Abstract
Osteopontin (OPN), a malignancy-associated secreted phosphoprotein, is a prognostic plasma biomarker for survival in metastatic breast cancer patients. We evaluated the role of OPN in Locally Advanced Breast Cancer (LABC) patients in predicting response to neoadjuvant chemotherapy and association with survival. Fifty-three patients with non-metastatic LABC were enrolled in this study and monitored serially for plasma OPN levels by ELISA during neoadjuvant chemotherapy prior to surgery. For fifty patients who had baseline OPN levels available for analysis, the median baseline OPN level was 63.6 ng/ml. Median patient follow up was 45 months and thirteen patients died from metastatic disease. Patients with baseline OPN levels ≥ 63.6 ng/ml were significantly more likely to die of their disease than those with baseline OPN < 63.6 ng/mL (Hazard Ratio = 3.4; 95% confidence interval 1.4-11.3; P = 0.011), and overall, baseline OPN level was significantly associated with survival (P = 0.002). There was little support for value of serial OPN determination in monitoring response to therapy in this patient population. Although the percentage of patients with baseline OPN levels < 63.6 ng/ml was higher in patients with pathological complete response than in those with no response, the difference was not statistically significant (64% and 14%, respectively (P = 0.066)). Thus, baseline plasma OPN level is a prognostic biomarker in this group of LABC patients, and could also be helpful in identifying LABC patients who will respond to neoadjuvant chemotherapy. Our results call for validation of our findings in large prospective trial data sets.
Keywords: Locally advanced breast cancer, neoadjuvant therapy, osteopontin, prognostic biomarker, predictive biomarker
Introduction
Locally advanced breast cancer (LABC) is considered an aggressive and advanced stage of non-metastatic breast cancer, accounting for approximately 5-15% of all breast cancer cases [1-3], with a five year overall survival rate of ~50% [3-6]. Current treatment for LABC is multimodal, involving neoadjuvant chemotherapy, surgery and radiotherapy [7,8]. Approximately 10%-20% of patients will achieve a clinical complete response (CR) and 50%-60% will achieve a partial response (PR) to neoadjuvant therapy. However, only one half to two-thirds of clinical CRs will be confirmed pathologically (pathological complete response, pCR, defined as no residual invasive breast cancer in the surgical specimen [1]). Response to neoadjuvant chemotherapy allows clinicians to identify patients who may have a good outcome, as pCR remains the best predictor for long-term survival [6,9].
Osteopontin (OPN) is a secreted, integrin-binding phosphoprotein that is expressed by several normal tissues and cell types [10,11]. OPN plays an important role in various aspects of malignancy, particularly those involved in tissue invasion and metastasis [10,12-18], and OPN levels have been associated with aggressiveness in several cancer types, including breast cancer.
We, as well as other groups, have shown by immunohistochemistry that elevated levels of OPN found in primary tumors may be correlated with a poor patient prognosis and tumor stage [19-21]. OPN can also be detected in the blood of patients with various forms of cancer, including breast, prostate, colon, lung, liver and stomach cancer and can be measured using an ELISA (enzyme-linked immunosorbent assay) [22-27]. Plasma OPN levels are found to be elevated in a majority of metastatic breast cancer patients and increased baseline levels of plasma OPN in metastatic breast cancer patients are associated with a worse prognosis and increased tumor burden [23,25]. Additionally, in metastatic breast cancer patients monitored by serial OPN blood levels, survival decreases (despite treatment) as plasma OPN levels increase over time [23,25]. Plasma OPN may thus have both a prognostic and a predictive role in metastatic breast cancer, making monitoring plasma OPN levels from metastatic breast cancer patients throughout treatment and over their disease course potentially useful to predict aggressive tumor behavior. In contrast, we recently reported data obtained for early breast cancer patients that failed to show prognostic value for baseline plasma levels in those patients, although we did find elevated plasma OPN in post-baseline samples from a subset of patients [26].
The present study is, to our knowledge, the first study to measure plasma OPN serially in LABC patients. Serial measurement of plasma OPN levels over treatment may potentially provide information with respect to patient response to neoadjuvant therapy and long-term survival. The ability to more accurately monitor response to neoadjuvant therapy may lead to better management of these patients.
