Abstract
The present systematic review critically summarizes results of clinical studies investigating chemical agents to reduce initiation or inactivation of root caries lesions (RCLs). Outcomes were DMFRS/DFRS (decayed, missing, filled root surfaces), surface texture (hard/soft), and/or RCI (root caries index). Three electronic databases were screened for studies from 1947 to 2014. Cross-referencing was used to further identify articles. Article selection and data abstraction were done in duplicate. Languages were restricted to English and German. Mean differences (MD) were calculated for changes in DMFRS/DFRS. Risk ratios (RR) were calculated for changes in surface texture and RCI in a random effects model. Thirty-four articles with 1 or more agents were included; they reported 30 studies with 10,136 patients who were 20 to 101 y old; and they analyzed 28 chemical agents (alone or in combination). Eleven studies investigated dentifrices, 10 rinses, 8 varnishes, 3 solutions, 3 gels, and 2 ozone applications. Meta-analyses revealed that dentifrices containing 5,000 ppm F- (RR = 0.49; 95% confidence interval [95% CI] = 0.42, 0.57; high level of evidence) or 1.5% arginine plus 1,450 ppm F- (RR = 0.79; 95% CI = 0.64, 0.98; very low level) are more effective in inactivating RCLs than dentifrices containing 1,100 to 1,450 ppm F-. Self-applied AmF/SnF2-containing dentifrice and rinse decreased the initiation of RCLs when compared with NaF products (standardized MD = 0.15; 95% CI = −0.22, 0.52; low level). Patients rinsing with a mouth rinse containing 225 to 900 ppm F- revealed a significantly reduced DMFRS/DFRS (MD = −0.18; 95% CI = −0.35, −0.01; low level) when compared with a placebo rinse. Significantly reduced RCI was found for CHX (MD = −0.67; 95% CI = −1.01, −0.32; very low level) as well as SDF (MD = −0.33; 95% CI = −0.39, −0.28; very low level) when compared with placebo varnish. Regular use of dentifrices containing 5,000 ppm F- and quarterly professionally applied CHX or SDF varnishes seem to be efficacious to decrease progression and initiation of root caries, respectively. However, this conclusion is based on only very few well-conducted randomized controlled trials.
Keywords: remineralization, demineralization, prevention, clinical, geriatric dentistry, meta-analyses
Introduction
In an aging world population, dental care and the knowledge regarding prevention of caries is improving, resulting in more retained teeth than what past generations had (Ettinger 1999; US Department of Health and Human Services 2000; Griffin et al. 2004). Besides, the prevalence of gingival recessions increases with age. Thus, root surfaces are more frequently exposed to the oral environment; consequently, the risk for developing root caries lesions (RCLs) is rising, as reported for Germany, where RCL prevalence increased from 15.5% in 1997 to 45% in 2006 in 65- to 74-y-olds (Michaelis and Schiffner 2006).
Caries lesions are supposed to develop more rapidly in dentin than in enamel due to a higher critical pH for dentin that is more frequently reached in surrounding dental biofilm (Peters 2010). Moreover, the access to approximal RCLs for restorative management is limited or requires extensive removal of sound dental hard tissues. Therefore, several approaches to prevent initiation (Burt et al. 1986; Mojon et al. 1998; Tan et al. 2010) or inactivate RCLs (Papas et al. 2007; Ekstrand et al. 2013) have been proposed.
Clinical studies showed that the initiation of RCLs might be significantly reduced by the implementation of preventive dental programs (Mojon et al. 1998) and/or by chemical agents being professionally applied by the dentist (Baca et al. 2009) or by the patients’ themselves (Jensen and Kohout 1988; DePaola 1993). Some of these interventions were shown to prevent new RCLs and/or reverse active into inactive ones. Several narrative reviews with respect to prevention of RCLs have been recently published (Leake 2001; Rodrigues et al. 2011; Ellwood et al. 2012; Walls and Meurman 2012; Gluzman et al. 2013). Nonetheless, no quantitative data synthesis (meta-analysis) has yet been published focusing on the efficacy of various agents to prevent or inactivate RCLs.
Thus, this systematic review aimed to critically summarize and evaluate results of clinical studies investigating chemical agents to reduce initiation of RCLs or inactivate existing ones.
Materials and Methods
Review Design
The present review aimed to systematically retrieve and analyze clinical studies investigating chemical agents to reduce the initiation of RCLs and/or increase their inactivation. A literature search was performed, and study inclusion followed predefined criteria. Extracted data were analyzed, assessing RCL initiation and/or their inactivation for various chemical agents (fluoride compounds, chlorhexidine, ozone treatment, etc.) in different delivery systems (dentifrice, mouth rinse, and varnish). Although analyses showed that different chemical agents may reduce the initiation of RCLs (Appendix Tables 2 and 3), meta-analyses were planned for chemical agents with similar intervention and outcome measures investigated in more than 1 study.
Search Strategy
A database search was performed in PubMed, EMBASE, and Cochrane Central Register of Controlled Trials for clinical studies investigating root caries initiation (development) and root caries inactivation. We independently reviewed title and abstract of articles retrieved by the use of a search strategy (Table 1) for articles published between January 1947 and May 2014. We were not blinded to journal names or article authors. Language was restricted to English and German. A detailed sequence of filtering search results to include relevant articles can be found in the appendix. Gray literature was not evaluated. Agreement concerning study inclusion or data extraction was achieved by discussion. Selected articles were screened full-text. Cross-referencing was performed to identify further articles to be assessed.
Table 1.
