Abstract
The lack of readily available biomarkers is a significant hindrance towards progressing to effective therapeutic and preventative strategies for Alzheimer’s disease (AD). Blood-based biomarkers have potential to overcome access and cost barriers and greatly facilitate advanced neuroimaging and cerebrospinal fluid biomarker approaches. Despite the fact that preanalytical processing is the largest source of variability in laboratory testing, there are no currently available standardized preanalytical guidelines. The current international working group provides the initial starting point for such guidelines for standardized operating procedures (SOPs). It is anticipated that these guidelines will be updated as additional research findings become available. The statement provides (1) a synopsis of selected preanalytical methods utilized in many international AD cohort studies, (2) initial draft guidelines/SOPs for preanalytical methods, and (3) a list of required methodological information and protocols to be made available for publications in the field in order to foster cross-validation across cohorts and laboratories.
Keywords: Biomarkers, blood, serum, plasma, Alzheimer’s disease, dementia, diagnosis, treatment
1. Introduction
There is a large concern regarding the lack of reproducibility of research findings across independent laboratories, within laboratory settings, and particularly from academic laboratory settings to industry settings [1–4]. In fact, an “unspoken rule” among venture capital firms is that 50% of published studies will not replicate in industrial labs [4] and the NIH recently outlined a plan to address this problem [2]. While there are a large number of factors contributing to this issue, one key factor is the substantial variability in study designs, definitions, outcomes, and analytic models that make replication less likely [1]. While in the discovery phase of science, it is important to have substantial flexibility; however, as scientific discovery proceeds closer to the clinic, there is an increased need for optimization and standardization if these discoveries are to replicate reliably and pass regulatory authority. Unfortunately, there is oftentimes a disconnect between academic and industrial laboratories that hampers movement of important scientific discovery to clinical practice, and the generation of standardized methods is one way to bridge this gap. The purpose of this whitepaper is the generation of the first set of guidelines for use in research of blood-based biomarkers of Alzheimer’s disease (AD).
A major impediment to therapeutic development and clinical trial design for AD is the lack of a sensitive, easily-obtained biomarker of disease [8–10]. Biomarkers of disease presence, subtypes (i.e., endophenotypes), treatment response, and progression are needed to advance therapeutic and preventative opportunities for this rapidly growing health care crisis [8, 11–13]. Biomarkers are also considered promising tools to enhance all phases of drug discovery & development programs by allowing validation of mechanisms of action (MoA) [14]. They can be employed in clinical trials to improve diagnostic accuracy in trial participants, thus allowing cohorts of patients to be enriched with cases of AD (patient enrichment) [15, 16]. In light of this, such markers may not only be useful in patient identification, selection and stratification into clinical trials, but may also be useful in the identification of novel therapeutic targets.
Over the last two decades, the search for biomarkers that have diagnostic and prognostic utility in AD has grown exponentially [9,11] with the majority of work focusing on neuroimaging and cerebrospinal (CSF) methodologies [9,11,17]. Advanced neuroimaging and CSF techniques yield highly accurate diagnostic accuracy within clinic-based settings for detecting AD and blood-based biomarkers represent an approach for enhancing the utility of imaging and CSF-based modalities by serving as a generalized screening tool. In fact, it has been proposed that blood-based methods can serve as the first step in a multi-step diagnostic process [10] as is the case with many other pathologies, such as cardiovascular diseases, infectious diseases, and cancer. All screen positives could be referred for neuroimaging or CSF assessment for confirmatory purposes (e.g. for diagnostics or enrollment into clinical trials).
There has been a significant increase in research efforts examining the potential for blood-based biomarkers of AD. While the search was largely unsuccessful for decades, recent work shows promise. In a seminal study, Ray and colleagues [18] analyzed 120 plasma-based proteins and developed an algorithm consisting of an 18-biomarker panel that accurately distinguished AD patients from healthy controls with an overall classification accuracy of 89% as well as accurately identified 81% of mild cognitive impairment (MCI) patients who progressed to AD within a 2 to 6-year follow-up period [18]. This study represented the first major support for the notion that an AD biomarker profile could yield excellent accuracy; however, enthusiasm waned when the findings did not cross-validate on an independent assay platform [19]. Despite this initial setback, other groups have continued to identify promising signals in peripheral blood, suggesting that a blood-based AD screen may be on the horizon [20–29]. Recently, data from well-characterized international cohorts have yielded additional candidate biomarkers and panels [25,30]. In the Texas Alzheimer’s Research and Care Consortium (TARCC) cohort a serum-based algorithm yielded a 30-protein profile with a sensitivity of 88% and specificity of 82% for clinical AD diagnosis [31]. The biomarker panel from baseline plasma collected in the Australia Imaging Biomarkers and Lifestyle Study of Ageing (AIBL) study consisted of 18 analytes that could distinguish AD from healthy controls with a sensitivity of 85% and specificity of 93% [29]. A 17-biomarker panel was associated with the diagnosis of MCI and AD in independent cohorts from the University of Pennsylvania and Washington University in St. Louis, and two of these analytes were found to be highly correlated with the CSF t-tau/Aβ42 ratio[30], a strong predictor of future cognitive decline [32,33]. There have been several markers consistently altered in AD across cohorts. As outlined by Kiddle and colleagues [34], an example of these markers (and number of cohorts they have been replicated across) include: apolipoprotein E (5 cohorts), alpha-2-macroglobulin (5 cohorts), complement C3 (5 cohorts), pancreatic prohormone (5 cohorts), serum amyloid P (4 cohorts), tumor necrosis factor (2 cohorts), serum albumin (4 cohorts). Many of these blood-based studies are similar in terms of utilizing a common analytical platform; however, the biomarker panels obtained are strikingly different, sharing only a few common analytes. For example, in the study by Hu and colleagues, several markers were significantly related to dementia status but in the opposite direction across cohorts despite the use of the same analytic platform. Additionally, several studies have examined the Alzheimer’s Disease Neuroimaging Initiative (ADNI) proteomic database with different protein signatures reported [29–31]. The discrepant findings may be due to the approach employed as the ADNI cohort was utilized as the validation sample with the protein signatures being developed in other cohorts (i.e. University of Pennsylvania, Washington University, AIBL, TARCC). For comprehensive recent reviews of AD proteomic studies conducted across a broad range of cohorts see Lista and colleagues [35] and Kiddle and colleagues [34].
Apart from the fact that different initial panels were tested (along with different study design), inconsistencies across study findings could be attributable to many preanalytical variables, both technical and biological, across studies which may have significant impact on the outcomes of the proteomic analyses. There are numerous possible sources of preanalytical variations or errors across studies [36]; however out of these, we have attempted to highlight only a few important ones. For example, selection of study participants in terms of their ethnicity, lifestyle parameters, and statistically sufficient numbers could be an important source of variation. In addition, within-subject variation has long been highlighted as a possible source of concern as participants need to adhere to certain guidelines during the course of the study [37]. Variations could also be introduced by work staff in terms of sample collection mode, collection tubes, preparation, transportation, handling, storage and processing as well as different calibration protocols of the equipment being used [37,38]. One of the most important factors is the fraction of the blood used for testing (serum vs plasma) as not only the abundance of a particular analyte may vary in these different fractions, but additives such as heparin, citrate or ethylenediaminetetraacetic acid (EDTA) influence the required processing methods and their presence may impact biomarker stability and detectability [39–41]. Table 1 presents a list of some of the uncontrollable and controllable variables that can impact findings from studies of blood-based biomarkers in AD. The uncontrollable variables should be reported in the methods of protocols and taken into account statistically, whereas the controllable variables represent scientific areas where harmonization can occur.
Table 1.
