Abstract
The outbreak of extensively drug-resistant tuberculosis (XDR-TB) has become an increasing problem in many TB-burdened countries. The underlying drug resistance mechanisms, including the genetic variation favored by selective pressure in the resistant population, are partially understood. Recently, the first case of XDR-TB was reported in Malaysia. However, the detailed genotype family and mechanisms of the formation of multiple drugs resistance are unknown. We sequenced the whole genome of the UM 1072388579 strain with a 2-kb insert-size library and combined with that from previously sequenced 500-bp-insert paired-end reads to produce an improved sequence with maximal sequencing coverage across the genome. In silico spoligotyping and phylogenetic analyses demonstrated that UM 1072388579 strain belongs to an ancestral-like, non-Beijing clade of East Asia lineage. This is supported by the presence of a number of lineage-specific markers, including fadD28, embA, nuoD and pks7. Polymorphism analysis showed that the drug-susceptibility profile is correlated with the pattern of resistance mutations. Mutations in drug-efflux pumps and the cell wall biogenesis pathway such as mmpL, pks and fadD genes may play an important role in survival and adaptation of this strain to its surrounding environment. In this work, fifty-seven putative promoter SNPs were identified. Among them, we identified a novel SNP located at -4 T allele of TetR/acrR promoter as an informative marker to recognize strains of East Asian lineage. Our work indicates that the UM 1072388579 harbors both classical and uncommon SNPs that allow it to escape from inhibition by many antibiotics. This study provides a strong foundation to dissect the biology and underlying resistance mechanisms of the first reported XDR M. tuberculosis in Malaysia.
Introduction
The global rise of extensively drug-resistant tuberculosis (XDR-TB) has jeopardized efforts in the treatment and control of TB. XDR-TB is commonly caused by Mycobacterium tuberculosis which is resistant to rifampicin, isoniazid, fluoroquinolones, and one of the three second-line injectable antibiotics: kanamycin, amikacin or capreomycin [1]. XDR-TB cases have since been reported by 100 countries worldwide, including South Africa [2], India [3], East Asia [4, 5] and European countries [6–8]. In most XDR-TB-burdened countries, previous attempts to address this epidemic have been obviously unsuccessful as they face huge obstacles in the rapid diagnosis and control of this drug-resistant TB. In Malaysia, we have also recently reported, to our knowledge, the first XDR-TB case [9]. However, little is known about the nature of this strain and such information is obviously required for better diagnosis and control of this drug-resistant TB.
The evolutionary origin and nature of the XDR M. tuberculosis strains remain unknown. Two possible explanations have been postulated to describe the occurrence and transmission of XDR-TB worldwide. The first explanation involves clonal expansion and spreading of one strain harboring several drug-resistance mutations [10–12]. Alternatively, it appears that drug-resistance mutational events occurred multiple times separately in different strains, proposing repeated selection from a pool of pre-existing strains through the chemotherapeutic usage pattern rather than the spread of a single drug-resistant strain [13]. The advent of high throughput Next Generation Sequencing technologies (NGS) provide a step forward in drug-resistant TB research to decipher the biology, adaptation and evolution of these “extreme” strains. Although there are whole genome sequence data for XDR in the international databases [12, 14–18], the whole genome sequences of XDR strains from Southeast Asia tropical countries are still lacking. In 2013, we sequenced the genome of the first XDR M. tuberculosis strain UM 1072388579 with a 500-bp insert-size library [9]. Here, we sequenced the UM 1072388579 genome with a 2-kb insert-size library and combined the genomic sequence data with that from the previous sequencing using the small DNA insert library to improve genome assembly. In Malaysia, only one XDR-TB case has been reported so far. The origin and the genotype of XDR M. tuberculosis in the country are totally unclear. In this study, we demonstrated that the UM 1072388579 strain harbors an ancestral-like spoligotype, which is close to the Beijing clade of East Asia lineage.
At this stage of knowledge, there is still a need for thorough investigation of SNPs present in drug resistance associated genes and intergenic regions (IGRs) although several classical mutations such as katG, ndh, pncA, rpoB and gyrA have been reported [19]. With this goal in mind, we comprehensively analyzed the underlying molecular genetic basis for drug resistance in order to identify novel resistance mutations. Genetic characterization of clinical isolates requires systematic SNP analysis. Thus, it is hoped that the thoroughly analysis of the UM 1072388579 genome will help to provide critical information for the XDR M. tuberculosis in Malaysia.
Materials and Methods
Ethic statement
The isolate used in this study was obtained from the previously published study [9]. All labels on the source sample have been erased with the exception of sample type and clinical diagnosis. Thus there is no information traceable back to the patient from whom the isolate was obtained. As such, this genomic study is exempt from ethical approval in our teaching hospital. (http://www.ummc.edu.my/view/content.php?ID=VGxSWlBRPT0=).
Strain and drug-susceptibility testing
M. tuberculosis strain UM 1072388579 was isolated from sputum of a 57 year-old man in the Mycobacteriology Laboratory, University Malaya Medical Centre, Kuala Lumpur, Malaysia. Culture of the clinical isolate was performed using a BACTEC MGIT 960 Culture system (Becton Dickinson) as described in the previous study [20]. An hundred microliter aliquot of MGIT broth was removed for microscopy examination with Auramine and Ziehl-Neelsen staining to ensure the presence of acid fast bacilli on the day of detection of culture positive. Gram-staining was performed on the same aliquot of broth to confirm there was no bacterial contamination. For identification of mycobacterial species, 1 mL of aliquot of MGIT broth was transferred to a screw-capped 1 mL tube for GenoType Mycobacterium CM assay [20].
Drug susceptibility testing of the clinical isolate was performed on the isolated M. tuberculosis strain using a BACTEC MGIT 960 Culture system [20]. The concentrations of drugs used for testing were 1.0 μg/mL rifampicin, 0.2 μg/mL isoniazid, 2.5 μg/mL kanamycin, 1.0 μg/mL amikacin, 2.5 μg/mL capreomycin, 2.0 μg/mL streptomycin, 1.0 μg/mL ciprofloxacin, 2.0 μg/mL ofloxacin, 5.0 μg/mL ethambutol, 5.0 μg/mL ethionamide and 4.0 μg/mL para-salicylic acid. The UM 1072388579 isolate was tested using the MTBDRplus and MTBDRsl assays but the commercially available tests would not be able to identify resistance to specific drugs due to the lack of well-known mutations associated to a drug resistant phenotype.
Genomic DNA extraction
Genomic DNA was carried out in a Class III biological safety cabinet according to the chemical lysis method [21]. In this study, a hundred Lowenstein-Jensen culture slants was used to obtain sufficient total DNA (40 μg) for both small and large insert library sizes whole genome sequencing. All visible colonies from Lowenstein-Jensen medium were collected into a microcentrifuge tube containing 350 μL Tris-EDTA buffer (10 mM Tris-base and 1 mM EDTA, pH 8.0). The suspension was mixed with 50 μL of lysozyme (10 mg/mL) and 10 μL of RNAse A and incubated at 37°C for 2 hours. The mixture was then incubated with 50 μL of proteinase K (10 mg/mL) at 55°C for 20 minutes. Next, the mixture was mixed with 100 μL of 10% (w/v) of SDS and incubated at 37°C for 1 hour. After 1 hour incubation, proteins were precipitated with 5 M NaCl and 100 μL of Cetyltrimethyl Ammonium Bromide (CTAB), followed by incubation at 65°C for 10 minutes. Genomic DNA was then purified and precipitated with equal volume of chloroform: isoamyl alchohol (24:1, v/v) and isopropanol, respectively. The tube was then centrifuged at 10,000 ×g for 20 minutes at 4°C. It is important to pipette the DNA very slowly when transferring the aqueous (upper) phase to avoid disturbing the material at the interface. Genomic DNA was washed from the pellet by adding 650 μL of ice-cold 70% (v/v) ethanol and centrifuged at 10,000 ×g for 5 minutes at 4°C. The washing step was repeated for three times. Finally, the pellet was dissolved in nuclease-free distilled water. The pellet of DNA was not dried completely as desiccated DNA is very hard to dissolve. The quantity and quality of the extracted genomic DNA was determined using NanoDrop 2000c spectrophotometer (Thermo Fisher Scientific). Pure DNA sample is indicated by A260/A280 ratio between 1.8–2.0. In addition, a total sample quantity of 6 μg and 40 μg is required for short-insert library and large-insert library, respectively.
Genome sequencing and assembly
Whole genome sequencing of UM 1072388579 was performed using Illumina HiSeq 2000 Sequencer (Illumina) in a 2×90 bp paired-end mode on 500-bp and 2-kb library sizes. Illumina library was prepared using TruSeq v3 Reagent Kits (Illumina). Qualified DNA sample was sheared into smaller fragments by Covaris S/E210. The selected library fragments were purified through gel-electrophoresis, then selectively enriched and amplified by PCR. All raw reads were first pre-processed using FASTX-Toolkit (http://hannonlab.cshl.edu/fastx_toolkit/) trimming bases with a Phred quality below Qv20 from the 3’-end of the reads, retaining small-insert reads ≥ 80 bp and large-insert reads ≥ 30 bp. Two nucleotides were trimmed from the 5’-terminal of the reads. All reads with 40% bases having Qv ≤ 20 were then filtered out. Pre-processed reads from both libraries were assembled with Velvet version 1.2.07 [22] using k-mer setting = 63, insert length = 503, -ins_length_sd = 103 and -min_pair_count = 15. Additional parameter of-shortMatePaired = yes was set for large insert library. The generated sequences assembled from the Velvet assembly were then scaffolded using SSPACE Basic v2.0 [23] with more stringent parameters than software default to achieve higher accuracy assembly (parameters:-z 100, -k 15, -a 0.3, -n 30 and -T 10). GapFiller v1.10 was employed to perform gap filling by using paired-end sequencing data from both libraries [24, 25] with parameter settings-m = 60, -o = 15, -r = 0.8,–n = 30, -t = 30 and -T = 10.
