Abstract
Studies that investigated the association between socio-economic position (SEP) and obesity in children suggest inconsistent results. The aim of this study is to summarize and quantify the current evidence on SEP and risks of overweight and obesity in children aged 0–15 years. Relevant studies published between 1990 to Sep 4, 2014 were searched in Medline, Web of Science, Embase, and the Cochrane Database of Systematic Reviews. Risk estimates from individual studies were pooled using random-effects models, according to lowest vs the highest SEP category. A total of 62 articles were included in the meta-analysis. The odds of both overweight risk and obesity risk were higher in the children with lowest SEP than in those with highest SEP (OR, 1.10, 95% CI: 1.03–1.17, and OR, 1.41, 95% CI: 1.29–1.55, respectively). Sub-group analyses showed that the inverse relationships between SEP and childhood overweight and obesity were only found in high-income countries and in more economic developed areas. In conclusion, our study suggests that children with lower SEP had higher risks of overweight and obesity, and the increased risks were independent of the income levels of countries.
The prevalence of childhood overweight and obesity has been increasing at an alarming rate throughout the world. A previous study estimated that 23.8% of boys and 22.6% of girls in developed countries and 12.9% of boys and 13.4% of girls in developing countries were overweight or obese in 20131. Overweight and obesity in early life are associated with increased risk of hypertension, heart disease, diabetes mellitus, and sleep disturbances in adulthood2,3. Many factors have been identified to explain the current dramatic global increase in the prevalence of overweight and obesity in children, which include: lack of physical activity, large birth weight, increased television viewing, parental obesity, maternal tobacco smoking during pregnancy, nutritional factors, genetic influence and more4,5,6,7.
There is also a growing body of evidence that suggests that socio-economic position (SEP) is a risk factor for obesity. Family income, living space, parental educational level and car or house ownership were reported to modify children’s behavior relative to energy balance, thus affecting the likelihood of childhood obesity8,9. However, this relationship was inconsistent in different studies. In some studies, lower level of SEP was an independent risk factor of overweight and obesity in children10,11,12, while in other studies, children with higher level of SEP were significantly more likely to be overweight or obese13,14,15.
For the prevention of childhood overweight and obesity, it is crucial to investigate how the diseases are patterned by SEP. To our knowledge, no quantitative review has been undertaken previously to summarize the relationship between SEP and childhood overweight and obesity. We therefore conducted a systematic review and meta-analysis of the evidence for the relation between SEP and risks of overweight and obesity in children aged 0–15 years.
Results
Results of the literature search
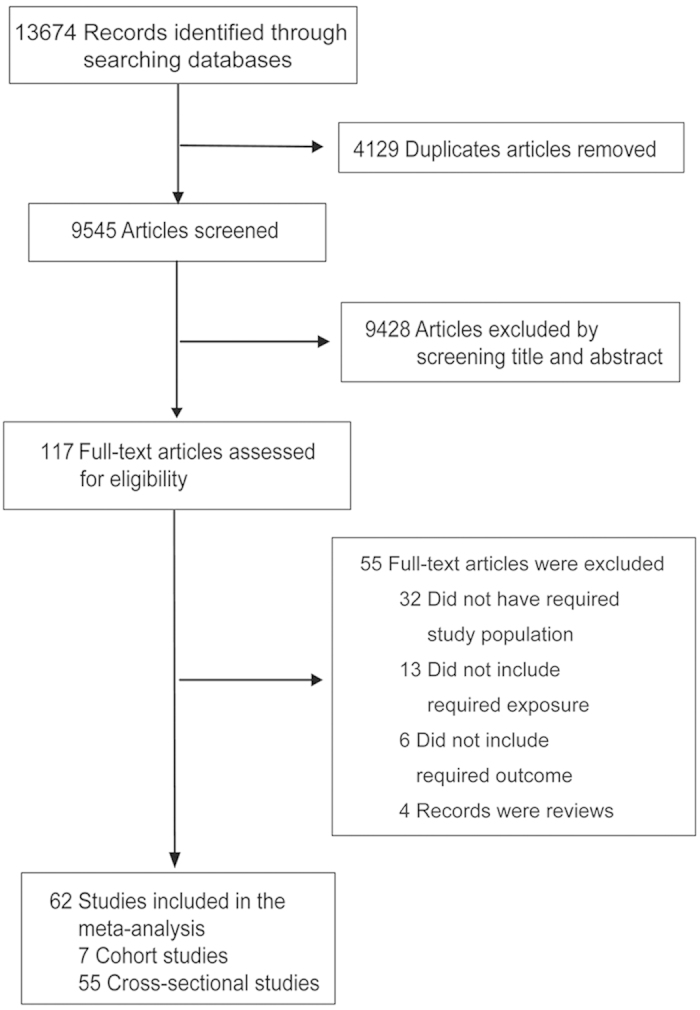
The article selection procedure is shown in Fig. 1. Briefly, after excluding 4129 articles due to overlap between search categories, 9545 articles were screened. 9428 articles were excluded by screening title and abstract, and 117 full-text articles were assessed for eligibility. A total of 62 articles fulfilled the inclusion criteria and were included in the meta-analysis, including 7 cohort studies16,17,18,19,20,21,22 and 55 cross-sectional studies10,11,12,13,14,15,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71, which involved approximately 1,305,217 participants (Table S1). A total of 54 estimates from 26 individual studies were available for assessing the association between SEP and risk of childhood overweight, 55 estimates from 28 individual studies were available for assessing the association between SEP and risk of childhood obesity, and 53 estimates from 29 individual studies were available for assessing the association between SEP and risk of childhood overweight including obesity. The higher number of risk estimates compared with number of articles was due to the fact that some studies conducted more than one individual cohort (in different regions, age groups or sexes) and some studies included more than one measure of SEP. The sum of the numbers of the individual studies in three pooled analyses were more than 62 because some studies reported both overweight and obesity outcomes. The quality assessment of the included studies was presented in detail in the supplementary material (Table S2–S3).
