Abstract
Vaccination is the primary strategy for the prevention and control of influenza outbreaks. However, the manufacture of influenza vaccine requires a high-yield seed strain, and the conventional methods for generating such strains are time consuming. In this study, we developed a novel method to rapidly generate high-yield candidate vaccine strains by integrating error-prone PCR, site-directed mutagenesis strategies, and reverse genetics. We used this method to generate seed strains for the influenza A(H1N1)pdm09 virus and produced six high-yield candidate strains. We used a mouse model to assess the efficacy of two of the six candidate strains as a vaccine seed virus: both strains provided complete protection in mice against lethal challenge, thus validating our method. Results confirmed that the efficacy of these candidate vaccine seed strains was not affected by the yield-optimization procedure.
Keywords: Influenza A virus, vaccine, vaccine production, high-yield strain, error-prone PCR
Introduction
Influenza viruses cause occasional pandemics and seasonal epidemics, thus presenting continuous challenges to public health. Vaccination is the primary strategy used to slow and stop transmission of the virus and to reduce the effect of the disease. A high-yield vaccine seed strain is required for vaccine manufacturing and, thus, is key to a successful influenza vaccination program. However, it is not uncommon that strains recommended as influenza vaccine strains by the World Health Organization (WHO) have low yields in chicken embryonic eggs (hereafter referred to as eggs) (Gerdil, 2003). Low-yield strains must be engineered into high-yield strains, a process that can be time consuming and, thus, significantly delay vaccine production. Almost three months were required for the WHO collaborative laboratories and vaccine companies to generate suitable vaccine strains to produce vaccine against the 2009 pandemic influenza virus, A(H1N1)pdm09 (Chen et al., 2010; Robertson et al., 2011). Without this delay, the vaccine could have lessened the effect of the pandemic’s second wave of infection and reduced the number of associated deaths. Thus, the ability to rapidly generate high-yield vaccine strains is a critical factor in preventing and controlling influenza outbreaks.
Two common strategies have been used to generate influenza vaccine seed viruses: 1) co-infection of a cell or an egg with two viruses, one with high-yield features and another with antigenically matched hemagglutinin and neuraminidase (Kilbourne, 1969; Kilbourne and Murphy, 1960); and 2) reverse genetics to generate a virus with antigenically matched hemagglutinin and neuraminidase, and internal genes from another virus as backbone, which help improve yields (Fodor et al., 1999; Horimoto et al., 2007; Neumann et al., 1999; Nicolson et al., 2005). During the past decades, the co-infection method has been used widely to generate vaccine seed viruses. The disadvantage of co-infection is that the reassortment events cannot be well controlled and may lead to viruses with undesired traits (Fulvini et al., 2011; Ottmann et al., 2010). Thus, instead of co-infection, egg adaption is often used to improve seed virus growth in eggs (Gambaryan et al., 1999; Robertson et al., 1987; Rogers et al., 1983; Widjaja et al., 2006). In contrast to the co-infection method, the reverse genetics method can define the genomic constellation (Fodor et al., 1999; Horimoto et al., 2007; Neumann et al., 1999; Nicolson et al., 2005). However, it is difficult to generate a high-yield seed strain if the hemagglutinin and neuraminidase are not compatible with the other six gene segments from the backbone virus, and this method does not readily allow for selecting different combinations of gene segments that may result in higher yield viruses. In recent years, a recombinant technique has been used to increase the yields of influenza vaccine candidates (Adamo et al., 2009; Gomila et al., 2013; Harvey et al., 2011; Harvey et al., 2010; Jing et al., 2012; Pan et al., 2012). These reassortants, which have chimeric hemagglutinin or neuraminidase, had considerably more seed virus growth in eggs or Madin-Darby canine kidney (MDCK) cells. However, these methods usually require weeks to generate a desired strain with high yields.
In this study, we developed a novel error-prone PCR (epPCR)–based mutagenesis approach to rapidly generate high-yield influenza vaccine strains.
Results
epPCR-based mutagenesis approach
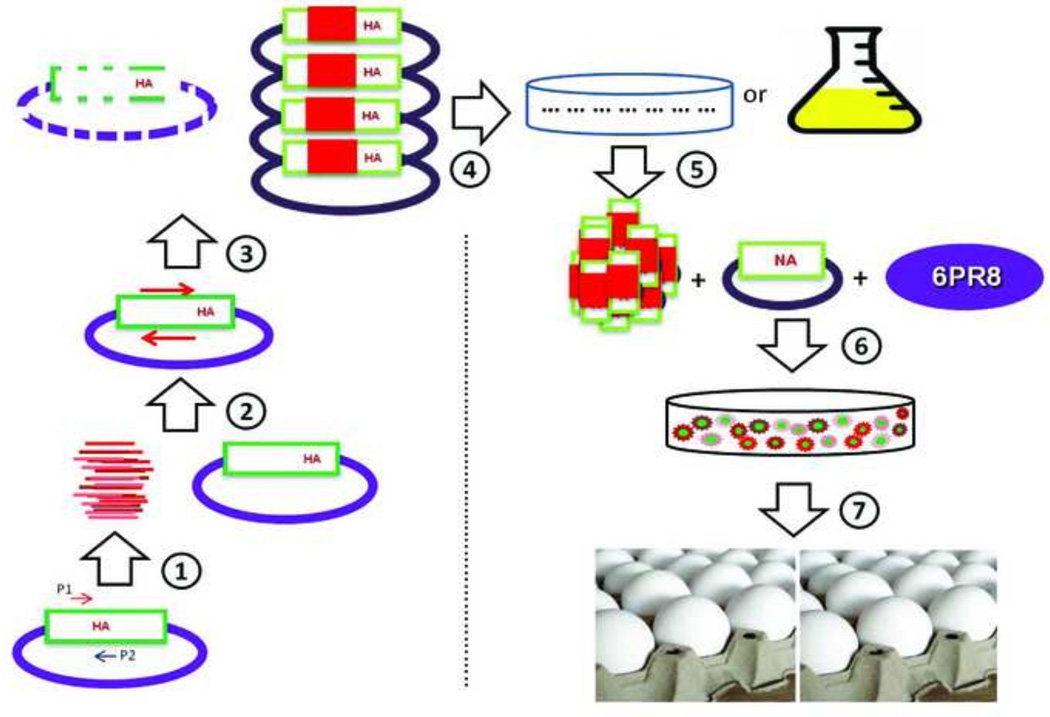
In this study, we developed an epPCR-based mutagenesis strategy for generating high-yield influenza vaccine candidates (Fig. 1). In this method, the epPCR products are used directly as primers for site-directed mutagenesis, and individual cloned plasmids are then extracted. Viruses are rescued by using the individual selected plasmids, and the rescued viruses are screened for a phenotype of high yield in eggs.
Figure 1.
Overall strategy for generating a hemagglutinin mutant library. Based on this method, chicken embryonic egg–propagated seed viruses with high yield can be selected for influenza vaccine candidate strains. The 130loop + 190helix or 190helix + 220loop in hemagglutinin gene of influenza A/California/04/09 (H1N1) virus are amplified by error-prone PCR (epPCR) by using a GeneMorph II Random Mutagenesis Kit (Agilent Technologies, Santa Clara, CA) (step 1). epPCR products are then used as primers in the site-directed mutagenesis (step 2). After DpnI digestion at 37°C for 1 h (step 3), the PCR product is transformed into XL1-Blue Supercompetent Cells (Agilent Technologies, Santa Clara, CA), and the cells are inoculated onto LB (Luria Bertani) plates or into LB medium (step 4). The individual plasmid or plasmid library is then extracted (step 5) and used with 6 internal genes from A/Puerto Rico/8/1934(H1N1) and the neuraminidase gene from CA/04 to rescue viruses (step 6). Rescued viruses are inoculated into 10-day-old chicken embryonic eggs to generate high-yield vaccine seed. The steps are indicated by circled numbers in the figure.
To validate our method, we used the hemagglutinin of CA/04 as the template to generate high-yield vaccine candidates. We first applied epPCR to breed the regions of receptor-binding sites: one region covered the 130 loop and 190 helix of the hemagglutinin gene (referred to as 130loop+190helix), and the other region covered the 190 helix and 220 loop of the hemagglutinin gene (referred to as 190helix+220loop). The epPCR products (234 bp for 130loop+190helix; 171 bp for 190helix+220loop) were subsequently used as primers in site-directed mutagenesis.
Broad diversity of the hemagglutinin mutants generated by the epPCR-based mutagenesis strategy
To evaluate the profile of the hemagglutinin mutant library, we sequenced a total of 292 clones (142 for 130loop+190helix; 150 for 190helix+220loop). Of the 292 clones, 111 carried at least one amino acid mutation while maintaining the correct open-reading frame. Of these 111 hemagglutinin mutants, 66 were derived from the 130loop+190helix epPCR products, and 45 were derived from the 190helix+220loop epPCR products. Ninety-eight of these 111 hemagglutinin mutants had a single amino acid mutation, eight had double mutations, and five had triple mutations. Except for two clones with the same mutations, all hemagglutinin mutants carried different mutations (Supplemental Table S1). The mutation profile analysis demonstrated that the mutated sites broadly spanned the entire target region from the 130loop to the 220loop. Of note, some of these mutations (V135I , A137T, P140L , H141Q , S146G , V155I , K156E, N159K, G173R , V176I , A189T , T200S , K212T, I219V) were observed in the hemagglutinin gene of the A(H1N1)pdm09 virus field strains.
