Abstract
Negative emotionality is a distinguishing feature of borderline personality disorder (BPD). However, this person-level characteristic has not been examined as a marker of vulnerability in the development of this disorder. The current study utilized a multi-method approach to examine the interplay between negative emotional reactivity and cumulative exposure to family adversity on the development of BPD symptoms across three years (ages 16–18) in a diverse, at-risk sample of adolescent girls (N=113). A latent variable of negative emotional reactivity was created from multiple assessments at age 16: (1) self-report, (2) emotion ratings to stressors from ecological assessments across one week, and (3) observer-rated negative affectivity during a mother-daughter conflict discussion task. Exposure to family adversity was measured cumulatively between ages 5 and 16 from annual assessments of family poverty, single parent household, and difficult life circumstances. Results from latent growth curve models demonstrated a significant interaction between negative emotional reactivity and family adversity, such that exposure to adversity strengthened the association between negative emotional reactivity and BPD symptoms. Additionally, family adversity predicted increasing BPD symptoms during late adolescence. These findings highlight negative emotional reactivity as a marker of vulnerability that ultimately increases risk for the development of BPD symptoms.
Keywords: negative emotional reactivity, borderline personality disorder, adolescence
Borderline personality disorder (BPD) emerges by late adolescence or young adulthood and is characterized by multiple debilitating symptoms, including cognitive deficits, tumultuous interpersonal relationships, and impulsive behaviors that interfere with occupational, academic, and social functioning (American Psychiatric Association [APA], 2013; Bagge, Nickell, Stepp, Durrett, Jackson, & Trull, 2004; Skodol et al., 2005; Soloff, Lynch, & Kelly, 2002; Stepp, 2012; Zweig-Frank & Paris, 2002). Moreover, an estimated 8–10% of individuals with BPD will die by suicide (APA, 2013; Holm & Severinsson, 2011). These devastating consequences speak to the urgent need for effective prevention strategies. However, successful prevention is predicated on elucidating markers of vulnerability so that at-risk youth can be reliably assessed and identified early.
Emotional vulnerability to environmental stressors is sine qua non for BPD symptom expression. For instance, the Diagnostic and Statistical Manual-5th edition (APA, 2013) explicitly conceptualizes BPD criteria regarding affective instability, paranoid ideation, and other transient psychotic experiences as reactions to a distressing event. Several prominent etiological theories of BPD development also view susceptibility in terms of child-level emotional vulnerabilities interacting with deleterious environmental circumstances or events (Batemen & Fonagy, 2003; Kernberg, 1984; Linehan, 1993). For example, the biosocial model postulates that BPD develops from transactions between an emotionally sensitive child and family systems ill-equipped to meet the child’s emotion regulation needs, which serve to further promote emotional reactivity and dysregulation in the child (Linehan, 1993; Crowell, Beauchaine, & Linehan, 2009). We previously found support for maintenance of the disorder consistent with biosocial theory by demonstrating the reciprocal, bi-directional nature of BPD symptoms and deleterious parenting practices across adolescence in a large, community sample of adolescent girls (N = 2,451; Stepp et al., 2014). Emotional vulnerability components of the biosocial model, however, have yet to be tested. In general most research has focused on cross-sectional associations between markers of emotion vulnerability and BPD in adult clinical samples.
Additionally, little longitudinal work has examined whether susceptibility to BPD symptoms varies as a function of exposure to adversity. Moreover, the high rates of childhood sexual abuse reported by adult patients with BPD has led most researchers examining environmental risk factors to focus exclusively on exposure to childhood abuse (Bornolova, Huibregtse, Hicks, Iacono, & McGue, 2013; Fossati, Madeddu, & Maffei, 1999). This relatively narrow focus ignores potent environmental risks related to exposure to childhood poverty that have been associated with altered stress responses, severe mental illness, and overall poor health (Evans, 2004; van Os, Kenis, & Rutten, 2010). Thus, we contextualize adversity in terms of the accumulation of multiple adversities impacting the child’s family system (Evans & Cassells, 2013; Evans & Kim, 2007). We limited adversities to difficulties that were not directed at, or solely experienced by, the child but were stressors veritably impacting the larger family system (e.g., poverty, crowded housing, parental incarceration, single parent household). Thus, we examine the impact of childhood sexual abuse separately from family adversity for two reasons. First, while the entire family often experiences trauma when a child is sexually abused, this may not necessarily be the case, especially if a member outside of the family perpetrates the abuse and/or the child does not disclose the event. Furthermore, by considering childhood sexual abuse separately from family adversity we are able to determine whether or not exposure to adversity impacting the broader family system has a specific influence on the development of BPD symptoms net the influence of exposure to childhood sexual abuse. Therefore, we chose not to include childhood sexual abuse in our conceptualization of family adversities. However, given the extensive body of work linking exposure to childhood sexual abuse and BPD, we did examine its’ effects on BPD symptom development separately from family adversity.
Accordingly, the current study focuses on the etiology of BPD by utilizing an intensive multi-method longitudinal study to examine negative emotional reactivity conferring vulnerability to BPD symptom development during late adolescence. Further, we examined the strength of the relationship between negative emotional reactivity and the development of BPD symptoms in the context of exposure to family adversity in a racially and economically diverse sample of adolescent girls oversampled for heightened BPD risk. To determine the unique impact of negative emotional reactivity and exposure to family adversity on BPD symptom development, we examined these relationships relative to temperamental factors and childhood sexual abuse.
Adolescence as a Window of Vulnerability
Despite the fact that adolescence represents an ideal developmental window to identify markers of vulnerability, most research on BPD has been conducted with adults. As adolescents are expected to engage in more independent emotion regulation and behavioral control strategies with age, deficits in self-regulatory skills become more apparent during this developmental period. Thus, for predisposed youth, it is not surprising that recognizable symptoms and features of BPD are likely to first manifest during adolescence (Bradley, Conklin, & Westen, 2005; Westen & Chang, 2000). Additionally, findings from community samples demonstrate that BPD symptoms and features peak during mid-adolescence and decline during late adolescence and young adulthood (Beauchaine et al., 2009; Bornovalova, Hicks, Iacono, & McGue, 2009; de Clercq, van Leeuwen, van den Noortgate, de Bolle, & de Fruyt, 2009; Goodman et al., 2010; Stepp et al., 2014). For example, Bornalova and colleagues (2009) examined the developmental trajectory of BPD symptoms across ages 14 to 24 years and reported the highest mean-level stability during the period from 14 to 17 years old, with a significant decline in mean-level symptoms from ages 17 to 24. Thus, aberrant patterns of consistently high and/or increasing levels of BPD symptoms are evident by late adolescence, which provides an opportunity to identify markers of vulnerability for the development of BPD symptoms.
The optimal acquisition of self-regulatory skills requires reliability and predictability in the child’s environment. Such environmental conditions afford caregivers greater opportunities to respond with sensitivity to the child’s emotional needs. In contrast, children embedded within families facing poverty and high levels of chronic stress are likely to encounter unstable housing conditions, changes in family structure, caregiver unemployment, family conflict and violence (Conger et al., 2002; Conger, Ge, Elder, Lorenz, & Simons, 1994; Evans, 2004). Exposure to these disruptions and adversities likely impedes the acquisition of interpersonal skills, decision-making abilities, emotion regulation skills, and identity development (Conger, Conger, & Martin, 2010). Moreover, children with high levels of emotional sensitivity and reactivity may be especially vulnerable to the detrimental effects of exposure resulting from such adversities (van Os et al., 2010).
Adolescent girls appear to be at particularly high risk for BPD features and their detrimental consequences. Although BPD is equally prevalent among males and females in most community samples (Coid, Yang, Tyrer, Roberts, & Ullrich, 2006; Grant et al., 2008; Lenzenweger, Lane, Loranger, & Kessler, 2007), significantly higher rates of BPD are consistently observed among females as compared to males in both clinical and forensic populations of adolescents and adults (Sansone & Sansone, 2009; Skodol & Bender, 2003; Eppright, Kashani, Robinson, & Reid, 1993; Grilo et al., 1995; Myers, Burkett, & Otto, 1993; for a review, see Miller et al., 2008). Evidence also shows that BPD is associated with greater distress and disability among women than men (Grant et al., 2008; Trull, Jahng, Tomko, Wood, & Sher, 2010), suggesting that girls may be in particular need of prevention and treatment efforts. As a result, the current study focuses on female-specific vulnerabilities identified in childhood and adolescence.
