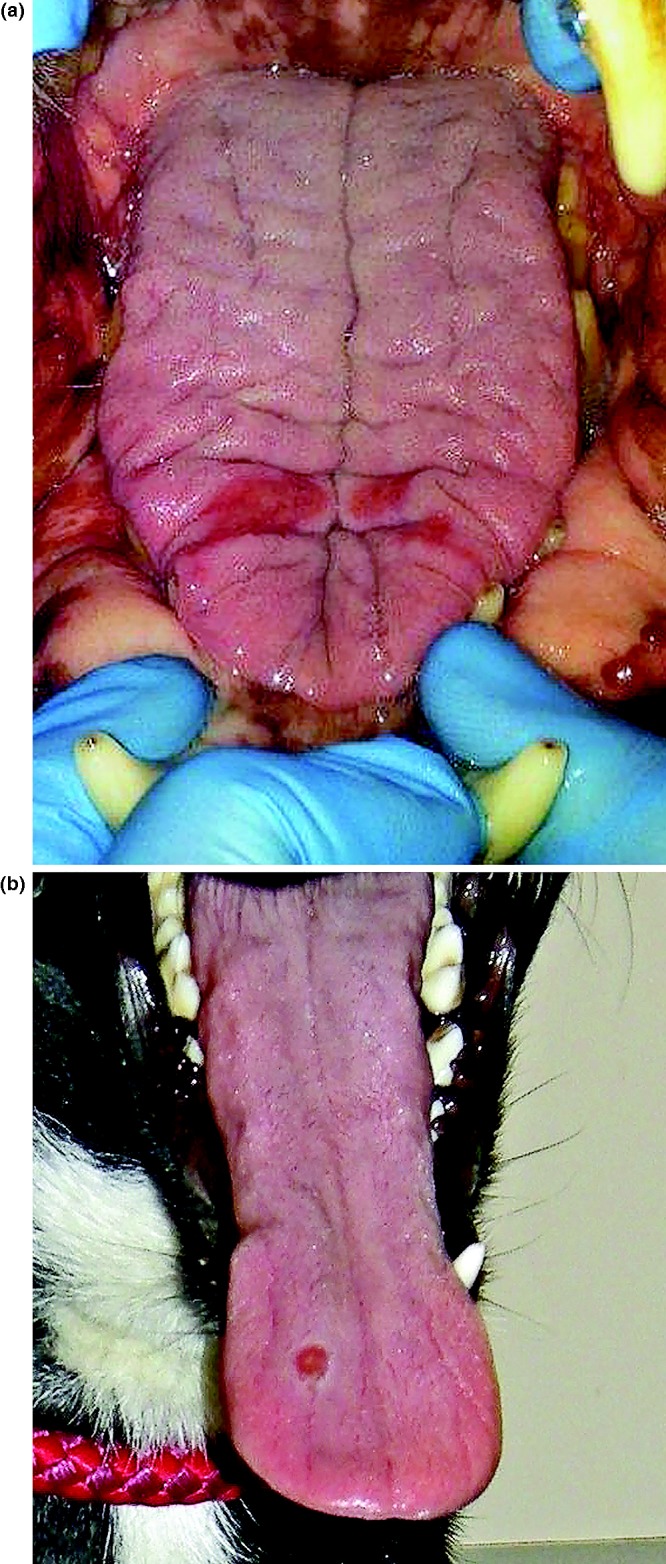
(a) Tongue lesions. (b) Tongue ulcer
The dogs’ clinical signs are summarised in Table 1. Pyrexia generally occurred early in the course of illness (39.8°C; 39.4–40.1°C) and hypothermia typically developed later in the disease course (37.4°C; 36.0–37.7°C).
TABLE 1:
Summary of presenting clinical signs of the 30 affected dogs
| Clinical sign | Number of dogs affected |
|---|---|
| Skin lesions | 30 |
| Anorexia | 20 |
| Vomiting | 20 |
| Lethargy | 19 |
| Hypothermia | 19 |
| Lameness | 10 |
| Icterus | 6 |
| Pyrexia | 6 |
| Diarrhoea | 4 |
| Petechiae | 4 |
| Seizures | 3 |
| Haematochezia | 2 |
| Haematemesis | 1 |
| Epistaxis | 1 |
| Polyuria/polydipsia | 1 |
| Ataxia | 1 |
| Behaviour change | 1 |
Fourteen dogs lived in the same household as one of the 30 confirmed CRGV cases. Of these 14 dogs, two developed skin lesions and AKI and six developed skin lesions without AKI (n=8). Thirteen of these 14 dogs were not part of the study population and the information on these dogs was obtained by questioning owners. The eight dogs became unwell between 20 days before and six days after the confirmed CRGV case that they lived with. All eight dogs were related to a confirmed CRGV case and/or each other.
Clinicopathological findings
Selected haematology, serum biochemistry, urinalysis and systolic blood pressure measurement results for the 30 dogs are presented in Table 2, with further detail of clinicopathological abnormalities presented in Table 3. Seven dogs demonstrated normocytic, normochromic anaemia at presentation, with a further eight dogs becoming anaemic after presentation. Absolute reticulocyte count was only available for two dogs which were anaemic at presentation and one dog subsequently. The anaemia was pre- or non-regenerative (median reticulocyte count 22.58×109/l). Blood smear examination was performed in 13 dogs and revealed schistocytes, burr cells and/or acanthocytes in five dogs and was unremarkable in the remainder. Fifteen dogs were thrombocytopaenic at presentation and four became thrombocytopaenic.
