Abstract
Background
Previous studies have reported conflicting findings regarding how the incidence of heart failure (HF) following acute myocardial infarction (AMI) has changed over time, and data on contemporary national trends are sparse.
Methods and Results
Using a complete national sample of 2,789,943 AMI hospitalizations of Medicare fee-for-service beneficiaries from 1998-2010, we evaluated annual changes in the incidence of subsequent HF hospitalization and mortality using Poisson and survival analysis models. The number of patients hospitalized for HF within 1 year following AMI declined modestly from 16.1 per 100 person-years in 1998 to 14.2 per 100 person years in 2010 (p<0.001). After adjusting for demographic factors, a relative 14.6% decline for HF hospitalizations after AMI was observed over the study period (incidence risk ratio 0.854, 95% confidence interval [CI] 0.809-0.901). Unadjusted 1-year mortality following HF hospitalization after AMI was 44.4% in 1998, which decreased to 43.2% in 2004-2005, but then increased to 45.5% by 2010. After adjusting for demographic factors and clinical comorbidities, this represented a 2.4% relative annual decline (hazard ratio [HR] 0.976, 95% CI 0.974-0.978) from 1998 to 2007, but a 5.1% relative annual increase from 2007 to 2010 (HR 1.051, 95% CI 1.039-1.064).
Conclusions
In a national sample of Medicare beneficiaries, HF hospitalization following AMI decreased from 1998 to 2010, which may indicate improvements in the management of AMI. In contrast, survival after HF following AMI remains poor, and has worsened from 2007 to 2010, demonstrating that challenges still remain for the treatment of this high-risk condition after AMI.
Keywords: heart failure, acute myocardial infarction, mortality, epidemiology
Introduction
Heart failure (HF) is a common and well-recognized complication during hospitalization for acute myocardial infarction (AMI) that is associated with substantially higher risk of death. 1-4 In contrast, the incidence of HF occurring after AMI is less well characterized. Trends in the incidence of HF following AMI have been examined in two surveillance cohorts, but the findings from these studies have been conflicting— data from Olmsted County indicated that the incidence of HF after AMI has decreased from 1979 to 1994,5 while data from the Framingham Heart Study suggested an increase in HF incidence after AMI from 1970 to 1999. 6 However, both of these study cohorts were relatively small, were constrained to demographically and geographically homogeneous populations, and did not represent subsequent HF incidence in the context of contemporary management strategies for AMI.
As such, there is little contemporary data on HF incidence after AMI in practice settings that reflect modern management of AMI. Rapid adoption of routine invasive strategies7 and intensive pharmacotherapy 8-10 may have improved myocardial salvage following AMI, thus lowering the subsequent risk of developing HF. On the other hand, improving survival from AMI may have created a population with greater residual myocardial injury and higher risk for developing HF. 6 Complicating matters is that the overall incidence of AMI itself has decreased in the past decade 9, 11 which may have resulted in AMI cohorts that increasingly have consisted of patients who break through intensive pharmacotherapy and who are thus at different levels of risk for developing HF.
Accordingly, we sought to examine recent national trends in the incidence and outcomes of patients with HF hospitalization following AMI using a complete sample of fee-for-service Medicare beneficiaries hospitalized for AMI from 1998 to 2010. This analysis provides insight as to whether modern management strategies for AMI have been successful for preserving myocardial function in a general population. We hypothesize that HF hospitalization rates have declined due to improvements AMI care, but that patients who were hospitalized for HF after AMI continue to be at high risk for death.
Methods
Data Sources
A complete sample of fee-for-service Medicare beneficiaries who were hospitalized from 1998 to 2011 was identified using inpatient MedPAR files from the Centers for Medicare and Medicaid Services (CMS). These administrative billing claims included information on patient demographics (age, sex, race), admission and discharge dates, and principal and secondary diagnosis codes as coded by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Medicare denominator files were used to ascertain beneficiary eligibility and enrollment in fee-for-service Medicare.
Cohort inclusion and exclusion criteria
Subjects were included in the study cohort if they were discharged alive from an acute-care hospital for a principal discharge diagnosis of AMI with ICD-9-CM codes of 410.xx between 1998 and 2010. We excluded patients with a principal discharge diagnosis of ICD-9CM codes 410.x2, as these represent subsequent episodes of AMI care. Patients admitted and discharged alive within the same day also excluded, as these episodes of care unlikely represented AMI. We also excluded 1) beneficiaries <65 years of age; 2) beneficiaries without at least 1 year of Medicare fee-for-service enrollment after their index AMI hospitalization in order to fully assess comorbidities and outcomes; 3) beneficiaries who resided outside of the 50 continental states, the District of Columbia or Puerto Rico; and 4) beneficiaries with conflicting dates of death and hospitalization. The unit of observation for this study was a hospital admission for AMI for a particular Medicare fee-for-service beneficiary in a particular calendar year. If a beneficiary had more than one AMI admission during a given calendar year, we selected one AMI admission at random as the index hospitalization for the study cohort in order to estimate a representative risk for subsequent HF hospitalization for each calendar year. For patients who were subsequently transferred to another acute-care hospital for AMI after an initial AMI hospitalization, the hospitalization after transfer was considered as the index AMI hospitalization.
Outcomes
Our first study outcome was to evaluate changes in HF hospitalization within 1 year of AMI, as defined by an admission to an acute-care hospital for a principal discharge diagnosis of HF as defined by following ICD-9-CM codes: 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 404.03, 404.13, and 404.93 and 428.xx. Our second study outcome was to examine yearly changes in the mortality rate among patients who were hospitalized for HF after AMI. Dates of death were recorded in the Medicare vital status file which report both in-hospital and out-of-hospital deaths.
Statistical analysis
Baseline characteristics of the cohort were tabulated across four time periods (1998-2001, 2002-2004, 2005-2007, 2008-2010). Patient demographics were categorized by age (65-74, 75-84, 85 years or older), sex, and race (white, black, other). Race was ascertained using the Medicare denominator file, which uses patient-reported data from the Social Security Administration.12 Coexisting illnesses were classified according to the categorization used by CMS for the AMI 30-day mortality measure.13 To evaluate the statistical significance of changes across years in patient characteristics, we used the chi-squared test for age and race categories, analysis of variance for age, and the Cochran-Armitage test for comorbidities.