Negative Emotional Reactivity as a Marker of Vulnerability for Borderline Personality Disorder
Individuals with BPD report increased emotional reactivity to negative events compared to healthy and psychiatric control groups (Jovev & Jackson, 2006; Pagano et al., 2004; Sinha & Watson, 1997; Stiglmayr et al., 2005; Trull, 1995). Negative emotional reactivity in response to daily stressors is associated with many forms of psychopathology and has been linked to genetic risk for depression and psychosis (Gottesman & Gould, 2003; Myin-Germeys & van Os, 2007; Wichers et al., 2007; Lataster et al., 2009). Extending this previous work, adults with BPD reported heightened negative emotional reactivity to daily stressors compared to healthy controls and patients with a psychotic disorder even when controlling for depression (Glaser, Os, Mengelers, & Myin-Germeys, 2008). Taken together these finding suggest that negative emotional reactivity is distinct from the stable and negative mood states characterizing depression. However, whether negative emotional reactivity is distinguishable from the temperament trait of emotionality is unknown.
Temperament emotionality reflects individual differences in the experience and expression of negative emotions (Buss & Plomin, 1984; Rothbart, 2007; Shiner, Buss, McClowry, Putnam, Saudino, & Zentner, 2012) and has been found to predict BPD symptoms in adolescence (Stepp, Keenan, Hipwell, & Krueger, 2014) and adulthood (Carlson, Egeland, & Sroufe, 2009). In the current study, we view negative emotional reactivity as a rapid and intense emotional response that occurs in the presence of a stressor; thus, while this construct is a near neighbor of temperament emotionality, it is nonetheless a more circumscribed aspect of emotional vulnerability relative to the broader temperament dimension. Therefore, we consider negative emotional reactivity as conceptually distinguishable from temperament emotionality. Furthermore, since previous work has identified temperament emotionality as a risk factor for BPD, in the current study we examine the incremental utility of negative emotional reactivity in the prediction of BPD symptoms net the influence of temperament emotionality.1
Much of the prior work examining negative emotionality as a vulnerability factor for BPD has relied on self-report measures, which may be biased in a number of ways. We extend this body of work by integrating information across multiple methods that vary by informant (self- versus observer-ratings), time-frame (from minutes to hours to several years), and context (laboratory versus home environments) to derive a latent factor of negative emotional reactivity. This novel methodological approach reduces measurement error thereby reducing shared method effects among negative emotional reactivity and BPD symptoms.
Childhood Adversity and Borderline Personality Disorder Risk
Stressful life events and childhood adversity are more commonly reported in patients with BPD compared to patients with other personality disorders and healthy controls. Patients with BPD often retrospectively report experiencing trauma and neglect during childhood and adolescence, with sexual abuse reported most frequently (Bandelow et al., 2005; Battle et al., 2004; Johnson, Smailes, Cohen, Brown, & Bernstein, 2000; Pietrek, Elbert, Weierstall, Müller, Rockstroh, 2013; Zanarini et al., 1997). Recent evidence from a longitudinal twin design suggests that the link between childhood abuse and BPD may be due to child vulnerabilities that confer risk for both abuse and BPD (Bornolova et al., 2013). The majority of work in this area has relied on retrospective reports of childhood abuse, which may conflate adversity exposure with negative cognitive biases associated with the disorder at the time of the assessment. Providing stronger support for family adversity as a risk factor, a recent study relying on prospective assessments demonstrated harsh parenting and family conflict predicted BPD at age 11 (Winsper, Zanarini, & Wolke, 2012). Additionally, samples have largely been comprised of White, middle-class women, limiting our ability to understand the impact of chronic poverty and its sweeping sequelae on the development of BPD symptoms in more diverse populations that would be expected to experience greater cumulative adversities and stress.
While the independent effects of childhood adversity and emotional vulnerability have been shown to relate to BPD, the transaction between these factors is complex and multi-faceted. A transactional model of BPD development would assume that youth with high levels of negative emotional reactivity are at increased risk for numerous adverse life events and are inadequately prepared to cope with them. This ineffective emotional response in turn sets them up to experience more stressful life events which further depletes their resources to cope. While the directionality of adverse experiences and negative emotional reactivity is difficult to determine (Glaser, van Os, Portegijs, & Myin-Germeys, 2006; Wichers et al., 2009), we use prospectively gathered data on adversity measured prior to our negative emotional reactivity assessment to investigate whether the relationship between child-level vulnerability and BPD symptom development is exacerbated for girls experiencing family adversity in the form of poverty, single parenthood, and other difficult life circumstances. Additionally, our measure of family adversity relied exclusively on parent-reports to further safeguard against confabulation between adversity exposure, negative emotional reactivity, and BPD symptoms.
Current Study
The current study examined negative emotional reactivity as a marker of vulnerability for the development of BPD in late adolescent girls. Within this broad goal, several more specific goals were addressed. First, using a multi-method index, we examined negative emotional reactivity as a predictor of aberrant developmental patterns of BPD symptoms. Based on normative personality development, we expected to find an overall decline in BPD symptoms during late adolescence. In contrast to this normative decline, we expected negative emotional reactivity to predict higher and/or increasing levels of BPD symptoms from age 16 to 18 years. Second, we examined the impact of exposure to family adversity across childhood and adolescence on the development of BPD symptoms. We expected that exposure to family adversity would predict higher levels and/or increasing levels of BPD symptoms across late adolescence. Third, we examined the interplay between negative emotional reactivity and childhood adversity as predictors of BPD symptom development in girls during late adolescence. We hypothesized that negative emotional reactivity would increase the risk for BPD symptoms, providing support for its role as a marker of vulnerability. Moreover, the relationship between negative emotional reactivity and BPD symptoms would be stronger in the context of greater exposure to family adversity. Conversely, we expected the relationship between negative emotional reactivity and BPD symptoms to be mitigated for those with less exposure to family adversity.
Method
Participants and Recruitment Procedures
Participants were recruited from the longitudinal Pittsburgh Girls Study (PGS) for a multi-method substudy on girls’ personality development (“Personality Study”). The PGS involves an urban community sample of four age cohorts of girls who were ages 5–8 years at the first assessment in 2000/2001 and have been followed with annual assessments for the past 14 years. The PGS sample was identified by oversampling from low-income neighborhoods, such that neighborhoods in which at least 25% of families were living at or below poverty level were fully enumerated and a random selection of 50% of households in all other neighborhoods were enumerated. Of the 2,875 eligible families that were contacted to determine interest in study participation, 2,450 families (85%) agreed to participate in the PGS and provided informed consent (see Hipwell et al., 2002; Keenan et al., 2010 for further details on PGS study design and recruitment).
A total of 113 adolescent girls (all age 16 at the time of recruitment) were selected from the larger PGS for participation in the Personality substudy in 2010–2012 (girls in age cohort 7 in 2010, cohort 6 in 2011, and cohort 5 in 2012). Girls were recruited based on their self-reports on the Affective Instability subscale of the Personality Assessment Inventory (PAI-AI; Morey, 1991; described further under Measures), which was administered as part of the PGS annual assessment battery. The sampling strategy was designed to produce a sample with a high degree of variability in this core symptom of BPD, and thus, a sample representing a wide range of risk for BPD. Unlike measures of temperament negative emotionality or trait neuroticism, the PAI-AI assesses mood intensity and variability (e.g., “My mood can shift quite suddenly”). The PAI-AI contains six items scored on a four-point scale (0=false, not at all true, 3=very true). These items were summed to create an AI index. Scores > 11 on the PAI-AI (two standard deviations above the mean score for community participants) suggest clinical significance (Morey, 1991; Trull, 1995; Trull, Useda, Conforti, & Doan, 1997). To ensure representation of girls with high levels of affective instability, participants with PAI-AI scores in the clinically significant range were oversampled. Accordingly, 26% percent of the subsample scored in the clinically significant range on this measure. Reflecting the demographic characteristics of the PGS, the subsample was racially and socioeconomically diverse (67% African American, 33% European American; 56% of families reported receiving public assistance in the past year).
Assessment Procedures and Measures
Overview
This multi-method study combines self- and parent-reports from the PGS with daily ecological assessments and observer-rated data collected in the Personality substudy. For the PGS, separate in-home interviews for both the girl and parent were conducted annually by trained interviewers using a laptop computer. Measures of BPD features across three consecutive years (spanning ages 16–18)2 as well as sociodemographic characteristics, stressful family experiences, temperament, and exposure to sexual abuse were obtained from these PGS interviews. Within the Personality substudy, adolescent BPD symptoms were assessed via semi-structured clinical interviews at age 16. Additionally, girls completed a one-week cellular phone-based ecological assessment protocol to measure daily emotional reactivity to negative events, which is further described below. As part of this substudy protocol, girls and their biological mothers were also videotaped while completing a structured conflict discussion task in the laboratory. All study procedures were approved by the University Institutional Review Board. Families were compensated for their participation.