Controllable and uncontrollable variables that can impact blood-biomarker findings within Alzheimer’s disease studies
| Controllable Variables | Uncontrollable Variables |
|---|---|
| Time of collection | Demographic characteristics (age, sex, ethnicity/race) |
| Fasting status | ApoE ε4 (and other genes) |
| Needle size & location of draw | Smoking status |
| Handling of tubes (e.g. inversions) | Gestation |
| Tube type and additives | Diet |
| Tube collection order | Medications |
| Time of sample in collection tube | Non-AD comorbidities |
| Centrifugation parameters | Alcohol use |
| Time from collection to freeze | Activity level |
| Temperature of freeze | |
| Freeze-thaw cycles | |
| Aliquot size |
A key step towards generating consistency across studies with regards to blood-based biomarkers is the establishment of guidelines for preanalytical protocols [8,42–45] mirroring the ongoing initiatives for CSF AD biomarkers [17,46,47]. In fact, such standardization efforts for blood-based biomarkers have been underway in other fields for some time [24,48–52] and the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM, available at http://efcclm.eu/) working group reported a substantial reduction in analytic error with improvements in standardization and reliability of instruments, reagents and techniques[53]. Notably, the STandards for Alzheimer’s Research in Blood biomarkers (STAR-B) was born out of this need and combined with the Blood-Based Biomarker Interest Group (BBBIG) to create a Professional Interest Area (PIA) of the Alzheimer’s Association International Society to Advance Alzheimer’s Research and Treatment (ISTAART; available at https://act.alz.org/site/SPageServer?pagename=ISTAART_homepage). The ultimate goal of this international working group is the advancement of blood-based biomarkers for the improvement of diagnosis, treatment, and care for those suffering from AD. This international collaboration recently has provided an overview regarding the status of the field [8] and the Alzheimer’s Association and Alzheimer’s Drug Discovery Foundation (ADDF) recently jointly convened a workshop to discuss the state of the field [54]. The current work from the working group was undertaken to (1) summarize selected methods across many ongoing longitudinal cohorts, (2) take an initial step towards the provision of guidelines for preanalytical methods for studies examining the development and role of blood-based biomarkers of AD, and (3) provide a minimum set of preanalytical variables that must be provided in publications (within the publication or as a supplement) in this line of work. Moreover, a set of next-step variables specific to the elderly and dementia populations to be examined have been proposed as areas for further research is needed on this topic to inform the next revision of the current guidelines.
2. Ongoing Studies
Protocols from 10 (ongoing) Alzheimer’ Disease cohort studies, collaborations as well as the National Institute on Aging (NIA) Best Practice Guidelines (also currently being updated) were reviewed. These studies were selected as they (1) denote ongoing longitudinal studies with specific foci (including blood-based) in biomarkers of AD, (2) represent a significant portion of the investigators and/or publications in the topic area, and (3) were willing to share detailed protocols regarding blood collection and processing. These studies also presented established protocols for requesting biological samples. Studies/groups that either did not respond to the request for protocols or that provided confidential methods were not included. The studies included the Alzheimer’s Center Amsterdam [55], Alzheimer’s Disease Cooperative Study (ADCS) [56], Alzheimer’s Disease Neuroimaging Initiative (ADNI) [57], Australian Imaging, Biomarkers and Lifestyle (AIBL) study [58, 59], Dominantly Inherited Alzheimer Network (DIAN) [60–62], Health and Aging Brain among Latino Elders (HABLE) [63], King’s Dementia Studies[64], NIA Best Practices[65], Texas Alzheimer’s Research and Care Consortium (TARCC) [25,26,31,66], and the Washington University Adult Children Study (ACS) [67, 68].
As reported in Table 1, there is significant consistency, but also inconsistency as well as lack of technical details across existing studies. The TARCC, ADCS, NIA Best Practices, and Alzheimer Center Amsterdam studies do not require fasting blood draws, whereas all others make use of them. On the other hand, while “overnight fast” was needed for several studies, only the DIAN protocol provided a definition for fasting duration (i.e. 8 hours). Many studies provided information regarding needle gauge to be used, though not all, with 21-gauge being the most commonly utilized size. Tube type varied across studies, with little consistency across the category of serum tube selected. Lavender/purple top EDTA plasma (K2) was commonly utilized for plasma collection. Centrifugation speed varied across studies by speed, duration, temperature and number of spins, with little consistency noted. Additionally, the number of revolutions per minute (rpm) in some studies but g-force in others was utilized for documentation of centrifugation speed. Sample preparation time (total) was most commonly less than or equal to two hours. Samples were most commonly stored immediately at −80° C, though some studies utilize immediate freeze on dry ice prior to placement in −80° C or liquid nitrogen. The most common long-term storage condition was −80° C.
3. Guidelines for Preanalytical Methods
There is a sizable literature documenting the impact of preanalytical methods on proteomic results, with most of the errors in laboratory testing coming from outside the analytic phase [37] and the majority originating from the preanalytical processing phase [69–72]. Specifically, the role of preanalytical variables – affecting the quality of the utilized samples and, consequently, the quality of the data produced – is frequently disregarded in clinical proteomic analyses [73]. In this regard, it has been suggested that 46% of the errors in laboratory testing comes from the preanalytical phase [74].
If any blood-based AD biomarkers are to move from research only (RUO) (discovery phase or cross-validation phase) to in vitro diagnostic (IVD) use, standardization of methodologies is compulsorily required. While there is still a great need for additional discovery in the area of blood-based biomarkers, there is also the necessity to “lock-down” or further clinically validate the potential utility of the putative markers currently available, which is the focus of the current guidelines. In the United States, all testing on human samples as clinical diagnostics must be performed within a regulated good laboratory practice (GLP) setting as defined by the Clinical Laboratory Improvement Amendment of 1988 (CLIA ‘88) and other associated regulatory guidelines[37]. Many procedures for reaching clinical diagnostic status are determined by standard protocols, standard operating procedures (SOPs) and national or international standards, which include the preanalytical procedures provided by the Clinical Laboratory Standards Institute (CLSI, available at http://clsi.org/) (formally the National Committee for Clinical Laboratory Standards), with strict adherence to such standards being important [37].
3.1 Pre-blood draw
There are a number of patient/participant-related factors that will impact blood marker results that cannot be accounted for unless proper documentation is obtained. Some physiological variables to consider include demographics (age, sex, race/ethnicity), overall health, food and beverages consumed prior to collection, chronic drugs/alcohol use, dietary supplements, smoking, gestation, diet, exercise, posture or bed rest, as well as patient medical conditions and medication status [37,45,48,50,52]. Attempts should be made to record information related to these variables as much as possible in order for appropriate adjustments to be made during analysis of results [37,48,50]. As can be seen from Table 2, the majority of ongoing studies utilize fasting blood-collection though the definition of fasting (i.e. 6, 8, 12hr) is not articulated, despite the fact that fasting duration has a known impact on many blood-based biomarker levels. Prior work also suggests that some, but not all, blood biomarkers exhibit diurnal fluctuations [75–77], which can have a substantial impact on the clinical significance of such markers [78]. Standardizing to a morning (before 10am fasting) blood draw would address the possible diurnal fluctuation issues by harmonizing sample collection times across studies.
Table 2.