The incidence of HF hospitalization after AMI discharge was calculated for each calendar year by dividing the number of patients who were hospitalized for HF by person-years of follow-up. Differences over time in unadjusted HF hospitalization rates after AMI were assessed using the Wald test in Poisson models that included a continuous variable of cohort year. Additional Poisson models adjusted for age, sex, race and a dummy indicator variable for calendar year were constructed to evaluate how the incident risk ratio (IRR) for HF hospitalization after AMI changed for a given calendar year compared with the baseline year of 1998; in these models age and sex were aggregated to the year-level.
For the mortality analysis, we considered the admission date of the HF hospitalization following AMI as the initial “time zero” in order to calculate the proportion of patients who died within 1 year. Mortality was reported in terms of proportion of patients who died within 30-, 90-, 180- days and 1 year. Trends in unadjusted HF mortality after AMI were assessed using regression models with a continuous variable of cohort year. We then constructed Cox proportional hazards models to examine changes in mortality after HF following AMI, adjusting for demographics and comorbid conditions. These models included dummy indicator variables that represented how the hazard ratio (HR) for mortality changed for a given calendar year compared with the baseline year of 1998.
Analyses were conducted using SAS version 9.3 (SAS Institute Inc., Cary, North Carolina). Significance level was considered to be p<0.01 using two-sided tests. Institutional Review Board review and approval was obtained through the Yale University Human Investigation Committee. Medicare claims data were provided through a data use agreement with CMS.
Results
Baseline characteristics of AMI cohort
The study cohort consisted of 2,789,943 AMI hospitalizations from 1998 to 2010. The overall cohort was elderly with mean age of 78.5 years, (standard deviation 8.0) with a slight male predominance (50.2%). The cohort became significantly older in more recent subgroups from 1998 to 2010, with mean age increasing from 78.1 to 78.9 years (p<0.0001). The proportion of patients coded with pre-existing HF or HF during the AMI hospitalization was high over the study period (range 40.2%-40.5%). Specific comorbidities noted with increased prevalence over time included renal failure (8.0% to 27.9%) and disorders of fluid, electrolyte and acid-base (10.9% to 18.9%). (p<0.001) (Table 1) Some other comorbidities exhibited statistically significant changes over time due to large numbers, but were stable in terms of absolute differences.
Table 1.
Baseline characteristics of Medicare patients hospitalized for AMI
| 1998-2001 | 2002-2004 | 2005-2007 | 2008-2010 | All | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N (AMI hospitalizations) | 905168 | 720850 | 606779 | 557146 | 2789943 | |||||
| Age (years) | ||||||||||
| mean (standard deviation) | 78.1 (7.7) | 78.5 (7.9) | 78.8 (8.2) | 78.9 (8.4) | 78.5 (8.0) | |||||
| Age categories | ||||||||||
| 65-74 | 348818 | 38.5% | 264707 | 36.7% | 217467 | 35.8% | 204246 | 36.7% | 1035238 | 37.1% |
| 75-84 | 370825 | 41.0% | 293094 | 40.7% | 239354 | 39.4% | 207128 | 37.2% | 1110401 | 39.8% |
| 85+ | 185525 | 20.5% | 163049 | 22.6% | 149958 | 24.7% | 145772 | 26.2% | 644304 | 23.1% |
| Race-sex categories | ||||||||||
| White male | 410469 | 45.3% | 322018 | 44.7% | 273699 | 45.1% | 251869 | 45.2% | 1258055 | 45.1% |
| White female | 399235 | 44.1% | 315188 | 43.7% | 262074 | 43.2% | 236373 | 42.4% | 1212870 | 43.5% |
| Black male | 24896 | 2.8% | 21110 | 2.9% | 18104 | 3.0% | 17801 | 3.2% | 81911 | 2.9% |
| Black female | 35969 | 4.0% | 30374 | 4.2% | 25616 | 4.2% | 24779 | 4.4% | 116738 | 4.2% |
| Other male | 17083 | 1.9% | 16133 | 2.2% | 13803 | 2.3% | 13542 | 2.4% | 60561 | 2.2% |
| Other female | 17516 | 1.9% | 16027 | 2.2% | 13483 | 2.2% | 12782 | 2.3% | 59808 | 2.1% |
| Comorbidites | ||||||||||
| Coronary atherosclerosis | 594524 | 65.7% | 494104 | 68.5% | 413051 | 68.1% | 379412 | 68.1% | 1881091 | 67.4% |
| Congestive heart failure | 382911 | 42.3% | 306677 | 42.5% | 257475 | 42.4% | 223953 | 40.2% | 1171016 | 42.0% |
| Specified arrhythmias | 338240 | 37.4% | 269608 | 37.4% | 228947 | 37.7% | 189864 | 34.1% | 1026659 | 36.8% |
| Diabetes mellitus or diabetes complications | 252095 | 27.9% | 201733 | 28.0% | 163671 | 27.0% | 151199 | 27.1% | 768698 | 27.6% |
| Chronic obstructive pulmonary disease | 174064 | 19.2% | 148773 | 20.6% | 128604 | 21.2% | 91244 | 16.4% | 542685 | 19.5% |
| Valvular or rheumatic heart disease | 142124 | 15.7% | 121183 | 16.8% | 110143 | 18.2% | 64873 | 11.6% | 438323 | 15.7% |