Methods
Patient enrollment and treatment course
Fifty-two female patients and one male patient diagnosed with LABC, being treated at the London Regional Cancer Program in London, Ontario, Canada, were enrolled during 2007-2011 into this study, which was approved by the Western University Health Sciences Research Ethics Board. All patients had a histologically confirmed clinical stage III breast cancer and were eligible for neoadjuvant therapy, excluding inflammatory breast cancer or patients with distant metastases. Patients with any prior history of invasive cancer or prior chemotherapy or radiotherapy were excluded. All patients provided written informed consent to participate in this study and to its results being published. No eligible patients declined participation. Patients received one of two standard neoadjuvant chemotherapy regimens: AC-T (doxorubicin 60 mg/m2 and cyclophosphamide 500 mg/m2 IV q3 weekly × 4 cycles followed by docetaxel 100 mg/m2 IV q3 weekly × 4 cycles) or FEC-D (5-fluorouracil 500 mg/m2, epirubicin 100 mg/m2 and cyclophosphamide 500 mg/m2 IV q3 weekly × 3 cycles followed by docetaxel 35 mg/m2 q weekly × 9 cycles). The patients receiving FEC-D received their regional external beam conformal radiotherapy (45 Gy in 25 fractions plus 5.4 Gy in 3 fractions or 9 Gy in 5 fractions depending on disease burden) concurrent with docetaxel therapy in the neoadjuvant setting versus identical radiotherapy in the adjuvant setting for AC-T patients. Neoadjuvant therapy was followed by modified radical mastectomy to remove the breast and axillary lymph nodes, which were examined pathologically. All surviving patients were followed for at least 2.5 years. The male patient died unexpectedly following chemotherapy cycle 2. Three female patients became metastatic during neoadjuvant therapy. Patient characteristics as well as tumor characteristics and subsequent occurrence of metastases during or after neoadjuvant therapy are listed in Table 1. All patients were followed prospectively and none were lost to follow-up.
Table 1.
Patient and tumor characteristics and sites of metastasis
| OPN number | Age at baseline | Gender | Tstage | Nstage | ER | PR | HER2 | Grade | Site of metastases |
|---|---|---|---|---|---|---|---|---|---|
| 01 | 53 | F | T3 | N1 | Pos | Pos | Pos | 2 | 0 |
| 02 | 52 | F | T4a | N0 | Unk | Unk | Unk | 1 | 0 |
| 03 | 68 | F | T4b | N1 | Pos | Pos | Neg | 1 | 0 |
| 04 | 52 | F | NA | NA | Pos | Pos | Neg | 3 | 0 |
| 05 | 50 | F | T4b | N1 | Pos | Neg | Pos | 3 | Liver |
| 06 | 64 | F | T3 | N1 | Pos | Neg | Equiv | 2 | 0 |
| 07 | 59 | F | T4b | N1 | Neg | Neg | Pos | 3 | Lung |
| 08 | 47 | F | T4b | N1 | Pos | Pos | Neg | 3 | Liver |
| 09 | 56 | F | T2 | N1 | Neg | Neg | Pos | 3 | 0 |
| 10 | 44 | F | T3 | N1 | Neg | Neg | Pos | 3 | 0 |
| 11 | 42 | F | T4b | N1 | Pos | pos | Neg | 3 | Lung/Liver/Bone |
| 12 | 76 | M | T4b | NX | Unk | Unk | Unk | 2 | Unk |
| 13 | 67 | F | T3 | N0 | Pos | Pos | Neg | 1 | 0 |
| 14 | 64 | F | T4b | N1 | Pos | Pos | Pos | 1 | Liver |
| 15 | 39 | F | T2 | N1 | Pos | Pos | Pos | 2 | Brain/Liver/Lung/Bone |
| 16 | 46 | F | T3 | N0 | Pos | Pos | Neg | 2 | 0 |
| 17 | 42 | F | T3 | N1 | Neg | Neg | Pos | 3 | Lung |
| 18 | 48 | F | T3 | N1 | Pos | Pos | Neg | 1 | 0 |
| 19 | 53 | F | T4b | N0 | Neg | Neg | Pos | 3 | 0 |
| 20 | 47 | F | T4b | N1 | Neg | Neg | Neg | 3 | 0 |
| 21 | 44 | F | T1c | N2 | Neg | Neg | Pos | 3 | 0 |
| 22 | 38 | F | T2 | N0 | Neg | Neg | Pos | 3 | 0 |
| 23 | 62 | F | T2 | N1 | Neg | Neg | Pos | 3 | Brain |
| 24 | 26 | F | T2 | N1 | Neg | Neg | Neg | 3 | 0 |
| 25 | 58 | F | T3 | N2 | Pos | Pos | Pos | 3 | 0 |
| 26 | 43 | F | T2 | N1 | Pos | Pos | Pos | 2 | 0 |
| 27 | 52 | F | T2 | N2 | Pos | Pos | Pos | 2 | 0 |
| 28 | 49 | F | T3 | N2a | Pos | Pos | Pos | 2 | 0 |
| 29 | 63 | F | T3 | N1 | Neg | Neg | Neg | 3 | 0 |
| 30 | 48 | F | T3 | N1 | Pos | Pos | Neg | 2 | 0 |
| 31 | 61 | F | T3 | N1 | Pos | Pos | Neg | 3 | 0 |
| 32 | 39 | F | T3 | N1 | Pos | Pos | Neg | 2 | Lung |
| 33 | 43 | F | T3 | N0 | Neg | Neg | Pos | 2 | 0 |
| 34 | 47 | F | T3 | N0 | Pos | Pos | Neg | 2 | 0 |
| 35 | 49 | F | T2 | N0 | Neg | Neg | Neg | 3 | Bone |
| 36 | 64 | F | T3 | N2 | Pos | Neg | Neg | 2 | Bone |
| 37 | 34 | F | T3 | N3 | Neg | Neg | Neg | 3 | 0 |
| 38 | 40 | F | T2 | N1 | Pos | Pos | Neg | 1 | 0 |
| 39 | 58 | F | T1 | N3 | Pos | Pos | Pos | 3 | 0 |
| 40 | 42 | F | T2 | N0 | Pos | Pos | Neg | 2 | 0 |
| 41 | 53 | F | T3 | N0 | Neg | Neg | Neg | 3 | 0 |