BPD symptoms
BPD symptoms were assessed in three consecutive years with girls’ reports at ages 16, 17, and 18 using questions from the screening questionnaire of the International Personality Disorders Examination (IPDE-BOR; Loranger et al., 1994). Although the IPDE screening questionnaire was originally developed for adults, this questionnaire has been validated for use in adolescent samples (Chanen et al., 2008; Stepp, Burke, Hipwell, & Loeber, 2012; Stepp, Pilkonis, Hipwell, Loeber, & Stouthamer-Loeber, 2010) and found to have adequate concurrent validity, sensitivity, and specificity to clinicians’ diagnosis in a sample of youth, with a score of 4 or greater considered to be clinically significant (Smith, Muir, & Blackwood, 2005). The IPDE-BOR consists of nine items (e.g., “I get into very intense relationships that don’t last”) rated either true or false (scored 1 or 0, respectively). Items were summed to yield a dimensional BPD symptom score in each year. One item, “I show my feelings for all to see,” reduced overall internal consistency alphas to unacceptable levels, and was therefore dropped from calculation of BPD symptom totals. In this sample, the average internal consistency for BPD symptom scores was adequate, α = .69, with values ranging from α = .65 (age 16) to α = .76 (age 18). Since the scale contained very few items, we also examined the average inter-item correlation to evaluate internal consistency (Clark & Watson, 2005; Nunnally, 1978, pp. 229–230). The overall average inter-item correlation was in the range reflecting adequate internal consistency (r = 0.23; Clark & Watson, 2005). Thus, based on both the coefficient alphas and the average inter-item correlations, we deemed these scales adequately internally consistent.
The upper quartile of the sample had an average score of 4, which is in the clinically significant range (Smith et al., 2005; Stepp, Burke, Hipwell, & Loeber, 2012). IPDE-BOR self-reports at each assessment year (ages 16–18) were also significantly correlated with clinician-rated BPD dimensional scores (r’s = .52–.60, p’s < .001, N = 113) based on the Structured Clinical Interview for DSM-IV Personality Disorders (SIDP-IV; Pfohl, Blum, & Zimmerman, 1997) administered at age 16. Because we lacked SIDP-IV interview data over multiple assessment years, we used repeated IPDE-BOR scores at ages 16–18 in this report, which allowed us to examine within-individual changes in BPD symptoms over this developmental window. During the age 16 assessment, six girls (5%) met full criteria for BPD (5 or more symptoms above threshold) and 20 girls (18%) met 3 or more criteria for BPD (indicating clinically significant symptoms; Clifton & Pilkonis, 2007) according to the SIDP-IV clinical interview. There was a high degree of variability in the presence of individual BPD symptoms above threshold, particularly excessive anger (36%) and affective instability (25%).
Family adversity
A composite measure of family adversity was comprised of prospectively gathered annual parent reports from Wave 1 (when girls were ages 5–7) through age 16 in the main PGS study. Measures used to compute family adversity included caregivers’ reports on the Difficult Life Circumstances Scale (DLC; Barnard, 1994), as well as single parent status (coded 1 if participant was living in a single parent household, and 0 if they were not) and family poverty (coded 1 if participant’s family was receiving some form of public assistance, and 0 if they were not) in each assessment year. The DLC is a 28-item questionnaire designed to assess life stressors and chronic family problems (e.g., regular arguments or conflicts with family members, partner absence or incarceration, lack of privacy or crowding in the home). Each item was coded yes (1) or no (0), and items were summed to yield an overall scale score for each assessment year. DLC scores in each year were recoded as 1 if the participant was in the top quartile of DLC scores in that year, and as 0 if the participant was not in the top quartile. The overall family adversity index was calculated based on the average of these categorical items (single parent status, family poverty, and DLC top quartile in each year) across time (Wave 1 through age 16) for each participant in order to capture their overall level of exposure to cumulative family adversity on a scale ranging from 0 to 1 (α=0.91). Similar approaches to quantifying cumulative risk have been used in previous studies to combine multiple risk factors into a single construct that is parsimonious and statistically sensitive in small samples (for a review, see Evans, Li, & Whipple, 2013). To characterize the sample in terms of individual risk factors, 62% reported single parent household status, 67% were receiving public assistance, and 66% were in the top quartile of DLC scores for at least one year within the assessment window.
Negative emotional reactivity
Negative emotional reactivity at age 16 was modeled as a latent variable comprised of three manifest variables, each reflecting a distinct method of assessment: 1) self-reported affective instability on the PAI-AI (Morey, 1991); 2) observer ratings of girls’ negative affective behavior in a laboratory conflict discussion with their mothers; and 3) girls’ self-reported emotions in response to negative events in daily life during a week-long ecological assessment protocol. The laboratory conflict discussion coding procedures and daily ecological assessment protocol are described in further detail below.
Conflict discussion task and behavioral coding procedures
Mothers and daughters were videotaped while completing an eight-minute structured discussion task designed to elicit conflict and negative emotion (Furman & Shomaker, 2008; McMakin et al., 2011; O’Connor, Hetherington, Reiss, & Plomin, 1995). This task is described in further detail elsewhere (see Whalen et al., in press). Briefly, mothers and daughters were asked to indicate common areas of conflict in their relationship, and then each dyad was asked to discuss a topic that they both rated highly in terms of frequency and severity of their conflicts. Videotapes of these discussions were then coded using the Revised Interactional Dimensions Coding System (IDCS-R; Furman & Shomaker, 2008), which was originally designed to observationally measure couples’ interactions during problem solving, but was modified for use with adolescents (Furman & Shomaker, 2008). The coding team included a master reliability coder, who was trained by the developers of the coding system, and several research assistants who were trained to acceptable levels of reliability. Coders were blind to each participant’s BPD scores and study hypotheses. Tapes were randomly assigned to each coder, and girls’ behaviors were coded separately from their mothers based on their own individual behaviors during the task. For the current analysis, we utilized ratings of girls’ negative affective behavior during the task, which was coded on a five-point Likert scale with half-point intervals (1= extremely uncharacteristic to 5= extremely characteristic). Examples of negative affective behaviors include negative facial expressions (e.g., eye rolling), body positioning (e.g., crossed arms), and negative emotional tone or quality of voice (e.g., using a harsh tone of voice or yelling). Twenty-one percent of the tapes were coded by all members of the team and were used to calculate intra-class correlation (ICC) coefficients for inter-rater agreement. The ICC for girls’ negative affective behavior codes was good (ICC = .82).
Daily ecological assessment
Girls were given modified, answer-only cellular telephones to use during the daily ecological assessment protocol. Participants were scheduled to receive a maximum of four scheduled telephone calls from research staff per day over the course of seven days to ask them a series of questions about their moods and behaviors. Calls were not scheduled at times when girls were in school or scheduled to work as requiring participants to answer calls during these activities directly violated school policies and most employer-employee contracts. On the last call of each day, participants were asked to rate on a 5-point Likert scale (1 = very slightly or not at all; 5 = extremely) the extent to which they felt four negative emotions (angry, nervous, sad, and upset) “at the worst point” of the most negative event that they experienced that day. The mean number of end-of-day assessments completed in this sample was 4.20 (SD = 1.53; Range = 1–7), and most participants (78%) completed 3 or more end-of-day assessments. Compliance in this study reflects rates commensurate with or greater than those reported in other studies (Silk et al., 2010; Silk Steinberg, & Morris, 2003; Hankin, Mermelstein, & Roesch, 2007). We compared girls with any missing data in the daily assessments (n = 27) to girls with complete data (n = 86) on all other variables included in the current study. The only significant difference was that those with missing data had higher age 15 temperament emotionality temperament scores, t = 2.60, df = 111, p = .01, compared to girls without missing data. Since age 15 temperament was included as a covariate in our analyses, we statistically corrected for any biases due to missing data. We calculated the within-person mean of these four affect ratings across the diary period for each participant to index their overall level of negative affective reactivity to events in daily life. The internal consistency of this construct was adequate (α = .71).
Covariates
To examine the unique main and interactive effects of family adversity and negative emotional reactivity while controlling for other potentially confounding variables, we included minority race (0 = European American; 1 = African American), reported experiences of childhood sexual abuse, and temperament emotionality as covariates. Additionally, because three different age cohorts of girls were recruited across three consecutive years when they reached age 16, we also controlled for potential cohort effects in our model.