| Iron deficiency or other anemias and blood disease | 141814 | 15.7% | 117097 | 16.2% | 96225 | 15.9% | 92967 | 16.7% | 448103 | 16.1% |
| Vascular or circulatory disease | 130627 | 14.4% | 109338 | 15.2% | 93629 | 15.4% | 87157 | 15.6% | 420751 | 15.1% |
| Disorders of fluid, electrolyte, acid-base | 98879 | 10.9% | 89468 | 12.4% | 105083 | 17.3% | 105459 | 18.9% | 398889 | 14.3% |
| Pneumonia | 76623 | 8.5% | 73940 | 10.3% | 66324 | 10.9% | 65370 | 11.7% | 282257 | 10.1% |
| Angina pectoris, old myocardial infarction | 77656 | 8.6% | 56924 | 7.9% | 44835 | 7.4% | 37978 | 6.8% | 217393 | 7.8% |
| Renal failure | 72228 | 8.0% | 85940 | 11.9% | 134582 | 22.2% | 155353 | 27.9% | 448103 | 16.1% |
| Other urinary tract disorders | 69486 | 7.7% | 71355 | 9.9% | 43033 | 7.1% | 21731 | 3.9% | 205605 | 7.4% |
| Dementia or other specified brain disorders | 58345 | 6.4% | 53769 | 7.5% | 47066 | 7.8% | 46669 | 8.4% | 205849 | 7.4% |
| History of infection | 38398 | 4.2% | 26317 | 3.7% | 20580 | 3.4% | 20799 | 3.7% | 106094 | 3.8% |
| Acute coronary syndrome | 37310 | 4.1% | 17290 | 2.4% | 10620 | 1.8% | 8097 | 1.5% | 73317 | 2.6% |
| Cerebrovascular disease | 36377 | 4.0% | 25774 | 3.6% | 19270 | 3.2% | 17950 | 3.2% | 99371 | 3.6% |
| Cancer | 29259 | 3.2% | 25229 | 3.5% | 22720 | 3.7% | 22131 | 4.0% | 99339 | 3.6% |
| Hemiplegia, paraplegia, paralysis, functional disability | 25710 | 2.8% | 18444 | 2.6% | 13525 | 2.2% | 17036 | 3.1% | 74715 | 2.7% |
| Stroke | 19160 | 2.1% | 14687 | 2.0% | 12624 | 2.1% | 10888 | 2.0% | 57359 | 2.1% |
| Protein-calorie malnutrition | 11475 | 1.3% | 10832 | 1.5% | 11500 | 1.9% | 16002 | 2.9% | 49809 | 1.8% |
| Asthma | 11375 | 1.3% | 10215 | 1.4% | 9062 | 1.5% | 8519 | 1.5% | 39171 | 1.4% |
| Metastatic cancer or acute leukemia | 7141 | 0.8% | 6557 | 0.9% | 6356 | 1.0% | 6112 | 1.1% | 26166 | 0.9% |
| End stage renal disease or dialysis | 3983 | 0.4% | 5222 | 0.7% | 6850 | 1.1% | 3525 | 0.6% | 19580 | 0.7% |
| Decubitus ulcer or chronic skin ulcer | 2457 | 0.3% | 7094 | 1.0% | 13454 | 2.2% | 11903 | 2.1% | 34908 | 1.3% |
Abbreviations: AMI, acute myocardial infarction
P<0.001 across time for all characteristics, except hemiplegia, paraplegia, paralysis, functional disability (p=.45)
HF hospitalization following AMI
A total of 366,841 patients were hospitalized for HF within a year of discharge from an AMI hospitalization over 2,373,651 patient-years of follow-up. The number of HF hospitalizations following AMI declined from 16.1 per 100 patient-years in 1998 to 14.2 per 100 patient-years by 2010 (p<0.001), with a transient increase in the unadjusted rate of HF hospitalization after AMI for the years 2002 and 2003 (Table 2 and Figure 1). Overall declines in HF hospitalization following AMI from 1998 to 2010 were observed across all age and race-sex groups. After adjusting for demographic factors using a Poisson model, the overall risk of HF hospitalization within 1 year after AMI declined by a relative 14.6% over the study period (IRR=0.854, 95% CI 0.809 to 0.901). (Table 3).
Table 2.
HF hospitalization after AMI
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of AMI hospitalizations | 216107 | 221405 | 230825 | 236831 | 244819 | 243503 | 232528 | 216260 | 199676 | 190843 | 191900 | 183023 | 182223 | |
| Patient-years of follow-up after AMI | 186605 | 189899 | 197444 | 201729 | 208658 | 206685 | 197474 | 182940 | 169470 | 161125 | 161468 | 155145 | 155009 | |
| Number of patients hospitalized for HF after AMI | 29987 | 30437 | 31745 | 31889 | 33101 | 33345 | 31428 | 28094 | 25124 | 23453 | 23594 | 22557 | 22087 | |
| Incidence of HF hospitalization (per 100 person-years) | ||||||||||||||
| Overall | 16.1 | 16.0 | 16.1 | 15.8 | 15.9 | 16.1 | 15.9 | 15.4 | 14.8 | 14.6 | 14.6 | 14.5 | 14.2 | <0.0001 |
| 66-74 | 11.8 | 11.8 | 11.8 | 11.6 | 11.8 | 11.7 | 11.4 | 11.1 | 10.5 | 10.2 | 10.5 | 10.2 | 10.0 | <0.0001 |
| 75-84 | 17.5 | 17.2 | 17.2 | 16.9 | 16.8 | 17.4 | 17.0 | 16.2 | 15.6 | 15.3 | 15.2 | 15.2 | 14.9 | 0.0003 |
| 85+ | 23.8 | 23.3 | 23.1 | 22.4 | 22.6 | 22.6 | 22.7 | 22.0 | 21.3 | 20.9 | 20.6 | 21.1 | 20.9 | <0.0001 |
| White male | 13.3 | 13.3 | 13.5 | 13.3 | 13.5 | 13.8 | 13.8 | 13.4 | 12.8 | 12.6 | 12.9 | 12.8 | 12.5 | 0.0032 |
| White female | 18.0 | 17.8 | 17.7 | 17.2 | 17.1 | 17.5 | 17.1 | 16.4 | 15.8 | 15.6 | 15.3 | 15.4 | 14.9 | <0.0001 |
| Black male | 19.7 | 19.9 | 19.0 | 20.1 | 20.6 | 19.5 | 19.3 | 18.8 | 20.0 | 19.0 | 18.4 | 18.7 | 17.8 | 0.002 |
| Black female | 23.8 | 23.6 | 24.1 | 23.0 | 23.7 | 23.8 | 23.2 | 22.6 | 22.3 | 21.6 | 21.6 | 20.4 | 21.9 | <0.0001 |
| Other male | 16.4 | 15.2 | 15.2 | 16.5 | 16.2 | 15.9 | 15.1 | 15.3 | 13.8 | 13.8 | 15.0 | 14.6 | 14.0 | 0.0006 |
| Other female | 20.7 | 21.8 | 21.9 | 21.9 | 20.1 | 20.1 | 20.1 | 19.3 | 19.1 | 17.1 | 18.2 | 17.5 | 18.2 | <0.0001 |
Abbreviations: AMI, acute myocardial infarction; HF, heart failure
Figure 1.