Search Strategy as used for PubMed and Embase.
| PubMed | |
| 1 | Search (((root[Title/Abstract]) OR dentin*[Title/Abstract]) OR tooth[Title/Abstract]) OR teeth[Title/Abstract] |
| 2 | Search (caries[Title/Abstract]) OR carious[Title/Abstract] |
| 3 | Search ((#1 and #2)) |
| 4 | Search root caries[MeSH Terms] |
| 5 | Search ((#3 or #4)) |
| 6 | Search ((clinical*[Title/Abstract]) OR adult[Title/Abstract]) OR elderly[Title/Abstract] |
| 7 | Search ((#5 and #6)) |
| 8 | Search (((((((((((remineralization) OR demineralization) OR remineralisation) OR demineralisation) OR texture) OR hard*) OR leathery) OR soft*) OR RCI) OR root caries index) OR dmf) |
| 9 | Search ((#7 and #8)) |
| Embase | |
| 1 | ((FT=root OR FT=dentin* ) OR FT=tooth ) OR FT=teeth |
| 2 | FT=caries OR FT=carious |
| 3 | 1 AND 2 |
| 4 | (FT=clincial* OR FT=adult ) OR FT=elderly |
| 5 | 3 AND 4 |
| 6 | ((FT=demineralization OR FT=demineralisation ) OR FT=remineralization ) OR FT=remineralisation |
| 7 | ((FT=texture OR FT=hard* ) OR FT=leathery ) OR FT=soft |
| 8 | (FT=RCI OR FT=root caries index ) OR FT=dmf |
| 9 | 6 OR 1 OR 8 |
| 10 | 5 AND 9 |
Study Selection
We included nonblinded and blinded (double-blinded), randomized and nonrandomized, controlled, and prospective studies, which had to fulfill certain inclusion criteria:
Participants: humans who retained a minimum of 1 natural tooth with exposed root surfaces with or without RCLs at the beginning completing the last exam of the study.
Intervention: preventive dental regimes (e.g., oral health instruction) and/or 1 or more chemical agents applied on 1 or more occasion by a dental professional (e.g., dentist, dental nurse) or self-applied by the patient.
Control: negative (placebo treatment), positive (other intervention; e.g., Duraphat varnish), or standard therapy.
Outcome: clinical or radiographic visible changes of active or inactive root caries. Visual-tactile criteria for active and inactive root caries were not classified in accordance to a certain score, since studies used different scoring systems (e.g., NIDR guideline, Pitts Diagnostic Criteria, definitions of Nyvad and Fejerskov 1986) or evaluation was based on other scoring systems. If possible, incremental change was defined as a surface being scored sound at baseline developing to (active) root caries, filled or missing surface, or a surface with (active) root caries at baseline developing to a filled or missing surface at follow-up. Since tooth loss might have been unrelated to root caries, missing surfaces were removed from data if information on missing teeth/surfaces was provided separately. Inactivation was defined as surfaces with active root caries (e.g., soft surface texture) at baseline that were identified as inactive caries (e.g., hard surface texture) or sound at follow-up.
Data Extraction
For longitudinal studies and clinical trials presented in different journals, only the most recent report of the study was used. Unpublished data were not sought from authors or obtained from other sources. Extracted data included:
study type and setting (if not given, university setting was assumed),
inclusion criteria and outcome definitions,
patients (age) and teeth (dentition),
mode of application (varnish, dentifrice, mouth rinse),
intervention program (operator applied or self-applied; supervised or unsupervised),
interventions (pharmaceutical agent, type of control group),
clinical parameters (continuous data—DMFRS/T [decayed, missing, filled root surfaces/teeth], root caries index [RCI]; dichotomous data—surface texture; both kinds of data as primary or secondary outcomes; if possible, relative data were recalculated to absolute numbers),
dropouts and follow-up (maximum follow-up over all groups was used), and
methodological issues (e.g., funding source for risk of bias assessment).
Data Synthesis and Grading
Data were tested for normal distribution (Shapiro-Wilk) and descriptively analyzed accordingly. The primary measures of effect between treatment and control groups were the mean differences (MDs) for studies based on the same units and standardized MDs for studies based on the same construct but different scales. Changes were calculated for the following outcomes: DMFRS/DFRS and RCI. Dichotomous outcome data (e.g., surface texture) were analyzed by calculating risk ratios (RRs) and 95% confidence intervals (95% CIs). Again, a random effects model was used to calculate a pooled estimate of effect (Mantel-Haenszel chi-square statistic; Mantel 1963). Heterogeneity was assessed via I 2 (Higgins and Thompson 2002). Risk of bias assessment was performed according to guidelines outlined by the Cochrane Collaboration (Higgins et al. 2011). Grading of evidence was performed according to the GRADE network levels, based on Grade Profiler 3.6 (Guyatt et al. 2008). Publication bias was assessed by funnel plots (Egger et al. 1997).
Results
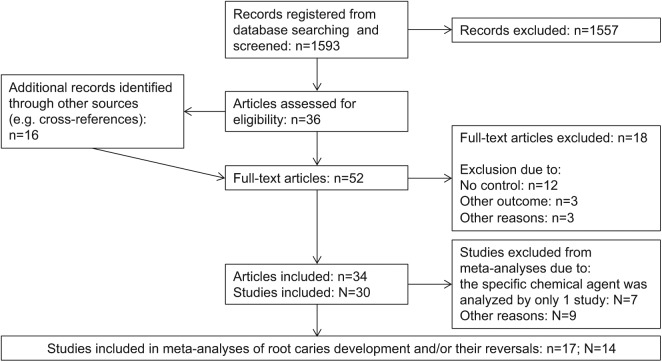
In sum, 1,593 articles were identified by screening electronic databases. Thirty-six articles were assessed for eligibility, and 16 were identified by other sources (e.g., cross-references). A total of 52 articles were screened full-text; 18 articles were excluded (Figure 1, Appendix Table 1). Eventually, 34 articles were included reporting 30 trials with 10,136 patients who were 20 to 101 y old and analyzing 28 chemical agents (Table 2, Appendix Tables 2 and 3). The median (25th/75th percentiles) follow-up time was 15 (12/24) mo. Eleven studies investigated dentifrices (Jensen and Kohout 1988; Banoczy and Nemes 1991; Baysan et al. 2001; Paraskevas et al. 2004; Papas et al. 2007; Papas et al. 2008; Vered et al. 2009; Ekstrand et al. 2013; Hu et al. 2013; Souza et al. 2013; Srinivasan et al. 2013), 10 rinses (Ripa et al. 1987; Banoczy and Nemes 1991; Ravald and Birkhed 1992; Wallace et al. 1993; Fure et al. 1998; Powell et al. 1999; Paraskevas et al. 2004; Wyatt and MacEntee 2004; Petersson et al. 2007; Wyatt et al. 2007), 8 varnishes (Schaeken et al. 1991; Ravald and Birkhed 1992; Powell et al. 1999; Banting et al. 2000; Baca et al. 2009; Fure and Lingstrom 2009; Tan et al. 2010; Zhang et al. 2013), 3 (fluoride) solutions (Fure and Lingstrom 2009; Tan et al. 2010; Zhang et al. 2013), 3 gels (Ravald and Birkhed 1992; DePaola 1993; Wallace et al. 1993), 2 ozone applications (Holmes 2003; Baysan and Lynch 2007), and 1 preventive dental regimes (Mojon et al. 1998). Eleven studies investigated both initiation of RCLs and the change of RCLs, 11 analyzed the change of RCLs, and 8 studied initiation of RCLs compared with baseline. The initiation of RCLs and their inactivation were described most often on the basis of surface texture (13 studies: Schaeken et al. 1991; Mojon et al. 1998; Baysan et al. 2001; Holmes 2003; Baysan and Lynch 2007; Papas et al. 2007; Petersson et al. 2007; Fure and Lingstrom 2009; Petersson et al. 2011; Ekstrand et al. 2013; Hu et al. 2013; Souza et al. 2013; Srinivasan et al. 2013), DFMRS/DFRS (12 studies: Ripa et al. 1987; Jensen and Kohout 1988; Schaeken et al. 1991; Ravald and Birkhed 1992; DePaola 1993; Wallace et al. 1993; Fure et al. 1998; Powell et al. 1999; Wyatt and MacEntee 2004; Baca et al. 2009; Tan et al. 2010; Zhang et al. 2013), ECM (electrical caries monitor; 5 studies: Baysan et al. 2001; Baysan and Lynch 2007; Petersson et al. 2007; Petersson et al. 2011; Hu et al. 2013), or RCI (4 studies: Banoczy and Nemes 1991; Wyatt and MacEntee 2004; Baca et al. 2009; Vered et al. 2009); only 8 studies used more than 1 assessment to describe RCLs. A detailed summary of included studies can be found in Appendix Tables 2 and 3.
