Abstract
BACKGROUND
Sexual minority girls (SMGs) report large substance use disparities and victimization experiences, yet there is a dearth of research that focuses exclusively on SMGs.
OBJECTIVE
To examine substance use and mental health disparities among SMGs and to determine whether disparities were larger for African American compared with European American girls.
METHOD
Data were used from Wave 11 of the Pittsburgh Girls Study, a multiple-cohort, prospective study of urban girls. Girls for the current analysis were aged 16 to 19 years. Fifty-five percent were African American. One hundred and seventy-three (8.3%) identified as SMGs, and 1,891 identified as heterosexual. Multiple regression analyses controlling for age, race, and parent education were conducted.
RESULTS
SMGs reported a robust pattern of large disparities in externalizing, internalizing, and borderline personality disorder symptoms. There was little evidence to suggest disparities were moderated by race.
CONCLUSION
SMGs and their families would benefit from intervention and prevention programs to reduce disparities among this highly vulnerable population.
Keywords: adolescent girls, sexual orientation, mental health, substance use, intersectionality
Substance use and mental health problems such as depression and suicidality are leading causes of adolescent morbidity and mortality (Lawrence, Gootman, & Sim, 2009); thus, it is critical that we identify individuals at high risk for such problems and develop interventions that can help reduce them. The minority stress hypothesis (Meyer, 2003; Rosario, Schrimshaw, Hunter, & Gwadz, 2002) suggests that compared with heterosexual individuals, lesbian, gay, and bisexual individuals experience higher levels of substance use and mental health problems due to minority stress experiences including discrimination and violent victimization. Evidence from the adolescent literature consistently shows that sexual minority youth (SMY; youth who report same-sex romantic or sexual attraction and/or same-sex behavior, orientation, or identity), compared with heterosexual youth, report higher levels of substance use, depression, and suicidality (Kann et al., 2011; Marshal et al., 2008; Marshal et al., 2011).
Compared with disparities among sexual minority boys, substance use disparities (Marshal et al., 2008) and disparities in some forms of violent victimization (Friedman et al., 2011) are higher among sexual minority girls (SMGs). Despite the potential higher risk for some negative outcomes among SMGs, historically research has either combined boys and girls or only focused on behavioral health problems (such as HIV risk behavior) among sexual minority boys. In contrast, relatively few studies have focused on the health and wellness of SMGs exclusively (however see Hipwell et al., 2013; Marshal, King, et al., 2012; Marshal, Sucato, et al., 2012), leaving a large gap in the literature and a dearth of understanding of SMG disparities and potential for long-term health problems. The primary goals of this article were to examine differences in the prevalence of internalizing symptoms (e.g., anxiety, depression symptoms, and suicidal thoughts), externalizing symptoms (e.g., substance use, oppositional defiant disorder, and conduct disorder symptoms), and internalizing–externalizing symptoms (borderline personality disorder symptoms, including self-injury) between heterosexual girls and SMGs.
Internalizing Symptoms Among Sexual Minority Girls
High rates of suicidality and depression symptoms in SMY are especially concerning for girls because evidence has long shown that adolescent girls suffer higher rates of depression than adolescent boys (Costello, Erkanli, & Angold, 2006). Although suicide mortality rates are higher for males than females regardless of sexual orientation (Nock et al., 2008), adolescent females are more likely to report having considered attempting suicide, made a suicide plan, and attempted suicide (Eaton et al., 2012). Lesbian and bisexual women are more likely to be depressed and to express suicidal ideation than are heterosexual women (King et al., 2008), which underscores the need to detect and prevent depression symptoms in adolescence. Rates of anxiety symptoms and disorders are also higher among adolescent girls compared with boys (Albano & Krain, 2005). There are relatively few studies in the SMY literature that examine anxiety disparities, although there is ample evidence that such disparities exist among sexual minority adults (King et al., 2008). In this article, we sought to build on the existing SMY disparities research by examining and reporting anxiety symptom disparities among SMGs.
Externalizing Symptoms Among Sexual Minority Girls
Substance use disparities are twice as large for sexual minority girls (odds ratio [OR] = 5.02) than for sexual minority boys (OR = 1.90; Marshal et al., 2008). Although the prevalence of substance use in adolescence is higher among boys than girls, any substance use by girls can be problematic because the threshold for resulting mental health outcomes may be lower among girl substance users, and because females show a more rapid progression from initiation of use to problem use (Johnson, Richter, Kleber, McLellan, & Carise, 2005; Randall et al., 1999). Some substance use behaviors, such as binge drinking, can pose unique health risks among girls such as sexual victimization (Champion et al., 2004) and unintended pregnancy due to risky sexual behavior when intoxicated (Nolen-Hoeksema, 2004).
