Abstract
Background and Purpose
Premature ventricular complexes (PVCs) detected from long-term electrocardiogram (ECG) recordings have been associated with an increased risk of ischemic stroke. Whether PVCs seen on routine ECG, commonly used in clinical practice, are associated with an increased risk of ischemic stroke remains unstudied.
Methods
This analysis included 24,460 participants (age 64.5+9.3 years, 55.1% Female, 40.0% African Americans) from the REasons for Geographic And Racial Differences in Stroke (REGARDS) study who were free of stroke at the time of enrollment. PVCs were ascertained from baseline ECG (2003-2007), and incident stroke cases through 2011 were confirmed by an adjudication committee.
Results
A total of 1,415 (5.8%) participants had at least one PVC at baseline, and 591 developed incident ischemic stroke during an average (SD) follow-up of 6.0 (2.0) years. In a Cox Proportional hazards model adjusted for age, sex, race, geographic region, education, prior heart disease, systolic blood pressure, blood pressure lowering medications, current smoking, diabetes, left ventricular hypertrophy by ECG, aspirin use and warfarin use, presence of PVCs was associated with 38% increased risk of ischemic stroke (HR (95% CI): 1.38 (1.05, 1.81)).
Conclusions
PVCs are common on routine screening ECGs, and are associated with an increased risk of ischemic stroke.
Keywords: Premature Ventricular Complexes, Ischemic Stroke, REGARDS
Introduction
Premature ventricular complexes (PVCs) are common findings on the resting electrocardiogram (ECG).1, 2 In a recent report from the Atherosclerosis Risk in Communities (ARIC) study, presence of PVCs on 2-minute ECG rhythm strips was associated with a higher risk of ischemic stroke.3 Notably, however, recording 2-minute ECG is not a common practice in clinical settings. Whether PVCs detected by the more conventional short term routine ECG are associated with increased risk of ischemic stroke remains unknown.
Methods
The goals and design of the REasons for Geographic and Racial Differences in Stroke (REGARDS) study have been published.4 REGARDS was designed to investigate causes of regional and racial disparities in stroke mortality, oversampling blacks and residents of the southeastern (stroke belt) United States. Individuals were recruited from a commercially available list of residents using mail and telephone contact. Demographic information and medical history were obtained by standardized telephone interview. A brief physical examination was conducted after the telephone interview, including standardized measurements of risk factors, collection of blood and urine, and recording of resting ECG. Participants are followed-up every 6 months by telephone for possible stroke events. Participants provided informed consent and the study was approved by all institutional review boards.
Of the 30,239 participants enrolled in REGARDS, we excluded 2953 with prevalent stroke or transient ischemic attack, 698 with poor quality ECG, and 2128 with missing covariates.
Details on stroke events adjudication have been previously published.5 In summary, reports of possible stroke during follow-up generated a request for retrieval of medical records that were centrally adjudicated by physicians. Stroke events were defined following the World Health Organization (WHO) definition.6 Events not meeting the WHO's definition but with symptoms lasting <24 hours and neuroimaging consistent with acute ischemia were classified as “clinical strokes.” This analysis included WHO-defined and clinical ischemic stroke and its subtype cardio-embolic stroke. Participants with incident hemorrhagic stroke were excluded.7
Statistical analysis
Cox proportional hazards models were used to examine the association between PVCs with incident ischemic stroke through 2011 with incremental adjustment for potential confounders as follows: 1) age, sex, race, geographic region and education; 2) further adjustment for blood pressure lowering medications, systolic blood pressure, current smoking, diabetes, left ventricular hypertrophy, atrial fibrillation, prior heart disease, 5) further adjustment for warfarin use, aspirin use.
All statistical computations were performed using SAS-9.2, SAS Institute, Cary, NC. A p-value < 0.05 was considered statistically significant.
Results
Out of the 24,460 participants (age 64.5±9.3 years, 55.1% female, 40.0% African Americans) included in this analysis, 1,415 (5.8%) had at least one PVC at baseline. Differences in the characteristics of participants with and without PVCs are shown in Table 1.