TABLE 2:
Selected data for the 30 confirmed cases
| At presentation | Last available result | ||||
|---|---|---|---|---|---|
| Parameter | Median | Range | Median | Range | Reference interval |
| Haematocrit (%) | 43.9 (n=28) | 26.0–65.3 | 34.3 (n=23) | 7.7–55.8 | 37–55% |
| Platelet count (×109/l) | 78 (n=26) | 1–401 | 50 (n=20) | 9–411 | 175–500×109/l |
| Neutrophil count (×109/l) | 11.6 (n=27) | 5.19–37.90 | 10.8 (n=20) | 4.49–33.9 | 2.8–10.5×109/l |
| Urea (mmol/l) | 46.4 (n=30) | 3.6–85.1 | 48.19 (n=25) | 17.3–113.8 | 2.0–9.0 mmol/l |
| Creatinine (µmol/l) | 406.5 (n=30) | 71–900 | 527.0 (n=25) | 209.0–1171.0 | 40–106 µmol/l (13 dogs) 44–159 µmol/l (16 dogs) |
| Phosphate (mmol/l) | 3.12 (n=26) | 1.28–6.20 | 3.54 (n=19) | 2.01–5.50 | 0.8–1.6 mmol/l (14 dogs) 0.81–2.20 mmol/l (12 dogs) |
| ALT (U/L) | 119 (n=25) | 48–950 | 92 (n=21) | 39–1260 | 0–25 U/L (10 dogs) 10–100 U/L (15 dogs) |
| ALKP (U/L) | 91.5 (n=28) | 16–650 | 63 (n=23) | 16–1395 | 0–50 U/L (11 dogs) 23–212 U/L (17 dogs) |
| Total bilirubin (µmol/l) | 12.0 (n=27) | 0–338 | 11.3 (n=18) | 5.0–640.0 | 0–15 µmol/l |
| AST (U/L) | 76.5 (n=6) | 51–473 | 112 (n=5) | 57–1179 | 0–49 U/L |
| CK (U/L) | 206 (n=8) | 112–881 | 235 (n=7) | 106–963 | 0–190 U/L |
| Albumin (g/l) | 27 (n=27) | 14–36 | 23 (n=23) | 14–34 | 26–40 g/l |
| Globulin (g/l) | 33 (n=25) | 22–58 | 25 (n=15) | 18–47 | 20–47 g/l |
| Sodium (mmol/l) | 144 (n=18) | 139–152 | 147 (n=15) | 136–157 | 139–154 mmol/l |
| Potassium (mmol/l) | 4.2 (n=18) | 2.8–5.3 | 4.5 (n=15) | 2.6–6.7 | 3.5–5.8 mmol/l |
| Prothrombin time (seconds) | 14 (n=8) | 4–19 | No further results available | 12–17 seconds | |
| Activated partial thromboplastin time (seconds) | 96.5 (n=8) | 12–143 | No further results available | 71–102 seconds | |
| Urine specific gravity | 1.020 (n=16) | 1.005–>1.050 | No further results available | ||
| Urine protein: creatinine ratio | 5.6 (n=11) | 1.35–16.58 | No further results available | <0.5 | |
| Systolic blood pressure (mmHg) | 176 (n=11) | 102–280 | 174 (n=9) | 110–290 | 100–150 mmHg |
TABLE 3:
Frequency of clinicopathological abnormalities
| Results at presentation | Results for additional patients identified as developing the abnormality during hospitalisation | ||||||
|---|---|---|---|---|---|---|---|
| Abnormality | Number of patients | Median | Range | Number of patients | Median | Range | Reference interval |
| Anaemia | 7/28 | 30.2 | 24.0–33.2 | 8 | 31.1 | 7.7–35.1 | 37–55% |
| Thrombocytopaenia | 15/26 | 46 | 1–81 | 4 | 49 | 9–162 | 175–500×109/l |
| Elevated serum urea concentration | 28/30 | 46.4 | 12.1–85.1 | 2 | 37.7 | 25.4–50.0 | 2.0–9.0 mmol/l |
| Elevated serum creatinine concentration | 26/30 | 476 | 155–900 | 4 | 494.5 | 352–671 | (40–106 µmol/l 13 dogs; 44–159 µmol/l, 16 dogs) |
| Hyperbilirubinaemia | 9/27 | 27 | 16–338 | 4 | 55 | 21–640 | 0–15 µmol/l |
| Hypoalbuminaemia | 10/27 | 23.5 | 14–25 | 9 | 24 | 17–25 | 26–40 g/l |
| Hypertension | 8/11 | 181 | 102–280 | 1 | 162 | 162 | 100–150 mmHg |
At presentation, 26 dogs were azotaemic. The non-azotaemic dogs became azotaemic after initial presentation (less than 24 hours to six days later). Basal cortisol was measured in eight dogs and excluded glucocorticoid deficient hypoadrenocorticism in all. Clotting times, measured in eight dogs, were not consistent with disseminated intravascular coagulation (DIC). Six dogs had canine-specific pancreatic lipase immunoreactivity measured (Idexx snap test n=4; quantitative cPLi n=2) and all had abnormal results (680 and above 1000 µg/l—reference range less than 200 µg/l).v
Urine dipstick and sediment examination was performed in 17 dogs revealing: haemoglobinuria or myoglobinuria (n=16), proteinuria (n=11, see Table 2) and glucosuria (n=6). Sediment examination revealed casts in nine dogs: granular (n=5), fatty (n=1), hyaline (n=2) and not described (n=1). Urine culture was negative in 11 of 12 dogs (faecal contaminants were cultured from the remaining case). Urine toxicology was negative in five of six dogs tested (Carmichael Torrance Veterinary Diagnostic Laboratory). Pentaethylene glycol (trace) was detected in one dog.
At presentation, nine dogs were oliguric, two were anuric and seven had normal urine output. Urine output was unknown in 13 dogs. International Renal Interest Society (IRIS) AKI grading at presentation was: grade I (n=3), II (n=4), III (n=8), IV (n=14) and V (n=1) (www.iris-kidney.com, 2013).
Abdominal ultrasonography (performed by a European diploma holder in Diagnostic Imaging in 11 dogs and a general practice veterinary surgeon in 2 dogs) revealed no evidence for chronic kidney disease (CKD) or pyelectasia (n=13). The kidneys appeared unremarkable in eight dogs and the remaining five had bilateral hyperechoic renal cortices. Three dogs had possible evidence for gastritis (thickened hypoechoic gastric rugal folds n=1; thickened hyperechoic rugal folds n=1; reduced gastric wall layer definition n=1); one dog had hyperechoic small intestinal mucosal striations and thickening and unevenness of the colonic mucosa which may have suggested enterocolitis. One additional dog had evidence for hepatopathy (hypoechoic hepatic parenchyma with cuffing of the portal veins). No other relevant abnormalities were identified on abdominal ultrasonography.
Leptospirosis microscopic agglutination testing (MAT) was performed in 15 cases. Ten had negative titres, obtained a median of three days (1–8 days) after the development of systemic signs. Five dogs had positive titres; their results and the results of additional leptospirosis testing are summarised in Table 4. FISH for Leptospires was performed on renal tissue from seven dogs and liver tissue from one dog.vi A positive result was obtained from six renal samples; Leptospires were seen in small localised clusters in three dogs (one of whom had a negative MAT titre) and diffusely throughout the renal tissue in three dogs (one of whom was not tested for Leptospirosis by MAT). The remaining results were negative. Leptospirosis PCR was performed on the renal tissue of three of the dogs with positive FISH results; one dog had a negative result and one had a positive result; one dog had PCR performed at two laboratoriesvi vii and discordant results were obtained. Leptospirosis PCR was performed on liver tissue from one dogvi and the result was negative.
TABLE 4:
Summary of Leptospirosis test results for the 5 dogs with positive Leptospira serology
| Case | Serovar for which positive result was obtained | Titre | Time (in months) since administration of last leptospirosis vaccine (canicola, icterohaemorrhagiae) | Timing of serology postdevelopment of skin lesions (days) | Timing of serology postdevelopment of systemic signs (days) | PCR on urine | PCR on blood | PCR on renal tissue*† | FISH result* | Previous anti-biotics? |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 |
L. bratislava L. australis |
1:400 1:100 |
7 | 6 | 2 | Negative | Negative | Not performed | Positive on renal tissue, diffuse | No |
| 2 |
L. copenhageni L. canicola L. icterohaemorrhagiae |
1:800 1:100 1:200 |
10 | 5 | 1 | Not performed | Not performed | Not performed | Positive on renal tissue, diffuse | Yes |
| 3 |
L. canicola L. copenhageni |
1:100 1:100 |
8 | 6 | 2 | Not performed | Not performed | Positive* Negative† |
Positive on renal tissue, clusters | Yes |
| 4 |
L. autumnalis L. icterohaemorrhagiae L. copenhageni L. bratislava |
1:400 1:100 1:100 1:100 |
7 | 2 | 2 | Negative | Not performed | Negative† Nega tive on liver tissue also* |
Not performed on renal tissue Negative on liver tissue |
Yes |
| 5 | Not specified | +ve combined IgG | 2 | 5 | Same day | Not performed | Not performed | Positive* | Positive, clusters | Yes |
*University of Bristol Veterinary Diagnostics
†Idexx Laboratories
FISH, fluorescence in situ hybridisation
Four dogs were tested for Dog Circovirus via PCR on splenic tissue, three via PCR on peripheral EDTA blood and six via FISH on renal tissue and all results were negative. Viral metagenomics was performed on renal tissue from two dogs; and on liver, spleen and lymph node from one of those dogs. No match was identified between viral nucleic acids enriched from those samples to known viruses.
Borrelia PCR (n=5) and Borrelia serology (n=2) results were negative. Renal heavy metal concentrations (lead, arsenic and cadmium) were measured in two dogs (Animal Health and Veterinary Laboratories Agency, Winchester) and were below reported reference intervals in both. Routine aerobic and anaerobic bacterial culture was performed on renal tissue from three dogs and results were negative.