Gene prediction and annotation
Protein coding sequences of UM 1072388579 were predicted using GeneMarkS v4.10d [26]. Annotation of coding sequences for UM 1072388579 was completed using BLAST (Basic Local Alignment Search Tool) searches against the NCBI non-redunctant (nr), SwissProt and COG databases. rRNAs and tRNAs were identified using RNAmmer v1.2 [27] and tRNAscan-SE v1.3.1 [28], respectively.
Determination of Principal genotypic group
To determine the principal genotypic group (PGG), the coding sequences of katG and gyrA were first retrieved from the sequenced genome using Artemis v12.0 sequence viewer [29]. The nucleotide polymorphism at katG codon 463 and gyrA codon 95 of UM 1072388579 was determined by compared with the katG and gyrA protein sequences retrieved from the H37Rv strain.
In silico Spoligotyping
Spoligotype of UM 1072388579 was inferred in silico from raw sequence files (fastq format) using SpolPred software with default parameters [30]. The result was then matched to the SpolDB4 [31] and SITVITWEB [32] spoligotype databases to determine the spoligotype pattern.
Genome-wide SNPs analysis
Single nucleotide polymorphism (SNP) discovery was performed using MUMmer v3.23 [33]. Nucmer algorithm (default parameters) of the MUMmer software package was used to align genomic sequences (contigs or complete genomes) to the H37Rv reference genome (RefSeq NC_000962) and primary SNP calls were generated by using show-snps algorithm (parameters:-Clr) from the same software package. SNPs from potential paralogous regions were excluded for further analysis. The SNPs discovered in UM 1072388579 were annotated based on the H37Rv genome annotation and classified as synonymous, non-synonymous or intergenic using ANNOVAR [34].
Phylogenetic analysis
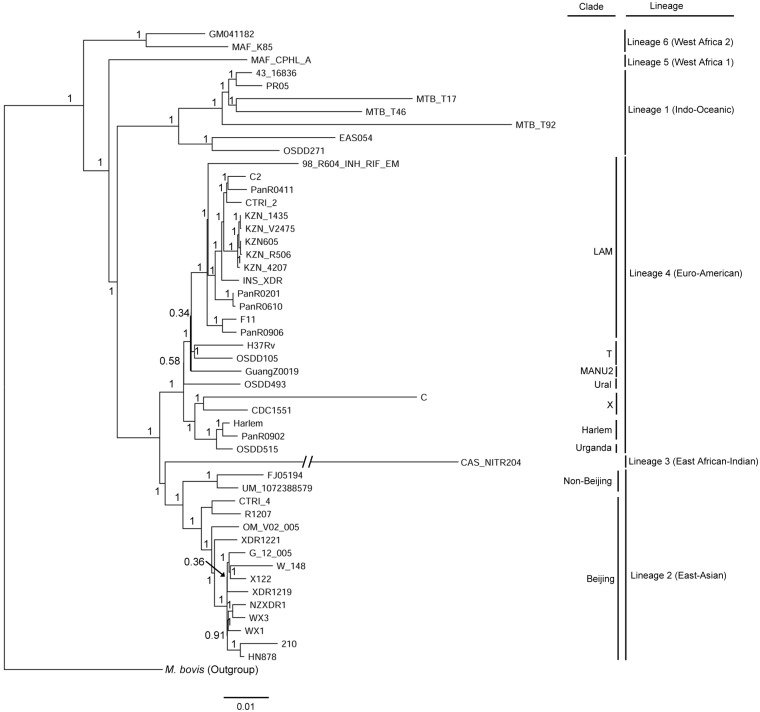
SNPs in 50 Mycobacterium genomes (including UM 1072388579, 48 M. tuberculosis representing the main six MTBC lineages, and the outgroup species M. bovis) (S1 Table) were identified using MUMmer v3.23. A total of 20,708 SNPs were found to be common in all the 50 genomes. SNPs in each genome were concatenated into single contiguous sequences and aligned. The resulting SNP-based alignment was used to perform Bayesian MCMC inference analysis using MrBayes v3.2.2 [35] (ran for 1,500,000 MCMC generations with sampling every 500 generations). The average SD of split frequencies was below 0.01 after 1.5 million generations, indicative of convergence. Posterior probabilities were averaged over the final 75% of trees (25% burn in). The phylogenetic tree was plotted using FigTree v1.4.2 (http://tree.bio.ed.ac.uk/software/figtree/).
Identification of SNPs in promoter region
One kilobase (kb) of upstream regions of annotated genes was retrieved from the UM 1072388579 genome using Artemis v12.0 sequence viewer [29]. The promoters were then predicted from these non-coding sequences using the Neural Network Promoter Prediction computer program (parameters: type of organism: prokaryote; minimum promoter score: 0.8) [36]. The predicted promoter regions were cross-checked with the SNPs identified in UM 1072388579 using in-house Perl script. Briefly, the Perl script compared the genomic location of each SNP against the predicted promoter regions and identified putative SNPs residing in the putative promoters.
Results and Discussion
Characteristics of the UM 1072388579 isolate
M. tuberculosis strain UM 1072388579 was isolated from a 57-year-old patient in University Malaya Medical Centre. The isolate was sub-cultured and re-tested for the susceptibility to first-line and second-line drugs twice using BACTEC MGIT 960 Culture system, prior to whole genome sequencing. The drug susceptibility tests confirmed that UM 1072388579 isolate is XDR M. tuberculosis. It was resistant to rifampicin, isoniazid, streptomycin, ethambutol, pyrazinamide, kanamycin, amikacin, capreomycin, ethionamide and fluoroquinolones (ofloxacin and ciprofloxacin) but sensitive to para-salicylic acid.
Genome sequence of UM 1072388579 strain from Malaysia
To gain insight into its underlying molecular mechanism in the development of XDR phenotype, we have sequenced the UM 1072388579 genome. The UM 1072388579 genome was sequenced to >99% completion with ~100-fold depth of genome sequence coverage. A total of 8,394,316 paired reads (0.73 Gb) of a 500-bp insert-size library and 11,190,552 paired reads (0.97 Gb) of a 2-kb insert-size library were generated by Illumina HiSeq 2000 Sequencing system. The mate pair combined sequencing data showed a lower number of contigs and a higher N50 value compared to that generated from the single short DNA insert library (Table 1). The assembly yielded a combined total length of 4,370,957 bases in 80 contigs (≥200 bases) which were then placed into 19 scaffolds (≥1,000 bases) with paired-end sequencing data from both libraries. The assembly has an N50 scaffold size of 1,081,051 bases with an average G+C content of 65.15%. The high G+C content indicates the more biased codon frequencies of the proteins in UM 1072388579 isolate [37]. A total of 4,159 coding DNA sequences (CDS) with length of ≥33 amino acids was predicted, from which 4,126 and 3,122 proteins were functional annotated using local BLAST similarity searches against NCBI nr and SwissProt databases, respectively (S2 Table). All the proteins were also ascribed to 21 different functional groups based on Clusters of Orthologous Groups (COGs) (S2 Table and S1 Fig). Apart from the poorly characterized categories: categories R (general functions prediction only) and S (function unknown), our result showed that UM 1072388579 strain has a great potential to synthesize various group of lipophilic molecules (palmitate, tuberculostearic acid and mycolic acid), essential amino acids, enzyme co-factors and vitamins (S2 Table and S1 Fig). By comparing the sequenced UM 1072388579 to H37Rv, we observed that the moaB3 gene, which is involved in molybdopterin biosynthesis, is totally missing in our isolate. The biosynthesis of molybdopterin is involved in the physiology and intracellular survival of M. tuberculosis [38]. Therefore, the moaB3 gene might not be important for pathogenesis. Since there are 21 genes dedicated to the molybdopterin biosynthesis [37], it is possible that other family members compensate for the loss of moaB3 gene. Furthermore, our pipeline showed that there is one rRNA operon for 5S, 16S and 23S and 45 tRNAs in the genome (Table 1).
Table 1. Comparison of short-insert paired-end (500-bp) and mate pair combined sequencing data.
| Details | Short-insert paired-end (500-bp) | Paired-end and mate pair combined (500-bp and 2-kb) |
|---|---|---|
| Sequencing depth | ~100× | ~100× |
| Total length of sequences (bp) | 4,290,533 | 4,370,957 |
| Total number of contigs (≥200 bp) | 184 | 80 |
| Total number of scaffolds (≥1,000 bp) | 89 | 19 |
| N50 (bp) | 108,779 | 1,081,051 |
| G+C (%) | 65.40 | 65.15 |
| Number of predicted protein coding-gene (≥ 33 amino acids) | 4,099 | 4,151 |
| Annotated protein coding regions (nr) | 4,069 | 4,126 |
| tRNAs | 45 | 45 |
| 5s rRNA | 1 | 1 |
| 16s rRNA | 1 | 1 |
| 23s rRNA | 1 | 1 |
We then captured all genetic differences of UM 1072388579 by comparing with the H37Rv reference genome. From that, a total of 1,397 genic SNPs were localized to the UM 1072388579. Of these polymorphisms, 536 and 861 of them were identified as synonymous SNPs (sSNPs) and non-synonymous SNPs (nsSNPs), respectively. The 861 nsSNPs were distributed in 644 genes. The details of identified SNPs in UM 1072388579 are available in the supplemental material (S3 Table).