Table 1. Baseline characteristics of the participants by presence of premature ventricular complexes (PVCs).
| PVCs | P-value | ||
|---|---|---|---|
|
|
|||
| Present (n = 1,415) | Absent (n = 23,045) | ||
| Age (years) | 68.3±9.2 | 64.3±9.3 | <0.01 |
| Women | 642 (45.4) | 12828 (55.7) | <0.01 |
| African American | 593 (41.9) | 9193 (39.9) | 0.13 |
| Education | |||
| No high school | 219 (15.5) | 2570 (11.1) | <0.01 |
| High school/no college | 372 (26.3) | 5889 (25.6) | |
| College or professional | 824 (58.2) | 14586 (63.3) | |
| Geographic Region | 0.03 | ||
| Non-Belt | 667 (47.2) | 10128 (43.9) | |
| Belt | 480 (33.9) | 8019 (34.8) | |
| Buckle | 268 (19.0) | 4898 (21.3) | |
| Current smoker | 184 (13.0) | 3219 (14.0) | 0.31 |
| Prior heart disease | 359 (25.4) | 3509 (12.2) | <0.01 |
| Hypertension | 915 (64.7) | 12958 (56.2) | <0.01 |
| Systolic blood pressure (mm Hg) | 130.1±16.9 | 126.9 ± 16.4 | <0.01 |
| Diabetes | 309 (21.8) | 4408 (19.1) | 0.01 |
| Body mass index (kg/m2) | 29.2±6.1 | 29.3±6.2 | 0.61 |
| Atrial Fibrillation | 134 (9.7) | 1768 (7.8) | 0.01 |
| Left ventricular hypertrophy | 158 (11.2) | 2171 (9.4) | 0.03 |
| Warfarin use | 49 (3.5) | 620 (2.7) | 0.08 |
| Aspirin use | 681 (48.1) | 9429 (40.9) | <0.01 |
During an average (SD) follow-up of 6.0 (2.0) years, 591 participants developed ischemic stroke, of which 162 was defined as cardio-embolic stroke. The incidence rate of ischemic stroke was higher in those with vs. without PVCs (6.7 vs. 4.2 per 1000 person years, p<0.01). Figure 1 shows the cumulative proportion of stroke events by the PVCs status.
Figure 1. Cumulative stroke rates in participants with and without premature ventricular complexes (PVCs).
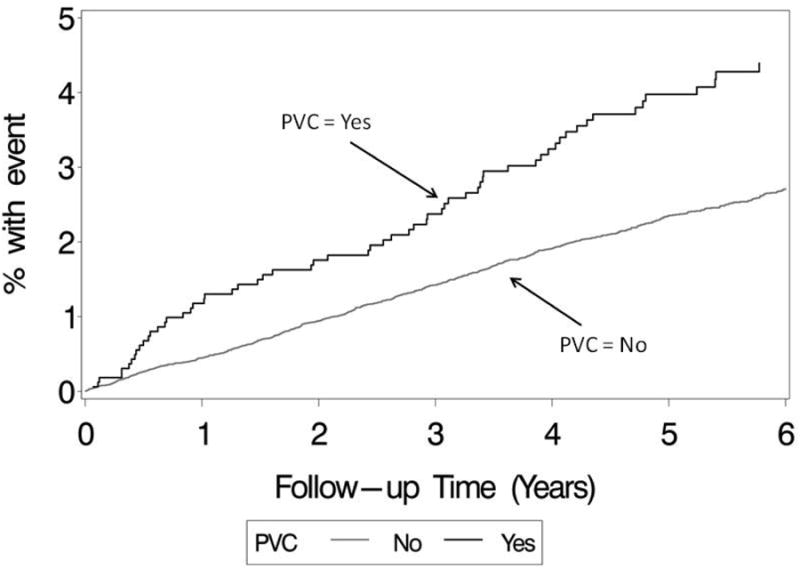
Table 2 shows the results of the association between PVCs and ischemic stroke. PVCs was associated with a 38% (95% CI: 5% to 81%) increased risk of ischemic stroke. The association between PVCs and cardio-embolic stroke was of similar strength (Hazard ratio (95%CI): 1.47(0.98, 2.43)), but the association did not reach a statistical significance possibly because of lack of enough power.
Table 2. Premature ventricular complexes and risk of ischemic stroke.
| PVCs | Participants (n) | Events (n) | Model 1* | Model 2† | Model 3‡ |
|---|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |||
| Absent | 23045 | 532 | Reference | Reference | Reference |
| Present | 1415 | 59 | 1.40 (1.07, 1.83) | 1.39 (1.06, 1.82) | 1.38 (1.05, 1.81) |
PVCs = Premature ventricular complexes, HR = Hazard Ratio, CI = Confidence Interval
Adjusted for age, sex, race, geographic region, and education level
Adjusted for model 1 covariates plus, prior heart disease, systolic blood pressure, use of antihypertensive medication, left ventricular hypertrophy by ECG, atrial fibrillation, diabetes, current smoking
Adjusted for model 2 covariates plus, use of warfarin and aspirin
Discussion
In this analysis from the REGARDS study, one of the largest US cohort studies, presence of PVCs on routine screening ECG was associated with higher risk of ischemic stroke. To our knowledge, this is the first study examining the relationship between PVCs detected by routine ECG recording and incident ischemic stroke. Previous studies were based on long term ECG recordings that are not routinely used at clinical settings.3, 8
The pathophysiologic mechanism through which PVCs may increase stroke risk is not yet well understood. Presence of PVCs has been associated with an increased risk of atrial fibrillation.3, 9 This means that the association between PVCs and ischemic stroke could potentially be mediated by AF, though in our study the association between PVC and stroke didn't change after adjusting for baseline AF. PVCs are known to cause sudden changes in heart rate, blood pressure, and stroke volume.2 Also, frequent PVCs have been associated with an abnormal left ventricular diastolic function and have the potential for cardiac remodeling,10, 11 which in turn may enhance thromboembolism.
