Abstract
Background
Attitudes and views are critical to the adoption of innovation. While there have been broadening calls for a standardized dental diagnostic terminology, little is known about the views of private practice dental team members towards the adoption of such a terminology.
Methods
A survey was developed using validated questions identified through literature review. Domain experts’ input allowed for further modifications. The final survey was administered electronically to 814 team members at a multi-office practice based in the Pacific Northwest.
Results
Response proportion was 92%. The survey had excellent reliability (Cronbach alpha coefficient = 0.87). Results suggested that participants showed, in general, positive attitudes and beliefs towards using a standardized diagnostic terminology in their practices. Additional written comments by participants highlighted the potential for improved communication with use of the terminology.
Conclusions
Dental providers and staff in one multi-office practice showed positive attitudes towards the use of a diagnostic terminology, specifically they believed it would improve communication between the dentist and patient as well as among providers, while expressing some concerns if using standardized dental diagnostic terms helps clinicians to deliver better dental care.
Practical Implications
As the dental profession is advancing towards the use of standardized diagnostic terminologies, successful implementation will require that dental team leaders prepare their dental teams by gauging their attitude toward the use of such a terminology.
Keywords: Dentistry, diagnostic terminology, attitudes and beliefs, electronic health record, International Classification of Diseases, Systematized Nomenclature of Medicine, Systematized Nomenclature of Dentistry, leadership, innovation, adoption
In medicine, use of clinical and health administrative data in health services research has been enabled by the use of a standard diagnostic terminology, the International Classification of Diseases (ICD), which was initially established by the World Health Organization in 1893 to categorize causes of death.1 In contrast, the dental profession has not yet generally adopted a standardized diagnostic terminology either for clinical care or administrative/billing purposes.2 With the advent of electronic health records (EHRs) in which “secondary” data use for research and quality improvement is becoming the norm, the need for standardized dental diagnostic terms has become a more pressing professional concern. Miller, for example, has highlighted that tracking the relationships among diagnosis, treatment, and outcomes hinges on the use of standardized diagnostic terms.2 Others have commented that quality measurement in dentistry would broadly benefit from the adoption of standardized diagnostic terms.3-5 In reality, we owe this to our patients and ultimately, the question if “dentists like it” is becoming somewhat secondary.
During the past decades, there have been several starts at developing a standardized dental diagnostic terminology, including efforts by Orlowsky in North Carolina in 19706, by the American Dental Association (ADA) with SNODENT (Systematized Nomenclature of Dentistry)7 in the early 1990s, and by Leake in the late 1990s.8 In 1998, the University of California, San Francisco developed the Z-codes9 based on Leake’s terms to which Creighton University made modifications for use in 2007 (N. Kimmes, DDS, oral communication, June 2008). While useful within the local settings at which they were developed, these previous dental diagnostic terminologies have not been widely implemented by the larger dental community, limiting the broader-reaching benefits of a common diagnostic terminology. Some stated reasons for the lack of wider adoption have been a limited ability to report specific conditions (e.g. incipient caries) for specific anatomic locations (e.g. tooth #3 occlusal surface)8 and not being freely available for integration into electronic health records by general practitioners or dental schools.10 Currently, SNOMED (Systematized Nomenclature of Medicine) contains the version SNODENT II diagnostic terms as well as many other oral health terms, for a total of close to 8,000. The dental content of SNOMED is however not limited to just the scope of SNODENT by IHTSDO (International Health Terminology Standards Development Organisation), the license holder of SNOMED. When they receive requests for dentistry concepts, it is forwarded to its International Dentistry SIG (Special Interest Group) for feedback on how to manage them (J. Millar, email communication, July 2014). SNOMED has the qualities of a good reference terminology, a terminology designed to provide common semantics for diverse implementations. A reference terminology is defined as a collection of terms, similar to a dictionary, and the relationships linking them; it is organized by meaning rather than alphabetically.11 However, a reference terminology such as SNOMED, which has been designed for data exchange and aggregation, may not be the best choice for direct implementation into the user interface12 of the EHR.
Instead, what is needed for clinical deployment in the EHR user interface is a purpose-built interface terminology,13 which has a manageable number of terms, incorporates language that clinicians are familiar with, and can be linked back to a reference terminology (SNOMED, in this case). In response to this need, in 2009, a Harvard-led research team proposed a practical standardized dental diagnostic interface terminology10 incorporating existing dental diagnostic concepts and terms such as the Z-codes, oral health terms contained in the International Classification of Diseases (ICD) - 9th/10th editions and relevant Systematized Nomenclature of Medicine Clinical Terms (SNOMED-CT). This terminology, originally called EZCodes, consisted of 13 major diagnostic categories, 80 subcategories, and 1,158 unique dental diagnostic terms and codes.14 As of 2014, the EZCodes dental diagnostic terminology has been renamed Dental Diagnostic System (DDS) and has evolved to now include 16 categories, 100 subcategories, and 1,518 unique terms, and now include a number of completely novel terms not previously available in SNOMED or ICD.
