Abstract
Background
Data on risk associated with 24-hour ambulatory diastolic (DBP24) versus systolic (SBP24) blood pressure are scarce.
Methods and Results
We recorded 24-hour blood pressure and health outcomes in 8341 untreated people (mean age, 50.8 years; 46.6% women) randomly recruited from 12 populations. We computed hazard ratios (HRs) using multivariable-adjusted Cox regression. Over 11.2 years (median), 927 (11.1%) participants died, 356 (4.3%) from cardiovascular causes, and 744 (8.9%) experienced a fatal or nonfatal cardiovascular event. Isolated diastolic hypertension (DBP24≥80 mm Hg) did not increase the risk of total mortality, cardiovascular mortality, or stroke (HRs≤1.54; P≥0.18), but was associated with a higher risk of fatal combined with nonfatal cardiovascular, cardiac, or coronary events (HRs≥1.75; P≤0.0054). Isolated systolic hypertension (SBP24≥130 mm Hg) and mixed diastolic plus systolic hypertension were associated with increased risks of all aforementioned end points (P≤0.0012). Below age 50, DBP24 was the main driver of risk, reaching significance for total (HR for 1-SD increase, 2.05; P=0.0039) and cardiovascular mortality (HR, 4.07; P=0.0032) and for all cardiovascular end points combined (HR, 1.74; P=0.039) with a nonsignificant contribution of SBP24 (HR≤0.92; P≥0.068); above age 50, SBP24 predicted all end points (HR≥1.19; P≤0.0002) with a nonsignificant contribution of DBP24 (0.96≤HR≤1.14; P≥0.10). The interactions of age with SBP24 and DBP24 were significant for all cardiovascular and coronary events (P≤0.043).
Conclusions
The risks conferred by DBP24 and SBP24 are age dependent. DBP24 and isolated diastolic hypertension drive coronary complications below age 50, whereas above age 50 SBP24 and isolated systolic and mixed hypertension are the predominant risk factors.
Keywords: ambulatory blood pressure monitoring, blood pressure component, cardiovascular diseases, population
Hypertension remains the predominant driver of cardiovascular disease. In 2001, hypertension caused 8 million deaths worldwide, representing 14% of global mortality.1 In an individual-subject meta-analysis of close to 1 million people, the risk of coronary heart disease and stroke gradually increased with blood pressure from levels as low as 115 mm Hg systolic and 75 mm Hg diastolic.2 The Framingham investigators3,4 and other researchers5 showed in studies published as early as 1971 that diastolic pressure was the strongest predictor of coronary heart disease below age 50 with an increase in the importance of systolic blood pressure with advancing age.
Using blood pressure levels of 140 mm Hg systolic and 90 mm Hg diastolic, current guidelines subdivide hypertension on conventional sphygmomanometry into isolated diastolic, isolated systolic, and diastolic combined with systolic (mixed) hypertension.6 Several population studies have demonstrated that isolated diastolic hypertension confers a cardiovascular risk that was intermediate between normotension and isolated systolic or mixed hypertension.7,8 Compared with conventional sphygmomanometry, ambulatory blood pressure monitoring substantially refines risk stratification.9 To our knowledge, no previous study has assessed the risks associated with isolated diastolic, isolated systolic, and mixed hypertension on 24-hour ambulatory monitoring or examined the age dependency of 24-hour diastolic and systolic ambulatory blood pressure as independent risk factors in the general population. We addressed these issues by analyzing the International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes (IDACO).10
Methods
Study Population
At the time of writing this report, the IDACO database10 included 12 randomly recruited population cohorts11–20 and 12 711 participants with available data on the conventional and ambulatory blood pressure. All participants gave informed written consent. We excluded participants if they were younger than 18 years (n=303), if they were taking antihypertensive drugs at baseline (n=2144), or if they had <10 daytime or 5 nighttime blood pressure readings (n=1923). Thus, the number of subjects included in the present analysis totaled 8341. (for details, see the Expanded Methods and Table I in the online-only Data Supplement).
Blood Pressure Measurement
Methods used for conventional and ambulatory blood pressure measurement are described in detail in the Expanded Methods in the online-only Data Supplement. Conventional blood pressure was the average of 2 consecutive readings. Portable monitors were programmed to obtain ambulatory blood pressure readings at 30-minute intervals throughout the whole day,12,19 or at intervals ranging from 1511,17,18 to 3012,19 minutes during daytime and from 3011,12,17–19 to 6014 minutes at night. To categorize levels of the ambulatory blood pressure, we followed the guidelines of the European Societies of Cardiology and Hypertension.6 Ambulatory hypertension was a 24-hour level of ≥130 mm Hg systolic or ≥80 mm Hg diastolic. Using these thresholds, we categorized participants as being normotensive, or as having isolated diastolic, isolated systolic, or mixed hypertension on 24-hour ambulatory monitoring.
Other Measurements
We used the questionnaires originally administered in each cohort to obtain information on each participant’s medical history and smoking and drinking habits. Body mass index was body weight in kilograms divided by height in meters squared. We measured serum cholesterol and blood glucose by automated enzymatic methods. Diabetes mellitus was the use of antidiabetic drugs, a fasting glucose of ≥7.0 mmol/L,21 a random glucose of ≥11.1 mmol/L,21 a self-reported diagnosis, or diabetes mellitus documented in practice or hospital records.
Ascertainment of Events
We ascertained vital status and the incidence of fatal and nonfatal diseases from the appropriate sources in each country, as described in previous publications.10,22 In most cohorts,11–18 information on vital status was obtained, even if participants dropped out from follow-up. Outcomes were coded according to the international classification of diseases, as described in the Expanded Methods in the online-only Data Supplement. Fatal and nonfatal stroke did not include transient ischemic attacks. Coronary events encompassed death from ischemic heart disease, sudden death, nonfatal myocardial infarction, and coronary revascularization. Cardiac events comprised coronary end points and fatal and nonfatal heart failure. Hospitalizations for unstable angina were coded as ischemic heart disease. In the Danish11 and Swedish14 cohorts, the diagnosis of heart failure required admission to hospital. In the other cohorts,12,13,15–20 heart failure was either a clinical diagnosis or the diagnosis on the death certificate, but in all cases it was validated against hospital files or the records held by family doctors. The composite cardiovascular end point included all aforementioned end points plus cardiovascular mortality. In analyses of fatal combined with nonfatal outcomes, we only considered the first event within each disease cluster.