Adolescents with behavioral disorders such as oppositional defiant disorder (ODD) and conduct disorder (CD) are at a greater risk for depression than those without ODD and CD (Wolff & Ollendick, 2006), and girls with disruptive behavior disorders may be more likely than boys to suffer from comorbid disorders, including depression, substance use, and antisocial personality disorder (Keenan, Loeber, & Green, 1999). The consequences of behavioral disorders such as CD are serious, including an increased risk compared with peers for arrest, high school dropout, unintended pregnancy, early and violent death, and substance dependence (Zoccolillo, Tremblay, & Vitraro, 1996). CD is the second-most common psychiatric diagnosis in adolescent girls, yet research studying CD in girls is limited because the disorder is more commonly diagnosed in boys (e.g., Hipwell & Loeber, 2006). There are even fewer studies focusing on CD in SMGs, yet risks for this population may be even more serious due to comorbidities. For example, in a study of 428 runaway adolescents in eight Midwestern cities, Whitbeck, Chen, Hoyt, Tyler, and Johnson (2004) found lesbian adolescent runaways to be more likely than heterosexual females to meet criteria for CD, as well as posttraumatic stress disorder and substance abuse. Another goal of this study therefore is to examine and describe SMG disparities in externalizing disorder symptoms such as ODD and CD in order to determine their potential contribution to long-term substance use and mental health problems.
Borderline Personality Disorder Symptoms in Sexual Minority Girls
Borderline personality disorder (BPD) is characterized by a heterogeneous set of symptoms that include impulsivity, affect dysregulation, and dysfunctional interpersonal relationships (American Psychiatric Association, 2000). When compared with other psychiatric disorders, BPD is distinct in the nosological landscape by its position on both the internalizing and externalizing dimensions of psychopathology (Eaton et al., 2011; James & Taylor, 2008). Several developmental theories of BPD place disruptions in the emotional system as key in the subsequent manifestation of other BPD features (Linehan, 1993; Putnam & Silk, 2005). Linehan’s (1993) biosocial theory of BPD is one of the most thoroughly delineated etiological models of BPD. According to the biosocial theory, BPD is primarily a disorder of the emotion regulation system and emerges from transactions between individuals with biological vulnerabilities to emotion sensitivity and environmental influences, specifically an invalidating family environment. Emotion dysregulation subsequently leads to maladaptive behavior patterns as either a direct consequence or to cope with the emotional response. Additionally, individuals with BPD engage in impulsive behaviors, such as substance use, and self-injury to regulate intense and sustained negative affective states (Brown, Comtois, & Linehan, 2002; Yen et al., 2004).
These hypotheses regarding the role of the invalidating environment in escalating emotion dysregulation are highly congruent with the minority stress hypothesis (Meyer, 2003; Rosario et al., 2002), which asserts that substance use and mental health disparities can be attributed to experiences with discrimination and violent victimization generated from many different social environments, including from within the family. Homophobia and its negative social consequences, including discrimination and violence toward SMY, most likely cause disruptions in family relationships and difficulties integrating sexual orientation and identity into one’s sense of self. There is ample evidence that SMY suffer from highly invalidating environments. For example, a recent meta-analysis showed that SMY report much higher rates of several forms of violent victimization including childhood sexual abuse, parent physical abuse, and being threatened by peers at school with a weapon (Friedman et al., 2011). And a long rich history of within-group studies show that SMY report distressingly high levels of gay-related bullying and victimization (D’Augelli, Pilkington, & Hershberger, 2002; Rosario et al., 2002). Recent research shows that there are higher rates of suicide behaviors among SMY living in socially conservative and presumably homophobic neighborhoods (Hatzenbuehler, 2011). Thus, based on minority stress theory, and an abundance of evidence suggests SMY suffer from highly invalidating environments, we hypothesize that these experiences may lead to higher rates of BPD symptoms among SMGs compared with heterosexual girls.
Examining the Intersection Between Sexual Orientation and Race
Rooted in critical race and feminist theories, a growing interest has developed over the past 10 years in the social sciences in whether and how multiple minority identities (e.g., gender, race, and sexual orientation), and important social stressors associated with minority experiences, might intersect in such a way to increase risk for substance use and mental health outcomes (Cole, 2009). The basic tenets and hypotheses of intersectionality are compelling from the perspective of understanding risk for health disparities among SMY. Given a long history of race-related health disparities due to minority stressors documented in the health sciences literature, and the potentially higher levels of homophobia in the African American community (see Dyer et al., 2012; Jeffries, Marks, Lauby, Murrill, & Millett, 2012), might African American SMGs be at higher risk for negative health outcomes than are European American SMGs due to the potential compounding and synergistic negative effects of multiple minority stress conditions? The final goal of this study is to examine whether or not there are significant interactions between sexual orientation and race predicting higher rates of substance use and mental health problems than we would observe if the combined effects of more than one minority identity were simply additive.