The adoption of standardized dental diagnostic terms must be considered in a context larger than the purely technical. In order to achieve their promise, these terms must be consistently entered by dental clinical team members in the course of their practices, which a practitioner is certainly less likely to do if s/he views standardized diagnostic terms as not being very useful. Our team’s experiences at sites with existing deployments in the academic setting have highlighted that there may be work to do in the broader socio-technical milieus in which these terms are being deployed: illogical placement of buttons, the need for a scroll bar to find a term in long list and tabs to click through multiple screens as part of the treatment plan were all considered less useful and dampened enthusiasm to use the terminology.15 Addressing these issues saw a significant increase in utilization. (Unpublished data) We identified no work in the literature that would enlighten us in this respect, so we undertook to evaluate the attitudes and views of clinical team members in large, multi-office practice based in the U.S. Pacific Northwest that had not adopted a standardized dental diagnostic terminology.
METHODS
Survey instrument development
Our work is grounded in the Technology Acceptance Model (TAM)16-18, one of the most widely researched models for linking behavior with attitudes and beliefs in the context of technical innovations. TAM17 and its extended versions, TAM219 and TAM320, are well-established and have been found to be reliable and robust parsimonious models for predicting user acceptance.17, 19-25 The constructs covered by TAM, TAM2 and TAM3 started with perceived usefulness and perceived ease of use (TAM); added job relevance, output quality, and result demonstrability (TAM2); to finally include computer self-efficacy, computer anxiety, computer playfulness, perceptions of external control, perceived enjoyment and objective usability (TAM3).20 We composed our survey from relevant items from the validated TAM17, 21, TAM225, and TAM320 surveys, as well as a Task Technology Fit (TTF) survey.26 Items that did not apply to the dental setting were excluded (e.g. “Display pages provide links to more detailed information”21, “To my knowledge, the hospital information system meets its production schedules, such as report delivery”26). Additionally, the research team developed several task-fit questions specifically for the dental setting using the Task-Fit survey26 as a guide and modifying some of its questions, e.g., “Standardized dental diagnostic terms would allow dental team members to use the same term to describe the same diagnosis.” Evaluation for additional face and construct validity was not deemed necessary as all questions were taken from previously validated surveys. The resulting survey instrument (see the Appendix) covered four TAM constructs: perceived usefulness, subjective norms and image, job relevance, and results demonstrability. These constructs were addressed through 11 items; each item was measured with a 5-point Likert scale ranging from 1 to 5 with the following textual anchors: 1 (strongly disagree), 2 (disagree), 3 (not disagree nor agree), 4 (agree), and 5 (strongly agree). There was also one open-ended question at the end of the questionnaire to solicit any additional views about standardized dental diagnostic terms that the participants may have wanted to convey.
Participants and survey administration
From November through December 2011, participants were recruited from a large dental private group practice, comprised of 54 dental offices located in three states in the U.S. Pacific Northwest. The offices range in size from 2-10 dental providers (dentists and hygienists) per office with 4-37 staff (dental assistants, front desk staff, sterilization staff) to support the providers in each office. The survey (see the Appendix) was sent via email to 814 dentists, dental hygienists, dental assistants, and nonclinical staff. The email was sent by the research team’s PI and not from the dental group practice’s leadership as per IRB protocol. To enhance participation, and therefore the soundness of our findings, reminder emails were sent on a weekly cycle with alerts to the practice managers about aggregate, de-identified response rates in an effort to encourage response. Permission to administer the survey was obtained from the dental group practice’s leadership, and IRB approval (protocol #23901) for the study was obtained from the Harvard Medical School’s Institutional Review Board.
Data analysis
Quantitative data analysis
Frequency statistics were calculated to determine the distribution of disciplines and primary roles of the participants. We evaluated the internal consistency within constructs by calculating the Cronbach alpha coefficient, and used Pearson’s Product Moment Correlation Coefficients to assess the relationships among items. We calculated the mean Likert score (1-5) for the 11 items and assessed the differences among them using one-way ANOVA. Multiple comparisons were addressed using Tukey’s Honestly Significant Difference (HSD) test.
Views and attitudes regarding the terminology were determined by calculating means (and standardized deviations) of agreement of statements concerning a standardized dental diagnostic terminology. A one-way repeated measured analysis of variance was used to calculate significant main effect of statements and Tukey’s Honestly Significant Difference (HSD) test was used to compare pairwise means.
