Abstract
Importance
High unemployment during the 2007-2009 Great Recession and eligibility expansions have increased the size and cost of Medicaid. To provide states with flexibility in administering the program while containing costs, the Deficit Reduction Act of 2005 (DRA) gave states the authority to impose cost-sharing strategies, including emergency department (ED) copayments for nonurgent visits. To our knowledge, there has been no previous longitudinal analysis of the effect of the DRA on health care utilization outcomes for Medicaid beneficiaries.
Objectives
To evaluate the effect of the DRA, which allowed states to enforce ED copayments for nonurgent visits, on ED utilization among Medicaid beneficiaries and to compare the effect among beneficiaries living in states that did and did not adopt ED copayments.
Design, Setting, and Participants
A difference-in-difference quasi-experimental approach was used to compare trends in ED use among Medicaid beneficiaries from January 2001 to December 2010. Eight states with ED copayments for nonurgent ED visits (copayment states) were compared with 10 states with zero ED copayments (control states). The study cohort was the population of individuals 19 to 64 years old enrolled in Medicaid for a full calendar year as collected by the Medical Expenditure Panel Survey, a nationally representative survey of noninstitutionalized US civilians. The cohort consisted of 3122 adult Medicaid recipients in copayment states and 7433 adult Medicaid recipients in control states.
Exposures
The main exposure was the copayment enforcement authority of the DRA. The study controlled for sex, age, race, marital status, income relative to the federal poverty level, educational level, and self-reported health status.
Main Outcomes and Measures
The primary outcome of this study was the change in the rate of ED utilization following the DRA. Additional outcomes included changes in the rate of outpatient medical provider visits and inpatient length of stay. Visits were not coded according to urgency, which prevented us from examining only nonurgent ED use.
Results
Estimates from a zero-inflated Poisson regression model detected no statistically significant change in annual ED admissions per Medicaid enrollee (change, 0.05; 95% CI, −0.05 to 0.16) in copayment states compared with control states following the DRA. There was also no change in the rate of outpatient medical provider visits (change, 0.02; 95% CI, −0.31 to 0.35) or in annual inpatient days (change, 0.13; 95% CI, −0.31 to 0.57) per Medicaid enrollee.
Conclusions and Relevance
Granting states permission to collect copayments for nonurgent visits under the DRA did not significantly change ED or outpatient medical provider use among Medicaid beneficiaries. This difference-in-difference quasi-experimental study found that granting states permission to collect copayments for nonurgent visits under the Deficit Reduction Act of 2005 did not significantly change ED or outpatient medical provider use among Medicaid beneficiaries.
Introduction
In recent years, Medicaid has faced the twin challenges of increasing enrollment and rising per-member costs. High unemployment during the 2007-2009 Great Recession, coupled with eligibility expansions authorized by the federal Deficit Reduction Act of 2005 (DRA) and the Patient Protection and Affordable Care Act (ACA), continues to expand the size and cost of Medicaid. Enrollment in Medicaid grew by 5.8% in 2008 and by 7.6% in 2009, while total Medicaid spending increased by 3.0% and 7.8%, respectively.1 According to the Centers for Medicare & Medicaid Services, Medicaid spending is projected to increase by 8.7% per year between 2011 and 2020, reflecting in part the ACA’s expansion of the program to a projected 13 million additional low-income adults.2
To offer states more flexibility in administering Medicaid programs and to contain costs, the DRA gave states discretion to institute sliding-scale premiums and copayments for Medicaid beneficiaries. In particular, cost sharing was permitted up to 5% of beneficiaries’ annual incomes.3 The use of cost sharing as a mechanism for changing health care utilization among low-income individuals is controversial. Previous research has demonstrated that low-income individuals who face higher cost sharing use fewer services in general, including those considered medically appropriate, and may deter Medicaid enrollment.4 Even small cost-sharing measures (eg, $3 copayments) have been demonstrated to place a large burden on those who have incomes low enough to qualify for Medicaid.5
The Emergency Medical Treatment and Labor Act of 1986 (EMTALA) ensured public access to emergent care regardless of ability to pay. However, between 1993 and 2003, emergency department (ED) visits grew by 26%, and the amount of uncompensated care delivered by nonfederal community hospitals grew between 1983 and 2004 from $6.1 billion to $40.7 billion.6 The DRA allowed states to collect payments from Medicaid beneficiaries as a condition of rendering services for nonurgent care, while ensuring continued access to emergent care through the EMTALA.