Method
Study Participants and Design
The Pittsburgh Girls Study (PGS) is a multiple-cohort, prospective study of urban girls designed to investigate the development of conduct problems and depression. Low-income neighborhoods were oversampled to have sufficient power to examine the effects of socioeconomic factors on psychopathology. Of 2,876 girls who were eligible by virtue of their age and who could also be located, 2,451 (85.2%) agreed to participate in the longitudinal study (see Hipwell et al., 2002; Keenan et al., 2010, for further details about the study design). Girls have been assessed annually since 2000 (Wave 1) when they were 5, 6, 7, and 8 years old. The University of Pittsburgh Institutional Review Board approved all study procedures. Prior to data collection, caregivers provided written informed consent and the girls provided verbal and written assent when developmentally appropriate.
Questions assessing sexual orientation were added to the PGS for the oldest cohort in 2008, which were used to conduct a pilot study (Marshal, King, et al., 2012; Marshal, Sucato, et al., 2012). The current study examined the most recent data available (Wave 11, ages 16–19; 86% retention) in which girls reported sexual orientation. Participants who responded to the sexual identity item in Wave 11 were included in the analyses (N = 2,064). The mean age of the sample was 17.20 years (SD = 1.28), and 39% of the girls were European American, 55% were African American, and about 6% were multiracial or representing another race.
Measures
Sexual Orientation
SMGs (n = 173, 8.3%) were self-identified. Participants were asked to endorse if they had a lesbian (n = 32), bisexual (n = 141), or heterosexual identity (n = 1,891) at Wave 11 using the following question: “Do you consider yourself to be (a) Heterosexual or straight; (b) Gay or lesbian; or (c) Bisexual?” Given the small number of bisexual and lesbian/gay girls, the two groups of girls were combined into a single SMGs group for the analyses.
Demographics
Demographic characteristics collected from the participants’ caretakers included each girl’s age, race (coded as European American = 0 and African American/other racial minority = 1), and caretaker’s highest level of education at Wave 11, with the exception that only Wave 10 caretaker education was available for girls in the oldest cohort. Level of education was dichotomized to represent low education (less than or equal to 12 years) or high education (greater than 12 years).
Externalizing Disorder Symptoms
Girls’ report of the frequency of substance use was assessed by the Nicotine, Alcohol, and Drug Use scale (adapted from Pandina, Labouvie, & White, 1984). In the current study, drug use outcomes were treated as binary variables indicating any past year use of cigarettes, marijuana or alcohol, or binge drinking (i.e., five or more drinks in one sitting). ODD and CD symptoms in the past year were assessed using a DSM-IV-based questionnaire: the Adolescent Self-Report Inventory–4 (Gadow & Sprafkin, 1998) though age 17 and the Adult Self-Report Inventory–4 (Gadow, Sprafkin, & Weiss, 2004) from age 18 years. Eight ODD symptoms were scored on 4-point scales (0 = never to 3 = very often). Through age 17, 15 CD symptoms, and from age 18, 13 CD were assessed. For each participant the average of the items was calculated yielding ODD and CD continuous scale scores with a possible range of 0 to 3.
Internalizing Disorder Symptoms
Depression symptom severity and suicidal ideation in the past year were assessed using the Adolescent Symptom Self-Report Inventory–4 (Gadow & Sprafkin, 1998) until age 18 when the Adult Self-Report Inventory–4 (Gadow et al., 2004) was used. Suicidal ideation was examined as a dichotomous outcome indicating if participants reported any suicidal ideation during the past year. Past year anxiety symptoms were operationalized as the total summary score on the Self-Report for Childhood Anxiety Related Disorders (Birmaher et al., 1997).
BPD Symptoms and Indicators
BPD symptoms were defined as the count of the 9 BPD items on the International Personality Disorders Examination (Smith, Muir, & Blackwood, 2005) used in other recent investigations with the current data set (Stepp, Burke, Hipwell, & Loeber, 2012). Self-injury was measured with a single item from the SCID-I (First, Spitzer, Gibbon, & Williams, 1996).
Statistical Analysis
Multiple regression analysis in SPSS was used to predict mental health problems, suicidal ideation, and substance use from SMY status after controlling for all study covariates: age, race, and parent education. Heterosexual girls were the reference group. Logistic or linear regression methods were used for dichotomous or continuous outcomes, respectively. Power analyses indicated that the sample size of the study (N = 2,064) provided ample statistical power (>.80) to detect a small main effect sizes (f2 = .02) using both multiple and logistic regression (Cohen, 1988; Faul, Erdfelder, Lang, & Buchner, 2007).
Next, we examined the potential moderating effects of race on the relation between sexual orientation and the outcome variables. For the moderation analyses, we excluded ethnic/racial minority participants who were not African American (Asian American, n = 12, and girls who endorsed a multiracial heritage, n = 103) to simplify our test of intersectionality reducing our total sample size for the interaction tests to 1,949. According to Aiken and West (1991), we had ample statistical power (>.80) to detect small interaction effects (assuming modest measurement reliability of .80) with this sample size. Interaction terms between sexual orientation and race were entered into the models with the main effects and controlling for the other covariates to determine if the effects of sexual orientation on mental health outcomes differed across racial groups. Significant interaction effects (p < .05) were further examined using simple slope analyses (Aiken & West, 1991).
