Abstract
Type 2 diabetes mellitus (T2DM) has become one of the most prevalent noncommunicable diseases in the past years. It is undoubtedly associated with atherosclerosis and increased risk for cardiovascular diseases. Incretins, which are intestinal peptides secreted during digestion, are able to increase insulin secretion and its impaired function and/or secretion is involved in the pathophysiology of T2DM. Dipeptidyl peptidase 4 (DPP4) is an ubiquitous enzyme that regulates incretins and consequently is related to the pathophysiology of T2DM. DPP4 is mainly secreted by endothelial cells and acts as a regulatory protease for cytokines, chemokines, and neuropeptides involved in inflammation, immunity, and vascular function. In T2DM, the activity of DPP4 seems to be increased and there are a growing number of in vitro and in vivo studies suggesting that this enzyme could be a new link between T2DM and atherosclerosis. Gliptins are a new class of pharmaceutical agents that acts by inhibiting DPP4. Thus, it is expected that gliptin represents a new pharmacological approach not only for reducing glycemic levels in T2DM, but also for the prevention and treatment of atherosclerotic cardiovascular disease in diabetic subjects. We aimed to review the evidences that reinforce the associations between DPP4, atherosclerosis, and T2DM.
1. Introduction
Atherosclerosis is the leading cause of death and an important cause of morbidity in patients with type 2 diabetes mellitus (T2DM) [1]. However, the mechanisms responsible for the accelerated atherosclerosis observed in T2DM are not yet fully understood [2]. Reduction in the bioavailability of nitric oxide (NO) in the periendothelial environment, which characterizes endothelial dysfunction, is the earliest event in the development of atherosclerosis [2]. Since the occurrence of endothelial dysfunction may be observed before the development of T2DM, it is suggested that these two entities, T2DM and atherosclerosis, may have common pathogenic mechanisms which enhances the possibility of a causal relationship between them [3]. Not only reduced endothelial NO bioavailability, but also inflammation has a role in the promotion of vascular damage in T2DM and has been receiving special attention [4]. Some recent findings add knowledge in these intricate mechanisms and relate the enzyme dipeptidyl peptidase 4 (DPP4) with them.
T2DM has a complex pathophysiology, mainly characterized by insulin resistance (IR) in fat, muscle, and liver tissues associated with pancreatic α and β cell dysfunctions [5, 6]. However, other factors play a role in the development of T2DM. Among them, stands out the incretin deficiency/resistance [5]. Glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide 1 (GLP-1) are the main incretins secreted by the gastrointestinal tract soon after a meal ingestion [7]. Both are able to enhance insulin secretion in a glucose-dependent fashion while suppressing glucagon secretion [6], although GIP has a more complex relationship with glucagon. Actually, GIP acts as a hormone that stabilizes glucose in T2DM by increasing glucagon response during hypoglycemia, the secretion rate of insulin during hyperglycemia, and both mechanisms when fasting glucose levels are around 8 mmol/L [8].
The state of incretin deficiency/resistance reflects the impairment of the “incretin effect,” defined as the amplification of insulin secretion in response to an oral glucose load when compared to the insulin response observed after the same glycemic levels achieved after intravenous glucose infusion [9]. Both GIP and GLP-1 have short half-lives, since they are rapidly degraded by DPP4, an ubiquitous enzyme found in soluble form in plasma or as a membrane component of many cells [10], including endothelial cells [11]. The findings of increased concentrations and activity of DPP4 in patients with diabetes [12–15] may justify, at least partially, the status of incretin deficiency/resistance related to T2DM.
In recent years, new drugs for the treatment of T2DM have emerged into the market, among which the gliptins stand out. These drugs act through the inhibition of DPP4; consequently they are able to ameliorate the incretin deficiency and to attenuate the hyperglucagonemia, two important aspects in the pathophysiology of the T2DM [6]. Gliptins and the GLP-1 receptors agonists comprise the group of incretin-based therapies for T2DM [7].
An important point to emphasize is the capacity of DPP4 to inactivate not only incretins, but also a number of cytokines, chemokines, and neuropeptides involved in inflammation, immunity, and vascular function [16]. Furthermore, the pharmacological inhibition of DPP4 is associated with attenuation of endothelial dysfunction and atherogenesis [17] and also with reduction of inflammatory markers [18]. Considering the higher concentrations and activity of DPP4 in patients with diabetes when compared to nondiabetic subjects [12–15], it is possible that DPP4 constitutes a new link between diabetes and atherosclerosis.
2. DPP4: A Regulatory Serine Exopeptidase
DPP4, also known as adenosine deaminase binding protein or cluster of differentiation 26 (CD26), is a serine exopeptidase able to inactivate various oligopeptides through the removal of N-terminal dipeptides. Its chemical structure remained relatively preserved over evolutionary process and it has been observed in very distinct species, including prokaryotes and eukaryotes organisms [19].
In humans, the DPP4 gene is located on chromosome 2q23, encoding a protein of 766 amino acids [19]. Immediately after its synthesis, DPP4 is incorporated into the plasma membrane of many cell types. It is a type II surface protein, which means that the greatest part of its structure, including the C-terminal domain, is in the extracellular portion [20]. However, under certain stimuli, like IR, tumor necrosis factor α (TNF-α), and chronic low-grade inflammation, DPP4 can be released from the membrane, constituting a soluble form [15, 20, 21].
DPP4 is widely expressed in many specialized cell types and has distinct functions independently of its form, anchored to the membrane or in soluble form. As a cell surface protein, it acts as a regulatory protease and participates in complex mechanisms such as cell-cell interaction and activation of transduction pathways of intracellular signals. The soluble form of DPP4 appears to be derived primarily from endothelial cells, epithelial cells, and leukocytes and, as previously mentioned, it is also endowed with enzymatic activity [20, 28].
DPP4 activation involves a dimerisation process with the formation of a homodimer. The activity of its monomeric form is not significant [29] which possibly explains the apparent dissociation observed between serum levels of DPP4 and its enzymatic activity in humans.
Like other serine proteases, this enzyme has no absolute specificity, although it has a better affinity for oligopeptides composed of proline, hydroxyproline, or alanine as the penultimate residue [19]. DPP4 has currently many known substrates (see Table 1).
Table 1.