Childhood sexual abuse was assessed by annual parent and child reports from ages 12 through 16 in the main PGS. Specifically, at the first assessment parents were asked one yes/no question regarding whether their child had ever experienced any type of sexual assault or abuse and subsequent assessments inquired about sexual assault/abuse occurring in the past year. Similarly, at the age 12 assessment girls were asked four yes/no questions regarding whether they had ever experienced different forms of sexual abuse while subsequent assessments inquired about sexual abuse in the past year. If any of these five questions were endorsed, the girl received a “1”, and if no items were endorsed, the girl received a “0” in that assessment year. Due to the low base rate of reported sexual abuse within each assessment wave, we created a dichotomous summary variable indicating whether a girl or her parent had reported sexual abuse at any time (0 = no reported childhood sexual abuse; 1 = reported childhood sexual abuse). Eight participants (7%) reported experiencing childhood sexual abuse through the age 16 assessment wave.
The temperament dimension reflecting emotionality was assessed via parent report when girls were 15 years-old using the Emotionality, Activity, and Sociability Temperament Survey (Buss & Plomin, 1984). The emotionality subscale consists of five items (e.g., “She cries easily”) scored using a five-point scale (1=a little to 5=a lot). This subscale has demonstrated construct validity in comparisons of girls with and without depression in a community sample (Goodyer, Ashby, Altham, Vize, & Cooper, 1993). In our study, the internal consistency coefficient for the emotionality scale was α=.75.
Data Analytic Plan and Procedures
Hypotheses were tested using latent growth curve models (LGCMs; Duncan, Duncan, & Strycker, 2006) in Mplus version 7 (Muthén & Muthén, 2012). Models were estimated using full-information maximum likelihood estimation with robust standard errors (MLR estimator), which can include missing data and is robust to non-normality. We began by testing an unconditional LGCM to examine the pattern of change in BPD symptoms from ages 16 to 18. We also used a confirmatory factor analysis (CFA) to establish a well-fitting measurement model for negative emotional reactivity. Fit of these models was evaluated holistically by examining multiple indices using conventional guidelines for evaluating good model fit: non-significant χ2 likelihood ratio test; Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) ≥ .95; Root Mean Square Error of Approximation (RMSEA) < .05; and the Standardized Root Mean Square Residual (SRMR) < .08 (Hu & Bentler, 1999; McDonald & Ho, 2002).
Next, we tested the full conditional model with all predictors and the interaction between negative emotional reactivity and family adversity. We also explored all other possible 2- and 3-way interactions in order to rule out moderation of results by other covariates in the model. Only statistically significant interaction terms were retained in the final model. Interactions with latent variable predictor of negative emotional reactivity required the addition of the “TYPE=RANDOM” statement to the “ANALYSIS” command in Mplus, which does not provide comprehensive model fit indices or standardized coefficients because the random statement results in more than one covariance matrix to evaluate. Thus, only unstandardized coefficients for the final model are reported. All predictors (other than manifest variables for the latent variable) were grand-mean centered prior to analysis.
Results
Preliminary Unconditional Growth and Measurement Models
Descriptive statistics (prior to centering) and correlations for all study variables are presented in Table 1. An unconditional linear growth model was initially fit to the BPD data at ages 16 to 18 to examine the developmental growth trajectory of BPD and variability around this trajectory. To disentangle the overall level of BPD from age 16 predictors, the intercept was fixed to the age 17 assessment. The linear model fit the data well, χ2 (1, N = 113) = 1.29, p = .26, RMSEA = .05, CFI = .997, TLI = .991, SRMR = .02. The intercept (M = 2.29, SE = 0.16, z = 14.32, p < .001) and slope (b = −0.21, SE = 0.09, z = −2.48, p = .01) differed significantly from zero. The significant negative slope indicates that BPD symptoms show an overall pattern of linear decrease from ages 16 to 18 years. Significant individual variability was found for the intercept (σ2 = 2.46, SE = 0.34, z = 7.31, p < .001), but not for the slope (σ2 = 0.22, SE = 0.24, z = 0.93, p = .35). These results indicate a high degree of variability within the sample around the mean level of BPD symptoms at age 17, but less variability around the mean rate of change in BPD symptoms over time. The correlation between intercept and slope was not significant (r = 0.16, SE = 0.21, p = .46 suggesting that the estimated mean rate of change over time was unrelated to the mean level of BPD symptoms at age 17.
Table 1.
Descriptive statistics and intercorrelations for all study variables (N = 113)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Race | |||||||||||
| 2. | Cohort | −0.26** | ||||||||||
| 3. | CSA | −0.18 | 0.13 | |||||||||
| 4. | FA | 0.36*** | −0.12 | −0.07 | ||||||||
| 5. | TEMP | 0.02 | −0.02 | −0.11 | 0.14 | |||||||
| 6. | PAI-AI | 0.29** | 0.06 | −0.08 | 0.36*** | 0.14 | ||||||
| 7. | EA-NA | 0.07 | 0.02 | −0.04 | 0.01 | 0.06 | 0.39*** | |||||
| 8. | LAB-NA | −0.02 | −0.08 | −0.06 | 0.09 | 0.19 | 0.30** | 0.44*** | ||||
| 9. | Age 16 BPD | 0.26** | 0.03 | −0.14 | 0.26** | 0.22* | 0.71*** | 0.31** | 0.16 | |||
| 10. | Age 17 BPD | 0.10 | 0.18 | 0.04 | 0.30** | 0.24* | 0.67*** | 0.38*** | 0.29* | 0.66*** | ||
| 11. | Age 18 BPD | 0.11 | 0.20* | 0.03 | 0.35*** | 0.10 | 0.62*** | 0.32** | 0.30* | 0.56*** | 0.64*** | |
|
| ||||||||||||
| M/% | 67.0% | 5.67 | 7.1% | 0.43 | 12.32 | 8.62 | 2.46 | 2.98 | 2.54 | 2.20 | 2.16 | |
| SD | 0.47 | 0.73 | 0.26 | 0.22 | 4.30 | 4.70 | 0.73 | 0.82 | 1.88 | 1.92 | 2.08 | |
Notes. Race coded 0 = European American, 1 = African American. Cohort = age at start of Pittsburgh Girls Study (range = 5–7). CSA = childhood sexual abuse (reported anytime from ages 12 to 16; coded 0 = no reported CSA, 1 = reported experiencing CSA). FA = family adversity index. TEMP = temperament negative emotionality (parent-report at age 15). PAI-AI = affective instability subscale from the PAI-BOR (Morey et al., 1991). EA-NA = average of negative affect ratings in response to daily negative events in the ecological assessment protocol. LAB-NA = girls’ negative affective behavior in the laboratory conflict discussion task. BPD = borderline personality disorder symptoms (self-report).
p < .05.
p < .01.
p < .001.
Next, we fit a CFA model for the latent negative emotional reactivity factor using three indicators: (1) self-report measure of affective instability, (2) observer-rated negative affective during a conflict discussion task, and (3) daily ecological assessment ratings of negative emotions in reaction to stress as manifest variables. The negative emotional reactivity factor was scaled by fixing the factor loading for the self-report indicator to 1. For this step only, in order to achieve model identification to produce fit indices, we constrained the other two factor loadings to equality. This model also fit the data well, χ2 (1, N = 113) = 1.05, p = .31, RMSEA = 0.02, CFI = .998, TLI = .993, SRMR = .03, and factor loadings were strong and significant (λ’s = .50, .62, .71, p’s < .001, for the self-report measure, observational ratings, and daily ecological assessment ratings, respectively).
Conditional Growth Model to Examine Main and Interactive Effects of Negative Emotional Reactivity and Family Adversity on BPD Growth Trajectories
After establishing good fit for the unconditional LGCM for BPD symptoms and a well-fitting measurement model for negative emotional reactivity, we tested a conditional model with BPD growth parameters regressed on mean-centered covariates, including cohort, minority race, temperament negative emotionality, childhood sexual abuse, family adversity, negative emotional reactivity, and the Negative Emotionality Reactivity X Family Adversity interaction term. Unstandardized coefficients for the final model are presented in Table 2. There was a significant effect of cohort on the BPD intercept, indicating that older girls from the PGS who were recruited into the study earlier had higher levels of BPD symptoms at age 17 than younger girls who were recruited later in the study. Race and temperament negative emotionality did not emerge as significant predictors but are important to retain in order to examine the unique main and interactive effects of negative emotional reactivity and family adversity. We also tested all other possible 2- and 3-way interactions between predictors, and none were statistically significant, indicating that cohort, race, temperament emotionality, and childhood sexual abuse did not moderate results.