Results
Table 1 provides the descriptive statistics for the outcome variables and demographic covariates for each group. Compared with heterosexual girls, SMGs reported significantly higher levels of all the mental health and substance use outcomes examined in the current study (Table 2). Specifically, SMGs demonstrated at least a twofold risk of engaging in any alcohol use (OR = 2.71, p < .001) or binge drinking (OR = 2.96, p < .001) compared with heterosexual girls in the past year. SMGs were also over five times more likely to report any cigarette use (OR = 5.18, p < .001) or any self-harm (OR = 6.87, p < .001) than heterosexual girls in the past year. They were nearly four times more likely to report marijuana use (OR = 3.61, p < .001) and suicidal ideation (OR = 4.43, p < .001) than heterosexual girls in the past year. Furthermore, SMG status corresponded with significantly higher symptom severity of CD (β = .18, p < .001), ODD (β = .11, p < .001), BPD (β = .16, p < .001), anxiety (β = .05, p < .05), and depression (β = .16, p < .001). These effects were observed even after controlling for age, race, and parent education.
Table 1.
Substance Use and Mental Health Outcomes, and Demographic Characteristics of Sexual Minority Girls and Heterosexual Girls in the Pittsburgh Girls Study.
| Sexual minority girls (n = 173) | Heterosexual girls (n = 1,891) | |
|---|---|---|
| Externalizing disorder symptoms | ||
| Alcohol use | 59.5% | 37.3% |
| Binge drinking | 32.9% | 15.8% |
| Cigarette use | 49.1% | 17.3% |
| Marijuana use | 50.3% | 21.0% |
| CD | 0.15 (0.19) | 0.08 (0.11) |
| ODD | 0.83 (0.52) | 0.83 (0.53) |
| Internalizing disorder symptoms | ||
| Anxiety | 15.10 (10.40) | 13.43 (9.44) |
| Depression | 0.85 (0.52) | 0.59 (0.43) |
| Suicidal ideation | 26.0% | 7.2% |
| BPD symptoms | ||
| BPD symptoms | 3.28 (2.10) | 2.19 (1.79) |
| Self-injury | 9.5% | 1.6% |
| Covariates | ||
| Minority race | 64.2% | 60.5% |
| Low parent education | 41.6% | 43.2% |
| Age | 17.35 (1.25) | 17.18 (1.28) |
Note. ODD = oppositional defiant disorder; CD = conduct disorder; BPD = borderline personality disorder. The table summarizes the percentage of girls in each sexual orientation group that endorsed each dichotomous outcome or the mean level (standard deviation) for each continuous outcome within each sexual orientation group.
Table 2.
Relations Between Sexual Orientation and Demographic Variables With Substance Use and Mental Health Outcomes in the Pittsburgh Girls Study.
| SMG status | Age | Minority race | Low parent education | |
|---|---|---|---|---|
| Externalizing symptoms | ||||
| Alcohol usea | 2.71 (1.92–3.82)*** | 1.57 (1.45–1.70)*** | 0.42 (0.35–0.51)*** | 0.78 (0.64–0.94)* |
| Binge drinkinga | 2.96 (2.03–4.31)*** | 1.83 (1.64–2.04)*** | 0.40 (0.31–0.52)** | 0.78 (0.60–1.01) |
| Cigarette usea | 5.18 (3.66–7.31)*** | 1.47 (1.34–1.62)*** | 0.47 (0.37–0.60)*** | 1.42 (1.12–1.80)** |
| Marijuana usea | 3.61 (2.60–5.03)*** | 1.33 (1.22–1.45)*** | 1.15 (0.92–1.43) | 1.01 (0.88–1.36) |
| ODDb | 0.11*** | −0.05* | 0.07** | 0.04 |
| CDb | 0.18*** | −0.04* | 0.08*** | 0.04 |
| Internalizing symptoms | ||||
| Anxietyb | 0.05* | −0.05* | 0.03 | 0.07** |
| Depressionb | 0.16*** | −0.02 | 0.01 | 0.05* |
| Suicidal ideationa | 4.43 (2.99–6.57)*** | 1.01 (0.89–1.146) | 0.66 (0.48–0.90)* | 1.03 (0.75–1.42) |
| BPD symptoms | ||||
| BPD symptomsb | 0.16*** | −0.07** | 0.11*** | 0.09*** |
| Self-injurya | 6.87 (3.57–13.24)*** | 0.82 (0.64–1.05) | 0.37 (0.20–0.70)** | 0.92 (0.49–1.72) |
Note. ODD = oppositional defiant disorder; CD = conduct disorder; BPD = borderline personality disorder.