Figure 1.
Study flow.
Table 2.
Chemical Agents and Their Product Names.
| Brand | Active Ingredients | Study |
|---|---|---|
| Dentifrice | ||
| Colgate Total Plus Whitening | 0.243% NaF + 0.3% triclosan + 2.0% copolymer | Papas et al. 2007; Vered et al. 2009 |
| Enamelon | 1,100 ppm F- as NaF + 1% CaSO4 + 1.1% NH4H2PO4 | Papas et al. 2008 |
| Meridol | 1,100 ppm F- as AmF/SnF2 | Banoczy and Nemes 1991; Paraskevas et al. 2004 |
| NaF (experimental, P&G) | 1,100 ppm F- as NaF | Jensen and Kohout 1988 |
| Prevident 5,000/Duraphat 5,000 | 5,000 ppm F- as NaF | Baysan et al. 2001; Ekstrand et al. 2013; Srinivasan et al. 2013 |
| SnF2 (experimental, P&G) | 0.0454% SnF2 | Papas et al. 2007 |
| 1,5% arginine plus 1,450 ppm F- (SMTP) (experimental, Colgate) | 1.5% arginine plus 1,450 ppm F- (SMTP) | Hu et al. 2013; Souza et al. 2013 |
| Gel | ||
| Luride | 1.2% F- as APF (acidulated phosphate fluoride) | Wallace et al. 1993 |
| SnF2 gel (experimental, Apoteksbolaget AB) | 0.4% SnF2 | Ravald and Birkhed 1992 |
| Prevident Plus Gel + Prevident Brush-on Gel | 12,000 ppm F- as NaF + 5,000 ppm F- as NaF | DePaola 1993 |
| Mouth rinse | ||
| ACT | 225 ppm F- as NaF | Wallace et al. 1993 |
| CHX rinse (experimental, Medisca Pharmaceutique Inc.) | 0.12% CHX | Wyatt and MacEntee 2004 |
| Dentan | 225 ppm F- as NaF | Ravald and Birkhed 1992 |
| Dentan Mint | 225 ppm F- as NaF | Fure et al. 1998 |
| Elmex sensitive rinse | 225 ppm F- as AmF/KF | Petersson et al. 2007 |
| Fluorigard Anti-cavity Dental Rinse | 225 ppm F- as NaF | Ripa et al. 1987 |
| Fluorinse | 900 ppm F- as NaF | Wyatt and MacEntee 2004 |
| Meridol | 225 ppm F- as AmF/SnF2 | Banoczy and Nemes 1991; Paraskevas et al. 2004 |
| Periogard/Peridex | 0.12% CHX | Powell et al. 1999; Wyatt et al. 2007 |
| Solution/varnish | ||
| Saforide | 38% SDF (silver diamine fluoride) | Tan et al. 2010; Zhang et al. 2013 |
| SnF2 solution (experimental, n/a) | 8% SnF2 | Fure and Lingstrom 2009 |
| Varnish | ||
| Carisolv | 0.475 NaOCl/2.23% NaF | Fure and Lingstrom 2009 |
| Cervitec | 1 % CHX + 1% thymol | Baca et al. 2009; Tan et al. 2010 |
| CHX varnish (experimental, n/a) | 10 % CHX | Banting et al. 2000 |
| EC 40 | 40% CHX | Schaeken et al. 1991 |
| Duraflor | 22,600 ppm F- as NaF | Powell et al. 1999 |
| Duraphat | 22,600 ppm F- as NaF | Schaeken et al. 1991; Ravald and Birkhed 1992; Fure and Lingstrom 2009; Tan et al. 2010 |
| Ozone | ||
| HealOzone | Ozone | Holmes 2003; Baysan and Lynch 2007 |
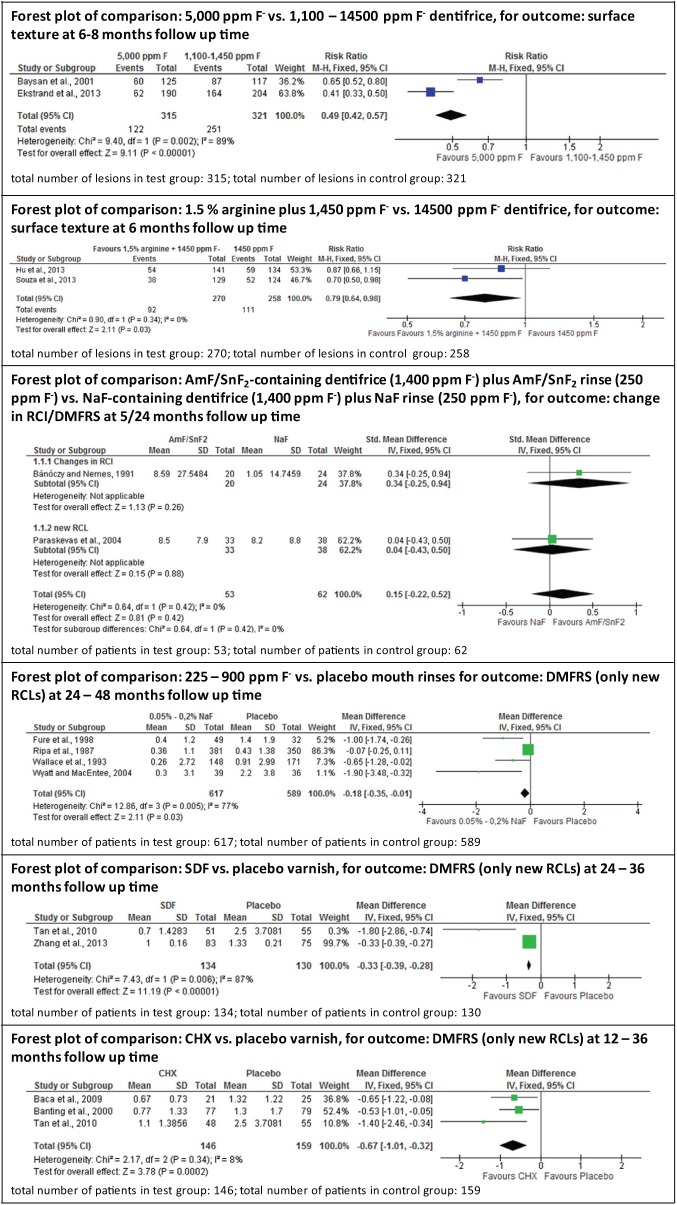
Although analyses showed that different chemical agents may be capable of reducing the initiation of RCLs, meta-analyses were performed only for chemical agents with similar interventions and outcome measures investigated in more than 1 study. Analyses could not be performed for varnish containing 22,500 ppm F- (Duraphat), since these studies used Duraphat as a control group without having a second (negative) control group (Ravald and Birkhed 1992; Fure and Lingstrom 2009) or the results were presented according to different indices (DMFRS or texture) and did not report all information required for recalculation (Schaeken et al. 1991; Tan et al. 2010). For CHX mouth rinses (Powell et al. 1999; Wyatt and MacEntee 2004; Wyatt et al. 2007) and ozone treatment (Holmes 2003; Baysan and Lynch 2007), recalculation was not possible owing to insufficient data presentation. Thus, meta-analyses were performed only for dentifrice containing 5,000 ppm F- or 1.5% arginine plus 1,450 ppm F-, rinse containing 0.05% to 0.2% NaF (225 to 900 ppm F-), varnish containing SDF or CHX and combined use of dentifrice (1,500 ppm F-), and a rinse containing AmF/SnF2 (250 ppm F-). This strategy allowed meta-analyses of 17 articles, reporting 14 trials with 4,270 patients, of whom 75.4% completed the studies (Fig. 2).