Qualitative data analysis – Open-ended question
A subset (n=130) of the original 814 participants in the survey (see the Appendix) chose to answer an additional “open-ended question” “If there is anything else you would like us to know about your views towards standardized dental diagnostic terms, please let us know below: Open-Ended Response.” The entries contained responses that varied from concise (e.g., 1-word responses or no comments) to lengthy (e.g., a sentence, or short paragraph responses). Each response was categorized into a nominal, 7-point scale by 2 independent raters (a dentist and a biomedical statistician) in order to create a single, numerical variable. The resulting variable would represent a quantitative version of the participants’ responses. The seven categories were positive with respect to a standardized dental diagnostic terminology, ambivalent, negative with respect to a standardized dental diagnostic terminology, don’t know, no comment, and the feeling that a standardized dental diagnostic terminology would be redundant.
We used Cohen Kappa to find the inter-rater agreement between the two raters. Each rater conducted a separate adjudication. An un-weighted kappa was performed because the groupings represented nominal scores where there was no natural ordering. The raters later conferred in order to come to consensus on the observed, differing adjudications. We also performed a test of association between respondent’s occupation/role and response, as well as measured frequency of response by occupation/role.
RESULTS
Participants
A total of 749 (92%, response proportion) completed surveys (see the Appendix) were received. 68% of the participants provided direct patient care (i.e., dentists, hygienists, dental assistants) and 32% were nonclinical staff, which included patient service representatives, records technicians, and practice managers. Detailed information and other characteristics of participants are shown in Table 1. The average years of experience was 13.6 years (SD = 11.6) for all of the roles combined. Dentists and dental specialists had an average of 17.8 years of experience and dental hygienists had an average of 13.0 years of experience. Dental assistants represented the group with the least experience, tallying on average 10.8 years. We also calculated the distribution of the types of dentistry practiced by the dentists, as categorized by the dental practice itself. The bulk of the dentist respondents were general dentists (70%), with orthodontists coming in a distant second (10%) (Table 1).
Table 1. Primary roles and specialties for dentists or specialists.
| Roles | Frequency (%) | Avg. Years of Experience (SD) |
|---|---|---|
| Dentist or dental specialist | 147 (19%) | 17.8 (13.4) |
| Dental hygienist | 120 (16%) | 13.0 (10.5) |
| Dental assistant | 246 (33%) | 10.8 (9.9) |
| Nonclinical | 236 (32%) | 12.6 (13.2) |
| Total | 749 | 13.6 (11.6) |
| Primary disciplines for dentist or specialist |
Frequency |
|---|---|
| General dentist | 97 (70%) |
| Orthodontist | 14 (10%) |
| Endodontist | 9 (7%) |
| Oral surgeon | 7 (5%) |
| Periodontist | 3 (2%) |
| Emergency dentist | 3 (2%) |
| Other | 3 (2%) |
| Pediatric dentist | 1 (1%) |
| Implant dentist | 1 (1%) |
| Prosthodontist | 0 (0%) |
| Not reported/missing | 9 (7%) |
| Total | 147 |
Reliability of survey questions
The survey questions had excellent internal consistency within constructs as shown by high values of Cronbach alpha coefficients (Table 2). We also calculated Pearson’s Product Moment Correlation Coefficients (Table 4). Most of the correlations are in the positive direction, where most of the items are highly and positively inter-correlated except, as expected, the one item that was negatively framed (i.e., ‘I would have difficulty explaining why standardized dental diagnostic terms are beneficial’).
Table 2. Internal Reliability.
| Construct | Cronbach alpha |
|---|---|
| Perceived usefulness | .88 |
| Subjective norm and image | .76 |
| Result demonstrability | −1.3 |
| Overall | .87 |
‘Job relevance’ could not be calculated because it had only one item.
Table 4. Correlation Coefficients Agreement Ratings to Statements.