Reported effects are odds ratios (95% confidence interval) that were estimated using logistic regression.
Reported effects are standardized regression coefficients estimated using multiple linear regression models.
p < .05.
p < .01.
p < .001.
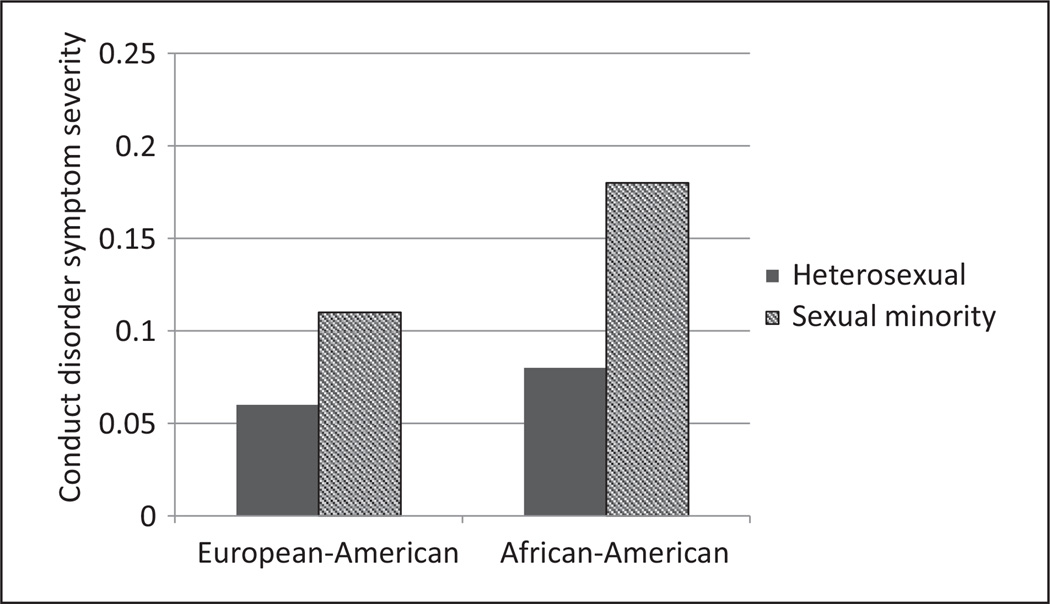
There was a significant interaction between sexual orientation status and race predicting CD (β = .09, p < .02). Consistent with intersectionality theory, the largest disparities between sexual minority girls and heterosexual girls were detected among African American girls (β = .20, p < .001) compared with CD disparities for European American girls, which was significant but much smaller (β = .12, p < .01; see Figure 1); however, the remaining 10 interaction terms were not significant by conventional standards (all ps > .05).
Figure 1.
Racial and sexual orientation differences of conduct disorder symptoms levels.
Discussion
The results of this study demonstrate a pronounced pattern of SMG substance use and mental health disparities across several broad domains of internalizing and externalizing disorder symptoms and borderline personality disorder symptoms and provide several valuable contributions to the literature. First, it is one of the first studies to examine and report SMG group differences in externalizing problems such as ODD and CD. Historically, SMGs have reported higher rates of substance use and abuse compared with heterosexual girls, and this disparity may be larger for SMGs than it is for sexual minority boys (Marshal et al., 2008). According to problem behavior theory (Donovan & Jessor, 1985), externalizing behaviors such as substance use, ODD, and CD symptoms are part of a larger syndrome of problem behaviors that are expected to be highly correlated among high-risk youth. Results from this study are consistent with the tenets of this theory, demonstrating that SMGs are more likely to report higher rates of substance use, ODD, and CD. More research is needed to understand whether these behaviors are more likely to cluster together among SMGs.
Second, this study is one of the first to report higher rates of BPD symptoms among SMGs compared with heterosexual girls. Recent evidence from the current sample of girls shows that childhood attention deficit hyper-activity disorder and ODD symptom trajectories are associated with BPD symptoms at age 14 (Stepp et al., 2012). The origins of BPD are thought to be in part due to predisposing biological vulnerabilities in the context of a highly invalidating social or contextual environment (Crowell, Beauchaine, & Linehan, 2009). Indeed, for many SMGs, social and contextual invalidation of one’s gay/lesbian or bisexual identity is an incessant and pervasive social stressor (Meyer, 2003; Rosario et al., 2002) that occurs in multiple contexts including the home, school, church, government, and more. Although we did not assess and test differential rates of BPD diagnosis, our results showing (a) a higher level of BPD symptoms among SMGs and (b) higher levels of some precursors of BPD including ODD symptoms in this same sample (Stepp et al., 2012) suggest that SMGs may be at increased risk for developing BPD.