| 42 | 44 | F | T3 | N1 | Pos | Pos | Pos | 2 | 0 |
| 43 | 45 | F | T3 | N0 | Pos | Neg | Neg | 2 | 0 |
| 44 | 57 | F | T2 | N0 | Pos | Neg | Pos | 3 | 0 |
| 45 | 60 | F | T3 | N0 | Pos | Pos | Neg | 2 | bone |
| 46 | 50 | F | T3 | N2 | Neg | Neg | Neg | 3 | lung |
| 47 | 44 | F | T3 | N1 | Pos | Pos | Neg | 1 | 0 |
| 48 | 45 | F | T3 | N1 | Pos | Pos | Neg | 2 | 0 |
| 49 | 62 | F | T3 | N2a | Pos | Neg | Pos | 3 | 0 |
| 50 | 51 | F | T3 | NX | Pos | Pos | Pos | 2 | 0 |
| 51 | 58 | F | T2 | N1 | Pos | Pos | Pos | 3 | 0 |
| 52 | 31 | F | T2 | N3 | Pos | Pos | Pos | 3 | 0 |
| 53 | 62 | F | T2 | N3 | Pos | Pos | Neg | 2 | 0 |
ER, estrogen receptor; equiv, equivocal; NA, non available; neg, negative; pos, positive; PR, progesterone receptor; unk, unknown.
Plasma sample collection and OPN analysis
Blood samples for OPN measurement were collected in tubes with EDTA anticoagulant and processed as previously reported [22]. OPN was measured in plasma samples by ELISA (Human Osteopontin EIA Kit, catalogue #ADI-900-142, Enzo Life Sciences, Ann Arbor, MI) as previously described [27]. Samples were collected at baseline (just prior to the first cycle of chemotherapy) and again just prior to each subsequent chemotherapy cycle treatment or every three weeks throughout neoadjuvant treatment for patients receiving their docetaxel weekly, followed by one sample collected pre-operatively. Plasma OPN values from 90 healthy women were as previously reported [26].
Pathological assessment
Surgical specimens were sent for final pathological assessment. Tumor response to neoadjuvant chemotherapy was substratified as follows [28]:
i) Complete pathological response (pCR) (No evidence of residual invasive tumor in breast or axilla).
ii) Partial response (PR) (at least a 30% decrease in residual tumor volume).
iii) No evidence of response (stable disease) (SD).
iv) Progression of disease (PD) (at least a 20% increase in residual tumor volume).
Statistical analysis
Population OPN levels were characterized with Box plots for OPN in healthy women and LABC patients at baseline. Repeated measures analysis of variance was used to compare OPN levels across cycles of treatment, with Dunnet’s multiple comparisons test used to make pair-wise comparisons between cycle 1 and subsequent cycles. The effect of baseline OPN on overall survival was evaluated using Cox regression. Patients were categorized according to the median baseline OPN and the Kaplan-Meier technique was used to estimate survival. The two groups were compared using the log-rank statistic and hazard ratios were estimated using Cox regression. The relationship between baseline OPN levels and response to chemotherapy was evaluated using Fisher’s exact test and the Mann-Whitney-test. The relationship between serial OPN levels during neoadjuvant chemotherapy and response was evaluated using Fisher’s exact test. SAS 9.3 was used for all statistical analyses (SAS Institute Inc., Cary NC). P-values less than 0.05 were considered to be statistically significant.
Results
Plasma OPN levels in ng/ml for each patient over the course of neoadjuvant chemotherapy are shown in Figure 1. Patient 12, who was the only male in the study, died following the second cycle of chemotherapy from what appeared to be treatment-related toxicity. A baseline OPN level of 69.7 ng/ml was measured and at cycle two, just prior to his death, OPN level was elevated to 141.3 ng/ml. The two OPN values for this patient were not used for the following analyses.
Figure 1.
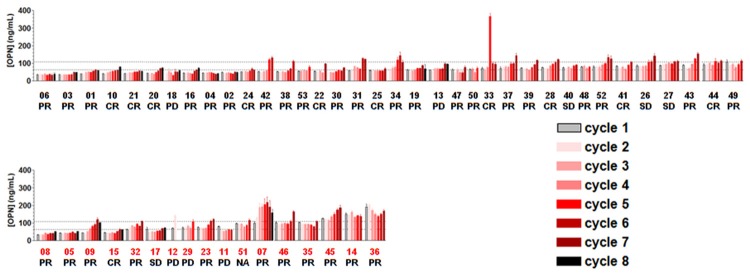
Plasma OPN levels (ng/ml) during neoadjuvant therapy with final response to treatment and survival for all 53 LABC patients. At every treatment cycle plasma samples were obtained and OPN was measured in triplicate by ELISA. Average OPN levels are shown in ng/ml. Final patient response is denoted as complete response (CR), partial response (PR), stable disease (SD) or progressive disease (PD). Patient numbers (see Table 1) in black (upper panel) indicate patients who are alive and red (lower panel) numbers indicate patients who have died. Patients in each panel are grouped according to increasing baseline OPN, except patients for which no baseline OPN was obtained in which case OPN at cycle 2 was used. Patient 12 is a male patient who died following 2 neoadjuvant cycles. The dotted lines indicate upper limit of OPN levels in a cohort of 90 healthy women (108.6 ng/mL) [26] and median value at baseline/cycle 1 (63.6 ng/mL), respectively.