| (b) | (c) | (d) | (e) | (f) | (g) | (h) | (i) | (j) | (k) | |
|---|---|---|---|---|---|---|---|---|---|---|
| (a) | .51* | .54* | .59* | .71* | .54* | .48* | .41* | .71* | .54* | −.32* |
| (b) | .64* | .73* | .43* | .49* | .41* | .68* | .55* | .45* | −.09* | |
| (c) | .75* | .51* | .50* | .39* | .60* | .58* | .45* | −.13* | ||
| (d) | .58* | .58* | .44* | .64* | .62* | .53* | −.20* | |||
| (e) | .51* | .42* | .40* | .65* | .54* | −.33* | ||||
| (f) | .55* | .54* | .59* | .55* | −.23* | |||||
| (g) | .48* | .50* | .53* | −.24* | ||||||
| (h) | .57* | .53* | −.09* | |||||||
| (i) | .67* | −.31* | ||||||||
| (j) | −.42* |
denotes p < .05; letters correspond to the statements in Table 3
Views and attitudes regarding standardized dental diagnostic terms
Table 3 shows the means and standard deviations of the responses to the 11 items. Higher mean scores correspond to higher average agreement within an item. The range between the two extreme means was nearly 2 points on the rating scale from ‘disagree’ to ‘agree’ according to the textual description anchors. The item with the highest average Likert score was “Standardized dental diagnostic terms would allow dental team members to use the same term to describe the same diagnosis” (x̄e = 4.32), followed by “standardized dental diagnostic terms would be useful” (x̄a = 4.26). The negatively-phrased item “I would have difficulty explaining why standardized dental diagnostic terms are beneficial” received the lowest rating in terms of agreement (x̄k = 2.47) followed by “Standardized dental diagnostic terms allow clinicians to deliver better dental care than those who do not use them (x̄h = 3.61).”
Table 3. Means of agreement (and standardized deviations) of statements concerning a standardized dental diagnostic terminology. This table is in the original order from the sequence in which the questions were asked. Each of the items is sequenced from a-k and the survey instrument categories are grouped together adjacently.
| Item | Category | Mean(x̄t) | SD |
|---|---|---|---|
| a: Standardized dental diagnostic terms would be useful |
Perceived Usefulness | 4.26 | 0.7 |
| b: Standardized dental diagnostic terms would improve the quality of care that I would deliver |
Perceived Usefulness | 3.77 | 1.0 |
| c: Standardized dental diagnostic terms would increase clinical productivity |
Perceived Usefulness | 3.85 | 0.9 |
| d: Standardized dental diagnostic terms would enhance effectiveness of providing care |
Perceived Usefulness | 3.93 | 0.9 |
| e: Standardized dental diagnostic terms would allow dental team members to use the same term to describe the same diagnosis |
Perceived Usefulness | 4.32 | 0.7 |
| f: Clinicians, who influence my behavior, think that standardized dental diagnostic terms are important |
Subjective Norm | 3.81 | 0.8 |
| g: In general, the practice has supported the philosophy of standardized dental diagnostic terms |
Subjective Norm | 3.96 | 0.7 |
| h: Standardized dental diagnostic terms allow clinicians to deliver better dental care than those who do not use them |
Subjective Norm | 3.61 | 0.9 |
| i: Standardized dental diagnostic terms would be important to me as a dental clinic team member |
Job Relevance | 4.07 | 0.7 |
| j: I believe that I could communicate to others the impact of standardized dental diagnostic terms |
Results Demonstrability | 3.93 | 0.7 |
| k: I would have difficulty explaining why standardized dental diagnostic terms are beneficial |
Results Demonstrability | 2.47 | 1.0 |
Table 4 shows a correlation matrix of all of the items. Since each of the 11 items are correlated, the tenet of independence is violated, hence the one-way, repeated measures ANOVA for correlated data was performed to test whether the mean Likert scores (agreement) were the same across the 11 items. Conducting the test revealed that there was a significant difference in the mean Likert Scores among the 11 items with a corresponding F-statistic of F = 426.76 and p-value of p < .001. The subsequent Tukey’s test for pairwise differences (Honestly Significant Difference =HSD) was conducted to determine which of the items was significantly different from the others. There were a total of 56 pairwise comparison tests conducted among items and 75% of them showed significant differences from another, while 25% had no evidence of significant differences. For example, the statement (e) “standardized dental diagnostic terms would allow dental team members to use the same term to describe the same diagnosis” and (a) “standardized dental diagnostic terms would be useful” were the highest rated items and were statistically significantly different from one another, while both (a) and (e) had statistically significantly higher mean agreement than (i) “standardized dental diagnostic terms would be important to me as a dental clinic team member.”
Open-ended question
16 out of 130 (16/130 = 12%) responses showed disagreement between the 2 raters while 114 out of 130 (114/130 = 88%) responses showed agreement between raters. The un-weighted kappa coefficient was κ = 0.84 with a 95% confidence interval of (0.77, 0.91). Given the judgment criteria determined by Viera (2005),27 a kappa coefficient (κ) of 0.84 represents “almost perfect agreement”. The confidence interval and corresponding z-score of 19.8 (p-value = 0) suggests that there is evidence that the kappa coefficient is significantly different from zero.