Genotype of UM 1072388579
Principal genetic group (PGG) of our clinical isolate was first defined based on the combination of nucleotide polymorphisms at katG codon 463 and gyrA codon 95 [39]. We found that UM 1072388579 is grouped into PGG1 with KatG463 CTG (Leu) and GyrA95 ACC (Thr), in contrast to PGG3 [KatG463 CGG (Arg) and GyrA95 AGC (Ser)] for H37Rv strain. PGG1 organisms are evolutionarily old and related to Mycobacterium bovis, notorious for causing bovine tuberculosis [39]. Sreevatsan et al. (1997) also reported that PGG1 organisms are ancestral to PGG2 and PGG3 M. tuberculosis. Based on the PGG grouping, UM 1072388579 is thought to be an ancient strain, although this evolutionary hypothesis that was proposed by Sreevatsan et al. (1997) is based on only two nsSNPs [39].
Six major lineages of M. tuberculosis have been described, including the Indo-Oceanic (East African Indian, EAI), East Asian (non-Beijing and Beijing), East African-Indian (Central Asian, CAS), Euro-American (Haarlem, Latin American Mediterranean (LAM), T, X, Urganda and Ural clades), West African 1 and West African 2 lineages [31]. XDR-TB has been associated with almost every M. tuberculosis genotype family, such as Euro-American (Haarlem, LAM, T, X, Ural) [12, 14, 40], Central Asian (CAS) [41] and Beijing [40, 42]. Here, we determined the spoligotype of UM 1072388579 by using SpolPred and matching the read to the SpolDB4 database. The result showed that UM 1072388579 strain exhibits an almost complete, ancestral-like spoligotype pattern (777777777777731, ST. no 246) [43, 44] as it misses spacer 40 only (Table 2). However, the result showed that it cannot be clustered unambiguously in any known genotype family (Table 2). Non-Beijing isolates with such ancestral-like spoligotype patterns belong to the East Asia lineage [43, 45].
Table 2. Spoligotypes of UM 1072388579 and FJ05194 strains.
| Strain | SIT a | Clade |
|---|---|---|
| UM 1072388579 | 246 | Unassignable |
| FJ05194 | 643 | Unassignable |
| LN130 | 1 | Beijing |
a SIT correspond to the Spoldb4 international database code accessible at http://www.pasteur-guadeloupe.fr/tb/bd_myco.html.
A SNP in fadD28 gene (codon 507) was previously used as a marker to identify M. tuberculosis isolates of the Beijing clade and genetically similar non-Beijing East Asia lineage isolates [46]. Conversely, no SNP was observed in fadD28 for isolates from other genotype families (EAI, T, LAM, MANU, Haarlem and S clades) [46]. To support that UM 1072388579 strain belongs to the non-Beijing clade of East Asian lineage, we have identified lineage-specific SNPs at fadD28 (I507I), embA (A2856G), nuoD (A201T) and pks7 (C5787T) [47] in our isolate (Table 3).
Table 3. Lineage-specific SNPs shared between the UM 1072388579 and FJ05194.
A phylogenetic tree was then constructed based on a genome-wide set of SNPs to further gain insight into the genotype of UM 1072388579. Forty-nine additional published M. tuberculosis whole genomes were used for the comparative phylogenetic analysis (S1 Table). The result agrees well with a previously published phylogenetic tree [42, 48] and our isolate is clustered together with FJ05194, which is very close to the Beijing clade of East Asian lineage (Fig 1). FJ05194 strain was isolated from a patient in Fujian, China [15]. Both strains share similar lineage-specific markers [46, 47] that characterize the non-Beijing clade of East Asian lineage (Table 3). Considering that both strains of UM 1072388579 and FJ05194 were clustered together, we used the same algorithm to identify the spoligotype pattern of FJ05194. The result obviously showed that FJ05194 has an ancestral-like spoligotype pattern (777777757777771, ST. no 643) which is almost similar to our strain (Table 2). LN130 strain [40] with the known Beijing clade was included in the same analysis to confirm that the results are valid (Table 2). Non-Beijing isolates of ST no. 246 and 623 ancestral-like spoligotypes were reported to be genetically similar to Beijing clade [46], which have emerged from the South part of China, Guangxi autonomous region [44]. Wan and collaborators also proposed that such ancestral strains are mainly found in Guangxi, which are thought to be representatives of East Asia lineage branching out prior the occurrence of the modern Beijing isolates [44]. Overall, it is tempting to speculate that UM 1072388579 represents the ancestor of the Beijing clade that originated from the South part of China.
Fig 1. Comparative phylogenetic analysis of UM 1072388579 strain along with 50 previously published genomes.
Phylogenetic tree was constructed based on overall SNPs extracted from genome sequences. The numbers on branches indicate Bayesian posterior probability values. M. tuberculosis isolates are clustered into respective genotype families based on spoligotyping-defined M. tuberculosis clade and lineage. The tree is rooted with M. Bovis BCG strain ATCC 35743 as outgroup.
Drug resistance patterns of UM 1072388579
We focused on the nsSNPs to determine the pattern of resistance mutations in each drug tested. Our polymorphism analysis demonstrated that the presence of resistance mutations were consistent with the drug-resistant phenotype (Table 4).
Table 4. Polymorphisms in UM 1072388579 strain inferred to be associated with drug resistance.
| Drug resistance effect | Gene name | Mutation | Function |
|---|---|---|---|
| Isoniazid | katG (Rv1908c) | R463L and L141F | Catalase/peroxidase |
| Rifampicin | rpoB (Rv0667) | S450L | RNA polymerase (β subunit) |
| Ethambutol | embB (Rv3795) | Q497R | Arabinosyl transferase |
| Ethionamide | ethA (Rv3854c) | Ins862C | Monooxygenase |
| Rv0565c | R110H | Probable monooxygenase | |
| Rv1936 | Q68H | Probable monooxygenase | |
| Rv3618 | D117Y | Probable monooxygenase | |
| Fluoroquinolone (ofloxacin and ciprofloxacin) | gyrA (Rv0006) | E21Q, S91P, S95T and G668D | DNA gyrase (subunit A) |
| Streptomycin | gidB (Rv3919c) | G30V | 7-methylguanosine methyltransferase |
| Kanamycin and amikacin | eis (Rv2416) | A22G | Enhanced intracellular survival protein |
| Capreomycin | tlyA (Rv1694) | Ins363GC | 2’-O-methyltransferase |
| Cycloserine | cycA (Rv1704c) | R93L | D-serine/alanine/glycine transporter protein |
| DdlA (Rv2981) | T365A | D-alanine:D-alanine ligase | |
| alr (Rv3423) | S22L | D-alanine racemase |
The underlying molecular mechanisms of isoniazid resistance are complex as they are mediated by several genes including katG, inhA, mabA-inhA IGR and other unknown genes [49]. For UM 1072388579, isoniazid resistance might be associated with the R463L and L141F mutations in katG, the catalase/peroxidase that converts pro-drug isoniazid into an active form [50]. As previously reported [51, 52], R463L mutation has higher catalase activity than other resistance mutations and this may play a role in virulence of drug-resistant M. tuberculosis strains. However, R463L mutation is known not to be associated with isoniazid resistance [53]. L141F is a rare mutation in katG, which was frequently found in isolates with low level resistance to isoniazid [54], but it has not been confirmed to be associated to a resistant phenotype. Interestingly, previous study revealed that the catalase and isoniazid oxidation activities were not detected in KatGL141F-R463L mutant [52]. In our case, it could be that a gene mutation conferring a lower level of resistance occurred first, followed by the acquisition of a second mutation in another gene that yielded a greater resistance for the strain. Collectively, they could have a cumulative effect in the development of isoniazid resistance in UM 1072388579.
With respect to rifampicin resistance, UM 1072388579 has the mutation of S450L in rpoB (β subunit of RNA polymerase). In addition, we identified two non-frameshift insertions (Ins629PP and Ins631S) in ponA1 (penicillin-binding protein 1A) that is responsible for the biosynthesis of peptidoglycan layer in the cell wall. Previous functional genetic analysis confirmed that M. tuberculosis isolates containing the ponA1 mutation had a greater survival advantage in the presence of rifampicin [55]. Previous studies showed that depletion of ponA1 increase susceptibility to β-lactam antibiotics in M. smegmatis [56], suggested mutation in ponA1 might play a role to inhibit activities of some antibiotics. However, the exact role of the ponA1 mutations in UM 1072388579 remains unknown.
Ethambutol resistance of our isolate is most likely caused by the Q497R mutation in the transmembrane protein embB [57]. Interestingly, embB mutations have been reported that did not associate with ethambutol-resistance alone, but were related to both ethambutol and rifampicin resistance [58]. In UM 1072388579 isolate, the mutation in embB might have a role in the inhibition of both rifampicin and ethambutol activities.
In M. tuberculosis, DNA gyrase (encoded by gyrA and gyrB genes) is the common target for fluoroquinolones [59]. Polymorphism analysis shows a mutation in gyrA at the position of S91P. Ethionamide resistance in UM 1072388579 can be explained by the frameshift insertion in ethA. Like many anti-TB drugs, ethionamide is a pro-drug which requires metabolic activation by the enzyme ethA, a monooxygenase. Thus, a frameshift mutation in amino acid 288 caused by 1 bp insertion causes our clinical isolate to be resistant to ethionamide. We have also checked out SNPs in known genes coding the probable monooxygenase and found that UM 1072388579 strain carried mutations in Rv0565c, Rv1936 and Rv3618 (Table 4). The role of the mutations in these putative monooxygenase genes in fluoroquinolones resistance thus deserves greater attention.