Table 2.
Unstandardized regression coefficients from the final conditional latent growth curve model
| Covariates | BPD Intercept
|
BPD Slope
|
||
|---|---|---|---|---|
| B | SE | B | SE | |
| Race | −0.06 | 0.24 | −0.32 | 0.22 |
| Cohort | 0.32* | 0.13 | 0.19 | 0.13 |
| TEMP | 0.30 | 0.22 | −0.35 | 0.21 |
| CSA | 0.14 | 0.24 | 0.48* | 0.21 |
| FA | 1.04 | 0.54 | 0.95* | 0.45 |
| NER | 3.68*** | 0.41 | 0.04 | 0.29 |
| NER x FA | 2.17* | 0.89 | 0.14 | 0.93 |
Notes. Race coded 0 = European American, 1 = African American. Cohort = age at start of Pittsburgh Girls Study (range = 5–7). CSA = childhood sexual abuse (reported anytime from ages 12 to 16; coded 0 = no reported CSA, 1 = reported CSA). FA = family adversity index. TEMP = temperament negative emotionality (parent-report at age 15). NER = negative emotional reactivity latent variable. BPD = borderline personality disorder symptoms (self-report). BPD intercept is fixed at the age 17 assessment. BPD Slope = rate of change in BPD symptoms from ages 16 to 18.
p < .05.
p < .01.
p < .001.
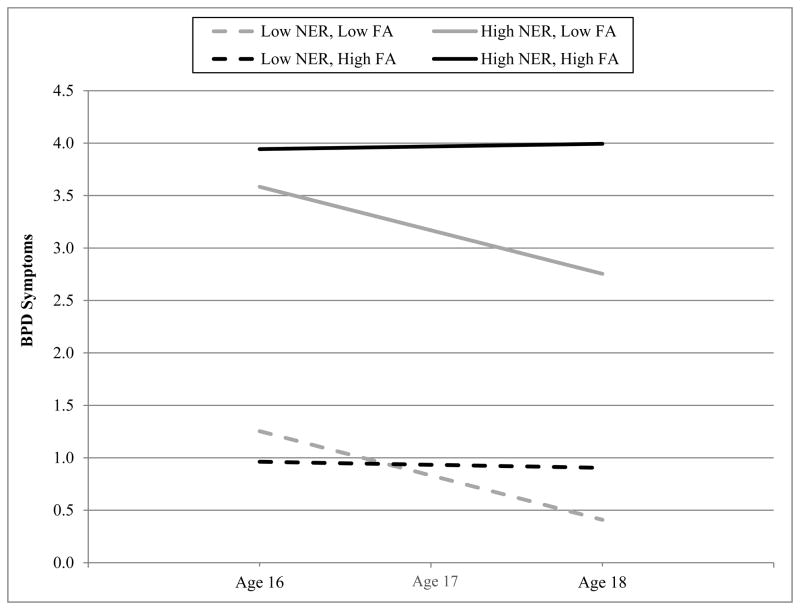
As shown in Table 2, greater levels of negative emotional reactivity predicted a higher mean level of BPD symptoms at age 17, but this effect was moderated by family adversity, as indicated by the significant Negative Emotional Reactivity X Family Adversity interaction effect on intercept. Negative emotional reactivity did not have a main effect on rate of change (slope) in BPD symptoms over time, nor was there a significant interaction between negative emotional reactivity and family adversity for slope. However, greater levels of both family adversity and childhood sexual abuse positively predicted the slope of BPD symptoms over time. To aid in the interpretation of these effects, we plotted the model-implied intercepts and simple slopes and tested their significance (i.e., whether they differed significantly from zero) at high and low levels (−/+1SD) of the predictors using methods described by Preacher, Curran, and Bauer (2006). As illustrated in Figure 1, the influence of family adversity on the mean level of BPD symptoms at age 17 depended on the level of negative emotional reactivity, such that girls who were more emotionally reactive and who also had been exposed to greater family adversity had the highest BPD symptoms at age 17, followed by those who were high in negative emotional reactivity and had been exposed to less adversity. On the other hand, those with low negative emotional reactivity had much lower levels of BPD symptoms at age 17, regardless of their exposure to family adversity. The main effect of family adversity on the rate of change in BPD (i.e., slope) is also visible in Figure 1, demonstrating that BPD symptoms remained relatively stable over time for those exposed to more adversity (high family adversity) and only appear to decrease from ages 16 to 18 for those with low family adversity. However, it should be noted that the slope only differed significantly from zero for those with high negative emotional reactivity and low family adversity, b = −0.43, SE = 0.14, z = −3.07, p < .001, and did not reach significance for those with low negative emotional reactivity and low family adversity, b = −0.42, SE = 0.27, z = −1.52, p = .13. This may be due to the much higher level of BPD symptoms at age 16 (thus, having more room for decrease over time) in those with higher negative emotional reactivity, and also the greater level of variability in trajectories of BPD symptoms for those with high negative emotional reactivity and low family adversity (as reflected in the higher standard error). Hence, girls with greater levels of negative emotional reactivity who were also exposed to more family adversity had the highest mean levels of BPD symptoms, and demonstrated the most maintenance of these symptoms over time.
Figure 1.
Interaction between negative emotional reactivity (NER) and exposure to family adversity (FA) predicting borderline personality disorder (BPD) symptoms at age 17 (intercept) and main effect of FA on rate of change in BPD symptoms from ages 16 to 18. Lines represent model-estimated simple slopes at -1SD to +1SD from the mean of NER and FA.
We also probed the significant effect of childhood sexual abuse on the BPD slope. BPD symptoms remained relatively stable from ages 16 to 18 (i.e., did not significantly decrease over time) for girls who reported experiencing childhood sexual abuse, b = −0.08, SE = 0.10, z = −0.88, p = .38. BPD symptoms only showed a significant decrease among those who did not report experiencing childhood sexual abuse, b = −0.34, SE = 0.11, z = −3.03, p = .003. The effect of childhood sexual abuse was not moderated by negative emotional reactivity or any other covariate. However, these results should be interpreted with caution given the very low base rate of childhood sexual abuse (7%) in this small sample.
Discussion
This study adds to knowledge about the role of emotional vulnerabilities in the development of BPD by demonstrating direct and environmentally-moderated effects of girls’ negative emotional reactivity on BPD symptoms during late adolescence. Although postulated as a critical vulnerability factor in the etiology and development of the disorder, these prospective relationships have not been examined in previous research with adolescents. The use of latent growth curve models revealed a steady decline in BPD symptoms across ages 16 to 18 years mirroring findings from community samples regarding normative changes in personality across development (Beauchaine et al., 2009; Bornovalova et al., 2009; de Clercq et al., 2009; Goodman et al., 2010; Stepp et al., 2014). In the aggregate, these findings suggest girls who fail to desist from BPD symptoms by late adolescence warrant additional assessment for risk.
We found support for our hypothesis that heightened negative emotional reactivity interferes with this maturational decline in BPD symptoms even after controlling for temperamental emotionality. Specifically, findings demonstrated that negative emotional reactivity predicted an overall higher level of BPD symptoms and that exposure to family adversity significantly moderated this effect. As we expected, the relationship between negative emotional reactivity and BPD symptoms was stronger for girls with higher levels of exposure to family adversity. Conversely, the association between our marker of emotional vulnerability and BPD symptoms was weaker in the absence of such adversities.
Contrary to our hypothesis, the interaction between negative emotional reactivity and family adversity did not predict increasing rates of BPD symptoms late adolescence. However, girls heightened negative emotional reactivity and greater exposure to family adversity maintained a high level of BPD symptoms over time. Additionally, our findings revealed a main effect for exposure to family adversity and increasing rates of BPD symptoms. These findings suggest exposure to environmental adversity is a risk factor for increasing levels of BPD symptoms over time even among girls with low levels of negative emotional reactivity.
In sum, our findings are consistent with the large body of research documenting the adverse health outcomes associated with exposure to childhood poverty and the accumulation of risk factors tied to this type of deprivation, such as crowded and substandard housing, family turmoil and violence, and child separations from caregivers due to parental incarceration, drug use, or out-of-area employment (Evans, 2004; Evans & Cassells, 2013; Johnson et al., 2000; van Os et al., 2010). Childhood poverty likely confers vulnerability to poor health via the accumulation of these additional stressors and adversities, which have been linked to aberrant stress responses across multiple regulation systems (Evans & Casseslls, 2013; Evans & Kim, 2007). Consistent with our conceptualization of family adversity as a cumulative index of a myriad of family adversities, previous work suggests that the sheer number of risk factors to which a child is exposed predicts mental health outcomes more so than exposure to a specific type or specific clustering of risk factors (Evans et al., 2014). Future work is needed to determine the impact of cumulative family adversity on other stress regulation systems and how these relationships confer risk for BPD.