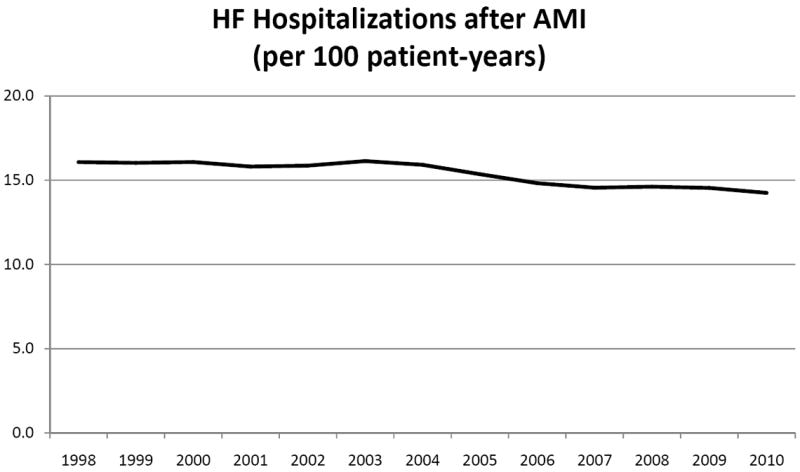
HF Hospitalizations after AMI, per 100-patient years.
Table 3.
Change in incidence rate ratio for HF after AMI
| 1 Year | |||
|---|---|---|---|
| IRR | 95% CI | ||
| 1998 | 1.000 | baseline | |
| 1999 | 0.986 | 0.939 | 1.035 |
| 2000 | 0.982 | 0.935 | 1.031 |
| 2001 | 0.961 | 0.916 | 1.009 |
| 2002 | 0.964 | 0.918 | 1.011 |
| 2003 | 0.975 | 0.929 | 1.023 |
| 2004 | 0.961 | 0.915 | 1.009 |
| 2005 | 0.924 | 0.879 | 0.972 |
| 2006 | 0.890 | 0.845 | 0.937 |
| 2007 | 0.870 | 0.826 | 0.917 |
| 2008 | 0.871 | 0.826 | 0.917 |
| 2009 | 0.869 | 0.824 | 0.917 |
| 2010 | 0.854 | 0.809 | 0.901 |
Abbreviations: AMI, acute myocardial infarction; CI, confidence interval; HF, heart failure
Mortality after HF hospitalization following AMI
The proportion of patients hospitalized for HF after AMI who died within 1 year of HF hospitalization was 44.4% in 1998 which remained stable up to 2001 (44.5%), and then declined to a nadir of 43.2% in 2004-2005; the 1-year mortality rate after HF hospitalization then increased to 45.5% by 2010. (Table 4 and Figure 2) Similar patterns were observed for 30-, 90- and 180-day mortality. Using a Cox proportion hazards model to adjust for patient demographic characteristics and comorbidities, we found that the hazard ratio for death after HF hospitalization following AMI declined by a relative 10.8% over the overall study period from 1998 to 2010 (HR=0.892, 95% CI 0.869 to 0.916). (Table 5) In the adjusted analyses, the relative annual decline in the hazard for death was 2.4% from 1998 to 2007 (HR=0.976, 95%CI 0.974 to 0.978), followed by a relative annual increase of 5.1% from 2007 to 2010 (HR=1.051, 95%CI 1.039 to 1.064).
Table 4.
1-year mortality among patients hospitalized for HF after AMI
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 29987 | 30437 | 31745 | 31889 | 33101 | 33345 | 31428 | 28094 | 25124 | 23453 | 23594 | 22557 | 22087 | |
| 30-days | 13.4% | 13.5% | 13.4% | 13.3% | 12.6% | 12.8% | 12.5% | 12.5% | 12.4% | 12.8% | 12.8% | 13.0% | 13.1% | <0.0001 |
| 90-days | 24.2% | 24.1% | 24.5% | 24.2% | 23.4% | 23.6% | 23.3% | 23.4% | 23.5% | 23.9% | 23.8% | 24.8% | 24.8% | <0.0001 |
| 180-days | 33.3% | 33.3% | 33.6% | 33.4% | 32.5% | 32.6% | 32.3% | 32.3% | 32.8% | 33.0% | 32.9% | 34.3% | 34.5% | <0.0001 |
| 1-year | 44.4% | 44.3% | 44.6% | 44.5% | 43.5% | 43.4% | 43.2% | 43.2% | 43.8% | 44.0% | 44.3% | 45.7% | 45.5% | <0.0001 |
Abbreviations: AMI, acute myocardial infarction; HF, heart failure
Figure 2.