The classical mutations that are associated with streptomycin resistance in rpsL (ribosomal protein S12) and in rrs (16S ribosomal RNA) genes were not identified in UM 1072388579. Previous study showed that mutations of these two genes contributed to only 70% cases of total streptomycin resistant isolates [60], implying that there must be other gene(s) which can be involved in the streptomycin resistance in UM 1072388579. Therefore, resistance to streptomycin is most likely attributed to the mutation in gidB at the position of G30V (Table 4). The gidB encodes SAM-dependent methyltransferase that catalyzes methylation at the position G527 in the 16S ribosomal RNA, giving an additional hydrophobic binding site for streptomycin [61]. As previously noted [61], mutations in gidB are the source for conferring low-level streptomycin resistance in Streptomyces coelicolor. Feuerriegel et al. (2012) reported that L16R, A205A and V110V in gidB were associated to phylogenetic features rather than being involved in drug resistance [62]. However, mutations at the position of G34A, V65G, G71A, V88G, L91P, S100F, A138V and A200E might be associated with streptomycin resistance as these mutations occur exclusively in streptomycin resistant strains [62]. Like our study, Spies et al. (2011) showed some mutations (codons 30, 45, 48, 49, 51, 52, 67, 75, 117 and 164) were associated with low-level streptomycin resistance in streptomycin resistant strains that contained no mutations in the rpsL or rrs genes [63]. Up until now, reasons for streptomycin-resistant strains exhibiting no mutation in rrs or rpsL and shift to mutation in gidB remain unknown [63, 64].
The drug-susceptibility test also showed that UM 1072388579 is resistant to kanamycin, amikacin and capreomycin. Unlike a previous study [65], kanamycin and amikacin resistance in UM 1072388579 might be associated with a non-synonymous mutation in eis gene (A22G). Capreomycin resistance of our isolate might be correlated with the frameshift insertion in tlyA (2’-O-methyltransferase). The functionality tlyA gene was disrupted by insertion mutation to catalyze methylation reaction on 23S rRNA (at nucleotide C1920) and 16S rRNA (at nucleotide C1409). Capreomycin resistance is attributed by the defect of this methylation reaction on 23S rRNA and 16S rRNA [66]. As in our work, a recent study discovered a novel frameshift insertion, Ins49GC in capreomycin-resistant M. tuberculosis strains [67].
It should be noted that our clinical isolate also harbors several mutations which are associated with D-cycloserine (Table 4), though susceptibility to these drugs was not examined. To date, the resistance mechanisms of D-cycloserine are poorly understood. D-cycloserine is a cyclic analog of D-alanine that hinders the action of D-alanine:D-alanine ligase (Ddl) and D-alanine racemase (Alr), which are involved in the peptidoglycan biosynthesis [19]. It is a second-line drug used to treat MDR-TB and XDR-TB because of less D-cycloserine-resistant M. tuberculosis is reported [68, 69]. However, it is less potent as compared to that of first-line drugs [69]. A recent comparative genomic analysis revealed that M. bovis bacillus Calmette-Guérin (BCG) containing a nsSNP in the cycA gene (bacterial D-alanine/D-serine/glycine transporter) is more resistant to D-cycloserine as compared to wild-type M. tuberculosis and M. bovis [70]. Additionally, we also identified non-synonymous mutations in ddlA (D-alanine:D-alanine ligase) and alr (D-alanine racemase) (Table 4). The mutations observed in ddlA and alr putatively prevent D-cycloserine from hindering with peptidoglycan biosynthesis. Taken together, mutations of cycA, ddlA and alr in UM 1072388579 are presumably involved in D-cycloserine resistance by blocking of D-cycloserine uptake.
Physiological fitness
Bacterial pathogens pay a physiological cost for the acquisition of resistance mutations. The physiological cost includes reduction of growth rate, less invasiveness or less transmissibility. However, the fitness cost of resistance mutations can be alleviated by fitness-compensatory mutations [71]. In this work, we found that UM 1072388579 carried a nsSNP in rpoC at the position of A734V. rpoC mutations have been reported as compensatory mutations which ameliorate the fitness costs incurred by mutations associated with rifampin resistance in both Salmonella enterica [72] and in M. tuberculosis [73]. These mutations have vital compensatory roles to increase mycobacterial transmissibility [73] and growth rate [74].
Analysis of mutations related cell mobility, cell wall biogenesis pathway and transmembrane efflux pumps
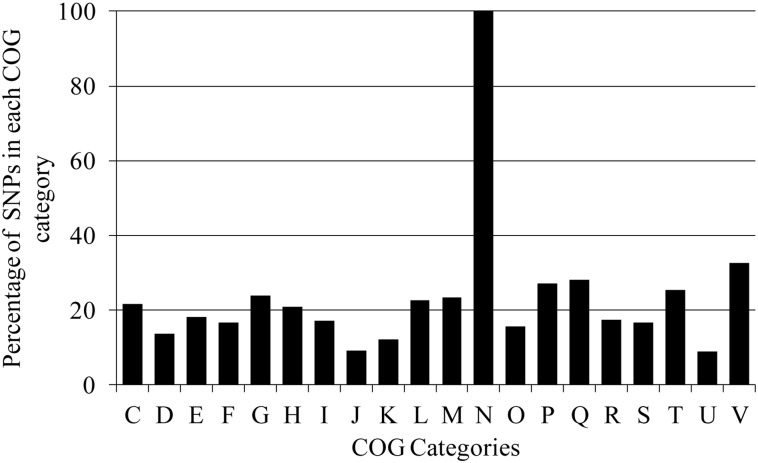
For further functional analysis, all proteins with nsSNPs were classified into various functional groups based on COGs in order to thoroughly search for the gene SNPs that are involved in adaptation, transmission, survival as well as development of acquired drug resistance. The number of gene SNPs in each COG category was normalized with respect to the number of genes in the category and expressed as percentage (%). As reported in [16], UM 1072388579 contains much more missense mutations in proteins belonging to the category N (cell mobility) (Fig 2). Surprisingly, we found that all 65 genes encoding PE and PPE protein families (category N) underwent non-synonymous mutations. These two gene families occupy about 10% of the mycobacterial genome [37]. It has been extensively postulated that these protein families play important roles in bacterial virulence and evasion of antigen-specific host responses through antigenic variation [75].
Fig 2. The distribution of individual genic SNPs into various functional groups based on COGs analysis.
C: Energy production and conversion; D: Cell cycle control, cell division, chromosome partitioning; E: Amino acid transport and metabolism; F: Nucleotide transport and metabolism; G: Carbohydrate transport and metabolism; H: Coenzyme transport and metabolism; I: Lipid transport and metabolism; J: Translation, ribosomal structure and biogenesis; K: Transcription; L: Replication, recombination and repair; M: Cell wall/membrane/envelope biogenesis; N: Cell motility; O: Posttranslational modification, protein turnover, chaperones; P: Inorganic ion transport and metabolism; Q: Secondary metabolites biosynthesis, transport and catabolism; R: General function prediction only; S: Function unknown; T: Signal transduction mechanisms; U: Intracellular trafficking, secretion, and vesicular transport and V: Defense mechanisms.
Unlike most other pathogens, M. tuberculosis acquires drug resistance through the sequential acquisition and accumulation of resistance mutations in the chromosome during sub-optimal drug treatment instead of horizontal gene transfer [19]. Therefore, it is interesting to identify mutations in genes other than well-known drug-resistance genes. The reduction of drug-efflux pump activities and alteration of cell wall permeability provide a “stepping stone” for the development of full-blown antibiotics resistance [76]. In this regard, we mined the literature on the nsSNPs found in UM 1072388579 that are related to the cell wall biogenesis pathway and transmembrane drug-efflux pumps. The unusual complexity of the mycobacterial mycolic acid-containing cell wall renders a permeability barrier, making M. tuberculosis naturally resistant to many drugs [19]. With the knowledge of this intrinsic resistance mechanism, several anti-TB drugs, such as isoniazid [77] and ethambutol [78] were discovered to target the cell wall biogenesis pathways. Accumulating evidence revealed that mutations in the mmpL, pks and fadD genes are probably associated with drug resistance in M. tuberculosis [40, 55, 79]. There are 13 important mmpL genes in the M. tuberculosis genome, which encode membrane proteins that play an essential role in the lipids transport [80]. pks genes encoding the polyketide synthases are involved in the lipopolysaccharide and complex lipids biosynthesis. The co-localization of mmpL with pks and fadD in the M. tuberculosis genome proposes a function for these proteins in the transport of complex lipids [80]. A previous study further proved a functional crosstalk between pks13 and fadD32 enzymes in mycolic acid biosynthesis [81]. Mutations in the mmpL, pks and fadD genes were also suggested to have a compensatory role in drug resistance [40]. In this work, we identified quite a high density of mutations in these gene families (Table 5). However, there is no literature showing how mutations in these protein families can affect drug resistance in M. tuberculosis. We postulate that the mutations in these genes disrupt the cell wall structure and its permeability for anti-TB drugs.