To further demonstrate the diversity of the mutant library, we used next-generation sequencing to sequence the plasmid library generated by 130loop+190helix epPCR products. The readings showed that 63.8% of the sequences had nucleotide changes, and 83.9% of those led to effective amino acid mutations with correct open-reading frames. The mutations were distributed among the 130loop and the 190helix at both the nucleotide and amino acid levels (Supplemental Fig. S1).
Rapid generation of higher yield strains by using the epPCR-based mutagenesis strategy
To determine if seed strains with high yield could be directly rescued from the 111 mutants, we recovered the highest-yield viruses by transfection, inoculated them into 10-day-old eggs, and subsequently determined HA titers for comparison with the HA titers for the wild-type virus. The wild-type virus had an HA titer of 32, and six mutants (nos. 22, 58, 79, 81, 88, and 114) had an HA titer of at least 128 in passage one (Table 1). Of note, the HA titers of the wild-type virus remained stable at 32 in passages two and three, but the titers of mutant viruses number 81 and 88 increased to 512 after passage two and three, respectively (Table 1).
Table 1.
Characterization of influenza A(H1N1)pdm09 vaccine candidates generated by using an error-prone PCR–based mutagenesis strategy
| HA titera, passage no. |
HI titerb, passage no. |
Mutation (residue no.)c | |||||
|---|---|---|---|---|---|---|---|
| Virus | 1 | 2 | 3 | 1 | 2 | 3 | |
| Wild type | 32 | 32 | 32 | 3,200 | 3,200 | 3,200 | – |
| Mutant, d no. | |||||||
| 22 | 128 | 256 | 256 | 3,200 | 3,200 | 3,200 | K133N (130), V178M (175) |
| 58 | 128 | 256 | 128 | 3,200 | 3,200 | 3,200 | K149E (146) |
| 79 | 128 | 128 | 256 | 3,200 | 3,200 | 1,600 | K157I (154) |
| 81 | 128 | 128 | 512 | 1,600 | 1,600 | 1,600 | K133I (130) |
| 88 | 256 | 512 | 256 | 1,600 | 1,600 | 3,200 | K157I (153), I169T (166) |
| 114 | 256 | 128 | 256 | 3,200 | 3,200 | 3,200 | K212T (209) |
HA, hemagglutination.
HI, hemagglutination inhibition. Titers were determined by using ferret serum (anti-CA/04).
Mutations in the hemagglutinin protein sequence of the mutant, H3 numbering; the residue numbers are residues in the hemagglutinin of influenza A(H1N1)pdm09 virus.
Reverse genetics–derived viruses were generated by using hemagglutinin of wild-type influenza A/California/04/09 (H1N1) virus (CA/04) virus or hemagglutinin mutants derived from error-prone PCR, neuraminidase of CA/04, and six other gene segments (polymerases PA [polymerase acidic subunit], PB1 [polymerase basic subunit 1], and PB2 and nucleoprotein, matrix protein, and nonstructural protein) from influenza A/PR/8/34(H1N1) virus.
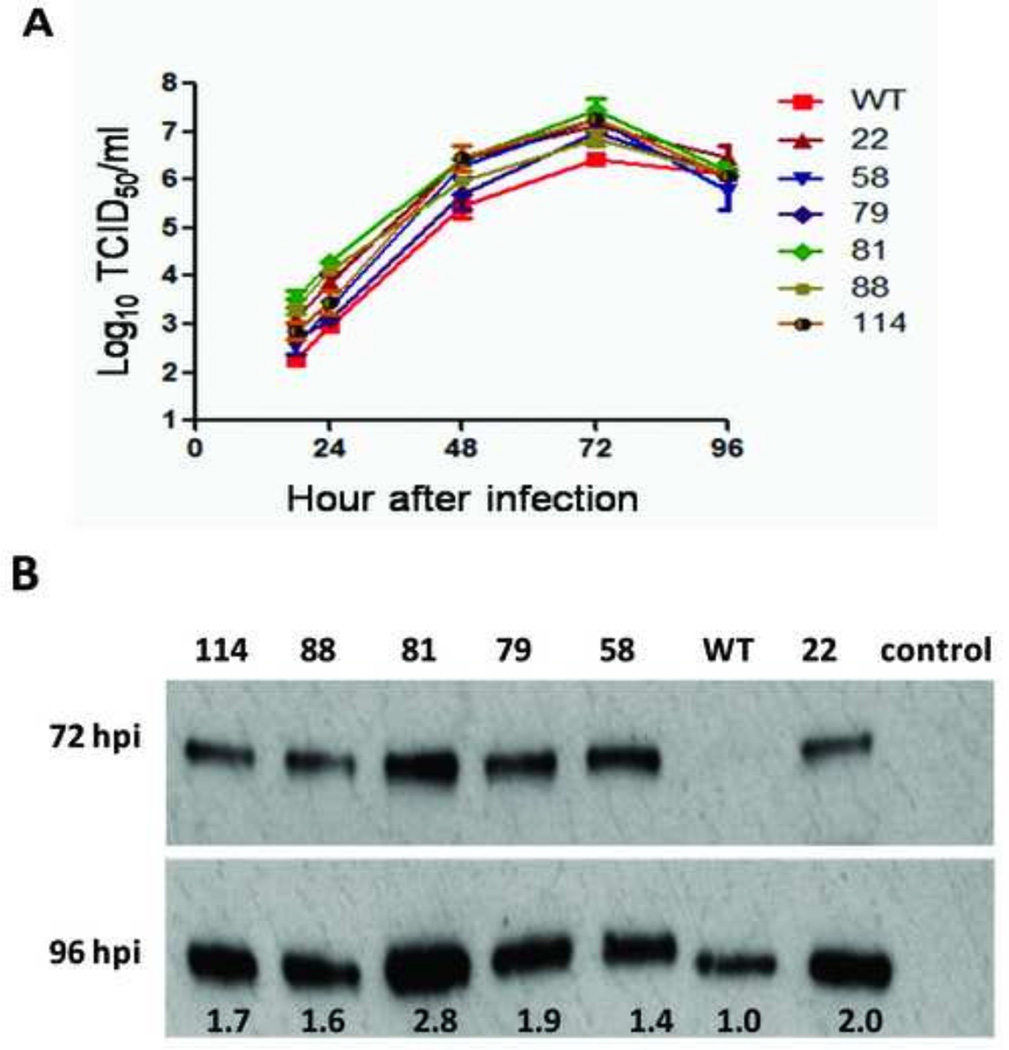
Viral growth kinetics demonstrated that these six hemagglutinin mutants replicated more efficiently than the wild-type virus in MDCK cells (Fig. 2A). The peak HA titers of these viruses reached 128–512 in MDCK cells, but the peak titer was only 32 for the wild-type virus. Among these six mutants, numbers 22 and 81 yielded the highest HA titer (512) in MDCK cells. The peak TCID50 of these mutants was 0.4–1.0 log10 TCID50 higher than that for wild-type virus (Fig. 2A).
Figure 2.
Characterization of the high-yield influenza A(H1N1)pdm09 vaccine candidates generated by using the error-prone PCR–based mutagenesis strategy. Viruses were inoculated into Madin-Darby canine kidney cells at a multiplicity of infection of 0.001. (A) Growth curves for wild-type (WT) and mutant viruses (nos. 22, 58, 79, 81, 88, and 144) measured by 50% tissue culture infectious dose (TCID50; values shown below columns) at various hours after infection (hpi). (B) Western blot showing the nucleoprotein expression level for the WT and mutant viruses (viruses shown above columns).
The Western blot assay results for cell lysate tested 72 h and 96 h after inoculation confirmed these results. Nucleoprotein expression for the mutant viruses was stronger than that for the wild-type strain. The nucleoprotein expression level for mutants number 22, 58, 79, 81, 88, and 114 were 2.0-, 1.4-, 1.9-, 2.8-, 1.6-, and 1.7-fold higher, respectively, than that for the wild-type virus (Fig. 2B).