Summary of select preanalytical processing elements across ongoing cohorts
| Cohort | Fasting | Needle | Serum | Plasma | Centrifuge Speed/ Time | Processing Time | Storage Method (Immediate) |
Storage Method (Long-term) |
|---|---|---|---|---|---|---|---|---|
| TARCC[25,26, 31,66] |
No | ND | Serum- separating tubes (tiger tops) |
BD EDTA tubes (purple top) |
1300xg/ 10 minutes Room temperature |
2 hours; sample processing started within 1hr of draw |
Frozen on wet ice if unable to be frozen immediately; placed in −20 °C freezer |
−80 °C |
| ADNI[57] | Yes | 21G | (plain red tops) |
EDTA tubes | 3000rpm/ 15 minutes | 2 hours; sample processing started within one hour following blood draw |
Frozen on dry ice for 20 minutes then shipped same day; upon arrival samples are thawed, re- aliquoted and placed in −80 °C |
−80 °C |
| AIBL[58,59] | Yes | 21G | Sarstedt s- monovette serum-gel (brown top) |
a) Sarstedt s-monovette lithium heparin (green top) b) Sarstedt s-monovette EDTA tubes (with PGE added) (purple top) |
Serum: 1800xg/ 15 minutes 20 °C Plasma: Step1: 200g/10 minutes 20 °C Step2: 800g/15 minutes 20 °C |
Total processing must be completed within 3.5 hours; Blood processing must be started within 20 minutes of after blood draw |
Frozen immediately at −80 °C |
Liquid nitrogen |
| ADCS[56] | ND | ND | EDTA tubes | 3000rpm/10 minutes | ND | −80 °C | −80 °C | |
| NIA Best Practice Guidelines[65] |
Ideal but not required |
Small gauge needle |
ND | EDTA or Heparin tubes |
ND | ND | Quick freeze with dry ice, then placed in - 80 °C freezer |
−80 °C |
| HABLE[63] | Yes | 21G | Serum- separating tubes (tiger tops) |
BD EDTA tubes (purple top) |
1300xg/10 minutes Room temperature |
2 hours; sample processing started within 1hr of draw |
−80 °C | −80 C° |
| DIAN[60,61] | Yes | 21G Butterfly |
Red Top Plain tubes |
EDTA tubes (lavender top) |
2000xg/15 minutes Room temperature |
Process serum after allowing to sit at room temperature for 30 min |
Flash Freeze on dry ice at site, shipped, stored at −80 °C, thawed, aliquot, re- flash frozen on dry ice and stored at −80 °C |
−80 °C Liquid Nitrogen (subset) |
| ACS[67,68] | Yes | 21G Butterfly |
N/A | EDTA tubes | 2000xg/15 minutes 4 °C |
Within 1–2 hours of collection |
Receive samples on wet ice, aliquot, placed in −80 °C freezer/liquid Nitrogen |
−84 °C Liquid Nitrogen (subset) |
| King’s Dementia Studies[64] |
Yes | 21G or 23G (depending on vein size) |
Serum Tube (gold top) |
EDTA tubes (purple top) |
3000rpm/8 minutes | Time from blood draw to samples freezing kept within 2–3hours |
−80 ° C | −80 °C |
| Alzheimer Center Amsterdam [55] |
No | 21 G BD (also 22,23 G present). |
BD serum gel tubes (red top) |
BD EDTA tubes (purple top) |
1800 g/10 minutes 40°C |
<2 hours, usually within 1 hour. |
Immediately frozen at −80 °C |
−80 °C |
Note: ND=not documented in protocol
3.2 Blood collection
There are a number of variables associated with the blood collection procedure itself that can impact laboratory assay results. Needle gauge, single- or multi-draw needles, and needle composition can impact assay results [37], with hemolysis being a major consideration [79–82]. For example, in an emergency department setting, use of a 22-gauge needle was significantly associated with increased risk of hemolysis [83]. Based on prior results, a 21-gauge needle is preferred [82,84,85]. Needles can be composed of various materials including stainless steel, aluminum, titanium, chromium, iron, manganese, nickel and alloys which may impact assays that measure various metals within the blood. A detailed description of how to perform a venipuncture is provided by CLSI document H3-A6. There are advantages and disadvantages for both serum and plasma, which can fluctuate based on the specific marker of interest (e.g. see Rai and Vitzthum [37]).
The site used for blood withdrawal is also an important aspect to consider [86]. The median cubital vein, usually easily found and accessed, is considered the preferred site. The preparation of the blood collection sites necessitates an accurate cleaning of the skin with alcohol (2-propanol) that should be allowed to evaporate, given that the contamination of blood with residual alcohol may induce hemolysis, increase the concentrations of some analytes therefore producing interferences [87]. In addition, the position of the patient (standing, lying, sitting) can have an impact on the hematocrit, and, thus, may cause fluctuations in the levels of the analytes [88].
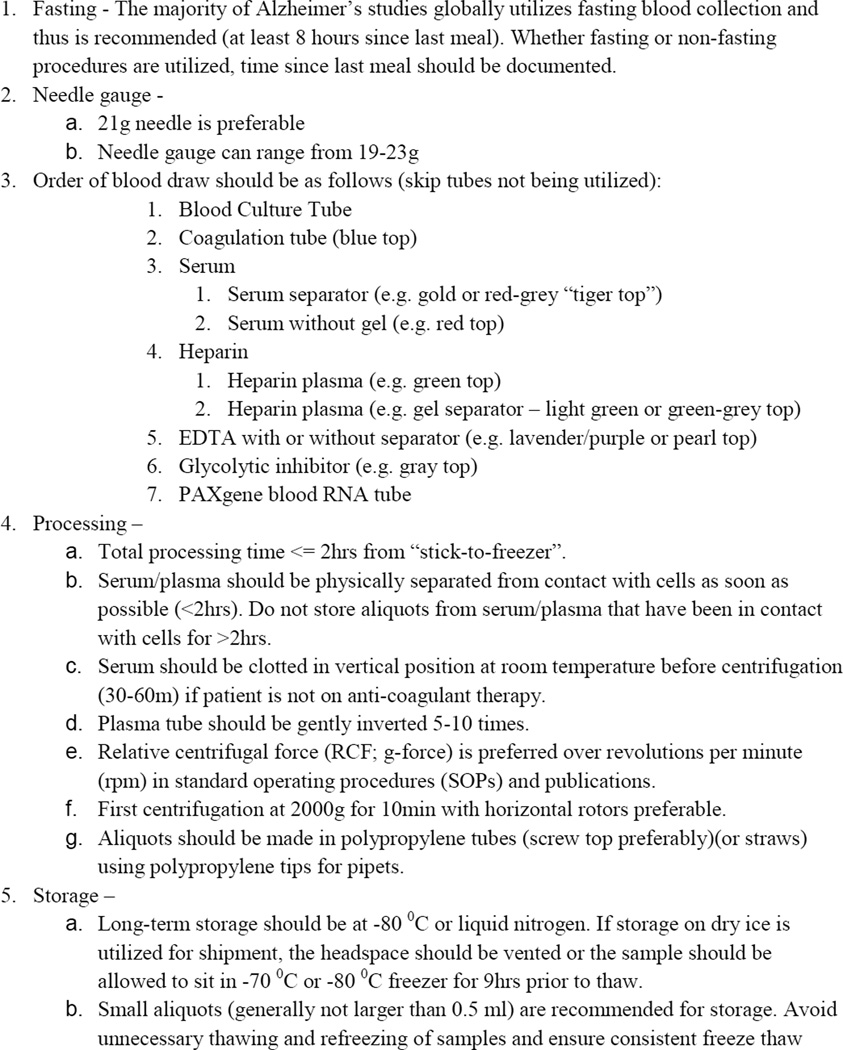
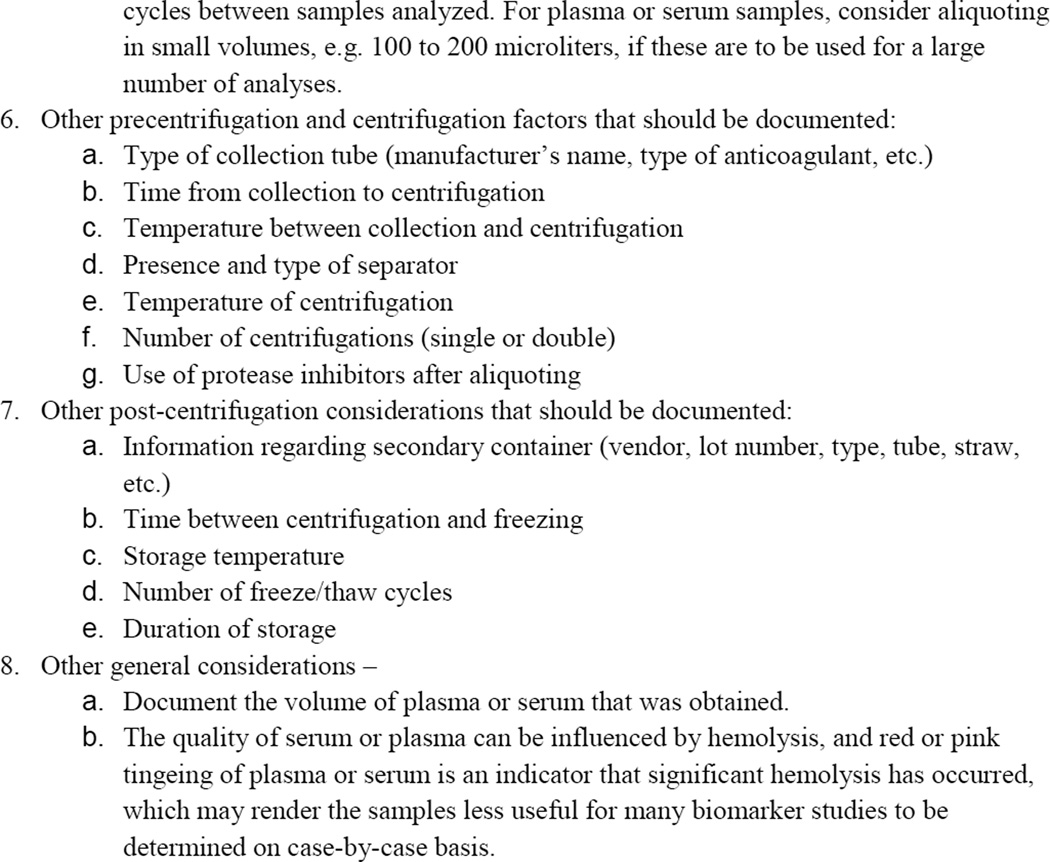
Moreover, the collection tube can significantly have an affect the obtained results [37,82]. In fact, tube components of rubber stoppers, tube wall materials, surfactants, anticoagulants, separator gels, clot activators, anticoagulants can all impact assay results [82]. In order to comply with Occupational Safety and Health Administration (OSHA, available at https://www.osha.gov/) guidelines to minimize risks from shattering tubes, plastic tubes have replaced glass collection tubes [82,89]. While plastic tubes offer many advantages, such as increased gas and water permeability, they also offer several disadvantages such as adhesion of proteins to tube walls [82], which has been an issue identified for CSF AD biomarkers [90–93]. A detailed review of the impact of tube components on blood-based assay performance has been published by Bowen 2010 [82]. The order of tube collection in blood draw is also important (CLSI H3-A6 and Rai and Vitzthum [37]) and the current recommendations can be found in Figure 1.
Figure 1.
Preanalytic Processing Guidelines
3.3 Blood processing