As a result of the DRA, some states implemented ED copayments for visits determined to be nonurgent after an initial triage assessment by a health care provider. The rationale for this policy is that, by mandating copayments for nonurgent ED use, Medicaid beneficiaries will decrease their reliance on the ED for primary care and instead obtain care from an outpatient medical provider. Research evaluating the use of services through 2006, the year after the DRA, found no significant decrease in the utilization of ED services in states that instituted copayments.7
While some states initiated copayments before 2006, states’ ability to enforce copayment policies under the DRA did not begin until 2006. Before 2006, states could request minimal copayments, but hospitals could not legally refuse to provide services if the beneficiary was unable to meet the copayment requirement. The DRA allowed states the enforcement authority to make treatment contingent on collecting payments. To our knowledge, there has been no previous longitudinal analysis of the effect of the DRA’s enforcement authority on health utilization outcomes for Medicaid beneficiaries.
The primary objective of this study was to evaluate the effect of the DRA, which allowed states to enforce ED copayments for nonurgent visits, on ED utilization among Medicaid beneficiaries. We compared the effect among beneficiaries living in states that did (copayment states) and did not (control states) adopt ED copayments. We also examined 2 secondary outcomes. First, we evaluated whether the DRA enforcement of ED copayments increased the use of outpatient medical providers, as anticipated by policy makers. Second, we examined whether the DRA enforcement was associated with increased inpatient length of stay among Medicaid beneficiaries. We hypothesized that delays in seeking care because of copayment enforcement may result in patients seen later in the course of illness.
Methods
Approval for this study was obtained from the institutional review board of The Johns Hopkins University School of Medicine. Approval for accessing state-identified data was obtained from the Agency for Healthcare Research and Quality. No individual-level data were used.
Study Design
We used a difference-in-difference quasi-experimental approach to evaluate the effect of the DRA on ED utilization in copayment states compared with control states. We examined trends from 2001 to 2010. Because we were interested in the potential effect of the DRA’s enforcement mechanism, which came into effect in 2006, we used data from 2001 to 2005 for the prepolicy period and data from 2007 to 2010 as the postpolicy period.8
Copayment states included Florida, Kentucky, Minnesota, Montana, Ohio, Pennsylvania, South Carolina, and Washington (eTable in the Supplement). These states instituted copayments (range, $3-$15) at staggered times from 2002 to 2006. Control states included California, Colorado, Connecticut, Georgia, Louisiana, Maryland, Michigan, North Carolina, Virginia, and Texas. To our knowledge, there is no published information on the proportion of hospitals in states that are pursuing the collection of copayments.
Database
We used the Household Component of the Medical Expenditure Panel Survey, a nationally representative survey of noninstitutionalized US civilians.9 The Household Component collects data from a sample of families and individuals in selected communities across the United States and oversamples African Americans, Hispanics, and Asians. Survey data are validated against payment receipts and insurance claims data.
Study Population
The study cohort was the population of individuals 19 to 64 years old enrolled in Medicaid for a full calendar year. Those 18 years or younger were excluded because cost-sharing rules are different for children in Medicaid and because their patterns of use are determined in part by parental behaviors.10,11 Adults 65 years or older were excluded because they would be covered by Medicare.