Table 5. Summary of potential mutations associated with cell wall biogenesis pathway, transmembrane efflux pumps and transporters in UM 1072388579.
| Gene name | Mutation | |
|---|---|---|
| Cell wall biogenesis pathway | mmpL2 | R426H |
| mmpL5 | I948V and T794I | |
| mmpL9 | H328P | |
| mmpL12 | S381P | |
| mmpL13a | A276fs | |
| pks3 | X489Y | |
| pks5 | L2061R and L2061R | |
| pks6 | E204A, R1402P and N28fs | |
| pks7 | E814A, L973P and F1489C | |
| pks8 | A1357T | |
| pks12 | P3649A, H2147Q, R1652C, P236fs and V238fs | |
| pks15 | V333A and G488fs | |
| FadD2 | I81M | |
| FadD11.1 | P5fs | |
| FadD13 | T213A | |
| FadD14 | E150G | |
| FadD15 | T100I | |
| FadD21 | L543I | |
| FadD23 | E422Q | |
| FadD29 | W19L | |
| FadD30 | P207L | |
| FadD32 | G227S | |
| FadD34 | S16W | |
| Transmembrane efflux pumps and transporters | Rv0194 | M74T and P1098L |
| Rv1218c | Q243P | |
| Rv1458c | T133A | |
| Rv2688 | P156T |
We then analyzed mutations in transmembrane efflux pumps and transporters which belong to the category V (defense mechanism) as they may be directly associated with the development of XDR phenotype. We found that UM 1072388579 carried several non-synonymous mutations in ATP-binding protein ABC transporters Rv0194 (M74T and P1098L), tetronasin-transport ATP-binding protein ABC transporter Rv1218c (Q243P), antibiotic-transport ATP-binding protein ABC transporter Rv1458c (T133A) and antibiotic-transport ATP-binding protein ABC transporter Rv2688 (P156T) (Table 5). As previously reported [82], overexpression of ATP-binding protein ABC transporters Rv0194 conferred multidrug (ampicillin, vancomycin, novobiocin, and erythromycin) resistance to Mycobacterium smegmatis. Resistant M. tuberculosis strains tend to contain more mutations in the ATP-binding protein ABC transporters Rv0194 compared to that of the sensitive strains [55]. Balganesh and collaborators (2010) demonstrated that the ΔRv1218c mutant of M. tuberculosis showed a significant increase in the inhibitory for ethidium bromide, bisanilopyrimidines (BAPS), pyrroles novobiocins, biarylpiperazines and pyridines compared to that of the wild-type M. tuberculosis [83]. This suggests that Rv1218c plays a role to efflux these compounds from M. tuberculosis. Moreover, the expression level of Rv1218c [84] and Rv1458c [85] are closely related to the formation of MDR and XDR phenotypes. Previous study further proved that Rv2686c-Rv2687c-Rv2688c proteins are active ABC drug transporters which pump out ciprofloxacin from the bacterial cell [86].
Analysis of mutations in intergenic regions
Compared to the SNPs, the role of IGRs in the formation of drug resistance has received little attention. Gene promoters, part of the IGRs, are the regulatory regions that govern the expression of downstream genes [87]. A recent promoter analysis indicated that mutations in the thyA and thyX promoters would lead to the up-regulation of thyA and thyX expression [40]. We predicted 57 putative promoters containing SNPs (S4 Table). Of them, SNP −4 (C/T) in the proximal promoter region of the TetR/acrR gene is of interest. For convenient description hereafter, the nucleotide A at the ATG translational start site of the gene was designated +1, and nucleotides upstream of +1 were assigned negative numbers. AcrR is a transcriptional repressor which negatively regulates the AcrAB operon [88]. In Escherichia coli, mutations in acrR gene significantly increase the expression level of AcrA, a component of the AcrAB multi-drug efflux pump to confer a high-level resistance to fluoroquinolones [89]. Therefore, it is possible that the fluoroquinolones resistance in UM 1072388579 is contributed by the reduced cellular accumulation of fluoroquinolones by the AcrAB multi-drug efflux pump in addition to the alteration of drug targeted DNA gyrase.
We then further examined whether the other 48 M. tuberculosis strains contain this unique promoter SNP. Thorough analysis indicated that this mutation is present in 15 M. tuberculosis strains (including UM 1072388579). All belong to the East Asian lineage (Table 6 and S2 Fig). Among them, nine strains (UM_1072388579, FJ05194, X122, XDR1221, XDR1219, WX1, WX3, CTRI-4 and NZXDR1) exhibit the XDR phenotype. M. tuberculosis 210 and HN878 are drug susceptible strains, while G-12-005, OM-V02_005, R1207 and W-148 are known to be MDR M. tuberculosis strains. Although we cannot derive a conclusion that the presence of the mutation in the TetR/acrR promoter is correlated with drug resistance, the SNP may be an informative marker to recognize candidates of the East Asian lineage.
Table 6. Polymorphism of TetR/acrR promoter in M. tuberculosis strains.
| No | Strain | Nucleotide at −4 allele | Genotype family a |
|---|---|---|---|
| 1 | H37Rv | C | Euro-American lineage 4 strain, T |
| 2 | 43–16836 | C | Indo-Oceanic lineage 1 strain |
| 3 | EAS054 | C | Indo-Oceanic lineage 1 strain |
| 4 | MTB T17 | C | Indo-Oceanic lineage 1 strain |
| 5 | MTB T46 | C | Indo-Oceanic lineage 1 strain |
| 6 | MTB T92 | C | Indo-Oceanic lineage 1 strain |
| 7 | OSDD271 | C | Indo-Oceanic lineage 1 strain, EAI |
| 8 | CAS/NITR204 | C | East African-Indian lineage 3 |
| 9 | GuangZ0019 | C | Euro-American lineage 4 strain, MANU2 |
| 10 | 98-R604 INH-RIF-EM | C | Euro-American lineage 4 strain, LAM family |
| 11 | C | C | Euro-American lineage 4 strain, X |
| 12 | C2 | C | Euro-American lineage 4 strain, LAM family |
| 13 | CDC1551 | C | Euro-American lineage 4 strain, X3 |
| 14 | CTRI-2 | C | Euro-American lineage 4 strain, LAM9 |
| 15 | F11 | C | Euro-American lineage 4 strain, LAM3 |
| 16 | Harlem | C | Euro-American lineage 4 strain, Haarlem |
| 17 | INS_XDR | C | Euro-American lineage 4 strain, LAM |
| 18 | KZN_605 | C | Euro-American lineage 4 strain, LAM4 |
| 19 | KZN_R506 | C | Euro-American lineage 4 strain, LAM4 |
| 20 | KZN_V2475 | C | Euro-American lineage 4 strain, LAM4 |
| 21 | KZN_1435 | C | Euro-American lineage 4 strain, LAM4 |
| 22 | KZN_4207 | C | Euro-American lineage 4 strain, LAM4 |
| 23 | OSDD105 | C | Euro-American lineage 4 strain, T2 |
| 24 | OSDD493 | C | Euro-American lineage 4 strain, Ural |
| 25 | OSDD515 | C | Euro-American lineage 4 strain, Uganda 1 |
| 26 | PanR0201 | C | Euro-American lineage 4 strain, LAM-c2 |
| 27 | PanR0411 | C | Euro-American lineage 4 strain, LAM9-c1 |
| 28 | PanR0610 | C | Euro-American lineage 4 strain, LAM-c2 |
| 29 | PanR0902 | C | Euro-American lineage 4 strain, Haarlem |
| 30 | PanR0906 | C | Euro-American lineage 4 strain, LAM-c3 |
| 31 | MAF CPHL_A | C | Mycobacterium africanum (West Africa 1) lineage 5 |
| 32 | MAF GM041182 | C | Mycobacterium africanum (West Africa 2) lineage 6 |
| 33 | MAF K85 | C | Mycobacterium africanum (West Africa 2) lineage 6 |
| 35 | PRO5 | C | Indo-Oceanic lineage 1 strain |
| 36 | UM 1072388579 | T | East Asia lineage 2 strain, non-Beijing |
| 37 | FJ05194 | T | East Asia lineage 2 strain, non-Beijing |
| 38 | 210 | T | East-Asian lineage 2 strain, Beijing |
| 39 | CTRI-4 | T | East-Asian lineage 2 strain, Beijing-like |
| 40 | G-12-005 | T | East-Asian lineage 2 strain, Beijing |
| 41 | HN878 | T | East-Asian lineage 2 strain, Beijing |
| 42 | NZXDR1 | T | East-Asian lineage 2 strain |
| 43 | OM-V02_005 | T | East-Asian lineage 2 strain, Beijing |
| 44 | R1207 | T | East-Asian lineage 2 strain, Beijing |
| 45 | W-148 | T | East-Asian lineage 2 strain, Beijing |
| 46 | WX1 | T | East-Asian lineage 2 strain, Beijing |
| 47 | WX3 | T | East-Asian lineage 2 strain, Beijing |
| 48 | X122 | T | East-Asian lineage 2 strain, Beijing |
| 49 | XDR1219 | T | East-Asian lineage 2 strain, Beijing |
| 50 | XDR1221 | T | East-Asian lineage 2 strain, Beijing |
a LAM: Latin American Mediterranean; EAI: East African Indian
Conclusions
In this work, we generated an improved UM 1072388579 genome using more advanced mate pair combined sequencing approach. Our analyses revealed that UM 1072388579 belongs to a non-Beijing clade of East Asian lineage 2 which is very close to the Beijing clade. Interestingly, we postulated that UM 1072388579 is an ancient strain, which most likely represents the ancestor of the Beijing clade. However, at this stage of knowledge, its evolutionary origin and history is only partially understood due to the limited genome sequences of such genotype family in Malaysia and other regions of the world. Genetic mutations related to first-line and second-line anti-TB drugs are well described. The presence of classical and uncommon SNPs in genes and IGRs allows our clinical isolate to escape from multiple tested drugs. Other SNPs listed in this study deserve specific attention as they may afford a selective advantage in the presence of antibiotic to adapt, survive and spread to its surrounding population. Further studies are required to confirm the functional importance of these mutations in the formation of XDR phenotype or greater fitness within the population. This report will help to evaluate the geographical and temporal dynamic of the occurrence of XDR-TB in Malaysia as well as other regions of the world. We hope that the faithful execution of UM 1072388579 genome sequence and in-depth analysis of the genome content will serve as a landmark for future TB research.