OPN values at baseline/cycle 1 were obtained for 50 patients. Mean OPN value was 70.3 ng/ml at baseline/cycle 1, while median value was 63.6 ng/mL (range 33.3-189.8). We have previously measured plasma OPN levels of 90 healthy women and found a mean value of 32.0 ng/mL (median value 26.3 ng/ml (range 11.8-108.6 ng/ml) [26] (Figure 2).
Figure 2.
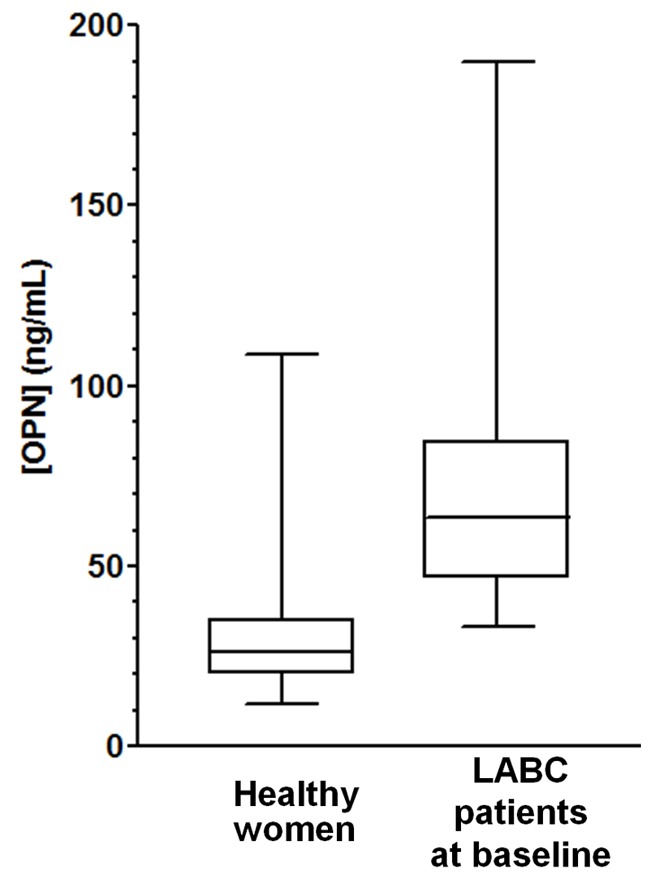
Plasma OPN levels at baseline of 50 patients with LABC compared to OPN levels of 90 healthy women. The boxes show OPN values between the 25th and 75th percentiles, with whiskers showing ranges; lines within the boxes mark the median values. OPN values from healthy women were as reported [26].
OPN levels across 7 cycles of neoadjuvant treatment were compared for the 34 patients for whom we had a complete set using repeated measures analysis of variance which was significant overall (P < 0.001). Although differences in patient plasma OPN levels between cycles 1 (baseline) and cycles 2 through 4 were non-significant, differences between cycles 1 and 5, cycles 1 and 6, and between cycles 1 and 7 were statistically significant (P < 0.05, P < 0.001, and P < 0.001, respectively, (Supplemental Figure 1). Overall, all but three baseline samples as well as the majority of samples from cycles 2-8 have OPN values within the normal range (i.e. ≤ 108.6 ng/ml) (Figure 1).
Association between baseline OPN values and overall survival
Baseline OPN, when treated as a continuous variable, was found to be significantly associated with overall survival (P = 0.002). To further evaluate the association of OPN values with overall survival, the LABC patients were divided into 2 groups: OPN < 63.6 ng/ml vs. OPN ≥ 63.6 ng/ml, the median OPN value at baseline. We noted that by comparison, the majority (92%) of healthy women had OPN values < 63.6 ng/ml. The Kaplan-Meier survival curve indicates that patients with baseline OPN ≥ 63.6 ng/ml were more likely to die of their disease than patients with baseline OPN < 63.6 (Figure 3). The log rank test showed that this difference was statistically significant (P = 0.011; Hazard Ratio 3.4; 95% confidence interval: 1.4-11.3).
Figure 3.