Third, this study provides very little evidence to suggest that for some girls and young women, a combination of gay-related stressors and race-related stressors may synergistically interact to produce a higher level of outcomes. We found only one significant interaction effect (out of 11 total tests) showing that conduct disorder symptom disparities were larger for African American SMGs than they were for European American SMGs. This lack of strong support for the intersectionality hypothesis has been demonstrated in other large studies examining SMY disparities that also found few significant interactions with race (Talley, Aranda, Birkett, Marshal, & Hughes, in press). One possible explanation for these null findings is that we did not measure and examine stressors associated with sexual orientation and race status, per se, but other factors associated with sexual minority and racial minority identities. Future research that attempts to replicate these findings and more closely examine the potential driving mechanisms underlying the interaction effects is warranted.
Finally, this study adds to the small literature that focuses exclusively on SMGs. Previous studies in the SMY literature have identified robust gender differences of substance use (Marshal et al., 2008) and the experience of some social stressors, such as being threatened by peers in school (Friedman et al., 2011). These early gender disparities warrant additional attention as some of these adolescent experiences may be precursors to disparities experienced by lesbian adults (Cochran, Ackerman, Mays, & Ross, 2004; Hughes & Wilsnack, 1997; King et al., 2008). Our recent research examining trajectories of substance use, depression, and suicide disparities among SMGs supports this hypothesis, showing that disparities in adolescence persist or even increase as SMGs transition to young adulthood (Dermody et al., 2013; Marshal, Burton, Chisolm, Sucato, & Friedman, 2013; Marshal, King, et al., 2012; Marshal, Sucato, et al., 2012).
There are several limitations of the current study. We conducted a cross-sectional investigation; thus, we cannot make statements about long-term disparities or outcomes among SMGs. Nor were we able to examine factors associated with the coming out process, and whether change in sexual orientation over time and the timing of coming out, for example, was associated with concomitant changes in mental health symptoms over time. Second, results from this study are not generalizable to all girls in Pittsburgh or other similarly sized cities because girls from low-income neighborhoods were oversampled. Also, despite having a relatively large sample of SMGs, only a small proportion identified as gay/ lesbian because the majority of SMGs in our study identified as bisexual. Previous studies have shown that heterogeneity with respect to how youth identify (gay vs. bisexual) accounts for much of the variability in outcomes among SMY; thus, understanding these potential influences is important. Future longitudinal studies using the PGS sample will be able to describe change over time in SMG self-identification and will further elucidate the role of SMG identity on disparities.
In summary, using a large epidemiological sample of adolescent girls and young women, we found a very robust pattern of large substance use and mental health disparities after controlling for several key demographic covariates including age, race, and socioeconomic status. We also found that the size of the disparities was the same for almost all of our outcomes across African American and European American subsamples. Despite these alarmingly big disparities reported by SMGs, it is important to recognize that many SMGs did not report substance use or mental health problems. For example, most SMGs did not report a history of binge drinking. Furthermore, the vast majority of SMGs did not report a history of suicidality or nonsuicidal self-harm. It will be important for future research to focus on SMGs who are happy and healthy despite the potentially high levels of adversity they face living in a very homophobic and violent culture. Researchers, clinicians, and especially SMGs and their families will benefit from more research to help elucidate the best mechanisms for reducing distress in this highly vulnerable population, and preventing long-term serious substance use and mental health problems.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This manuscript was supported by the National Institutes of Health (grant numbers MH056630, DA012237, and DA030385).
MPM conceived of the study, participated in its design and coordination and drafted the manuscript; SSD participated in the design of the study, conducted all of the statistical analyses, and drafted the Method and Results sections; MPM, SDS, NM, TC and AEH contributed to data analysis decisions and data interpretation; All authors contributed to writing components of the Introduction and Discussion. All authors read, edited, and approved the final manuscript.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Aiken L, West S. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Albano AM, Krain A. Anxiety and anxiety disorders in girls. In: Bell DJ, Foster SL, Mash EJ, editors. Handbook of behavioral and emotional problems in girls. New York, NY: Springer; 2005. pp. 79–116. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Arlington, VA: American Psychiatric Publishing; 2000. text revision. [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, McKenzie Neer S. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and non-suicidal self-injury in women with borderline personality disorder. Journal of Abnormal Psychology. 2002;111:198–202. doi: 10.1037//0021-843x.111.1.198. [DOI] [PubMed] [Google Scholar]