Statistical Analysis
For database management and statistical analysis, we used SAS software, version 9.3 (SAS Institute, Cary, NC). Missing data were imputed using cohort- and sex-specific regression equations with age as explanatory variable (for details, see the Expanded Methods and Table II in the online-only Data Supplement). We tabulated the incidence of end points by blood pressure status on ambulatory measurement. We computed 95% confidence intervals (CIs) of rates as R±1.96 × √(R/T), where R and T are the rate and the denominator used to calculate the rate. We compared means and rates using the large-sample z test and proportions by the χ2 statistic, respectively. We plotted the incidence of end points across categories of the ambulatory blood pressure, using Cox models standardized to the sex distribution and mean age in the whole study population. We compared hazard ratios (HRs) between categories of the ambulatory blood pressure using the Wald χ2 statistic.
In multivariable-adjusted Cox regression analyses, we accounted for cohort, sex, age, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, and diabetes mellitus. To adjust for cohort, we pooled participants recruited in the European Project on Genes in Hypertension (Kraków, Novosibirsk, Padova, and Pilsen).18 We ascertained that the proportional hazard assumption was fulfilled by testing the interaction between blood pressure and follow-up time. We compared hazard ratios between subgroups according to age, sex, or ethnicity, using the appropriate interaction terms. To assess the prognostic significance of diastolic blood pressure at different levels of systolic blood pressure, and vice versa, we modeled the 10-year absolute risk of a composite cardiovascular end point using Cox regression, while standardizing to the average of the distributions in the whole study population (mean or ratio) of cohort, sex, age, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, and diabetes mellitus. Statistical significance was a α-level <0.05 on 2-sided tests.
Results
Baseline Characteristics
The 8341 participants included 5489 Europeans (65.8%), 1280 Asians (15.3%), and 1572 South Americans (18.9%), and 3888 women (46.6%). Age ranged from 18 to 94 years and averaged (±SD) 50.8±15.8 years. At enrollment, 2474 participants (29.7%) were smokers and 4061 (48.7%) reported intake of alcohol. In the whole study population, conventional blood pressure averaged (±SD) 128.7±21.4 mm Hg systolic and 78.6±11.3 mm Hg diastolic, whereas the 24-hour ambulatory blood pressure was 122.1±13.5 mm Hg systolic and 73.1±8.2 mm Hg diastolic.
Table 1 shows the participants’ baseline characteristics by categories of the 24-hour ambulatory blood pressure. Normotensive participants and patients with isolated diastolic hypertension had similar characteristics except for the proportion of women (52.6 versus 36.5%) and drinkers (45.0 versus 54.4%), and body mass index (24.5 versus 25.9 kg/m2) and serum cholesterol (5.48 versus 5.67 mmol/L). Patients with mixed or isolated systolic hypertension were older, more obese, had higher serum cholesterol and blood glucose levels, and were more likely to be diabetic than those with isolated diastolic hypertension (Table 1). The proportions of isolated diastolic, isolated systolic, and mixed hypertension were 5.9%, 3.9%, and 6.1%, respectively, among younger participants (aged <50 years), whereas the corresponding frequencies were 4.1%, 16.3%, and 18.4% among older adults (aged ≥50 years).
Table 1.
Baseline Characteristics of Participants by Categories of 24-Hour Ambulatory Blood Pressure
| Characteristic | Normotension | Isolated Diastolic Hypertension | Mixed Hypertension | Isolated Systolic Hypertension |
|---|---|---|---|---|
| Number of subjects | 5969 | 408 | 1071 | 893 |
| European, (%) | 3908 (65.5)‡ | 221 (54.2) | 720 (67.2)‡ | 640 (71.7)‡ |
| Asian, (%) | 983 (16.5) | 55 (13.5) | 140 (13.1) | 102 (11.4) |
| South American, (%) | 1078 (18.1)‡ | 132 (32.4) | 211 (19.7)‡ | 151 (16.9)‡ |
| Women, (%) | 3141 (52.6)‡ | 149 (36.5) | 315 (29.4)† | 283 (31.7) |
| Smokers, (%) | 1741 (29.2) | 132 (32.4) | 348 (32.5) | 253 (28.3) |
| Drinking alcohol, (%) | 2684 (45.0)‡ | 222 (54.4) | 652 (60.9)† | 503 (56.3) |
| Diabetes mellitus, (%) | 266 (4.5) | 23 (5.6) | 89 (8.3) | 92 (10.3)† |
| Cardiovascular disorders, (%) | 243 (4.1) | 23 (5.6) | 59 (5.5) | 67 (7.5) |
| Mean characteristic (SD) | ||||
| Age, y | 47.9 (15.7) | 48.7 (11.4) | 58.0 (12.0)‡ | 62.3 (13.8)‡ |
| Body mass index, kg/m2 | 24.5 (3.9)‡ | 25.9 (4.2) | 26.6 (4.2)† | 26.5 (4.4)* |
| Conventional blood pressure | ||||
| Systolic, mm Hg | 121.7 (16.3) | 131.5 (13.2) | 151.3 (22.8) | 146.8 (22.8) |
| Diastolic, mm Hg | 75.1 (9.3) | 86.6 (8.2) | 92.0 (10.9) | 82.0 (10.3) |
| 24-hour blood pressure | ||||
| Systolic, mm Hg | 115.7 (7.9) | 124.5 (4.0) | 143.6 (11.4) | 137.6 (7.8) |
| Diastolic, mm Hg | 69.6 (5.3) | 82.9 (2.7) | 87.2 (6.0) | 74.5 (4.1) |
| Blood glucose, mmol/L | 5.03 (1.17) | 5.11 (1.25) | 5.44 (1.66)† | 5.45 (1.64)† |
| Serum cholesterol, mmol/L | 5.48 (1.13)† | 5.67 (1.13) | 5.78 (1.14) | 5.86 (1.14)† |
Hypertension was a 24-hour ambulatory blood pressure ≥130 mm Hg or 80 mm Hg diastolic. Mixed hypertension refers to diastolic combined with systolic hypertension. Significance of the difference with isolated diastolic hypertension:
P≤0.05;
P≤0.01; and
P≤0.001. Significance levels were not calculated for blood pressure values, used to categorize participants.
Incidence of Events
In the whole study population, median follow-up was 11.2 years (5th to 95th percentile interval, 2.5 –18.2). Across cohorts, median follow-up ranged from 2.5 years (2.3–2.6) in Jingning to 17.2 years (5.3–20.4) in Noorderkempen. During 92 379 person-years of follow-up, 927 participants died (10.0 per 1000 person-years) and 744 experienced a fatal or nonfatal cardiovascular event (8.25 per 1000 person-years). Mortality included 356 cardiovascular and 548 non-cardiovascular deaths and 23 deaths from unknown cause. Considering cause-specific first cardiovascular events, the incidence of fatal and nonfatal stroke amounted to 78 and 203, respectively. Cardiac events consisted of 216 fatal and 425 nonfatal events, including 90 fatal and 141 nonfatal cases of acute myocardial infarction, 122 deaths from ischemic heart disease, 56 sudden deaths, 37 fatal and 140 nonfatal cases of heart failure, and 71 cases of surgical or percutaneous coronary revascularization.