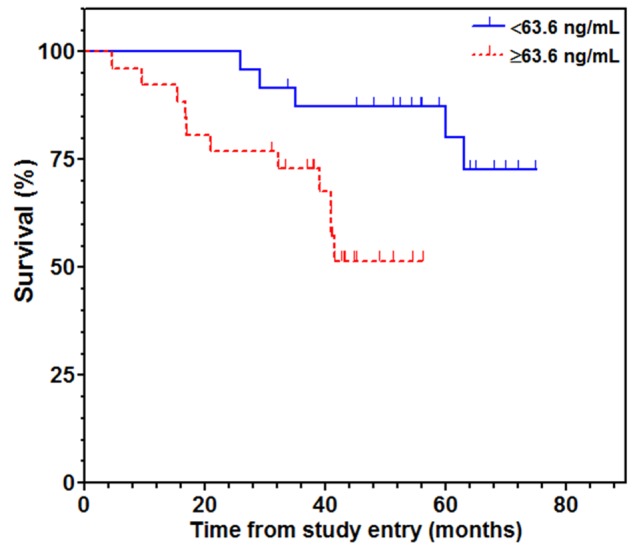
Association of plasma OPN concentrations at baseline with LABC patient survival. Kaplan-Meier survival curves were constructed after dividing the patients into two groups according to the median OPN value at baseline/cycle 1 (63.6 ng/mL). (log-rank test; P = 0.011).
Association of OPN values with response to neoadjuvant therapy
The majority of the female LABC patients (62% or 32 out of 52) had a PR to neoadjuvant therapy; eleven patients (21%) had a CR, four patients (8%) had PD and four individuals (8%) had SD (Figure 1). Plasma OPN levels at baseline were compared with the final pathologic response to neoadjuvant chemotherapy. The median OPN value at baseline/cycle 1 for patients with CR was 55.5 ng/ml, while for patients with no response to neoadjuvant therapy (SD or PD), the median OPN value was higher at 75.8 ng/ml (Figure 4), however this difference was not statistically significant (P = 0.057). Mean OPN values at baseline were also higher for non-responders than for patients with complete response (75.1 ng/mL vs 60.0 ng/mL). Although the percentage of patients with baseline OPN levels < 63.6 ng/ml was higher for patients with pCR (seven out of eleven, 64%) than for those with no response (one out of seven, 14%), the difference was not statistically significant (P = 0.066). As noted above, serial OPN measurements showed an increase in OPN levels during successive cycles of neoadjuvant chemotherapy. There was no relationship between variations in OPN levels during neoadjuvant therapy and patient response (P = 0.586).
Figure 4.
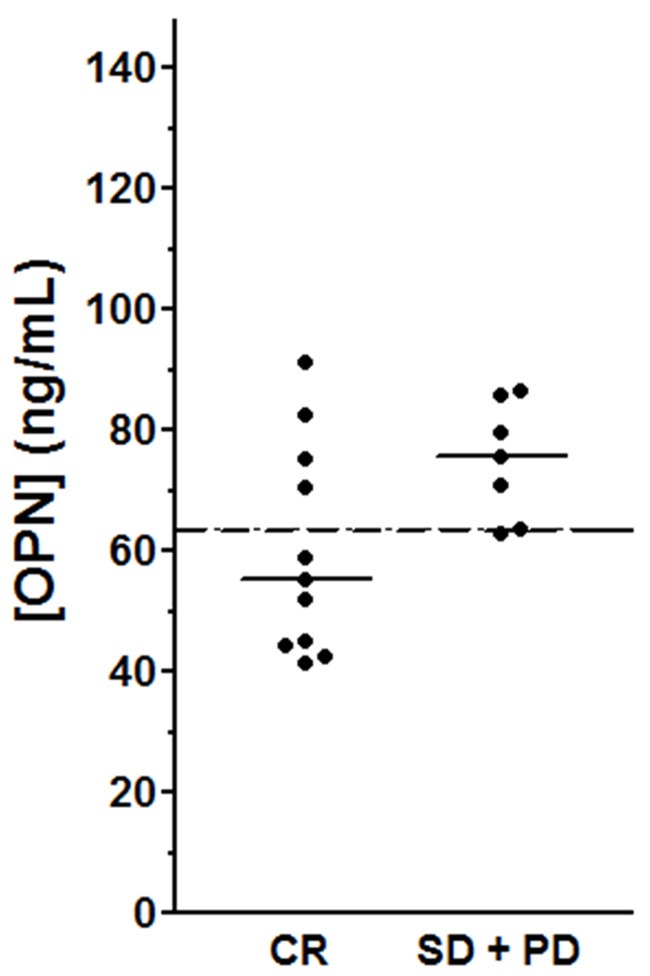
OPN levels at baseline for complete responders and non-responders to neoadjuvant treatment. Lines indicate median OPN value for eleven patients with pCR (55.5 ng/ml) and median OPN value for seven patients with SD or PD was (75.8 ng/ml) (P = 0.054). Dashed line indicates the median OPN value at baseline (63.6 ng/mL) of the entire group of patients.
Association of response to neoadjuvant therapy and survival
Patients that were responders (pCR or PR) did not differ from non-responders (SD or PD) in terms of survival (P = 0.518). We also compared survival of the eight patients that did not respond to neoadjuvant treatment to the survival of the eleven patients that had pCR (Supplemental Figure 2). Although the median survival rate of patients with pCR was higher, the difference was not significant (P = 0.083).