CLSI H18-A4 provides detailed information regarding procedures for handling and processing blood specimens for laboratory tests. The time from blood-draw to storage, storage temperature, centrifugation parameters, storage volume and container type are all important considerations for sample processing [37,44,79,94,95]. A key point for consideration is the separation of the sample from the tubes immediately after centrifugation. While the processing time may vary by study and the importance by protein being measured, one should not store aliquots from serum/plasma that have been in contact with cells for more than two hours [79]. Review of Table 1 shows that the majority of ongoing protocols require the total processing time to be 2 hours or less, which is preferable. See H18-A4 for a detailed list of uncentrifuged specimen stability for a range of times and sample types. Per H18-A4, centrifugation parameters that should not be subject to variation are: horizontal rotors should be utilized and first centrifugation speed should be at 2000g for 10 minutes [50]. Parameters that are subject to variation but should be documented include: (1) presence and type of separator, (2) temperature of centrifugation, (3) number of centrifugations (single or double). With regards to post-centrifugation processing, the parameters that should not be subject to variation include: (1) serum/plasma is not to be heated or otherwise inactivated, and (2) no storage at −20° C. Parameters subject to variation but requiring documentation include: (1) type of secondary container (tube, straw), (2) time interval between centrifugation and freezing, (3) sample temperature prior to aliquoting and freezing, (4) storage temperature, (5) number of freeze/thaw cycles, and (6) duration of storage[50,79]. Polypropylene tips and tubes are recommended to reduce adherence of analytes to walls.
3.4 Storage
It has been well acknowledged that protein stability and enzymatic activity are strictly dependent on temperature [96]. Long-term storage should be at −80° C or liquid nitrogen. According to Rai and colleagues [50], liquid nitrogen storage should represent an excellent system to ensure protein stability. However, this way is not often practicable in comparison with the availability of −80°C freezers. Hence, the long-term storage temperature should be set at −80°C, using freezers whose temperature oscillations are absent or extremely diminished. If storage on dry ice is utilized for shipment, the headspace should be vented or the sample should be allowed to sit in −70° C freezer for nine hours prior to thaw to facilitate protein stability [97]. Figure 1 provides the proposed guidelines for preanalytical processing outlined here.
4. Minimum data required for publication
In order for attempts to be made at cross-validation of biomarker findings across cohorts and laboratories, a minimum amount of information is required in addition to utilizing common methods. The select preanalytical elements outlined above need to be made available to the scientific community within the manuscript or online supplement. Figure 1 not only provides the current guidelines, but also a template for provision of key pre-analytic elements to be provided within publications for use by other teams.
5. Elderly- and dementia-specific pre-analytic processing variables requiring additional research
While the current guidelines provide the first-step in the process towards the generation of standards for the field, there remain several topics that require additional research. Most importantly relates to the question of how these preanalytical methods require modification for geriatric populations. For example, the World Health Organization points out skin breakdown as a potential complication of capillary sampling among elderly patients [98]. However, a systematic study of the impact of the proposed guidelines specifically among the elderly has not been undertaken. In fact, review of the previously published materials (including CLSI documents) does not provide information that is age-specific. Therefore, it is recommended that the need for specific alterations in the guidelines for the target population be undertaken with the current guidelines as a starting framework.
6. Conclusions and future perspectives
In order for blood-based biomarker work in AD to progress, there is a need for adoption of guidelines for to standardize preanalytical methods across cohorts and laboratories [8,42]. Such guidelines will allow for validation/cross-validation across laboratories and cohorts to further validate the clinical performance of putative markers where signals have been established. The current guidelines are an attempt to verify such existing putative markers for specific clinical utilities and are not intended to stifle in any way new discoveries, which are certainly needed in the blood-based AD biomarker arena. The Blood Based Biomarkers (PIA) of ISTAART combined the efforts of the STAR-B and BBBIG working groups for a single cohesive effort. This working group recently published a position paper on the future of blood-based biomarkers of AD in which several needed areas of work were outlined, which included the need for guidelines and/or standards for preanalytical methods [8]. The current project reflects the continued efforts of that working group and development of the first such international guidelines for preanalytical processing of bloods in AD research. It is anticipated that these guidelines will be updated as needed based on advancements of the field.
There are multiple potential clinical utilities for blood-based AD biomarkers, and the study design must be reflective of that particular purpose. For example, blood-based AD biomarkers of disease presence, amyloid positivity, CSF biomarker positive (i.e. diagnostic markers) may be developed within clinic settings of case-control designs; however, if such markers are to be clinically useful in primary care settings, they must be tested/evaluated within such settings as the diagnostic accuracy will vary greatly due to the difference in disease base rates and diagnostic practice [99–101]. To date, no such studies have been carried out validating putative blood-based AD biomarkers within primary care settings. Issues around analytical assay validation, discovery versus clinical diagnostic-grade platforms, etc. have also received little attention. As with preanalytical processing variables, CLSI guidelines are currently available for assessing performance of assays (e.g. EP5, EP6, EP7, EP10, EP14, EP15, EP17, ILA21, ILA23), which should be followed if the assay is to move towards clinical application.