Dipeptidyl peptidase 4 (DPP4) substrates.
| β-Casomorphin-2 | GLP-1* and -2* | MCP |
| Aprotinin | Glucagon | MDC |
| Bradykinin | GRF | Morphiceptin |
| BNP* | GRP | Neuropeptide Y |
| CLIP | IGF-1 | PACAP27 |
| Chromogranin | IL-1β | PACAP38 |
| Endomorphin-1 | IL-2 | Procalcitonin |
| Endomorphin-2 | GCP-2 (CXCL6) | Peptide YY |
| Enterostatin | Mig (CXCL9) | PHM |
| Eotaxin (CCL11) | IP-10 (CXCL10) | RANTES (CCL5) |
| Monomeric fibrin (α-chain) | I-TAC (CXCL11) | Substance P* |
| GHRH | SDF-1α and -1β (CXCL12)* | Vasostatin I |
| GIP* | LD78β (CCL3L1) | VIP |
BNP: B-type natriuretic peptide, formerly named brain natriuretic peptide; CLIP: corticotropin-like intermediate lobe peptide; GHRH: growth hormone-releasing hormone; GIP: glucose-dependent insulinotropic polypeptide; GLP-1: glucagon-like peptide 1; GLP-2: glucagon-like peptide 2; GRF: growth hormone-releasing factor; GRP: gastrin-releasing peptide; IGF-1: insulin-like growth factor 1; IL-1β: interleukin-1β; IL-2: interleukin-2; GCP-2: granulocyte chemotactic protein 2; IP-10: interferon γ-inducible protein 10; I-TAC: interferon γ-inducible T cell alpha chemoattractant; SDF-1α: stromal cell-derived factor 1α; SDF-1β: stromal cell-derived factor 1β; LD78β: isoform of macrophage inflammatory protein-1α (MIP-1α); MCP: monocyte chemotactic protein; MDC: macrophage-derived chemokine; PACAP27: pituitary adenylate cyclase-activating peptide 27; PACAP38: pituitary adenylate cyclase-activating peptide 38; PHM: peptide histidine methionine; RANTES: regulated on activation, normal T-cell expressed and secreted; VIP: vasoactive intestinal peptide. *Peptides whose endogenous levels of intact to cleaved forms are significantly different following genetic inactivation or chemical inhibition of DPP4 activity in vivo. Adapted from [20, 28, 30].
Since DPP4 has a wide capacity to act in various peptides, it appears to regulate several physiological pathways involved not only in glucose homeostasis but also in inflammation, immunity, and vascular and cardiac functions [16, 30]. These properties reinforce the hypothesis that this enzyme may act on regulatory mechanisms of endothelial function and inflammatory processes by incretin-dependent and also incretin-independent pathways.
3. The Role of DPP4 in Diabetes Pathophysiology and Related Complications
Since incretin hormones are rapidly degraded by DPP4, it is reasonable to assume that an increase in DPP4 level and/or enzymatic activity may contribute to the impaired incretin effect observed in patients with T2DM [12]. Preliminary studies assessing DPP4 activity in patients with T2DM have shown contradictory results such as reduced [31, 32] or increased activity [12, 13, 30]. However, these disparate results may have occurred due to the use of drugs such as metformin and glitazones, which are both able to promote a decrease in DPP4 activity [33–35].
A more recent study [15] that compared serum levels and plasma activity of the DPP4 among patients with T2DM and healthy subjects showed significant higher levels and activity of the DPP4 in those with diabetes than in controls, but only after excluding patients treated with metformin and/or glitazones.
Interestingly, not only patients with T2DM but also those at prediabetes status appear to have an impairment of incretin effect. It has been shown that patients with prediabetes exhibit decreased GLP-1 and unaltered GIP levels, as compared to those with normal glucose tolerance [36]. Therefore, it is suggested that the reduction in GLP-1 levels and/or a greater GIP resistance may contribute to impairment in insulin secretion in patients with prediabetes [36, 37].
Regardless of the glucose tolerance status (normal glucose tolerance, prediabetes, or T2DM), a 4-year longitudinal study showed that baseline DPP4 activity and GLP-1 were negatively associated. Moreover, DPP4 activity was an independent predictor of risk for developing prediabetes (relative risk (RR): 2.77; 95% confidence interval (CI): 1.38–5.55; P < 0.01) and T2DM (RR: 5.10; 95% CI: 1.48–17.61; P < 0.05) after adjustment for confounding risk factors [38]. The hypothesis that the changes in incretins in prediabetes are directly related to DPP4 seems to be a plausible one. Considering the cardiovascular (CV) complications of diabetes, this hypothesis acquired even greater relevance since a number of studies provided evidence for the pleiotropic effects of GLP-1 on the CV system [39–43].
Advanced glycation end products (AGEs) are a well-known consequence of the chronic hyperglycemia related to uncontrolled diabetes. They are formed by nonenzymatic reaction between reducing sugars and amino groups of proteins, lipids, and nucleic acids. The interaction between AGE and its receptor (RAGE) elicits oxidative stress generation, thereby evoking proliferative, inflammatory, and fibrotic reactions, which impairs structural integrity and function of many proteins. An active participation of AGEs-RAGE axis in the accelerated atherosclerosis observed in diabetes was already denoted [44]. In respect of DPP4, it was demonstrated that levels of AGEs are independently correlated with the levels of this enzyme [45]. Curiously, AGEs enhance the expression of DPP4 and its release [45], while DPP4 increases RAGE gene expression [46], suggesting the existence of a cross talk between the AGEs-RAGE axis and DPP4 in the pathogenesis of diabetes-associated complications [44].
4. Interaction between DPP4 and Endothelium
Endothelial cells independent of their site, that is, microvascular or macrovascular compartments, are probably the main endogenous source of DPP4. Its activity at endothelial milieu appears to be more substantial than that of the circulating form [47]. Endothelial cells from microvascular compartment showed significant increased expression of DPP4, as well as enzymatic activity, after chronic exposure to high glucose concentrations in vitro [48]. Microcirculation is the site of tissue nutrition, of gas exchange, and also of removal of cellular excreta and, although DPP4 is present in all vascular beds, hyperglycemia is able to increase the DPP4 activity only from the endothelial cells at the microvascular compartment [49].
In vivo studies added important knowledge about the action of gliptins on atherosclerosis and, interestingly, have suggested that DPP4 inhibition has GLP-1-independent effects, possibly through regulation of other enzyme substrates, acting on attenuation of endothelial dysfunction and atherogenesis [17]. Among them, the chemokine stromal cell-derived factor 1α (SDF-1α) has received special attention. SDF-1α is highly expressed by the human bone marrow endothelium and it is implicated in the migration, proliferation, differentiation, and survival of many cell types, including human hematopoietic stem cells and progenitor cells [50, 51]. This chemokine has its own receptor, named CXCR4, which is a seven-transmembrane G-protein receptor widely expressed by a variety of cell types, including hematopoietic, endothelial, and stromal cells [51]. The SDF-1α-CXCR4 axis participates in the recruitment of endothelial progenitor cells (EPCs) from bone marrow to areas of vascular damage, constituting an important mechanism of vascular repair [52, 53]. There is a positive relationship between the number of EPCs and the improvement in vascular repair and, actually, EPCs are used as a marker to assess endothelial function. It was demonstrated that DPP4 inhibition with a gliptin (sitagliptin) increased the number of EPCs, possibly due to a concomitant increase on the levels of SDF-1α [52]. Furthermore, this mechanism may be also responsible for the observed improvement in endothelial function in patients with T2DM following pharmacological inhibition of DPP4 with other gliptins (vildagliptin) [54]. All these effects mediated by DPP4 inhibition may confer some properties to gliptins that are related to reduction of endothelial damage and also to improvement in endothelial function, with possibly atheroprotective action.
5. DPP4 and Inflammation
DPP4 also seems to play an important role in low-grade inflammation [55] and particularly in the development of inflammatory reactions in patients with T2DM [15]. IR per se and the chronic low-grade inflammation present in T2DM may increase the expression and release of DPP4 from several tissues [15]. Indirect markers of IR, such as fasting insulin and homeostasis model assessment to quantify insulin resistance (HOMA-IR), were positively associated with DPP4 expression in visceral adipose tissue (VAT) macrophages [56]. These macrophages, as well as the visceral adipocytes, were able to release DPP4 when stimulated by TNF-α [56].