Figure 1. Flowchart for the selection of eligible studies.
Effect of SEP on overweight and obesity in children
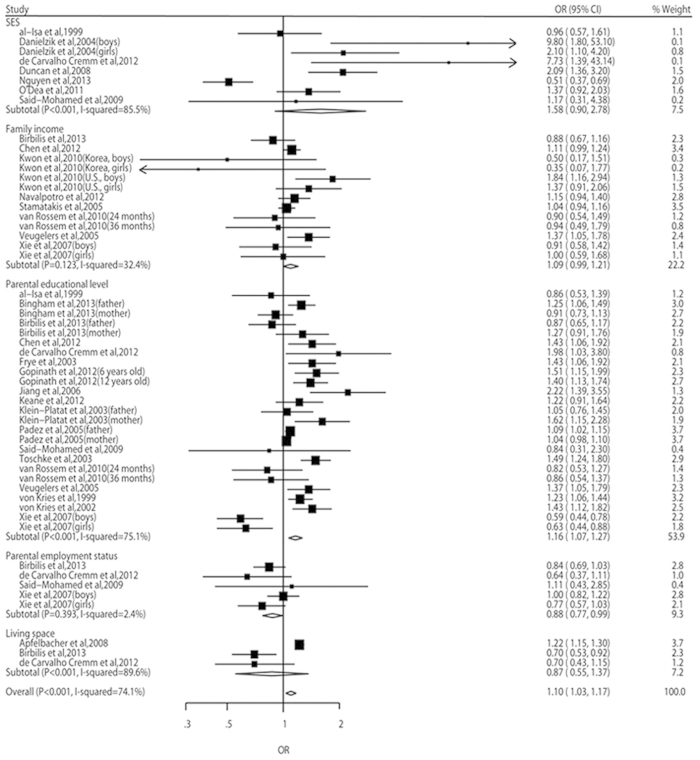
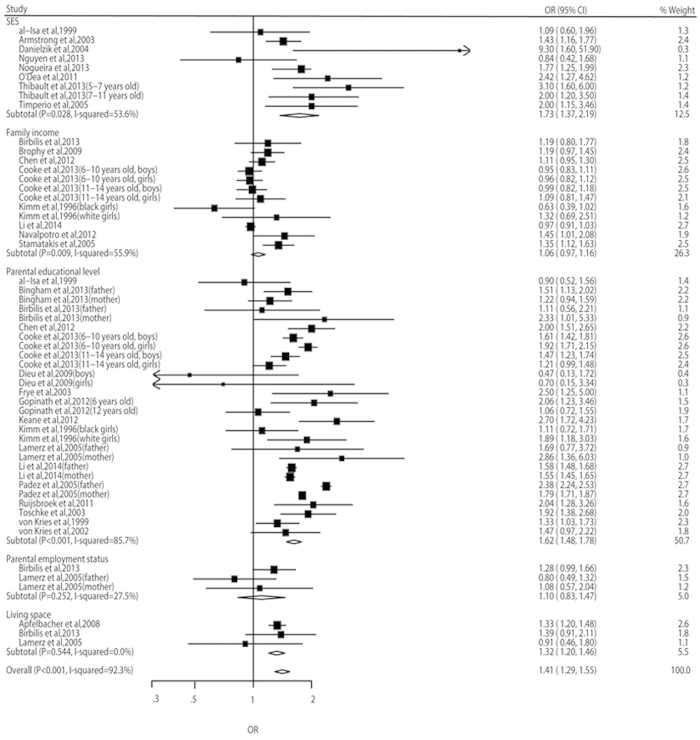
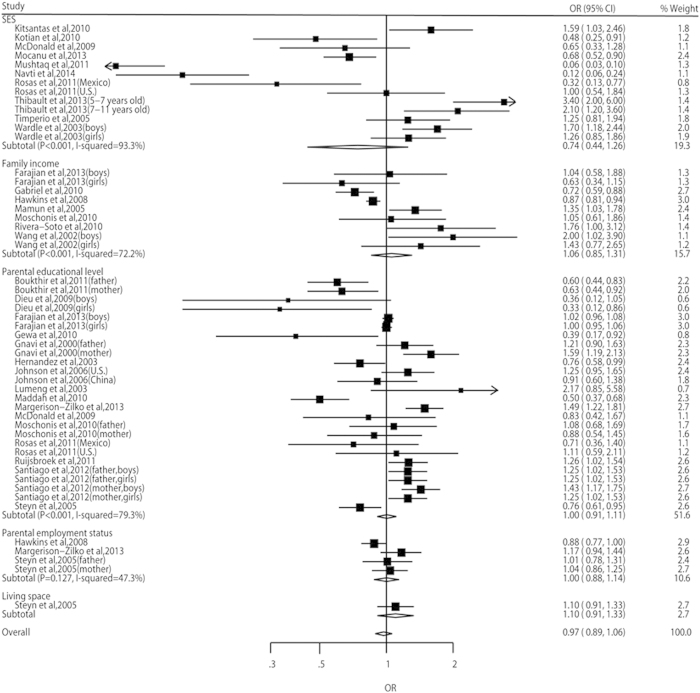
In the meta-analyses, the odds of both overweight risk and obesity risk were higher in the children with lowest SEP than in those with highest SEP (OR, 1.10, 95% CI: 1.03–1.17, and OR, 1.41, 95% CI: 1.29–1.55, respectively) (Figs 2 and 3). However, the risk of overweight including obesity didn’t show statistical significance between different SEP groups (OR, 0.97, 95% CI: 0.89–1.06) (Fig. 4). A significant heterogeneity was observed for all three pooled analyses, i.e. overweight (P = 0.001, I2 = 74.1%), obesity (P < 0.001, I2 = 92.3%) and overweight including obesity (P < 0.001, I2 = 85.2%).
Figure 2. Relative risks and 95% CIs of overweight for the lowest vs highest SEP category in children aged 0–15 years.
Figure 3. Relative risks and 95% CIs of obesity for the lowest vs highest SEP category in children aged 0–15 years.
Figure 4. Relative risks and 95% CIs of overweight including obesity for the lowest vs highest SEP category in children aged 0–15 years.
Subgroup analyses
In the subgroup analyses by income level of countries, children with lowest SEP had a 16% (95% CI: 9%−24%) higher risk of overweight, a 43% (95% CI: 30%−58%) higher risk of obesity and a 23% (95% CI: 13%−33%) higher risk of overweight including obesity in high-income countries. However, in middle-income countries, the risks of overweight and obesity didn’t show significant differences between different SEP groups and children with lowest SEP had a 42% (95% CI: 28%−54%) lower risk of overweight including obesity. Only one study from a low-income country was included (Table 1).When we performed sub-groups analyses for different geographical areas, children with lowest SEP had higher risks of overweight, obesity and overweight including obesity in North America, Europe and Oceania. Especially in Oceania, children with lowest SEP had a 50% higher risk of overweight and a 73% higher risk of obesity (OR, 1.50, 95% CI: 1.29–1.73, and OR, 1.73, 95% CI: 1.15–2.59, respectively). But in Asia/Middle East, Latin America and Africa, the risks of overweight and obesity didn’t show significant differences between different SEP groups and children with lowest SEP had lower risk of overweight including obesity (Table 1). When we performed sub-group analyses for different sexes, only studies included both sexes showed higher risks of overweight and obesity in children with lowest SEP, and this may caused by the fact that there were not enough studies conducted in boys and girls separately (Table 1). In other sub-group analyses such as adjustment, publication year and study design, the increased risks of overweight and obesity persisted in the majority of analyses (Table 1). Moreover, significant heterogeneity was present for the majority of sub-group analyses (Table 1).