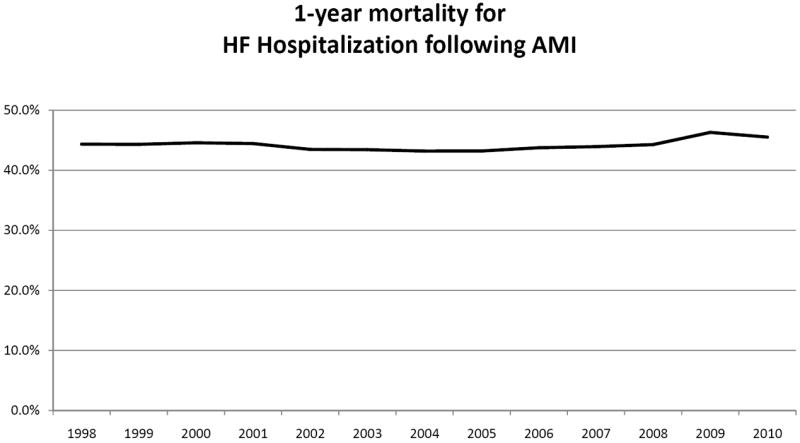
1-year mortality for HF Hospitalization following AMI.
Table 5.
Hazard Ratio for risk-adjusted mortality within 1 year of HF hospitalization after AMI
| HR | 95% CI | ||
|---|---|---|---|
| 1998 | 1.000 | baseline | |
| 1999 | 0.987 | 0.964 | 1.011 |
| 2000 | 0.977 | 0.954 | 1.000 |
| 2001 | 0.956 | 0.934 | 0.979 |
| 2002 | 0.914 | 0.893 | 0.936 |
| 2003 | 0.892 | 0.871 | 0.913 |
| 2004 | 0.862 | 0.841 | 0.883 |
| 2005 | 0.841 | 0.820 | 0.862 |
| 2006 | 0.828 | 0.807 | 0.849 |
| 2007 | 0.825 | 0.804 | 0.847 |
| 2008 | 0.862 | 0.840 | 0.885 |
| 2009 | 0.878 | 0.856 | 0.902 |
| 2010 | 0.892 | 0.869 | 0.916 |
Abbreviations: AMI, acute myocardial infarction; CI, confidence interval; HF, heart failure; HR, hazard ratio Analyses adjusted for patient demographics and comorbidities
Discussion
Using a complete sample of fee-for-service Medicare beneficiaries, our study found that the incidence of HF hospitalization following AMI decreased from 1998 to 2010. The observed 1-year mortality for patients hospitalized for HF after AMI remains high at 45.5% in 2010, and has increased since 2007.
Our analysis extends prior work examining trends in HF hospitalizations after AMI. While previous studies had the benefit of clinical confirmation of AMI and HF, they were limited to small geographic settings, consisted of homogenous demographic populations, and evaluated subjects prior to the introduction of modern AMI strategies. As such it is not surprising that long-term secular trends in HF incidence after AMI were conflicting. Researchers examining the Olmsted County cohort reported that the 5-year incidence of HF after AMI decreased from 40% from 1979-84 to 33% from 1990-94, which the authors attributed to increased use of reperfusion therapy. 5 In contrast, researchers in the Framingham Heart Study found that 5-year rates of HF after Q-wave AMI increased from 27.6 to 31.9 per 100 patients between 1970-79 and 1990-99. 6 While only reporting rates of HF that occurred during the AMI hospitalization, the Worcester Heart Attack Study tracked 25-year trends (1975 to 2001), and found that the HF rate increased by a relative 37% after adjusting for patient demographics and AMI characteristics. 4 These somewhat conflicting results from these separate studies are likely due to a combination of factors: 14 1) differences in type of AMI (Q-wave only versus any type of AMI, 2) first incident AMI only versus any AMI, 3) differences in timing of HF ascertainment (in-hospital only versus inclusion of post-discharge HF events, and method of HF ascertainment (Framingham clinical criteria versus administrative codes), 4) differences in follow-up period for determining HF endpoints, 5) inclusion of outpatients with HF versus inpatients only), and 6) regional differences (Massachusetts versus Minnesota). Ultimately, it may be difficult to draw useful inferences between our study examining the recent past (1998-2010) with those from Framingham (1970-1999) and Olmsted County (1979-1994) given the advances in clinical management of AMI and HF. The age difference between our study cohort (Medicare patients with mean age 78 years) compared with Framingham and Olmsted County cohorts (mean age 66-67 years) also limit the ability to compare outcomes meaningfully.
Our study found that on the national level, the adjusted risk for HF hospitalization within 1 year after AMI declined modestly over the 1998 to 2010 period. One potential explanation for this finding is that improvements in myocardial salvage and more complete revascularization after AMI occurred during this time, which resulted in fewer subsequent HF events. The National Cardiovascular Data Registry has reported higher use of reperfusion therapy and cardiac catheterization after AMI, which is consistent with this hypothesis. 8 Another possible reason is increased use of AMI pharmacotherapies that reduce adverse ventricular remodeling (e.g. inhibitors of the renin-angiotensin-aldosterone system) and neuro-horomonal activation (e.g. beta adrenergic antagonists) thus reducing subsequent HF events. Studies have documented that use of such medications after AMI have also increased significantly over the past decade. 9, 15-17
The decrease in HF hospitalizations after AMI may also reflect a shift towards increased surveillance of HF in the outpatient setting, resulting in greater HF diagnosis and treatment that reduces the need for hospitalization. A Canadian study found that the HF hospitalization rate has declined faster than outpatient and emergency department encounters, suggesting that some of the decline in HF admissions may be attributed towards outpatient care settings.18 Whether this phenomenon exists for HF patients in the U.S. remains to be investigated.