On the other hand, treatment of human vascular endothelial cells with sitagliptin is able to inhibit TNF-α induction of plasminogen activator inhibitor type-1 (PAI-1), intercellular adhesion molecule-1 (ICAM-1), and vascular cell adhesion molecule-1 (VCAM-1) mRNA and protein expression [17]. DPP4 inhibition is also able to decrease serum levels of inflammatory cytokines, such as interleukin-6 and interleukin-18, in patients with T2DM [18]. Taken together, these evidences suggest the existence of a pathophysiological interaction between DPP4, endothelial dysfunction, and inflammation, factors that are directly linked to the pathogenesis and clinical manifestations of T2DM and atherosclerosis.
6. DPP4 as an Adipokine
Adipose tissue (AT) is definitely an endocrine organ. It expresses and secretes several proteins, known as adipokines, as well as inflammatory cytokines [57, 58]. Adipokines and cytokines participate in the main pathophysiological mechanism linking obesity, IR, T2DM, and atherosclerotic disease [58, 59]. Recently, DPP4 was identified as a new adipokine, possibly linking AT to IR and the metabolic syndrome [21].
In a series of basic and clinical researches, including a proteomic profile of human adipocyte, it was demonstrated that (1) DPP4 is highly expressed in and released by adipocytes; (2) DPP4 inhibits insulin-stimulated Akt phosphorylation in muscle and adipocyte, therefore impeding insulin signaling, and this effect was totally reversed by a DPP4 inhibitor which strongly suggest its role in IR; (3) DPP4 levels are higher in obese as compared to lean subjects and its expression is increased in VAT of obese when compared to subcutaneous adipose tissue (SAT) of obese or lean subjects; (4) DPP4 concentration correlated with several biochemical parameters, such as insulin, leptin (directly), and adiponectin (inversely) [21]. To further refine these observations, Sell et al. [60] studied DPP4 expression and release by VAT and SAT in a cohort of 196 subjects before an open abdominal surgery, by collecting AT biopsies. These authors demonstrated a positive relationship between DPP4 expression and body mass index in both SAT and VAT, with VAT exhibiting higher expression. Furthermore, VAT released more DPP4 than SAT. Interestingly, DPP4 serum levels were higher in insulin resistant as compared to insulin sensitive subjects matched for BMI. Taken together, these data demonstrated that DPP4 is a new adipokine associated with increased visceral obesity, IR, and metabolic syndrome, which are all well-known risk factors for atherosclerotic disease.
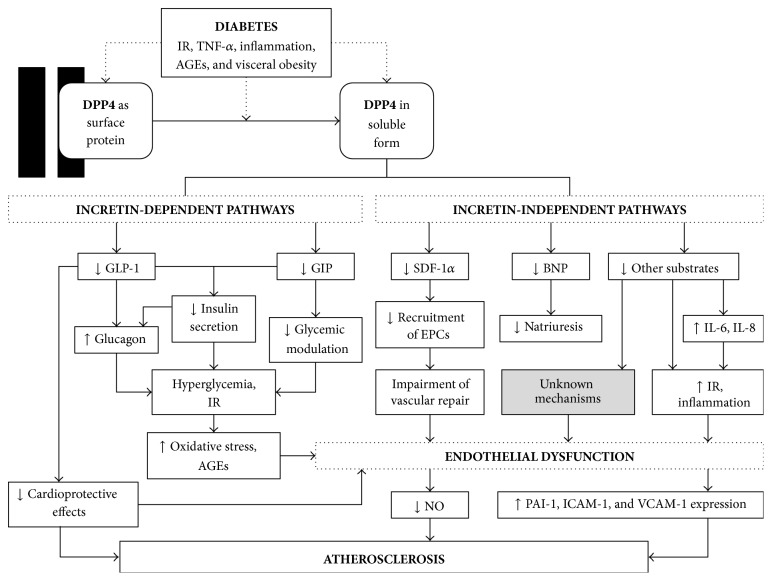
Figure 1 provides a schematic diagram illustrating the above-mentioned associations between DPP4, T2DM, insulin resistance, and atherosclerosis.
Figure 1.
Schematic diagram illustrating the role of DPP4 and its associations with diabetes, insulin resistance, and atherosclerosis. AGEs: advanced glycation end products; BNP: B-type natriuretic peptide; DPP4: dipeptidyl peptidase 4; EPCs: endothelial progenitor cells; GIP: glucose-dependent insulinotropic polypeptide; GLP-1: glucagon-like peptide 1; ICAM-1: intercellular adhesion molecule-1; IL-6: interleukin-6; IL-8: interleukin-8; IR: insulin resistance; NO: nitric oxide; PAI-1: plasminogen activator inhibitor type-1; SDF-1α: stromal cell-derived factor 1α; TNF-α: tumor necrosis factor α; VCAM-1: vascular cell adhesion molecule-1.
7. Impact of DPP4 Inhibition on Atherosclerotic Cardiovascular Disease: Some Clinical Aspects
Several DPP4 inhibitors have been launched in the market and are now being used for the treatment of T2DM (vildagliptin, sitagliptin, saxagliptin, linagliptin, and alogliptin) [7]. All of them proved efficacy in glycemic control with impressive safety and tolerance profiles [26]. Gliptins can be used as monotherapy or in combination with other oral agents (in dual or triple therapy) and even with insulin [61]. A systematic review and meta-analyses showed similar efficacy and safety for gliptins as monotherapy or as combination therapy for T2DM [62].
As add-on therapy to metformin, DPP4 inhibitors reduced mean A1c by 0.5–1.1% compared with placebo [63–66]. Considering the glycemic control achieved by a combination of metformin with sulfonylureas or glitazones, gliptins provided comparable improvements [67–69], although with reduced risk of hypoglycemia and weight gain when compared to sulphonylureas and greater cost to the patients. However, in a recent retrospective analysis, gliptins in combination with metformin showed better metabolic control, lower rates of hypoglycemia, and even lower health costs in comparison to metformin and other oral agents in subjects with T2DM and renal impairment [70]. A study [71] comparing gliptins, sulphonylureas, insulin, and GLP-1 receptor agonists for use after metformin is ongoing and will possibly add knowledge about the most appropriate drugs for the treatment of T2DM.
Several meta-analyses of phase III randomized clinical trials (RCTs) have been published evaluating the impact of DPP4 inhibitors on CV outcomes. Frederich et al. [72] and Johansen et al. [73] showed, respectively, that saxagliptin and linagliptin were able to reduce CV outcomes (hazard ratio (HR) from 0.34 to 0.43) when compared to other agents, including placebo. No differences in CV events were observed by Schweizer et al. [74] and Engel et al. [75] when, respectively, vildagliptin and sitagliptin were compared to other oral drugs or placebo. Eighteen RCTs were analyzed together in a meta-analysis that included 8544 patients treated for at least 24 weeks with gliptins or other oral antidiabetic drugs. These investigators found that gliptins may possibly reduce risk of adverse CV events by observing a RR of 0.48 (95% CI: 0.31–0.75; P = 0.001) for any adverse CV event and a RR of 0.40 (95% CI: 0.18–0.88, P = 0.02) for nonfatal myocardial infarction (MI) or acute coronary syndrome in those treated with a DPP4 inhibitor [76]. Similar results were obtained by Monami et al. [61] in a meta-analysis enrolling almost 42000 patients with T2DM. They found that gliptins promoted a 29% reduction in major cardiovascular events (MACE), mostly due to reducing MI (<36%) and all-cause mortality (<40%). Individually, vildagliptin and saxagliptin were associated with less MACE [61].