Table 1. Sub-group analyses for studies included in the analysis (lowest vs highest SEP category).
| Sub-group analysis | Pooled OR (95% CI), P-value for the heterogeneity Q test, I2 statistics (%), number of estimates in included studies (n) | |||||
|---|---|---|---|---|---|---|
| n | Risk estimates of overweight | n | Risk estimates of obesity | n | Risk estimates of overweight including obesity | |
| Sex | ||||||
| Boys | 6 | 1.03 (0.67–1.57); P < 0.001, I2 = 81.6 | 6 | 1.24 (0.92–1.65); P < 0.001, I2 = 89.4 | 7 | 1.25 (1.01–1.55); P < 0.001, I2 = 77.1 |
| Girls | 6 | 0.96 (0.67–1.39); P = 0.005, I2 = 70.2 | 7 | 1.13 (0.81–1.57); P < 0.001, I2 = 91.2 | 7 | 1.09 (0.91–1.30); P = 0.007, I2 = 66.4 |
| Combined | 42 | 1.13 (1.06–1.21); P < 0.001, I2 = 72.3 | 42 | 1.49 (1.34–1.66); P < 0.001, I2 = 92.5 | 39 | 0.90 (0.79–1.03); P < 0.001, I2 = 86.9 |
| Income | ||||||
| High-income | 37 | 1.16 (1.09–1.24); P < 0.001, I2 = 68.9 | 50 | 1.43 (1.30–1.58); P < 0.001, I2 = 92.7 | 32 | 1.23 (1.13–1.33); P < 0.001, I2 = 76.4 |
| Middle-income | 17 | 0.95 (0.78–1.15); P < 0.001, I2 = 78.6 | 5 | 1.14 (0.74–1.77); P = 0.002, I2 = 76.4 | 20 | 0.58 (0.46–0.72); P < 0.001, I2 = 87.2 |
| Low | 0 | − | 0 | – | 1 | 0.39 (0.17–0.92) |
| Geographical area | ||||||
| North America | 4 | 1.42 (1.21–1.67); P = 0.714, I2 = 0.0 | 12 | 1.22 (1.01–1.47); P < 0.001, I2 = 90.2 | 8 | 1.34 (1.19–1.50); P = 0.471, I2 = 0.0 |
| Europe | 25 | 1.11 (1.04–1.19); P < 0.001, I2 = 70.9 | 32 | 1.53 (1.36–1.73); P < 0.001, I2 = 93.9 | 21 | 1.14 (1.04–1.25); P < 0.001, I2 = 80.9 |
| Oceania | 4 | 1.50 (1.29–1.73); P = 0.407, I2 = 0.0 | 4 | 1.73 (1.15–2.59); P = 0.056, I2 = 60.3 | 4 | 1.39 (1.13–1.70); P = 0.703, I2 = 0.0 |
| Asia/Middle East | 14 | 0.89 (0.73–1.08); P < 0.001, I2 = 79.6 | 7 | 1.12 (0.81–1.54); P = 0.006, I2 = 67.2 | 6 | 0.35 (0.16–0.74); P < 0.001, I2 = 90.9 |
| Latin America | 4 | 1.23 (0.58–2.60); P = 0.003, I2 = 78.6 | 0 | – | 6 | 0.72 (0.62–0.83); P = 0.609, I2 = 0.0 |
| Africa | 3 | 1.01 (0.55–1.86); P = 0.898, I2 = 0.0 | 0 | – | 8 | 0.68 (0.51–0.91); P < 0.001, I2 = 87.3 |
| Adjustment | ||||||
| Minimally adjusted | 28 | 1.10 (1.01–1.18); P < 0.001, I2 = 76.9 | 34 | 1.42 (1.27–1.60); P < 0.001, I2 = 91.8 | 31 | 0.87 (0.73–1.04); P < 0.001, I2 = 87.3 |
| Maximally adjusted | 26 | 1.11 (0.97–1.27); P < 0.001, I2 = 71.5 | 21 | 1.39 (1.19–1.62); P < 0.001, I2 = 89.8 | 22 | 1.02 (0.93–1.13); P < 0.001, I2 = 81.6 |
| Publication year | ||||||
| < 2010s | 27 | 1.15 (1.06–1.25); P < 0.001, I2 = 76.1 | 25 | 1.41 (1.22–1.62); P < 0.001, I2 = 88.6 | 22 | 1.06 (0.94–1.19); P < 0.001, I2 = 71.2 |
| ≥2010s | 27 | 1.04 (0.93–1.17); P < 0.001, I2 = 72.2 | 30 | 1.41 (1.27–1.58); P < 0.001, I2 = 90.4 | 31 | 0.90 (0.79–1.03); P < 0.001, I2 = 89.1 |
| Design | ||||||
| Cohort | 4 | 0.87 (0.68–1.11); P = 0.986, I2 = 0.0 | 4 | 1.43 (1.07–1.91); P < 0.001, I2 = 98.0 | 8 | 1.19 (0.98–1.44); P < 0.001, I2 = 86.4 |
| Cross-sectional | 50 | 1.11 (1.04–1.19); P < 0.001, I2 = 75.6 | 51 | 1.41 (1.28–1.56); P < 0.001, I2 = 89.1 | 45 | 0.92 (0.83–1.02); P < 0.001, I2 = 85.4 |
Publication bias
Visual assessment of funnel plots (Figure S1) showed that the studies were distributed fairly symmetrically about the combined effect size, which suggests little publication bias. Egger’s regression test and Begg-Mazumdar test also showed that there was no potential publication bias when pooling the results of overweight (Egger’s regression test (p = 0.997), and Begg-Mazumdar test (p = 0.788)), obesity (Egger’s regression test (p = 0.181), and Begg-Mazumdar test (p = 0.141)) and overweight including obesity (Egger’s regression test (p = 0.619), and Begg-Mazumdar test (p = 0.056)).