- Champion HL, Foley KL, Durant RH, Hensberry R, Altman D, Wolfson M. Adolescent sexual victimization, use of alcohol and other substances, and other health risk behaviors. Journal of Adolescent Health. 2004;35:321–328. doi: 10.1016/j.jadohealth.2003.09.023. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Ackerman D, Mays VM, Ross MW. Prevalence of non-medical drug use and dependence among homosexually active men and women in the US population. Addiction. 2004;99:989–998. doi: 10.1111/j.1360-0443.2004.00759.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cole ER. Intersectionality and research in psychology. American Psychologist. 2009;64:170–180. doi: 10.1037/a0014564. [DOI] [PubMed] [Google Scholar]
- Costello JE, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? Journal of Child Psychology and Psychiatry. 2006;47:1263–1271. doi: 10.1111/j.1469-7610.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin. 2009;135:495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Augelli AR, Pilkington NW, Hershberger SL. Incidence and mental health impact of sexual orientation victimization of lesbian, gay, and bisexual youths in high school. School Psychology Quarterly. 2002;17:148–167. [Google Scholar]
- Dermody SS, Marshal MP, Cheong JW, Burton CM, Friedman MS, Aranda F, Hughes T. Longitudinal disparities of hazardous drinking between sexual minority and heterosexual individuals from adolescence to young adulthood. Journal of Youth and Adolescence. 2013 doi: 10.1007/s10964-013-9905-9. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE, Jessor R. Structure of problem behavior in adolescence and young adulthood. Journal of Consulting and Clinical Psychology. 1985;53:890–904. doi: 10.1037//0022-006x.53.6.890. [DOI] [PubMed] [Google Scholar]
- Dyer TP, Shoptaw S, Guadamuz TE, Plankey M, Kao U, Ostrow D, Stall R. Application of Syndemic Theory to black men who have sex with men in the multicenter AIDS cohort study. Journal of Urban Health. 2012;89:697–708. doi: 10.1007/s11524-012-9674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Wechsler H. Youth risk behavior surveillance—United States, 2011. MMWR Surveillance Summary. 2012;61(SS04):1–162. [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, Hasin DS. Borderline personality disorder co-morbidity: Relationship to the internalizing-externalizing structure of common mental disorders. Psychological Medicine. 2011;41:1041–1050. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-1-CV) Washington, DC: American Psychiatric Press; 1996. [Google Scholar]
- Friedman MS, Marshal MP, Guadamuz TE, Wei C, Wong CF, Saewyc EM, Stall R. A meta-analysis of disparities in childhood sexual abuse, parental physical abuse, and peer victimization among sexual minority and sexual nonminority individuals. American Journal of Public Health. 2011;101:1481–1494. doi: 10.2105/AJPH.2009.190009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadow K, Sprafkin J. Child Symptom Inventory–4 screening manual. Stony Brook, NY: Checkmate Plus; 1998. [Google Scholar]
- Gadow K, Sprafkin J, Weiss M. The Adult Self-Report Inventory–4. Stony Brook, NY: Checkmate Plus; 2004. [Google Scholar]
- Hatzenbuehler ML. The social environment and suicide attempts in lesbian, gay, and bisexual youth. Pediatrics. 2011;127:896–903. doi: 10.1542/peds.2010-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipwell AE, Loeber R. Do we know which interventions are effective for disruptive and delinquent girls? Clinical Child and Family Psychology Review. 2006;9:221–255. doi: 10.1007/s10567-006-0012-2. [DOI] [PubMed] [Google Scholar]
- Hipwell AE, Loeber R, Stouthamer-Loeber M, Keenan K, White HR, Kroneman L. Characteristics of girls with early onset disruptive and antisocial behaviour. Criminal Behaviour and Mental Health. 2002;12:99–118. doi: 10.1002/cbm.489. [DOI] [PubMed] [Google Scholar]
- Hipwell AE, Stepp SD, Keenan K, Allen A, Hoffmann A, Rottingen L, McAloon R. Examining links between sexual risk behaviors and dating violence involvement as a function of sexual orientation. Journal of Pediatric and Adolescent Gynecology. 2013;26:212–218. doi: 10.1016/j.jpag.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes TL, Wilsnack SC. Use of alcohol among lesbians: Research and clinical implications. American Journal of Orthopsychiatry. 1997;67:20–36. doi: 10.1037/h0080208. [DOI] [PubMed] [Google Scholar]
- James LM, Taylor J. Revisiting the structure of mental disorders: Borderline personality disorder and the internalizing/externalizing spectra. British Journal of Clinical Psychology. 2008;47:361–380. doi: 10.1348/014466508X299691. [DOI] [PubMed] [Google Scholar]
- Jeffries WLIV, Marks G, Lauby J, Murrill CS, Millett GA. Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among black men who have sex with men. AIDS and Behavior. 2012;17:1–12. doi: 10.1007/s10461-012-0189-y. [DOI] [PubMed] [Google Scholar]