Risk by Categories of Ambulatory Blood Pressure
Median years of follow-up (5th to 95th percentile interval) amounted to 11.4 (2.6–18.3), 9.7 (2.4–18.2), 11.0 (2.7–17.3), and 10.8 (2.5–17.8) in normotensive individuals and in patients with isolated diastolic, isolated systolic, and mixed hypertension, respectively. Table 2 shows that the incidence rates were similar (P≥0.13) in normotensive participants and in patients with isolated diastolic hypertension except for cardiac end points (3.1 versus 5.9 events per 1000 person-years; P=0.021) and coronary events (2.2 versus 4.6 events per 1000 person-years; P=0.024). Compared with isolated diastolic hypertension, event rates were higher (P<0.001) in patients with mixed or isolated systolic hypertension. After standardization to the sex distribution (46.6% women) and mean age (50.8 years) in the whole study population, the incidence of a composite cardiovascular end point gradually increased from normotension, over isolated diastolic hypertension onto isolated systolic and mixed hypertension (Figure 1). Detailed information on the number of participants at risk, those retained in the analysis, and those with a cardiovascular (Table III in the online-only Data Supplement) or cardiac (Table IV in the online-only Data Supplement) end point is available by 2-year intervals in the online Data Supplement.
Table 2.
Incidence of End Points by Categories of 24-Hour Ambulatory Blood Pressure
| End Point | Normotension | Isolated Diastolic Hypertension | Mixed Hypertension | Isolated Systolic Hypertension |
|---|---|---|---|---|
| Number of participants | 5969 | 408 | 1071 | 893 |
| Total mortality | ||||
| Number of deaths | 493 | 25 | 204 | 205 |
| Rate | 7.3 (6.6–7.9) | 6.0 (3.6–8.3) | 18.3 (15.8–20.8)‡ | 22.0 (19.0–25.0)‡ |
| Cardiovascular mortality | ||||
| Number of deaths | 151 | 11 | 101 | 93 |
| Rate | 2.2 (1.9–2.6) | 2.6 (1.1–4.2) | 9.1 (7.3–10.8)‡ | 10.0 (7.9–12.0)‡ |
| Noncardiovascular mortality | ||||
| Number of deaths | 328 | 14 | 100 | 106 |
| Rate | 4.8 (4.3–5.4) | 3.4 (1.6–5.1) | 9.0 (7.2–10.7)‡ | 11.4 (9.2–13.5)‡ |
| All cardiovascular events | ||||
| Number of events | 329 | 28 | 200 | 187 |
| Rate | 4.9 (4.4–5.5) | 6.8 (4.3–9.4) | 18.9 (16.3–21.5)‡ | 21.1 (18.1–24.1)‡ |
| Cardiac events | ||||
| Number of events | 211 | 24 | 124 | 118 |
| Rate | 3.1 (2.7–3.6)* | 5.9 (3.5–8.2) | 11.5 (9.5–13.5)‡ | 13.1 (10.7–15.4)‡ |
| Coronary events | ||||
| Number of events | 151 | 19 | 91 | 87 |
| Rate | 2.2 (1.9–2.6)* | 4.6 (2.5–6.7) | 8.3 (6.6–10.0)‡ | 9.5 (7.5–11.5)‡ |
| Stroke | ||||
| Number of events | 106 | 5 | 76 | 69 |
| Rate | 1.6 (1.3–1.9) | 1.2 (0.1–2.3) | 7.0 (5.4–8.6)‡ | 7.6 (5.8–9.3)‡ |
Hypertension was a 24-hour ambulatory blood pressure ≥130 mm Hg systolic or 80 mm Hg diastolic. Incidence rates reflect the number of events per 1000 person-years. Significance of the difference with isolated diastolic hypertension:
P≤0.05; and
P≤0.001.
Figure 1.
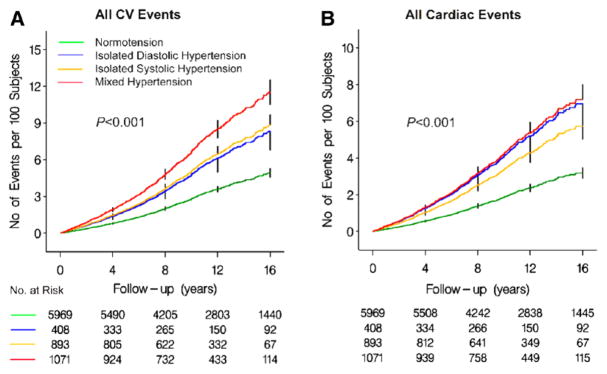
Incidence of the composite cardiovascular (CV) end point (A) and fatal combined with nonfatal cardiac events (B) in 4 categories of the ambulatory blood pressure. Incidence was standardized to the sex distribution (46.6% women) and mean age (50.8 years) in the whole study population. For each blood pressure category, the number of subjects at risk is given at the beginning of each 4-year interval. The time axis was curtailed at 16 years when ≈10% of participants were still being followed up. Tables III and IV in the online-only Data Supplement provide more detailed information by 2-year intervals up to 22 years on the number of participants at risk, the number of events, and the number of participants no longer followed up. Vertical bars denote the standard error. P values are for the differences across the 4 blood pressure categories.
In further multivariable-adjusted analyses with normotension as reference (Table 3), isolated diastolic hypertension did not increase the risk of total and cardiovascular mortality or stroke (HRs ≤1.54; P≥0.18), but was associated with a higher risk of a composite cardiovascular end point and of fatal combined with nonfatal cardiac and coronary events (HRs ≥1.75; P≤0.0054). With normotension as reference, both mixed and isolated systolic hypertension were associated with an increased risk of all end points under study (P≤0.0012) with the exception of noncardiovascular mortality (P≥0.096). The HRs were significantly higher (P≤0.046) in patients with mixed hypertension than in those with isolated systolic hypertension, except for fatal combined with nonfatal cardiac (P=0.065) and coronary events (P=0.17).
Table 3.