Outcome Variables
The main dependent variable was the total number of ED visits for each individual. Visits were not coded according to urgency, which prevented us from examining only nonurgent ED use. We also evaluated the total annual visits to outpatient medical providers and the mean inpatient length of stay (in days) for all individuals as secondary outcomes. Outpatient medical providers were defined as physicians with the following specialties: internal medicine, general practice, family medicine, obstetrics and gynecology, and osteopathy. For the purpose of this study, all visits to internal medicine physicians (with and without a subspecialty) were included because subspecialties were not coded in the Medical Expenditure Panel Survey.
Control Variables
At the person level, the study controlled for the sex, age, race, marital status, income relative to the federal poverty level, educational level, and self-reported health status of Medicaid enrollees. Self-reported health rather than a count of comorbidities was used because it is less likely to be affected by health care utilization.12,13
Statistical Analysis
A difference-in-difference analysis was conducted in which changes in outcomes in copayment states were estimated and compared with changes in outcomes in control states. The difference-in-difference design allowed for comparison of each group of states with itself before and after the policy while adjusting for observed differences in patient characteristics. We modeled a time trend in outcomes for copayment states and control states to capture changes that might be due to the gradual implementation or awareness of the cost-sharing policies. This design prevented bias from 2 possible sources. First, a difference between copayment states and control states that remained constant before and after implementation of the DRA could not be mistaken for a policy effect. Second, by controlling for the person-level demographic and health characteristics noted above, we could better distinguish implementation of a cost-sharing policy from contemporaneous changes in the case mix of Medicaid enrollees. Copayment states and control states had similar levels of Medicaid managed care, primary care case management, and per capita primary care physicians (eTable in the Supplement).14-16 State fixed effects were included in all regressions to control for time-invariant unobservable differences between states.17 The unit of analysis was the person-year level.
We estimated separate zero-inflated Poisson regression models for ED visits, inpatient length of stay, and outpatient medical provider visits. This model specification accommodated excess zeros in the dependent variables corresponding to nonusers of a particular service. We estimated the effect of the copayment policy on annual utilization per person by computing differences in use, predicted with the regression models, before and after introduction of copayments in copayment states. We then subtracted the analogous difference predicted for control states to obtain a difference-in-difference estimate. We used bootstrapping with 500 replications to estimate a CI for this difference-in-differences estimate. Our main estimate was calculated by comparing the average predictions across prepolicy and postpolicy years. To test for any significant time trends in ED use, we also compared the models’ predictions in each postimplementation year (eg, 2007) with the mean predictions for all years preceding the copayment policy. This approach enabled us to incorporate estimates of the main policy effect, as well as the time trend and policy interaction term, in a nonlinear model.18
We performed several sensitivity analyses. First, we changed the postpolicy period to 2008 to 2010 to give the DRA more time to be implemented. Second, because states instituted different copayment amounts, we restricted copayment states to those with the highest copayments (Florida, Minnesota, and Kentucky) to determine whether higher copayments resulted in greater effect on ED utilization and secondary outcomes. Third, we estimated a logistic regression model for the probability that Medicaid enrollees had any inpatient admissions through the ED. All analyses were conducted using statistical software (STATA 13; StataCorp LP).
Results
The study cohort consisted of 3122 adult Medicaid recipients in copayment states and 7433 adult Medicaid recipients in control states. There was no significant difference in the sex composition or age distribution between copayment states and control states (Table 1). However, patients in copayment states were more likely to be single and of nonwhite race, report fair or poor health status, and have an income below the federal poverty level (P < .01 for all).