Several studies have examined how HF incidence differs across race and sex,19-21 but few have examined differences specifically in post-infarction cohorts. Our study found that HF hospitalization after AMI decreased for all race-sex groups, but black patients and women continue to suffer an excess absolute burden from HF. The explanation for why black and female subject have higher risk of HF after AMI is likely multi-factorial— differences in AMI treatments, secondary prevention of cardiovascular risk factors, and care settings all may play a role. For example, one study reported that after AMI black patients had higher rates of death, re-hospitalization, angina, and lower quality of life compared with white patients, but these differences did not persist after adjusting for patient factors and site of care. 22 Many studies have reported lower rates of coronary interventions after AMI for black and female patients, 23, 24,25, 26 which may alter the completeness of revascularization and subsequent risk for HF. Differences in rates of HF after AMI may also be due to differences in competing risks due to non-cardiovascular deaths, which appears particularly influential for black men. 21 Our study illustrates that black and female patients continue have higher incidence of HF after AMI, similar to the pre-infarction setting; additional efforts towards improving the care and outcomes of these high risk groups are needed. The HF hospitalization rate after AMI declined somewhat more slowly than the overall HF hospitalization rate in general Medicare population. HF hospitalizations declined by 29.5% in the Medicare population overall from 1998 to 2008 27 compared with a 11.3% decline after AMI in the current study from 1998 to 2010. This may reflect concern by clinicians that patients with recent AMI who develop HF would be at high risk for worsening or recurrent ischemia; as a result such patients would more likely to be hospitalized compared with a general cohort of HF patients. Alternatively, the slower decline in HF hospitalizations after AMI may represent differential thresholds for admission if clinicians were less likely to treat HF patients with a recent AMI in outpatient settings compared with patients with non-ischemic HF. Finally, our findings may also reflect differences in how risk factors for ischemic versus non-ischemic HF etiologies have changed over the study period with corresponding differentials in HF hospitalization rates over time.
A shift in the location of HF treatment over time also may explain the increase in risk-adjusted mortality for HF hospitalization following AMI from 2007 to 2010. Improvements in AMI care that decreased development of HF may have translated into decreased mortality in the beginning of the study period, followed by increasing mortality if only the most severely ill HF patients were admitted in the latter half of the decade. It is possible that mortality from HF after AMI has worsened in recent years, but this is not consistent with the improvements in AMI care noted above that have likely reduced the incidence of HF after AMI, as well as not consistent with studies demonstrating that quality of care for HF patients has improved in terms of increased use of HF pharmacotherapies. 28, 29 Alternatively, mortality may have increased due to higher atherosclerotic burden or increased severity of comorbidities over time. For example, the prevalence of renal failure increased more than three-fold over the study period, which may indicate a greater extent of cardiovascular disease for AMI patients who subsequently develop HF in recent years. While mortality continued to increase after 2007 even after adjusting for renal failure and other comorbidities, this does not exclude the possibility that these HF patients had higher atherosclerotic burden over time as administrative codes control for presence of disease and not its severity. The hypothesis that recent increases in mortality for HF following AMI is due to selection of sicker patients who were hospitalized will need to be clinically confirmed in future studies.
Only 54.3% of patients hospitalized with HF hospitalization after AMI survived to one year in the final year of this contemporary cohort of older subjects. In comparison, 1-year survival after HF following AMI was modestly higher in other studies: 1-year survival was 72% in the Olmsted County 30, and 1-year survival for HF in general in the Framingham Heart Study was 57% for men and 64% for women.31 Clearly, older patients hospitalized for HF following AMI appear to be at higher risk for death, and as such this population may benefit from more frequent surveillance and in some cases more intense treatments. For example is has been well-established that older HF patients are less likely to be prescribed beta-blockers and inhibitors of the angiotensin-renin-aldosterone system, 32-38 Similarly, cardiac resynchronization therapy is effective in older patients 39, 40 but also underused. 36, 41 Compared with younger populations, older patients typically have the highest absolute risks for death after AMI and HF, and as result would receive the greatest absolute benefit from such therapies. Future studies should be conducted to identify clinical needs and opportunities for improving HF outcomes in this population.
Limitations
Our study has several potential limitations. We were not able to distinguish incident from prevalent cases of HF, and not able to separate patients with AMI complicated by HF from patients with prior HF who were admitted for AMI. We examined the Medicare fee-for service population, and trends in HF hospitalization rates following AMI may differ in younger patients or those with different health insurance. Third, HF ascertainment was not based on clinical criteria, and hospitals may have changed patterns of medical coding of HF over time; comorbidities were ascertained from administrative codes and not clinically confirmed. Our study focused on HF hospitalizations and was not able to assess changes in HF care in outpatient clinics or emergency departments, and as such may have underestimated overall HF incidence rates. Although we were unable to differentiate systolic versus diastolic HF using administrative data, it is likely that most AMI patients who develop HF would have systolic dysfunction.
Conclusion
Using a complete sample of Medicare patients, our study found that the proportion of patients who developed HF following hospitalization for AMI decreased by 14.4% from 1998 to 2010. In contrast, the risk for death within 1 year after HF hospitalization following AMI decreased by a relative 3.4% annually from 1998 to 2007, but was followed by an annual relative increase of 5.1% from 2007 to 2010. HF hospitalization within 1 year after AMI remains a marker of high-risk, with nearly half of patients dying within a year following the development of HF.
Supplementary Material
Acknowledgments
Funding Sources: Dr. Chen was affiliated with the Section of Cardiovascular Medicine, Department of Medicine, Yale University School of Medicine, during the time this research was conducted. This work was supported by an Agency for Healthcare Research and Quality Career Development Award (1K08HS018781-01) for Dr. Chen. Dr. Krumholz is supported by Grant U01 HL105270-02 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. Dr. Dharmarajan is supported by a National Institutes of Health T32 training grant in cardiovascular disease (2T32HL007854-16A1) from Columbia University.