Questions about the validity of these comparisons must be taken in account, since many pitfalls in primary composite endpoints and CV adjudication methods were noted [73]. It is also not clear how these potential benefits may be mediated, but possibly these drugs acted through the improvement in endothelial function, inflammation, and reduction of atherosclerosis [77]. Interestingly, an in vivo experiment recently demonstrated that vildagliptin or sitagliptin reduced MI size in rats in a glucose-dependent manner through GLP-1 receptor-protein kinase A pathway [78], while linagliptin attenuated neointima formation after vascular injury and in vitro vascular smooth muscle cells proliferation beyond the glucose-lowering effect [79].
Table 2 shows some characteristics of phase IV clinical trials evaluating the impact of long-term DPP4 inhibition on CV outcomes. In RCTs designed to demonstrate noninferiority, alogliptin and saxagliptin were neutral regarding MACE [22, 23]. In the EXAMINE trial [22], involving patients with T2DM who had recent hospitalization for acute coronary syndrome, MACE rates did not differ between those who used alogliptin compared to placebo (HR: 0.96; upper boundary of the one sided repeated confidence interval: 1.16; P = 0.32 for superiority; P < 0.001 for noninferiority) after a follow-up period greater than 40 months (median of 18 months). In the SAVOR-TIMI 53 trial [23], DPP4 inhibition with saxagliptin did not alter the rate of CV events (HR: 1.0; 95% CI: 0.89 to 1.12; P = 0.99 for superiority; P < 0.001 for noninferiority), although a higher heart failure hospitalization rate among saxagliptin users has been detected (HR: 1.27; 95% CI: 1.07–1.51; P = 0.007) during follow-up (median 2.1 years).
Table 2.
Prospective, randomized, controlled trials involving DPP4 inhibitors (gliptins) and cardiovascular outcomes in diabetic patients.
| Gliptin versus comparator | Study | Doses (mg/day) | Composite primary endpoints | Population |
|---|---|---|---|---|
| Alogliptin versus placebo [22] | Examination of cardiovascular outcomes with alogliptin versus standard of care (EXAMINE)* | 6.25, 12.5, or 25 | Nonfatal MI, nonfatal stroke, or CV death | Patients with T2DM recently hospitalized for an ACS (n = 5380) |
|
| ||||
| Saxagliptin versus placebo [23] | Saxagliptin assessment of vascular outcomes recorded in patients with diabetes mellitus – thrombolysis in myocardial infarction 53 trial (SAVOR-TIMI 53)** | 2.5 or 5 | Nonfatal MI, nonfatal ischemic stroke, or CV death | High-risk CV patients with T2DM (n = 16492) |
|
| ||||
| Linagliptin versus glimepiride [24] | Cardiovascular outcome study of the DPP-4 inhibitor linagliptin (CAROLINA)** | 5 | Nonfatal MI, nonfatal stroke, hospitalization for unstable angina, or CV death | High-risk CV patients with T2DM (n = ~6000) |
|
| ||||
| Sitagliptin versus placebo [25] | Trial to evaluate cardiovascular outcomes after treatment with sitagliptin (TECOS)*** | 50 or 100 | Nonfatal MI, nonfatal stroke, or hospitalization for unstable angina | Patients with T2DM and previous CV disease (n = ~14000) |
The increased risk of hospitalization for heart failure associated with the use of gliptins still requires further analysis. In a later study with SAVOR-TIMI 53 data [80], it was demonstrated that although the absolute risk of hospitalization for heart failure was highest among the 12.8% of patients who had a history of this condition, the relative risk of hospitalization for the same cause among patients assigned to saxagliptin was similar regardless of the baseline history (HR: 1.21; 95% CI: 0.93–1.58 versus HR: 1.32; 95% CI: 1.04–1.65; P = 0.68 for interaction). Moreover, in a reanalysis of the EXAMINE trial [81], including patients with a history of heart failure and/or high baseline levels of N-terminal pro-B-type natriuretic peptide, there was no evidence of an increased risk of CV outcomes or the rate of hospitalization for heart failure among patients assigned to alogliptin compared to placebo. During follow-up, alogliptin did not induce the onset of heart failure in patients without this diagnosis, or worsening of symptoms in patients with this previous diagnosis [81].
Despite these evidences, in a recent meta-analysis of 94 RCTs enrolling 85224 patients, including data from SAVOR-TIMI 53 and EXAMINE trials, Savarese et al. [82] observed that gliptins did not affect all-cause and CV mortality, as well as stroke, both in short- (<29 weeks) and long-term (≥29 weeks) therapies. With respect to the risk of MI, they also noted that gliptins reduced this risk in short-term treatment (RR: 0.58; 95% CI: 0.36–0.94; P = 0.02), but it did not persist in the long-term. Furthermore, long-term treatment with gliptins was associated with a 15.8% increase in the risk of heart failure (RR: 1.15; CI: 1.01–1.32; P = 0.03). So, it is still not possible to rule out the existence of an interaction between DPP4 inhibition and heart failure. As mentioned above, B-type natriuretic peptide (BNP) and substance P are both substrates of the DPP4 enzyme and may have implications on the possible association between heart failure and gliptins use, since it is already known that BNP levels increased more than 100 times in patients with heart failure and substance P is able to increase sympathetic activity during combined inhibition of angiotensin-converting enzyme and DPP4 [30, 77, 83, 84].
Regarding the risk of MI, patients enrolled in RCTs assessing the CV safety of gliptins have some characteristics that could be responsible for the observed diversities in the obtained results. To investigate it, Dicembrini and Mannucci [85] performed a meta-analysis with RCTs designed for glycemic endpoints that had a duration of 52 weeks or longer. All RCTs were identified from Savarese et al. [82], except those studies with a CV endpoint. During a mean follow-up of 86.3 weeks, gliptins were associated with a significant reduction of MI (RR: 0.48; 95% CI: 0.31–0.73; P = 0.001) similar to that observed in short-term therapy by Savarese et al. [82]. The authors concluded that maybe gliptins have a protective effect only in earlier stages of the natural history of T2DM (i.e., in younger subjects with a short duration of disease and without an established CV disease) whereas this benefit is lost in older patients with already established CV disease [85]. Therefore, there seems to be a window of opportunity for gliptins to reduce CV outcomes in subjects with T2DM that must be further investigated with studies primarily aimed at CV outcomes. The CAROLINA [24] and TECOS [25] trials, involving, respectively, linagliptin and sitagliptin, are still in progress and will possibly provide additional important information about the impact of pharmacological inhibition of DPP4 on CV outcomes.