| Enrollees in states with copayments n (%) |
Enrollees in states without copayments n (%) |
p-value | |
|---|---|---|---|
|
| |||
| Total | 3122 (100) | 7433 (100) | |
|
| |||
| Age | 0.2 | ||
| 19-35 | 1549 (49.6) | 3722 (50.1) | |
| 36-50 | 1033 (33.1) | 2434 (32.7) | |
| 50-64 | 540 (17.3) | 1227 (16.5) | |
|
| |||
| Gender | 0.2 | ||
| Female | 2329 (74.6) | 5419 (72.9) | |
|
| |||
| Race | 0.0014 | ||
| White | 1770 (56.7) | 4428 (59.6) | |
| Non-white | 1352 (43.3) | 3005 (40.4) | |
|
| |||
| Marital Status | <0.0001 | ||
| Single | 1415 (45.3) | 3164 (42.6) | |
| Married | 851 (27.3) | 2756 (37.1) | |
| Separated/Divorced | 773 (24.8) | 1311 (17.6) | |
| Widowed | 83 (2.7) | 202 (2.7) | |
|
| |||
| Education | <0.0001 | ||
| Less than HS | 1319 (42.2) | 3717 (50.0) | |
| Graduated HS | 1227 (39.3) | 2409 (32.4) | |
| Some College | 540 (17.3) | 1210 (16.3) | |
|
| |||
| Income relative to FPL |
<0.0001 | ||
| <100% | 1864 (59.7) | 3887 (52.3) | |
| 100%-200% | 847 (27.1) | 2449 (32.9) | |
| >200% | 411 (13.1) | 1097 (14.8) | |
|
| |||
| Perceived health status |
<0.0002 | ||
| Excellent-Good | 2018 (64.6) | 5063 (68.1) | |
| Fair-Poor | 1011 (32.4) | 2190 (29.5) | |
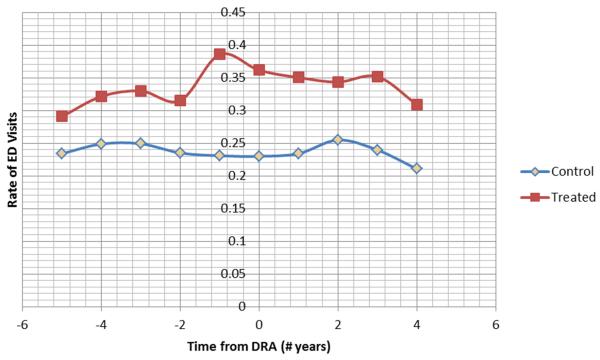
The Figure shows that copayment states had higher unadjusted rates of ED visits before 2006; however, it does not indicate that ED visits declined in copayment states after 2006. The regression models confirm this observation. In particular, when we compared the average predictions across prepolicy and postpolicy years, we found that the DRA did not lead to significant differences in the rate of ED visits per enrollee (change, 0.05; 95% CI, −0.05 to 0.16) in copayment states compared with control states. Our estimate of the effect of the copayment policy remained essentially unchanged when we restricted copayment states to those with the highest copayments (Florida, Minnesota, and Kentucky) and when we considered the post-DRA policy to include only 2008 to 2010.
There was also no significant time trend in ED use when comparing each post implementation year with the mean use in all years preceding the copayment policy (Table 2). In fact, the positive and borderline significant estimate in 2010 suggests that, on average, ED visits among patients in control states fell faster than rates in copayment states.
Table 2.
Estimated Effect of Co-Payments on ED Visits per Enrollee (Poisson Model) in Copayment States
| Poisson Model | |||
|---|---|---|---|
| Observed Rate Change* |
95% CI** | P value |
|
| Mean Difference |
0.05 | −0.05 to 0.16 | 0.30 |
| 2007 | −0.04 | −0.19 to 0.11 | 0.56 |
| 2008 | 0.02 | −0.08 to 0.13 | 0.66 |
| 2009 | 0.09 | −0.02 to 0.20 | 0.11 |
| 2010 | 0.15 | −0.00 to 0.30 | 0.05 |
indicate change in rates of ED visits per enrollee when compared to the pre-policy mean difference
CI was calculated using bootstrapping with 500 samples
Next, we evaluated the effect of ED copayments on the use of outpatient medical providers and total inpatient days per year. We found no change in the rate of outpatient medical provider visits in copayment states compared with control states after the DRA (change, 0.02; 95% CI, −0.31 to 0.35). A zero-inflated Poisson regression model with all individuals (including those not admitted to the hospital) found no effect of the DRA on annual inpatient days as measured by length of stay (change in per-enrollee inpatient days, 0.13; 95% CI, −0.31 to 0.57). Last, we detected no significant change in the probability that Medicaid enrollees were admitted to a hospital through the ED after implementation of the DRA (change in admission probability, −0.00; 95% CI, −0.03 to 0.02).