Faecal culture, performed in seven dogs, yielded E. coli. PCRs for E. coli virulence genes (eaeA, stx 1 and 2, LT1 and ST1 and 2) were negative in all seven, providing no evidence for infection with enteropathogenic E. coli, verotoxigenic E. coli or enterotoxigenic E. coli.
Skin lesion cultures, performed in 11 dogs, were positive in 7, yielding Staphylococcus intermedius (n=1), Staphylococcus aureus (n=1), coagulase positive Staphylococcus (n=1), non-haemolytic Streptococcus (n=1), β haemolytic Streptococcus (n=1), Enterococcus (n=1), E. coli (n=3), Pseudomonas aeruginosa and Corynebacterium (n=1). Three dogs cultured more than one bacterium. Blood culture was performed in one dog and was negative.
Histopathology
Full post mortem examination was performed in five dogs by pathologists with a Diploma of the American or European College of Veterinary Pathologists, or equivalent. Tissue samples for histopathology were obtained post mortem by the case veterinarians in the remaining 25 cases. Renal histopathology was available for all 30 dogs and skin histopathology for 24 dogs. The most prominent histological changes were noted in the kidney and skin. For the kidney, the most striking changes involved the glomeruli, with frequent fibrinoid necrosis of glomerular arterioles, characterised by distortion of vessel walls with an eosinophilic, hyalinised, smudgy material, intermingled with low numbers of degenerate and viable neutrophils, fragmented red blood cells and mild amounts of karyorrhectic debris (Fig 4). Frequent vessels were occluded by thrombi. The majority of the glomeruli were affected and for individual glomeruli these changes ranged from mild and segmental to global and severe. Also, frequent glomerular tufts were congested and partially occluded by haemorrhage. Increased cellularity of the glomerular tufts consistent with endothelial cell hypertrophy and swelling was identified in 17 cases. Fibrinoid necrosis of intralobular and arcuate arteries was occasionally observed (Fig 4). Twenty-nine dogs had concurrent evidence of tubular necrosis, ranging from mild to marked, often with concurrent evidence of tubular restitution. In affected kidneys, micro-organisms, viral cytopathic effects and metazoan parasites were not identified. When performed, Warthin-Starry stains did not reveal argyrophilic organisms (Leptospires) within the tissue sections.
FIG 4:
Photomicrographs of a glomerulus and an intralobular artery from a dog with CRGV, stained with haematoxylin and eosin [H&E] (a and c) and Masson's trichrome (b and d). There is fibrinoid vascular necrosis (asterisks) of intralobular arteries and arterioles. Glomerular capillaries are severely distended and contain red blood cells, many of which are fragmented. Distension of glomerular capillaries is due to dissolution of the mesangial matrix (mesangiolysis). Tubules are undergoing degeneration and necrosis; most tubules contain protein casts whereas some contain red blood cell casts.
In the skin samples, the epidermis was focally to diffusely ulcerated. The subjacent dermis was often undergoing coagulative necrosis. At the level of the adnexa, the hair follicles had reduced to absent sebaceous glands, reduced cellularity and were separated by increased fibrous tissue and an attenuated follicular epithelium. The affected follicles were often bordered by variable numbers of neutrophils, foamy macrophages and karyorrhectic debris (Fig 5); this often obscured the follicular epithelium interface and sebaceous gland units. In most cases, the deep dermis and subcutis were thickened by a layer of maturing fibrovascular tissue. Occasionally this fibrovascular tissue replaced portions of the adnexa. In a few cases (n=6), fibrinoid necrosis was observed in the small dermal arterioles (Fig 6). Rarely, thrombi were identified in such vessels. In one case, similar necro-ulcerative changes were identified in skin from the lip. In samples from the oral cavity lesions, similar ulceration of the mucosa was observed with associated necrosis, inflammation and fibrovascular change of the submucosa.
FIG 5:
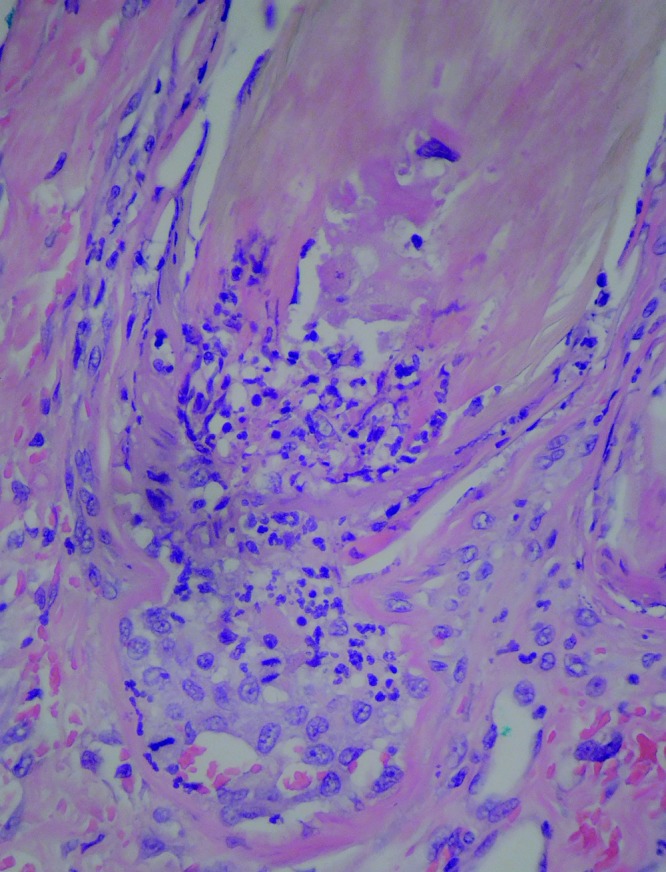
Photomicrograph of a necrotic hair follicle with neutrophilic infiltrates
FIG 6:
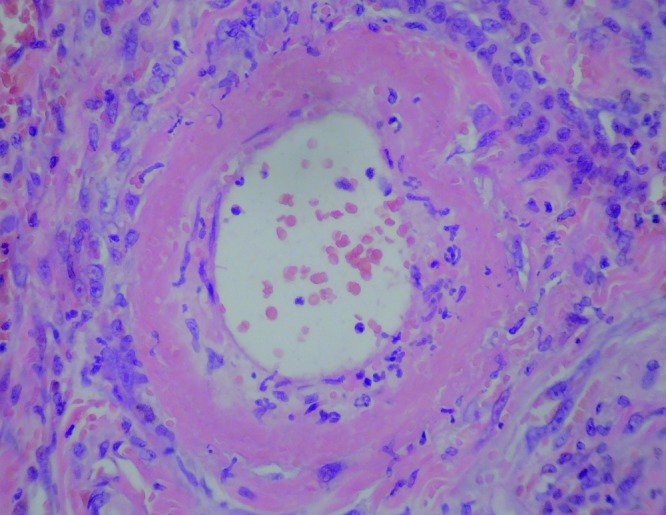
Photomicrograph of a small dermal artery with fibrinoid necrosis of the vessel wall
The majority of other tissues evaluated (stomach, n=2; small intestine, n=6; colon, n=2; liver, n=14; pancreas, n=4; heart, n=2; spleen, n=9; lung, n=1; brain, n=1; eye, n=1; salivary gland, n=1; urinary bladder, n=3; tongue, n=2; soft palate, n=1; bone marrow, n=2; adrenal gland, n=2; tonsil, n=1; skeletal muscle, n=1 and lymph node, n=2) appeared unremarkable, but occasionally exhibited mild, non-specific changes (see online supplementary appendix 1).