8. Conclusion
The activity of DPP4 seems to be increased in patients with T2DM and there are a fair number of in vitro and in vivo studies demonstrating that this enzyme is able to interact with proinflammatory pathways and to impair endothelial function through incretin-dependent and independent mechanisms, potentially providing a new link between T2DM and atherosclerosis. In this way, it has been demonstrated that DPP4 is a new adipokine associated with increased visceral obesity, IR, and metabolic syndrome, which is consistent with its possible link with atherosclerosis. Many studies showed that DPP4 inhibition attenuated endothelial dysfunction, inflammation, and atherosclerotic process, but available phase IV studies did not associate the use of gliptins with reduced CV events in T2DM. In light of current evidence, we believe that further clinical studies with gliptins are warranted, especially those primarily aimed to investigate cardiovascular outcome.
Abbreviations
- AGEs:
Advanced glycation end products
- AT:
Adipose tissue
- BMI:
Body mass index
- BNP:
B-type natriuretic peptide
- CD26:
Cluster of differentiation 26
- CI:
Confidence interval
- CV:
Cardiovascular
- DPP4:
Dipeptidyl peptidase 4
- EPCs:
Endothelial progenitor cells
- GIP:
Glucose-dependent insulinotropic polypeptide
- GLP-1:
Glucagon-like peptide 1
- HR:
Hazard ratio
- HOMA-IR:
Homeostasis model assessment to quantify insulin resistance
- ICAM-1:
Intercellular adhesion molecule-1
- IR:
Insulin resistance
- MACE:
Major cardiovascular events
- MI:
Myocardial infarction
- NO:
Nitric oxide
- PAI-1:
Plasminogen activator inhibitor type-1
- RAGE:
Receptor for advanced glycation end products
- RCTs:
Randomized clinical trials
- RR:
Relative risk
- SAT:
Subcutaneous adipose tissue
- SDF-1α:
Stromal cell-derived factor 1α
- T2DM:
Type 2 diabetes
- TNF-α:
Tumor necrosis factor α
- VAT:
Visceral adipose tissue
- VCAM-1:
Vascular cell adhesion molecule-1.
Conflict of Interests
Wellington Santana da Silva Júnior has no conflict of interests to disclose. Amélio Fernando de Godoy-Matos has received honoraria for lectures, travel support, and consultancy services from pharmaceutical companies manufacturing diabetes treatments, including Novartis, Novo Nordisk, and Takeda. He was also a Principal Investigator for clinical trials involving GLP-1RA from Sanofi-Aventis. Luiz Guilherme Kraemer-Aguiar is a Principal Investigator of a clinical trial involving Vildagliptin from Novartis and receives a research grant from the National Council for Scientific and Technologic Development (CNPq) and from the Carlos Chagas Filho Foundation for Research Support in the State of Rio de Janeiro (FAPERJ).
References
- 1.Beckman J. A., Creager M. A., Libby P. Diabetes and atherosclerosis epidemiology, pathophysiology, and management. Journal of the American Medical Association. 2002;287(19):2570–2581. doi: 10.1001/jama.287.19.2570. [DOI] [PubMed] [Google Scholar]
- 2.Natali A., Ferrannini E. Endothelial dysfunction in type 2 diabetes. Diabetologia. 2012;55(6):1559–1563. doi: 10.1007/s00125-011-2445-5. [DOI] [PubMed] [Google Scholar]
- 3.Tabit C. E., Chung W. B., Hamburg N. M., Vita J. A. Endothelial dysfunction in diabetes mellitus: molecular mechanisms and clinical implications. Reviews in Endocrine and Metabolic Disorders. 2010;11(1):61–74. doi: 10.1007/s11154-010-9134-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nilsson J., Bengtsson E., Fredrikson G. N., Björkbacka H. Inflammation and immunity in diabetic vascular complications. Current Opinion in Lipidology. 2008;19(5):519–524. doi: 10.1097/MOL.0b013e32830f47cd. [DOI] [PubMed] [Google Scholar]
- 5.Defronzo R. A. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009;58(4):773–795. doi: 10.2337/db09-9028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Godoy-Matos A. F. The role of glucagon on type 2 diabetes at a glance. Diabetology & Metabolic Syndrome. 2014;6(1, article 91) doi: 10.1186/1758-5996-6-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deacon C. F., Mannucci E., Ahrén B. Glycaemic efficacy of glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors as add-on therapy to metformin in subjects with type 2 diabetes—a review and meta analysis. Diabetes, Obesity and Metabolism. 2012;14(8):762–767. doi: 10.1111/j.1463-1326.2012.01603.x. [DOI] [PubMed] [Google Scholar]
- 8.Christensen M. B., Calanna S., Holst J. J., Vilsbøll T., Knop F. K. Glucose-dependent insulinotropic polypeptide: blood glucose stabilizing effects in patients with type 2 diabetes. The Journal of Clinical Endocrinology & Metabolism. 2014;99(3):E418–E426. doi: 10.1210/jc.2013-3644. [DOI] [PubMed] [Google Scholar]
- 9.Cernea S., Raz I. Therapy in the early stage: incretins. Diabetes Care. 2011;34(supplement 2):S264–S271. doi: 10.2337/dc11-s223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holst J. J. On the physiology of GIP and GLP-1. Hormone and Metabolic Research. 2004;36(11-12):747–754. doi: 10.1055/s-2004-826158. [DOI] [PubMed] [Google Scholar]
- 11.Matheeussen V., Baerts L., de Meyer G., et al. Expression and spatial heterogeneity of dipeptidyl peptidases in endothelial cells of conduct vessels and capillaries. Biological Chemistry. 2011;392(3):189–198. doi: 10.1515/bc.2011.002. [DOI] [PubMed] [Google Scholar]
- 12.Ryskjær J., Deacon C. F., Carr R. D., et al. Plasma dipeptidyl peptidase-IV activity in patients with type-2 diabetes mellitus correlates positively with HbAlc levels, but is not acutely affected by food intake. European Journal of Endocrinology. 2006;155(3):485–493. doi: 10.1530/eje.1.02221. [DOI] [PubMed] [Google Scholar]
- 13.Mannucci E., Pala L., Ciani S., et al. Hyperglycaemia increases dipeptidyl peptidase IV activity in diabetes mellitus. Diabetologia. 2005;48(6):1168–1172. doi: 10.1007/s00125-005-1749-8. [DOI] [PubMed] [Google Scholar]
- 14.Venkatesham A., Srinivas M., Krishna D. R., Narayana P. Differential expression of Dipeptidyl peptidase-IV (DPP-IV) in Indian type-2 diabetic population. Journal of Association of Physicians of India. 2009;57(9):627–630. [PubMed] [Google Scholar]
- 15.Lee S. A., Kim Y. R., Yang E. J., et al. CD26/DPP4 levels in peripheral blood and T cells in patients with type 2 diabetes mellitus. Journal of Clinical Endocrinology and Metabolism. 2013;98(6):2553–2561. doi: 10.1210/jc.2012-4288. [DOI] [PubMed] [Google Scholar]
- 16.Fadini G. P., Avogaro A. Cardiovascular effects of DPP-4 inhibition: Beyond GLP-1. Vascular Pharmacology. 2011;55(1–3):10–16. doi: 10.1016/j.vph.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Hu Y., Liu H., Simpson R. W., Dear A. E. GLP-1-dependent and independent effects and molecular mechanisms of a dipeptidyl peptidase 4 inhibitor in vascular endothelial cells. Molecular Biology Reports. 2013;40(3):2273–2279. doi: 10.1007/s11033-012-2290-8. [DOI] [PubMed] [Google Scholar]
- 18.Rizzo M. R., Barbieri M., Marfella R., Paolisso G. Reduction of oxidative stress and inflammation by blunting daily acute glucose fluctuations in patients with type 2 diabetes: role of dipeptidyl peptidase-IV inhibition. Diabetes Care. 2012;35(10):2076–2082. doi: 10.2337/dc12-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matteucci E., Giampietro O. Dipeptidyl peptidase-4 (CD26): knowing the function before inhibiting the enzyme. Current Medicinal Chemistry. 2009;16(23):2943–2951. doi: 10.2174/092986709788803114. [DOI] [PubMed] [Google Scholar]
- 20.Lambeir A.-M., Durinx C., Scharpé S., de Meester I. Dipeptidyl-peptidase IV from bench to bedside: an update on structural properties, functions, and clinical aspects of the enzyme DPP IV. Critical Reviews in Clinical Laboratory Sciences. 2003;40(3):209–294. doi: 10.1080/713609354. [DOI] [PubMed] [Google Scholar]
- 21.Lamers D., Famulla S., Wronkowitz N., et al. Dipeptidyl peptidase 4 is a novel adipokine potentially linking obesity to the metabolic syndrome. Diabetes. 2011;60(7):1917–1925. doi: 10.2337/db10-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White W. B., Cannon C. P., Heller S. R., et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. The New England Journal of Medicine. 2013;369(14):1327–1335. doi: 10.1056/nejmoa1305889. [DOI] [PubMed] [Google Scholar]
- 23.Scirica B. M., Bhatt D. L., Braunwald E., et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. The New England Journal of Medicine. 2013;369(14):1317–1326. doi: 10.1056/nejmoa1307684. [DOI] [PubMed] [Google Scholar]
- 24.CAROLINA. A multicentre, international, randomised, parallel group, double blind study to evaluate cardiovascular safety of linagliptin versus glimepiride in patients with type 2 diabetes mellitus at high cardiovascular risk. NCT01243424, 2014, http://clinicaltrials.gov/show/NCT01243424.