Figure 2.
Quantitative meta-analyses for different chemical agents. DMFRS/DFRS (decayed, missing, filled root surfaces) or new root caries lesions (RCLs) were used to calculate mean differences (MDs) and 95% confidence intervals (95% CIs) for studies using the same units and standardized mean differences (SMDs) and 95% CIs for studies using the same construct but different scales. Surface texture scores were used to calculate risk ratio (RR) and 95% CI. Forest plots, heterogeneity parameter (I2) as well as overall statistics (Z, P) are given.
Patients using dentifrice containing 5,000 ppm F- (RR = 0.49; 95% CI = 0.42, 0.57; Baysan et al. 2001; Ekstrand et al. 2013) or dentifrices containing 1.5% arginine plus 1,450 ppm F- (RR = 0.79; 95% CI = 0.64, 0.98; Hu et al. 2013; Souza et al. 2013) showed significantly higher numbers of RCLs being inactivated than patients using dentifrice containing 1,100 to 1,450 ppm F-. Self-applied AmF/SnF2-containing dentifrice (1,400 ppm F-) plus AmF/SnF2-containing rinse (250 ppm F-) decreased the initiation of RCLs when compared with a NaF-containing dentifrice (1,400 ppm F-) plus NaF rinse (250 ppm F-; standardized MD = 0.15; 95% CI = −0.22, 0.52; Banoczy and Nemes 1991; Paraskevas et al. 2004). Patients rinsing with a fluoride mouth rinse (225 to 900 ppm F-) revealed a significantly reduced DMFRS/DFRS (MD = −0.18; 95% CI = −0.35, −0.01) compared with those rinsing with a placebo rinse (Ripa et al. 1987; Wallace et al. 1993; Fure et al. 1998; Wyatt and MacEntee 2004). Compared with a respective placebo varnish, professionally applied 1% or 10% CHX varnish (MD = −0.67; 95% CI = −1.01, −0.32; Banting et al. 2000; Baca et al. 2009; Tan et al. 2010) as well as professionally applied SDF varnish (MD = −0.33; 95% CI = −0.39, −0.28; Tan et al. 2010; Zhang et al. 2013) reduced initiation of RCLs significantly. Indirect comparisons were not analyzed.
Although no meta-analysis could be performed, fluoride varnish (22,500 ppm F-) applied every 3 mo seems to reduce the initiation of RCL more efficaciously (Schaeken et al. 1991; Tan et al. 2010) and inactivate significantly more RCLs (Schaeken et al. 1991) when compared with placebo control or standard oral hygiene. Moreover, a higher number of RCLs may be inactivated when additionally treated with ozone, as compared with no treatment. For CHX mouth rinses, all studies reported no significant difference in RCL outcomes when compared to no treatment or placebo treatment.
Risk of bias was assessed for all 30 studies (Table 3). Twenty-nine studies were randomized controlled trials; 1 study was a nonrandomized but controlled trial (Mojon et al. 1998). Risk of bias was very low for 5 studies (Baysan et al. 2001; Wyatt and MacEntee 2004; Wyatt et al. 2007; Tan et al. 2010; Petersson et al. 2011). Adverse events possibly related to one of the used products were only reported in 2 studies (Banting et al. 2000; Papas et al. 2007). Eleven studies were not sponsored by the manufactures of the tested products. Grading of evidence for meta-analyses showed a high level of evidence for dentifrices containing 5,000 ppm F-; a low level for AmF/SnF2 fluoride and fluoride mouth rinse; and a very low level for SDF solution, CHX varnish, and 1.5% arginine plus 1,450 ppm F- containing dentifrice (Appendix Table 4).