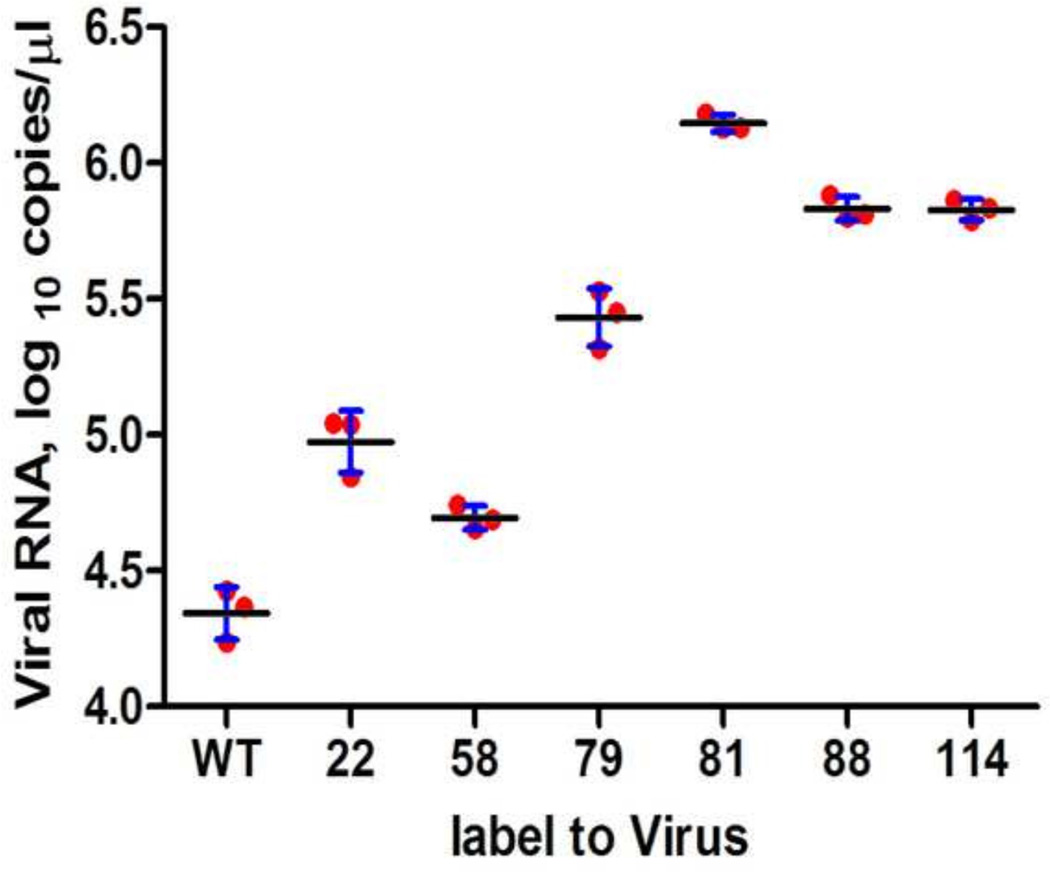
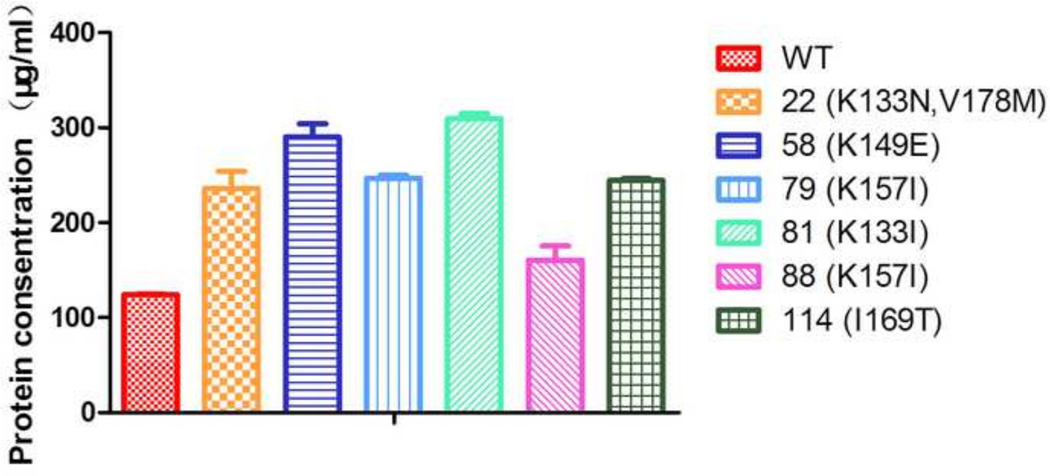
Consistent with our HA assay results, qPCR results for the six selected mutants showed higher yields than those for the wild-type virus. On average, viral RNA levels in allantoic fluid of eggs inoculated with mutants number 22, 58, 79, 81, 88 and 114 were 4.3-, 2.3-, 12.3-, 64.6-, 30.9-, and 30.9-fold (copies/µl) higher, respectively, than levels in allantoic fluid of eggs inoculated with the wild-type strain (Fig. 3). The total protein concentrations of mutants number 22, 58, 79, 81, 88 and 114 were 1.90-, 2.33-, 1.99-, 2.50-, 1.30- and 1.97-fold (µg/ml) higher, respectively, than that of the wild-type strain (Fig. 4). These results further confirmed that, compared with the wild-type virus, the six selected mutants generated by the epPCR-based mutagenesis strategy grew more efficiently in eggs.
Figure 3.
Quantification of wild-type (WT) and mutant viruses propagated in eggs as determined by using a hemagglutinin gene–specific quantitative reverse transcription PCR method. Results are expressed as the median (horizontal bars) RNA copy number (1 µl cDNA) ± SD (vertical bars).
Figure 4.
Total protein quantification of wild-type (WT) and mutant viruses that purified from the allantoic fluids of 11-day-old embryonated chicken eggs. Results are expressed as the median (horizontal bars) protein concentration ±SD (vertical bars).
One-way HI assays using post-infection ferret antiserum raised against CA/04 showed that the homologous HI titers of 3,200 for CA/04 (Table 1). The heterologous HI titers of the six mutant viruses were 3,200 or 1,600, demonstrating that these candidates had few antigenic differences from the wild-type strain.
High-yield vaccine candidates providing full protection against lethal challenge in mice
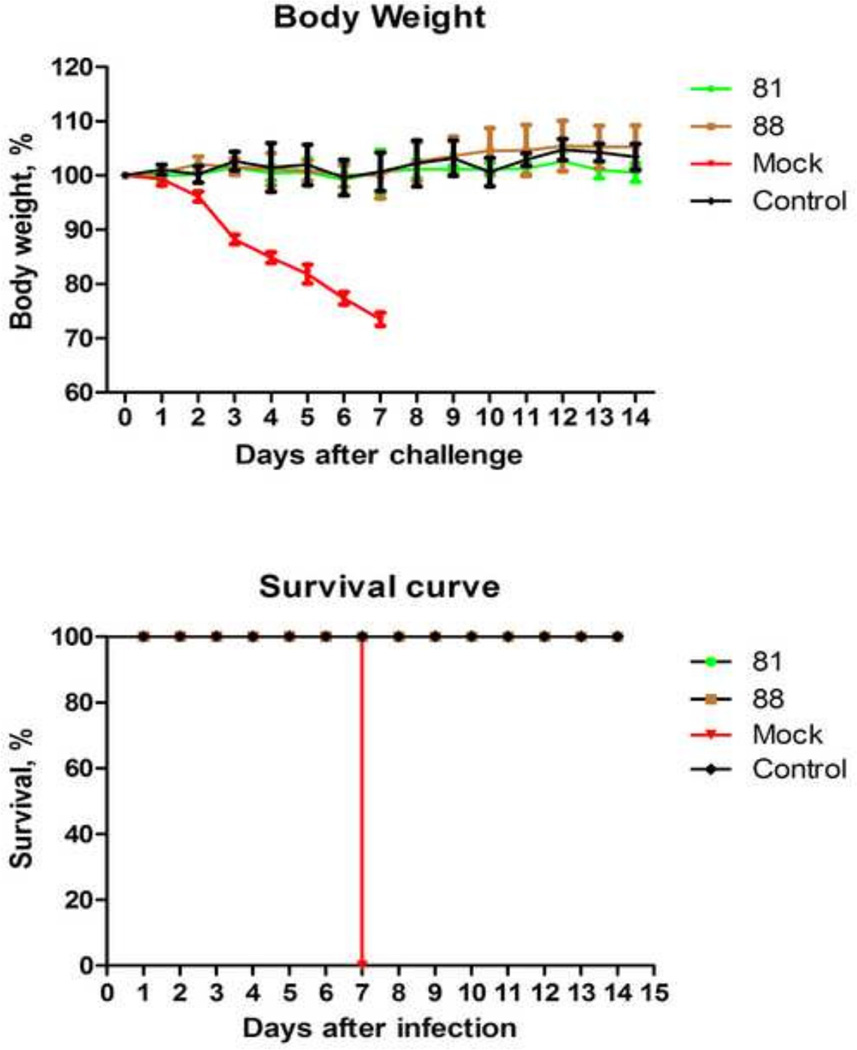
To confirm that our mutagenesis approach had not affected subsequent vaccine efficacy, we selected the two mutants with the highest HA titers (mutants no. 81 and 88) as vaccine candidates and evaluated their efficacy in a mouse model. Serum samples collected from vaccinated mice 2 weeks after the booster vaccine was administered exhibited HI titers substantially higher than those for the mock-vaccinated group (Table 2). After viral challenge, virus replication (reaching levels up to 105.4TCID50/ml) was detected in the lungs of all mock-vaccinated mice; no virus was detected in any of the vaccinated mice (Table 2). Mice in the mutant number 81– and 88– vaccinated groups did not lose weight, but the mock-vaccinated mice were lethargic and rapidly lost weight (Fig. 5A). All vaccinated mice survived the lethal challenge; all mock-vaccinated mice died 7 days after challenge (Fig. 5B).