Discussion
SEP has been described as inversely related to obesity in adulthood72,73,74. Our findings further suggest that low SEP is associated with a 10% higher risk of overweight and a 41% higher risk of obesity in children aged 0–15 years. However, according to the sub-group analyses by income level of countries, this relationship was only found in high-income countries. In addition, sub-group analyses by geographical areas showed that children with low SEP had higher risks of overweight and obesity only in North America, Europe and Oceania, and the included studies conducted in these areas were all from economic developed countries with high income level. Thus, we concluded that the increased risks were independent of the income levels of countries. Previous studies indicated that overweight and obesity tended to affect more people from a low socio-economic background in developed countries rather than in developing economies75,76,77. This relationship has been further confirmed in children in our quantitative analyses. Higher risks of overweight and obesity in children with lower SEP in developed countries may be related to less access to healthy food and to safe exercise, less interest in weight control, cultural standards of physical effectiveness, and discrimination against socioeconomic advancement75,78, and insufficient food supply is rare even in families with low SEP. However, situations were different in developing countries and less economic developed areas, where malnutrition and opulence co-exist, food availability remains a daily challenge in populations with low SEP and overweight is subsequently perceived as a sign of weath77. These factors may explain why increased risks of childhood overweight and obesity associated with lower SEP were only found in high-income countries and in more economic developed areas.
The pooled analysis found that the risk of overweight including obesity didn’t show statistical significance between different SEP groups. This may be explained by the fact that this pooled analysis involved more studies from middle-income countries and one study from a low-income country, and it is possible that including data on SEP and overweight including obesity from these countries would have changed the picture. However, the sub-group analyses showed that children with low SEP also had a higher risk of overweight including obesity in high-income countries and in more economic developed areas, which was consistent with the overweight and obesity outcomes. Low SEP was even a protective factor for overweight including obesity in middle-income and low-income countries, and also in less economic developed areas.
In adults, the inverse relationship between SEP and obesity was reported to be more pronounced in women than in men75,79,80. However, in our sub-group analyses by sex, the risks of overweight and obesity didn’t show significant differences between SEP groups for both boys and girls, and only boys with low SEP showed a higher risk of overweight including obesity. The inconsistent results for children and adults may due to the fact that children and adults have different patterns on obesity risk classified by SEP, and may also due to the limited studies included in our analyses. Further studies are needed to identify the relationship of SEP and the risks of overweight and obesity for boys and girls separately.
Parental educational level was the most frequently used method as measure of SEP among the included studies. The subtotal point estimates of overweight and obesity risks patterned by parental educational level were greater than other subtotal and overall point estimates. This means that parental educational level was more consistently inversely associated with childhood overweight and obesity than other indicators. This conclusion was also supported by a previous review8. As an important socio-economic indicator, parental educational level influences the family’s knowledge and beliefs, and these are considered important for healthy lifestyles and the development of overweight and obesity. However, SEP is a multifactor construct, and parental educational level does not entirely capture the material and financial aspects of socio-economic status. The literature reported on a range of different indicators (e.g. income, educational levels and occupation) as being suitable measures of SEP81. Therefore, we included SES, family income, parental educational level, parental employment status and living space as a comprehensive measure of SEP in our meta-analyses.
Some mechanisms may explain the higher risks of overweight and obesity in children with low SEP. Children from lower socio-economic strata may have diets rich in low cost energy dense food82,83, participate less in physical activity or sports84, and have lower awareness of weight control85. On the basis of our findings, we advocate that development programmes should be an essential component of overweight and obesity control in children. Public health interventions aimed at relieving economic hardship may reduce the risks of childhood overweight and obesity, especially in the developed countries. Future research should provide more information on the mechanisms of how lower SEP may influence childhood obesity and on the effectiveness of specific public health interventions to combat obesity in children.
