To the Editor: Chronic sleep curtailment is endemic in modern societies. The majority of the daily testosterone release in men occurs during sleep.1 Sleep fragmentation and obstructive sleep apnea are associated with reduced testosterone levels.2 In older men, morning testosterone levels are partly predicted by total sleep time.3 Testosterone is critical in male sexual behavior and reproduction, but also has important beneficial effects on muscle mass and strength, adiposity, bone density, and vigor and well-being.4 We investigated the effect of 1 week of sleep restriction on testosterone levels in young healthy men.
METHODS
The protocol was approved by the University of Chicago institutional review board. Volunteers responded to flyers posted around campus. Exclusion criteria included a history of endocrine or psychiatric disorders, irregular bedtimes, and sleep complaints. Written informed consent was obtained from 28 persons. Ten men passed all screening tests and completed the study, which was performed between January 2003 and September 2009. The sample size was estimated using data from previous work on the hormonal impact of sleep restriction.
After 1 week of 8-hour bedtimes (from 11 PM to 7 AM) at home, the participants spent 11 days in the laboratory for 3 nights of 10-hour bedtimes (from 10 PM to 8 AM; rested condition) followed by 8 nights of 5-hour bedtimes (from 12:30 AM to 5:30 AM; sleep restriction). Sleep was recorded each night and visually scored in stages 1, 2, 3, 4, and rapid eye movement (REM). Blood sampling every 15 to 30 minutes for 24 hours was initiated after the second 10-hour night and after the seventh 5-hour night. Samples were assayed for total testosterone and cortisol using an immunochemiluminescent assay (Immulite, Los Angeles, California). (To convert serum testosterone to ng/dL, divide by 0.0347; to convert serum cortisol to μg/dL, divide by 27.588.) Participants completed the visual analog scales for global vigor and global affect at 2-hour intervals each day.5 Comparisons between conditions were performed using 2-sided nonparametric Wilcoxon tests with a significance level of .05 (JMP7; SAS Institute, Cary, North Carolina).
RESULTS
The 10 healthy men had a mean (SD) age of 24.3 (4.3) years and a mean (SD) body mass index of 23.5 (2.4) (calculated as weight in kilograms divided by height in meters squared). Total (SD) sleep time decreased from 8 hours 55 minutes (35 min) to 4 hours 48 minutes (6 min) with sleep restriction (P = .002). Relative to the rested condition, during each restricted night, participants lost a total (SD) of 2 hours 45 minutes (29 min) of stage-2 sleep (P = .002) and 1 hour 3 minutes (18 min) of REM sleep (P = .002) and gained 9 minutes (8 min) of sleep in stages 3 + 4 (P = .01).
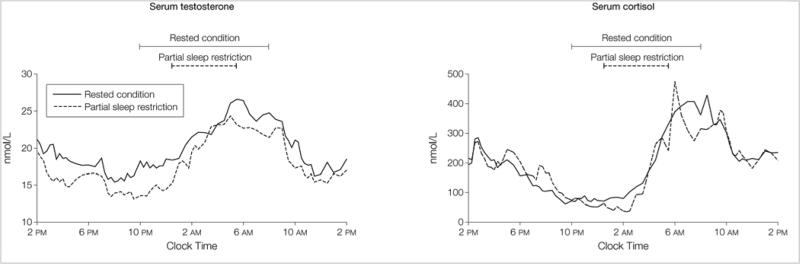
During waking hours common to both conditions (8 AM-10 PM), testosterone levels were lower after sleep restriction than in the rested condition (16.5 [2.8] nmol/L vs 18.4 [3.8] nmol/L; P = .049). The effect of restricted sleep was especially apparent between 2 PM and 10 PM (15.5 [3.1] nmol/L vs 17.9 [4.0] nmol/L; P = .02). Daytime cortisol profiles were similar under both conditions (Figure). Daily sleep restriction was associated with a progressive decrease in mean (SD) vigor scores from 28 (5) after the first night to 19 (7) after the seventh night (P = .002).
Figure.