Table 2.
Pathogenesis and immunologic responses in vaccinated mice challenged with mouse-adapted influenza A/California/04/09 (H1N1) virus
| Vaccine group | Log10TCID50/ml, mean ± SDa | log2HI titer, mean ± SDb | log2HI titer, mean ± SDc |
|---|---|---|---|
| Mutant no. (mutation) | |||
| 81 (K133I) | Below detection limit | 8.32 ± 0.70 | 8.12 ±0.45 |
| 88 (K157I, I169T) | Below detection limit | 8.12 ± 0.45 | 8.12 ±0.45 |
| Mock | 5.4 ± 0.1 | Below detection limit | Below detection limit |
Groups of BALB/c mice were inoculated intranasally under light anesthesia with 10× the 50% lethal dose of mouse-adapted CA/04 virus. Three mice from each group were euthanized on day 4 after virus challenge, and virus titers in lungs were determined by TCID50 (50% tissue culture infectious dose) in MDCK cells.
Serum samples were collected 2 weeks after the booster vaccine was administered, and antibody response levels against the immunogen mutant were measured by using the HI (hemagglutination inhibition) assay.
Serum samples were collected 2 weeks after the booster vaccine was administered, and antibody response levels against the wide type were measured by using the HI (hemagglutination inhibition) assay.
Figure 5.
Protective effect of high-yield vaccine candidates in mice challenged with mouse-adapted influenza A/California/04/09 (H1N1) virus. Groups of control; mock-vaccinated; and mutant number 81–, 88–vaccinated mice were intranasally inoculated with 10 × the 50% lethal dose of virus, after which their body weights (A) and survival times (B) were monitored for 14 days. Results are shown as the mean ± SD in each group (A).
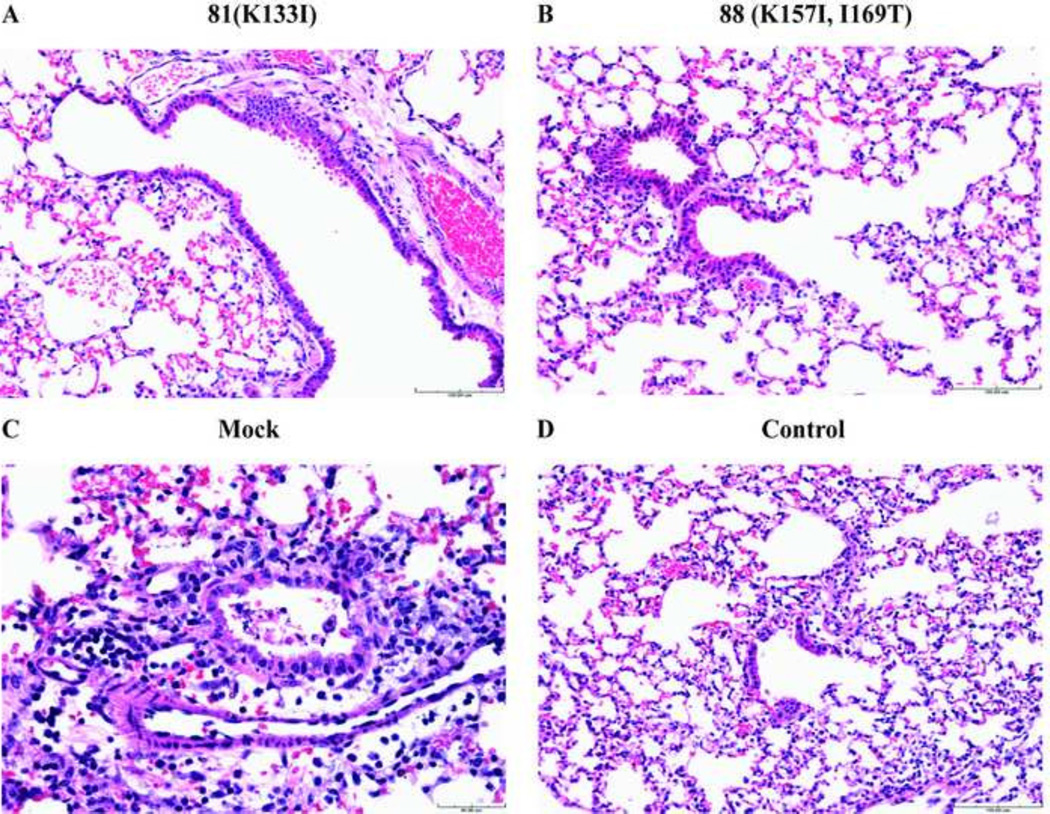
Photomicrographs of hematoxylin and eosin–stained lung sections are shown in Fig. 5. Mock-vaccinated mice displayed acute, diffuse, necrotizing bronchitis and bronchiolitis 4 days after challenge (Fig. 6C). No histopathologic changes were observed in the mice vaccinated with mutants number 81 or 88 (Fig. 6), demonstrating effective protection of both vaccine candidates from the lethal mouse-adapted CA/04 challenge. Thus, our results indicate that the high-yield candidate vaccines generated by our epPCR-based mutagenesis strategy did not have altered antigenicity and could serve as potential seed strains for the manufacture of influenza vaccines.
Figure 6.
Histopathologic findings in hematoxylin and eosin–stained lung samples from vaccinated and mock-vaccinated mice challenged with mouse-adapted influenza A(H1N1)pdm09 virus. Four days after challenge, groups of mutant number 81–vaccinated (A), mutant number 88–vaccinated (B), and mock-vaccinated (C) mice were euthanized, and lungs were collected for histopathologic examination; non-vaccinated, non-challenged mice served as environmental controls (D). A, B, and D) Scale bar =100 µm; C) scale bar = 40 µm.
Receptor-binding models of improved-yield mutants
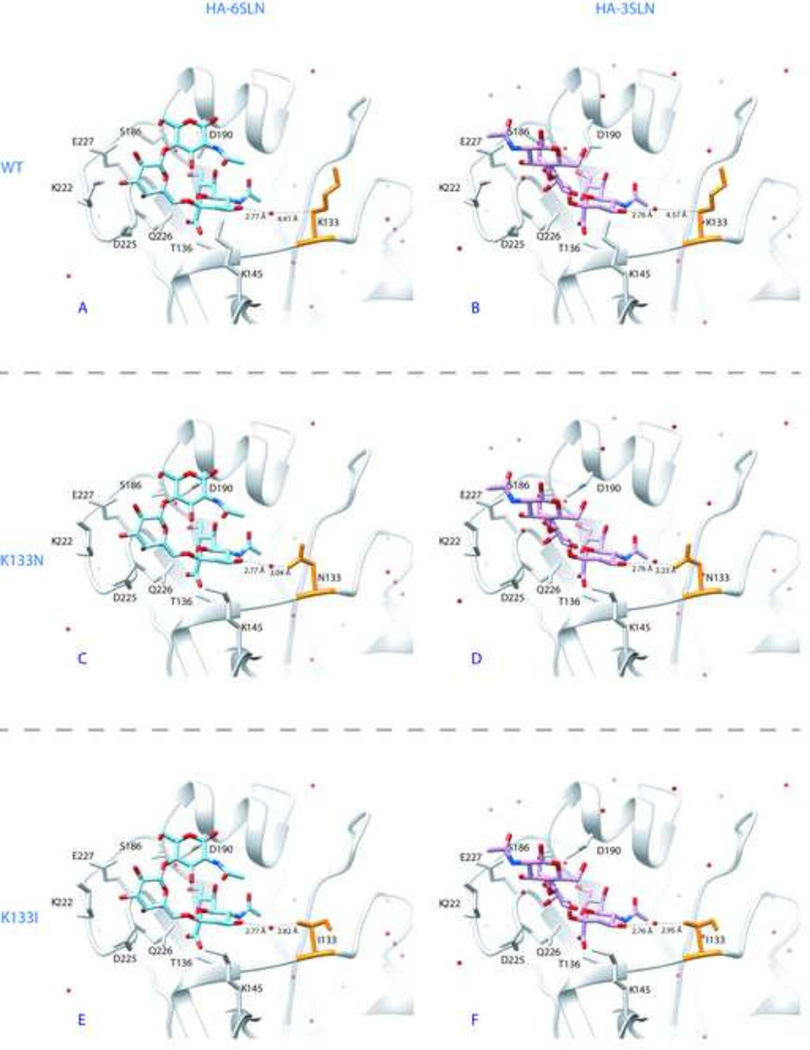
Among the six mutation sites, only mutants number 22 and 81 had residue 133 located in the receptor-binding sites of hemagglutinin (Supplemental Fig. S2). These crystal structures of the bindings between the hemagglutinin of influenza A(H1N1)pdm09 and glycan analogs 6SLN or 3SLN were used in computational mutation simulations to study the effects of amino acid modifications on hemagglutinin-receptor bindings.
As measurements of binding modifications caused by mutations, we calculated the distances between the oxygen atom of a water molecule (which formed a hydrogen bond between amino acid residue 133 and glycan receptors) and the nearest atoms of sialic acid and the distances between the oxygen atom of a water molecule and residue 133. Moreover, as a quantification of hemagglutinin–glycan binding avidities, we obtained the PoseScore (Fan et al, 2011) for structural interactions between glycans and all wild-type and computationally mutated hemagglutinin structures (Fig. 7).