Footnotes
Conflict of Interest Disclosures: Dr. Krumholz reports that he chairs a cardiac scientific advisory board for UnitedHealth and is the recipient of a research grant from Medtronic, Inc., through Yale University. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References
- 1.Weir RA, McMurray JJ, Velazquez EJ. Epidemiology of heart failure and left ventricular systolic dysfunction after acute myocardial infarction: Prevalence, clinical characteristics, and prognostic importance. Am J Cardiol. 2006;97:13F–25F. doi: 10.1016/j.amjcard.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Steg PG, Dabbous OH, Feldman LJ, Cohen-Solal A, Aumont M-C, López-Sendón J, Budaj A, Goldberg RJ, Klein W, Anderson FA. Investigators for the Global Registry of Acute Coronary Events. Determinants and prognostic impact of heart failure complicating acute coronary syndromes: Observations from the Global Registry of Acute Coronary Events (GRACE) Circulation. 2004;109:494–499. doi: 10.1161/01.CIR.0000109691.16944.DA. [DOI] [PubMed] [Google Scholar]
- 3.Velazquez EJ, Pfeffer MA. Acute heart failure complicating acute coronary syndromes: A deadly intersection. Circulation. 2004;109:440–442. doi: 10.1161/01.CIR.0000113460.23813.50. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg RJ, Spencer FA, Yarzebski J, Lessard D, Gore JM, Alpert JS, Dalen JE. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–1378. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 5.Hellermann JP, Goraya TY, Jacobsen SJ, Weston SA, Reeder GS, Gersh BJ, Redfield MM, Rodeheffer RJ, Yawn BP, Roger VL. Incidence of heart failure after myocardial infarction: Is it changing over time? Am J Epidemiol. 2003;157:1101–1107. doi: 10.1093/aje/kwg078. [DOI] [PubMed] [Google Scholar]
- 6.Velagaleti RS, Pencina MJ, Murabito JM, Wang TJ, Parikh NI, D’Agostino RB, Levy D, Kannel WB, Vasan RS. Long-term trends in the incidence of heart failure after myocardial infarction. Circulation. 2008;118:2057–2062. doi: 10.1161/CIRCULATIONAHA.108.784215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehta SR, Cannon CP, Fox KA, Wallentin L, Boden WE, Spacek R, Widimsky P, McCullough PA, Hunt D, Braunwald E, Yusuf S. Routine vs selective invasive strategies in patients with acute coronary syndromes: A collaborative meta-analysis of randomized trials. JAMA. 2005;293:2908–2917. doi: 10.1001/jama.293.23.2908. [DOI] [PubMed] [Google Scholar]
- 8.Roe MT, Messenger JC, Weintraub WS, Cannon CP, Fonarow GC, Dai D, Chen AY, Klein LW, Masoudi FA, McKay C, Hewitt K, Brindis RG, Peterson ED, Rumsfeld JS. Treatments, trends, and outcomes of acute myocardial infarction and percutaneous coronary intervention. J Am Coll Cardiol. 2010;56:254–263. doi: 10.1016/j.jacc.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. New Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 10.Masoudi FA, Foody JM, Havranek EP, Wang Y, Radford MJ, Allman RM, Gold J, Wiblin RT, Krumholz HM. Trends in acute myocardial infarction in 4 US states between 1992 and 2001: Clinical characteristics, quality of care, and outcomes. Circulation. 2006;114:2806–2814. doi: 10.1161/CIRCULATIONAHA.106.611707. [DOI] [PubMed] [Google Scholar]
- 11.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: Progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 12.Eicheldinger C, Bonito A. More accurate racial and ethnic codes for Medicare administrative data. Health Care Financ Rev. 2008;29:27–42. [PMC free article] [PubMed] [Google Scholar]
- 13.Krumholz HM, Wang Y, Mattera JA, Wang Y, Han LF, Ingber MJ, Roman S, Normand S-LT. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113:1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 14.Jhund PS, McMurray JJ. Heart failure after acute myocardial infarction: A lost battle in the war on heart failure? Circulation. 2008;118:2019–2021. doi: 10.1161/CIRCULATIONAHA.108.813493. [DOI] [PubMed] [Google Scholar]
- 15.Lewis WR, Ellrodt AG, Peterson E, Hernandez AF, LaBresh KA, Cannon CP, Pan W, Fonarow GC. Trends in the use of evidence-based treatments for coronary artery disease among women and the elderly: Findings from the Get With The Guidelines quality-improvement program. Circ Cardiovasc Qual Outcomes. 2009;2:633–641. doi: 10.1161/CIRCOUTCOMES.108.824763. [DOI] [PubMed] [Google Scholar]
- 16.Michaels AD, Maynard C, Every NR, Barron HV. Early use of ACE inhibitors in the treatment of acute myocardial infarction in the United States: Experience from the National Registry of Myocardial Infarction 2. Am J Cardiol. 1999;84:1176–1181. doi: 10.1016/s0002-9149(99)00530-5. [DOI] [PubMed] [Google Scholar]
- 17.Setoguchi S, Glynn RJ, Avorn J, Levin R, Winkelmayer WC. Ten-year trends of cardiovascular drug use after myocardial infarction among community-dwelling persons > or =65 years of age. Am J Cardiol. 2007;100:1061–1067. doi: 10.1016/j.amjcard.2007.04.052. [DOI] [PubMed] [Google Scholar]
- 18.Ezekowitz JA, Kaul P, Bakal JA, Quan H, McAlister FA. Trends in heart failure care: Has the incident diagnosis of heart failure shifted from the hospital to the emergency department and outpatient clinics? Eur J Heart Fail. 2010;13:142–147. doi: 10.1093/eurjhf/hfq185. [DOI] [PubMed] [Google Scholar]
- 19.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. New Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in us men and women: Nhanes i epidemiologic follow-up study. Arch Intern Med. 2001;161:996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 21.Huffman MD, Berry JD, Ning H, Dyer AR, Garside DB, Cai X, Daviglus ML, Lloyd-Jones DM. Lifetime risk for heart failure among white and black americans: Cardiovascular lifetime risk pooling project. J Am Coll Cardiol. 2013;61:1510–1517. doi: 10.1016/j.jacc.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spertus JA, Jones PG, Masoudi FA, Rumsfeld JS, Krumholz HM. Factors associated with racial differences in myocardial infarction outcomes. Ann Intern Med. 2009;150:314–324. doi: 10.7326/0003-4819-150-5-200903030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gillum RF. Coronary artery bypass surgery and coronary angiography in the United States, 1979-1983. Am Heart J. 1987;113:1255–1260. doi: 10.1016/0002-8703(87)90952-5. [DOI] [PubMed] [Google Scholar]