- 25. TECOS: a randomized, placebo controlled clinical trial to evaluate cardiovascular outcomes after treatment with sitagliptin in patients with type 2 diabetes mellitus and inadequate glycemic control ( NCT00790205), http://clinicaltrials.gov/show/NCT00790205.
- 26.Rosenstock J., Marx N., Kahn S. E., et al. Cardiovascular outcome trials in type 2 diabetes and the sulphonylurea controversy: rationale for the active-comparator CAROLINA trial. Diabetes and Vascular Disease Research. 2013;10(4):289–301. doi: 10.1177/1479164112475102. [DOI] [PubMed] [Google Scholar]
- 27.Green J. B., Bethel M. A., Paul S. K., et al. Rationale, design, and organization of a randomized, controlled Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS) in patients with type 2 diabetes and established cardiovascular disease. American Heart Journal. 2013;166(6):983–989.e7. doi: 10.1016/j.ahj.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 28.Drucker D. J. Dipeptidyl peptidase-4 inhibition and the treatment of type 2 diabetes: preclinical biology and mechanisms of action. Diabetes Care. 2007;30(6):1335–1343. doi: 10.2337/dc07-0228. [DOI] [PubMed] [Google Scholar]
- 29.Aertgeerts K., Ye S., Tennant M. G., et al. Crystal structure of human dipeptidyl peptidase IV in complex with a decapeptide reveals details on substrate specificity and tetrahedral intermediate formation. Protein Science. 2004;13(2):412–421. doi: 10.1110/ps.03460604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vanderheyden M., Bartunek J., Goethals M., et al. Dipeptidyl-peptidase IV and B-type natriuretic peptide. from bench to bedside. Clinical Chemistry and Laboratory Medicine. 2009;47(3):248–252. doi: 10.1515/CCLM.2009.065. [DOI] [PubMed] [Google Scholar]
- 31.Meneilly G. S., Demuth H.-U., McIntosh C. H. S., Pederson R. A. Effect of ageing and diabetes on glucose-dependent insulinotropic polypeptide and dipeptidyl peptidase IV responses to oral glucose. Diabetic Medicine. 2000;17(5):346–350. doi: 10.1046/j.1464-5491.2000.00236.x. [DOI] [PubMed] [Google Scholar]
- 32.Korosi J., McIntosh C. H. S., Pederson R. A., et al. Effect of aging and diabetes on the enteroinsular axis. Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 2001;56(9):M575–M579. doi: 10.1093/gerona/56.9.m575. [DOI] [PubMed] [Google Scholar]
- 33.Lenhard J. M., Croom D. K., Minnick D. T. Reduced serum dipeptidyl peptidase-IV after metformin and pioglitazone treatments. Biochemical and Biophysical Research Communications. 2004;324(1):92–97. doi: 10.1016/j.bbrc.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 34.Lindsay J. R., Duffy N. A., McKillop A. M., et al. Inhibition of dipeptidyl peptidase IV activity by oral metformin in Type 2 diabetes. Diabetic Medicine. 2005;22(5):654–657. doi: 10.1111/j.1464-5491.2005.01461.x. [DOI] [PubMed] [Google Scholar]
- 35.Green B. D., Irwin N., Duffy N. A., Gault V. A., O'Harte F. P. M., Flatt P. R. Inhibition of dipeptidyl peptidase-IV activity by metformin enhances the antidiabetic effects of glucagon-like peptide-1. European Journal of Pharmacology. 2006;547(1–3):192–199. doi: 10.1016/j.ejphar.2006.07.043. [DOI] [PubMed] [Google Scholar]
- 36.Laakso M., Zilinskaite J., Hansen T., et al. Insulin sensitivity, insulin release and glucagon-like peptide-1 levels in persons with impaired fasting glucose and/or impaired glucose tolerance in the EUGENE2 study. Diabetologia. 2008;51(3):502–511. doi: 10.1007/s00125-007-0899-2. [DOI] [PubMed] [Google Scholar]
- 37.Abdul-Ghani M. A., DeFronzo R. A. Pathophysiology of prediabetes. Current Diabetes Reports. 2009;9(3):193–199. doi: 10.1007/s11892-009-0032-7. [DOI] [PubMed] [Google Scholar]
- 38.Zheng T., Gao Y., Baskota A., Chen T., Ran X., Tian H. Increased plasma DPP4 activity is predictive of prediabetes and type 2 diabetes onset in Chinese over a four-year period: result from the China National Diabetes and Metabolic Disorders Study. The Journal of Clinical Endocrinology & Metabolism. 2014;99(11):E2330–E2334. doi: 10.1210/jc.2014-1480. [DOI] [PubMed] [Google Scholar]
- 39.Dokken B. B., la Bonte L. R., Davis-Gorman G., Teachey M. K., Seaver N., McDonagh P. F. Glucagon-like peptide-1 (GLP-1), immediately prior to reperfusion, decreases neutrophil activation and reduces myocardial infarct size in rodents. Hormone and Metabolic Research. 2011;43(5):300–305. doi: 10.1055/s-0031-1271777. [DOI] [PubMed] [Google Scholar]
- 40.Dokken B. B., Piermarini C. V., Teachey M. K., et al. Glucagon-like peptide-1 preserves coronary microvascular endothelial function after cardiac arrest and resuscitation: potential antioxidant effects. American Journal of Physiology—Heart and Circulatory Physiology. 2013;304(4):H538–H546. doi: 10.1152/ajpheart.00282.2012. [DOI] [PubMed] [Google Scholar]
- 41.Noyan-Ashraf M. H., Shikatani E. A., Schuiki I., et al. A glucagon-like peptide-1 analog reverses the molecular pathology and cardiac dysfunction of a mouse model of obesity. Circulation. 2013;127(1):74–85. doi: 10.1161/circulationaha.112.091215. [DOI] [PubMed] [Google Scholar]
- 42.Robinson E., Cassidy R. S., Tate M., et al. Exendin-4 protects against post-myocardial infarction remodelling via specific actions on inflammation and the extracellular matrix. Basic Research in Cardiology. 2015;110, article 20 doi: 10.1007/s00395-015-0476-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ravassa S., Beaumont J., Huerta A., et al. Association of low GLP-1 with oxidative stress is related to cardiac disease and outcome in patients with type 2 diabetes mellitus: a pilot study. Free Radical Biology and Medicine. 2015;81:1–12. doi: 10.1016/j.freeradbiomed.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 44.Yamagishi S., Fukami K., Matsui T. Crosstalk between advanced glycation end products (AGEs)-receptor RAGE axis and dipeptidyl peptidase-4-incretin system in diabetic vascular complications. Cardiovascular Diabetology. 2015;14(1, article 2) doi: 10.1186/s12933-015-0176-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tahara N., Yamagishi S.