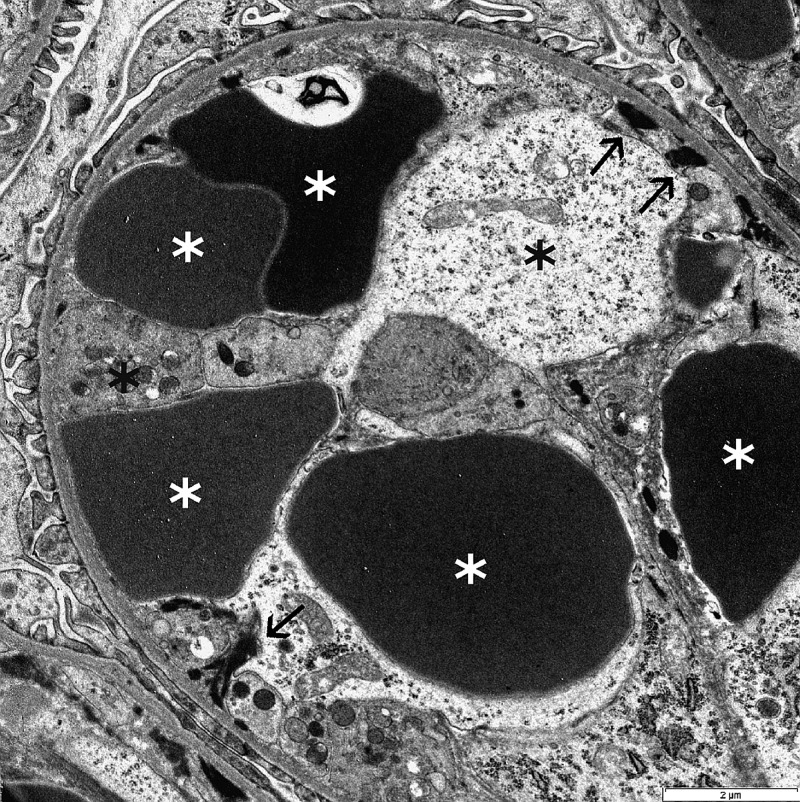
Electron microscopy was performed in three dogs and revealed distension of the glomerular capillary loops by erythrocytes, occasional schistocytes and rare polymorphonuclear cells. Endothelial cells, when identifiable, were severely swollen. Podocyte foot processes were globally effaced. Occasionally, mesangiolysis (dissolution of mesangium) was noted. Immune complexes were not identified. Immunostaining was negative for IgG, IgM, IgA, C3, C1q, kappa light chain (KLC) and lambda light chain (LLC) (Fig 7).
FIG 7:
Electron micrograph of a glomerular capillary loop from a dog with cutaneous and renal glomerular vasculopathy (CRGV). There are multiple deformed red blood cells (white asterisks) and swollen endothelial cells (black asterisks). A few small aggregates of fibrin tactoids are present at the periphery of the capillary loop (arrows)
Renal tissue from two dogs was submitted to two separate laboratories with both laboratories receiving both samples (Department of Medical Microbiology and Immunology, School of Medicine, University of California, Davis, USA; University of Bristol Veterinary Diagnostics, School of Veterinary Sciences, University of Bristol, Langford, Bristol, UK) for evaluation with a broad spectrum set of 16S rRNA-directed probes (to detect bacterial genetic material). From one laboratory, a clear 16S band was identified in the tissue of one dog and a faint band in the other. Staphylococcaceae were identified in both samples. The other laboratory identified solely Leptospires in both samples.
PCR for verotoxin 1 and 2, performed on the kidneys from four dogs, gave negative results. FISH for shiga toxin, performed on the kidneys from six dogs, was also negative.
Management
Ten cases were managed at referral centres and 20 in primary practice. Initial management typically consisted of intravenous fluid therapy (n=26) and antibiotic therapy (n=26) and is summarised in Table 5. Ten cases were managed with an indwelling urinary catheter for measurement of urine output. Three cases underwent continuous renal replacement therapy.
TABLE 5:
Summary of case management
| Treatment | Number of cases |
|---|---|
| Antibiotics | |
| Amoxicillin-clavulanate | 21 |
| Marbofloxacin | 4 |
| Enrofloxacin | 4 |
| Cefalexin | 2 |
| Clindamycin | 1 |
| Metronidazole | 1 |
| Pradofloxacin | 1 |
| Cefuroxime | 1 |
| >1 antibiotic | 5 |
| No antibiotic | 3 |
| Not recorded | 1 |
| Route of antibiotic administration | |
| Intravenous | 15 |
| Oral | 3 |
| Subcutaneous | 8 |
| Other medications | |
| Corticosteroids (anti-inflammatory dose) | 7 |
| Corticosteroids (immunosuppressive dose) | 1 |
| Amlodipine | 2 |
| Furosemide | 16 |
| Mannitol | 6 |
| Dopamine | 1 |
| Pentoxyfilline | 1 |
| Blood products | |
| Whole blood | 1 |
| Packed red cells | 1 |
| Fresh frozen plasma | 1 |
| CRRT | 3 |
CRRT, continuous renal replacement therapy
Outcome
Twenty-four dogs died, or were euthanised, solely due to their disease and six were euthanised at the owners’ request. IRIS AKI grade progressed in 10 dogs, reduced in 2 and was unchanged in 12. Terminally, IRIS grades were: II (n=1), III (n=8), IV (n=13), V (n=3) and unknown (n=5). Causes of death/euthanasia were: oligoanuria (n=9), anaemia and thrombocytopaenia (n=2), progressive azotaemia (n=6), unspecified clinical deterioration (n=3), suspected DIC (n=1), dyspnoea (n=1), collapse (n=1), ascites (n=1) and owners’ request due to concurrent disease(s), financial constraints or concern regarding prognosis (n=6). Median time from onset of clinical signs to death or euthanasia was seven days (1–16 days).
Discussion
CRGV has been recognised in the USA for almost 30 years (Carpenter and others 1988), but has only sporadically been reported in individual dogs elsewhere. This is the first case series of dogs with CRGV in the UK.
Most of the dogs in this case series were initially evaluated at their primary practice for a skin lesion (or lesions) which was considered consistent with pyoderma, pododermatitis, a bite/sting, or a wound. Systemic signs developed a median of four days later, but some dogs were unwell concurrently. Initial investigations revealed renal azotaemia attributable to AKI. Pre-renal causes were excluded via assessment of urine specific gravity, lack of response to intravenous fluid therapy and exclusion of hypoadrenocorticism. Abdominal imaging, where available, was used to exclude post-renal causes. CKD was excluded via a combination of clinical history and imaging findings. Eleven of the dogs (36.7 per cent) received NSAIDs before the diagnosis of AKI; although it is possible that their use exacerbated AKI, the histopathologic lesions were not consistent with NSAIDs being the sole cause of the AKI.
Other known causes of AKI were explored as thoroughly as possible in most of the dogs. Leptospirosis, which can cause similar clinical and laboratory signs to those seen in this case series (Rentko and others 1992, Birnbaum and others 1998, Greene and others 2006, Sykes and others 2011), was further investigated with serology, PCR on peripheral blood, renal and hepatic tissue, and FISH on renal and hepatic tissue. The five dogs with positive Leptospirosis titres (1:100–1:800) had been vaccinated less than 1 year before testing and although vaccinal titres often decline by four months post-vaccination, they can sometimes persist for longer (Sykes and others 2011) leading to false-positive results. Additionally, only single titres above 1:1600 are considered significant for indicating infection in vaccinated dogs (Tangeman and Littman 2013), whereas the positive titre results obtained in the five dogs in this study were relatively low. It is possible that the titres would have been higher if MAT testing had not been performed so early in the disease process. Only 55 per cent of dogs with leptospirosis were diagnosed by a single MAT titre obtained within 72 hours of initial presentation in one study (Tangeman and Littman 2013). Convalescent phase samples could not, however, be obtained in the dogs in this study given the short survival time.