Discussion
Consistent with a previous study7 that examined ED copayments through 2006, our difference-in-difference analysis of data over a 10-year period did not demonstrate a reduction in ED use following the DRA enforcement. We also found no evidence that ED copayments were associated with increased use of outpatient medical providers. Medicaid enrollees in copayment states for nonurgent visits also did not have a significant increase in inpatient length of stay or a change in the likelihood of being admitted to a hospital through the ED after implementation of the DRA.
Several factors may have contributed to these findings. Although copayment states were given enforcement authority, provisions necessary for collecting copayments may be difficult to meet. First, the EMTALA requires that hospitals provide appropriate medical screening to persons seeking medical care through an ED and that hospitals treat and stabilize anyone with an emergency medical condition. Fear of violating the provisions of the EMTALA may serve as a disincentive to turn away persons with nonurgent needs. Second, and relatedly, ED health care providers may have difficulty determining whether a visit was due to a medical emergency or was nonurgent.19 There is no consensus on what constitutes a nonurgent visit, which helps account for the wide variation in estimates for nonurgent ED visits (range, 8%-60% of all ED visits).20-23 Third, ED staff are required to give the beneficiary the name of an accessible Medicaid health care provider, which, given the national shortage of Medicaid health care providers, may be difficult for many EDs.24 Fourth, once an initial triage is completed and the patient’s condition is determined to be nonurgent, hospitals may be less willing to bear the added administrative burden of determining to whom the copayments apply, especially when the copayment amount is small. In this setting, the proportion of hospitals enforcing the copayment provisions and seeking to collect ED copayments for nonurgent visits is unclear.
An additional explanation for these findings is that patients may have been unaware of cost-sharing provisions. Given that repeat users of the ED may have been more likely to know about copayment policies, we examined the changes in use for persons with at least 1 ED visit. In this population, we continued to find no evidence of a reduction in ED use. Even when patients are aware of the provisions, they (like their ED health care providers) may have difficulty distinguishing urgent from nonurgent care. Additional explanations for our findings could include rapid growth in Medicaid enrollment from 2007 to 2011 as a result of the Great Recession and state Medicaid expansions that preceded the ACA.1 Medicaid enrollment for the previously uninsured has been demonstrated to increase the use of the ED.25
Nationally, ED visits account for only 2% to 6% of Medicaid health expenditures, whereas hospital care accounts for one-third of all costs.26 This cost breakdown may serve as a disincentive for policy makers and hospital administrators to focus cost-saving provisions on the ED. However, some states (eg, Washington) are putting increased pressure on hospitals to decrease nonurgent ED admissions by reducing or eliminating Medicaid reimbursements for enrollees who visit the ED for specified nonurgent conditions.27
This study has several limitations. First, we were unable to determine whether an ED visit was deemed nonurgent and whether a copayment was requested. Second, although we controlled for patient-level factors, new Medicaid enrollees may have differed from previous beneficiaries in ways that we did not observe, which could have affected ED use and inpatient length of stay.28 Third, our model evaluated the use of outpatient medical providers rather than primary care physicians alone. Visits to all internal medicine physicians were included because subspecialties were not coded in the Medical Expenditure Panel Survey. It is also possible that different distributions of these medical providers in copayment states and control states may have contributed to our findings. Fourth, copayment rules can vary by Medicaid eligibility segment, which we do not observe in the data and which may make it more difficult for health care providers to determine when a copayment applies.