To date, there are numerous signals for putative blood-based biomarkers and biomarker panels, though no consensus has been reached so far following Institute of Medicine (IOM) guidelines [102]. The purpose of the provision of the current guidelines from the international working group is to begin the process and dialogue of moving towards standardized methods that can be utilized to move putative blood-based biomarkers closer to clinical or additional research practices. An important step will be the detailed disclosure of the pre-analytic parameters used for collection of clinical samples in publications of the clinical evaluation of biomarkers. The current document provides information regarding the minimum necessary information regarding these pre-analytic methods utilized to facilitate cross-validation of methods across research teams. Additional working group documents will address both analytic and post-analytic variables.
Systematic review: Recent research points towards many promising signals in the search for blood-based biomarkers for Alzheimer’s disease. However, there remain inconsistencies and failures to replicate in the literature. With the increased emphasis from the National Institutes of Health (NIH) on increasing the reproducibility of science, there is a great need for guidelines in this line of research, similar to ongoing initiatives in neuroimaging and cerebrospinal fluid biomarkers.
Interpretation: There are currently many different protocols for the pre-analytic processing of blood samples in Alzheimer’s disease biomarker work. Guidelines were generated by this international working group as was a minimum set of information that warrants inclusion in research publications.
Future Directions: These guidelines will provide a starting-point for harmonization of procedures for the validation phase of blood-based biomarker science in Alzheimer’s disease. As new research becomes available, these guidelines will be updated as needed.
Acknowledgment
Sid E. O’Bryant has multiple patients pending, submitted by the University of North Texas Health Science Center wherein he is an inventor and receives research grants from the National Institutes of Health, National Institute on Aging, award number R01AG039389 and P30AG12300. Veer Gupta reports not conflicts of interests. Kim Henriksen has research supported by the Danish Research Foundation and reports no conflicts of interests. Melissa Edwards reports no conflicts of interests. Andreas Jeromin holds affiliations with Atlantic Biomarkers, LLC and reports no conflict of interests. Chantal Bazenet reports no conflicts of interests. Holly Soares holds affiliations with Bristol-Myers Squibb and reports no conflicts of interests. Simon Lovestone reports no conflicts of interests. Harald Hampel is supported by the AXA Research Fund, the Fondation Université Pierre et Marie Curie and the Fondation pour la Recherche sur Alzheimer, Paris, France. The research leading to these results has received funding from the program “Investissements d’avenir” ANR-10-IAIHU-06. Thomas Montine receives funding from the National Institutes of Health, award Number P50AG05136 and reports no conflict of interest. Kaj Blennow has research supported by the Swedish Research Council and has served on Advisory Boards for Innogenetics, Belgium. Tatiana Foroud reports no conflict of interest. Maria Carrillo reports no conflict of interest. Neill Graff-Radford reports no conflict of interest. Christoph Laske reports no conflict of interest. Monique Breteler reports no conflict of interest. Leslie Shaw reports no conflict of interest. John Q. Trojanowski may accrue revenue in the future on patents submitted by the University of Pennsylvania wherein he is co-Inventor and received revenue from the sale of Avid to Eli Lily as co-inventor on imaging related patents submitted by the University of Pennsylvania. Nicole Schupf reports no conflicts of interests. Robert A. Rissman reports no conflicts of interests. Anne M. Fagan reports no conflicts of interests. Pankaj Oberoi and Robert Umek hold affiliations with Meso Scale Discovery and report no conflicts of interests Michael W. Weiner reports no conflicts of interests. Paula Grammas reports no conflicts of interests. Holly Posner holds affiliations with Pfizer Inc. and reports no conflicts of interests. Ralph Martins reports no conflicts of interests.
Appendix
†Additional members of the Blood-Based Biomarker Interest Group (BBBIG) and STandards for Alzheimer’s Research in Blood biomarkers (STAR-B) include Howard M. Fillit, Alzheimer’s Drug Discovery Foundation, New York, NY, USA; Lisa J. Bain, Elverson, PA, USA; David Wholley and Judy Siuciak, The Biomarkers Consortium, Foundation for the National Institutes of Health, USA; David Holtzman, Department of Neurology, Washington University School of Medicine, St. Louis, MO, USA; Gary Kong, Edith Cowan University, Australia; Andrew Saykin, Indiana University, Center for Neuroimaging, IN, USA; Robert Nagele, University of Medicine and Dentistry of New Jersey School of Osteopathic Medicine, NJ, USA; Dwight German, Department of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX, USA; Diane Stephenson, Critical Path Institute, USA; Andrew Watt, Alzheimer’s Australia Dementia Research Foundation, Australia; Howard Schulman, Caprion Proteomics, USA; Pedro Pesini, Araclon Biotech S.L., Spain; Tony Phelps, National Institutes of Aging, USA; Steve Younkin, Mayo Clinic, Jacksonville, FL, USA; Thomas Kodadek, Departments of Chemistry & Cancer Biology, The Scripps Research Institute, Scripps Florida, Jupiter, FL, USA; Morten Karsdal, Nordic Bioscience Biomarkers and Research, Neurodegenerative Diseases, Herlev, Denmark; Anders Lonneborg and Magnus Sjogren, DiaGenic ASA, Oslo, Norway; William Hu, Department of Neurology, Center for Neurodegenerative Disease Research, Emory University School of Medicine, Atlanta, USA; Tony Wyss-Coray, Department of Neurology and Neurological Sciences, Stanford University School of Medicine, Stanford, California, USA; Joyce Suhy, SynarcImaging, San Fransisco, CA, USA; Dan Perry, Alliance for Aging Research, Washington, DC, USA; Rachel L. Nosheny, La Jolla, CA, and Stanford, CA, USA; Hugo Vanderstiechele, AD x Neurosciences, Gent, Belgium; Steven Warring, Marshfield Clinic; Donald Royal, University of Texas Health Science Center – San Antonio, TX, USA; George Perry, University of Texas San Antonio, TX, USA
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference
- 1.Ioannidis JPA. Why Most Published Research Findings Are False. PLoS Med. 2005;2:e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins FS, Tabak L. NIH plans to enhance reproducibility. Nature. 2014;505:612–613. doi: 10.1038/505612a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trouble at the lab. [Accessed February 27, 2014];The Economist 2013. Available at http://www.economist.com/news/briefing/21588057-scientists-think-science-self-correcting-alarming-degree-it-not-trouble.
- 4.Prinz F, Schlange T, Asadullah K. Believe it or not: How much can we rely on published data on potential drug targets? Nat Rev Drug Discov. 2011;10:712–713. doi: 10.1038/nrd3439-c1. [DOI] [PubMed] [Google Scholar]
- 5.Thies W, Bleiler L Alzheimer's Association. 2013 Alzheimer's disease facts and figures. Alzheimers Dement. 2013;9:208–245. doi: 10.1016/j.jalz.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary Costs of Dementia in the United States. N Engl J Med. 2013;368:1326–1334. doi: 10.1056/NEJMsa1204629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alzheimer's Association. Changing the trajectory of Alzheimer's disease. 2010 Available at http://www.alz.org/documents_custom/trajectory.pdf.
