Abstract
Background/Purpose
Growing evidence suggests behavioral interventions that target a few key behaviors may be effective at improving population level health outcomes, health status indicators, social, economic, physical environments, personal capacity and biological outcomes. A theoretical framework that targets both social and cognitive mechanisms of behavioral interventions is outlined as critical for understanding “ripple effects” of behavioral interventions on influencing a broad range of outcomes associated with improved health and wellbeing.
Methods/Results
Evidence from randomized controlled trials is reviewed and demonstrates support for “ripple effects” – the effects that behavioral interventions have on multiple outcomes beyond the intended primary target of the interventions. These outcomes include physical, psychological and social health domains across the lifespan.
Conclusions
Cascading effects of behavioral interventions have important implications for policy that argue for a broader conceptualization of health that integrates physical, mental, and social wellbeing outcomes into future research to show the greater return on investment.
Behavioral Medicine in the Age of Specialization
Could the dominant approach to behavioral medicine have been somewhat misguided? Much of biomedical research places the emphasis on understanding very specific mechanisms associated with very specific defects. For example, the National Institutes of Health (NIH) defines personalized medicine as “the science of individualized prevention and therapy” (1). Furthermore, the NIH and FDA have announced a new collaboration on translational science to accelerate research into medical products and therapies (2). The intention is to work with academic experts, companies, doctors, patients, and the public to make personalized medicine a reality. The notion of personalized medicine may offer promise of genetic medicine, rapid paced sequencing technology, informatics, and computer science to enhance the care of patients in an individualized approach. Although there may be promise for personalized medicine, there is growing evidence that suggests the field of behavioral medicine is moving beyond personalized medicine in the coming decade to address population health.
Improving the quality of the healthcare experience and focusing on population health, has recently been embraced by leaders at the Institute of Healthcare Improvement, and across many public health and healthcare organizations (3, 4). Population health has generally been defined as the health outcomes of groups of individuals as well as the distributions of health outcomes within a group (5–7). These outcomes are influenced by patterns of health determinants and policies, and interventions that link determinants to policies to improve entire population health and to reduce inequalities between populations (5). Rather than providing a single behavioral intervention based on a behavioral deficit or personal characteristic evidence increasingly suggests that behavioral interventions that target a few key behaviors may be effective at improving population level health outcomes, health status indicators, social, economic, physical environments, personal capacity and biological outcomes (5, 6). Relative cost-effectiveness of resource allocation to multiple determinants has also been included as a specific measure of population health (8). The purpose of this paper, based on my presidential address, is to argue for a more comprehensive approach of conceptualizing evidence-based interventions for improving population level health outcomes and quality of life.
“The Part Can Never Be Well Unless the Whole is Well”
Plato
This idea that a more comprehensive conceptualization of health is essential for wellbeing dates back to the beginning of the inception of the field of behavioral medicine. In 1948 the World Health Organization defined health as “a state of complete physical, mental, and social well-being, and not merely the absence of disease or infirmity” (9). Consistent with these early conceptions of health and wellbeing, the Society of Behavioral Medicine was established in 1979 as a multidisciplinary field “dedicated to promoting the study of the interactions of behavior with biology and the environment, and applying that knowledge to improve the health and wellbeing of individuals, families, communities, and populations.” Thus, these early definitions of the field continue to reflect a need for a broader perspective of understanding health behaviors and outcomes relevant to overall quality of life and wellbeing.
This paper will argue that there is a strong evidence base that demonstrates that behavior change interventions work to improve the health and longevity of individuals, families, communities, and populations. The following review almost exclusively focuses on results from accumulating systematic randomized controlled trials to demonstrate that there is a compelling case for adopting a more comprehensive or multi-behavioral model of behavioral medicine (see Electronic Supplement Materials (ESM) for slides from Presidential Address).