Supporting Information
A: RNA processing and modification; C: Energy production and conversion; D: Cell cycle control, cell division, chromosome partitioning; E: Amino acid transport and metabolism; F: Nucleotide transport and metabolism; G: Carbohydrate transport and metabolism; H: Coenzyme transport and metabolism; I: Lipid transport and metabolism; J: Translation, ribosomal structure and biogenesis; K: Transcription; L: Replication, recombination and repair; M: Cell wall/membrane/envelope biogenesis; N: Cell motility; O: Posttranslational modification, protein turnover, chaperones; P: Inorganic ion transport and metabolism; Q: Secondary metabolites biosynthesis, transport and catabolism; R: General function prediction only; S: Function unknown; T: Signal transduction mechanisms; U: Intracellular trafficking, secretion, and vesicular transport and V: Defense mechanisms.
(TIF)
The ATG start codon is shown in boldface and assigned as +1, and nucleotides upstream of +1 were denoted as negative numbers. The SNP is highlighted in box.
(PDF)
(PDF)
Genes predicted in UM 1072388579 genome have been annotated by local BLAST similarity searches against NCBI nr, SwissProt and COG databases.
(XLSX)
(XLSX)
The flanking genes of promoters containing SNPs are functional annotated using local BLAST similarity searches against NCBI nr, SwissProt and COG databases.
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files. The genome sequences are available from DDBJ/EMBL/GeneBank with the accession AMXW00000000. The version described in this paper is version AMXW02000000.
Funding Statement
This study was supported by High Impact Research MoE Grant UM.C/625/1/HIR/MOHE/MED/31 (Account no. H-20001-00-E000070) from the Ministry of Education Malaysia. Codon Genomics SB provided support in the form of salaries for authors JSK, KWL, YCT and WYY, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
References
- 1. Jassal M, Bishai WR. Extensively drug-resistant tuberculosis. Lancet Infect Dis. 2009;9(1): 19–30. 10.1016/S1473-3099(08)70260-3 [DOI] [PubMed] [Google Scholar]
- 2. Gandhi NR, Moll A, Sturm AW, Pawinski R, Govender T, Lalloo U, et al. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet. 2006;368(9547): 1575–80. [DOI] [PubMed] [Google Scholar]
- 3. Michael JS, John TJ. Extensively drug-resistant tuberculosis in India: a review. Indian J Med Res. 2012;136(4): 599–604. [PMC free article] [PubMed] [Google Scholar]
- 4. Tang S, Zhang Q, Yu J, Liu Y, Sha W, Sun H, et al. Extensively drug-resistant tuberculosis at a tuberculosis specialist hospital in Shanghai, China: clinical characteristics and treatment outcomes. Scand J Infect Dis. 2011;43(4): 280–5. 10.3109/00365548.2010.548080 [DOI] [PubMed] [Google Scholar]
- 5. Murase Y, Maeda S, Yamada H, Ohkado A, Chikamatsu K, Mizuno K, et al. Clonal expansion of multidrug-resistant and extensively drug-resistant tuberculosis, Japan. Emerg Infect Dis. 2010;16(6): 948–54. 10.3201/eid1606.091844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Migliori GB, Ortmann J, Girardi E, Besozzi G, Lange C, Cirillo DM, et al. Extensively drug-resistant tuberculosis, Italy and Germany. Emerg Infect Dis. 2007;13(5): 780–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kozinska M, Brzostek A, Krawiecka D, Rybczynska M, Zwolska Z, Augustynowicz-Kopec E. [MDR, pre-XDR and XDR drug-resistant tuberculosis in Poland in 2000–2009]. Pneumonol Alergol Pol. 2011;79(4): 278–87. [PubMed] [Google Scholar]
- 8. Casali N, Nikolayevskyy V, Balabanova Y, Ignatyeva O, Kontsevaya I, Harris SR, et al. Microevolution of extensively drug-resistant tuberculosis in Russia. Genome Res. 2012;22(4): 735–45. 10.1101/gr.128678.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ng KP, Yew SM, Chan CL, Chong J, Tang SN, Soo-Hoo TS, et al. Draft Genome Sequence of the First Isolate of Extensively Drug-Resistant (XDR) Mycobacterium tuberculosis in Malaysia. Genome Announc. 2013;1(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bifani PJ, Plikaytis BB, Kapur V, Stockbauer K, Pan X, Lutfey ML, et al. Origin and interstate spread of a New York City multidrug-resistant Mycobacterium tuberculosis clone family. JAMA. 1996;275(6): 452–7. [PubMed] [Google Scholar]
- 11. Cox HS, Sibilia K, Feuerriegel S, Kalon S, Polonsky J, Khamraev AK, et al. Emergence of extensive drug resistance during treatment for multidrug-resistant tuberculosis. N Engl J Med. 2008;359(22): 2398–400. 10.1056/NEJMc0805644 [DOI] [PubMed] [Google Scholar]
- 12. Ioerger TR, Koo S, No EG, Chen X, Larsen MH, Jacobs WR Jr., et al. Genome analysis of multi- and extensively-drug-resistant tuberculosis from KwaZulu-Natal, South Africa. PLoS One. 2009;4(11): e7778 10.1371/journal.pone.0007778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ioerger TR, Feng Y, Chen X, Dobos KM, Victor TC, Streicher EM, et al. The non-clonality of drug resistance in Beijing-genotype isolates of Mycobacterium tuberculosis from the Western Cape of South Africa. BMC Genomics. 2010;11: 670 10.1186/1471-2164-11-670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Karuthedath Vellarikkal S, Vir Singh A, Kumar Singh P, Garg P, Mohan Katoch V, Katoch K, et al. Draft Genome Sequence of an Extensively Drug-Resistant Mycobacterium tuberculosis Clinical Isolate of the Ural Strain OSDD493. Genome Announc. 2013;1(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lin N, Liu Z, Zhou J, Wang S, Fleming J. Draft Genome Sequences of Two Super-XDR Isolates of M. tuberculosis from China. FEMS Microbiol Lett. 2013. [DOI] [PubMed] [Google Scholar]
- 16. Ilina EN, Shitikov EA, Ikryannikova LN, Alekseev DG, Kamashev DE, Malakhova MV, et al. Comparative genomic analysis of Mycobacterium tuberculosis drug resistant strains from Russia. PLoS One. 2013;8(2): e56577 10.1371/journal.pone.0056577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guio H, Tarazona D, Galarza M, Borda V, Curitomay R. Genome analysis of 17 extensively drug-resistant strains reveals new potential mutations for resistance. Genome Announc. 2014;2(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. O'Toole RF, Johari BM, Mac Aogain M, Rogers TR, Bower JE, Basu I, et al. Draft Genome Sequence of the First Isolate of Extensively Drug-Resistant Mycobacterium tuberculosis in New Zealand. Genome Announc. 2014;2(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Almeida Da Silva PE, Palomino JC. Molecular basis and mechanisms of drug resistance in Mycobacterium tuberculosis: classical and new drugs. J Antimicrob Chemother. 2011;66(7): 1417–30. 10.1093/jac/dkr173 [DOI] [PubMed] [Google Scholar]
- 20. Ng KP, Rukumani DV, Chong J, Kaur H. Identification of Mycobacterium species following growth detection with the BACTEC MGIT 960 system by DNA line probe assay. The International Journal of Mycobacteriology. 2014;3(2): 82–7. [DOI] [PubMed] [Google Scholar]
- 21. Somerville W, Thibert L, Schwartzman K, Behr MA. Extraction of Mycobacterium tuberculosis DNA: a question of containment. J Clin Microbiol. 2005;43(6): 2996–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zerbino DR, Birney E. Velvet: algorithms for de novo short read assembly using de Bruijn graphs. Genome Res. 2008;18(5): 821–9. 10.1101/gr.074492.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Boetzer M, Henkel CV, Jansen HJ, Butler D, Pirovano W. Scaffolding pre-assembled contigs using SSPACE. Bioinformatics. 2011;27(4): 578–9. 10.1093/bioinformatics/btq683 [DOI] [PubMed] [Google Scholar]
- 24. Boetzer M, Pirovano W. Toward almost closed genomes with GapFiller. Genome Biol. 2012;13(6): R56 10.1186/gb-2012-13-6-r56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nadalin F, Vezzi F, Policriti A. GapFiller: a de novo assembly approach to fill the gap within paired reads. BMC Bioinformatics. 2012;13 Suppl 14:S8 10.1186/1471-2105-13-S14-S8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lomsadze A, Ter-Hovhannisyan V, Chernoff YO, Borodovsky M. Gene identification in novel eukaryotic genomes by self-training algorithm. Nucleic Acids Res. 2005;33(20): 6494–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lagesen K, Hallin P, Rodland EA, Staerfeldt HH, Rognes T, Ussery DW. RNAmmer: consistent and rapid annotation of ribosomal RNA genes. Nucleic Acids Res. 2007;35(9): 3100–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lowe TM, Eddy SR. tRNAscan-SE: a program for improved detection of transfer RNA genes in genomic sequence. Nucleic Acids Res. 1997;25(5): 955–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rutherford K, Parkhill J, Crook J, Horsnell T, Rice P, Rajandream MA, et al. Artemis: sequence visualization and annotation. Bioinformatics. 2000;16(10): 944–5. [DOI] [PubMed] [Google Scholar]