-I., Takeuchi M., et al. Serum levels of advanced glycation end products (AGEs) are independently correlated with circulating levels of dipeptidyl peptidase-4 (DPP-4) in humans. Clinical Biochemistry. 2013;46(4-5):300–303. doi: 10.1016/j.clinbiochem.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 46.Ishibashi Y., Matsui T., Maeda S., Higashimoto Y., Yamagishi S.-I. Advanced glycation end products evoke endothelial cell damage by stimulating soluble dipeptidyl peptidase-4 production and its interaction with mannose 6-phosphate/insulin-like growth factor II receptor. Cardiovascular Diabetology. 2013;12(1, article 125) doi: 10.1186/1475-2840-12-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Augustyns K., Bal G., Thonus G., et al. The unique properties of dipeptidyl-peptidase IV (DPP IV / CD26) and the therapeutic potential of DPP IV inhibitors. Current Medicinal Chemistry. 1999;6(4):311–327. [PubMed] [Google Scholar]
- 48.Pala L., Mannucci E., Pezzatini A., et al. Dipeptidyl peptidase-IV expression and activity in human glomerular endothelial cells. Biochemical and Biophysical Research Communications. 2003;310(1):28–31. doi: 10.1016/j.bbrc.2003.08.111. [DOI] [PubMed] [Google Scholar]
- 49.Pala L., Pezzatini A., Dicembrini I., et al. Different modulation of dipeptidyl peptidase-4 activity between microvascular and macrovascular human endothelial cells. Acta Diabetologica. 2012;49(supplement 1):S59–S63. doi: 10.1007/s00592-010-0195-3. [DOI] [PubMed] [Google Scholar]
- 50.Aiuti A., Webb I. J., Bleul C., Springer T., Gutierrez-Ramos J. C. The chemokine SDF-1 is a chemoattractant for human CD34+ hematopoietic progenitor cells and provides a new mechanism to explain the mobilization of CD34+ progenitors to peripheral blood. The Journal of Experimental Medicine. 1997;185(1):111–120. doi: 10.1084/jem.185.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lapidot T., Kollet O. The essential roles of the chemokine SDF-1 and its receptor CXCR4 in human stem cell homing and repopulation of transplanted immune-deficient NOD/SCID and NOD/SCID/B2mnull mice. Leukemia. 2002;16(10):1992–2003. doi: 10.1038/sj.leu.2402684. [DOI] [PubMed] [Google Scholar]
- 52.Fadini G. P., Boscaro E., Albiero M., et al. The oral dipeptidyl peptidase-4 inhibitor sitagliptin increases circulating endothelial progenitor cells in patients with type 2 diabetes: possible role of stromal-derived factor-1alpha. Diabetes Care. 2010;33(7):1607–1609. doi: 10.2337/dc10-0187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jungraithmayr W., De Meester I., Matheeussen V., Baerts L., Arni S., Weder W. CD26/DPP-4 inhibition recruits regenerative stem cells via stromal cell-derived factor-1 and beneficially influences ischaemia-reperfusion injury in mouse lung transplantation. European Journal of Cardio-Thoracic Surgery. 2012;41(5):1166–1173. doi: 10.1093/ejcts/ezr180. [DOI] [PubMed] [Google Scholar]
- 54.van Poppel P. C. M., Netea M. G., Smits P., Tack C. J. Vildagliptin improves endothelium-dependent vasodilatation in type 2 diabetes. Diabetes Care. 2011;34(9):2072–2077. doi: 10.2337/dc10-2421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Takasawa W., Ohnuma K., Hatano R., Endo Y., Dang N. H., Morimoto C. Inhibition of dipeptidyl peptidase 4 regulates microvascular endothelial growth induced by inflammatory cytokines. Biochemical and Biophysical Research Communications. 2010;401(1):7–12. doi: 10.1016/j.bbrc.2010.08.112. [DOI] [PubMed] [Google Scholar]
- 56.Zhong J., Rao X., Deiuliis J., et al. A potential role for dendritic cell/macrophage-expressing DPP4 in obesity-induced visceral inflammation. Diabetes. 2013;62(1):149–157. doi: 10.2337/db12-0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Scherer P. E. Adipose tissue: from lipid storage compartment to endocrine organ. Diabetes. 2006;55(6):1537–1545. doi: 10.2337/db06-0263. [DOI] [PubMed] [Google Scholar]
- 58.Galic S., Oakhill J. S., Steinberg G. R. Adipose tissue as an endocrine organ. Molecular and Cellular Endocrinology. 2010;316(2):129–139. doi: 10.1016/j.mce.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 59.Shulman G. I. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. New England Journal of Medicine. 2014;371(12):1131–1141. doi: 10.1056/nejmra1011035. [DOI] [PubMed] [Google Scholar]
- 60.Sell H., Blüher M., Klöting N., et al. Adipose dipeptidyl peptidase-4 and obesity: correlation with insulin resistance and depot-specific release from adipose tissue in vivo and in vitro. Diabetes Care. 2013;36(12):4083–4090. doi: 10.2337/dc13-0496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Monami M., Ahrén B., Dicembrini I., Mannucci E. Dipeptidyl peptidase-4 inhibitors and cardiovascular risk: ameta-analysis of randomized clinical trials. Diabetes, Obesity and Metabolism. 2013;15(2):112–120. doi: 10.1111/dom.12000. [DOI] [PubMed] [Google Scholar]
- 62.Craddy P., Palin H. J., Johnson K. I. Comparative effectiveness of dipeptidylpeptidase-4 inhibitors in type 2 diabetes: a systematic review and mixed treatment comparison. Diabetes Therapy. 2014;5(1):1–41. doi: 10.1007/s13300-014-0061-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bosi E., Camisasca R. P., Collober C., Rochotte E., Garber A. J. Effects of vildagliptin on glucose control over 24 weeks in patients with type 2 diabetes inadequately controlled with metformin. Diabetes Care. 2007;30(4):890–895. doi: 10.2337/dc06-1732. [DOI] [PubMed] [Google Scholar]
- 64.DeFronzo R. A., Hissa M. N., Garber A. J., et al. The efficacy and safety of saxagliptin when added to metformin therapy in patients with inadequately controlled type 2 diabetes with metformin alone. Diabetes Care. 2009;32(9):1649–1655. doi: 10.2337/dc08-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Forst T., Uhlig-Laske B., Ring A., et al. Linagliptin (BI 1356), a potent and selective DPP-4 inhibitor, is safe and efficacious in combination with metformin in patients with inadequately controlled type 2 diabetes. Diabetic Medicine. 2010;27(12):1409–1419. doi: 10.1111/j.1464-5491.2010.03131.x. [DOI] [PubMed] [Google Scholar]