In cases of acute leptospirosis, histopathology often reveals mild renal tubular necrosis and interstitial oedema (Greene and others 2006) with focal areas of hepatic necrosis characterised by cellular disassociation of the hepatic cords (Van den Ingh and others 2006). This contrasts with the histopathological findings in this case series; no typical hepatic lesions were identified and the predominant renal lesion was TMA. Acute to peracute, periacinar hepatocellular loss with associated haemorrhage was observed in one dog in this series. This raised concern for leptospirosis, however, this case exhibited fibrinoid necrosis of small portal vessels, and consequently the periacinar changes may also have represented ischaemic change associated with the fibrinoid necrosis. In addition, both PCR and FISH on paraffin embedded sections of the affected liver were negative for Leptospira sp., making acute leptospirosis less likely. There was no evidence of argyrophilic Leptospires with silver staining, although this technique can fail to identify Leptospires during acute leptospirosis (Greene and others 2006). With the exception of calcinosis cutis, which was not identified in any dog in this series, skin lesions have not previously been reported in association with canine leptospirosis (Munday and others 2005).
FISH and PCR detected Leptospires in the renal tissues of some of the CRGV affected dogs reported in this series; however, this does not confirm clinical infection, as some dogs are asymptomatic maintenance hosts for Leptospires (Monahan and others 2009). Although a causal relationship between leptospirosis and CRGV cannot be fully excluded, the low number of positive leptospirosis test results in this case series was felt unlikely to support a diagnosis of acute leptospirosis as the clinical picture, outcome and histopathological findings differed significantly from those previously reported with acute leptospirosis.
Histopathologically, AKI in the dogs in this case series was found to be attributable to TMA. A search of the International Veterinary Renal Pathology Service database of more than 1000 renal biopsies from small animals, revealed TMA to account for below 1 per cent of all diagnoses reached (Cianciolo R, unpublished data). TMAs are characterised by inflammation and damage to vascular endothelium, leading to widespread formation of microthrombi, consumptive thrombocytopaenia, microangiopathic haemolytic anaemia and multiorgan dysfunction (Noris and others 2012). Five cases in this series (38.5 per cent of dogs in whom a blood smear was examined) had evidence for burr cells, schistocytes or acanthocytes; additionally 19 dogs were thrombocytopaenic and 13 dogs were hyperbilirubinaemic by the time of death. All of these findings can be the result of microangiopathy (Rebar and others 1981, Ruggenenti and others 2001); however, other mechanisms could also have been contributing to the anaemia, thrombocytopaenia and hyperbilirubinaemia.
Known differential diagnoses for canine TMA include CRGV (Carpenter and others 1988) and haemolytic uraemic syndrome (HUS). HUS has previously been reported in five dogs (Holloway and others 1993, Chantrey and others 2002, Dell'Orco and others 2005), three cats (Aronson and Gregory 1999) and a number of other species (Morris and others 1987, Roby and others 1987, Garcia and others 2002, Dickinson and others 2008). CRGV has been almost exclusively reported in greyhounds (Carpenter and others 1988, Hendricks 2000), although there is one report of an affected Great Dane (Rotermund and others 2002). In contrast, HUS in dogs has been reported in a variety of breeds: Yorkshire terrier, miniature poodle, Labrador retriever, German shepherd dog and boxer (Holloway and others 1993, Chantrey and others 2002, Dell'Orco and others 2005). Similarly, many breeds were represented in this case series. It is unclear at this time whether canine HUS and CRGV are truly two distinct disease processes. Dogs with CRGV typically present with acute onset skin lesions affecting the distal limbs; kidney injury and haematological abnormalities are variably reported (Carpenter and others 1988). In contrast skin lesions have not previously been reported in dogs with HUS (Holloway and others 1993, Chantrey and others 2002, Dell'Orco and others 2005). The proportion of dogs in the UK that develop CRGV without developing AKI is unknown at this stage; however, 42.9 per cent of dogs in contact with those reported in this study, developed skin lesions without biochemical evidence of AKI and it would have been interesting to review dermal and renal histopathology in these dogs had it been available. Previous reports indicate that non-azotaemic dogs with CRGV tend to have reduced glomerular filtration rates and renal histopathology showing mild, multifocal, endothelial glomerular changes (Hertzke and others 1995, Cowan and others 1997).
Clinicopathologic findings previously reported in dogs with CRGV include anaemia, thrombocytopaenia, azotaemia, high serum liver enzyme activity, high muscle enzyme activity, haematuria, proteinuria and poorly concentrated urine (Carpenter and others 1988, Cowan and others 1997), similar to the abnormalities identified in the dogs in this case series. Previous reports have not further classified the anaemia (Carpenter and others 1988, Cowan and others 1997). In this case series the anaemia appeared pre- or non-regenerative and the former was considered most likely. Possible aetiologies considered included gastrointestinal haemorrhage secondary to uraemia or microangiopathic red cell injury. Hypoalbuminaemia (identified in 63.3 per cent of the confirmed cases in this series) may support gastrointestinal haemorrhage, without excluding other possible causes.
Histopathological findings previously reported with CRGV (Carpenter and others 1988, Hertzke and others 1995) correlate with those seen in this case series. The majority of the skin lesions in this case series, as in previous reports of CRGV, involved the distal extremities. This could be attributable to the increased number of smaller calibre vessels in this location and an increased propensity to infarction.
Microscopic lesions in abdominal organs other than the kidneys in dogs with CRGV were reported as being consistent with uraemia and hypovolaemia in one report (Carpenter and others 1988). Hyalinisation and rare thrombi were identified in the submucosa of the stomach, and small and large intestine in another report (Hertzke and others 1995). Fibrinoid necrosis of smaller vessels was identified in this case series but thrombi were not identified in abdominal organs other than the kidney.
Glomerular ultrastructural changes previously reported with CRGV (Hertzke and others 1995) were similar to the changes identified in this case series. Immune complexes, complement and immunoglobulins have not previously been identified in the kidneys of dogs affected by CRGV (Carpenter and others 1988, Hertzke and others 1995) and were not identified in this population of UK dogs.
As discussed, canine TMAs can be the result of CRGV or HUS, which may represent two variants of the same disease with the same aetiology, or which may be two separate diseases. The most common form of HUS in human beings, termed STEC-HUS or D+HUS, is associated with E. coli or Shigella dysenteriae shiga toxin (Uchida and others 1999, Noris and others 2012, Salvadori and Bertoni 2013). Co-infection with Salmonella or Campylobacter may also be important (Ardissino and others 2014a). STEC-HUS typically starts with watery, then haemorrhagic, diarrhoea followed by thrombocytopaenia, haemolysis and azotaemia (Tarr and others 2005, Salvadori and Bertoni 2013). STEC-HUS appears a median of seven days after the onset of diarrhoea (Tarr and others 2005). In this case series, a diarrhoeic prodrome was only reported in four dogs; however, if owners were not specifically questioned about prodromal diarrhoea, this information may have been missed. In contrast, four of the five dogs previously reported with HUS had diarrhoeic prodromes (Holloway and others 1993, Dell'Orco and others 2005).