Figure 7.
The three-dimensional structures of the hemagglutinin of the wild–type (WT) influenza A/California/04/09 (H1N1) virus and mutant viruses (nos. 22 and 81) in contact with human-like receptor analog 6SLN (panels A, C, and E) and avian-like receptor analog 3SLN (panels B, D, and F). The protein structures of hemagglutinin are shown in light grey; residue 133 is in orange. The side chains of interacting residues on the receptor-binding sites are labeled with residue names and locations. The single letter amino acid annotations were used together with H3 numbering for all binding residues. 6SLN is shown in cyan, and 3SLN is shown in magenta. Red dots indicate the oxygen atoms from all water molecules that are in contact with hemagglutinin side chains. The distances (in angstroms) between the water molecule and the nearest atom on both the protein and ligand sides are indicated by dashed lines. (A) WT hemagglutinin with lysine at position 133 in contact with 6SLN. (B) WT hemagglutinin with lysine at position 133 in contact with 3SLN. (C) K133N mutant hemagglutinin with asparagine at position 133 in contact with 6SLN. (D) K133N mutant hemagglutinin receptor-binding sites with asparagine at position 133 in contact with 3SLN. (E) Mution K133I at the hemagglutinin receptor-binding site with isoleucine at position 133 in contact with 6SLN. (F) Mutant K133I with isoleucine at position 133 in contact with 3SLN. Simulations on the hemagglutinin were performed by using the FoldX empirical force field (Schymkowitz et al., 2005), and the structure was visualized by using Chimera (Pettersen et al., 2004); PoseScore (Fan et al., 2011) was used to estimate the likeness of the WT and mutant protein–glycan binding avidities to that of the native virus.
When the hemagglutinin bound to 3SLN, the wild-type structure with a polar and positively charged lysine at residue 133 had a distance of 4.57 Å to the linker water molecule, and the whole interaction had a PoseScore of −6.32 (Fig. 7B). The K133N mutant had a polar, but neutral, asparagine at residue 133, which was only 2.23 Å from the linker water molecule, and its PoseScore wass −7.04 (Fig. 7D). The K133I mutant had a nonpolar and neutral isoleucine at residue 133, which was 2.95 Å to the linker water molecule, and its PoseScore was −6.88 (Fig. 7F). These results showed that both the contact distances and pose binding scores were decreased by substituting a charged lysine with neutral asparagine or isoleucine. Thus, given that smaller contact distances and lower PoseScores suggest stronger interactions between glycans and proteins, mutations K133N and K133I could lead to increased 3SLN bindings compared with what the wild-type strain does. These stronger hemagglutinin–3SLN bindings for mutants number 22 and 81, compared with that for the wild type strain, may contribute to the higher replication efficiencies of these two mutants in eggs and MDCK cells.
Of interest, the structural simulation showed that both the contact distances and pose binding scores between hemagglutinin and 6SLN were also decreased by substituting a charged lysine with neutral asparagine or isoleucine. When the hemagglutinin bound to 6SLN, the wild-type structure with a polar and positively charged lysine at residue 133 had a distance of 4.41 Å to the linker water molecule and the whole interaction had a PoseScore of −11.83 (Fig. 7A). The K133N mutant had a polar but neutral asparagine, which wass only 2.04 Å from the linker water molecule, and its PoseScore wass −12.18 (Fig. 7C). The K133I mutant had a nonpolar and neutral isoleucine at residue 133, which was 2.82 Å from the linker water molecule, and its PoseScore was −14.42 (Fig. 7E). These results suggested that mutations K133N and K133I could lead to stronger 6SLN bindings in mutants number 88 and 81 than in the wild-type virus.
Discussion
Conventional site-directed mutagenesis strategies depend on virus variants that are manually selected and usually have a single or a few mutations; egg-adaptation strategy depends on the virus variants generated by error in natural viral RNA replication (viral quasispecies) resulting from the lack of proofreading capacity in viral RNA polymerase. The small pool of virus variants produced by these approaches is a bottleneck in the process of selecting high-yield seed strains for influenza vaccine production. Thus, we hypothesized that the in vitro breeding of a diverse influenza virus variant library by epPCR would enhance the process for generating high-yield strains. The epPCR method has been widely used to generate libraries of mutant proteins for phenotype selection (Cherry et al., 1999; Cirino, 2003; Daugherty et al., 2000; Wan et al., 1998; Zang et al., 2006). By integrating epPCR, site-directed mutagenesis, and reverse genetics, we developed a novel strategy for rapidly generating high-yield vaccine candidates. Our data show that this strategy allows for the rapid generation of high-yield vaccine candidates for the A(H1N1)pdm09 virus. Whole-virus inactivated vaccines derived from two high-yield candidates that we generated provided full protection against lethal A(H1N1)pdm09 virus challenge in mice.
In a recent study, an epPCR strategy was developed to generate influenza mutant library for phenotype selection (Imai et al., 2012; Wu et al., 2013). In these studies, the epPCR was used to amplify the partial HA or whole NA genes, and the amplified fragment or gene need to be digested with restriction enzyme and then subcloned to a plasmid for virus rescuing using reverse genetics. Unlike their approaches for generating influenza mutant library, our strategy integrated the epPCR and site mutagenesis approach by using the epPCR product directly as primers for site mutagenesis. Therefore, through two single PCRs, one epPCR and another site mutagenesis PCR, we can target any region of an influenza gene segment to generate plasmid mutant library without designing any restriction enzyme site. Such a strategy allows us to skip the subcloning step, which is required by the methods described in (Imai et al., 2012; Wu et al., 2013). Therefore, our approach developed here would be much less labor intensive and more efficient. It is worth mentioning that our method can potentially be used for generating mutant libraries for phenotype selection for not only influenza virus but also many other microbes.
The mechanism(s) by which the mutations in the hemagglutinin gene improve virus replication are poorly understood. Previous studies suggested that the functional balance between receptor binding of the hemagglutinin and the receptor-releasing property of the neuraminidase is critical for efficient replication of influenza viruses (Mitnaul et al., 2000; Wagner et al., 2002). Mutations near the receptor-binding sites of the hemagglutinin are known to affect the replication abilities of viruses (Chen et al., 2010; Hartgroves et al., 2010; Lugovtsev et al., 2005; Robertson et al., 2011). In this study, we constructed a hemagglutinin plasmid library targeted to the receptor-binding sites of influenza A(H1N1)pdm09 virus. By using the cloned mutant hemagglutinin genes, we successfully rescued 43 viruses without subsequent egg passages. Of these 43 viruses, six mutants had improved yields in eggs.
Among the mutations in the hemagglutinin of the six selected vaccine candidates in our study (Table 1), mutations K157I and K212T were previously reported in the high-yield A(H1N1)pdm09 vaccine strains generated in eggs (Robertson et al., 2011). Identification of these two previously reported mutations, which improved the yields of A(H1N1)pdm09 virus, validates the effectiveness of our strategy. Our strategy is further validated by the fact that we also found some novel sites in the hemagglutinin that improved yields without changing virus antigenicity. For example, K133, which was found in two high-yield mutants, is absent in the hemagglutinin of the contemporary human seasonal influenza A(H1N1) virus and is highly conserved in both the A(H1N1)pdm09 virus and its precursor, the hemagglutinin gene of the 1918 pandemic H1N1 influenza virus. The K133N HA mutation was predicted to broadly change the electrostatic potentials surrounding the receptor-binding domain (Li et al., 2013). As shown in receptor-binding models (Fig. 6), the substitution of a positively charged lysine in position 133 by a polar uncharged asparagine or hydrophobic isoleucine could contribute to the increase in binding avidity and be responsible for the improved yield of these mutants in eggs and MDCK cells.
A previous study predicted the important role of K133 and K149 in receptor-binding affinity and in the virulence of A(H1N1)pdm09 virus (Meroz et al., 2011). Substitution of K133R or K149R in “swine-like” A(H1N1)pdm09 virus reduced its pathogenicity (Meroz et al., 2011). The mutants with K133N or K149E mutations that were identified in this study have higher yield properties and may have lower pathogenicity compared with that of the wide-type strain; which would ensure a safer vaccine production. In addition, two of six selected mutants with improved yields harbor K157I mutations. It has been reported that mutants with K157E mutations are preferred for replication of A/California/7/2009(H1N1) virus in MDCK cells and eggs (Chen et al., 2010). Our results also indicate that the presence of a isoleucine residue with hydrophobic site chain in position 157 of hemagglutinin improves the growth ability of the A(H1N1)pdm09 virus.