- 66.Rhee E. J., Lee W. Y., Min K. W., et al. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor gemigliptin compared with sitagliptin added to ongoing metformin therapy in patients with type 2 diabetes inadequately controlled with metformin alone. Diabetes, Obesity and Metabolism. 2013;15(6):523–530. doi: 10.1111/dom.12060. [DOI] [PubMed] [Google Scholar]
- 67.Göke B., Gallwitz B., Eriksson J., Hellqvist Å., Gause-Nilsson I., D1680C00001 Investigators Saxagliptin is non-inferior to glipizide in patients with type 2 diabetes mellitus inadequately controlled on metformin alone: a 52-week randomised controlled trial. International Journal of Clinical Practice. 2010;64(12):1619–1631. doi: 10.1111/j.1742-1241.2010.02510.x. [DOI] [PubMed] [Google Scholar]
- 68.Filozof C., Gautier J.-F. A comparison of efficacy and safety of vildagliptin and gliclazide in combination with metformin in patients with type 2 diabetes inadequately controlled with metformin alone: a 52-week, randomized study. Diabetic Medicine. 2010;27(3):318–326. doi: 10.1111/j.1464-5491.2010.02938.x. [DOI] [PubMed] [Google Scholar]
- 69.Bolli G., Dotta F., Rochotte E., Cohen S. E. Efficacy and tolerability of vildagliptin vs. pioglitazone when added to metformin: a 24-week, randomized, double-blind study. Diabetes, Obesity and Metabolism. 2008;10(1):82–90. doi: 10.1111/j.1463-1326.2007.00820.x. [DOI] [PubMed] [Google Scholar]
- 70.Sicras-Mainar A., Navarro-Artieda R. Economic impact of combining metformin with dipeptidyl peptidase-4 inhibitors in diabetic patients with renal impairment in spanish patients. Diabetes & Metabolism Journal. 2015;39(1):74–81. doi: 10.4093/dmj.2015.39.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nathan D. M., Buse J. B., Kahn S. E., et al. Rationale and design of the glycemia reduction approaches in diabetes: a comparative effectiveness study (GRADE) Diabetes Care. 2013;36(8):2254–2261. doi: 10.2337/dc13-0356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Frederich R., Alexander J. H., Fiedorek F. T., et al. A systematic assessment of cardiovascular outcomes in the saxagliptin drug development program for type 2 diabetes. Postgraduate Medicine. 2010;122(3):16–27. doi: 10.3810/pgm.2010.05.2138. [DOI] [PubMed] [Google Scholar]
- 73.Johansen O. E., Neubacher D., von Eynatten M., Patel S., Woerle H.-J. Cardiovascular safety with linagliptin in patients with type 2 diabetes mellitus: a pre-specified, prospective, and adjudicated meta-analysis of a phase 3 programme. Cardiovascular Diabetology. 2012;11, article 3 doi: 10.1186/1475-2840-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schweizer A., Dejager S., Foley J. E., Couturier A., Ligueros-Saylan M., Kothny W. Assessing the cardio-cerebrovascular safety of vildagliptin: meta-analysis of adjudicated events from a large Phase III type 2 diabetes population. Diabetes, Obesity and Metabolism. 2010;12(6):485–494. doi: 10.1111/j.1463-1326.2010.01215.x. [DOI] [PubMed] [Google Scholar]
- 75.Engel S. S., Round E., Golm G. T., Kaufman K. D., Goldstein B. J. Safety and tolerability of sitagliptin in type 2 diabetes: pooled analysis of 25 clinical studies. Diabetes Therapy. 2013;4(1):119–145. doi: 10.1007/s13300-013-0024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Patil H. R., Al Badarin F. J., Al Shami H. A., et al. Meta-analysis of effect of dipeptidyl peptidase-4 inhibitors on cardiovascular risk in type 2 diabetes mellitus. The American Journal of Cardiology. 2012;110(6):826–833. doi: 10.1016/j.amjcard.2012.04.061. [DOI] [PubMed] [Google Scholar]
- 77.Ussher J. R., Drucker D. J. Cardiovascular biology of the incretin system. Endocrine Reviews. 2012;33(2):187–215. doi: 10.1210/er.2011-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hausenloy D. J., Whittington H. J., Wynne A. M., et al. Dipeptidyl peptidase-4 inhibitors and GLP-1 reduce myocardial infarct size in a glucose-dependent manner. Cardiovascular Diabetology. 2013;12(1, article 154) doi: 10.1186/1475-2840-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Terawaki Y., Nomiyama T., Kawanami T., et al. Dipeptidyl peptidase-4 inhibitor linagliptin attenuates neointima formation after vascular injury. Cardiovascular Diabetology. 2014;13(1, article 154) doi: 10.1186/s12933-014-0154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Scirica B. M., Raz I., Cavender M. A., et al. Abstract 17503: outcomes of patients with type 2 diabetes and known congestive heart failure treated with saxagliptin: analyses of the SAVOR-TIMI 53 study. Circulation. 2013;128A17503 [Google Scholar]
- 81.Standl E. Saxagliptin, alogliptin, and cardiovascular outcomes. The New England Journal of Medicine. 2014;370(5, article 484) doi: 10.1056/NEJMc131388035;SA1. [DOI] [PubMed] [Google Scholar]
- 82.Savarese G., Perrone-Filardi P., D'Amore C., et al. Cardiovascular effects of dipeptidyl peptidase-4 inhibitors in diabetic patients: a meta-analysis. International Journal of Cardiology. 2015;181:239–244. doi: 10.1016/j.ijcard.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 83.Standl E. Saxagliptin, alogliptin, and cardiovascular outcomes. The New England Journal of Medicine. 2014;370(5):483–484. doi: 10.1056/NEJMc1313880. [DOI] [PubMed] [Google Scholar]
- 84.Devin J. K., Pretorius M., Nian H., Yu C., Billings F. T., IV, Brown N. J. Substance P increases sympathetic activity during combined angiotensin-converting enzyme and dipeptidyl peptidase-4 inhibition. Hypertension. 2014;63(5):951–957. doi: 10.1161/hypertensionaha.113.02767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dicembrini I., Mannucci E. Risk of myocardial infarction in trials with dipeptidyl peptidase-4 inhibitors: is duration of study a real issue? International Journal of Cardiology. 2015 doi: 10.1016/j.ijcard.2015.02.034. [DOI] [PubMed] [Google Scholar]