The strengths of this meta-analysis are that we reviewed and included a wide range of studies to make a quantitative assessment on SEP and risks of childhood overweight and obesity, as the literature diverges on whether low SEP is a risk factor of overweight and obesity in children, and the pooled results were more precise with more narrow confidence intervals due to the larger sample size, compared with each individual study.
A major limitation of our study is that there were potential heterogeneities in majority of the analyses, and although we did random-effects and sub-group analyses, these are unlikely to have fully accounted for heterogeneity. Another important limitation is that the definitions of overweight and obesity and the classification of SEP may be different across studies, and this may be another explanation of heterogeneity existed among the studies. Overweight and obesity may be defined differently according to anthropometric measurements in different countries as different populations may have different optimal cutoff points in determining overweight and obesity. The measures of SEP such as parental educational level and family income may vary significantly between countries due to differences in country educational and economies systems. However, the SEP groups were divided into two extreme categories, the lowest and the highest, therefore, we assume that we have captured the sense of SEP, irrespective of time and site86. In addition, some included studies didn’t make adjustment for other factors or only make adjustment for a few important factors, thus, the risk of overweight or obesity in these studies may be contributed to other factors. In this study, we used SES, family income, parental educational level, parental employment status and living space as measures of SEP. Other indicators such as ownership of assets and neighbourhood environments were also measures of SEP. However, this study was unable to select more SEP indicators for further analysis due to the limitation of the datasets.
In conclusion, this first systematic review and meta-analysis suggests that children with lower SEP had higher risks of overweight and obesity, and the increased risks were independent of the income levels of countries.
Methods
Search strategy and eligibility criteria
We followed the guidelines published by the Meta-analysis of Observational Studies in Epidemiology (MOOSE) group to complete the meta-analysis (Table S4)87. To identify eligible articles published in English-speaking peer-reviewed journals, we searched Medline, Web of Science, Embase, and the Cochrane Database of Systematic Reviews (1990 to Sep 4, 2014). We selected synonymous terms and used these to develop the search strategy (Panel S1). In addition, we also manually reviewed the references of all retrieved articles and recent reviews to identify relevant studies. We included studies after 1990, since we sought to examine evidence from the period most applicable to the present status of overweight and obesity control. The search strategy was not limited by study design.
The eligible studies should meet the following inclusion criteria: the study population consisted of children aged 0–15 years; the association between SEP and overweight/obesity was assessed; presented risk estimates with confidence intervals or sufficient information to calculated these; and used socio-economic status (SES), family income, parental educational level, parental employment status or living space as individual measures of SEP. Cross-sectional, cohort, and case-control studies were all included in the analysis. Only studies clearly defined overweight or obesity using a recognized standard were included, and studies only reported the body mass index (BMI) classification were excluded from analysis.
Data extraction
Two investigators (S.W. and Y.D.) independently extracted the following data from each publication: author, country, study design, sample size, age, SEP measure, outcome (overweight or obesity or overweight including obesity), number with overweight or obesity in study, risk estimates with 95% CIs, and factors adjusted for. Countries were classified according to geographical area (North America, Europe, Oceania, Asia/Middle East, Latin America or Africa) and income category according to the World Bank definition (high-income, upper-middle-income, lower-middle-income or low-income country). We extracted estimates for boys and girls separately when possible. If a study reported risk estimates with more than one measure of SEP, each estimate was extracted separately. We included the most adjusted estimate when a study reported more than one risk estimate. The quality of each study was assessed by two investigators (F.W. and J.H.), using methods recommended by Wells and colleagues88.
Statistical analysis
We used odds ratios (ORs) as summary estimates throughout the procedure. We extracted the lowest vs the highest SEP category from each study, using highest SEP as the reference group. The measures of different SEP groups included lowest vs highest SES, lowest vs highest family income, lowest vs highest parental educational level, none vs any of parental employment, and lowest vs highest living space. If presented in a reverse order, we back-calculated the point estimate and 95% CIs. The log ORs from the individual studies and corresponding standard error (SE; calculated from the confidence limits) were used to perform the analysis86.