Concerns have been raised that even single amino acid substitution near receptor-binding sites may change the antigenicity of influenza viruses (Koel et al., 2013). However, mutations near the receptor-binding sites of the hemagglutinin, such as L119I, A186D, N125D, and D127E, have been used as seed viruses for the A(H1N1)pdm09 vaccine (Chen et al., 2010). The HI assay results in our study indicate that the six high-yield candidate vaccine strains had few antigenic changes from the CA/04 wild-type strain (Table 1). For example, although K133 was recently documented to be involved in B cell epitopes recognized by monoclonal antibodies (Krause et al., 2011; O'Donnell et al., 2012; Whittle et al., 2011), in our study, mutation K133N did not alter the antibody-binding avidities of K133N mutant to anti-A(H1N1)pdm09 virus ferret serum; this finding has also been reported elsewhere (Li et al., 2013). Moreover, inactivated vaccines based on two testing candidates that yielded the highest titers in eggs provided full protection against lethal challenge in experiments with mice. These results provide further evidence that the epPCR-based mutagenesis strategy combined with serologic assays, such as the HI assay, could be used for rapid generation of influenza seed viruses.
In summary, we report the use of a novel epPCR-based site-directed mutagenesis strategy to rapidly generate a diverse influenza hemagglutinin plasmid library and the application of this method to generate high-yield candidate strains for production of A(H1N1)pdm09 virus vaccine candidates. The mutations associated with high yield in our study could facilitate a quick response to future outbreaks caused by A(H1N1)pdm09 virus and its variants. Moreover, this novel strategy could also be applied to the breeding of other functional regions of a gene to rapidly generate diverse mutant libraries for gain-of-function studies for influenza and potentially other pathogens.
Materials and Methods
Cells and viruses
MDCK cells and human embryonic kidney (293T) cells (both from American Type Culture Collection, Manassas, VA) were used for propagation and culture of influenza virus. The cells were maintained at 37°C with 5% CO2 in Dulbecco's Modified Eagle Medium (GIBCO/BRL, Grand Island, NY) supplemented with 5% fetal bovine serum (FBS) (Atlanta Biologicals, Lawrenceville, GA), penicillin–streptomycin, and amphotericin B (GIBCO/BRL, Grand Island, NY). The wild-type strain of A/California/04/09 (H1N1) virus (CA/04) was used in the mutant library construction (Fig. 1); mouse-adapted CA/04 (Ilyushina et al, 2010) was used for challenge experiments.
All viruses generated by reverse genetics were propagated in MDCK cells and cultured at 37°C with 5% CO2 in Opti-MEM medium (GIBCO/BRL, Grand Island, NY) supplemented with 1 µg/ml of TPCK (N-tosyl-L-phenylalanine chloromethyl ketone)-Trypsin (Sigma-Aldrich, St. Louis, MO), penicillin–streptomycin, and amphotericin B (GIBCO/BRL, Grand Island, NY). Virus titers were determined by 50% tissue culture infectious dose (TCID50) in MDCK cells.
Primers
Four primers were used in this study: 1) 130loop_F, 5'-TCA TGG CCC AAT CAT GAC TCG AAC-3'; 2) 190helix_F, 5'-TGG GGC ATT CAC CAT CCA TCT ACT-3'; 3) 190helix_R, 5'-AAC ATA TGT ATC TGC ATT CTG ATA-3'; and 4) 220loop_R, 5'-TAG TGT CCA GTA ATA GTT CAT TCT-3'. Primers 130loop_F and 190helix_R were used to amplify the sequence covering the 130-loop and 190-helix of the receptor-binding site in the hemagglutinin gene of influenza virus. Primers 190helix_F and 220loop_R were used to amplify the sequence covering the 190-helix and 220-loop of the receptor-binding site in the hemagglutinin gene of influenza virus.
epPCR-based mutagenesis method to generate hemagglutinin mutants of influenza virus
We used the GeneMorph II Random Mutagenesis Kit (Agilent Technologies, Santa Clara, CA) according to the manufacturer’s instructions to perform epPCR. The resulting products were used as primers to perform site directed mutagenesis. The epPCR amplification mixture contained 17.75 µl of water, 5 µl of 10× buffer, 1 µl of 2.5 mM deoxyribonucleotide triphosphates, 1 µl of 10 µmol primer (each), 2 µl of hemagglutinin plasmid of CA/04 (10 pg/µl), and 1 µl of Mutazyme II DNA polymerase (Agilent Technologies, Santa Clara, CA). The parameters of the epPCR were as follows: one cycle at 95°C for 5 min, followed by 30 cycles at 94°C for 1 min, 50°C for 1 min, and 72°C for 2 min, and then one cycle at 72°C for 10 min. Site-directed mutagenesis was performed by using the QuikChange II Site-Directed Mutagenesis Kit (Stratagene, La Jolla, CA) according to the manufacturer’s instructions. In brief, the PCR mixture included 36 µl of water, 5 µl of 10× buffer, 1 µl of 2.5 mM deoxyribonucleotide triphosphates, 2 µl of epPCR product (25 ng/µl), 2 µl of hemagglutinin plasmid (10 ng/µl), and 1 µl of PfuUltra High-Fidelity DNA Polymerase (Agilent Technologies, Santa Clara, CA) (2.5 U/µl). After digestion with DpnI (a restriction enzyme that only cleaves methylated DNA) at 37°C for 1 h, the PCR product (2 µl) was transfected into XL1-Blue Supercompetent Cells (Agilent Technologies, Santa Clara, CA). The transformed cells were directly inoculated onto LB (Luria Bertani) agar plates or into LB medium.
Generation of reassortant viruses by reverse genetics
The reassortant viruses were rescued by transfection in co-cultured 293T cells and MDCK cells, as described elsewhere (Ye et al, 2010), using mutated hemagglutinin gene, unmodified neuraminidase gene of CA/04, and six internal genes from influenza A/PR/8/1934(H1N1) virus. At day 3 after transfection, the media and cells were inoculated into 10-day-old eggs (0.2 ml/egg). Ninety-six hours after inoculation, we collected the allantoic fluids from the eggs for viral titration.
Genomic sequencing
Virion RNA and cDNA were prepared as previously described (Ye et al, 2010). Sequencing was performed at the Life Sciences Core Laboratories Center at Cornell University (Ithaca, NY) by using the automated 3730 DNA Analyzer (Applied Biosystems, Foster City, CA), which utilizes Big Dye Terminator chemistry and AmpliTaq-FS DNA Polymerase. Deep sequencing was performed by the Beijing Genomics Institute (Shenzhen, China), using a MiSeq sequencer (Illumina, Shanghai, China).
Growth kinetics in MDCK cells
To determine the growth kinetics of viruses, we inoculated the MDCK cells with influenza virus at a multiplicity of infection of 0.001 TCID50 and incubated the cells in 5% CO2 at 37°C for 1 h. The inocula were removed and washed two times with phosphate-buffered saline (PBS). The cells were then incubated (37°C in 5% CO2) in Opti-MEM I (GIBCO, Grand Island, NY) containing TPCK–trypsin (1 µg/ml). At specified time points after inoculation, 200 µl of supernatants were collected, aliquoted, and stored at −70°C until use. Virus titers in supernatants collected at the different time points were determined by TCID50 in MDCK cells.
Western blot assay
The Western blot assay was used to compare the yields of the vaccine candidates with those of the wild-type strain. The cell supernatants were lysed and then analyzed by Western blot assay. Western blots were developed by using horseradish peroxidase-conjugated goat anti-mouse IgG (Santa Cruz Biotechnology, Santa Cruz, CA) and an enhanced chemiluminescence detection system (ECL GE Healthcare, Pittsburgh, PA) and then exposed to X-ray film. The primary antibodies used in the Western blot assay were influenza nucleoprotein monoclonal antibodies from the Biodefense and Emerging Infections Research Resources Repository (Manassas, VA).
Quantitative reverse transcription PCR (qRT-PCR)
qRT-PCR was used to determine the level of viral RNA in the allantoic fluid of eggs inoculated with an influenza virus. Viral RNA (50 µl total) was isolated from 200 µl of sample by using a Gene JET Viral RNA Purification Kit (Thermo Fisher Scientific, Pittsburgh, PA). Influenza virus–specific Primer Uni12 (5’-AGCAAAAGCAGG-3’) and 10 µl of template RNA were used in the cDNA synthesis (total volume of 25 µl); the cDNA synthesis was carried out using SuperScript III Reverse Transcriptase (Invitrogen, Grand Island, NY) according to the manufacturer’s instructions. Primers 130loop_F and 190helix_R were used in the qPCR, which consisted of 5 µl of Master Mix (Applied Biosystems, Foster City, CA), 500 nM each primer, 2 µl of target cDNA, and sufficient diethylpyrocarbonate (DEPC)-treated water to make a volume of 10 µl. The cDNA was amplified by 40 two-step PCR cycles (3 s at 95°C for denaturation of the DNA, 20 s at 60°C for primer annealing and extension). qPCR amplifications were measured by using the Stratagene Mx3005P qPCR System (Agilent Technologies, Santa Clara, CA). As a sample standard, we used the pHW 2000 plasmid vector with the hemagglutinin gene of CA/04, which was serially diluted 10-fold to generate the standard curve. The amplification results were shown as Log10 copies/µl.
Total protein quantification
Viruses were purified from the allantoic fluids of 11-day-old embryonated chicken eggs by low-speed clarification (4000 rpm, 20 min, 4 °C) followed by ultracentrifugation through a cushion of 30%–60% sucrose in a 70Ti rotor (Beckman Coulter, Fullerton, California) (37,500 rpm, 3 h, 4 °C). The virus band was collected and purified through a cushion of 30% sucrose in a 70Ti rotor (37,500 rpm, 3 h, 4 °C). The virus pellet was resuspended in 200ul PBS and the total amount of purified virion proteins was determined by Quant-iT™ protein assay kit (Invitrogen, USA).