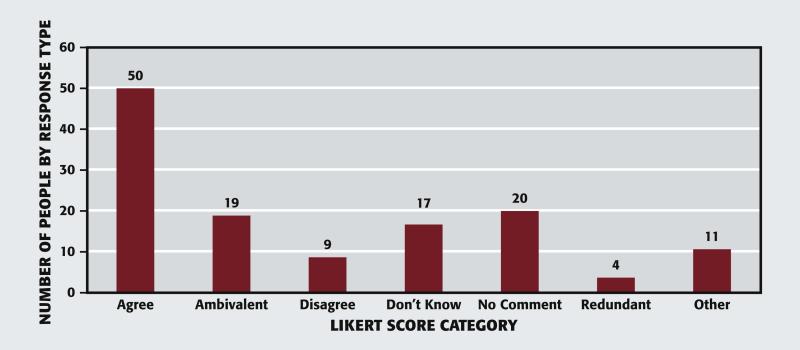
Figure 1 is a bar plot representing the distribution of 130 responses to the “open-ended question”. Fifty (38%) respondents indicated support for a standardized diagnostic dental terminology. Specifically, they commented that the terminology would improve communication between providers, patients, and other providers; other respondents reported that a terminology would raise the standard of care, it would improve digital charting, and it would prevent treatment from being performed without an accurate diagnosis in the patient record, e.g., “Stops patient confusion and gets patients and doctors/staff on the same page.”
Figure.
Open-ended question responses.
Nineteen (15%) participants reported that they had mixed feelings about the use of a standardized diagnostic dental terminology because the terminology would not affect the quality of care that they provide, however, it would improve office efficiency, charting and inter-office communication, e.g. “Standardized dental diagnostic terms would certainly improve communication and understanding among providers, specialists and the team members but I am not sure I see how that can have much of a direct impact in the area of productivity.”
Nine (7%) responses indicated a lack of support for the use of a standardized dental diagnostic terminology. The rationales contained within the responses included the difficulty of altering one’s workflow to enter diagnostic terms, the burden of additional data entry, the belief that use of a terminology would not influence dental treatment or provider’s quality of care, and the concern that providers would be spending more time entering data than delivering care to the patient, e.g. “That no matter what terms we use as a team or otherwise it will not impact my quality of care to our patients!”
Seventeen (13%) respondents reported a lack of knowledge about the terminology (e.g., “I am not exactly sure what standardized dental diagnostic terms are, from the sounds of it I gather Terms that are used universally to diagnose dental patients. I would understand this better if it were explained to me”), while twenty (15%) respondents marked that they had no comment (e.g. “none”).
Four (3%) respondents believed a standardized dental diagnostic terminology would be redundant to efforts already in place at the dental practice group (e.g., “We have a good system of coding/terminology in place which works well”), and 11 (8%) respondents had a variety of other comments, e.g., “I believe training would be important to ensure all providers are using terms and procedures consistently.”
We conducted a χ2 test of association between the occupation/role of the participants and their respective responses to the open-ended question. This revealed evidence of a weak association between occupation/role and responses to implementation of standardized dental diagnostic terms. The χ2 test yielded a value of 12.66 and a corresponding p-value of .058, which would be considered marginal significance. 64% of the participants who produced positive statements with respect to a standardized dental diagnostic terminology were dentists, dentist specialists, and dental hygienists compared to 32% of dental assistants and patient service representatives
DISCUSSION
The benefits of standardized diagnostic terms, such as the DDS terminology, have long been expounded and include enhancing our ability to perform epidemiological research, quality measurements and develop evidence-based guidelines, in addition to other efficient secondary data uses.10 Indeed, there has been an increasing public push for the use of standardized dental diagnostic terms, including by the American Dental Association.28 On the other hand, the threat of reimbursement tied to patient outcomes is a concern voiced by practitioners when the topic of diagnostic terms comes up. In the medical arena, diagnostic coding may indeed affect reimbursement from insurance carriers because the diagnosis determines the medical treatment code (CPT) upon which reimbursement is based. Requiring documentation of a dental diagnosis should however not create trepidation, as it should soundly underscore and explain why the specific treatment was chosen for the patient. Armed with these diagnostic terms, dental practices and the profession will be able quickly to answer questions like, “how many of our patients with localized moderate chronic periodontitis received treatment according to the AAP guidelines?”29, rather than just “how many scaling and root planing procedures did we do last month?” As is the case with any other innovation, the chasm between the potential and real benefits of a standardized diagnostic terminology is in large part defined by the attitudes and practices of the primary users: in short, if users do not utilize a diagnostic terminology, it cannot be useful. We, thus, sought to document the attitudes of dental team members in a large private practice with respect to the use of standardized dental diagnostic terms.