Table 3.
Risk of Bias of Included Studies.
| RSS | AC | BPP | BOA | IOD | SR | SM | COI | |
|---|---|---|---|---|---|---|---|---|
| Included in meta-analyses | ||||||||
| Baysan et al. 2001 | + | + | + | + | + | + | − | ? |
| Ekstrand et al. 2013 | − | − | + | ? | ? | + | − | − |
| Hu et al. 2013 | ? | ? | + | + | + | + | − | ? |
| Souza et al. 2013 | ? | ? | + | ? | + | + | − | ? |
| Banocy and Nemes 1991 | ? | ? | + | + | ? | + | ? | ? |
| Paraskevas et al. 2004 | ? | + | + | + | + | + | − | ? |
| Fure et al. 1998 | ? | ? | n/a | ? | + | + | − | ? |
| Ripa et al. 1987 | ? | ? | + | + | + | + | + | ? |
| Wallace et al. 1993 | + | + | n/a | + | + | ? | − | ? |
| Wyatt and MacEntee 2004 | + | ? | + | + | + | + | + | ? |
| Baca et al. 2009 | + | ? | + | + | ? | + | − | + |
| Banting et al. 2000 | ? | ? | + | + | + | + | ? | ? |
| Tan et al. 2010 | − | + | + | + | + | + | + | ? |
| Zhang et al. 2013 | + | ? | n/a | + | + | − | + | ? |
| Excluded from meta-analyses | ||||||||
| Baysan and Lynch 2007 | ? | − | n/a | + | + | + | + | ? |
| DePaola 1993 | ? | ? | ? | ? | + | + | ? | ? |
| Fure and Lingstrom 2009 | + | + | − | + | + | + | + | ? |
| Holmes 2003 | ? | ? | + | + | + | + | + | ? |
| Jensen and Kohout 1988 | + | ? | + | + | + | + | − | ? |
| Mojon et al. 1998 | − | − | n/a | − | ? | + | − | ? |
| Papas et al. 2007 | + | + | + | + | + | − | − | − |
| Papas et al. 2008 | + | + | + | + | − | + | − | ? |
| Petersson et al. 2007 | ? | ? | + | + | + | + | − | ? |
| Petersson et al. 2011 | + | + | + | + | + | + | ? | + |
| Powell et al. 1999 | + | ? | n/a | + | + | + | + | ? |
| Ravald and Birkhed 1992 | + | ? | n/a | + | ? | + | + | ? |
| Schaeken et al. 1991 | − | − | − | + | + | + | + | ? |
| Srinivasan et al. 2013 | + | + | − | + | + | + | − | − |
| Vered et al. 2009 | ? | ? | + | + | ? | + | − | ? |
| Wyatt et al. 2007 | + | + | + | + | + | + | + | ? |
−, high; +, low; ?, unknown; n/a, blinding not possible due to different treatments.
AC, allocation concealment; BOA, blinding of outcome assessment; BPP, blinding of participants and personnel; COI, conflict of interest; IOD, incomplete outcome data; RSS, random sequence generation; SM, sponsoring by manufacturer; SR, selective reporting.
Discussion
The present review investigated primary and secondary prevention of RCLs for different chemical agents. A variety of studies on 28 agents was extracted from the literature with the aim of investigating the initiation of RCLs and/or their inactivation. This reflects that, obviously, no gold standard therapy for noninvasive treatment of RCLs has been agreed on yet. The highest number of studies was found for CHX and fluoride varnish as well as for NaF rinses, with all 3 being analyzed in only 4 studies each. Several authors observed improved and intensified oral hygiene for all patients by participating, even in control groups (Banoczy and Nemes 1991; Ravald and Birkhed 1992; DePaola 1993; Baysan et al. 2001; Papas et al. 2007; Hu et al. 2013; Souza et al. 2013). These findings could be considered to be the study effect (Banoczy and Nemes 1991), underlining that regular dental checkups to remotivate patients to perform oral hygiene properly seem to be first choice to manage RCLs (Nyvad and Fejerskov 1986).
This systematic review of the literature identified different types of application and agents to reduce the initiation or to inactivate RCLs. Meta-analyses were carried out only where comparisons of agents were investigated in more than 1 study (6 comparisons):
Daily use of dentifrice containing 5,000 ppm F- seems to be more efficacious in reducing active RCLs (193 of 315 lesions inactivated) than dentifrice containing 1,100 to 1,450 ppm F- (70 of 321 lesions inactivated). This is in line with a previous review (Marinho et al. 2003) and several studies (Marks et al. 1994; Biesbrock et al. 2001; Stookey et al. 2004; Davies and Davies 2008) reporting a fluoride dose-response for enamel caries lesions. Thus, especially for elderly people with exposed root surfaces, high-dose fluoride toothpaste inactivating 51% more RCLs compared with standard fluoride toothpaste seems recommendable.
Daily use of dentifrice containing 1.5% arginine plus 1,450 ppm F- inactivates 21% more RCLs (178 of 270 lesions inactivated) than dentifrice containing 1,450 ppm F- (147 of 258 lesions inactivated). This is consistent with studies (no meta-analysis available) on enamel caries lesions in 7- to 14-y-old patients (Srisilapanan et al. 2013; Yin, Hu, Fan, et al. 2013; Yin, Hu, Li, et al. 2013). Nonetheless, evidence level was graded as very low, and both studies included in this meta-analysis showed a high risk of bias, indicating that further high-qualitative clinical studies are warranted.
Daily use of AmF/SnF2-containing dentifrice (1,400 ppm F-) plus AmF/SnF2-containing rinse (250 ppm F-) does not seem to prevent root caries more efficaciously than NaF-containing dentifrice (1,400 ppm F-) plus NaF-containing rinse (250 ppm F-). This corroborates findings for enamel caries lesions around brackets of orthodontic patients (Ogaard et al. 2006). For this agent, no systematic review on enamel caries lesions is available. For root caries studies, randomization procedures and allocation concealment were not thoroughly explained and both studies used different outcomes.
This review found a trend (small effect [Cohen 1988]; MD = −0.18) toward a lower number of new RCLs for additional daily use of 225 to 900 ppm F- as compared with placebo rinses. Concurrently, one of the studies (Ripa et al. 1987) observed no significant differences in 3-y coronal DMFS increments. In contrast, a previous review revealed a significantly lower coronal caries incidence for additional fluoride rinse, as compared to placebo or nonrinsing (Marinho et al. 2003). Since the findings for coronal caries showed a rather good efficacy, it seems plausible to recommend the daily use of NaF rinses to reduce not only the initiation of coronal caries lesions but also the initiation of RCLs.