Multivariable-Adjusted Hazard Ratios Associated With Isolated Diastolic, Isolated Systolic, and Mixed Ambulatory Hypertension
| End Point (Number of End Points) | Isolated Diastolic Hypertension | P | Mixed Hypertension | P | Isolated Systolic Hypertension | P |
|---|---|---|---|---|---|---|
| Mortality | ||||||
| Total (927) | 1.14 (0.76–1.71) | 0.54 | 1.63 (1.37–1.93) | <0.0001 | 1.33 (1.12–1.57) | 0.0012 |
| Cardiovascular (356) | 1.54 (0.82–2.87) | 0.18 | 2.49 (1.91–3.25) | <0.0001 | 1.86 (1.42–2.44) | <0.0001 |
| Noncardiovascular (548) | 1.00 (0.58–1.72) | 0.99 | 1.22 (0.97–1.53) | 0.096 | 1.05 (0.84–1.32) | 0.66 |
| Fatal and nonfatal events combined | ||||||
| All cardiovascular (744) | 1.75 (1.18–2.59) | 0.0054 | 2.44 (2.03–2.93) | <0.0001 | 1.81 (1.50–2.19) | <0.0001 |
| Cardiac (477) | 1.96 (1.28–3.01) | 0.0022 | 2.16 (1.72–2.73) | <0.0001 | 1.70 (1.34–2.16) | <0.0001 |
| Coronary (348) | 2.00 (1.23–3.25) | 0.0052 | 2.19 (1.67–2.87) | <0.0001 | 1.77 (1.34–2.35) | <0.0001 |
| Stroke (256) | 1.33 (0.53–3.33) | 0.54 | 3.06 (2.25–4.16) | <0.0001 | 2.13 (1.55–2.92) | <0.0001 |
Ambulatory normotension is the referent group. All models were adjusted for cohort, sex, age, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, and diabetes mellitus. The cause of death was unknown in 23 cases.
Risks Associated with Diastolic and Systolic Blood Pressures
In line with previous publications based on the conventionally measured blood pressure,4–6 we stratified our multivariable-adjusted analyses by age group (<50 and ≥50 years, Table 4). Median years of follow-up (5th to 95th percentile interval) amounted to 12.1 (2.5–18.6) and 11.1 (2.6–17.6) in younger and older participants, respectively. In younger participants, in fully adjusted models, which included both diastolic and systolic blood pressure, diastolic blood pressure predicted total (HR for 1-SD increase, 2.05; P=0.0039) and cardiovascular mortality (HR, 4.07; P=0.0032) and the composite cardiovascular end point (HR, 1.74; P=0.039), whereas 24-hour systolic blood pressure was not significantly associated with these end points (HR, ≤0.92; P≥0.068; Table 4). In older participants, systolic pressure predicted total and cardiovascular mortality and all of the end points combining fatal with nonfatal events (HR, ≥1.19; P≤0.0002), whereas diastolic pressure did not significantly predict any outcome (0.96≤HR≤1.14; P≥0.10). Analyses based on daytime (Table V in the online-only Data Supplement) or nighttime (Table VI in the online-only Data Supplement) blood pressure, or restricted to the 7949 subjects free of cardiovascular disease at baseline (Table VII in the online-only Data Supplement), or excluding 1 cohort at a time (Table VIII in the online-only Data Supplement), confirmed the results given in Table 4. Compared with the conventional blood pressure, 24-hour diastolic and systolic pressure retained their predictive superiority in all participants (Table IX in the online-only Data Supplement) as well as in categories based on blood pressure status on conventional measurement (online-only Data Supplement, pages 5–6).
Table 4.
Multivariable-Adjusted Standardized Hazard Ratios for 24-Hour Systolic and Diastolic Blood Pressures by Age Group
| End Point | <50 years (n=3761)
|
≥50 years (n=4580)
|
|||||
|---|---|---|---|---|---|---|---|
| n | Diastolic Pressure | Systolic Pressure | n | Diastolic Pressure | Systolic Pressure | ||
| Mortality | |||||||
| Total | A | 64 | 1.38 (1.08–1.77)† | 1.20 (0.86–1.66) | 863 | 1.17 (1.10–1.25)‡ | 1.21 (1.14–1.29)‡ |
| FA | 2.05 (1.26–3.33)† | 0.56 (0.30–1.05) | 1.03 (0.94–1.13) | 1.19 (1.08–1.30)‡ | |||
| Cardiovascular | A | 16 | 2.34 (1.61–3.39)‡ | 2.23 (1.32–3.78)† | 340 | 1.31 (1.18–1.44)‡ | 1.47 (1.35–1.61)‡ |
| FA | 4.07 (1.60–10.4)† | 0.44 (0.13–1.56) | 0.96 (0.85–1.10) | 1.51 (1.34–1.70)‡ | |||
| Noncardiovascular | A | 46 | 1.13 (0.83–1.55) | 0.93 (0.61–1.42) | 502 | 1.06 (0.97–1.16) | 1.03 (0.94–1.12) |
| FA | 1.73 (0.96–3.12) | 0.53 (0.25–1.13) | 1.09 (0.95–1.25) | 0.96 (0.84–1.10) | |||
| Fatal plus nonfatal events | |||||||
| All cardiovascular | A | 47 | 1.65 (1.27–2.14)‡ | 1.68 (1.19–2.36)† | 697 | 1.36 (1.27–1.46)‡ | 1.44 (1.35–1.53)‡ |
| FA | 1.74 (1.03–2.93)* | 0.92 (0.47–1.81) | 1.06 (0.97–1.17) | 1.39 (1.27–1.51)‡ | |||
| Cardiac | A | 37 | 1.53 (1.12–2.08)† | 1.52 (1.01–2.27)* | 440 | 1.26 (1.16–1.38)‡ | 1.37 (1.26–1.48)‡ |
| FA | 1.67 (0.92–3.03) | 0.88 (0.40–1.90) | 1.01 (0.90–1.14) | 1.36 (1.22–1.52)‡ | |||
| Coronary | A | 28 | 1.63 (1.16–2.30)† | 1.67 (1.07–2.62)* | 320 | 1.25 (1.13–1.38)‡ | 1.35 (1.23–1.48)‡ |
| FA | 1.73 (0.87–3.45) | 0.92 (0.37–2.24) | 1.01 (0.88–1.15) | 1.35 (1.18–1.53)‡ | |||
| Stroke | A | 7 | 2.31 (1.25–4.27)† | 2.43 (1.12–5.26)* | 249 | 1.61 (1.43–1.81)‡ | 1.65 (1.49–1.83)‡ |
| FA | 2.24 (0.62–8.20) | 1.04 (0.21–5.26) | 1.14 (0.97–1.34) | 1.52 (1.32–1.76)‡ | |||
n indicates the number of events. The cause of death was unknown in 23 cases. Hazard ratios, presented with 95% confidence interval, express the risk associated with a 1-SD increase in 24-hour systolic (13.5 mm Hg) or diastolic (8.2 mm Hg) blood pressures. All models were adjusted for cohort, sex, age, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, and diabetes mellitus. Adjusted models (A) include either systolic or diastolic blood pressure, whereas fully adjusted models (FA) include both systolic and diastolic blood pressures in addition to the aforementioned covariables. Significance of the hazard ratios:
P≤0.05;
P≤0.01, and
P≤0.001. The interactions of diastolic and systolic pressure with age (continuous) in fully adjusted models were significant or borderline significant for cardiovascular mortality (0.036≤P≤0.058), all cardiovascular events (0.0037≤P≤0.0048), and coronary events (0.012≤P≤0.043).