- 8.Henriksen K, O'Bryant S, Hampel H, Trojanowski JQ, Montine TJ, Jeromin A, et al. The future of blood-based biomarkers for Alzheimer's disease. Alzheimers Dement. 2014;10:115–131. doi: 10.1016/j.jalz.2013.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thal LJ, Kantarci K, Reiman EM, Klunk WE, Weiner MW, Zetterberg H, et al. The role of biomarkers in clinical trials for Alzheimer disease. Alzheimer Dis Assoc Disord. 2006;20:6–15. doi: 10.1097/01.wad.0000191420.61260.a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schneider P, Hampel H, Buerger K. Biological marker candidates of alzheimer's disease in blood, plasma, and serum. CNS Neurosci Ther. 2009;15:358–374. doi: 10.1111/j.1755-5949.2009.00104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anonymous. Consensus report of the Working Group on: "Molecular and Biochemical Markers of Alzheimer's Disease". The Ronald and Nancy Reagan Research Institute of the Alzheimer's Association and the National Institute on Aging Working Group. Neurobiol Aging. 1998;19:109–116. [see comment][erratum appears in Neurobiol Aging 1998 May-Jun;19(3):285] [PubMed] [Google Scholar]
- 12.Blennow K. Biomarkers in Alzheimer's disease drug development. Nat Med. 2010;16:1218–1222. doi: 10.1038/nm.2221. [DOI] [PubMed] [Google Scholar]
- 13.Petersen RC, Trojanowski JQ. Use of Alzheimer disease biomarkers: Potentially yes for clinical trials but not yet for clinical practice. JAMA. 2009;302:436–437. doi: 10.1001/jama.2009.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hampel H, Lista S. Use of biomarkers and imaging to assess pathophysiology, mechanisms of action and target engagement. J Nutr Health Aging. 2013;17:54–63. doi: 10.1007/s12603-013-0003-1. [DOI] [PubMed] [Google Scholar]
- 15.Blennow K, Hampel H, Zetterberg H. Biomarkers in amyloid-β immunotherapy trials in Alzheimer’s disease. Neuropsychopharmacology. 2014;39:189–201. doi: 10.1038/npp.2013.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blennow K, Hampel H, Weiner M, Zetterberg H. Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat Rev Neurol. 2010;6:131–144. doi: 10.1038/nrneurol.2010.4. [DOI] [PubMed] [Google Scholar]
- 17.Mattsson N, Andreasson U, Persson S, Arai H, Batish SD, Bernardini S, et al. The Alzheimer's Association external quality control program for cerebrospinal fluid biomarkers. Alzheimers Dement. 2011;7:386–395. doi: 10.1016/j.jalz.2011.05.2243. e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ray S, Britschgi M, Herbert C, Takeda-Uchimura Y, Boxer A, Blennow K, et al. Classification and prediction of clinical Alzheimer's diagnosis based on plasma signaling proteins. Nat Med. 2007;13:1359–1362. doi: 10.1038/nm1653. [DOI] [PubMed] [Google Scholar]
- 19.Soares HD, Chen Y, Sabbagh M, Rohrer A, Schrijvers E, Breteler M. Identifying early markers of Alzheimer's disease using quantitative multiplex proteomic immunoassay panels. Ann NY Acad Sci. 2009;1180:56–67. doi: 10.1111/j.1749-6632.2009.05066.x. [DOI] [PubMed] [Google Scholar]
- 20.Eli Lilly and Company. Apr 6; https://investor.lilly.com/releasedetail2.cfm?ReleaseID=662647.
- 21.Booij BB, Lindahl T, Wetterberg P, Skaane NV, Saebo S, Feten G, et al. A gene expression pattern in blood for the early detection of Alzheimer's disease. J Alzheimers Dis. 2011;23:109–119. doi: 10.3233/JAD-2010-101518. [DOI] [PubMed] [Google Scholar]
- 22.Buerger K, Ernst A, Ewers M, Uspenskaya O, Omerovic M, Morgenthaler NG, et al. Blood-based microcirculation markers in Alzheimer's disease-diagnostic value of midregional pro-atrial natriuretic peptide/C-terminal endothelin-1 precursor fragment ratio. Biol Psychiatry. 2009;65:979–984. doi: 10.1016/j.biopsych.2009.01.032. [DOI] [PubMed] [Google Scholar]
- 23.Laske C, Leyhe T, Stransky E, Hoffmann N, Fallgatter AJ, Dietzsch J. Identification of a blood-based biomarker panel for classification of Alzheimer's disease. Int J Neuropsychopharmacol. 2011;14:1147–1155. doi: 10.1017/S1461145711000459. [DOI] [PubMed] [Google Scholar]
- 24.Laske C, Schmohl M, Leyhe T, Stransky E, Maetzler W, Berg D, et al. Immune profiling in blood identifies sTNF-R1 performing comparably well as biomarker panels for classification of Alzheimer's disease patients. J Alzheimers Dis. 2013;34:367–375. doi: 10.3233/JAD-121558. [DOI] [PubMed] [Google Scholar]
- 25.O'Bryant SE, Xiao G, Barber R, Reisch J, Doody R, Fairchild T, et al. A serum protein-based algorithm for the detection of Alzheimer disease. Arch Neurol. 2010;67:1077–1081. doi: 10.1001/archneurol.2010.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Bryant SE, Xiao G, Barber R, Huebinger R, Wilhelmsen K, Edwards M, et al. A blood-based screening tool for Alzheimer's disease that spans serum and plasma: findings from TARC and ADNI. PLoS One. 2011;6:e28092. doi: 10.1371/journal.pone.0028092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nagele E, Han M, DeMarshall C, Belinka B, Nagele R. Diagnosis of Alzheimer's disease based on disease-specific autoantibody profiles in human sera. PLoS One. 2011;6:e23112. doi: 10.1371/journal.pone.0023112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reddy MM, Wilson R, Wilson J, Connell S, Gocke A, Hynan L, et al. Identification of candidate IgG biomarkers for Alzheimer's disease via combinatorial library screening. Cell. 2011;144:132–142. doi: 10.1016/j.cell.2010.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Doecke JD, Laws SM, Faux NG, Wilson W, Burnham SC, Lam CP, et al. Blood-based protein biomarkers for diagnosis of Alzheimer disease. Arch Neurol. 2012;69:1318–1325. doi: 10.1001/archneurol.2012.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu WT, Holtzman DM, Fagan AM, Shaw LM, Perrin R, Arnold SE, et al. Plasma multianalyte profiling in mild cognitive impairment and Alzheimer Disease. Neurology. 2012;79:897–905. doi: 10.1212/WNL.0b013e318266fa70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O'Bryant SE, Xiao G, Barber R, Reisch J, Hall J, Cullum CM, et al. A blood-based algorithm for the detection of Alzheimer's disease. Dement Geriatr Cogn Disord. 2011;32:55–62. doi: 10.1159/000330750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fagan AM, Roe CM, Xiong C, Mintun MA, Morris JC, Holtzman DM. Cerebrospinal fluid tau/β-amyloid42 ratio as a prediction of cognitive decline in nondemented older adults. Arch Neurol. 2007;64:343–349. doi: 10.1001/archneur.64.3.noc60123. [DOI] [PubMed] [Google Scholar]
- 33.Hansson O, Zetterberg H, Buchhave P, Londos E, Blennow K, Minthon L. Association between CSF biomarkers and incipient Alzheimer's disease in patients with mild cognitive impairment: A follow-up study. Lancet Neurol. 2006;5:228–234. doi: 10.1016/S1474-4422(06)70355-6. [DOI] [PubMed] [Google Scholar]