- Johnson PB, Richter L, Kleber HD, McLellan AT, Carise D. Telescoping of drinking-related behaviors: Gender, racial/ethnic, and age comparisons. Substance Use & Misuse. 2005;40:1139–1151. doi: 10.1081/JA-200042281. [DOI] [PubMed] [Google Scholar]
- Kann L, Olsen EO, McManus T, Kinchen S, Chyen D, Harris WA, Wechsler H. Sexual identity, sex of sexual contacts, and health-risk behaviors among students in grades 9–12—Youth risk behavior surveillance, selected sites, United States, 2001–2009. MMWR CDC Surveillance Summaries. 2011;60(SS07):1–133. [PubMed] [Google Scholar]
- Keenan K, Hipwell A, Chung T, Stepp S, Stouthamer-Loeber M, Loeber R, McTigue K. The Pittsburgh Girls Study: Overview and initial findings. Journal of Clinical Child & Adolescent Psychology. 2010;39:506–521. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Loeber R, Green S. Conduct disorder in girls: A review of the literature. Clinical Child and Family Psychology Review. 1999;2:3–19. doi: 10.1023/a:1021811307364. [DOI] [PubMed] [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, Nazareth I. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008;8:70. doi: 10.1186/1471-244X-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence RS, Gootman JA, Sim LJ. Adolescent health services: Missing opportunities. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Marshal MP, Burton CM, Chisolm DJ, Sucato GS, Friedman MS. Cross-sectional evidence for a stress-negative affect pathway to substance use among sexual minority girls. Clinical and Translational Science. 2013;6:321–322. doi: 10.1111/cts.12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J, Brent DA. Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review. Journal of Adolescent Health. 2011;49:115–123. doi: 10.1016/j.jadohealth.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R, King KM, Miles J, Gold MA, Morse JQ. Sexual orientation and adolescent substance use: A meta-analysis and methodological review. Addiction. 2008;103:546–556. doi: 10.1111/j.1360-0443.2008.02149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, King KM, Stepp SD, Hipwell A, Smith H, Chung T, Markovic N. Trajectories of alcohol and cigarette use among sexual minority and heterosexual girls. Journal of Adolescent Health. 2012;50:97–99. doi: 10.1016/j.jadohealth.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Sucato G, Stepp SD, Hipwell A, Smith HA, Friedman MS, Markovic N. Substance use and mental health disparities among sexual minority girls: Results from the Pittsburgh girls study. Journal of Pediatric and Adolescent Gynecology. 2012;25:15–18. doi: 10.1016/j.jpag.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clinical Psychology Review. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Pandina RJ, Labouvie EW, White HR. Potential contributions of the life span developmental approach to the study of adolescent alcohol and drug use-the Rutgers Health and Human Development Project. Journal of Drug Issues. 1984;14:253–268. [Google Scholar]
- Putnam KM, Silk KR. Emotion dysregulation of the development of borderline personality disorder. Development and Psychopathology. 2005;17:899–925. doi: 10.1017/s0954579405050431. [DOI] [PubMed] [Google Scholar]
- Randall CL, Roberts JS, Del Boca FK, Carroll KM, Connors GJ, Mattson ME. Telescoping of landmark events associated with drinking: A gender comparison. Journal of Studies on Alcohol and Drugs. 1999;60:252–260. doi: 10.15288/jsa.1999.60.252. [DOI] [PubMed] [Google Scholar]
- Rosario M, Schrimshaw EW, Hunter J, Gwadz M. Gay-related stress and emotional distress among gay, lesbian and bisexual youths: A longitudinal examination. Journal of Consulting and Clinical Psychology. 2002;70:967–975. doi: 10.1037//0022-006x.70.4.967. [DOI] [PubMed] [Google Scholar]
- Smith DJ, Muir WJ, Blackwood DHR. Borderline personality disorder characteristics in young adults with recurrent mood disorders: A comparison of bipolar and unipolar depression. Journal of Affective Disorders. 2005;87:17–23. doi: 10.1016/j.jad.2005.02.019. [DOI] [PubMed] [Google Scholar]
- Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. Journal of Abnormal Child Psychology. 2012;40:7–20. doi: 10.1007/s10802-011-9530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley AE, Aranda F, Birkett M, Marshal MP, Hughes T. Exploring alcohol use behaviors among heterosexual and sexual minority adolescents: Intersections with sex, age, and race/ethnicity. 2013 doi: 10.2105/AJPH.2013.301627. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitbeck LB, Chen X, Hoyt DR, Tyler KA, Johnson KD. Mental disorder, subsistence strategies, and victimization among gay, lesbian, and bisexual homeless and runaway adolescents. Journal of Sex Research. 2004;41:329–342. doi: 10.1080/00224490409552240. [DOI] [PubMed] [Google Scholar]
- Wolff JC, Ollendick TH. The comorbidity of conduct problems and depression in childhood and adolescence. Clinical Child and Family Psychology Review. 2006;9:201–220. doi: 10.1007/s10567-006-0011-3. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, Morey LC. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. American Journal of Psychiatry. 2004;161:1296–1298. doi: 10.1176/appi.ajp.161.7.1296. [DOI] [PubMed] [Google Scholar]
- Zoccolillo M, Tremblay R, Vitaro F. DSM-III-R and DSM-III criteria for conduct disorder in preadolescent girls: specific but insensitive. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:461–470. doi: 10.1097/00004583-199604000-00012. [DOI] [PubMed] [Google Scholar]