Behavioral Clusters and Ripples
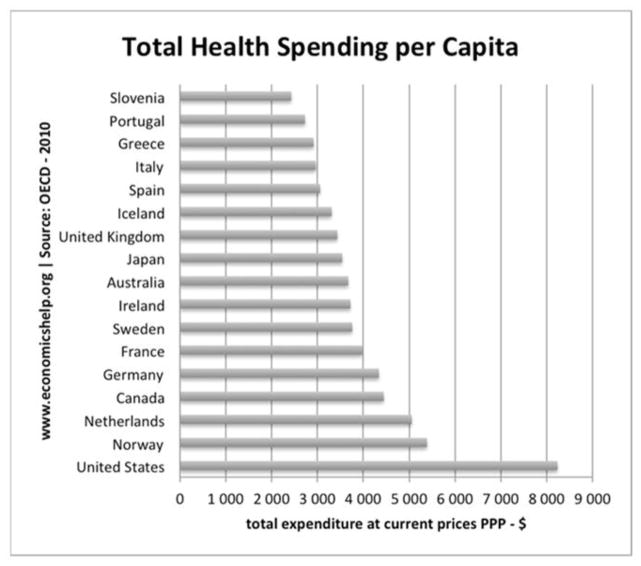
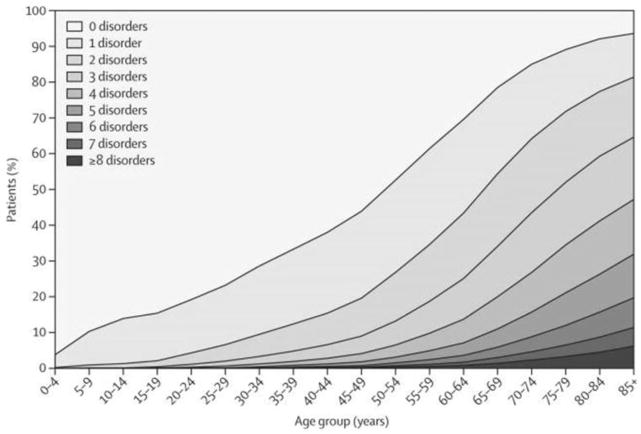
The United States has the highest costs associated with health care expenditures per capita (Figure 1) (10) and among the poorest health outcomes compared to other countries (11). Individuals with multiple chronic conditions are now estimated to include more than one-quarter of all adults in the United States and by age 65 most individuals will have at least two or more chronic conditions (Figure 2) (12). Furthermore, evidence suggest that addressing multiple health behaviors may have additive effects on reducing mortality rates at a population level (13). Matheson and colleagues evaluated the associations between healthy lifestyle habits and mortality in a large, population-based sample stratified by body mass index. The hazard ratios for all cause mortality decreased for individuals who adhered to one or more healthy habits. Even more importantly, in a pooled analysis it was shown that the adoption of each additional healthy habit decreased all-cause mortality between 29–85% (13). These findings are important because they demonstrate the additive effect of engaging in multiple healthy lifestyle behaviors on increasing longevity rates at a population level.
Figure 1.
Healthcare spending per capita
Figure 2.
Multi-morbidity by age
According to the Oxford Alliance for Health, it has been suggested that most chronic diseases are linked to a limited number of health behaviors and that chronic diseases cluster (8). The benefits of preventive health behaviors and the adverse effects of risky health behaviors on morbidity and mortality have been a strong focus of previous research (14). In particular the co-occurrence of lifestyle patterns has been shown to have synergistic effects beyond the expected added effects of separate behaviors on morbidity and mortality (15–17). These synergistic effects have most strongly been shown to increase risk of premature mortality from engaging it high-risk behaviors such as smoking and excessive alcohol use (15–17). Thus, there is a growing attention to managing multiple health-risk behaviors as opposed to single risk factors to increase the effectiveness and decrease the costs of intervention for improving population health outcomes (18).
Indeed, a growing literature has also shown that intervening on preventive health behaviors has substantial “ripple effects” on improving multiple outcomes such as physical, mental and social health, and wellbeing. Thus, the substantial effects on population health may be achieved without a complex level of differential diagnoses as is required in contemporary molecular medicine. In short, the notion that behaviors cluster and show “ripple effects” has important implications for the field of behavioral medicine; and suggests that interventions that target a relatively small number of behaviors may be cost-effective for both people with illness and those who hope to prevent illness.
Many health and social behaviors cluster, and are often driven by common underlying psychological attributes. In youth, health behaviors have been shown to cluster not only with other health behaviors but also with mental and social factors associated with improved quality of life. The complexity of clustering patterns between physical activity, sedentary behaviors and diet was shown in a recent review by Leech et al. (19) and is somewhat difficult to interpret in that sedentary behavior and physical activity are sometimes positively associated. However, large-scale studies in youth that integrate a broader range of physical, mental and social domains have more clearly shown that both risk-taking (20) and mental health factors (21, 22) clustered in the expected directions with eating unhealthy diets and engaging in less physical activity. Problem behavior theory has also shown that risk taking, drug use, and poor diet cluster and are driven by common underlying psychological and social attributes (i.e. risking taking, unconventional social behaviors) (20, 21, 23, 24). Furthermore, social factors such as parental social support and supervision have been shown to be positively associated with improved physical and mental health wellbeing in youth (25). Overall, these studies demonstrate that physical, mental and social behaviors cluster in youth.
Clustering of physical, psychological and social factors has also been examined across the lifespan in young, middle-aged, and older adults. In a study by Grant and colleagues (26) of college-age adults across 21 countries, it was found that life satisfaction- a construct defined as positive subjective wellbeing and characterized by positive hedonic affect- was positively associated with multiple health behaviors such as not smoking, engaging in physical activity, using sun protection, eating fruit and limiting fat intake (after adjusting for age, gender and data clustering). In a recent study by Griffin et al. (27) a cluster analysis was applied in a cohort study involving over 96,000 adults ages 45 years and older. Results demonstrated three dominant clusters related to smoking status, cancer screening and physical activity behaviors. In the high health-risk cluster there were stronger associations with being male, living alone, having low income, living in a poor neighborhood, being psychologically distressed and experiencing low quality of life. Consistent with these findings a population study of over 4,000 adults aged 65 or older showed that more women than men engaged in a higher number of healthy lifestyle behaviors (28). Men in particular who were physically active and drank less alcohol were most likely to engage in these behaviors if they were also non-smokers (28).