Although we interpret with caution due to the small number who reported childhood sexual abuse, exposure to such abuse also predicted increases in BPD symptoms during late adolescence. These findings are consistent with existing studies linking childhood sexual abuse and BPD (Bandelow et al., 2005; Battle et al., 2004; Johnson, Smailes, Cohen, Brown, & Bernstein, 2000; Zanarini et al., 1997). It is important to also consider that childhood sexual abuse in the current study included any instance of sexual abuse that occurred across childhood and adolescence. While little work has examined whether exposure to childhood sexual abuse during specific developmental windows heightens risk for BPD, both the preschool and adolescent years may represent such windows of vulnerability. Pietrek and colleagues (2013) retrospectively examined several types of childhood adversities across ages 3–16 years in a sample of adult inpatients. They found that sexual abuse reported during the preschool (ages 3–5) and adolescent (ages 14–16) years explained a significant amount of variance in BPD diagnosis during adulthood but not in diagnoses of major depressive disorder or schizophrenia. Due to low base rates in the current study, further refinement of sexual abuse, such as by the developmental timing of the abuse (i.e., childhood versus adolescence), was not feasible. Future work is clearly needed to further explicate the nature of the relationship between the timing of exposure to abuse and BPD risk.
There are several strengths to our current study. Importantly, one distinctive aspect lies in our measurement of negative emotional reactivity. We evaluated negative emotional reactivity as a latent trait by incorporating information across multiple methods that varied by informant, time scale, and ecological validity. This analytic strategy enhanced the precision of our emotional vulnerability signal by reducing measurement error. Each referent represented distinct elements of the unitary trait. Adolescent girls’ negative affect during a conflict discussion with their mothers is germane to the developmental period and interpersonal stressors are particularly relevant for BPD pathology. The daily ecological assessment method is consistent with well-established protocols designed to examine negative emotional reactivity to daily stressors in risk for psychopathology, especially schizophrenia and depression (Gottesman & Gould, 2003; Myin-Germeys & van Os, 2007; Wichers et al., 2007; Lataster et al., 2009). It is widely accepted that the use of multiple reporters improves validity (Achenbach, 2006; Holmbeck, Li, Schurman, Friedman, & Coakley, 2002). However, the inclusion of multiple modalities is rarely practiced, and we are not aware of any previous studies that have combined multiple indices of emotional reactivity in this way. We hope future investigations will undertake such efforts to integrate information from multiple sources in hopes of improving validity when measuring markers of vulnerability to psychopathology.
Additional strengths of this study included the use of a longitudinal design and a racially and economically diverse community sample oversampled for BPD risk. The prospective design allowed us to examine the associations between negative emotional reactivity, family adversity, and the developmental trajectories of BPD symptoms without retrospective bias, which has been a major limitation of previous studies relying on adult reports of childhood experiences (Bandelow et al., 2005; Battle et al., 2004; Johnson et al., 2000; Zanarini et al., 1997). The use of community participants rather than clinical patients ensures that the prospective associations observed are more representative of the development of BPD that unfolds in the general population and are less likely to be biased by the effects of treatment or characteristics that are specific to those that seek treatment.
This study is not without limitations. Our indices of negative emotional reactivity were not measured prior to age 16 so it is not possible to determine the reciprocal influence of childhood adversity and negative emotional reactivity. While we cannot rule out that negative emotional reactivity would predispose girls to more adversity, the prospective nature of our assessments and the nature of our family adversity variable (e.g., poverty, parent incarceration) lessen concerns that girls’ negative emotional reactivity would be driving exposure to such adversities. As girls enter young adulthood and exert more control over their environment, it will be important to examine reciprocal associations between negative emotional reactivity and exposure to adversity. Another limitation concerns the limited generalizability of our findings. The sample did not include boys and so the findings may not generalize to male-only or mixed-gender samples. In addition, BPD was not measured repeatedly with a semi-structured interview but relied on interview guided self-reports. However, this measure has been widely used in adolescent community and psychiatric patient samples and its relationship to diagnosis is well established (Loranger et al., 1994; Chanen et al., 2008). Finally, the strong bivariate correlations between the self-report measure of negative emotional reactivity and borderline symptoms reflect shared method variance at least to some extent. However, since we used the self-report measure as a referent of a latent negative emotional reactivity variable, we reduced the overlap between negative emotional reactivity and BPD symptoms due to shared method variance.
Our findings have several implications for etiological models of BPD. Consistent with several developmental theories of BPD, negative emotional reactivity during adolescence is a vulnerability factor, heightening risk for symptoms of the disorder. Furthermore, we found further support for the notion that this emotional vulnerability is environmentally moderated by exposure to the cumulative effects of family adversity. While most theoretical models stress the role of parental responses to the child or childhood trauma as potential stressors preceding the onset of the disorder, we have extended this framework by demonstrating that the environmental risk is also apparent at the level of family adversity. This finding is consistent with previous work demonstrating the link between family level adversities, especially those associated with the experience of poverty, and other forms of severe mental illness (Evans, 2004; van Os et al., 2010).
Although more research is needed to directly inform prevention and intervention efforts, the findings from the current study offer several things to consider. First, developing screening instruments for the detection of negative emotional reactivity among youth exposed to chronic poverty and family stress may be beneficial for identifying youth in most need of services. Findings also suggest potential avenues for prevention strategies. Vulnerable youth with high levels of negative emotional reactivity might benefit from stress inoculation training to enhance emotion regulation in the face of environmental stressors. Additionally, eliminating stressors occurring in the family system may be integral to prevention and intervention efforts, especially for emotionally vulnerable youth.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (MH056630), the National Institute on Drug Abuse (DA012237). Dr. Stepp’s effort was supported by K01 MH086713.
Footnotes
To ensure the distinguishability of temperament emotionality from the more circumscribed indicators of negative emotional reactivity, we ran an additional confirmatory factor analysis that included temperament emotionality as one of the manifest indicators. The factor loading for temperament emotionality was non-significant, suggesting that temperament emotionality is not an informative indicator of our latent variable and does not share much in common with the other indicators included. Based on this evidence, temperament emotionality appears distinct from negative emotional reactivity.
Because the youngest cohort of girls had not yet reached age 18 by the most recent PGS assessment wave, BPD data at age 18 are missing for nine girls. The estimation methods described herein allow missing data, and therefore, the entire sample was included in the reported analyses.