Mouse vaccination and challenge
To assess the antigenicity and protective efficacy of high-yield mutant viruses, we vaccinated a group of 6-week-old female BALB/c mice (Harlan Laboratories, Indianapolis, IN) by intramuscular administration of 128 hemagglutination (HA) units (in 50-µl volumes) of a formaldehyde-inactivated vaccine candidate, mutant number 81 (n = 10 mice) or mutant number 88 (n = 10 mice). Two weeks later, we administered a booster vaccine. Mock-vaccinated mice (n = 10) received a volume of PBS equal to the amount of vaccine administered to the vaccinated mice. Five mice that were not vaccinated and not challenged served as environmental controls. Two weeks after the booster vaccination, mice were anesthetized and challenged by intranasal inoculation with mouse-adapted CA/04 at 10× the 50% lethal dose (LD50). Serum samples were collected from mice before challenge and tested by using an HA inhibition (HI) assay. To determine lung virus titers, we euthanized three mice at day 4 after challenge. Lungs were homogenized and resuspended in 1 ml of sterile PBS, and virus titers were determined in MDCK cells. The samples were also stained with hematoxylin and eosin stain for pathologic examination. The survival rate, clinical signs, and body weight of the remaining mice were monitored for 14 days after the challenge. All animal studies were approved by the Office of Regulatory Compliance Institutional Biosafety Committee and the Institutional Animal Care and Use Committee of Mississippi State University.
HA and HI assays
HA and HI assays were performed by using a 0.5% suspension of turkey red blood cells as described in the WHO Manual on Animal Influenza Diagnosis and Surveillance (http://www.who.int/csr/resources/publications/influenza/whocdscsrncs20025rev.pdf).
Structural modeling
Crystal structures of the hemagglutinin protein (Protein Databank [PDB] accession nos. 3LZG, 3UBN, and 3UBQ of the A(H1N1)pdm09 virus and the binding sites of carbohydrates 6'-Sialyl-N-acetyllactosamine (6SLN) and 3'-Sialyl-N-acetyllactosamine (3SLN) to this protein were obtained from PDB (Xu et al., 2013). Structural simulation of amino acid mutations was performed on the hemagglutinin by using the FoldX platform with its empirical force field (Schymkowitz et al., 2005) with crystal waters under the following conditions: temperature of 298K, pH 7, 0.05 ion strength. Chimera (Pettersen et al., 2004) was used to visualize the binding structures and measure contact distances. PoseScore, which was designed for ranking near-native ligand–protein interacting structures (Fan et al., 2011), was used to estimate the likeness of the protein–glycan binding avidities of the wild-type and mutant to that of the native virus. The computational analysis of mutation effects on HA–glycan bindings was focused on the mutants with 133 (H3 numbering) location only because the other mutations are not located in the receptor-binding sites of hemagglutinin and did not modify the PoseScores of the hemagglutinin of the wild-type virus.
Supplementary Material
Highlights.
Conventional methods for generating high-yield influenza vaccine seed is time consuming
A novel strategy was developed for rapidly generating high-yield influenza vaccine seeds
This method integrates error-prone PCR, site-directed mutagenesis strategies, and reverse genetics
This method was validated by generating effective influenza A(H1N1)pdm09 vaccine candidates
Acknowledgments
We thank Dr. Matthew Ross for technical support. This study was partially supported by grants 1R15AI107702 and P20GM103646 from National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Accession numbers. The Crystal structures of the hemagglutinin protein were downloaded from Protein Data bank with accession numbers: 3LZG, 3UBN, and 3UBQ.
References
- Adamo JE, Liu T, Schmeisser F, Ye Z. Optimizing viral protein yield of influenza virus strain A/Vietnam/1203/2004 by modification of the neuraminidase gene. Journal of virology. 2009;83:4023–4029. doi: 10.1128/JVI.02391-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Wang W, Zhou H, Suguitan AL, Jr, Shambaugh C, Kim L, Zhao J, Kemble G, Jin H. Generation of live attenuated novel influenza virus A/California/7/09 (H1N1) vaccines with high yield in embryonated chicken eggs. Journal of virology. 2010;84:44–51. doi: 10.1128/JVI.02106-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherry JR, Lamsa MH, Schneider P, Vind J, Svendsen A, Jones A, Pedersen AH. Directed evolution of a fungal peroxidase. Nat Biotechnol. 1999;17:379–384. doi: 10.1038/7939. [DOI] [PubMed] [Google Scholar]
- Cirino PC, Mayer KM, Umeno D. Generating mutant libraries using error-prone PCR. Methods Mol Biol. 2003;231:3–9. doi: 10.1385/1-59259-395-X:3. [DOI] [PubMed] [Google Scholar]
- Daugherty PS, Chen G, Iverson BL, Georgiou G. Quantitative analysis of the effect of the mutation frequency on the affinity maturation of single chain Fv antibodies. Proceedings of the National Academy of Sciences of the United States of America. 2000;97:2029–2034. doi: 10.1073/pnas.030527597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan H, Schneidman-Duhovny D, Irwin JJ, Dong G, Shoichet BK, Sali A. Statistical potential for modeling and ranking of protein-ligand interactions. J Chem Inf Model. 2011;51:3078–3092. doi: 10.1021/ci200377u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fodor E, Devenish L, Engelhardt OG, Palese P, Brownlee GG, Garcia-Sastre A. Rescue of influenza A virus from recombinant DNA. Journal of virology. 1999;73:9679–9682. doi: 10.1128/jvi.73.11.9679-9682.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulvini AA, Ramanunninair M, Le J, Pokorny BA, Arroyo JM, Silverman J, Devis R, Bucher D. Gene constellation of influenza A virus reassortants with high growth phenotype prepared as seed candidates for vaccine production. PloS one. 2011;6:e20823. doi: 10.1371/journal.pone.0020823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambaryan AS, Robertson JS, Matrosovich MN. Effects of egg-adaptation on the receptor-binding properties of human influenza A and B viruses. Virology. 1999;258:232–239. doi: 10.1006/viro.1999.9732. [DOI] [PubMed] [Google Scholar]
- Gerdil C. The annual production cycle for influenza vaccine. Vaccine. 2003;21:1776–1779. doi: 10.1016/s0264-410x(03)00071-9. [DOI] [PubMed] [Google Scholar]
- Gomila RC, Suphaphiphat P, Judge C, Spencer T, Ferrari A, Wen Y, Palladino G, Dormitzer PR, Mason PW. Improving influenza virus backbones by including terminal regions of MDCK-adapted strains on hemagglutinin and neuraminidase gene segments. Vaccine. 2013;31:4736–4743. doi: 10.1016/j.vaccine.2013.08.026. [DOI] [PubMed] [Google Scholar]
- Hartgroves LC, Koudstaal W, McLeod C, Moncorge O, Thompson CI, Ellis J, Bull C, Havenga MJ, Goudsmit J, Barclay WS. Rapid generation of a well-matched vaccine seed from a modern influenza A virus primary isolate without recourse to eggs. Vaccine. 2010;28:2973–2979. doi: 10.1016/j.vaccine.2010.02.012. [DOI] [PubMed] [Google Scholar]
- Harvey R, Guilfoyle KA, Roseby S, Robertson JS, Engelhardt OG. Improved antigen yield in pandemic H1N1 (2009) candidate vaccine viruses with chimeric hemagglutinin molecules. Journal of virology. 2011;85:6086–6090. doi: 10.1128/JVI.00096-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey R, Nicolson C, Johnson RE, Guilfoyle KA, Major DL, Robertson JS, Engelhardt OG. Improved haemagglutinin antigen content in H5N1 candidate vaccine viruses with chimeric haemagglutinin molecules. Vaccine. 2010;28:8008–8014. doi: 10.1016/j.vaccine.2010.09.006. [DOI] [PubMed] [Google Scholar]
- Horimoto T, Murakami S, Muramoto Y, Yamada S, Fujii K, Kiso M, Iwatsuki-Horimoto K, Kino Y, Kawaoka Y. Enhanced growth of seed viruses for H5N1 influenza vaccines. Virology. 2007;366:23–27. doi: 10.1016/j.virol.2007.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilyushina NA, Khalenkov AM, Seller JP, Forrest HL, Bovin NV, Marjuki H, Barman S, Webster RG, Webby RJ. Adaptation of pandemic H1N1 influenza viruses in mice. Journal of virology. 2010;84:8607–8616. doi: 10.1128/JVI.00159-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature. 2012;486:420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing X, Phy K, Li X, Ye Z. Increased hemagglutinin content in a reassortant 2009 pandemic H1N1 influenza virus with chimeric neuraminidase containing donor A/Puerto Rico/8/34 virus transmembrane and stalk domains. Vaccine. 2012;30:4144–4152. doi: 10.1016/j.vaccine.2012.04.073. [DOI] [PubMed] [Google Scholar]