Taken together these clustering studies across the lifespan demonstrate that health behaviors cluster with mental and social wellbeing (as well as environmental and social conditions). Thus, developing interventions that intentionally target physical, psychological and social outcomes related to wellbeing may be a cost-effective approach for improving population health.
Mechanisms Underlying Ripple Effects
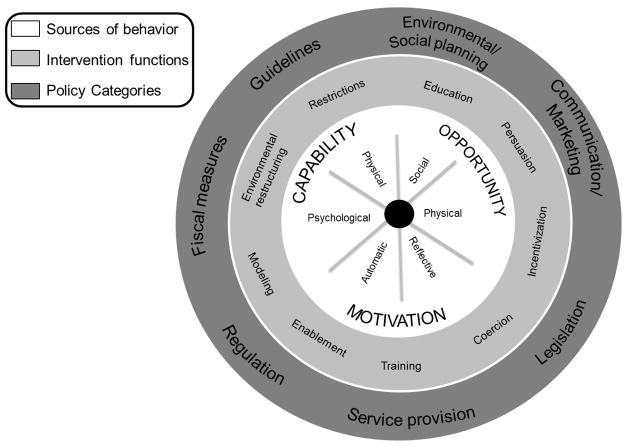
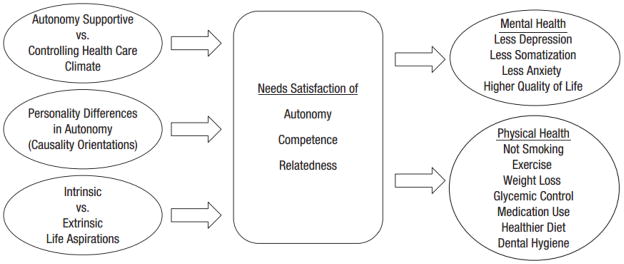
A key question arises from clustering studies - what are the underlying mechanisms that could be targeted to impact a broad range of outcomes related to wellbeing and improved quality of life? Self-Determination Theory (29) argues that all humans have three basic psychological needs that include autonomy (feeling like you have input), competence (feeling effective), and relatedness (feeling understood and cared for by others) that lead to long-term motivation and self-regulation of healthy lifestyles and overall wellbeing. Targeting these three needs are essential for the development of positive psychological growth, integrity, and wellbeing of individuals and for having a high potential to impact multiple behaviors long-term. For example, in a recent meta-analysis of 184 studies this approach was shown to effectively improve a broad range of both mental and physical health outcomes (Figure 3) (30). Consistent with Self-Determination Theory, a recently conducted meta-analysis of 19 behavioral change frameworks by Michie and colleagues, showed that all the basic frameworks can be reduced to a few common domains (Figure 4) (31). Most importantly the three essential intervention elements identified as most relevant in this meta-analysis were capability (behavioral skills), opportunity (environmental conditions) and motivation (drive). These core constructs map onto interventions that either promote behavioral skills or social conditions for shaping health behavioral changes that can be targeted for individuals, families, communities, and population level outcomes. Given the strong theoretical support that behavioral interventions can impact a broad range of outcomes related to wellbeing it is important to understand if these effects occur consistently across a range of systematic randomized trials.
Figure 3.
Self-Determination Theory
Figure 4.
Behavior Change Wheel
Based on the integration of theoretical frameworks presented above, both cognitive and social mechanisms may be important in understanding “ripple effects”. There is growing support that shows that cognitive-behavioral interventions lead to increases in domain specific cognitive constructs related to self-regulation across a variety of domains (including adherence with medical regimens, increasing physical activity) which in turn lead to improvements in both physical and mental health outcomes which are mediated by improvements in overall self-worth and general self-esteem (32–35). Specifically, interventions that target domain specific self-efficacy have been shown to cascade on improving global constructs of self-worth and overall wellbeing that in turn leads to improved mental and social health outcomes. For example, a growing number of studies have demonstrated that cognitive mechanisms are associated with or act as mediators in understanding the effects of physical activity on decreasing depression in both youth and adults. These studies (which include both cross sectional as well as randomized controlled trials) show that both specific self-efficacy for physical activity as well as global self-worth and self-esteem mediated the effects of physical activity on reducing depression (33, 36–39).
A growing evidence-base has also shown that social mediators are also instrumental in achieving “ripple effects”. Interventions based on our work have shown in the Active by Choice Today (ACT) trial (40–42) that a social climate-based intervention (autonomy-supportive) increased minutes of physical activity in intervention versus comparison schools in a large randomized trial during the afterschool hours. Increases in physical activity were also associated with improvements in motivation and perceptions of support from afterschool staff. Interestingly in a follow-up qualitative study, improvements in the quality of student and teacher relationships were reported among intervention schools which was an unexpected social outcome (43). More recently, van Stralen et al. (44) showed that in a school-based multicomponent intervention to increase sports participation in youth, self-efficacy, social support and habit strength were positively associated with increases in sport participation. In addition, changes in social support, self-efficacy, perceived planning skills, enjoyment and habit strength were positively associated with improvements in out-door play. In another study by Eather and colleagues (45), Fit-4-Fun, elementary aged youth participated in an intervention that targeted improving the social support from teachers and the school environmental for physical activity. Both teacher support and the perceived school environment mediated the effect of the intervention on improving physical activity in youth at a 6-month follow-up.