Discussion
Tumor response to neoadjuvant treatment is a predictor of prognosis and overall survival for the LABC patient population. In the current study, both baseline plasma OPN and serial plasma OPN levels were evaluated as a novel method for determining prognosis and monitoring tumor response to neoadjuvant chemotherapy of LABC patients. We found that baseline OPN was valuable prognostically in terms of relationship with overall survival, and there was a trend towards association between plasma OPN at baseline and response to neoadjuvant therapy. In contrast, there was little support for value of serial OPN determination in monitoring response to therapy in this patient population.
Our results show that during the course of neoadjuvant treatment, as the patients receive additional cycles of chemotherapy, a statistically significant increase is seen in OPN levels at later cycles (5-7) compared to earlier cycles (1-4). This increase in plasma OPN levels during neoadjuvant chemotherapy occurred for most patients, regardless of response. Thus serial measurements may be of limited value in determining response of LABC patients to neoadjuvant chemotherapy. Cytotoxic chemotherapies that are used for cancer treatment can stimulate the immune system. Up-regulation of OPN expression in immune cells allows for increased macrophage adhesion, migration, cytokine release and phagocytosis, all of which are important events of the immune and inflammatory response [29,30]. Therefore, it is possible that the increased plasma OPN levels observed in patients over the course of neoadjuvant chemotherapy is from two different sources: OPN expressed by immune cells as a component of the inflammatory response, and that secreted by the primary tumor itself [14,19,26]. Further work is required in order to determine the exact source of plasma OPN detected during treatment.
We have recently reported that, in a group of 90 healthy women, plasma OPN levels ranged from 11.8-108.6 ng/ml [26]. Based on this, a level of 108.6 ng/ml has been used as the upper limit of normal in the present study and OPN levels above this value were considered elevated. We have previously shown that in a cohort of 70 patients with metastatic breast cancer, 70% had elevated levels of OPN [23] and that patients with increased plasma OPN levels had significantly shorter survival times. In line with this, Bramwell et al. [25] reported that in a larger cohort of women with metastatic breast cancer, 66% had elevated baseline OPN levels that were inversely and significantly associated with survival. In addition, serial monitoring of OPN levels revealed that in that cohort of patients an increase of > 250 ng/ml at any time was the most prognostic variable for poor survival. This association of increasing OPN levels over time with poor prognosis supported the use of serial monitoring of OPN levels in order to help make treatment decisions by determining response. The majority (73%) of that group of metastatic patients was not receiving systemic chemotherapy. We suggest that one reason we were able to see prognostic value for increasing OPN levels in the metastatic patients but not for the LABC patients is that there was not the confounding variable of host response to systemic therapy at the same time. In a cohort of postmenopausal women with early breast cancer, only 4 women out of 314 (1.2%) had elevated OPN (> 108.6 ng/ml) at baseline (Supplemental Figure 2) [26]. It indicated that a mean baseline plasma OPN of 46 ng/ml (range 22.6-290), which did not differ statistically from normal levels [26], did not support a prognostic value of plasma OPN for early breast cancer patients. There was, however, evidence of higher mean OPN plasma levels in some patients post-baseline, compared to baseline OPN levels for those patients, suggesting a utility for obtaining serial plasma samples. While plasma OPN levels have thus been reported to be elevated in women with metastatic disease but not with early breast cancer, levels for patients with locally advanced disease had not been previously studied. Our results presented here show that most LABC patients have plasma OPN levels that are not elevated above the normal range at baseline.
When comparing baseline OPN levels to final pathologic response, we found a trend towards a higher median OPN level (75.8 ng/ml) for patients who did not respond to treatment compared to the group of eleven patients who had pCR to treatment (55.5 ng/ml) (P = 0.057). The majority of non-responders also had OPN values ≥ 63.6 ng/ml at baseline, while the majority of patients with pCR had OPN values < 63.6 ng/ml at baseline (P = 0.066). These differences, although not reaching statistical significance in this group of patients, are clinically interesting as they may help identify which patients are likely to respond to neoadjuvant chemotherapy, and are worthy of further study. Although there is evidence in the literature for an association between achievement of pCR to neoadjuvant chemotherapy and molecular subtype [31], our present study is not designed to assess this. Nevertheless, the surrogate for outcome (pCR) is less relevant given the relationship that was identified between baseline OPN and survival. Future studies with larger sample sizes will be able to examine any relationships between OPN levels and molecular subtype, which could be clinically useful when determining patient prognosis at baseline.
Importantly, our results show a clear association between baseline OPN levels and survival. Log-rank test and Cox proportional hazards regression revealed that patients with baseline OPN levels above the median were significantly more likely to die of their disease than those with baseline OPN levels below the median (hazard ratio = 3.4; 95% confidence interval 1.4 - 11.3; P = 0.011), and that overall, baseline OPN level was significantly associated with survival (P = 0.002). Therefore, OPN represents the first known prognostic plasma tumor biomarker for overall survival in both locally advanced and metastatic breast cancer patients.