Copayments are seen as a tool to instill personal financial responsibility and to enable beneficiaries to make better choices regarding where and when to seek health care.4 As states expand Medicaid coverage under the ACA, many are using Medicaid expansion as an opportunity to negotiate waivers with the Centers for Medicare & Medicaid Services to expand cost-sharing strategies, including higher-than-nominal copayments and monthly premiums. In this effort, the ED has been frequently cited as a target for cost sharing because of the commonly held belief that frequent users contribute to the rising cost of Medicaid.26 Under the final rule released in July 2013 by the Centers for Medicare & Medicaid Services implementing Medicaid provisions of the ACA, states may now impose cost sharing for nonemergency services, with no upper limit for families with incomes above 150% of the federal poverty level and $8 for families with incomes below 150% of the federal poverty level.29
Conclusions
Our results suggest that, as Medicaid expands under the ACA, the effect of an unprecedented number of cost-sharing strategies will need to be evaluated carefully for intended and unintended consequences. Imposing cost sharing in a low-income population may not, on its own, discourage the use of the ED for nonurgent care or increase primary care visits. Moreover, because there are no standardized clinical criteria for defining a nonurgent visit, enforcing copaymentsmay be impractical. Rather than using ED cost sharing to change beneficiary behavior—a strategy that has shown little success—additional policy levers and incentives that promote the use of preventive care should be explored.
Supplementary Material
Figure 1.
Unadjusted Rate of ED Visits in Copayment (Treated) States versus Zero Copayment (Control) States Before and After the DRA
Acknowledgments
Funding/Support: Dr Siddiqui’s salary was supported by National Research Service Award 1T32HS019488-02 from the Agency for Healthcare Research and Quality for Postdoctoral Comparative Effectiveness Development Training. Mr Roberts received support from a T-32 National Research Service Award from the Agency for Healthcare Research and Quality, a predoctoral dissertation award from the Jayne Koskinas Ted Giovanis Foundation for Health and Policy, and the Hal Cohen CareFirst Blue Cross Blue Shield Scholarship. Dr Pollack’s salary is supported by Career Development Award K07CA151910 from the National Cancer Institute and the Office of Behavioral and Social Sciences Research, National Institutes of Health.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Appendix
Appendix Table.
| States | Copayment amount ($) |
Medicaid Managed Care Enrollment (%) |
Primary Care Case Management Enrollment (%)** |
Medicaid Patient Centered Medical Home |
|---|---|---|---|---|
| STATES with COPAYMENTS | ||||
| Washington | 3 | 86.7 | 0.6 | Yes |
| Florida | 5% ($15 cap)* | 64.5 | 31.6 | Yes |
| Minnesota | 6 | 63.8 | 0.0 | Yes |
| Montana | 5 | 74.6 | 99.9 | Yes |
| South Carolina | 3 | 100 | 13.8 | Yes |
| Kentucky | 5% ($6 cap)* | 88.2 | 44.0 | Yes |
| Ohio | 3 | 73.5 | 0.0 | Yes |
| Pennsylvania | 3 | 81.7 | 17.5 | Yes |
| STATES without COPAYMENTS | ||||
| Texas | 0 | 67.0 | 33.7 | Yes |
| California | 0 | 55.1 | 0.0 | Yes |
| Maryland | 0 | 79.5 | 0.0 | Yes |
| Georgia | 0 | 91.0 | 9.1 | No |
| Michigan | 0 | 86.2 | 0.0 | Yes |
| Louisiana | 0 | 63.7 | 99.9 | Yes |
| Virginia | 0 | 59.2 | 10.7 | Yes |
| North Carolina | 0 | 77.5 | 98.3 | Yes |
| Connecticut | 0 | 69.9 | 1.1 | Yes |
| Colorado | 0 | 94.6 | 5.1 | Yes |
As percent of total payment with cap on copayment amount
Of those enrolled in Medicaid Managed Care
Footnotes
Author Contributions: Dr Siddiqui and Mr Roberts had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Siddiqui, Pollack.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Siddiqui, Roberts.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Siddiqui, Roberts.