In summary, there is growing support that demonstrates from a theoretical perspective that targeting both cognitive and social mediators within the context of behavioral interventions for individual, family, community or populations- will be most efficacious. Thus, investigators should intentionally integrate cognitive and social elements into their behavioral interventions for long-term lifestyle change to be more cost-effective rather than utilizing intervention approaches that target only a single outcome.
Evidence of Intervention Effects
A crucial question still remains- is there evidence that behavioral interventions have spill over- “ripple effects”-beyond their intended primary target? Evidence-based trials show not only that interventions are effective but that there are “ripple effects”. Because of the benefits of “ripple effects”, some of the advantages of behavioral interventions might be underestimated. To elucidate the mechanisms of “ripple effects” it is important to understand the essential elements of effective evidence-based interventions. Two types of “ripple effects” are included in this review. First, interventions that target a specific outcome may have an unintended “ripple effect” in which the intervention impacts one or more outcomes beyond the originally intended target. Secondly, and most importantly, investigators that target cognitive and social mediators of behavioral change have the ability to deliberately impact multiple outcomes. In this review of “ripple effects”, systematic evidence is reviewed across the lifespan from primarily randomized controlled trials of health behavior interventions that show effects for at least a 1 year duration or longer (see ESM for slides).
Children and Adolescent Populations
“Ripple effects” have been demonstrated in pediatric randomized controlled trials across a variety of health behavior interventions. In the obesity area, research by Epstein and colleagues (46) and by Robinson (47) have shown that by simply limiting the amount of time that youth are offered screen time while still allowing for choice of viewing content results in reducing screen time (the intended outcome of interest). While changes in weight related outcomes were also intended outcomes in these studies, additional unintended ripple effects were found which included reduced energy intake (46) and eating fewer meals in front of the television (47).
Both randomized controlled laboratory and school-based studies that include large samples of youth have shown that interventions which integrate behavioral skill building approaches and teacher support for increasing physical activity have additional benefits on improving spelling and math skills as well as cognitive functioning (48–50). Laboratory studies involving elementary through high school age youth have shown that increases in the dose of physical activity resulted in the target behavior of increasing physical activity (48). However, “ripple effects” also showed significant improvements in memory, attention, and executive functioning such as improved ability for planning and decision-making. School-based studies by Donnelly and colleagues (49) have further shown that teacher support and skill building interventions that promote positive youth engagement in the target behavior of physical activity also showed “ripple effects” on improving spelling and math skills specifically. Furthermore, work by Hillman and colleagues (50) has shown that acute exercise activates brain regions related to improving executive functioning and more complex cognitive processing such as planning and decision making (using measures of neuroelectric changes during cognitive performance tasks). In particular, acute exercise in Hillman and colleague’s study improved response accuracy in incongruent tasks and reading comprehension relative to resting states. These increases in higher level cognitive functioning are critical to self-regulation processes that have been linked to long-term adherence for engaging in healthy lifestyle behaviors.
More evidence of the “ripple effect” comes from the drug prevention literature. Botvin’s Life Skills Training (LST) program is an effective school-based drug prevention program that was intentionally designed to target both cognitive and social mechanisms to lead to improved outcomes across a range of health risk behavior outcomes (51–53). For example, the LST programs specifically target social resistance skills (resisting peer pressure) and social and personal competence skills (positive decision making and improving interpersonal communication skills) and have been shown to result in numerous long-term benefits on targeted behaviors such as preventing smoking, alcohol intake and illicit drug use in youth. In addition these interventions show “ripple effects” on improving social norms, attitudes and self-esteem related to drug use behaviors. The LST curriculum has also been adapted for violence prevention programs (e.g., targeting anger management, conflict resolution skills) and has shown additional benefits on decreasing target behaviors such as verbal and physical aggression as well as broader “ripple effects” on decreasing delinquency. These studies also demonstrate the importance of how the LST school-based interventions can be designed to impact multiple systems including individual level psychological and social outcomes such as improving self-esteem and social norms for resisting drug use (53). At the school level, these programs have led to improvements in the culture for resisting drug use through social climate-based approaches that shift peer norms and psychological skills for resisting drug use (53).
In summary, the trials reviewed above provide selective examples of well-designed systematic evidence that “ripple effects” occur across both health promotion and risk prevention behaviors in youth and that these effects are long-term- lasting at least 1 year or longer.
Adult Populations
A variety of randomized controlled trials have also shown “ripple effects” of behavioral interventions on improving multiple health, psychological, and social health outcomes in young, middle-age and older adults. For example, in a study by Werch and colleagues (54), an intervention approach was used to target the mechanisms underlying multiple health outcomes in young college-age adults. The intervention was based on the “behavior-image” model. This approach argues that activating or creating new social images and prototypes of possible selves can motivate change in divergent health risk and health promoting behaviors based on self-regulation theory. Participants were given feedback to encourage public commitment to multiple concrete goals. The effects of this intervention showed a cascading of intended beneficial outcomes including decreasing alcohol intake, increasing fruit and vegetable intake, and increasing relaxation activities. This study also showed support for the cognitive mediation of the intentional cascading of the effects such that self-efficacy was shown to mediate both the intervention effect on increasing fruit and vegetable intake as well as the intervention effects on increasing engagement in relaxation activities.