24-Hour Profiles of Serum Testosterone and Serum Cortisol According to Bedtime Condition
Shown are mean values. In the rested condition, bedtimes were from 10 PM to 8 AM. Values for partial sleep restriction were taken after 1 week of restriction, for which bedtimes were from 12:30 AM to 5:30 AM. On average over the 68 time points, the SD of testosterone levels at each time point was 5.01 nmol/L (range, 2.98-7.53 nmol/L) in the rested condition and 4.26 nmol/L (range, 2.82-6.92 nmol/L) in the restricted condition. On average over the 68 time points, the SD of cortisol levels at each time point was 67.1 nmol/L (range, 15.2-142.7 nmol/L) in the rested condition and 54.0 nmol/L (range, 7.7-162.3 nmol/L) in the restricted condition.
COMMENT
Daytime testosterone levels were decreased by 10% to 15% in this small convenience sample of young healthy men who underwent 1 week of sleep restriction to 5 hours per night, a condition experienced by at least 15% of the US working population. By comparison, normal aging is associated with a decrease of testosterone levels by 1% to 2% per year.6 This testosterone decline was associated with lower vigor scores but not with increased levels of cortisol, a stress-responsive hormone that can inhibit gonadal function. Symptoms and signs of androgen deficiency include low energy, reduced libido, poor concentration, and increased sleepiness, all of which may be produced by sleep deprivation in healthy individuals. Additional investigations of the links between sleep and testosterone are needed to determine whether sleep duration should be integrated in the evaluation of androgen deficiency.
Acknowledgments
Funding/Support: This work was supported by the National Heart, Lung, and Blood Institute grant 5R01HL72694-5, by the National Institute of Diabetes and Digestive and Kidney Diseases grant P60DK-020595, and by the National Institutes of Health grant MO1-RR-00055.
Role of the Sponsor: The funding agencies had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Leproult had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Leproult, Van Cauter.
Acquisition of data: Leproult, Van Cauter.
Analysis and interpretation of data: Leproult, Van Cauter.
Drafting of the manuscript: Leproult, Van Cauter.
Critical revision of the manuscript for important intellectual content: Leproult, Van Cauter.
Statistical analysis: Leproult, Van Cauter.
Obtained funding: Van Cauter.
Additional Contributions: We thank the volunteers who participated in this demanding study and the research and technical staff of the Clinical Resource Center, the Diabetes Research and Training Center, and the Sleep Research Laboratory at the University of Chicago. Volunteers were compensated for their participation; staff members were not compensated outside of their salaries.
Conflict of Interest Disclosures: Both authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1.Axelsson J, Ingre M, Akerstedt T, Holmbäck U. Effects of acutely displaced sleep on testosterone. J Clin Endocrinol Metab. 2005;90(8):4530–4535. doi: 10.1210/jc.2005-0520. PubMed | Link to Article. [DOI] [PubMed] [Google Scholar]
- 2.Andersen ML, Tufik S. The effects of testosterone on sleep and sleep-disordered breathing in men: its bidirectional interaction with erectile function. Sleep Med Rev. 2008;12(5):365–379. doi: 10.1016/j.smrv.2007.12.003. PubMed | Link to Article. [DOI] [PubMed] [Google Scholar]
- 3.Penev PD. Association between sleep and morning testosterone levels in older men. Sleep. 2007;30(4):427–432. doi: 10.1093/sleep/30.4.427. PubMed. [DOI] [PubMed] [Google Scholar]
- 4.Bremner WJ. Testosterone deficiency and replacement in older men. N Engl J Med. 2010;363(2):189–191. doi: 10.1056/NEJMe1006197. PubMed | Link to Article. [DOI] [PubMed] [Google Scholar]
- 5.Monk TH. A visual analogue scale technique to measure global vigor and affect. Psychiatry Res. 1989;27(1):89–99. doi: 10.1016/0165-1781(89)90013-9. PubMed | Link to Article. [DOI] [PubMed] [Google Scholar]
- 6.Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR. Baltimore Longitudinal Study of Aging. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. J Clin Endocrinol Metab. 2001;86(2):724–731. doi: 10.1210/jcem.86.2.7219. PubMed | Link to Article. [DOI] [PubMed] [Google Scholar]