One challenge of an innovation like standardized dental diagnostic terms is that they are relatively abstract compared to, say, a panoramic radiograph machine. Indeed, of the open-ended responses, 16% reflected confusion about what a standardized dental diagnostic terminology entails. Clearly, education and training on the benefits, rationale, and use of the dental diagnostic terminology before implementation is one essential component of the implementation and dissemination of any standardized dental diagnostic terminology.
Looking globally at the results, the group surveyed had remarkably positive attitudes towards standardized dental diagnostic terms. Research has revealed that perceived usefulness is a strong determinant of usage intentions,19 and across the range of perceived usefulness questions, the individuals surveyed agreed that standardized dental diagnostic terms would be useful. We should not discount the supportive role of the sub-culture in which these dental care-team members work: the dental practice is a closed panel staff model dental practice with centralized leadership and a documented commitment to innovation as a core value. Respondents largely agreed that the “practice has supported the philosophy of dental diagnostic terms”. A milieu with these qualities would seem ripe for the implementation of standardized dental diagnostic terms, and indeed, this group practice went on recently to implement the DDS terminology. By contrast, if a practice were to identify that its team members were not so positively inclined toward an innovation like standardized dental diagnostic terms, the organization should work on understanding and influencing these views prior to the inevitable disruption of innovation implementation.
A number of responses expressed doubt about whether the use of standardized terms would improve patient care. This is especially relevant, as healthcare providers tend to be more reluctant to adopt innovative change that does not directly influence patient care.30 One way to deploy dental diagnostic terms to enhance patient care is to use them to drive clinical decision support that might, for instance, remind a dental care team when a patient requires scaling and root planning.
On the other hand, the responses to the open-ended questions reflected optimism that use of a standardized dental diagnostic terminology would enhance communication: over half of the respondents expressing positive views about a standardized dental diagnostic terminology mentioned communication as an issue. This could imply that lack of communication among providers or between patients and providers is a concern in the dental clinic environment. Beyond communication within the practice, communication between referring providers and referring medical physicians would be made more efficient with standardization of diagnostic terms. Standardized diagnostic terminologies will be indispensable in the age of interoperable electronic medical records, further facilitating the integration of oral health into general health.31
As with any innovation, the adoption and use of standardized dental diagnostic terms brings change. Entering diagnostic terms certainly leads to a shift in the provider’s workflow, a concern that was raised in the open-ended responses. Training is needed up-front to empower the entire dental care team to use the terminology correctly in the course of their busy days: this training should extend to include the front office staff as well as the direct clinical care team members, given the role that the office staff have in patient and payer interactions. Our goal, of course, is not that standardized dental diagnostic terms simply be used but that they are used correctly, and we need look no further than our medical colleagues to know there will likely be trials and tribulations assuring valid and complete use of terms. The DDS terminology creation and revision process has been grounded in tracking and optimizing valid use since its inception.9 While there may be advantages to having professional coders enter diagnostic terms, it is our belief that the team directly providing dental care to the patient is in the best position to do complete, high-fidelity diagnostic term entry. With this in mind, the attitudes and views of the dental care team take on elevated importance with respect to promoting the shift to widespread use of standardized dental diagnostic terms.
As demonstrated in our previous work, standardized dental diagnostic terms do not exist in a vacuum: they are accessible to the dental care team through the interface of the EHR, which influences user experience of the terms.15 To ensure that the EHR contributes rather than inhibits correct diagnostic term entry, authors EK, RR, OT, MW and JW have worked to refine the DDS terminology interface in the axiUm EHR (Exan Group) with support from the National Institutes of Dental and Craniofacial Research (5R01DE021051). AxiUm is the EHR in use at the group practice in which we conducted the survey (see the Appendix).
Challenges regarding change are not new. In the words of leadership guru John Kotter, “Guiding change may be the ultimate test of the leader – no business survives over the long term if it can’t reinvent itself.”32 As we advocate for the reinvention of the profession to one that systematically and correctly documents diagnostic terms, we will continue to track and learn from the private practice pioneers that are leading the way. The current study was conducted before implementing the DDS dental diagnostic terminology within the group practice. We believe that providers’ attitudes and beliefs will change after experiencing the DDS terminology in their EHR as part of their daily work. In future work, we will measure and report on updates in attitudes and beliefs regarding the use of a standardized dental diagnostic terminology.
CONCLUSION
The attitudes of end-users are strong predictors of the acceptance of an innovation. Before implementation of the DDS terminology in an American private dental group, this study examined attitudes and beliefs towards the use of a standardized dental diagnostic terminology among team members of a 54 private dental office practice. Most dental providers and staff showed positive attitudes towards the use of standardized terms, largely indicating that they believe that this innovation would be useful, particularly in terms of improving communication between the dentist and patient as well as among providers.
Acknowledgments
This research reported in this article was supported by grant R01 DE023061 from the National Institute of Dental & Craniofacial Research of the National Institutes of Health.