“Ripple effects” have also been demonstrated in trials that target weight control and smoking cessation in women and ethnic minorities. A randomized controlled trial by Mata and colleagues (55) examined whether exercise specific motivation could transfer to eating regulation behaviors during a lifestyle weight control program for women. The intervention was designed to increase general motivation for behavioral changes for weight management as well as autonomous exercise motivation. The trial showed a significantly greater effect of the intervention as compared to control group on the targeted outcomes of increasing physical activity and reducing weight over 12 months. However, even more interesting was the “ripple effects” of the intervention such that both general self-determination and autonomous exercise motivation predicted improvements in multiple eating self-regulation outcomes such as eating self-efficacy, eating restraint, eating disinhibition, external eating and emotional eating. In another controlled trial to reduce smoking, African Americans adults were randomized to either a brief motivational interview approach or a brief behavioral educational approach to reduce smoking over 12 months (56). Both interventions successfully reduced smoking at 12 months. Interestingly, secondary data analyses were conducted to evaluate the impact of the interventions on reducing binge drinking. A “ripple effect” demonstrated that the interventions were effective in reducing binge drinking at 6 months although the effects diminished over 12 months. Perhaps intentionally targeting binge drinking in addition to smoking reductions could have led to greater long-term impact in this trial.
Another example of a system related “ripple effect” comes from several large trials such as the Look AHEAD (Action for Health in Diabetes) trial (57) and the Women’s Health trial (58). Although neither trial showed effects on primary endpoints of reduced events or mortality, both trials evaluated the effects of these programs on weight loss and dietary change in both treated and untreated spouses. While treated spouses in the Look AHEAD trial showed the intended targeted effects on weight loss, interestingly untreated wives and husbands in the Look AHEAD trial also showed significant decreases in weight if their spouses participated in the intensive lifestyle condition over 12 months as compared to the control condition. In the Women’s Health Trial while the treated wives showed reductions in energy and fat intake, the “ripple effect” on untreated husbands also showed improvements in reducing energy intake and fat intake as compared to untreated spouses in the control condition. Interestingly improvements in treated wives attitudes for healthy eating and availability of foods in the home were key mechanisms underlying the positive dietary changes seen in the untreated spouses in the Women’s Health Trial (58).
A growing number of studies in adults provide evidence supporting the “ripple effect” of increasing physical activity on improving mental health outcomes such as depression. In the trial by Kerr et al. (59), women were either randomized to a behavioral intervention that targeted increasing motivation and social support for physical activity or a control condition. The effects of the intervention not only increased the targeted outcome of physical activity from baseline to 12-months but also demonstrated a “ripple effect” on decreasing depression from baseline to 6- and 12-months of treatment participants as compared to those in the control group.
As individuals transition into later adulthood and older age there are a number of large scale trials that have shown the benefits of behavioral interventions on impacting more than one chronic disease condition through “ripple effects”. For example, in a trial by Power et al. (60) a self-regulation intervention that was delivered over the phone by nurses resulted in not only decreasing blood pressure, which was the intended targeted outcome, but also led to a unintended improvements in HbA1c outcomes in those patients who also were diagnosed with diabetes. Work by Lorig and colleagues over several decades has also utilized an innovative behavioral intervention that targets self-efficacy and peer norms as underlying mechanisms for deliberately influencing an array of physical, psychological and social outcomes related to overall wellbeing (61). In a number of randomized controlled trials that implemented a comprehensive self-regulation approach targeting skill mastery, reinterpretation of negative symptoms, modeling and group persuasion, results showed effects on a variety of positive outcomes (e.g., improved self-reported health status, physical activity, stretching exercises, relaxation exercises, communication with physicians, self-efficacy) and interestingly showed a “ripple effect” on decreasing health care utilization (62).
In summary this selective review of studies that focus on young, middle-aged, and older adults across the lifespan provides strong support for both intentional and unintentional “ripple effects”. Furthermore, the effectiveness of the behavioral interventions that target both cognitive and social mechanisms led to broader impacts on physical, mental and social outcomes.
Conclusions
In this article, I have reviewed the evidence for conceptualizing a new model of behavioral medicine that may lead to improvements in population health. A general approach to behavioral medicine that focuses on proven interventions for a small number of behaviors might have substantial effects on population health outcomes. This review has demonstrated that there is a compelling case for adopting a more comprehensive or multi-behavioral model of behavioral medicine. By intentionally developing interventions that target underlying cognitive and social mechanisms we will more likely see cascading effects across physical, mental and social outcomes of wellbeing which will ultimately lead to a higher return on our investment.
As communities consider early interventions with significant “ripple effects”, they are challenged in finding the budgetary support and rationale for implementing them. This reflects a series of practical issues related to the United States health policy decision-making. For example, policy makers look for a “return on investment” from social programs, not just in terms of the more abstract improvement of quality of life or productivity, but in real savings to other government programs. Yet, by definition, early intervention may well show a very long-term return on investment. How we can change and build evidence to impact decision makers is a critical area of investigation. Future research is needed to demonstrate both the cost-effectiveness of behavioral interventions and the cost-savings to society.