Contributor Information
Stephanie D. Stepp, University of Pittsburgh School of Medicine
Lori N. Scott, University of Pittsburgh School of Medicine
Neil P. Jones, University of Pittsburgh School of Medicine
Diana J. Whalen, University of Pittsburgh
Alison E. Hipwell, University of Pittsburgh School of Medicine
References
- Achenbach TM. As others see us clinical and research implications of cross-informant correlations for psychopathology. Current Directions in Psychological Science. 2006;15(2):94–98. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Bagge CL, Nickell A, Stepp SD, Durrett C, Jackson K, Trull TJ. Borderline personality disorder features predict negative outcomes 2 years later. Journal of Abnormal Psychology. 2004;113(2):279–288. doi: 10.1037/0021-843X.113.2.279. [DOI] [PubMed] [Google Scholar]
- Bandelow B, Krause J, Wedekind D, Broocks A, Hajak G, Rüther E. Early traumatic life events, parental attitudes, family history, and birth risk factors in patients with borderline personality disorder and healthy controls. Psychiatry Research. 2005;134(2):169–179. doi: 10.1016/j.psychres.2003.07.008. [DOI] [PubMed] [Google Scholar]
- Barnard KE. Difficult life circumstances scale. Seattle, WA: NCAST Publications; 1994. [Google Scholar]
- Bateman AW, Fonagy P. The development of an attachment-based treatment program for borderline personality disorder. Bulletin of the Menninger Clinic. 2003;67(3):187–211. doi: 10.1521/bumc.67.3.187.23439. [DOI] [PubMed] [Google Scholar]
- Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, Sanislow CA, et al. Childhood maltreatment associated with adult personality disorders: Findings from the collaborative longitudinal personality disorders study. Journal of Personality Disorders. 2004;18(2):193–211. doi: 10.1521/pedi.18.2.193.32777. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: A biology x sex x environment interaction model of antisocial and borderline traits. Development and Psychopathology. 2009;21(3):735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Development and Psychopathology. 2009;21(4):1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Huibregtse BM, Hicks B, Iacono W, McGue M. Tests of a direct effect of childhood abuse on adult borderline personality disorder traits: A longitudinal discordant twin design. Journal of Abnormal Psychology. 2013;122:180–194. doi: 10.1037/a0028328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley R, Zittel Conklin C, Westen D. The borderline personality disorder diagnosis in adolescents: gender differences and subtypes. Journal of Child Psychology and Psychiatry. 2005;46:1006–1019. doi: 10.1111/j.1469-7610.2004.00401.x. [DOI] [PubMed] [Google Scholar]
- Buss AH, Plomin R. Temperament: Early developing personality traits. Hillsdale, NJ: Erlbaum; 1984. [Google Scholar]
- Chanen AM, Jovev M, Djaja D, McDougall E, Yuen HP, Rawlings D, Jackson HJ. Screening for borderline personality disorder in outpatient youth. Journal of Personality Disorders. 2008;22(4):353–364. doi: 10.1521/pedi.2008.22.4.353. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Constructing validity: Basic issues in objective scale development. Psychological Assessment. 1995;7(3):309– 319. doi: 10.1037/pas0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifton A, Pilkonis PA. Evidence for a single latent class of Diagnostic and Statistical Manual of Mental Disorders borderline personality pathology. Comprehensive Psychiatry. 2007;48(1):70–78. doi: 10.1016/j.comppsych.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Coid J, Yang M, Tyrer P, Roberts A, Ullrich S. Prevalence and correlates of personality disorder among adults aged 16 to 74 in Great Britain. British Journal of Psychiatry. 2006;188:423–431. doi: 10.1192/bjp.188.5.423. [DOI] [PubMed] [Google Scholar]
- Conger RD, Conger KJ, Martin MJ. Socioeconomic Status, Family Processes, and Individual Development. Journal of Marriage and the Family. 2010;72(3):685–704. doi: 10.1111/j.1741-3737.2010.00725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger RD, Ge X, Elder GH, Lorenz FO, Simons RL. Economic Stress, Coercive Family Process, and Developmental Problems of Adolescents. Child Development. 1994;65(2):541–561. [PubMed] [Google Scholar]
- Conger RD, Wallace LE, Sun Y, Simons RL, McLoyd VC, Brody GH. Economic pressure in African American families: A replication and extension of the family stress model. Developmental Psychology. 2002;38(2):179–193. [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan M. A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin. 2009;135(3):495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Clercq B, van Leeuwen K, van den Noortgate W, de Bolle M, de Fruyt F. Childhood personality pathology: Dimensional stability and change. Development and Psychopathology. 2009;21(Special Issue 03):853–869. doi: 10.1017/S0954579409000467. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Strycker A. An Introduction to latent variable growth curve modeling: Concepts, issues, and application. 2. Mahwah, NJ: Lawrence Erlbaum Associates, Inc., Publishers; 2006. [Google Scholar]
- Eppright TD, Kashani JH, Robinson BD, Reid JC. Comorbidity of conduct disorder and personality disorders in an incarcerated juvenile population. American Journal of Psychiatry. 1993;150:1233–1236. doi: 10.1176/ajp.150.8.1233. [DOI] [PubMed] [Google Scholar]
- Evans GW. The environment of childhood poverty. American Psychologist. 2004;59:77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Evans GW, Cassells RC. Childhood poverty, cumulative risk exposure, and mental health in emerging adults. Clinical Psychological Science. 2013 doi: 10.1177/2167702613501496. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Kim P. Childhood poverty and health: Cumulative risk exposure and stress dysregulation. Psychological Science. 2007;18:953–957. doi: 10.1111/j.1467-9280.2007.02008.x. [DOI] [PubMed] [Google Scholar]
- Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psycholological Bulletin. 2013;139(6):1342–1396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- Fossati A, Madeddu F, Maffei C. Borderline personality disorder and childhood sexual abuse: a meta-analytic study. Journal of Personality Disorders. 1999;13(3):268–280. doi: 10.1521/pedi.1999.13.3.268. [DOI] [PubMed] [Google Scholar]
- Furman W, Shomaker LB. Patterns of interaction in adolescent romantic relationships: Distinct features and links to other close relationships. Journal of Adolescence. 2008;31(6):771–788. doi: 10.1016/j.adolescence.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser JP, van Os J, Portegijs PJ, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. Journal of Psychosomatic Research. 2006;61(2):229–236. doi: 10.1016/j.jpsychores.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Glaser JP, van Os J, Mengelers R, Myin-Germeys I. A momentary assessment study of the reputed emotional phenotype associated with borderline personality disorder. Psychological Medicine. 2008;38:1231–1239. doi: 10.1017/S0033291707002322. [DOI] [PubMed] [Google Scholar]
- Goodman M, Patil U, Triebwasser J, Diamond E, Hiller A, Hoffman P, Goldberg S, et al. Parental viewpoints of trajectories to borderline personality disorder in female offspring. Journal of Personality Disorders. 2010;24:204–216. doi: 10.1521/pedi.2010.24.2.204. [DOI] [PubMed] [Google Scholar]
- Goodyer IM, Ashby L, Altham PM, Vize C, Cooper PJ. Temperament and major depression in 11 to 16 year olds. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1993;34(8):1409–1423. doi: 10.1111/j.1469-7610.1993.tb02099.x. [DOI] [PubMed] [Google Scholar]
- Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. American Journal of Psychiatry. 2003;160:636–645. doi: 10.1176/appi.ajp.160.4.636. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, Smith SM, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69(4):533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Becker DF, Walker ML, Levy KN, Edell WS, McGlashan TH. Psychiatric comorbidity in adolescent inpatients with substance use disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34(8):1085–1091. doi: 10.1097/00004583-199508000-00019. [DOI] [PubMed] [Google Scholar]
- Hipwell AE, Loeber R, Stouthamer-Loeber M, Keenan K, White HR, Kroneman L. Characteristics of girls with early onset disruptive and antisocial behaviour. Criminal Behaviour and Mental Health. 2002;12(1):99–118. doi: 10.1002/cbm.489. [DOI] [PubMed] [Google Scholar]
- Holm AL, Severinsson E. Struggling to recover by changing suicidal behaviour: Narratives from women with borderline personality disorder. International Journal of Mental Health Nursing. 2011;20(3):165–173. doi: 10.1111/j.1447-0349.2010.00713.x. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN, Li ST, Schurman JV, Friedman D, Coakley RM. Collecting and managing multisource and multimethod data in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27(1):5–18. doi: 10.1093/jpepsy/27.1.5. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Johnson JG, Smailes EM, Cohen P, Brown J, Bernstein DP. Associations between four types of childhood neglect and personality disorder symptoms during adolescence and early adulthood: Findings of a community-based longitudinal study. Journal of Personality Disorders. 2000;14(2):171–187. doi: 10.1521/pedi.2000.14.2.171. [DOI] [PubMed] [Google Scholar]
- Jovev M, Jackson HJ. The relationship of borderline personality disorder, life events and functioning in an Australian psychiatric sample. Journal of Personality Disorders. 2006;20:205–217. doi: 10.1521/pedi.2006.20.3.205. [DOI] [PubMed] [Google Scholar]