- 34.Kiddle SJ, Sattlecker M, Proitsi P, Simmons A, Westman E, Bazenet C, et al. Candidate blood proteome markers of Alzheimer’s disease onset and progression: a systematic review and replicaiton study. J Alzheimer Dis. 2014;38:515–531. doi: 10.3233/JAD-130380. [DOI] [PubMed] [Google Scholar]
- 35.Lista S, Faltraco F, Prvulovic D, Hampel H. Blood and plasma-based proteomic biomarker research in Alzheimer's disease. Prog Neurobiol. 2013;101–102:1–17. doi: 10.1016/j.pneurobio.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 36.Lista S, Faltraco F, Hampel H. Biological and methodological challenges of blood-based proteomics in the field of neurological research. Prog Neurobiol. 2013;101–102:18–34. doi: 10.1016/j.pneurobio.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 37.Rai AJ, Vitzthum F. Effects of preanalytical variables on peptide and protein measurements in human serum and plasma: Implications for clinical proteomics. Expert Rev Proteomics. 2006;3:409–426. doi: 10.1586/14789450.3.4.409. [DOI] [PubMed] [Google Scholar]
- 38.Tatsumi N, Miwa S, Lewis SM for the International Society of Hematology and the International Council for Standardization in Haematology. Specimen collection, storage, and transmission to the labortory for hematological tests. Int J Hematol. 2002;75:261–268. doi: 10.1007/BF02982039. [DOI] [PubMed] [Google Scholar]
- 39.Narayanan S. Effect of anticoagulants used for blood collection on laboatory tests. Proc JCLA. 1993;7:1–10. [Google Scholar]
- 40.Weber M, Rabenau B, Stanisch M, Nef HM, Mollmann H, Elsasser A, et al. Influence of sample type on soluble CD40 ligand assessment in patients with acute coronary syndromes. Thromb Res. 2007;120:811–814. doi: 10.1016/j.thromres.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 41.Issaq HJ, Xiao Z, Veenstra TD. Serum and plasma proteomics. Chemical Reviews. 2007;107:3601–3620. doi: 10.1021/cr068287r. [DOI] [PubMed] [Google Scholar]
- 42.Galasko D, Golde TE. Biomarkers for Alzheimer's disease in plasma, serum and blood -Conceptual and practical problems. Alzheimers Res Ther. 2013;5:10. doi: 10.1186/alzrt164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rembach A, Ryan TM, Roberts BR, Boecke JD, Wilson WJ, Watt AD, et al. Progress towards a consensus on biomarkers for Alzheimer's disease: A review of peripheral analytes. Biomark Med. 2013;7:641–662. doi: 10.2217/bmm.13.59. [DOI] [PubMed] [Google Scholar]
- 44.Watt AD, Perez KA, Rembach AR, Masters CL, Villemagne VL, Barnham KJ. Variability in blood-based amyloid-β assays: The need for consensus on pre-analytical processing. J Alzheimers Dis. 2012;30:323–336. doi: 10.3233/JAD-2012-120058. [DOI] [PubMed] [Google Scholar]
- 45.Vanderstichele H, Van Kerschaver E, Hesse C, Davidsson P, Buyse MA, Andreasen N, et al. Standardization of measurement of β-amyloid (1–42) in cerebrospinal fluid and plasma. Amyloid. 2000;7:245–258. doi: 10.3109/13506120009146438. [DOI] [PubMed] [Google Scholar]
- 46.Carrillo MC, Blennow K, Soares H, Lewczuk P, Mattsson N, Oberoi P, et al. Global standardization measurement of cerebral spinal fluid for Alzheimer's disease: An update from the Alzheimer's Association Global Biomarkers Consortium. Alzheimers Dement. 2013;9:137–140. doi: 10.1016/j.jalz.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 47.Mattsson N, Andreasson U, Persson S, Carrillo MC, Collins S, Chalbot S, et al. CSF biomarker variability in the Alzheimer's Association quality control program. Alzheimers Dement. 2013;9:251–261. doi: 10.1016/j.jalz.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Cancer Institute. NCI best practices for biospecimen resources 2007. http://biospecimens.cancer.gov/bestpractices/2011-NCIBestPractices.pdf.
- 49.De Paoli P. Biobanking in microbiology: From sample collection to epidemiology, diagnosis and research. FEMS Microbiol Rev. 2005;29:897–910. doi: 10.1016/j.femsre.2005.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rai AJ, Gelfand CA, Haywood BC, Warunek DJ, Yi J, Schuchard MD, et al. HUPO Plasma Proteome Project specimen collection and handling: Towards the standardization of parameters for plasma proteome samples. Proteomics. 2005;5:3262–3277. doi: 10.1002/pmic.200401245. [DOI] [PubMed] [Google Scholar]
- 51.Apple FS, Jesse RL, Newby LK, Wu AH, Christenson RH. National Academy of Clinical Biochemistry and IFCC Committee for Standardization of Markers of Cardiac Damage Laboratory Medicine Practice Guidelines: Analytical issues for biochemical markers of acute coronary syndromes. Circulation. 2007;115:e352–e355. doi: 10.1161/CIRCULATIONAHA.107.182881. [DOI] [PubMed] [Google Scholar]
- 52.Lippi G, Becan-McBride K, Behúlová D, Bowen RA, Church S, Delanghe J, et al. Preanalytical quality improvement: In quality we trust. Clin Chem Lab Med. 2013;51:229–241. doi: 10.1515/cclm-2012-0597. [DOI] [PubMed] [Google Scholar]
- 53.Ceriotti F, Cappelletti P, Caputo M, Di Serio F, Messeri G, Ottomano C, et al. A risk-analysis approach to the evaluation of analytical quality. Clin Chem Lab Med. 2011;50:67–71. doi: 10.1515/CCLM.2011.740. [DOI] [PubMed] [Google Scholar]
- 54.Snyder HM, Carrillo MC, Grodstein F, Henriksen K, Jeromin A, Lovestone S, et al. Developing novel blood-based biomarkers for Alzheimer’s disease. Alzheimers Dement. 2010;10:109–114. doi: 10.1016/j.jalz.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. [Accessed on Feburary 27, 2014]; http://arcresearch.eu/
- 56. [Accessed on Feburary 27, 2014]; http://www.adcs.org/
- 57. [Accessed on Feburary 27, 2014]; http://www.adni-info.org/
- 58.Ellis KA, Bush AI, Darby D, De Fazio D, Foster J, Hudson P, et al. The Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging: methodology and baseline characteristics of 1112 individuals recruited for longitudinal study of Alzheimer’s disease. Int Psychogeriatr. 2009;21:672–687. doi: 10.1017/S1041610209009405. [DOI] [PubMed] [Google Scholar]
- 59. [Accessed on Feburary 27, 2014]; http://www.aibl.csiro.au/
- 60.Morris JC, Aisen PS, Bateman RJ, Benzinger TL, Cairns NJ, Fagan AM, et al. Developing an international network for Alzheimer’s research: the Dominantly Inherited Alzheimer Network. Clinical Investigation. 2012;2:975–984. doi: 10.4155/cli.12.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. [Accessed on Feburary 27, 2014]; http://www.dian-info.org/
- 62.Bateman RJ, Aisen PS, De Strooper B, Fox NC, Lemere CA, Ringman JM, et al. Autosomal-dominant Alzheimer's disease: a review and proposal for the prevention of Alzheimer's disease. Alzheimers Res Ther. 2011;3:1. doi: 10.1186/alzrt59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. [Accessed on Feburary 28, 2014]; http://web.unthsc.edu/research/IAADR.