Conclusions
LABC patients have a poor overall prognosis, due to their high risk of tumor recurrence and development of future metastases. The study reported here demonstrates a statistically significant difference in survival between patients according to baseline plasma OPN levels, and a trend towards association of baseline OPN levels and response to neoadjuvant therapy. In this group of patients, baseline OPN is superior over response to neoadjuvant therapy as a prognostic biomarker. Our results strongly support the need for prospective clinical trials to further validate the utility of measuring plasma OPN levels in LABC patients.
Acknowledgements
Supported by awards from the Lloyd Carr-Harris Foundation and the London Regional Cancer Program.
Disclosure of conflict of interest
AFC received in-kind research support and royalties from Enzo Life Sciences Inc., for sale of OPN antibody products. The other authors have no competing interests to disclose.
Supporting Information
References
- 1.Giordano SH. Update on locally advanced breast cancer. Oncologist. 2003;8:521–530. doi: 10.1634/theoncologist.8-6-521. [DOI] [PubMed] [Google Scholar]
- 2.Chia S, Swain SM, Byrd DR, Mankoff DA. Locally Advanced and Inflammatory Breast Cancer. J. Clin. Oncol. 2008;26:786–790. doi: 10.1200/JCO.2008.15.0243. [DOI] [PubMed] [Google Scholar]
- 3.Newman LA. Epidemiology of locally advanced breast cancer. Semin Radiat Oncol. 2009;19:195–203. doi: 10.1016/j.semradonc.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Valero VV, Buzdar AU, Hortobagyi GN. Locally Advanced Breast Cancer. Oncologist. 1996;1:8–17. [PubMed] [Google Scholar]
- 5.Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, Feuer EJ, Thun MJ American Cancer Society. Cancer Statistics, 2004. CA Cancer J Clin. 2004;54:8–29. doi: 10.3322/canjclin.54.1.8. [DOI] [PubMed] [Google Scholar]
- 6.Yalcin B. Overview on locally advanced breast cancer: defining, epidemiology, and overview on neoadjuvant therapy. Exp Oncol. 2013;35:250–252. [PubMed] [Google Scholar]
- 7.Kaufmann M, Hortobagyi GN, Goldhirsch A, Scholl S, Makris A, Valagussa P, Blohmer JU, Eiermann W, Jackesz R, Jonat W, Lebeau A, Loibl S, Miller W, Seeber S, Semiglazov V, Smith R, Souchon R, Stearns V, Untch M, von Minckwitz G. Recommendations from an international expert panel on the use of neoadjuvant (primary) systemic treatment of operable breast cancer: an update. J Clin Oncol. 2006;24:1940–1949. doi: 10.1200/JCO.2005.02.6187. [DOI] [PubMed] [Google Scholar]
- 8.Gralow JR, Burstein HJ, Wood W, Hortobagyi GN, Gianni L, von Minckwitz G, Buzdar AU, Smith IE, Symmans WF, Singh B, Winer EP. Preoperative therapy in invasive breast cancer: pathologic assessment and systemic therapy issues in operable disease. J Clin Oncol. 2008;26:814–819. doi: 10.1200/JCO.2007.15.3510. [DOI] [PubMed] [Google Scholar]
- 9.Alm El-Din MA, Taghian AG. Breast conservation therapy for patients with locally advanced breast cancer. Semin Radiat Oncol. 2009;19:229–235. doi: 10.1016/j.semradonc.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 10.Wai PY, Kuo PC. The role of Osteopontin in tumor metastasis. J Surg Res. 2004;121:228–241. doi: 10.1016/j.jss.2004.03.028. [DOI] [PubMed] [Google Scholar]
- 11.Rangaswami H, Bulbule A, Kundu GC. Osteopontin: role in cell signaling and cancer progression. Trends Cell Biol. 2006;16:79–87. doi: 10.1016/j.tcb.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Tuck AB, Chambers AF, Allan AL. Osteopontin overexpression in breast cancer: knowledge gained and possible implications for clinical management. J Cell Biochem. 2007;102:859–868. doi: 10.1002/jcb.21520. [DOI] [PubMed] [Google Scholar]
- 13.Rittling SR, Chambers AF. Role of osteopontin in tumour progression. Br J Cancer. 2004;90:1877–1881. doi: 10.1038/sj.bjc.6601839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anborgh PH, Mutrie JC, Tuck AB, Chambers AF. Role of the metastasis-promoting protein osteopontin in the tumour microenvironment. J Cell Mol Med. 2010;14:2037–2044. doi: 10.1111/j.1582-4934.2010.01115.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allan AL, George R, Vantyghem SA, Lee MW, Hodgson NC, Engel CJ, Holliday RL, Girvan DP, Scott LA, Postenka CO, Al-Katib W, Stitt LW, Uede T, Chambers AF, Tuck AB. Role of the integrin-binding protein osteopontin in lymphatic metastasis of breast cancer. Am J Pathol. 2006;169:233–246. doi: 10.2353/ajpath.2006.051152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tuck AB, Hota C, Chambers AF. Osteopontin(OPN)-induced increase in human mammary epithelial cell invasiveness is urokinase (uPA)-dependent. Breast Cancer Res Treat. 2001;70:197–204. doi: 10.1023/a:1013095329825. [DOI] [PubMed] [Google Scholar]