Finally, often, interventions with significant “ripple effects” may be multi-faceted in nature. As investigators and communities seek to develop these interventions, they must braid together multiple funding streams (often originating at the federal level) to create sufficient resources for the intervention to be successful. This braiding often occurs informally, with localities having to manage different grant requirements (from performance measures to financial accounting). But more systematic approaches need to be undertaken for interventions that have long-term impact on health and wellbeing. In general, funding challenges will continue to be important to advance this more comprehensive model of multi-behavioral approach in the field of behavioral medicine. Funding agencies will need to provide more collaborative and integrated mechanisms rather than silo funding for impacting only single disease outcomes. Researchers and behavioral scientists will need to consider being creative in bridging partnerships and funding sources to compare innovative approaches to better understand how to enhance the cascading effects of behavioral interventions.
Supplementary Material
Acknowledgments
The work was supported, in part, by a grant to Dawn K. Wilson, Ph.D. from the National Institutes of Child Health and Human Development (R01 HD072153). I would like to thank Robert M. Kaplan, Ph.D., Ken Resnicow, Ph.D., and Jeffrey Levi, Ph.D. for their critical input in developing this paper. I would also like to acknowledge Sara M. St. George, Ph.D., Kassandra Alia, M.A., and Nevelyn Trumpeter, M.S., for their support and input on the slides for the presentation (see Electronic Supplement Materials); and my husband Gregory A. King, M.D. for his patience and support during my presidency.
Footnotes
Conflict of Interest and Adherence to Ethical Standards
Dr. Dawn K. Wilson, Ph.D. has no conflict of interest. The studies followed appropriate informed consent procedures and adhered to appropriate ethical standards and the Helsinki Declaration. This studies from the University of South Carolina were approved by the University of South Carolina Institutional Review Board.
The paper was given as part of the Presidential Address at the 35th Annual Society of Behavioral Medicine Meeting and Scientific Sessions.
References
- 1.Cornetta K, Brown CG. Perspective: Balancing Personalized Medicine and Personalized Care. Acad Med. 2013;88:309–313. doi: 10.1097/ACM.0b013e3182806345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hamburg MA, Collins FS. The path to personalized medicine. N Engl J Med. 2010;363:301–304. doi: 10.1056/NEJMp1006304. [DOI] [PubMed] [Google Scholar]
- 3.Feeley D. Leading improvement in population health: focusing on population health requires a new leadership approach. Healthc Exec. 2013;29:82, 84–85. [PubMed] [Google Scholar]
- 4.Stoto MA. Academy Health. 2013. Population health in the affordable care act era. [Google Scholar]
- 5.Kindig D, Stoddart G. What is population health? Am J Public Health. 2003;93:380–383. doi: 10.2105/ajph.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kindig DA. Understanding population health terminology. Milbank Q. 2007;85:139–161. doi: 10.1111/j.1468-0009.2007.00479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kindig DA, Asada Y, Booske B. A population health framework for setting national and state health goals. JAMA. 2008;299:2081–2083. doi: 10.1001/jama.299.17.2081. [DOI] [PubMed] [Google Scholar]
- 8.Suhrcke M, Nugent RA, Stuckler D, Rocco L. Chronic disease: an economic perspective. London: Oxford Health Alliance; 2006. [Google Scholar]
- 9.Taylor SE. Health Psychology. McGraw Hill; 2012. [Google Scholar]
- 10.Organization for Economic Cooperation and Development. US Health Care System from an International Perspective. Paris, France: 2012. [Google Scholar]
- 11.Woolf SH, Aron L. US Health in International Perspective: Shorter Lives, Poorer Health. National Academies Press; 2013. [PubMed] [Google Scholar]
- 12.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications of health care, research, and medical education: A cross sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 13.Matheson EM, King DE, Everett CJ. Healthy lifestyle habits and mortality in overweight and obese individuals. J Am Board Fam Med. 2012;25:9–15. doi: 10.3122/jabfm.2012.01.110164. [DOI] [PubMed] [Google Scholar]
- 14.Spring B, Moller AC, Coons MJ. Multiple health behaviours: overview and implications. J Public Health. 2012;34:i3–i10. doi: 10.1093/pubmed/fdr111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kvaavik E, Batty GD, Ursin G, Huxley R, Gale CR. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: the United Kingdom health and lifestyle survey. Arch Intern Med. 2010;170:711–718. doi: 10.1001/archinternmed.2010.76. [DOI] [PubMed] [Google Scholar]
- 16.McCullough ML, Patel AV, Kushi LH, et al. Following cancer prevention guidelines reduces risk of cancer, cardiovascular disease, and all-cause mortality. Cancer Epidemiol Biomarkers Prev. 2011;20:1089–1097. doi: 10.1158/1055-9965.EPI-10-1173. [DOI] [PubMed] [Google Scholar]