Administrative, technical, or material support: Siddiqui.
Study supervision: Pollack.
Conflict of Interest Disclosures: None reported.
Disclaimer: This study was done prior to Dr Siddiqui joining the White House Social and Behavioral Sciences Team. The views expressed herein do not necessarily represent the White House Social and Behavioral Sciences Team, the General Services Administration, or the United States.
References
- 1.Young K, Clemans-Cope L, Lawton E, Holahan J, Kaiser Family Foundation [Accessed July 17, 2014];Medicaid spending growth in the Great Recession and its aftermath, FY 2007-2012. 2014 Jul 3; http://kff.org/medicaid/issue-brief/medicaid-spending-growth-in-the-great-recession-and-its-aftermath-fy-2007-2012/
- 2.Congressional Budget Office [Accessed June 6, 2014];The budget and economic outlook: 2014-2024. 2014 Feb 4; http://www.cbo.gov/publication/45010.
- 3.Centers for Medicare & Medicaid Services [Accessed February 6, 2014];The Deficit Reduction Act: important facts for state government officials. 2006 https://www.cms.gov/Regulations-and-Guidance/Legislation/DeficitReductionAct/downloads/checklist1.pdf.
- 4.Saloner B, Sabik L, Sommers BD. Pinching the poor? Medicaid cost sharing under the ACA. N Engl J Med. 2014;370(13):1177–1180. doi: 10.1056/NEJMp1316370. Medline:24670163. [DOI] [PubMed] [Google Scholar]
- 5.Selby JV. Cost sharing in the emergency department—is it safe? Is it needed? N Engl J Med. 1997;336(24):1750–1751. doi: 10.1056/NEJM199706123362411. Medline:9180095. [DOI] [PubMed] [Google Scholar]
- 6.Haley J, Zuckerman S, Kaiser Family Foundation [Accessed February 8, 2014];Is lack of coverage a short- or long-term condition? 2003 Jul 30; http://kff.org/uninsured/issue-brief/is-lack-of-coverage-a-short-or/
- 7.Mortensen K. Copayments did not reduce Medicaid enrollees’ nonemergency use of emergency departments. Health Aff (Millwood) 2010;29(9):1643–1650. doi: 10.1377/hlthaff.2009.0906. Medline:20820020. [DOI] [PubMed] [Google Scholar]
- 8.Kaiser Family Foundation [Accessed September 9, 2014];Annual updates on eligibility rules, enrollment and renewal procedures, and cost-sharing practices in Medicaid and CHIP. 2013 Jan 23; http://kff.org/medicaid/report/annual-updates-on-eligibility-rules-enrollment-and/
- 9.Cohen JW, Monheit AC, Beauregard KM, et al. The Medical Expenditure Panel Survey: a national health information resource. Inquiry. 1996-1997;33(4):373–389. Medline:9031653. [PubMed] [Google Scholar]
- 10.Gindi RM, Jones LI. [Accessed October 14, 2014];Reasons for emergency room use among US children: National Health Interview Survey, 2012. 2014 Jul; http://www.cdc.gov/nchs/data/databriefs/db160.htm. [PubMed]
- 11.Yoffe SJ, Moore RW, Gibson JO, et al. A reduction in emergency department use by children from a parent educational intervention. Fam Med. 2011;43(2):106–111. Medline:21305425. [PubMed] [Google Scholar]
- 12.Manor O, Matthews S, Power C. Self-rated health and limiting longstanding illness: inter-relationships with morbidity in early adulthood. Int J Epidemiol. 2001;30(3):600–607. doi: 10.1093/ije/30.3.600. Medline:11416091. [DOI] [PubMed] [Google Scholar]
- 13.Schnittker J, Bacak V. The increasing predictive validity of self-rated health. PLoS One. 2014;9(1):e84933. doi: 10.1371/journal.pone.0084933. doi:10.1371/journal.pone.0084933.Medline:24465452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Medicare & Medicaid Services [Accessed October 12, 2014];Medicaid managed care enrollment report. 2011 Jul 1; http://www.medicaid.gov/medicaid-CHIP-Program-Information/By-Topics/Data-and-Systems/Downloads/2011-Medicaid-MC-Enrollment-Report.pdf.