Next, based on the data given in Table 4, we tested the interactions of 24-hour systolic and diastolic blood pressures with age, ethnicity, and sex. Using age as a continuous variable, the interaction terms with diastolic and systolic pressure in fully adjusted models were significant or borderline significant for cardiovascular mortality (0.036≤P≤0.058), the composite cardiovascular end point (0.0037≤P≤0.0048), and coronary events (0.012≤P≤0.043). When excluding 1 cohort at a time (Table VIII in the online-only Data Supplement), the interactions with age consistently retained significance for the composite cardiovascular end point (0.0009≤P≤0.050). For cardiovascular mortality and coronary events the interactions of age with systolic and diastolic blood pressure remained formally or borderline significant (0.0079≤P≤0.093), but lost significance for cardiovascular mortality after excluding Ohasama, Jingning, or Noorderkempen (0.12≤P≤0.20) and for coronary events with Montevideo removed (0.10≤P≤0.15). The hazard ratios associated with systolic and diastolic blood pressure were similar in Asians and whites (Table X in the online-only Data Supplement). As reported previously,22 the hazard ratios associated with 24-hour systolic blood pressure were higher in women than men (Table XI in the online-only Data Supplement) for all cardiovascular end points (P≤0.019) with the exception of cardiovascular mortality (P=0.079) and stroke (P=0.64). For 24-hour diastolic blood pressure, the fully adjusted hazard ratios were similar in women and men (P≥0.45).
Finally, we used Cox regression to model the 10-year absolute risk of a composite cardiovascular end point in relation to 24-hour diastolic pressure at different levels of 24-hour systolic pressure and vice versa. Figure 2 shows that the 10-year risk of fatal combined with nonfatal cardiovascular events increased (P<0.001) with 24-hour diastolic pressure irrespective of the level of systolic pressure. Risk also increased with the 24-hour systolic pressure independent of the 24-hour diastolic pressure.
Figure 2.
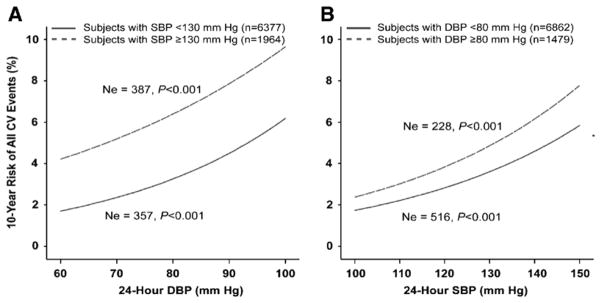
Ten-year absolute risk of a composite cardiovascular (CV) end point associated with 24-hour diastolic blood pressure (DBP, A) and 24-hour systolic blood pressure (SBP, B) in participants with normal (full line) or elevated (dashed line) systolic pressure (A) or normal or elevated diastolic pressure (B) on ambulatory measurement. The cut-off points for 24-hour hypertension were ≥130 mm Hg systolic and ≥80 mm Hg diastolic, respectively. For each risk function, the number (n) of subjects contributing to the risk function is given. In the Cox regression models, 10-year absolute risk was standardized to the average of the distributions in the whole study population (mean or ratio) of cohort, sex, age, body mass index, smoking and drinking, serum cholesterol, history of cardiovascular disease, and diabetes mellitus. Ne indicates the number of events in each group. P values denote the significance of the independent contribution of diastolic pressure (A) or systolic pressure (B).
Discussion
Our analysis included 8341 untreated people randomly recruited from 12 populations and covered on average >11 years of follow-up (median). The key finding was that the risks conferred by diastolic and systolic blood pressure as measured by noninvasive 24-hour ambulatory monitoring were age dependent. Diastolic pressure and isolated diastolic hypertension were the drivers of coronary complications, in particular below age 50 years, whereas above age 50 years systolic pressure and isolated systolic and mixed hypertension became the predominant determinants of risk.
Systolic pressure increases with age until the eighth decade of life.23 By contrast, diastolic pressure rises only until 50 years of age, after which it becomes steady or even slightly decreases.23 In the Framingham Heart Study,3,4 increasing age entailed a shift from diastolic to systolic pressure as the main predictor of cardiovascular risk. Below age 50 years, diastolic pressure was the strongest predictor, whereas the opposite occurred above 50 years of age. Khattar and colleagues used intra-arterial ambulatory blood pressure monitoring in 688 untreated hypertensive patients and obtained similar findings.24 Our current study, based on noninvasive 24-hour ambulatory blood pressure monitoring and the analysis of cause-specific outcomes in general populations, consolidated these findings.
Several studies based on conventional sphygmomanometry25–27 or on the self-measured blood pressure at home28 reported that isolated diastolic hypertension confers low cardiovascular risk, in particular at young age. The Honolulu Heart Program25 reported on 8006 Japanese-American men followed for 20 years. Cutoff levels for diastolic and systolic hypertension were levels of 90 and 160 mm Hg, respectively. For men aged 45 to 54 years, the relative risks compared with normotension were 1.4 (95% CI, 1.0–2.1), 4.3 (2.9–6.3), and 4.8 (2.1–11.0) for isolated diastolic, mixed, and isolated systolic hypertension.25 For men aged 55 to 68 years, the corresponding hazard ratios were 1.8 (1.3–2.5), 1.7 (1.2–2.4), and 1.2 (0.7–2.0), respectively.25 Fang and colleagues26 used the same blood pressure criteria as the Honolulu investigators to categorize systolic and diastolic hypertension in 1560 participants (<60 years) in a worksite hypertension control program. Over 4.5 years of follow-up, 24 participants got a myocardial infarction (3.9 events per 1000 person-years). The rate was higher in the patients with mixed hypertension than in those with isolated diastolic hypertension (5.2 versus 2.2 per 1000 patient-years).26 No myocardial infarction occurred in participants with diastolic hypertension and a systolic blood pressure <140 mm Hg.26 Strandberg and coworkers recruited 3267 initially healthy Finnish men, aged 30 to 45 years, and followed mortality for up to 32 years.27 With normotension as reference (blood pressure <160 mm Hg systolic and <90 mm Hg diastolic), the hazard ratios for mortality were 2.71 (2.00–3.66) in patients with mixed hypertension, but only 1.39 (1.04–1.87) or 1.14 (0.77–1.69) in patients with isolated diastolic hypertension and systolic pressure between 140 and 160 mm Hg or <140 mm Hg, respectively.27
The Ohasama investigators28 followed 1913 participants aged 40 or older (average 61 years) for 8 years. The blood pressure thresholds based on home blood pressure were 137 mm Hg systolic and 84 mm Hg diastolic. The cardiovascular death rate was similar (0.33 versus 0.26 deaths per 100 person-years) in normotensive participants and in those with isolated diastolic hypertension. Patients with mixed or isolated systolic hypertension on self-measurement at home had significantly elevated death rates amounting to 1.11 and 2.04 per 100 person-years, respectively.