- 17.Furger KA, Allan AL, Wilson SM, Hota C, Vantyghem SA, Postenka CO, Al-Katib W, Chambers AF, Tuck AB. Beta(3) integrin expression increases breast carcinoma cell responsiveness to the malignancy-enhancing effects of osteopontin. Mol Cancer Res. 2003;1:810–819. [PubMed] [Google Scholar]
- 18.Xuan JW, Hota C, Shigeyama Y, D’Errico JA, Somerman MJ, Chambers AF. Sitedirected mutagenesis of the arginine-glycine-aspartic acid sequence in osteopontin destroys cell adhesion and migration functions. J Cell Biochem. 1995;57:680–690. doi: 10.1002/jcb.240570413. [DOI] [PubMed] [Google Scholar]
- 19.Tuck AB, O’Malley FP, Singhal H, Harris JF, Tonkin KS, Kerkvliet N, Saad Z, Doig GS, Chambers AF. Osteopontin expression in a group of lymph node negative breast cancer patients. Int J Cancer. 1998;79:502–508. doi: 10.1002/(sici)1097-0215(19981023)79:5<502::aid-ijc10>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 20.Rudland PS, Platt-Higgins A, El-Tanani M, De Silva Rudland S, Barraclough R, Winstanley JH, Howitt R, West CR. Prognostic significance of the metastasis associated protein osteopontin in human breast cancer. Cancer Res. 2002;62:3417–3427. [PubMed] [Google Scholar]
- 21.Coppola D, Szabo M, Boulware D, Muraca P, Alsarraj M, Chambers AF, Yeatman TJ. Correlation of osteopontin protein expression and pathological stage across a wide variety of tumor histologies. Clin Cancer Res. 2004;10:184–190. doi: 10.1158/1078-0432.ccr-1405-2. [DOI] [PubMed] [Google Scholar]
- 22.Bautista DS, Saad Z, Chambers AF, Tonkin KS, O’Malley FP, Singhal H, Tokmakejian S, Bramwell V, Harris JF. Quantification of osteopontin in human plasma with an ELISA: basal levels in pre- and postmenopausal women. Clin Biochem. 1996;29:231–239. doi: 10.1016/0009-9120(96)84728-a. [DOI] [PubMed] [Google Scholar]
- 23.Singhal H, Bautista DS, Tonkin KS, O’Malley FP, Tuck AB, Chambers AF, Harris JF. Elevated plasma osteopontin in metastatic breast cancer associated with increased tumor burden and decreased survival. Clin Cancer Res. 1997;3:605–611. [PubMed] [Google Scholar]
- 24.Hotte SJ, Winquist EW, Stitt L, Wilson SM, Chambers AF. Plasma osteopontin: associations with survival and metastasis to bone in men with hormone-refractory prostate carcinoma. Cancer. 2002;95:506–512. doi: 10.1002/cncr.10709. [DOI] [PubMed] [Google Scholar]
- 25.Bramwell VH, Doig GS, Tuck AB, Wilson SM, Tonkin KS, Tomiak A, Perera F, Vandenberg TA, Chambers AF. Serial plasma osteopontin levels have prognostic value in metastatic breast cancer. Clin Cancer Res. 2006;12:3337–3343. doi: 10.1158/1078-0432.CCR-05-2354. [DOI] [PubMed] [Google Scholar]
- 26.Bramwell VH, Tuck AB, Chapman JA, Anborgh PH, Postenka CO, Al-Katib W, Shepherd LE, Han L, Wilson CF, Pritchard KI, Pollak MN, Chambers AF. Assessment of osteopontin in early breast cancer: correlative study in a randomised clinical trial. Breast Cancer Res. 2014;16:R8. doi: 10.1186/bcr3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anborgh PH, Wilson SM, Tuck AB, Winquist E, Schmidt N, Hart R, Kon S, Maeda M, Uede T, Stitt LW, Chambers AF. New dual monoclonal ELISA for measuring plasma osteopontin as a biomarker associated with survival in prostate cancer: clinical validation and comparison of multiple ELISAs. Clin Chem. 2009;55:895–903. doi: 10.1373/clinchem.2008.117465. [DOI] [PubMed] [Google Scholar]
- 28.Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 29.Denhardt DT, Noda M, O’Regan AW, Pavlin D, Berman JS. Osteopontin as a means to cope with environmental insults: regulation of inflammation, tissue remodeling and cell survival. J Clin Invest. 2001;107:1055–1061. doi: 10.1172/JCI12980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Giachelli CM, Steitz S. Osteopontin: a versatile regulator of inflammation and biomineralization. Matrix Biol. 2000;19:615–622. doi: 10.1016/s0945-053x(00)00108-6. [DOI] [PubMed] [Google Scholar]
- 31.Houssami N, Macaskill P, von Minckwitz G, Marinovich ML, Mamounas E. Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur J Cancer. 2012;48:3342–3354. doi: 10.1016/j.ejca.2012.05.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