- Kilbourne ED. Future influenza vaccines and the use of genetic recombinants. Bull World Health Organ. 1969;41:643–645. [PMC free article] [PubMed] [Google Scholar]
- Kilbourne ED, Murphy JS. Genetic studies of influenza viruses. I. Viral morphology and growth capacity as exchangeable genetic traits. Rapid in ovo adaptation of early passage Asian strain isolates by combination with PR8. J Exp Med. 1960;111:387–406. doi: 10.1084/jem.111.3.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koel BF, Burke DF, Bestebroer TM, van der Vliet S, Zondag GC, Vervaet G, Skepner E, Lewis NS, Spronken MI, Russell CA, Eropkin MY, Hurt AC, Barr IG, de Jong JC, Rimmelzwaan GF, Osterhaus AD, Fouchier RA, Smith DJ. Substitutions near the receptor binding site determine major antigenic change during influenza virus evolution. Science. 2013;342:976–979. doi: 10.1126/science.1244730. [DOI] [PubMed] [Google Scholar]
- Krause JC, Tsibane T, Tumpey TM, Huffman CJ, Basler CF, Crowe JE., Jr A broadly neutralizing human monoclonal antibody that recognizes a conserved, novel epitope on the globular head of the influenza H1N1 virus hemagglutinin. Journal of virology. 2011;85:10905–10908. doi: 10.1128/JVI.00700-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Myers JL, Bostick DL, Sullivan CB, Madara J, Linderman SL, Liu Q, Carter DM, Wrammert J, Esposito S, Principi N, Plotkin JB, Ross TM, Ahmed R, Wilson PC, Hensley SE. Immune history shapes specificity of pandemic H1N1 influenza antibody responses. J Exp Med. 2013;210:1493–1500. doi: 10.1084/jem.20130212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lugovtsev VY, Vodeiko GM, Levandowski RA. Mutational pattern of influenza B viruses adapted to high growth replication in embryonated eggs. Virus Res. 2005;109:149–157. doi: 10.1016/j.virusres.2004.11.016. [DOI] [PubMed] [Google Scholar]
- Meroz D, Yoon SW, Ducatez MF, Fabrizio TP, Webby RJ, Hertz T, Ben-Tal N. Putative amino acid determinants of the emergence of the 2009 influenza A (H1N1) virus in the human population. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:13522–13527. doi: 10.1073/pnas.1014854108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitnaul LJ, Matrosovich MN, Castrucci MR, Tuzikov AB, Bovin NV, Kobasa D, Kawaoka Y. Balanced hemagglutinin and neuraminidase activities are critical for efficient replication of influenza A virus. Journal of virology. 2000;74:6015–6020. doi: 10.1128/jvi.74.13.6015-6020.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann G, Watanabe T, Ito H, Watanabe S, Goto H, Gao P, Hughes M, Perez DR, Donis R, Hoffmann E, Hobom G, Kawaoka Y. Generation of influenza A viruses entirely from cloned cDNAs. Proceedings of the National Academy of Sciences of the United States of America. 1999;96:9345–9350. doi: 10.1073/pnas.96.16.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolson C, Major D, Wood JM, Robertson JS. Generation of influenza vaccine viruses on Vero cells by reverse genetics: an H5N1 candidate vaccine strain produced under a quality system. Vaccine. 2005;23:2943–2952. doi: 10.1016/j.vaccine.2004.08.054. [DOI] [PubMed] [Google Scholar]
- O’Donnell CD, Vogel L, Wright A, Das SR, Wrammert J, Li GM, McCausland M, Zheng NY, Yewdell JW, Ahmed R, Wilson PC, Subbarao K. Antibody pressure by a human monoclonal antibody targeting the 2009 pandemic H1N1 virus hemagglutinin drives the emergence of a virus with increased virulence in mice. MBio. 2012:3. doi: 10.1128/mBio.00120-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottmann M, Duchamp MB, Casalegno JS, Frobert E, Moules V, Ferraris O, Valette M, Escuret V, Lina B. Novel influenza A(H1N1) 2009 in vitro reassortant viruses with oseltamivir resistance. Antiviral therapy. 2010;15:721–726. doi: 10.3851/IMP1576. [DOI] [PubMed] [Google Scholar]
- Pan W, Dong Z, Meng W, Zhang W, Li T, Li C, Zhang B, Chen L. Improvement of influenza vaccine strain A/Vietnam/1194/2004 (H5N1) growth with the neuraminidase packaging sequence from A/Puerto Rico/8/34. Hum Vaccin Immunother. 2012;8:252–259. doi: 10.4161/hv.18468. [DOI] [PubMed] [Google Scholar]
- Pettersen EF, Goddard TD, Huang CC, Couch GS, Greenblatt DM, Meng EC, Ferrin TE. UCSF Chimera-a visualization system for exploratory research and analysis. J Comput Chem. 2004;25:1605–1612. doi: 10.1002/jcc.20084. [DOI] [PubMed] [Google Scholar]
- Robertson JS, Bootman JS, Newman R, Oxford JS, Daniels RS, Webster RG, Schild GC. Structural changes in the haemagglutinin which accompany egg adaptation of an influenza A(H1N1) virus. Virology. 1987;160:31–37. doi: 10.1016/0042-6822(87)90040-7. [DOI] [PubMed] [Google Scholar]
- Robertson JS, Nicolson C, Harvey R, Johnson R, Major D, Guilfoyle K, Roseby S, Newman R, Collin R, Wallis C, Engelhardt OG, Wood JM, Le J, Manojkumar R, Pokorny BA, Silverman J, Devis R, Bucher D, Verity E, Agius C, Camuglia S, Ong C, Rockman S, Curtis A, Schoofs P, Zoueva O, Xie H, Li X, Lin Z, Ye Z, Chen LM, O’Neill E, Balish A, Lipatov AS, Guo Z, Isakova I, Davis CT, Rivailler P, Gustin KM, Belser JA, Maines TR, Tumpey TM, Xu X, Katz JM, Klimov A, Cox NJ, Donis RO. The development of vaccine viruses against pandemic A(H1N1) influenza. Vaccine. 2011;29:1836–1843. doi: 10.1016/j.vaccine.2010.12.044. [DOI] [PubMed] [Google Scholar]
- Rogers GN, Paulson JC, Daniels RS, Skehel JJ, Wilson IA, Wiley DC. Single amino acid substitutions in influenza haemagglutinin change receptor binding specificity. Nature. 1983;304:76–78. doi: 10.1038/304076a0. [DOI] [PubMed] [Google Scholar]
- Schymkowitz JW, Rousseau F, Martins Ie, Ferkinghoff-Borg J, Stricher F, Serrano L. Prediction of water and metal binding sites and their affinities by using the Fold-X force field. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:10147–10152. doi: 10.1073/pnas.0501980102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner R, Matrosovich M, Klenk HD. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev Med Virol. 2002;12:159–166. doi: 10.1002/rmv.352. [DOI] [PubMed] [Google Scholar]
- Wan L, Twitchett MB, Eltis LD, Mauk AG, Smith M. In vitro evolution of horse heart myoglobin to increase peroxidase activity. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:12825–12831. doi: 10.1073/pnas.95.22.12825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle JR, Zhang R, Khurana S, King LR, Manischewitz J, Golding H, Dormitzer PR, Haynes BF, Walter EB, Moody MA, Kepler TB, Liao HX, Harrison SC. Broadly neutralizing human antibody that recognizes the receptor-binding pocket of influenza virus hemagglutinin. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:14216–14221. doi: 10.1073/pnas.1111497108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widjaja L, llyushina N, Webster RG, Webby RJ. Molecular changes associated with adaptation of human influenza A virus in embryonated chicken eggs. Virology. 2006;350:137–145. doi: 10.1016/j.virol.2006.02.020. [DOI] [PubMed] [Google Scholar]
- Wu NC, Young AP, Dandekar S, Wijersuriya H, Al-Mawsawi LQ, Wu TT, Sun R. Systematic identification of H274Y compensatory mutations in influenza A virus neuraminidase by high-throughput screening. Journal of virology. 2013;87:1193–1199. doi: 10.1128/JVI.01658-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R, Krause JC, McBride R, Paulson JC, Crowe JE, Jr, Wilson IA. A recurring motif for antibody recognition of the receptor-binding site of influenza hemagglutinin. Nat Struct Mol Biol. 2013;20:363–370. doi: 10.1038/nsmb.2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye J, Sorrell EM, Cai Y, Shao H, Xu K, Pena L, Hickman D, Song H, Angel M, Medina RA, Manicassamy B, Garcia-Sastre A, Perez DR. Variations in the hemagglutinin of the 2009 H1N1 pandemic virus: potential for strains with altered virulence phenotype? PLoS Pathog. 2010;6:el001145. doi: 10.1371/journal.ppat.1001145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zang H, Irimia A, Choi JY, Angel KC, Loukachevitch LV, Egli M, Guengerich FP. Efficient and high fidelity incorporation of dCTP opposite 7,8-dihydro-8-oxodeoxyguanosine by Sulfolobus solfataricus DNA polymerase Dpo4. J Biol Chem. 2006;281:2358–2372. doi: 10.1074/jbc.M510889200. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.