- 30. Coll F, Mallard K, Preston MD, Bentley S, Parkhill J, McNerney R, et al. SpolPred: rapid and accurate prediction of Mycobacterium tuberculosis spoligotypes from short genomic sequences. Bioinformatics. 2012;28(22): 2991–3. 10.1093/bioinformatics/bts544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brudey K, Driscoll JR, Rigouts L, Prodinger WM, Gori A, Al-Hajoj SA, et al. Mycobacterium tuberculosis complex genetic diversity: mining the fourth international spoligotyping database (SpolDB4) for classification, population genetics and epidemiology. BMC Microbiol. 2006;6: 23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Demay C, Liens B, Burguiere T, Hill V, Couvin D, Millet J, et al. SITVITWEB--a publicly available international multimarker database for studying Mycobacterium tuberculosis genetic diversity and molecular epidemiology. Infect Genet Evol. 2012;12(4): 755–66. 10.1016/j.meegid.2012.02.004 [DOI] [PubMed] [Google Scholar]
- 33. Kurtz S, Phillippy A, Delcher AL, Smoot M, Shumway M, Antonescu C, et al. Versatile and open software for comparing large genomes. Genome Biol. 2004;5(2): R12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38(16): e164 10.1093/nar/gkq603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ronquist F, Teslenko M, van der Mark P, Ayres DL, Darling A, Hohna S, et al. MrBayes 3.2: efficient Bayesian phylogenetic inference and model choice across a large model space. Syst Biol. 2012;61(3): 539–42. 10.1093/sysbio/sys029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Reese MG. Application of a time-delay neural network to promoter annotation in the Drosophila melanogaster genome. Comput Chem. 2001;26(1): 51–6. [DOI] [PubMed] [Google Scholar]
- 37. Cole ST, Brosch R, Parkhill J, Garnier T, Churcher C, Harris D, et al. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature. 1998;393(6685): 537–44. [DOI] [PubMed] [Google Scholar]
- 38. Williams MJ, Kana BD, Mizrahi V. Functional analysis of molybdopterin biosynthesis in mycobacteria identifies a fused molybdopterin synthase in Mycobacterium tuberculosis . J Bacteriol. 2011;193(1): 98–106. 10.1128/JB.00774-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sreevatsan S, Pan X, Stockbauer KE, Connell ND, Kreiswirth BN, Whittam TS, et al. Restricted structural gene polymorphism in the Mycobacterium tuberculosis complex indicates evolutionarily recent global dissemination. Proc Natl Acad Sci U S A. 1997;94(18): 9869–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhang H, Li D, Zhao L, Fleming J, Lin N, Wang T, et al. Genome sequencing of 161 Mycobacterium tuberculosis isolates from China identifies genes and intergenic regions associated with drug resistance. Nat Genet. 2013;45(10): 1255–60. 10.1038/ng.2735 [DOI] [PubMed] [Google Scholar]
- 41. Hasan R, Jabeen K, Ali A, Rafiq Y, Laiq R, Malik B, et al. Extensively drug-resistant tuberculosis, Pakistan. Emerg Infect Dis. 2010;16(9): 1473–5. 10.3201/eid1609.100280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ilina EN, Shitikov EA, Ikryannikova LN, Alekseev DG, Kamashev DE, Malakhova MV, et al. Comparative genomic analysis of w drug resistant strains from Russia. PLoS One. 2013;8(2): e56577 10.1371/journal.pone.0056577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Flores L, Van T, Narayanan S, DeRiemer K, Kato-Maeda M, Gagneux S. Large sequence polymorphisms classify Mycobacterium tuberculosis strains with ancestral spoligotyping patterns. J Clin Microbiol. 2007;45(10): 3393–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wan K, Liu J, Hauck Y, Zhang Y, Zhao X, Liu Z, et al. Investigation on Mycobacterium tuberculosis diversity in China and the origin of the Beijing clade. PLoS One. 2011;6(12): e29190 10.1371/journal.pone.0029190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Comas I, Homolka S, Niemann S, Gagneux S. Genotyping of genetically monomorphic bacteria: DNA sequencing in Mycobacterium tuberculosis highlights the limitations of current methodologies. PLoS One. 2009;4(11): e7815 10.1371/journal.pone.0007815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chuang PC, Chen HY, Jou R. Single-nucleotide polymorphism in the fadD28 gene as a genetic marker for East Asia Lineage Mycobacterium tuberculosis . J Clin Microbiol. 2010;48(11): 4245–7. 10.1128/JCM.00970-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Coll F, McNerney R, Guerra-Assuncao JA, Glynn JR, Perdigao J, Viveiros M, et al. A robust SNP barcode for typing Mycobacterium tuberculosis complex strains. Nat Commun. 2014;5: 4812 10.1038/ncomms5812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lanzas F, Karakousis PC, Sacchettini JC, Ioerger TR. Multidrug-resistant tuberculosis in panama is driven by clonal expansion of a multidrug-resistant Mycobacterium tuberculosis strain related to the KZN extensively drug-resistant M. tuberculosis strain from South Africa. J Clin Microbiol. 2013;51(10): 3277–85. 10.1128/JCM.01122-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Guo H, Seet Q, Denkin S, Parsons L, Zhang Y. Molecular characterization of isoniazid-resistant clinical isolates of Mycobacterium tuberculosis from the USA. J Med Microbiol. 2006;55(Pt 11): 1527–31. [DOI] [PubMed] [Google Scholar]
- 50. Heym B, Zhang Y, Poulet S, Young D, Cole ST. Characterization of the katG gene encoding a catalase-peroxidase required for the isoniazid susceptibility of Mycobacterium tuberculosis . J Bacteriol. 1993;175(13): 4255–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cade CE, Dlouhy AC, Medzihradszky KF, Salas-Castillo SP, Ghiladi RA. Isoniazid-resistance conferring mutations in Mycobacterium tuberculosis KatG: catalase, peroxidase, and INH-NADH adduct formation activities. Protein Sci. 2010;19(3): 458–74. 10.1002/pro.324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sekiguchi J, Miyoshi-Akiyama T, Augustynowicz-Kopec E, Zwolska Z, Kirikae F, Toyota E, et al. Detection of multidrug resistance in Mycobacterium tuberculosis . J Clin Microbiol. 2007;45(1): 179–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. van Doorn HR, Kuijper EJ, van der Ende A, Welten AG, van Soolingen D, de Haas PE, et al. The susceptibility of Mycobacterium tuberculosis to isoniazid and the Arg—>Leu mutation at codon 463 of katG are not associated. J Clin Microbiol. 2001;39(4): 1591–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Brossier F, Veziris N, Truffot-Pernot C, Jarlier V, Sougakoff W. Performance of the genotype MTBDR line probe assay for detection of resistance to rifampin and isoniazid in strains of Mycobacterium tuberculosis with low- and high-level resistance. J Clin Microbiol. 2006;44(10): 3659–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Farhat MR, Shapiro BJ, Kieser KJ, Sultana R, Jacobson KR, Victor TC, et al. Genomic analysis identifies targets of convergent positive selection in drug-resistant Mycobacterium tuberculosis . Nat Genet. 2013;45(10): 1183–9. 10.1038/ng.2747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Billman-Jacobe H, Haites RE, Coppel RL. Characterization of a Mycobacterium smegmatis mutant lacking penicillin binding protein 1. Antimicrob Agents Chemother. 1999;43(12): 3011–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sreevatsan S, Stockbauer KE, Pan X, Kreiswirth BN, Moghazeh SL, Jacobs WR Jr., et al. Ethambutol resistance in Mycobacterium tuberculosis: critical role of embB mutations. Antimicrob Agents Chemother. 1997;41(8): 1677–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Shi R, Zhang J, Otomo K, Zhang G, Sugawara I. Lack of correlation between embB mutation and ethambutol MIC in Mycobacterium tuberculosis clinical isolates from China. Antimicrob Agents Chemother. 2007;51(12): 4515–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Xu C, Kreiswirth BN, Sreevatsan S, Musser JM, Drlica K. Fluoroquinolone resistance associated with specific gyrase mutations in clinical isolates of multidrug-resistant Mycobacterium tuberculosis . J Infect Dis. 1996;174(5): 1127–30. [DOI] [PubMed] [Google Scholar]
- 60. Sreevatsan S, Pan X, Stockbauer KE, Williams DL, Kreiswirth BN, Musser JM. Characterization of rpsL and rrs mutations in streptomycin-resistant Mycobacterium tuberculosis isolates from diverse geographic localities. Antimicrob Agents Chemother. 1996;40(4): 1024–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Okamoto S, Tamaru A, Nakajima C, Nishimura K, Tanaka Y, Tokuyama S, et al. Loss of a conserved 7-methylguanosine modification in 16S rRNA confers low-level streptomycin resistance in bacteria. Mol Microbiol. 2007;63(4): 1096–106. [DOI] [PubMed] [Google Scholar]