Several subject-level meta-analyses2,7,8 addressed the role of systolic and diastolic blood pressure or various subtypes of hypertension as cardiovascular risk factors. All were based on conventional sphygmomanometry. Kelly and colleagues7 did a prospective cohort study (from 1991 until 2000) in a nationally representative sample of 169 577 Chinese women and men, aged 40 years or more. These investigators used blood pressure levels of 90 mm Hg diastolic and 140 mm Hg systolic to classify subjects. Compared with normotension, relative risks of cardiovascular disease incidence and mortality were 2.73 (2.60–2.86) and 2.53 (2.39–2.68) for combined systolic and diastolic hypertension, 1.78 (1.69–1.87) and 1.68 (1.58–1.78) for isolated systolic hypertension, and 1.59 (1.43–1.76) and 1.45 (1.27–1.65) for isolated diastolic hypertension.7 The Asia Pacific Cohort Studies Collaboration8 studied 346 570 participants from 36 cohort studies. Outcomes were fatal and nonfatal cardiovascular disease. In multivariable-adjusted Cox regression, with normal blood pressure (<80 mm Hg diastolic and 120 mm Hg systolic) as the reference, hazard ratios were 1.81 (1.61–2.04), 2.18 (2.00–2.37), and 3.42 (3.17–3.70) for isolated diastolic, isolated systolic, and mixed hypertension, respectively.8 The Prospective Studies Collaboration2 demonstrated in 958 074 participants (61 cohort studies) that at ages 40 to 69 years, each 20-mm Hg increase in systolic blood pressure or 10-mm Hg increase in diastolic blood pressure was associated with more than a doubling in the death rates of stroke, ischemic heart disease, or other vascular death. These findings in subject-level meta-analyses with a large sample size are in keeping with our current study that made use of ambulatory blood pressure monitoring instead of conventional sphygmomanometry.
Our findings argue against the suggestion to abandon diastolic pressure measurement and to rely only on systolic blood pressure for the management of hypertension.29 Moreover, reversibility of the risk by blood pressure lowering treatment in patients with isolated diastolic hypertension30 confirms that certainly in younger individuals diastolic blood pressure is a risk factor that must be treated. The prevalence of isolated diastolic hypertension on 24-hour ambulatory blood pressure measurement was 4.9% in the whole untreated IDACO cohort and 17.2% among untreated patients with ambulatory hypertension. In the National Health Examination Survey (NHES) and National Health and Nutrition Examination Survey (NHANES) studies, 6% to 9% of subjects with elevated blood pressure readings had an isolated elevation of diastolic blood pressure with a normal systolic blood pressure.31
Our current study has some potential limitations. First, the number of end points in some subgroups was relatively small, in particular in the younger age group, in whom healthy elastic arteries might lead to a relatively less elevated systolic than diastolic blood pressure. Diastolic blood pressure is the driving force in the coronary circulation. This constellation might explain why diastolic hypertension is a risk factor for premature coronary heart disease and therefore for cardiac events below age 50. Second, patients with diastolic or mixed hypertension can progress to isolated systolic hypertension, so called burned-out hypertension, because with aging large arteries stiffen, so that systolic blood pressure rises and diastolic blood pressure falls. Our categorical analyses did not account for this phenomenon. Finally, we could not adjust for the serum lipid profile over and beyond total serum cholesterol, because too few participants had measurements of low-density or high-density cholesterol. We also did not account for measures of renal function, because they were only available in 4808 of our participants. However, we previously demonstrated that the incremental predictive value of renal function in an epidemiological setting is small compared with the 24-hour ambulatory blood pressure.32 Other factors we did not account for include family history of heart disease, and use of medications after enrolment.
In conclusion, we show that the risks conferred by diastolic and systolic blood pressure on 24-hour ambulatory measurement are age dependent. The 24-hour diastolic blood pressure and isolated diastolic hypertension drive coronary complications below age 50, whereas above age 50 the 24-hour systolic blood pressure is the predominant risk factor.
Supplementary Material
CLINICAL PERSPECTIVE.
No previous study has assessed the risks associated with isolated diastolic, isolated systolic, and mixed hypertension on 24-hour ambulatory monitoring or examined the age dependency of 24-hour systolic and diastolic ambulatory blood pressures as independent risk factors in the general population. In 8341 untreated people (mean age, 50.8 years; 46.6% women) randomly recruited from 12 populations and followed up for a median of 11.2 years, the risks conferred by diastolic and systolic ambulatory blood pressure were age dependent. Ambulatory diastolic pressure and isolated diastolic hypertension drove coronary complications below age 50 years, whereas above 50 years of age 24-hour systolic pressure and isolated systolic and mixed hypertension were the predominant determinants of risk. Our findings argue against the suggestion to abandon diastolic pressure measurement and to rely only on systolic pressure for the management of hypertension. Moreover, in younger individuals elevated diastolic pressure as assessed by 24-hour ambulatory monitoring is a risk factor that must be treated.
Acknowledgments
We gratefully acknowledge the expert assistance of Sandra Covens and Annick De Soete (Studies Coordinating Center, Leuven, Belgium).