- Keenan K, Hipwell A, Chung T, Stepp S, Stouthamer-Loeber M, Loeber R, McTigue K. The Pittsburgh Girls Study: overview and initial findings. Journal of Clinical Child and Adolescent Psychology. 2010;39(4):506–521. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kernberg O. Severe personality disorders: Psychotherapeutic strategies. New Haven, CT: Yale University Press; 1984. [Google Scholar]
- Lataster T, Wichers M, Jacobs N, Mengelers R, Derom C, Thiery E, van Os J, Myin-Germeys I. Does reactivity to stress cosegregate with subclinical psychosis? A general population twin study. Acta Psychiatrica Scandinavica. 2009;119:45–53. doi: 10.1111/j.1600-0447.2008.01263.x. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Lane M, Loranger AW, Kessler RC. DSM-IV personality disorders in the national comorbidity replication (NCSR) Biological Psychiatry. 2007;62:553–564. doi: 10.1016/j.biopsych.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Cognitive Behavioral Treatment of Borderline Personality Disorder. New York: Guilford Press; 1993. [Google Scholar]
- Loranger AW, Sartorius N, Andreoli A, Berger P, Buchheim P, Channabasavanna SM, Ferguson B. The International Personality Disorder Examination. Psychological Assessment Resources, Inc; 1994. [DOI] [PubMed] [Google Scholar]
- McDonald RP, Ho MR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7(1):64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- McMakin DL, Burkhouse KL, Olino TM, Siegle GJ, Dahl RE, Silk JS. Affective functioning among early adolescents at high and low familial risk for depression and their mothers: A focus on individual and transactional processes across contexts. Journal of Abnormal Child Psychology. 2011;39(8):1213–1225. doi: 10.1007/s10802-011-9540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AL, Muehlenkamp JJ, Jacobson CM. Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clinical Psychology Review. 2008;28(6):969–981. doi: 10.1016/j.cpr.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Morey LC. Personality assessment inventory: Professional manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Muthén BO, Muthén LK. Mplus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- Myers WC, Burkett RC, Otto TA. Conduct disorder and personality disorders in hospitalized adolescents. Journal of Clinical Psychiatry. 1993;54:21–26. [PubMed] [Google Scholar]
- Myin-Germeys I, van Os J. Stress-reactivity in psychosis: Evidence for an affective pathway to psychosis. Clinical Psychology Review. 2007;27:409–424. doi: 10.1016/j.cpr.2006.09.005. [DOI] [PubMed] [Google Scholar]
- Nunnally JC. Psychometric theory. 2. New York, NY: McGraw-Hill; 1978. pp. 229–230. [Google Scholar]
- O’Connor TG, Hetherington EM, Reiss D, Plomin R. A twin-sibling study of observed parent-adolescent interactions. Child Development. 1995;66(3):812–829. [PubMed] [Google Scholar]
- Pagano ME, Skodol AE, Stout RL, Shea MT, Yen S, Grilo CM, Sanislow CA, et al. Stressful life events as predictors of functioning: findings from the Collaborative Longitudinal Personality Disorders Study. Acta Psychiatrica Scandinavica. 2004;110:421–429. doi: 10.1111/j.1600-0447.2004.00398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrek C, Elbert T, Weierstall R, Müller O, Rockstroh B. Childhood adversities in relation to psychiatric disorders. Psychiatry Research. 2013;206:103–110. doi: 10.1016/j.psychres.2012.11.003. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured Interview for DSM-IV Personality: SIDP-IV. Washington, DC: American Psychiatric Association; 1997. [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31(4):437–448. [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31(4):437–448. [Google Scholar]
- Rothbart MK. Temperament, development, and personality. Current Directions in Psychological Science. 2007;16(4):207–212. [Google Scholar]
- Sansone RA, Sansone LA. The families of borderline patients: The psychological environment revisited. Psychiatry. 2009;6(2):19–24. [PMC free article] [PubMed] [Google Scholar]
- Shiner RL, Buss KA, McClowry SG, Putnam SP, Saudino KJ, Zentner M. What is temperament now? Child Development Perspectives. 2012;6(4):436–444. [Google Scholar]
- Silk JS, Forbes EE, Whalen DJ, Jakubcak JL, Thompson WK, Ryan ND, Dahl RE. Daily emotional dynamics in depressed youth: A cell phone ecological momentary assessment study. Journal of Experimental Child Psychology. 2010 doi: 10.1016/j.jecp.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Steinberg L, Morris AS. Adolescents’ Emotion Regulation in Daily Life: Links to Depressive Symptoms and Problem Behavior. Child Development. 2003;74(6):1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- Sinha BK, Watson DC. Psychosocial predictors of personality disorder traits in a non-clinicalsample. Personality and Individual Differences. 1997;22:527–537. [Google Scholar]
- Skodol AE, Bender DS. Why are women diagnosed borderline more than men? Psychiatric Quarterly. 2003;74(4):349–360. doi: 10.1023/a:1026087410516. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Pagano ME, Bender DS, Shea MT, Gunderson JG, Yen S, Stout RL, et al. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychological Medicine. 2005;35(3):443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DJ, Muir WJ, Blackwood DHR. Borderline personality disorder characteristics in young adults with recurrent mood disorders: A comparison of bipolar and unipolar depression. Journal of Affective Disorders. 2005;87(1):17–23. doi: 10.1016/j.jad.2005.02.019. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Lynch KG, Kelly TM. Childhood abuse as a risk factor for suicidal behavior in borderline personality disorder. Journal of Personality Disorders. 2002;16(3):201–214. doi: 10.1521/pedi.16.3.201.22542. [DOI] [PubMed] [Google Scholar]
- Stepp SD. Development of Borderline Personality Disorder in Adolescence and Young Adulthood: Introduction to the Special Section. Journal of Abnormal Child Psychology. 2012;40:1–5. doi: 10.1007/s10802-011-9594-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. Journal of Abnormal Child Psychology. 2012;40(1):7–20. doi: 10.1007/s10802-011-9530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Pilkonis PA, Hipwell AE, Loeber R, Stouthamer-Loeber M. Stability of borderline personality disorder features in girls. Journal of Personality Disorders. 2010;24(4):460–472. doi: 10.1521/pedi.2010.24.4.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Whalen DJ, Scott LN, Zalewski M, Loeber R, Hipwell AE. Reciprocal effects of parenting and borderline personality disorder symptoms in adolescent girls. Development and Psychopathology. 2014;20:1–18. doi: 10.1017/S0954579413001041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiglmayr CE, Grathwol T, Linehan MM, Ihorst G, Fahrenberg J, Bohus M. Aversive tension in patients with borderline personality disorder: a computer-based controlled field study. Acta Psychiatrica Scandinavica. 2005;111:372–379. doi: 10.1111/j.1600-0447.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- Trull TJ. Borderline personality disorder features in nonclinical young adults: I. Identification and validation. Psychological Assessment. 1995;7(1):33–41. doi: 10.1037/1040-3590.7.1.33. [DOI] [Google Scholar]
- Trull TJ, Jahng S, Tomko RL, Wood PK, Sher KJ. Revised NESARC personality disorder diagnoses: Gender, prevalence, and comorbidity with substance dependence disorders. Journal of Personality Disorders. 2010;24(4):412–426. doi: 10.1521/pedi.2010.24.4.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Useda JD, Conforti K, Doan BT. Borderline personality disorder features in nonclinical young adults: 2. Two-year outcome. Journal of Abnormal Psychology. 1997;106(2):307–314. doi: 10.1037//0021-843x.106.2.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature. 2010;468:203–212. doi: 10.1038/nature09563. [DOI] [PubMed] [Google Scholar]
- Westen D, Chang C. Personality pathology in adolescence: a review. Adolescent Psychiatry. 2000;25:61–100. [Google Scholar]
- Whalen DJ, Scott LN, Jakubowski K, McMakin D, Hipwell AE, Silk J, Stepp SD. Affective behavior during mother-daughter conflict and borderline personality disorder severity across adolescence. Personality Disorders: Theory, Research, and Treatment. doi: 10.1037/per0000059. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichers MC, Myin-Germeys I, Jacobs N, Peeters F, Kenis G, Derom C, Vlietinck R, et al. Evidence that moment-to-moment variation in positive emotions buffer genetic risk for depression: a momentary assessment twin study. Acta Psychiatrica Scandinavica. 2007;115:451–457. doi: 10.1111/j.1600-0447.2006.00924.x. [DOI] [PubMed] [Google Scholar]
- Wichers M, Geschwind N, Jacobs N, Kenis G, Peeters F, Derom C, Thiery E, et al. Transition from stress sensitivity to a depressive state: Longitudinal twin study. British Journal of Psychiatry. 2009;195:498–503. doi: 10.1192/bjp.bp.108.056853. [DOI] [PubMed] [Google Scholar]
- Winsper C, Zanarini M, Wolke D. Prospective study of family adversity and maladaptive parenting in childhood and borderline personality disorder symptoms in a nonclinical population at 11 years. Psychological Medicine. 42:2404–2420. doi: 10.1017/S0033291712000542. [DOI] [PubMed] [Google Scholar]
- Zanarini M, Williams A, Lewis R, Reich R, Vera S, Marino M, Levin A, et al. Reported pathological childhood experiences associated with the development of borderline personality disorder. American Journal of Psychiatry. 1997;154(8):1101–1106. doi: 10.1176/ajp.154.8.1101. [DOI] [PubMed] [Google Scholar]
- Zweig-Frank Hallie, Paris J. Predictors of outcome in a 27-year follow-up of patients with borderline personality disorder. Comprehensive Psychiatry. 2002;43(2):103–107. doi: 10.1053/comp.2002.30804. [DOI] [PubMed] [Google Scholar]