Appendix Survey Instrument Items
Perceived Usefulness
Ia = Standardized dental diagnostic terms would be useful.
Ib = Standardized dental diagnostic terms would improve the quality of care that I would deliver.
Ic = Standardized dental diagnostic terms would increase clinical productivity.
Id = Standardized dental diagnostic terms would enhance the effectiveness of providing care.
Ie = Standardized dental diagnostic terms would allow dental team members to use the same term to describe the same diagnosis.
Subjective Norms and Image
If = Clinicians, who influence my behavior, think that standardized dental diagnostic terms are important.
Ig = In general, LDG* has supported the philosophy of standardized dental diagnostic terms.
Ih = Standardized dental diagnostic terms allow clinicians to deliver better dental care than those who do not use them.
Job Relevance
Ii = Standardized dental diagnostic terms would be important to me as a dental clinic team member.
Result Demonstrability
Ij = I believe that I could communicate to others the impact of standardized dental diagnostic terms.
Ik = I would have difficulty explaining why standardized dental diagnostic terms are beneficial.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure. None of the authors reported any disclosures.
Contributor Information
Dr. Rachel B. Ramoni, Department of Oral Health Policy and Epidemiology, Harvard School of Dental Medicine, Boston, MA, Undiagnosed Diseases Coordinating Center, Harvard Medical School, Boston, MA.
Dr. Muhammad F. Walji, Department of Diagnostic and Biomedical Sciences, The University of Texas Health Science Center at Houston, School of Dentistry, Houston, Texas.
Dr. Soyun Kim, Department of Oral Health Policy and Epidemiology, Harvard School of Dental Medicine, Boston, MA.
Dr. Oluwabunmi Tokede, Department of Oral Health Policy and Epidemiology, Harvard School of Dental Medicine, Boston, MA.
Dr. Lyle McClellan, Willamette Dental Group, Hillsboro, OR.
Ms. Kristen Simmons, Willamette Dental Group, Hillsboro, OR.
Dr. Eugene Skourtes, Willamette Dental Group, Hillsboro, OR.
Dr. Alfa Yansane, Department of Oral Health Policy and Epidemiology, Harvard School of Dental Medicine, Boston, MA.
Dr. Joel M. White, Department of Preventive and Restorative Dental Sciences, School of Dentistry, University of California, San Francisco, CA.
Dr. Elsbeth Kalenderian, Department of Oral Health Policy and Epidemiology, Harvard School of Dental Medicine, Boston, MA, and chief of quality, Harvard Dental Center, Harvard School of Dental Medicine, Boston, MA.
References
- 1.O’Malley KJ, Cook KF, Price MD, et al. Measuring diagnoses: ICD code accuracy. Health services research. 2005;40(5 Pt 2):1620–39. doi: 10.1111/j.1475-6773.2005.00444.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller CS. Where are the diagnostic codes in dentistry? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(2):131–2. doi: 10.1016/j.tripleo.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 3.Bader JD. Challenges in quality assessment of dental care. J Am Dent Assoc. 2009;140(12):1456–64. doi: 10.14219/jada.archive.2009.0084. [DOI] [PubMed] [Google Scholar]
- 4.Garcia RI, Inge RE, Niessen L, DePaola DP. Envisioning success: the future of the oral health care delivery system in the United States. J Public Health Dent. 2010;70(Suppl 1):S58–65. doi: 10.1111/j.1752-7325.2010.00185.x. [DOI] [PubMed] [Google Scholar]
- 5.Dental Quality Alliance . Dental Quality Measurement in Dentsitry: A Guidebook. American Denta Association (ADA); Feb, 2012. [Google Scholar]
- 6.Leake JL. Diagnostic codes in dentistry--definition, utility and developments to date. J Can Dent Assoc. 2002;68(7):403–6. [PubMed] [Google Scholar]
- 7.National Committee on Vital and Health Statistics (NCVHS) Subcommittee on Standards and Security . SNODENT Update. American Dental Association; Chicago, Ill: 2004. [Google Scholar]
- 8.Leake JL, Main PA, Sabbah W. A system of diagnostic codes for dental health care. J Public Health Dent. 1999;59(3):162–70. doi: 10.1111/j.1752-7325.1999.tb03266.x. [DOI] [PubMed] [Google Scholar]
- 9.White JM, Kalenderian E, Stark PC, et al. Evaluating a dental diagnostic terminology in an electronic health record. Journal of Dental Education. 2011;75(5):605–15. [PMC free article] [PubMed] [Google Scholar]