Sources of Funding
The European Union (grants IC15-CT98-0329-EPOGH, LSHM- CT-2006–037093 InGenious HyperCare, HEALTH-F4-2007–201550 HyperGenes, HEALTH-F7-2011- 278249 EU-MASCARA, HEALTH- F7-305507 HOMAGE, and the European Research Council Advanced Researcher Grant 294713 EPLORE) and the Fonds voor Wetenschappelijk Onderzoek Vlaanderen, Ministry of the Flemish Community, Brussels, Belgium (G.0734.09, G.0881.13 and G.088013) supported the Studies Coordinating Centre (Leuven, Belgium). The European Union (grants LSHM-CT-2006–037093 and HEALTH-F4-2007–201550) also supported the research groups in Shanghai, Kraków, Padova and Novosibirsk. The Danish Heart Foundation (grant 01-2-9-9A-22914), and the Lundbeck Fonden (grant R32-A2740) supported the studies in Copenhagen. The Ohasama study received support via the Grants for Scientific Research (23249036, 23390171, 24591060, 24390084, 24591060, 24790654, 25461205, 25461083 and 25860156) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; and a Health Labour Science Research Grant (H23-Junkankitou [Seishuu]-Ippan-005) from the Ministry of Health, Labour, and Welfare, Japan; the Japan Arteriosclerosis Prevention Fund; and the Grant from the Daiwa Securities Health Foundation. The National Natural Science Foundation of China (grants 30871360, 30871081, 81170245, and 81270373), Beijing, China, and the Shanghai Commissions of Science and Technology (grant 07JC14047 and the “Rising Star” program 06QA14043 and 11QH1402000) and Education (grant 07ZZ32 and the “Dawn” project 08SG20) supported the JingNing study in China. The Comisión Sectorial de Investigación Científica de la Universidad de la República (Grant I+D GEFA-HT-UY) and the Agencia Nacional de Innovación e Investigación supported research in Uruguay. The 1R01AG036469 from the National Institute on Aging and Fogarty International Center is supporting the Maracaibo Aging Study.
Appendix
List of IDACO Investigators
Copenhagen, Denmark
Tine W Hansen, MD, PhD; Hans Ibsen MD, DSci; Jørgen L Jeppesen, MD, DMSci; Susanne Rasmussen MD, PhD; Christian Torp-Pedersen, MD, DMSci
Ohasama, Japan
Kei Asayama, MD, PhD; Naomi Fukushima, MSc; Azusa Hara, PhD; Takuo Hirose, PhD; Miki Hosaka, MSc; Yutaka Imai, MD, PhD; Ryusuke Inoue, MD, PhD; Masahiro Kikuya, MD, PhD; Hirohito Metoki, MD, PhD; Kyoko Nomura, MD, PhD, MPH; Taku Obara, PhD; Takayoshi Ohkubo, MD, PhD; Michihiro Satoh, PhD; Megumi Tsubota-Utsugi, PhD, MPH
Noordenkempen, Belgium
Yu-Mei Gu, MD; Azusa Hara, PhD; Lotte Jacobs, PhD; Yu Jin, MD, PhD; Tatyana Kuznetsova, MD, PhD; Yan-Ping Liu, MD; Thibault Petit, MD; Jan A Staessen, MD, PhD; Lutgarde Thijs, MSc; Zhenyu Zhang, MD
Uppsala, Sweden
Kristina Björklund-Bodegård, MD, PhD; Lars Lind, MD, PhD
Montevideo, Uruguay
José Boggia, MD, PhD; Inés Lujambio, MD; Leonella Luzardo, MD MSc; Edgardo Sandoya, MD; Carlos Schettini, MD; Emma Schwedt, MD; Hugo Senra, MD; Mariana Sottolano, MD
JingNing, China
Qifang Huang, MD PhD; Lihua Li, MD PhD; Yan Li, MD, PhD; Changsheng Sheng, MD, PhD; Jiguang Wang, MD, PhD
Novosibirsk, Russian Federation
Sofia Malyutina, MD, PhD; Yuri Nikitin, MD, PhD
Dublin, Ireland
Eamon Dolan, MD, PhD; Eoin O’Brien, DSc, MD
Pilsen, Czech Republic
Jan Filipovský, MD, PhD; Jitka Seidlrova, MD, PhD
Padova, Italy
Edoardo Casiglia, MD; Valérie Tikhonoff, MD, PhD
Kraków, Poland
Marcin Cwynar, MD, PhD; Danuta Czarnecka, MD, PhD; Tomasz Grodzicki, MD, PhD; Kalina Kawecka-Jaszcz, MD, PhD; Agnieszka Olszanecka, MD, PhD; Katarzyna Stolarz-Skrzypek, MD, PhD; Wiktoria Wojciechowska, MD, PhD
Maracaibo, Venezuela
Gustavo E. Calmon, MD, MSc; Inara J. Chacon, MD, MSc; Carlos A. Chavez, MD; Vanessa G. Felix, PhD; Gladys E. Maestre, MD, PhD; Jesus D. Melgarejo BSc; Luis J. Mena, PhD; Egle R. Silva, MD
Footnotes
Disclosures
None.
References
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 3.Kannel WB, Gordon T, Schwartz MJ. Systolic versus diastolic blood pressure and risk of coronary heart disease. Am J Cardiol. 1971;27:335–346. doi: 10.1016/0002-9149(71)90428-0. [DOI] [PubMed] [Google Scholar]
- 4.Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, Levy D. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103:1245–1249. doi: 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- 5.Stamler J, Neaton JD, Wentworth D. Blood pressure (systolic and diastolic) and risk of fatal coronary heart disease. Hypertension. 1989;13(suppl I):I-2–I-12. doi: 10.1161/01.hyp.13.5_suppl.i2. [DOI] [PubMed] [Google Scholar]
- 6.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker-Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Manolis A, Nilsson PM, Redon J, Struijker-Boudier HA, Viigimaa M, Adamopoulos S, Bertomeu V, Clement D, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, O’Brien E, Ponikowski P, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B. 2007 guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2007;28:1462–1536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 7.Kelly TN, Gu D, Chen J, Huang JF, Chen JC, Duan X, Wu X, Yau CL, Whelton PK, He J. Hypertension subtype and risk of cardiovascular disease in Chinese adults. Circulation. 2008;118:1558–1566. doi: 10.1161/CIRCULATIONAHA.107.723593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arima H, Murakami Y, Lam TH, Kim HC, Ueshima H, Woo J, Suh I, Fang X, Woodward M on behalf of the Asia Pacific Cohort Studies Collaboration. Effects of prehypertension and hypertension subtype on cardiovascular disease in the Asia-Pacific region. Hypertension. 2012;59:1118–1123. doi: 10.1161/HYPERTENSIONAHA.111.187252. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P. European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848. doi: 10.1097/00004872-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, Li Y, Dolan E, Tikhonoff V, Seidlerová J, Kuznetsova T, Stolarz K, Bianchi M, Richart T, Casiglia E, Malyutina S, Filipovsky J, Kawecka-Jaszcz K, Nikitin Y, Ohkubo T, Sandoya E, Wang J, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA, O’Brien E IDACO Investigators. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit. 2007;12:255–262. doi: 10.1097/mbp.0b013e3280f813bc. [DOI] [PubMed] [Google Scholar]