- 64. [Accessed on Feburary 28, 2014]; http://www.kcl.ac.uk/
- 65.Honig L, Kukull W, Mayeux R. Atherosclerosis and AD: Analysis of data from the US National Alzheimer’s Coordinating Center. Neurology. 2005;64:494–500. doi: 10.1212/01.WNL.0000150886.50187.30. [DOI] [PubMed] [Google Scholar]
- 66. [Accessed on Feburary 27, 2014]; http://www.txalzresearch.org/
- 67.Coats M, Morris JC. Antecedent biomarkers of Alzheimer’s disease: The adult children study. J Geriatr Psychiatry Neurol. 2005;18:242–244. doi: 10.1177/0891988705281881. [DOI] [PubMed] [Google Scholar]
- 68. [Accessed on Feburary 27, 2014]; http://alzheimer.wustl.edu/
- 69.Bonini P, Plebani M, Ceriotti F, Rubboli F. Errors in laboratory medicine. Clin Chem. 2002;48:691–698. [PubMed] [Google Scholar]
- 70.Boone DJ, Steindel SD, Herron R, Howanitz PJ, Bachner P, Meier F, et al. Transfusion medicine monitoring practices: A study of the College of American Pathologists/Centers for Disease Control and Prevention Outcomes Working Group. Arch Pathol Lab Med. 1995;119:999–1006. [PubMed] [Google Scholar]
- 71.Plebani M, Carraro P. Mistakes in a stat laboratory: Types and frequency. Clin Chem. 1997;43:1348–1351. [PubMed] [Google Scholar]
- 72.Schleicher E. The clinical chemistry laboratory: Current status, problems and diagnostic prospects. Anal Bioanal Chem. 2006;384:124–131. doi: 10.1007/s00216-005-0185-4. [DOI] [PubMed] [Google Scholar]
- 73.Ferguson RE, Hochstrasser DF, Banks RE. Impact of preanalytical variables on the analysis of biological fluids in proteomic studies. Proteomics Clin Appl. 2007;1:739–746. doi: 10.1002/prca.200700380. [DOI] [PubMed] [Google Scholar]
- 74.Becan-McBride K. Laboratory sampling: Does the process affect the outcome? J Intraven Nurs. 1999;22:137–142. [PubMed] [Google Scholar]
- 75.Dominguez-Rodriguez A, Abreu-Gonzalez P. Preanalytic conditions of the C-reactive protein are of paramount importance to use as a predictor of cardiovascular disease in clinical practice. Int J Cardiol. 2012;158:467. doi: 10.1016/j.ijcard.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 76.Wipfler P, Heikkinen A, Harrer A, Pilz G, Kunz A, Golaszewski SM, et al. Circadian rhythmicity of inflammatory serum parameters: A neglected issue in the search of biomarkers in multiple sclerosis. J Neurol. 2013;260:221–227. doi: 10.1007/s00415-012-6622-3. [DOI] [PubMed] [Google Scholar]
- 77.Lachno DR, Vanderstichele H, de Groote G, Kostanjevecki V, De Meyer G, Siemers ER, et al. The influence of matrix type, diurnal rhythm and sample collection and processing on the measurement of plasma β-amyloid isoforms using the INNO-BIA plasma AB forms multiplex assay. J Nutr Health Aging. 2009;13:220–225. doi: 10.1007/s12603-009-0062-5. [DOI] [PubMed] [Google Scholar]
- 78.Domínguez Rodríguez A, Abreu González P. Diurnal variations in biomarkers used in cardiovascular medicine: clinical significance. Rev Esp Cardiol. 2009;62:1340–1341. doi: 10.1016/s1885-5857(09)73367-5. author reply 1342–1343. [DOI] [PubMed] [Google Scholar]
- 79.CLSI. Procedures for handling and processing of blood specimens for common laboratory tests; Approved Guideline - Fourth Edition. 30(10) H18-A4. [Google Scholar]
- 80.Kennedy C, Angermuller S, King R, Noviello S, Walker J, Warden J, et al. A comparison of hemolysis rates using intravenous catheters versus venipuncture tubes for obtaining blood samples. J Emerg Nurs. 1996;22:566–569. doi: 10.1016/s0099-1767(96)80213-3. [DOI] [PubMed] [Google Scholar]
- 81.Sharp MK, Mohammad SF. Scaling of hemolysis in needles and catheters. Ann Biomed Eng. 1998;26:788–797. doi: 10.1114/1.65. [DOI] [PubMed] [Google Scholar]
- 82.Bowen RA, Hortin GL, Csako G, Otañez OH, Remaley AT. Impact of blood collection devices on clinical chemistry assays. Clin Biochem. 2010;43:4–25. doi: 10.1016/j.clinbiochem.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 83.Dugan L, Leech L, Speroni KG, Corriher JB. Factors affecting hemolysis rates in blood samples drawn from newly placed IV sites in the emergency department. J Emerg Nurs. 2005;31:338–345. doi: 10.1016/j.jen.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 84.Stankovic AK, Smith S. Elevated serum potassium values: the role of preanalytic variables. Am J Clin Pathol. 2004;121(Suppl):S105–S112. doi: 10.1309/UEPQUM11WH9P8JNY. [DOI] [PubMed] [Google Scholar]
- 85.Narayanan SLF. Sampling technique. In: Shy W, editor. Therapeutic drug monitoring and toxicology by liquid chromatography. New York, NY: Marcel Dekker, Inc; 1985. pp. 79–88. [Google Scholar]
- 86.Lippi G, Blanckaert N, Bonini P, Green S, Kitchen S, Palicka V, et al. Haemolysis: an overview of the leading cause of unsuitable specimens in clinical laboratories. Clin Chem Laboratory Med. 2008;46:764–772. doi: 10.1515/CCLM.2008.170. [DOI] [PubMed] [Google Scholar]
- 87.Tammen H. Specimen collection and handling: standardization of blood sample collection. Methods Mol Biol. 2008;428:35–42. doi: 10.1007/978-1-59745-117-8_2. [DOI] [PubMed] [Google Scholar]
- 88.Burtis CA, Ashwood E. Tietz Fundamentals of Clinical Chemistry. Philadelphia, PA, USA: W.B. Saunders; 2001. [Google Scholar]
- 89.Ernst DJ. Plastic collection tubes decrease risk of employee injury. MLO Med Lab Obs. 2001;33:44–46. 48, 50. [PubMed] [Google Scholar]
- 90.Perret-Liaudet A, Pelpel M, Tholance Y, Dumont B, Vanderstichele H, Zorzi W, et al. Risk of alzheimer's disease biological misdiagnosis linked to cerebrospinal collection tubes. J Alzheimers Dis. 2012;31:13–20. doi: 10.3233/JAD-2012-120361. [DOI] [PubMed] [Google Scholar]
- 91.Lewczuk P, Beck G, Esselmann H, Bruckmoser R, Zimmermann R, Fiszer M, et al. Effect of sample collection tubes on cerebrospinal fluid concentrations of tau proteins and amyloid β peptides. Clin Chem. 2006;52:332–334. doi: 10.1373/clinchem.2005.058776. [DOI] [PubMed] [Google Scholar]
- 92.Perret-Liaudet A, Pelpel M, Tholance Y, Dumont B, Vanderstichele H, Zorzi W, et al. Cerebrospinal fluid collection tubes: A critical issue for alzheimer disease diagnosis. Clin Chem. 2012;58:787–789. doi: 10.1373/clinchem.2011.178368. [DOI] [PubMed] [Google Scholar]
- 93.Pica-Mendez AM, Tanen M, Dallob A, Tanaka W, Laterza OF. Nonspecific binding of Aβ42 to polypropylene tubes and the effect of Tween-20. Clin Chim Acta. 2010;411:1833. doi: 10.1016/j.cca.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 94.Rehak NN, Chiang BT. Storage of whole blood: Effect of temperature on the measured concentration of analytes in serum. Clin Chem. 1988;34:2111–2114. [PubMed] [Google Scholar]
- 95.Boyanton BL, Jr., Blick KE. Stability studies of twenty-four analytes in human plasma and serum. Clin Chem. 2002;48:2242–2247. [PubMed] [Google Scholar]
- 96.Mischak H, Apweiler R, Banks RE, Conaway M, Coon J, Dominiczak A, et al. Clinical proteomics: A need to define the field and to begin to set adequate standards. Proteomics Clin Appl. 2007;1:148–156. doi: 10.1002/prca.200600771. [DOI] [PubMed] [Google Scholar]
- 97.Murphy BM, Swarts S, Mueller BM, van der Geer P, Manning MC, Fitchmun MI. Protein instability following transport on dry ice. Nat Methods. 2013;10:278–298. doi: 10.1038/nmeth.2409. [DOI] [PubMed] [Google Scholar]
- 98. [Accessed on June 20, 2014]; http://www.guideline.gov/content.aspx?id=37621.
- 99.O'Bryant SE. Using blood markers for Alzheimer disease in clinical practice? Neurology. 2012;79:846–847. doi: 10.1212/WNL.0b013e318266fd21. [DOI] [PubMed] [Google Scholar]
- 100.Mayeux R. Evaluation and use of diagnostic tests in Alzheimer's disease. Neurobiol Aging. 1998;19:139–143. doi: 10.1016/s0197-4580(98)00014-1. [DOI] [PubMed] [Google Scholar]
- 101.Breteler MM. Mapping out biomarkers for Alzheimer disease. JAMA. 2011;305:304–305. doi: 10.1001/jama.2010.2017. [DOI] [PubMed] [Google Scholar]
- 102.Institute of Medicine. [Accessed on Feburary 28,2014];Evolution of Translational Omics: Lessons Learned and the Path Forward Report Brief 2012. http://www.iom.edu/Reports/2012/Evolution-of-Translational-Omics.aspx. [PubMed]