E. coli shiga toxin has not been identified in dogs with HUS (Holloway and others 1993, Chantrey and others 2002, Dell'Orco and others 2005) or CRGV (Rotermund and others 2002). Shiga toxin has been identified in one horse (Dickinson and others 2008) and two of three rabbits previously reported with HUS (Garcia and others 2002). Shiga toxin producing E. coli, Salmonella and Campylobacter were not identified in the faeces or kidneys of dogs in this study. Reasons for failing to identify toxin, or causative bacteria, may have included previous antibiotic administration, inappropriate sample handling or late collection of samples. In human beings, recovery of toxin-producing E. coli is highly dependent upon faecal culture being performed within six days of the onset of diarrhoea (Tarr and others 1990).
In one case series of 18 dogs with CRGV in the USA, seasonality was reported as early winter and early summer (Cowan and others 1997); in this case series, dogs presented over winter and early spring. In contrast, STEC-HUS in people is more commonly reported in the summer (Milford and others 1990, Boyce and others 1995). Seasonality of canine HUS has not been reported (Holloway and others 1993). Any potential seasonal distribution of CRGV may become apparent with time, provided disease surveillance continues.
Human STEC-HUS tends to occur either sporadically or in small geographical clusters (Milford and others 1990, Tarr and others 2005, Salvadori and Bertoni 2013), which may be similar to the findings in this case series and epidemiological investigations are ongoing. Although cases were reported from across the north and south of England, 36.7 per cent came from The New Forest, Hampshire. This high percentage could, however, be attributed to the geographical location of the primary investigators in Hampshire and increased awareness amongst local veterinarians.
In people, genetic or acquired conditions causing complement dysregulation can cause another TMA, known as atypical HUS (aHUS) (Noris and others 2012). Skin lesions have been reported alongside haemolysis and AKI with aHUS (which is not the case with STEC-HUS), but the incidence is rare (Ardissino and others 2014b). Even in patients with multiple genetic defects, aHUS may not develop until adulthood and an environmental trigger is considered likely for the development of disease (Salvadori and Bertoni 2013). Atypical HUS has not been reported in dogs; however, CRGV may bear some resemblance to this disease, especially given the concurrent findings of skin lesions and AKI identified in both diseases. An infectious or environmental trigger for CRGV may be suspected, given the number of in-contact dogs in this case series that developed skin lesions with or without AKI. It was also interesting to note that all of the affected in-contact dogs were related either to each other and/or to a confirmed case.
Dog Circovirus has recently been isolated from the tissues of dogs with vascular and granulomatous disease of unknown origin (Li and others 2013); however, a viral aetiology was considered unlikely in this case series: PCR, FISH and viral metagenomics (performed in an effort to detect any encapsulated virus potentially present in kidney tissue) results were negative, and histopathologically there was no evidence of viral cytopathic effect (cytoplasmic inclusion bodies) in any of the tissues examined. Negative results for viral metagenomics do not completely exclude a viral aetiology, however. The results could indicate that virus was present in low copy number, or that the virus was too remotely related to known viruses used for sequence alignment, or that the sample used was too autolysed to preserve the virus.
The significance of the Staphylococcaceae detected by 16S rRNA-directed probe in two dogs in this case series is unclear but, contamination with commensal skin bacteria is considered more likely than disease-causing infection, as the kidneys were not kept sterile before the DNA extraction phase. The negative urine and renal tissue culture results obtained support this hypothesis.
It is currently unknown if CRGV is a novel canine disease or if it is a variant of HUS, aHUS or indeed one of the other TMA's reported in man. These include ‘HUS of unknown aetiology’ and thrombotic thrombocytopaenic purpura (TTP) (Noris and others 2012). Evaluation of the canine complement system may provide further information regarding the aetiology of CRGV.
Management of human TMA's is dependent upon the underlying cause. Plasma therapy, antibiotic administration, monoclonal shiga toxin antibodies and renal transplantation have all been used in STEC-HUS. A recombinant, anti-C5 antibody (eculizumab) is the treatment of choice for human aHUS (Kavanagh and others 2013, Salvadori and Bertoni 2013) but the cost has prohibited its evaluation in dogs. Plasma exchange remains the treatment of choice for human TTP (Blombery and Scully 2014) and is a useful therapy for aHUS (Kavanagh and others 2013). Monoclonal antibody therapy to CD20 and classical immunosuppressive drug therapy have also been reported for management of human TTP (Blombery and Scully 2014). One dog with CRGV was reportedly ineffectively managed with immunosuppressive therapy (Rotermund and others 2002). The efficacy of plasma therapy and monoclonal antibody therapy has yet to be evaluated in CRGV.
Case selection bias could have been introduced in this case series. Fifty one of the 53 practices involved identified cases based on their awareness of CRGV and the presenting signs. Cases may have been missed in these practices without comprehensive searching of computerised record systems. The actual number of dogs affected by CRGV may therefore be higher than reported in this case series.
Six surviving dogs were strongly suspected, by the authors, to be suffering from CRGV. Renal histopathology was not available to confirm the diagnosis as, invasive procedures, like renal biopsy in patients with AKI showing apparent improvement to symptomatic management, are considered clinically difficult to justify. This may suggest that CRGV is not an invariably fatal disease.
Conclusion
CRGV is a TMA of unknown aetiology which, when azotaemia develops, currently appears to carry a grave prognosis. Vasculopathy, preferentially affecting the small vessels of the skin and kidneys in dogs, as identified in this case series, appears to be unique to CRGV and has not, to the authors’ knowledge, been reported associated with any other canine disease. Although this case series provides useful initial information about CRGV in the UK, the retrospective multicentre nature of the study is a limitation. Continued detailed clinical, clinicopathological and epidemiological evaluation will further enhance the understanding of the disease and will hopefully help to identify possible triggers, define prognostic indicators and determine the most appropriate management for these patients. The question remains as to whether this is an emerging disease or, one that was previously present but unrecognised.
Supplementary Material
Acknowledgments
The authors would like to thank the following veterinary surgeons: Roger Stobbs BVSc, MRCVS; Monica Augusto DVM CertSAM DipECVIM-CA MRCVS; Aran Mas DVM DipECVIM-CA MRCVS; Fabio Procoli DMV, MVetMed, DACVIM, DECVIM-CA, MRCVS; Stephen C B Perkins BVSc, BSc, MRCVS; Louise Ketteridge BVetMed, MRCVS; Ken C Smith BVM&S, PhD, FHEA, FRCPath, MRCVS; Norelene T Harrington BSc Vet Path, MVB, MVetMed, DipACVP, MRCVS; Nicholas G A Woodger BVetMed, BSc, MRCVS; Clare James BVSc, BSc, DipACVP, MRCVS; Kerstin Baiker Dr med vet, DVM, DiplECVP; Kerstin Erles DrMedVet, FRCPath, MRCVS; Stefanie B Gobelli Dr med vet, FVH; Isabelle Brodard; Darren J Lucas VetMB, MA, MRCVS; Edward M Roberts BVetMed, MRCVS; Roisin Dickinson BVetMed, MRCVS; Tara C Zilic BVetMed, MRCVS; Louise C Melling BVetMed, MRCVS; and Kobus Engelbrecht BVSc, MRCVS along with all of the other veterinary surgeons who very kindly submitted clinical records and samples for histopathology to Anderson Moores Veterinary Specialists. The authors would also like to thank owners of affected dogs, owners that returned questionnaires, and the New Forest District Council, Forestry Commission, New Forest Dog Owners Group and Anderson Moores Veterinary Specialists who provided funding for diagnostic testing. The authors would also like to thank Dr Paul S Bass BSc MD FRCPath for his valuable insights regarding the renal histopathology.
Footnotes
University of Bristol Veterinary Diagnostics, School of Veterinary Sciences, University of Bristol, Langford, Bristol BS40 5DU, UK.
Pesavento Research Group, University of California, Davis, School of Veterinary Medicine, 1 Shields Avenue, Davis, CA 95616, USA.