Professionally applied CHX (1% or 10%) compared with placebo varnish reduced the initiation of RCLs (moderate effect; MD = −0.67). With respect to coronal caries in children and young adults, it has been shown that CHX varnish revealed a significant caries-inhibiting effect when it is applied every 3 to 4 mo (Zhang et al. 2006). This review included 10 studies analyzing permanent molars, premolars, or all teeth. A narrative review of 22 studies observed inconclusive evidence for an anticaries effect of CHX-containing varnishes for different locations (young permanent dentition, proximal sites, fissures, white spot lesions, root caries; Twetman 2004). An additional caries-preventive effect of CHX varnishes could be revealed only for fissure caries when compared with no treatment in children with low fluoride exposure. In light of these reviews, the present meta-analysis underlines the possible (root) caries-inhibiting effect of CHX varnish.
Professionally applied SDF varnish may reduce the number of developing RCLs when compared with a placebo varnish (moderate effect; MD= −0.33). Application frequency varied from quarterly (Tan et al. 2010) to annually (Zhang et al. 2013). Earlier studies on SDF showed a significantly higher number of arrested caries lesions when compared to placebo or no treatment (Chu et al. 2002; Llodra et al. 2005; Yee et al. 2009; Zhi et al. 2012). Although these studies investigated the efficacy of SDF in arresting occlusal cavitated dentine caries in primary teeth up to 36 mo, only 1 study removed the superficial carious enamel. The lack of economic resources might be the reason why caries was not removed at the study site; nonetheless, the design of the study remains questionable. It is, however, interesting to note that SDF may reduce the initiation of RCLs.
The analyzed studies used several slightly different criteria to detect RCLs and/or to assess the activity (or inactivity) of RCLs, which may lead to certain biases. The most common factors were hardness, cavitation, color, and dimension of the lesions; sometimes, the distance of the lesion to the gingival margin was analyzed as well. The definition of these criteria and the presentation of the results varied widely within randomized controlled trials—with some reporting relative indices (ΔDMRS/T, changes in surface textures, and RCI) and some reporting absolute indices (DMFRS/T, surface texture). Extracting all information to recalculate data for the present meta-analysis was not possible for all studies, since not all findings were either assessed or reported. Therefore, no meta-analysis could be performed for fluoride varnish, CHX mouth rinse, and ozone application. Two studies—one analyzing both CHX (EC 40) and fluoride varnish (Duraphat; Schaeken et al. 1991) the other analyzing highly concentrated fluoride dentifrice (Duraphat 5000; Srinivasan et al. 2013)—had to be excluded from quantitative analyses. The gained evidence is additionally limited by the focus of the studies and the follow-up times. Some of the included studies observed the initiation and inactivation of RCLs but primarily investigated microbiology of residual (root) caries (Paraskevas et al. 2004; Papas et al. 2007). Follow-up times were rather short (median, 15 mo). Only 12 studies reported outcomes over 24 mo or longer. However, all these factors were reflected in risk-of-bias analysis and evidence grading.
In conclusion, this systematic review sorted out different chemical agents for professional use or home use for primary and secondary prevention of RCLs being studied at a higher level of evidence. Based on meta-analysis, dentifrice containing 5,000 ppm F- and professionally applied CHX or SDF varnish may inactivate existing and/or reduce the initiation of RCLs. However, results should be interpreted with caution, due to the low numbers of clinical trials for each agent, the high risk of bias within studies, and the limiting grade of evidence.
Author Contributions
R.J. Wierichs, H. Meyer-Lueckel, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Footnotes
This study was funded by the authors and their institution.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
References
- Baca P, Clavero J, Baca AP, Gonzalez-Rodriguez MP, Bravo M, Valderrama MJ. 2009. Effect of chlorhexidine-thymol varnish on root caries in a geriatric population: a randomized double-blind clinical trial. J Dent. 37(9):679–685. [DOI] [PubMed] [Google Scholar]
- Banoczy J, Nemes J. 1991. Effect of amine fluoride (AmF)/stannous fluoride (SnF2) toothpaste and mouthwashes on dental plaque accumulation, gingivitis and root-surface caries. Proc Finn Dent Soc. 87(4):555–559. [PubMed] [Google Scholar]
- Banting DW, Papas A, Clark DC, Proskin HM, Schultz M, Perry R. 2000. The effectiveness of 10% chlorhexidine varnish treatment on dental caries incidence in adults with dry mouth. Gerodontology. 17(2):67–76. [DOI] [PubMed] [Google Scholar]
- Baysan A, Lynch E. 2007. Clinical reversal of root caries using ozone: 6-month results. Am J Dent. 20(4):203–208. [PubMed] [Google Scholar]
- Baysan A, Lynch E, Ellwood R, Davies R, Petersson L, Borsboom P. 2001. Reversal of primary root caries using dentifrices containing 5,000 and 1,100 ppm fluoride. Caries Res. 35(1):41–46. [DOI] [PubMed] [Google Scholar]
- Biesbrock AR, Gerlach RW, Bollmer BW, Faller RV, Jacobs SA, Bartizek RD. 2001. Relative anti-caries efficacy of 1100, 1700, 2200, and 2800 ppm fluoride ion in a sodium fluoride dentifrice over 1 year. Community Dent Oral Epidemiol. 29(5):382–389. [DOI] [PubMed] [Google Scholar]
- Burt BA, Ismail AI, Eklund SA. 1986. Root caries in an optimally fluoridated and a high-fluoride community. J Dent Res. 65(9):1154–1158. [DOI] [PubMed] [Google Scholar]
- Chu CH, Lo EC, Lin HC. 2002. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 81(11):767–770. [DOI] [PubMed] [Google Scholar]