- 17.Tamakoshi A, Tamakoshi K, Lin Y, Yagyu K, Kikuchi S. Healthy lifestyle and preventable death: findings from the Japan Collaborative Cohort (JACC) Study. Prev Med. 2009;48:486–492. doi: 10.1016/j.ypmed.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 18.Prochaska JO, Velicer WF, Redding C, et al. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammograms. Prev Med. 2005;41:406–416. doi: 10.1016/j.ypmed.2004.09.050. [DOI] [PubMed] [Google Scholar]
- 19.Leech RM, McNaughton SA, Timperio A. The clustering of diet, physical activity and sedentary behavior in children and adolescents: a review. Int J Behav Nutr Phys Act. 2014;11:4. doi: 10.1186/1479-5868-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giannakopoulos G, Panagiotakos D, Mihas C, Tountas Y. Adolescent smoking and health-related behaviours: interrelations in a Greek school-based sample. Child Care Health Dev. 2009;35:164–170. doi: 10.1111/j.1365-2214.2008.00906.x. [DOI] [PubMed] [Google Scholar]
- 21.Paxton RJ, Valois RF, Watkins KW, Huebner ES, Drane JW. Associations between depressed mood and clusters of health risk behaviors. Am J Health Behav. 2007;31:272–283. doi: 10.5555/ajhb.2007.31.3.272. [DOI] [PubMed] [Google Scholar]
- 22.Iannotti RJ, Wang J. Patterns of physical activity, sedentary behavior, and diet in U.S. adolescents. J Adoles Health. 2013;53:280–286. doi: 10.1016/j.jadohealth.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chassin L, Pitts SC, Prost J. Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: predictors and substance abuse outcomes. J Consult Clin Psychol. 2002;70:67–78. [PubMed] [Google Scholar]
- 24.Prinstein MJ, Boergers J, Spirito A. Adolescents’ and their friends’ health-risk behavior: Factors that alter or add to peer influence. J Pediatr Psychol. 2001;26:287–298. doi: 10.1093/jpepsy/26.5.287. [DOI] [PubMed] [Google Scholar]
- 25.Mistry R, McCarthy WJ, Yancey AK, Lu Y, Patel M. Resilience and patterns of health risk behaviors in California adolescents. Prev Med. 2009;48:291–297. doi: 10.1016/j.ypmed.2008.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grant N, Wardle J, Steptoe A. The relationship between life satisfaction and health behavior: a cross-cultural analysis of young adults. Int J Behav Med. 2009;16:259–268. doi: 10.1007/s12529-009-9032-x. [DOI] [PubMed] [Google Scholar]
- 27.Griffin B, Sherman KA, Jones M, Bayl-Smith P. The Clustering of Health Behaviours in Older Australians and its Association with Physical and Psychological Status, and Sociodemographic Indicators. Ann Behav Med. 2014;48:205–214. doi: 10.1007/s12160-014-9589-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee Y, Back JH, Kim J, et al. Clustering of multiple healthy lifestyles among older Korean adults living in the community. Geriatr Gerontol Int. 2012;12:515–523. doi: 10.1111/j.1447-0594.2011.00788.x. [DOI] [PubMed] [Google Scholar]
- 29.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 30.Ng JY, Ntoumanis N, Thøgersen-Ntoumani C, et al. Self-determination theory applied to health contexts a meta-analysis. Perspect Psychol Sci. 2012;7:325–340. doi: 10.1177/1745691612447309. [DOI] [PubMed] [Google Scholar]
- 31.Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Annesi JJ, Unruh JL, Marti NC, Gorjala S, Tennant G. Effects of the Coach Approach intervention on adherence to exercise in obese women: assessing mediation of social cognitive theory factors. Res Q Exerc Sport. 2011;82:99–108. doi: 10.1080/02701367.2011.10599726. [DOI] [PubMed] [Google Scholar]
- 33.McPhie ML, Rawana JS. Unravelling the relation between physical activity, self-esteem and depressive symptoms among early and late adolescents: A mediation analysis. Ment Health Phys Act. 2012;5:43–49. [Google Scholar]
- 34.Minnix JA, Blalock JA, Marani S, Prokhorov AV, Cinciripini PM. Self-efficacy mediates the effect of depression on smoking susceptibility in adolescents. Nicotine Tob Res. 2011;13:699–705. doi: 10.1093/ntr/ntr061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Surkan PJ, Gottlieb BR, McCormick MC, Hunt A, Peterson KE. Impact of a health promotion intervention on maternal depressive symptoms at 15 months postpartum. Matern Child Health J. 2012;16:139–148. doi: 10.1007/s10995-010-0729-x. [DOI] [PubMed] [Google Scholar]
- 36.Dishman RK, Hales DP, Pfeiffer KA, et al. Physical self-concept and self-esteem mediate cross-sectional relations of physical activity and sport participation with depression symptoms among adolescent girls. Health Psychol. 2006;25:396. doi: 10.1037/0278-6133.25.3.396. [DOI] [PubMed] [Google Scholar]
- 37.Ryan MP. The antidepressant effects of physical activity: mediating self-esteem and self-efficacy mechanisms. Psychol Health. 2008;23:279–307. doi: 10.1080/14768320601185502. [DOI] [PubMed] [Google Scholar]
- 38.Pickett K, Yardley L, Kendrick T. Physical activity and depression: A multiple mediation analysis. Ment Health Phys Act. 2012;5:125–134. [Google Scholar]