- 10.Kalenderian E, Ramoni RL, White JM, et al. The development of a dental diagnostic terminology. Journal of Dental Education. 2011;75(1):68–76. [PMC free article] [PubMed] [Google Scholar]
- 11.Imel M, Campbell JR. Mapping from a Clinical Terminology to a Classification. American Health Information Management Association; Chicago, Il: [Accessed 10/7/2014]. 2003. http://library.ahima.org/xpedio/groups/public/documents/ahima/bok1_022744.hcsp?dDocName=bok1_022744. [Google Scholar]
- 12.Spackman KA, Campbell KE, Cote RA. SNOMED RT: a reference terminology for health care; Proceedings : a conference of the American Medical Informatics Association / … AMIA Annual Fall Symposium. AMIA Fall Symposium; 1997; pp. 640–4. [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenbloom ST, Miller RA, Johnson KB, Elkin PL, Brown SH. Interface terminologies: facilitating direct entry of clinical data into electronic health record systems. J Am Med Inform Assoc. 2006;13(3):277–88. doi: 10.1197/jamia.M1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tokede O, White J, Stark PC, et al. Assessing use of a standardized dental diagnostic terminology in an electronic health record. J Dent Educ. 2013;77(1):24–36. [PMC free article] [PubMed] [Google Scholar]
- 15.Walji MF, Kalenderian E, Tran D, et al. Detection and characterization of usability problems in structured data entry interfaces in dentistry. Int J Med Inform. 2013;82(2):128–38. doi: 10.1016/j.ijmedinf.2012.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989;13(3):319–40. [Google Scholar]
- 17.Holden RJ, Karsh BT. The technology acceptance model: its past and its future in health care. J Biomed Inform. 2010;43(1):159–72. doi: 10.1016/j.jbi.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adams D,A, Nelson R, Ryan, Todd P,A. Perceived Usefulness, Ease of Use, and Usage of Information Technology: A Replication. MIS Quarterly. 1992;16(2):227–47. [Google Scholar]
- 19.Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Management science. 2000:186–204. [Google Scholar]
- 20.Venkatesh V, Bala H. Technology Acceptance Model 3 and a research agenda on interventions. Decision Sciences. 2008;39(2):273–315. [Google Scholar]
- 21.Lederer AL, Maupin DJ, Sena MP, Zhuang Y. The technology acceptance model and the World Wide Web. Decision Support Systems. 2000;29:269–82. [Google Scholar]
- 22.Lee Y, Kozar KA, Larsen KRT. The Technology Acceptance Model: Past, Present and Future. Communications of the Association for Information Systems. 2003;12(50):752–80. [Google Scholar]
- 23.Wixom BH, Todd PA. A Theoretical Integration of User Satisfaction and Technology Acceptance. Information Systems Research. 2005;16(1):85–102. [Google Scholar]
- 24.Venkatesh V, Morris MG, Davis GB, Davis FD. User Acceptance of Information Technology: Toward a Unified View. MIS Quarterly. 2003;27(3):425–78. [Google Scholar]
- 25.Chismar WG, Wiley-Patton S. Test of the technology acceptance model for the internet in pediatrics. Proc AMIA Symp. 2002:155–9. [PMC free article] [PubMed] [Google Scholar]
- 26.Willis MJ, El-Gayar OF, Deokar AV. Evaluating Task-Technology Fit and User Performance for an Electronic Health Record System; Paper presented at: The Fifteenth Americas Conference on Information Systems; San Francisco, California. 2009. [Google Scholar]
- 27.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37(5):360–3. [PubMed] [Google Scholar]
- 28.American Dental Association . SNODENT Value and Benefit. American Dental Association; Chicago, Il: [Accessed 10/7/2014]. 2014. http://www.ada.org/en/member-center/member-benefits/practice-resources/dental-informatics/snodent/snodent-value-and-benefits. [Google Scholar]
- 29.Parameters of Care American Academy of Periodontology. J Periodontol. 2000;71(5 Suppl):i–ii. 847–83. doi: 10.1902/jop.2000.71.5-S.i. [DOI] [PubMed] [Google Scholar]
- 30.Van Der Meijden MJ, Tange HJ, Troost J, Hasman A. Determinants of success of inpatient clinical information systems: a literature review. J Am Med Inform Assoc. 2003;10(3):235–43. doi: 10.1197/jamia.M1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giddon DB, Swann B, Donoff RB, Hertzman-Miller R. Dentists as oral physicians: the overlooked primary health care resource. J Prim Prev. 2013;34(4):279–91. doi: 10.1007/s10935-013-0310-7. [DOI] [PubMed] [Google Scholar]
- 32.Kotter JP. Leading Change: Why Transformation Efforts Fail. Harvard Business Review. 2007 Jan;:1–9. [Google Scholar]