- Cohen J. 1988. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates. [Google Scholar]
- Davies RM, Davies GM. 2008. High fluoride toothpastes: their potential role in a caries prevention programme. Dent Update. 35(5):320–323. [DOI] [PubMed] [Google Scholar]
- DePaola PF. 1993. Caries in our aging population: what are we learning? In: Bowden GH, Tabak LA, editors. Cariology for the nineties. Rochester (NY): University of Rochester Press; p. 25–35. [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. 1997. Bias in meta-analysis detected by a simple, graphical test. BMJ. 315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekstrand KR, Poulsen JE, Hede B, Twetman S, Qvist V, Ellwood RP. 2013. A randomized clinical trial of the anti-caries efficacy of 5,000 compared to 1,450 ppm fluoridated toothpaste on root caries lesions in elderly disabled nursing home residents. Caries Res. 47(5):391–398. [DOI] [PubMed] [Google Scholar]
- Ellwood RP, Goma J, Pretty IA. 2012. Caries clinical trial methods for the assessment of oral care products in the 21st century. Adv Dent Res. 24(2):32–35. [DOI] [PubMed] [Google Scholar]
- Ettinger RL. 1999. Epidemiology of dental caries: a broad review. Dent Clin North Am. 43(4):679–694. [PubMed] [Google Scholar]
- Fure S, Gahnberg L, Birkhed D. 1998. A comparison of four home-care fluoride programs on the caries incidence in the elderly. Gerodontology. 15(2):51–60. [DOI] [PubMed] [Google Scholar]
- Fure S, Lingstrom P. 2009. Evaluation of different fluoride treatments of initial root carious lesions in vivo. Oral Health Prev Dent. 7(2):147–154. [PubMed] [Google Scholar]
- Gluzman R, Katz RV, Frey BJ, McGowan R. 2013. Prevention of root caries: a literature review of primary and secondary preventive agents. Spec Care Dentist. 33(3):133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin SO, Griffin PM, Swann JL, Zlobin N. 2004. Estimating rates of new root caries in older adults. J Dent Res. 83(8):634–638. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ; GRADE Working Group. 2008. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 336(7650):924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Green SG. editors. 2011. Cochrane handbook for systematic reviews of interventions: version 5.10 [updated March 2011]. Cochrane Collaboration; http://handbook.cochrane.org/ [Google Scholar]
- Higgins JP, Thompson SG. 2002. Quantifying heterogeneity in a meta-analysis. Stat Med. 21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- Holmes J. 2003. Clinical reversal of root caries using ozone, double-blind, randomised, controlled 18-month trial. Gerodontology. 20(2):106–114. [DOI] [PubMed] [Google Scholar]
- Hu DY, Yin W, Li X, Feng Y, Zhang YP, Cummins D, Mateo LR, Ellwood RP. 2013. A clinical investigation of the efficacy of a dentifrice containing 1.5% arginine and 1450 ppm fluoride, as sodium monofluorophosphate in a calcium base, on primary root caries. J Clin Dent. 24:A23–A31. [PubMed] [Google Scholar]
- Jensen ME, Kohout F. 1988. The effect of a fluoridated dentifrice on root and coronal caries in an older adult population. J Am Dent Assoc. 117(7):829–832. [DOI] [PubMed] [Google Scholar]
- Leake JL. 2001. Clinical decision-making for caries management in root surfaces. J Dent Educ. 65(10):1147–1153. [PubMed] [Google Scholar]
- Llodra JC, Rodriguez A, Ferrer B, Menardia V, Ramos T, Morato M. 2005. Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res. 84(8):721–724. [DOI] [PubMed] [Google Scholar]
- Mantel N. 1963. Chi-square tests with one degree of freedom, extensions of the Mantel-Haenszel procedure. J Am Stat Assoc. 58(303):690–700. [Google Scholar]
- Marinho VC, Higgins JP, Logan S, Sheiham A. 2003. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 4:CD002782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks RG, Conti AJ, Moorhead JE, Cancro L, D’Agostino RB. 1994. Results from a three-year caries clinical trial comparing NaF and SMFP fluoride formulations. Int Dent J. 44(3 Suppl 1):275–285. [PubMed] [Google Scholar]
- Michaelis W, Schiffner U. 2006. The Fourth German Oral Health Study (DMS IV). Köln: Institute of German Dentists, Deutscher Zahnärzte Verlag. [Google Scholar]
- Mojon P, Rentsch A, Budtz-Jorgensen E, Baehni PC. 1998. Effects of an oral health program on selected clinical parameters and salivary bacteria in a long-term care facility. Eur J Oral Sci. 106(4):827–834. [DOI] [PubMed] [Google Scholar]
- Nyvad B, Fejerskov O. 1986. Active root surface caries converted into inactive caries as a response to oral hygiene. Scand J Dent Res. 94(3):281–284. [DOI] [PubMed] [Google Scholar]
- Ogaard B, Alm AA, Larsson E, Adolfsson U. 2006. A prospective, randomized clinical study on the effects of an amine fluoride/stannous fluoride toothpaste/mouthrinse on plaque, gingivitis and initial caries lesion development in orthodontic patients. Eur J Orthod. 28(1):8–12. [DOI] [PubMed] [Google Scholar]
- Papas A, He T, Martuscelli G, Singh M, Bartizek RD, Biesbrock AR. 2007. Comparative efficacy of stabilized stannous fluoride/sodium hexametaphosphate dentifrice and sodium fluoride/triclosan/copolymer dentifrice for the prevention of periodontitis in xerostomic patients: a 2-year randomized clinical trial. J Periodontol. 78(8):1505–1014. [DOI] [PubMed] [Google Scholar]
- Papas A, Russell D, Singh M, Kent R, Triol C, Winston A. 2008. Caries clinical trial of a remineralising toothpaste in radiation patients. Gerodontology. 25(2):76–88. [DOI] [PubMed] [Google Scholar]
- Paraskevas S, Danser MM, Timmerman MF, van der Velden U, van der Weijden GA. 2004. Amine fluoride/stannous fluoride and incidence of root caries in periodontal maintenance patients: a 2 year evaluation. J Clin Periodontol. 31(11):965–971. [DOI] [PubMed] [Google Scholar]
- Peters MC. 2010. Strategies for noninvasive demineralized tissue repair. Dent Clin North Am. 54(3):507–525. [DOI] [PubMed] [Google Scholar]