- 39.Petty KH, Davis CL, Tkacz J, Young-Hyman D, Waller JL. Exercise effects on depressive symptoms and self-worth in overweight children: A randomized controlled trial. J Pediatr Psychol. 2009;34:929–939. doi: 10.1093/jpepsy/jsp007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilson DK, Kitzman-Ulrich H, Williams JE, et al. An overview of “The Active by Choice Today” (ACT) trial for increasing physical activity. Contemp Clin Trials. 2008;29:21–31. doi: 10.1016/j.cct.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilson DK, Van Horn ML, Kitzman-Ulrich H, et al. The results of the “Active by Choice Today” trial for increasing physical activity in underserved adolescents. Health Psychol. 2011;30:463–471. doi: 10.1037/a0023390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilson DK, Griffin S, Saunders RP, et al. Using process evaluation for program improvement in dose, fidelity and reach: the ACT trial experience. Int J Behav Nutr Phys Act. 2009;6:79. doi: 10.1186/1479-5868-6-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zarrett N, Skiles B, Wilson DK, McClintock L. A qualitative study of staff’s perspectives on implementing an after school program promoting youth physical activity. Eval Program Plann. 2012;35:417–426. doi: 10.1016/j.evalprogplan.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 44.van Stralen MM, de Meij J, Te Velde SJ, et al. Mediators of the effect of the JUMP-in intervention on physical activity and sedentary behavior in Dutch primary schoolchildren from disadvantaged neighborhoods. Int J Behav Nutr Phys Act. 2012;9:131. doi: 10.1186/1479-5868-9-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eather N, Morgan PJ, Lubans DR. Social support from teachers mediates physical activity behavior change in children participating in the Fit-4-Fun intervention. Int J Behav Nutr Phys Act. 2013;10:68. doi: 10.1186/1479-5868-10-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Epstein LH, Roemmich JN, Robinson JL, et al. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008;162:239–245. doi: 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 48.Davis CL, Tomporowski PD, McDowell JE, et al. Exercise improves executive function and achievement and alters brain activation in overweight children: a randomized, controlled trial. Health Psychol. 2011;30:91–98. doi: 10.1037/a0021766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Donnelly JE, Greene JL, Gibson CA, et al. Physical Activity Across the Curriculum (PAAC): a randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Prev Med. 2009;49:336–341. doi: 10.1016/j.ypmed.2009.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hillman CH, Pontifex MB, Raine LB, et al. The effect of acute treadmill walking on cognitive control and academic achievement in preadolescent children. Neurosci. 2009;159:1044–1054. doi: 10.1016/j.neuroscience.2009.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Botvin GJ, Griffin KW. Life skills training: Empirical findings and future directions. J Prim Prev. 2004;25:211–232. [Google Scholar]
- 52.Botvin GJ, Griffin KW, Nichols TD. Preventing youth violence and delinquency through a universal school-based prevention approach. Prev Sci. 2006;7:403–408. doi: 10.1007/s11121-006-0057-y. [DOI] [PubMed] [Google Scholar]
- 53.Botvin GJ, Griffin KW, Paul E, Macaulay AP. Preventing tobacco and alcohol use among elementary school students through life skills training. J Child Adolesc Subst Abuse. 2003;12:1–17. [Google Scholar]
- 54.Werch CEC, Bian H, Moore MJ, et al. Brief multiple behavior interventions in a college student health care clinic. J Adolesc Health. 2007;41:577–585. doi: 10.1016/j.jadohealth.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mata J, Silva MN, Vieira PN, et al. Motivational “spill-over” during weight control: Increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol. 2009;28:709–716. doi: 10.1037/a0016764. [DOI] [PubMed] [Google Scholar]
- 56.Stahre MA, Brewer RD, Fonseca VP, Naimi TS. Binge drinking among US active-duty military personnel. Am J Prev Med. 2009;36:208–217. doi: 10.1016/j.amepre.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 57.Gorin AA, Wing RR, Fava JL, et al. Weight loss treatment influences untreated spouses and the home environment: evidence of a ripple effect. Int J Obes. 2008;32:1678–1684. doi: 10.1038/ijo.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shattuck AL, White E, Kristal AR. How women’s adopted low-fat diets affect their husbands. Am J Public Health. 1992;82:1244–1250. doi: 10.2105/ajph.82.9.1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kerr J, Patrick K, Norman G, et al. Randomized control trial of a behavioral intervention for overweight women: impact on depressive symptoms. Depress Anxiety. 2008;25:555–558. doi: 10.1002/da.20320. [DOI] [PubMed] [Google Scholar]
- 60.Powers BJ, Olsen MK, Oddone EZ, Bosworth HB. The effect of a hypertension self-management intervention on diabetes and cholesterol control. Am J Med. 2009;122:639–646. doi: 10.1016/j.amjmed.2008.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lorig KR, Ritter PL, Laurent DD, Plant K. Internet-based chronic disease self-management: a randomized trial. Med Care. 2006;44:964–971. doi: 10.1097/01.mlr.0000233678.80203.c1. [DOI] [PubMed] [Google Scholar]
- 62.Ahn S, Basu R, Smith ML, et al. The impact of chronic disease self-management programs: healthcare savings through a community-based intervention. BMC. 2013;13:1141. doi: 10.1186/1471-2458-13-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.