Center for Zoonotic Diseases, Bacterial Diseases, and Antimicrobial Resistance, Institute for Veterinary Bacteriology, University of Bern, Hochschulstrasse 4, Bern CH-3012, Switzerland.
Batt Lab, University of Warwick Science Park, The Venture Centre, Sir William Lyons Road, Coventry CV4 7EZ, UK.
Dogs were seen at numerous different veterinary practices using multiple laboratories. Biochemistry reference ranges were therefore variable.
University of Bristol Veterinary Diagnostics.
Idexx Laboratories.
References
- ARDISSINO G. POSSENTI I. SALARDI S. TEL F. COLOMBO E. TESTA S. DAPRAI L. PICICCO D. COLOMBO R. M. & TORRESANI E. (2014a) Co-infection in children with bloody diarrhea caused by Shigatoxin-producing Escherichia coli: data of the North Italian HUS network. Journal of Paediatric Gastroenterology and Nutrition 59, 218–220 10.1097/MPG.0000000000000420 [DOI] [PubMed] [Google Scholar]
- ARDISSINO G. TEL F. TESTA S. MARZANO A. V. LAZZARI R. SALARDI S. & EDEFONTI A. (2014b) Skin involvement in atypical hemolytic uremic syndrome. American Journal of Kidney Disease 63, 652–655 10.1053/j.ajkd.2013.09.020 [DOI] [PubMed] [Google Scholar]
- ARONSON L. R. & GREGORY C. (1999) Possible hemolytic uremic syndrome in three cats after renal transplantation and cyclosporine therapy. Veterinary Surgery 28, 135–140 10.1053/jvet.1999.0135 [DOI] [PubMed] [Google Scholar]
- BIRNBAUM N. BARR S. C. CENTER S. A. SCHERMERHORN T. RANDOLPH J. F. & SIMPSON K. W. (1998) Naturally acquired Leptospirosis in 36 dogs: serological and clinicopathological features. Journal of Small Animal Practice 39, 231–236 10.1111/j.1748-5827.1998.tb03640.x [DOI] [PubMed] [Google Scholar]
- BLOMBERY P. & SCULLY M. (2014) Management of thrombotic thrombocytopenic purpura: current perspectives. Journal of Blood Medicine 5, 15–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- BOURHY P. BREMONT S. ZININI F. GIRY C. & PICARDEAU M. (2011) Comparison of real-time PCR assays for detection of pathogenic Leptospira spp. in blood and identification of variations in target sequences. Journal of Clinical Microbiology 49, 2154–2160 10.1128/JCM.02452-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- BOYCE T. G. SWERDLOW D. L. & GRIFFIN P. M. (1995) Escherichia coli 0157:H7 and the hemolytic-uremic syndrome. New England Journal of Medicine 333, 364–368 10.1056/NEJM199508103330608 [DOI] [PubMed] [Google Scholar]
- BURNENS A. P. FREY A. LIOR H. & NICOLET J. (1995) Prevalence and clinical significance of vero-cytotoxin-producing Escherichia coli (VTEC) isolated from cattle in herds with and without calf diarrhoea. Zentralblatt fur Veterinarmedizin (Journal of Veterinary Medicine) series B 42, 311–318 [DOI] [PubMed] [Google Scholar]
- CARPENTER J. L. ANDELMAN N. C. MOORE F. M. & KING N. W. Jr (1988) Idiopathic cutaneous and renal glomerular vasculopathy of greyhounds. Veterinary Pathology 25, 401–407 10.1177/030098588802500601 [DOI] [PubMed] [Google Scholar]
- CHANTREY J. CHAPMAN P. S. & PATTERSON-KANE J. C. (2002) Haemolytic-uraemic syndrome in a dog. Journal of Veterinary Medicine Series A 49, 470–472 10.1046/j.1439-0442.2002.00479.x [DOI] [PubMed] [Google Scholar]
- COWAN L. A. HERTZKE D. M. FENWICK B. W. & ANDREASEN C. B. (1997) Clinical and clinicopathologic abnormalities in greyhounds with cutaneous and renal glomerular vasculopathy: 18 cases (1992–1994). Journal of the American Veterinary Medical Association 210, 789–793 [PubMed] [Google Scholar]
- DELL'ORCO M. BERTAZZOLO W. PAGLIARO L. ROCCABIANCA P. & COMAZZI S. (2005) Hemolytic-uremic syndrome in a dog. Veterinary Clinical Pathology 34, 264–269 10.1111/j.1939-165X.2005.tb00052.x [DOI] [PubMed] [Google Scholar]
- DICKINSON C. E. GOULD D. H. DAVIDSON A. H. AVERY P. R. LEGARE M. E. HYATT D. R. & DEBROY C. (2008) Hemolytic-uremic syndrome in a postpartum mare concurrent with encephalopathy in the neonatal foal. Journal of Veterinary Diagnostic Investigation 20, 239–242 10.1177/104063870802000218 [DOI] [PubMed] [Google Scholar]
- EUBIG P. A. BRADY M. S. KHAN S. A. MAZZAFERRO E. M. & MORROW C. M. K. (2005) Acute renal failure in dogs after the ingestion of grapes or raisins: a retrospective evaluation of 43 dogs (1992–2002). Journal of Veterinary Internal Medicine 19, 663–674 [DOI] [PubMed] [Google Scholar]
- FERRER L. RABANAL R. FONDEVILA D. RAMOS J. A. & DOMINGO M. (1988) Skin lesions in canine leishmaniasis. Journal of Small Animal Practice 29, 381–388 10.1111/j.1748-5827.1988.tb02298.x [DOI] [Google Scholar]
- FISCHER J. R. LANE I. F. & STOKES J. (2009) Acute postrenal azotaemia: etiology, clinicopathology, and pathophysiology. Compendium: Continuing Education for Veterinarians 31, 520–530 [PubMed] [Google Scholar]
- FOURNEL C. CHABANNE L. CAUX C. FAURE J. R. RIGAL D. MAGNOL J. P. & MONIER J. C. (1992) Canine systemic lupus erythematosus. I: a study of 75 cases. Lupus 1, 133–139 10.1177/096120339200100303 [DOI] [PubMed] [Google Scholar]
- GARCIA A. MARINI R. P. FENG Y. VITSKY A. KNOX K. A. TAYLOR N. S. SCAUER D. B. & FOX J. G. (2002) A naturally occurring rabbit model of enterohemorrhagic Escherichia coli-induced disease. Journal of Infectious Diseases 186, 1682–1686 10.1086/345371 [DOI] [PubMed] [Google Scholar]
- GOLDFARB S. & ADLER S. H. (2001) Acute renal failure: pathophysiology and treatment. Nephrology 4, 1–12 [Google Scholar]
- GREENE C. E. SYKES J. E. BROWN C. A. & HARTMAN K. (2006) Leptospirosis. In Infectious Diseases of the Dog and Cat. 3rd edn Ed. Greene C. E. Saunders Elsevier Inc; Chapter 44 pp 402–417 [Google Scholar]
- HENDRICKS A. (2000) Akute Ulzerative Dermatitis Bei Einem Greyhound. Proceedings of the 46th Annual Congress of the Small Animal Veterinary Association, Dusseldorf, Germany: pp 62–63 [Google Scholar]
- HERTZKE D. M. COWAN L. A. SCHONING P. & FENWICK B. W. (1995) Glomerular Ultrastructural Lesions of Idiopathic Cutaneous and Renal Glomerular Vasculopathy of Greyhounds. Veterinary Pathology 32, 451–459 10.1177/030098589503200501 [DOI] [PubMed] [Google Scholar]
- HOLLOWAY S. SENIOR D. ROTH L. & TISHER C. C. (1993) Hemolytic uremic syndrome in dogs. Journal of Veterinary Internal Medicine 7, 220–227 10.1111/j.1939-1676.1993.tb01011.x [DOI] [PubMed] [Google Scholar]