- Petersson LG, Hakestam U, Baigi A, Lynch E. 2007. Remineralization of primary root caries lesions using an amine fluoride rinse and dentifrice twice a day. Am J Dent. 20(2):93–96. [PubMed] [Google Scholar]
- Petersson LG, Magnusson K, Hakestam U, Baigi A, Twetman S. 2011. Reversal of primary root caries lesions after daily intake of milk supplemented with fluoride and probiotic lactobacilli in older adults. Acta Odontol Scand. 69(6):321–327. [DOI] [PubMed] [Google Scholar]
- Powell LV, Persson RE, Kiyak HA, Hujoel PP. 1999. Caries prevention in a community-dwelling older population. Caries Res. 33(5):333–339. [DOI] [PubMed] [Google Scholar]
- Ravald N, Birkhed D. 1992. Prediction of root caries in periodontally treated patients maintained with different fluoride programmes. Caries Res. 26(6):450–458. [DOI] [PubMed] [Google Scholar]
- Ripa LW, Leske GS, Forte F, Varma A. 1987. Effect of a 0.05% neutral NaF mouthrinse on coronal and root caries of adults. Gerodontology. 6(4):131–136. [DOI] [PubMed] [Google Scholar]
- Rodrigues JA, Lussi A, Seemann R, Neuhaus KW. 2011. Prevention of crown and root caries in adults. Periodontol. 2000 55(1):231–249. [DOI] [PubMed] [Google Scholar]
- Schaeken MJ, Keltjens HM, Van Der Hoeven JS. 1991. Effects of fluoride and chlorhexidine on the microflora of dental root surfaces and progression of root-surface caries. J Dent Res. 70(2):150–153. [DOI] [PubMed] [Google Scholar]
- Souza ML, Cury JA, Tenuta LM, Zhang YP, Mateo LR, Cummins D, Ellwood RP. 2013. Comparing the efficacy of a dentifrice containing 1.5% arginine and 1450 ppm fluoride to a dentifrice containing 1450 ppm fluoride alone in the management of primary root caries. J Dent. 41(Suppl 2):S35–S41. [DOI] [PubMed] [Google Scholar]
- Srinivasan M, Schimmel M, Riesen M, Ilgner A, Wicht MJ, Warncke M, Ellwood RP, Nitschke I, Müller F, Noack MJ. 2013. High-fluoride toothpaste: a multicenter randomized controlled trial in adults. Community Dent Oral Epidemiol. 42(4):333–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srisilapanan P, Korwanich N, Yin W, Chuensuwonkul C, Mateo LR, Zhang YP, Cummins D, Ellwood RP. 2013. Comparison of the efficacy of a dentifrice containing 1.5% arginine and 1450 ppm fluoride to a dentifrice containing 1450 ppm fluoride alone in the management of early coronal caries as assessed using quantitative light-induced fluorescence. J Dent. 41(Suppl 2):S29–S34. [DOI] [PubMed] [Google Scholar]
- Stookey GK, Mau MS, Isaacs RL, Gonzalez-Gierbolini C, Bartizek RD, Biesbrock AR. 2004. The relative anticaries effectiveness of three fluoride-containing dentifrices in Puerto Rico. Caries Res. 38(6):542–550. [DOI] [PubMed] [Google Scholar]
- Tan HP, Lo EC, Dyson JE, Luo Y, Corbet EF. 2010. A randomized trial on root caries prevention in elders. J Dent Res. 89(10):1086–1090. [DOI] [PubMed] [Google Scholar]
- Twetman S. 2004. Antimicrobials in future caries control? A review with special reference to chlorhexidine treatment. Caries Res. 38(3):223–229. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. 2000. Oral health in america: a report of the surgeon general. Rockville (MD): US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; p. 308. [Google Scholar]
- Vered Y, Zini A, Mann J, DeVizio W, Stewart B, Zhang YP, Garcia L. 2009. Comparison of a dentifrice containing 0.243% sodium fluoride, 0.3% triclosan, and 2.0% copolymer in a silica base, and a dentifrice containing 0.243% sodium fluoride in a silica base: a three-year clinical trial of root caries and dental crowns among adults. J Clin Dent. 20(2):62–65. [PubMed] [Google Scholar]
- Wallace MC, Retief DH, Bradley EL. 1993. The 48-month increment of root caries in an urban population of older adults participating in a preventive dental program. J Public Health Dent. 53(3):133–137. [DOI] [PubMed] [Google Scholar]
- Walls AW, Meurman JH. 2012. Approaches to caries prevention and therapy in the elderly. Adv Dent Res. 24(2):36–40. [DOI] [PubMed] [Google Scholar]
- Wyatt CC, MacEntee MI. 2004. Caries management for institutionalized elders using fluoride and chlorhexidine mouthrinses. Community Dent Oral Epidemiol. 32(5):322–328. [DOI] [PubMed] [Google Scholar]
- Wyatt CC, Maupome G, Hujoel PP, MacEntee MI, Persson GR, Persson RE, Kiyak HA. 2007. Chlorhexidine and preservation of sound tooth structure in older adults: a placebo-controlled trial. Caries Res. 41(2):93–101. [DOI] [PubMed] [Google Scholar]
- Yee R, Holmgren C, Mulder J, Lama D, Walker D, van Palenstein Helderman W. 2009. Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res. 88(7):644–647. [DOI] [PubMed] [Google Scholar]
- Yin W, Hu DY, Fan X, Feng Y, Zhang YP, Cummins D, Mateo LR, Pretty IA, Ellwood RP. 2013. A clinical investigation using quantitative light-induced fluorescence (QLF) of the anticaries efficacy of a dentifrice containing 1.5% arginine and 1450 ppm fluoride as sodium monofluorophosphate. J Clin Dent. 24:A15–A22. [PubMed] [Google Scholar]
- Yin W, Hu DY, Li X, Fan X, Zhang YP, Pretty IA, Mateo LR, Cummins D, Ellwood RP. 2013. The anti-caries efficacy of a dentifrice containing 1.5% arginine and 1450 ppm fluoride as sodium monofluorophosphate assessed using quantitative light-induced fluorescence (QLF). J Dent. 41(Suppl 2):S22–S28. [DOI] [PubMed] [Google Scholar]
- Zhang Q, van Palenstein Helderman WH, van’t Hof MA, Truin GJ. 2006. Chlorhexidine varnish for preventing dental caries in children, adolescents and young adults: a systematic review. Eur J Oral Sci. 114(6):449–455. [DOI] [PubMed] [Google Scholar]
- Zhang W, McGrath C, Lo EC, Li JY. 2013. Silver diamine fluoride and education to prevent and arrest root caries among community-dwelling elders. Caries Res. 47(4):284–290. [DOI] [PubMed] [Google Scholar]
- Zhi QH, Lo EC, Lin HC. 2012. Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children. J Dent. 40(11):962–967. [DOI] [PubMed] [Google Scholar]