Strengths of our study include its large sample size, the length and thoroughness of its follow-up, and its diverse population. Few key limitations include our inability to explore dose-response effect, and mediation of putative association through incident AF (as seen in the ARIC study3) because of lack of data.
In conclusion, we showed that presence of PVCs on a routine ECG is associated with increased risk of ischemic stroke, independent of traditional risk factors of stroke. These findings suggest that incidentally detected PVCs, typically dismissed as benign findings, may be a risk marker for future stroke. Whether suppression of frequent PVCs with beta blockers or use of antiplatelet agents may reduce observed stroke risk remains unstudied.
Acknowledgments
The authors thank the participants, staff, and investigators, of the REGARDS study for their valuable contributions. A full list of REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Funding: This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health (NIH), and Department of Health and Human Services (DHHS).
Footnotes
Disclosures: Dr. Kissela participates in stroke event adjudication in a clinical trial.
References
- 1.Simpson RJ, Jr, Cascio WE, Schreiner PJ, Crow RS, Rautaharju PM, Heiss G. Prevalence of premature ventricular contractions in a population of african american and white men and women: The atherosclerosis risk in communities (aric) study. American heart journal. 2002;143:535–540. doi: 10.1067/mhj.2002.120298. [DOI] [PubMed] [Google Scholar]
- 2.Rautaharju P. Ectopic Ventricular Activity. In: Rautaharju P, Rautaharju F, editors. Investigative electrocardiology in epidemiological studies and clinical trials. 1st. London: Springer; 2007. p. 100.p. 112.3. [Google Scholar]
- 3.Agarwal SK, Heiss G, Rautaharju PM, Shahar E, Massing MW, Simpson RJ., Jr Premature ventricular complexes and the risk of incident stroke: The atherosclerosis risk in communities (aric) study. Stroke; a journal of cerebral circulation. 2010;41:588–593. doi: 10.1161/STROKEAHA.109.567800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 5.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Annals of neurology. 2011;69:619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO/MNH Task Force on Stroke and Other Cerebrovascular Disorders. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO task force on stroke and other cerebrovascular disorders. Stroke; a journal of cerebral circulation. 1989;20:1407–1431. doi: 10.1161/01.str.20.10.1407. [DOI] [PubMed] [Google Scholar]
- 7.Schneider AT, Kissela B, Woo D, Kleindorfer D, Alwell K, Miller R, et al. Ischemic stroke subtypes: A population-based study of incidence rates among blacks and whites. Stroke; a journal of cerebral circulation. 2004;35:1552–1556. doi: 10.1161/01.STR.0000129335.28301.f5. [DOI] [PubMed] [Google Scholar]
- 8.Engstrom G, Hedblad B, Juul-Moller S, Tyden P, Janzon L. Cardiac arrhythmias and stroke: Increased risk in men with high frequency of atrial ectopic beats. Stroke; a journal of cerebral circulation. 2000;31:2925–2929. doi: 10.1161/01.str.31.12.2925. [DOI] [PubMed] [Google Scholar]
- 9.Watanabe H, Tanabe N, Makiyama Y, Chopra SS, Okura Y, Suzuki H, et al. St-segment abnormalities and premature complexes are predictors of new-onset atrial fibrillation: The niigata preventive medicine study. American heart journal. 2006;152:731–735. doi: 10.1016/j.ahj.2006.05.032. [DOI] [PubMed] [Google Scholar]
- 10.Agarwal SK, Simpson RJ, Jr, Rautaharju P, Alonso A, Shahar E, Massing M, et al. Relation of ventricular premature complexes to heart failure (from the atherosclerosis risk in communities [aric] study) The American journal of cardiology. 2012;109:105–109. doi: 10.1016/j.amjcard.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Topaloglu S, Aras D, Cagli K, Yildiz A, Cagirci G, Cay S, et al. Evaluation of left ventricular diastolic functions in patients with frequent premature ventricular contractions from right ventricular outflow tract. Heart and vessels. 2007;22:328–334. doi: 10.1007/s00380-007-0978-9. [DOI] [PubMed] [Google Scholar]