A fixed effects model was used to estimate the pooled ORs and 95% CIs if there was no evidence of heterogeneity; otherwise, a random effect model was used. The Q-statistic and I-squared (I2) statistic were used to explore the heterogeneity among studies. For Q-statistic, we considered P < 0.1 as representative of statistically significant heterogeneity. For I2 statistic, large I2 (>50%) suggests substantial heterogeneity among studies. Subgroup analyses were conducted by stratifying the original data sets by the above mentioned study-level factors. Publication bias was visually assessed by funnel plots. Egger’s regression test89 and Begg-Mazumdar test90 were performed to further assess publication bias. Statistical analyses were conducted using Stata Version 12.0 software (Stata Corp, College Station, TX).
Additional Information
How to cite this article: Wu, S. et al. Socio-economic position as an intervention against overweight and obesity in children: a systematic review and meta-analysis. Sci. Rep. 5, 11354; doi: 10.1038/srep11354 (2015).
Supplementary Material
Footnotes
Author Contributions P.M. and J.H. conceived of the study. S.W., Y.D., F.W., and R.L. developed the study design and the outline of the report. S.W., Y.D. and F.W. searched the literature, did the meta-analysis, and prepared the first draft of the report. F.W. and P.M assessed the quality of included studies. Y.H. provided advice on the systematic review and meta-analysis. All authors reviewed and supported the final version of the report.
References
- Ng M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 384, 766–781 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz W. H. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 101, 518–525 (1998). [PubMed] [Google Scholar]
- Freedman D. S. Clustering of coronary heart disease risk factors among obese children. J Pediatr Endocrinol Metab. 15, 1099–1108 (2002). [DOI] [PubMed] [Google Scholar]
- Bammann K. et al. Socioeconomic factors and childhood overweight in Europe: results from the multi-centre IDEFICS study. Pediatr Obes. 8, 1–12 (2013). [DOI] [PubMed] [Google Scholar]
- Crespo C. J. et al. Television watching, energy intake, and obesity in US children: results from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 155, 360–365 (2001). [DOI] [PubMed] [Google Scholar]
- Weng S. F., Redsell S. A., Swift J. A., Yang M. & Glazebrook C. P. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch Dis Child. 97, 1019–1026 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle J., Carnell S., Haworth C. M. & Plomin R. Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am J Clin Nutr. 87, 398–404 (2008). [DOI] [PubMed] [Google Scholar]
- Shrewsbury V. & Wardle J. Socioeconomic status and adiposity in childhood: a systematic review of cross-sectional studies 1990-2005. Obesity (Silver Spring). 16, 275–284 (2008). [DOI] [PubMed] [Google Scholar]
- Manios Y. et al. Prevalence of obesity in preschool Greek children, in relation to parental characteristics and region of residence. BMC Public Health. 7, 178 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielzik S., Czerwinski-Mast M., Langnase K., Dilba B. & Muller M. J. Parental overweight, socioeconomic status and high birth weight are the major determinants of overweight and obesity in 5-7 y-old children: baseline data of the Kiel Obesity Prevention Study (KOPS). Int J Obes Relat Metab Disord. 28, 1494–1502 (2004). [DOI] [PubMed] [Google Scholar]
- Thibault H. et al. Prevalence and factors associated with overweight and obesity in French primary-school children. Public Health Nutr. 16, 193–201 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitsantas P. & Gaffney K. F. Risk profiles for overweight/obesity among preschoolers. Early Hum Dev. 86, 563–568 (2010). [DOI] [PubMed] [Google Scholar]
- Navti L. K., Ferrari U., Tange E., Bechtold-Dalla Pozza S. & Parhofer K. G. Contribution of socioeconomic status, stature and birth weight to obesity in Sub-Saharan Africa: cross-sectional data from primary school-age children in Cameroon. BMC Public Health. 14, 320 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen P. V., Hong T. K., Hoang T., Nguyen D. T. & Robert A. R. High prevalence of overweight among adolescents in Ho Chi Minh City, Vietnam. BMC Public Health. 13, 141 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotian M. S., S G. K. & Kotian S. S. Prevalence and determinants of overweight and obesity among adolescent school children of South karnataka, India. Indian J Community Med. 35, 176–178 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins S. S., Cole T. J. & Law C. Maternal employment and early childhood overweight: findings from the UK Millennium Cohort Study. Int J Obes (Lond). 32, 30–38 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Memarian E., Sundquist J., Zoller B. & Sundquist K. Neighbourhood deprivation, individual-level familial and socio-demographic factors and diagnosed childhood obesity: a nationwide multilevel study from sweden. Obes Facts. 7, 253–263 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumeng J. C., Gannon K., Cabral H. J., Frank D. A. & Zuckerman B. Association between clinically meaningful behavior problems and overweight in children. Pediatrics. 112, 1138–1145 (2003). [DOI] [PubMed] [Google Scholar]