- 11.Hansen TW, Jeppesen J, Rasmussen F, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure monitoring and mortality: a population-based study. Hypertension. 2005;45:499–504. doi: 10.1161/01.HYP.0000160402.39597.3b. [DOI] [PubMed] [Google Scholar]
- 12.Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–2189. doi: 10.1097/00004872-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Staessen JA, Bieniaszewski L, O’Brien ET, Imai Y, Fagard R. An epidemiological approach to ambulatory blood pressure monitoring: the Belgian Population Study. Blood Press Monit. 1996;1:13–26. [PubMed] [Google Scholar]
- 14.Ingelsson E, Björklund K, Lind L, Ärnlöv J, Sundström J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA. 2006;295:2859–2866. doi: 10.1001/jama.295.24.2859. [DOI] [PubMed] [Google Scholar]
- 15.Schettini C, Bianchi M, Nieto F, Sandoya E, Senra H. Ambulatory blood pressure: normality and comparison with other measurements. Hypertension Working Group. Hypertension. 1999;34(4 Pt 2):818–825. doi: 10.1161/01.hyp.34.4.818. [DOI] [PubMed] [Google Scholar]
- 16.Li Y, Wang JG, Gao P, Guo H, Nawrot T, Wang G, Qian Y, Staessen JA, Zhu D. Are published characteristics of the ambulatory blood pressure generalizable to rural Chinese? The JingNing population study. Blood Press Monit. 2005;10:125–134. doi: 10.1097/00126097-200506000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Kuznetsova T, Malyutina S, Pello E, Thijs L, Nikitin Y, Staessen JA. Ambulatory blood pressure of adults in Novosibirsk, Russia: interim report on a population study. Blood Press Monit. 2000;5:291–296. doi: 10.1097/00126097-200010000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Kuznetsova T, Staessen JA, Kawecka-Jaszcz K, Babeanu S, Casiglia E, Filipovský J, Nachev C, Nikitin Y, Peleská J, O’Brien E on behalf of the EPOGH Investigators. Quality control of the blood pressure phenotype in the European Project on Genes in Hypertension. Blood Press Monit. 2002;7:215–224. doi: 10.1097/00126097-200208000-00003. [DOI] [PubMed] [Google Scholar]
- 19.O’Brien E, Murphy J, Tyndall A, Atkins N, Mee F, McCarthy G, Staessen J, Cox J, O’Malley K. Twenty-four-hour ambulatory blood pressure in men and women aged 17 to 80 years: the Allied Irish Bank Study. J Hypertens. 1991;9:355–360. doi: 10.1097/00004872-199104000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Maestre GE, Pino-Ramírez G, Molero AE, Silva ER, Zambrano R, Falque L, Gamero MP, Sulbarán TA. The Maracaibo Aging Study: population and methodological issues. Neuroepidemiology. 2002;21:194–201. doi: 10.1159/000059524. [DOI] [PubMed] [Google Scholar]
- 21.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(suppl 1):S5–S20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 22.Boggia J, Thijs L, Hansen TW, Li Y, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Olszanecka A, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Maestre G, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes Investigators. Ambulatory blood pressure monitoring in 9357 subjects from 11 populations highlights missed opportunities for cardiovascular prevention in women. Hypertension. 2011;57:397–405. doi: 10.1161/HYPERTENSIONAHA.110.156828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Staessen JA, Wang J, Bianchi G, Birkenhäger WH. Essential hypertension. Lancet. 2003;361:1629–1641. doi: 10.1016/S0140-6736(03)13302-8. [DOI] [PubMed] [Google Scholar]
- 24.Khattar RS, Swales JD, Dore C, Senior R, Lahiri A. Effect of aging on the prognostic significance of ambulatory systolic, diastolic, and pulse pressure in essential hypertension. Circulation. 2001;104:783–789. doi: 10.1161/hc3201.094227. [DOI] [PubMed] [Google Scholar]
- 25.Petrovitch H, Curb JD, Bloom-Marcus E. Isolated systolic hypertension and risk of stroke in Japanese-American men. Stroke. 1995;26:25–29. doi: 10.1161/01.str.26.1.25. [DOI] [PubMed] [Google Scholar]
- 26.Fang J, Madhavan S, Cohen H, Alderman MH. Isolated diastolic hypertension. A favorable finding among young and middle-aged hypertensive subjects. Hypertension. 1995;26:377–382. doi: 10.1161/01.hyp.26.3.377. [DOI] [PubMed] [Google Scholar]
- 27.Strandberg TE, Salomaa VV, Vanhanen HT, Pitkälä K, Miettinen TA. Isolated diastolic hypertension, pulse pressure, and mean arterial pressure as predictors of mortality during a follow-up of up to 32 years. J Hypertens. 2002;20:399–404. doi: 10.1097/00004872-200203000-00014. [DOI] [PubMed] [Google Scholar]
- 28.Hozawa A, Ohkubo T, Nagai K, Kikuya K, Matsubara M, Tsuji I, Sadayoshi I, Satoh H, Hisamichi S, Imai Y. Prognosis of isolated systolic hypertension and isolated diastolic hypertension as assessed by self-measurement of blood pressure at home. The Ohasama Study. Arch Intern Med. 2001;160:3301–3306. doi: 10.1001/archinte.160.21.3301. [DOI] [PubMed] [Google Scholar]
- 29.Sever PS. Simple blood pressure guidelines for primary care. J Hum Hypertens. 1999;13:725–727. doi: 10.1038/sj.jhh.1000923. [DOI] [PubMed] [Google Scholar]
- 30.Veterans Administration Cooperative Study Group on Antihypertensive Agents. Effects of treatment on morbidity in hypertension. Circulation. 1972;45:991–1004. [Google Scholar]
- 31.Drizd T, Dannenberg AI, Engel A. Blood pressure levels in persons 18–74 years of age in 1976–1980 and trends in blood pressure from 1960 to 1980 in the United States. United States Vital and Health Statistics. 1986 Series II, N° 234 DHHS publication N° (PHS) 86–1684. [PubMed] [Google Scholar]
- 32.Boggia J, Thijs L, Li Y, Hansen TW, Kikuya M, Björklund-Bodegård K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Schwedt E, Sandoya E, Kawecka-Jaszcz K, Filipovsky J, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes (IDACO) Investigators. Risk stratification by 24-hour ambulatory blood pressure and estimated glomerular filtration rate in 5322 subjects from 11 populations. Hypertension. 2013;61:18–26. doi: 10.1161/HYPERTENSIONAHA.112.197376. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