- 15.National Academy for State Health Policy [Accessed October 15, 2014];Medical home & patient-centered care. 2013 http://www.nashp.org/med-home-map.
- 16.Hing E, Hsiao CJ. [Accessed October 21, 2014];National Center for Health Statistics data brief: state variability in supply of office-based primary care providers: United States, 2012. 2014 May; http://www.cdc.gov/nchs/data/databriefs/db151.htm. [PubMed]
- 17.Bertrand M, Duflo E, Mullainathan S. How much should we trust differences-in-differences estimates? Q J Econ. 2004;119(1):249–275. [Google Scholar]
- 18.Karaca-Mandic P, Norton EC, Dowd B. Interaction terms in nonlinear models. Health Serv Res. 2012;47(1, pt 1):255–274. doi: 10.1111/j.1475-6773.2011.01314.x. Medline:22091735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gill JM, Riley AW. Nonurgent use of hospital emergency departments: urgency from the patient’s perspective. J Fam Pract. 1996;42(5):491–496. Medline:8642367. [PubMed] [Google Scholar]
- 20.Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19(1):47–59. Medline:23379744. [PMC free article] [PubMed] [Google Scholar]
- 21.Ly N, McCaig LF. National Hospital Ambulatory Medical Care Survey: 2000 outpatient department summary. Adv Data. 2002;(327):1–27. Medline:12661587. [PubMed] [Google Scholar]
- 22.Pitts SR, Carrier ER, Rich EC, Kellermann AL. Where Americans get acute care: increasingly, it’s not at their doctor’s office. Health Aff (Millwood) 2010;29(9):1620–1629. doi: 10.1377/hlthaff.2009.1026. Medline:20820017. [DOI] [PubMed] [Google Scholar]
- 23.Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008;(7):1–38. Medline:18958996. [PubMed] [Google Scholar]
- 24.Texas Health and Human Services Commission [Accessed February 6, 2014];Co-pays for nonemergent use of hospital emergency rooms: cost effectiveness and feasibility analysis. 2008 May; http://www.hhsc.state.tx.us/reports/HospitalEmergencyRoomsAnalysis_0708.pdf.
- 25.Taubman SL, Allen HL, Wright BJ, Baicker K, Finkelstein AN. Medicaid increases emergency-department use: evidence from Oregon’s Health Insurance Experiment. Science. 2014;343(6168):263–268. doi: 10.1126/science.1246183. Medline:24385603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Handel DA, McConnell KJ, Wallace N, Gallia C. How much does emergency department use affect the cost of Medicaid programs? Ann Emerg Med. 2008;51(5):614–621. 621.e1. doi: 10.1016/j.annemergmed.2007.09.002. Medline:17996983. [DOI] [PubMed] [Google Scholar]
- 27.Trapp D. [Accessed October 17, 2014];American Medical News. Some states limit Medicaid fees for certain ED visits. 2011 http://www.amednews.com/article/20111017/government/310179946/4/
- 28.Natoli C, Cheh V, Verghese S. [Accessed March 13, 2014];Who will enroll in Medicaid in 2014? lessons from Section 1115 Medicaid waivers. 2011 May; https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/MedicaidDataSourcesGenInfo/downloads/Max_IB_1_080111.pdf.
- 29.Rosenbaum S. [Accessed March 19, 2014];Update: final rule on Medicaid and CHIP, including essential health benefits in alternative benefit plans; eligibility notices, fair hearings and appeals processes; premiums and cost sharing; and exchange eligibility and enrollment. 2013 http://www.healthreformgps.org/wp-content/uploads/Rosenbaum-update-on-part-2-final-7-15.pdf. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.