- 24.Peterson ED, Shaw LK, DeLong ER, Pryor DB, Califf RM, Mark DB. Racial variation in the use of coronary-revascularization procedures. Are the differences real? Do they matter? New Engl J Med. 1997;336:480–486. doi: 10.1056/NEJM199702133360706. [DOI] [PubMed] [Google Scholar]
- 25.Chen J, Rathore SS, Radford MJ, Wang Y, Krumholz HM. Racial differences in the use of cardiac catheterization after acute myocardial infarction. New Engl J Med. 2001;344:1443–1449. doi: 10.1056/NEJM200105103441906. [DOI] [PubMed] [Google Scholar]
- 26.Rathore SS, Chen J, Wang Y, Radford MJ, Vaccarino V, Krumholz HM. Sex differences in cardiac catheterization: The role of physician gender. JAMA. 2001;286:2849–2856. doi: 10.1001/jama.286.22.2849. [DOI] [PubMed] [Google Scholar]
- 27.Chen J, Normand S-LT, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998-2008. JAMA. 2011;306:1669–1678. doi: 10.1001/jama.2011.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fonarow GC, Heywood JT, Heidenreich PA, Lopatin M, Yancy CW. Temporal trends in clinical characteristics, treatments, and outcomes for heart failure hospitalizations, 2002 to 2004: Findings from Acute Decompensated Heart Failure National Registry (ADHERE) Am Heart J. 2007;153:1021–1028. doi: 10.1016/j.ahj.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 29.Masoudi FA, Gross CP, Wang Y, Rathore SS, Havranek EP, Foody JM, Krumholz HM. Adoption of spironolactone therapy for older patients with heart failure and left ventricular systolic dysfunction in the United States, 1998-2001. Circulation. 2005;112:39–47. doi: 10.1161/CIRCULATIONAHA.104.527549. [DOI] [PubMed] [Google Scholar]
- 30.Hellermann JP, Jacobsen SJ, Redfield MM, Reeder GS, Weston SA, Roger VL. Heart failure after myocardial infarction: Clinical presentation and survival. Eur J Heart Fail. 2005;7:119–125. doi: 10.1016/j.ejheart.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 31.Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham heart study subjects. Circulation. 1993;88:107–115. doi: 10.1161/01.cir.88.1.107. [DOI] [PubMed] [Google Scholar]
- 32.Komajda M, Follath F, Swedberg K, Cleland J, Aguilar JC, Cohen-Solal A, Dietz R, Gavazzi A, Van Gilst WH, Hobbs R, Korewicki J, Madeira HC, Moiseyev VS, Preda I, Widimsky J, Freemantle N, Eastaugh J, Mason J Study Group on Diagnosis of the Working Group on Heart Failure of the European Society of C. The EuroHeart Failure Survey programme--a survey on the quality of care among patients with heart failure in Europe. Part 2: Treatment. Eur Heart J. 2003;24:464–474. doi: 10.1016/s0195-668x(02)00700-5. [DOI] [PubMed] [Google Scholar]
- 33.Maggioni AP, Sinagra G, Opasich C, Geraci E, Gorini M, Gronda E, Lucci D, Tognoni G, Balli E, Tavazzi L. Beta blockers in patients with congestive heart failure: guided use in clinical practice I. Treatment of chronic heart failure with beta adrenergic blockade beyond controlled clinical trials: The BRING-UP experience. Heart. 2003;89:299–305. doi: 10.1136/heart.89.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Masoudi FA, Rathore SS, Wang Y, Havranek EP, Curtis JP, Foody JM, Krumholz HM. National patterns of use and effectiveness of angiotensin-converting enzyme inhibitors in older patients with heart failure and left ventricular systolic dysfunction. Circulation. 2004;110:724–731. doi: 10.1161/01.CIR.0000138934.28340.ED. [DOI] [PubMed] [Google Scholar]
- 35.Sin DD, McAlister FA. The effects of beta-blockers on morbidity and mortality in a population-based cohort of 11,942 elderly patients with heart failure. Am J Med. 2002;113:650–656. doi: 10.1016/s0002-9343(02)01346-3. [DOI] [PubMed] [Google Scholar]
- 36.Yancy CW, Fonarow GC, Albert NM, Curtis AB, Stough WG, Gheorghiade M, Heywood JT, McBride ML, Mehra MR, O’Connor CM, Reynolds D, Walsh MN. Influence of patient age and sex on delivery of guideline-recommended heart failure care in the outpatient cardiology practice setting: Findings from IMPROVE HF. Am Heart J. 2009;157:754–762 e752. doi: 10.1016/j.ahj.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 37.Forman DE, Cannon CP, Hernandez AF, Liang L, Yancy C, Fonarow GC. Get With the Guidelines Steering C, Hospitals. Influence of age on the management of heart failure: Findings from Get With The Guidelines-Heart Failure (GWTG-HF) Am Heart J. 2009;157:1010–1017. doi: 10.1016/j.ahj.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 38.Albert NM, Yancy CW, Liang L, Zhao X, Hernandez AF, Peterson ED, Cannon CP, Fonarow GC. Use of aldosterone antagonists in heart failure. JAMA. 2009;302:1658–1665. doi: 10.1001/jama.2009.1493. [DOI] [PubMed] [Google Scholar]
- 39.Delnoy PP, Ottervanger JP, Luttikhuis HO, Elvan A, Misier AR, Beukema WP, van Hemel NM. Clinical response of cardiac resynchronization therapy in the elderly. Am Heart J. 2008;155:746–751. doi: 10.1016/j.ahj.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 40.Killu AM, Wu JH, Friedman PA, Shen WK, Webster TL, Brooke KL, Hodge DO, Wiste HJ, Cha YM. Outcomes of cardiac resynchronization therapy in the elderly. Pacing Clin Electrophysiol. 2013;36:664–72. doi: 10.1111/pace.12048. Epub 2012 Dec 18. [DOI] [PubMed] [Google Scholar]
- 41.Curtis AB, Yancy CW, Albert NM, Stough WG, Gheorghiade M, Heywood JT, McBride ML, Mehra MR, Oconnor CM, Reynolds D, Walsh MN, Fonarow GC. Cardiac resynchronization therapy utilization for heart failure: Findings from IMPROVE HF. Am Heart J. 2009;158:956–964. doi: 10.1016/j.ahj.2009.10.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