- 62. Feuerriegel S, Oberhauser B, George AG, Dafae F, Richter E, Rusch-Gerdes S, et al. Sequence analysis for detection of first-line drug resistance in Mycobacterium tuberculosis strains from a high-incidence setting. BMC Microbiol. 2012;12: 90 10.1186/1471-2180-12-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Spies FS, Ribeiro AW, Ramos DF, Ribeiro MO, Martin A, Palomino JC, et al. Streptomycin resistance and lineage-specific polymorphisms in Mycobacterium tuberculosis gidB gene. J Clin Microbiol. 2011;49(7): 2625–30. 10.1128/JCM.00168-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Verma JS, Gupta Y, Nair D, Manzoor N, Rautela RS, Rai A, et al. Evaluation of gidB alterations responsible for streptomycin resistance in Mycobacterium tuberculosis . J Antimicrob Chemother. 2014;69(11): 2935–41. 10.1093/jac/dku273 [DOI] [PubMed] [Google Scholar]
- 65. Zaunbrecher MA, Sikes RD Jr., Metchock B, Shinnick TM, Posey JE. Overexpression of the chromosomally encoded aminoglycoside acetyltransferase eis confers kanamycin resistance in Mycobacterium tuberculosis . Proc Natl Acad Sci U S A. 2009;106(47): 20004–9. 10.1073/pnas.0907925106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Johansen SK, Maus CE, Plikaytis BB, Douthwaite S. Capreomycin binds across the ribosomal subunit interface using tlyA-encoded 2'-O-methylations in 16S and 23S rRNAs. Mol Cell. 2006;23(2): 173–82. [DOI] [PubMed] [Google Scholar]
- 67. Sowajassatakul A, Prammananan T, Chaiprasert A, Phunpruch S. Molecular characterization of amikacin, kanamycin and capreomycin resistance in M/XDR-TB strains isolated in Thailand. BMC Microbiol. 2014;14: 165 10.1186/1471-2180-14-165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Caminero JA, Sotgiu G, Zumla A, Migliori GB. Best drug treatment for multidrug-resistant and extensively drug-resistant tuberculosis. Lancet Infect Dis. 2010;10(9): 621–9. 10.1016/S1473-3099(10)70139-0 [DOI] [PubMed] [Google Scholar]
- 69. Hong W, Chen L, Xie J. Molecular basis underlying Mycobacterium tuberculosis D-cycloserine resistance. Is there a role for ubiquinone and meraquinone metabolic pathways? Expert Opin Ther Targets. 2014;18(6): 691–701. 10.1517/14728222.2014.902937 [DOI] [PubMed] [Google Scholar]
- 70. Garcia Pelayo MC, Uplekar S, Keniry A, Mendoza Lopez P, Garnier T, Nunez Garcia J, et al. A comprehensive survey of single nucleotide polymorphisms (SNPs) across Mycobacterium bovis strains and M. bovis BCG vaccine strains refines the genealogy and defines a minimal set of SNPs that separate virulent M. bovis strains and M. bovis BCG strains. Infect Immun. 2009;77(5): 2230–8. 10.1128/IAI.01099-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Schulz zur Wiesch P, Engelstadter J, Bonhoeffer S. Compensation of fitness costs and reversibility of antibiotic resistance mutations. Antimicrob Agents Chemother. 2010;54(5): 2085–95. 10.1128/AAC.01460-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Brandis G, Wrande M, Liljas L, Hughes D. Fitness-compensatory mutations in rifampicin-resistant RNA polymerase. Mol Microbiol. 2012;85(1): 142–51. 10.1111/j.1365-2958.2012.08099.x [DOI] [PubMed] [Google Scholar]
- 73. de Vos M, Muller B, Borrell S, Black PA, van Helden PD, Warren RM, et al. Putative compensatory mutations in the rpoC gene of rifampin-resistant Mycobacterium tuberculosis are associated with ongoing transmission. Antimicrob Agents Chemother. 2013;57(2): 827–32. 10.1128/AAC.01541-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Brandis G, Hughes D. Genetic characterization of compensatory evolution in strains carrying rpoB Ser531Leu, the rifampicin resistance mutation most frequently found in clinical isolates. J Antimicrob Chemother. 2013;68(11): 2493–7. 10.1093/jac/dkt224 [DOI] [PubMed] [Google Scholar]
- 75. Sampson SL. Mycobacterial PE/PPE proteins at the host-pathogen interface. Clin Dev Immunol. 2011;2011: 497203 10.1155/2011/497203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Nikaido H. Prevention of drug access to bacterial targets: permeability barriers and active efflux. Science. 1994;264(5157): 382–8. [DOI] [PubMed] [Google Scholar]
- 77. Schroeder EK, de Souza N, Santos DS, Blanchard JS, Basso LA. Drugs that inhibit mycolic acid biosynthesis in Mycobacterium tuberculosis . Curr Pharm Biotechnol. 2002;3(3): 197–225. [DOI] [PubMed] [Google Scholar]
- 78. Birch HL, Alderwick LJ, Bhatt A, Rittmann D, Krumbach K, Singh A, et al. Biosynthesis of mycobacterial arabinogalactan: identification of a novel alpha(1—>3) arabinofuranosyltransferase. Mol Microbiol. 2008;69(5): 1191–206. 10.1111/j.1365-2958.2008.06354.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ioerger TR, O'Malley T, Liao R, Guinn KM, Hickey MJ, Mohaideen N, et al. Identification of new drug targets and resistance mechanisms in Mycobacterium tuberculosis . PLoS One. 2013;8(9): e75245 10.1371/journal.pone.0075245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Domenech P, Reed MB, Barry CE 3rd. Contribution of the Mycobacterium tuberculosis MmpL protein family to virulence and drug resistance. Infect Immun. 2005;73(6): 3492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Gavalda S, Leger M, van der Rest B, Stella A, Bardou F, Montrozier H, et al. The Pks13/FadD32 crosstalk for the biosynthesis of mycolic acids in Mycobacterium tuberculosis . J Biol Chem. 2009;284(29): 19255–64. 10.1074/jbc.M109.006940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Danilchanka O, Mailaender C, Niederweis M. Identification of a novel multidrug efflux pump of Mycobacterium tuberculosis . Antimicrob Agents Chemother. 2008;52(7): 2503–11. 10.1128/AAC.00298-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Balganesh M, Kuruppath S, Marcel N, Sharma S, Nair A, Sharma U. Rv1218c, an ABC transporter of Mycobacterium tuberculosis with implications in drug discovery. Antimicrob Agents Chemother. 2010;54(12): 5167–72. 10.1128/AAC.00610-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Wang K, Pei H, Huang B, Zhu X, Zhang J, Zhou B, et al. The expression of ABC efflux pump, Rv1217c-Rv1218c, and its association with multidrug resistance of Mycobacterium tuberculosis in China. Curr Microbiol. 2013;66(3): 222–6. 10.1007/s00284-012-0215-3 [DOI] [PubMed] [Google Scholar]
- 85. Hao P, Shi-Liang Z, Ju L, Ya-Xin D, Biao H, Xu W, et al. The role of ABC efflux pump, Rv1456c-Rv1457c-Rv1458c, from Mycobacterium tuberculosis clinical isolates in China. Folia Microbiol (Praha). 2011;56(6): 549–53. [DOI] [PubMed] [Google Scholar]
- 86. Pasca MR, Guglierame P, Arcesi F, Bellinzoni M, De Rossi E, Riccardi G. Rv2686c-Rv2687c-Rv2688c, an ABC fluoroquinolone efflux pump in Mycobacterium tuberculosis . Antimicrob Agents Chemother. 2004;48(8): 3175–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Barnard A, Wolfe A, Busby S. Regulation at complex bacterial promoters: how bacteria use different promoter organizations to produce different regulatory outcomes. Curr Opin Microbiol. 2004;7(2): 102–8. [DOI] [PubMed] [Google Scholar]
- 88. Su CC, Rutherford DJ, Yu EW. Characterization of the multidrug efflux regulator AcrR from Escherichia coli . Biochem Biophys Res Commun. 2007;361(1): 85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Wang H, Dzink-Fox JL, Chen M, Levy SB. Genetic characterization of highly fluoroquinolone-resistant clinical Escherichia coli strains from China: role of acrR mutations. Antimicrob Agents Chemother. 2001;45(5): 1515–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A: RNA processing and modification; C: Energy production and conversion; D: Cell cycle control, cell division, chromosome partitioning; E: Amino acid transport and metabolism; F: Nucleotide transport and metabolism; G: Carbohydrate transport and metabolism; H: Coenzyme transport and metabolism; I: Lipid transport and metabolism; J: Translation, ribosomal structure and biogenesis; K: Transcription; L: Replication, recombination and repair; M: Cell wall/membrane/envelope biogenesis; N: Cell motility; O: Posttranslational modification, protein turnover, chaperones; P: Inorganic ion transport and metabolism; Q: Secondary metabolites biosynthesis, transport and catabolism; R: General function prediction only; S: Function unknown; T: Signal transduction mechanisms; U: Intracellular trafficking, secretion, and vesicular transport and V: Defense mechanisms.
(TIF)
The ATG start codon is shown in boldface and assigned as +1, and nucleotides upstream of +1 were denoted as negative numbers. The SNP is highlighted in box.
(PDF)
(PDF)
Genes predicted in UM 1072388579 genome have been annotated by local BLAST similarity searches against NCBI nr, SwissProt and COG databases.
(XLSX)
(XLSX)
The flanking genes of promoters containing SNPs are functional annotated using local BLAST similarity searches against NCBI nr, SwissProt and COG databases.
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files. The genome sequences are available from DDBJ/EMBL/GeneBank with the accession AMXW00000000. The version described in this paper is version AMXW02000000.