- KAVANAGH D. GOODSHIP T. H. & RICHARDS A. (2013) Atypical hemolytic uremic syndrome. Seminars in Nephrology 33, 508–530 10.1016/j.semnephrol.2013.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LI L. MCGRAW S. ZHU K. LEUTENEGGER C. M. MARKS S. L. KUBISKI S. GAFFNEY P. DELA CRUZ F. N. Jr WANG C. DELWART E. & PESAVENTO P. A. (2013) Circovirus in tissues of dogs with vasculitis and hemorrhage. Emerging Infectious Diseases 19, 534–541 10.3201/eid1904.121390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MILFORD D. V. TAYLOR C. M. GUTTRIDGE B. HALL S. M. ROWE B. & KLEANTHOUS H. (1990) Haemolytic uraemic syndromes in the British Isles 1985–8: association with Verocytotoxin producing Escherichia coli. Part 1: clinical and epidemiological aspects. Archives of Disease in Childhood 65, 716–721 10.1136/adc.65.7.716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MONAHAN A. M. CALLANAN J. J. & NALLY J. E. (2009) Review paper: host-pathogen interactions in the kidney during chronic leptospirosis. Veterinary Pathology 46, 792–799 10.1354/vp.08-VP-0265-N-REV [DOI] [PubMed] [Google Scholar]
- MOORE P. F. OLIVRY T. & NAYDAN D. (1994) Canine cutaneous epitheliotrophic lymphoma (mycosis fungoides) is a proliferative disorder of CD8+ T cells. American Journal of Pathology 144, 421–429 [PMC free article] [PubMed] [Google Scholar]
- MORRIS C. F. ROBERTSON J. L. MANN P. C. CLARK S. & DIVERS T. J. (1987) Hemolytic uremic-like syndrome in two horses. Journal of the American Veterinary Medical Association 191, 1453–1454 [PubMed] [Google Scholar]
- MUNDAY J. S. BERGEN D. J. & ROE W. D. (2005) Generalised calcinosis cutis associated with probable leptospirosis in a dog. Veterinary Dermatology 16, 401–406 10.1111/j.1365-3164.2005.00476.x [DOI] [PubMed] [Google Scholar]
- NORIS M. MESCIA F. & REMUZZI G. (2012) STEC-HUS, atypical HUS and TTP are all diseases of complement activation. Nature Reviews Nephrology 8, 622–633 10.1038/nrneph.2012.195 [DOI] [PubMed] [Google Scholar]
- PASS M. A. ODEDRA R. & BATT R. M. (2000) Multiplex PCRs for identification of Escherichia coli virulence genes. Journal of Clinical Microbiology 38, 2001–2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- REBAR A. H. LEWIS H. B. DENICOLA D. B. HALLIWELL W. H. & BOON G. D. (1981) Red cell fragmentation in the dog: an editorial review. Veterinary Pathology 18, 415–426 [DOI] [PubMed] [Google Scholar]
- RENTKO V. T. CLARK N. ROSS L. A. & SCHELLING S. H. (1992) Canine leptospirosis. A retrospective study of 17 cases. Journal of Veterinary Internal Medicine 6, 235–244 10.1111/j.1939-1676.1992.tb00345.x [DOI] [PubMed] [Google Scholar]
- ROBY K. A. W. BLOOM J. C. & BECHT J. L. (1987) Postpartum hemolytic-uremic syndrome in a cow. Journal of the American Veterinary Medical Association 190, 187–190 [PubMed] [Google Scholar]
- ROTERMUND A. PETERS M. HEWICKER-TRAUTWEIN M. & NOLTE I. (2002) Cutaneous and renal glomerular vasculopathy in a Great Dane resembling ‘Alabama rot’ of greyhounds. Veterinary Record 151, 510–512 10.1136/vr.151.17.510 [DOI] [PubMed] [Google Scholar]
- RUGGENENTI P. NORIS M. & REMUZZI G. (2001) Thrombotic microangiopathy, hemolytic uremic syndrome, and thrombotic thrombocytopenic purpura. Kidney International 60, 831–846 10.1046/j.1523-1755.2001.060003831.x [DOI] [PubMed] [Google Scholar]
- SALVADORI M. & BERTONI E. (2013) Update on hemolytic uremic syndrome: diagnostic and therapeutic recommendations. World Journal of Nephrology 2, 56–76 10.5527/wjn.v2.i3.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SYKES J. E. HARTMANN K. LUNN K. F. MOORE G. E. STODDARD R. A. & GOLDSTEIN R. E. (2011) 2010 ACVIM Small animal consensus statement on leptospirosis: diagnosis, epidemiology, treatment and prevention. Journal of Veterinary Internal Medicine 25, 1–13 10.1111/j.1939-1676.2010.0654.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- TANGEMAN L. E. & LITTMAN M. P. (2013) Clinicopathologic and atypical features of naturally occurring leptospirosis in dogs: 51 cases (2000–2010). Journal of the American Veterinary Medical Association 243, 1316–1322 10.2460/javma.243.9.1316 [DOI] [PubMed] [Google Scholar]
- TARR P. I. GORDON C. A. & CHANDLER W. L. (2005) Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet 365, 1073–1086 [DOI] [PubMed] [Google Scholar]
- TARR P. I. NEILL M. A. CLAUSEN C. R. WATKINS S. L. CHRISTIE D. L. & HICKMAN R. O. (1990) Escherichia coli 0157:H7 and the hemolytic uremic syndrome: importance of early cultures in establishing the etiology. Journal of Infectious Diseases 162, 553–556 10.1093/infdis/162.2.553 [DOI] [PubMed] [Google Scholar]
- UCHIDA H. KIYOKAWA N. HORIE H. FUJIMOTO J. & TAKEDA T. (1999) The detection of shiga toxins in the kidney of a patient with hemolytic uremic syndrome. Pediatric Research 45, 133–137 10.1203/00006450-199901000-00022 [DOI] [PubMed] [Google Scholar]
- VAN DEN INGH T. S. G. A. M., VAN WINKLE T., CULLEN J M., CHARLES J A. & DESMET V. J. (2006). Morphological Classification of Parenchymal Disorders of the Canine and Feline Liver. In: ROTHUIZEN J., BUNCH S. E., CHARLES J. A., et al. Chronic Hepatitis. WSAVA Standards for Clinical and Histological Diagnosis of Canine and Feline Liver Diseases. Philadelphia PA: Saunders Elsevier Ltd. Chapter 7. pp, 93-95. [Google Scholar]
- VAN DEN INGH T. S. G. A. M. VAN WINKLE T. CULLEN J. M. CHARLES J. A. & DESMET V. J. (2006) Morphological classification of parenchymal disorders of the canine and feline liver. WSAVA Standards for Clinical and Histological Diagnosis of Canine and Feline Liver Diseases 93–95 [Google Scholar]
- VICTORIA J. G. KAPOOR A. LI L. BLINKOVA O. SLIKAS B. & WANG C. (2009) Metagenomic analyses of viruses in stool samples from children with acute flaccid paralysis. Journal of Virology 83, 4642–4651 10.1128/JVI.02301-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WAIKAR S. S. LIU K. D. & CHERTOW G. M. (2008) Diagnosis, epidemiology and outcomes of acute kidney injury. Clinical Journal of the American Society of Nephrology 3, 844–861 10.2215/CJN.05191107 [DOI] [PubMed] [Google Scholar]
- WALKER D. & MCMAHON L. (2013) Acute kidney injury in dogs. Veterinary Record 172, 296 10.1136/vr.f1638 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.