- Margerison-Zilko C. E. & Cubbin C. Dynamic poverty experiences and development of overweight in a prospective cohort of US children aged 4-14 years. Obesity (Silver Spring). 21, 1438–1445 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruijsbroek A. et al. The development of socio-economic health differences in childhood: results of the Dutch longitudinal PIAMA birth cohort. BMC Public Health. 11, 225 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rossem L. et al. Socioeconomic status is not inversely associated with overweight in preschool children. J Pediatr. 157, 929-935 e921 (2010). [DOI] [PubMed] [Google Scholar]
- Wardle J. et al. Socioeconomic disparities in cancer-risk behaviors in adolescence: baseline results from the Health and Behaviour in Teenagers Study (HABITS). Prev Med. 36, 721–730 (2003). [DOI] [PubMed] [Google Scholar]
- al-Isa A. N. & Moussa M. A. Factors associated with overweight and obesity among Kuwaiti kindergarten children aged 3-5 years. Nutr Health. 13, 125–139 (1999). [DOI] [PubMed] [Google Scholar]
- Apfelbacher C. J. et al. Predictors of overweight and obesity in five to seven-year-old children in Germany: results from cross-sectional studies. BMC Public Health. 8, 171 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong J., Dorosty A. R., Reilly J. J. & Emmett P. M. Coexistence of social inequalities in undernutrition and obesity in preschool children: population based cross sectional study. Arch Dis Child. 88, 671–675 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingham D. D. et al. Socio-demographic and behavioral risk factors associated with the high prevalence of overweight and obesity in Portuguese children. Am J Hum Biol. 25, 733–742 (2013). [DOI] [PubMed] [Google Scholar]
- Birbilis M., Moschonis G., Mougios V. & Manios Y. Obesity in adolescence is associated with perinatal risk factors, parental BMI and sociodemographic characteristics. Eur J Clin Nutr. 67, 115–121 (2013). [DOI] [PubMed] [Google Scholar]
- Boukthir S. et al. Prevalence and risk factors of overweight and obesity in elementary schoolchildren in the metropolitan region of Tunis, Tunisia. Tunis Med. 89, 50–54 (2011). [PubMed] [Google Scholar]
- Brophy S. et al. Risk factors for childhood obesity at age 5: analysis of the millennium cohort study. BMC Public Health. 9, 467 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y. C. et al. Environmental factors associated with overweight and obesity in taiwanese children. Paediatr Perinat Epidemiol. 26, 561–571 (2012). [DOI] [PubMed] [Google Scholar]
- Cooke M. J., Wilk P., Paul K. W. & Gonneville S. L. Predictors of obesity among Metis children: socio-economic, behavioural and cultural factors. Can J Public Health. 104, e298–303 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Carvalho Cremm E. et al. Factors associated with overweight in children living in the neighbourhoods of an urban area of Brazil. Public Health Nutr. 15, 1056–1064 (2012). [DOI] [PubMed] [Google Scholar]
- Dieu H. T., Dibley M. J., Sibbritt D. W. & Hanh T. T. Trends in overweight and obesity in pre-school children in urban areas of Ho Chi Minh City, Vietnam, from 2002 to 2005. Public Health Nutr. 12, 702–709 (2009). [DOI] [PubMed] [Google Scholar]
- Duncan J. S., Schofield G., Duncan E. K. & Rush E. C. Risk factors for excess body fatness in New Zealand children. Asia Pac J Clin Nutr. 17, 138–147 (2008). [PubMed] [Google Scholar]
- Farajian P. et al. Socio-economic and demographic determinants of childhood obesity prevalence in Greece: the GRECO (Greek Childhood Obesity) study. Public Health Nutr. 16, 240–247 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye C. & Heinrich J. Trends and predictors of overweight and obesity in East German children. Int J Obes Relat Metab Disord. 27, 963–969 (2003). [DOI] [PubMed] [Google Scholar]
- Gabriel C. G. et al. Overweight and obesity related factors in schoolchildren in Santa Catarina State, Brazil. Arch Latinoam Nutr. 60, 332–339 (2010). [PubMed] [Google Scholar]
- Gewa C. A. Childhood overweight and obesity among Kenyan pre-school children: association with maternal and early child nutritional factors. Public Health Nutr. 13, 496–503 (2010). [DOI] [PubMed] [Google Scholar]
- Gnavi R. et al. Socioeconomic status, overweight and obesity in prepuberal children: a study in an area of Northern Italy. Eur J Epidemiol. 16, 797–803 (2000). [DOI] [PubMed] [Google Scholar]
- Gopinath B., Baur L. A., Burlutsky G., Robaei D. & Mitchell P. Socio-economic, familial and perinatal factors associated with obesity in Sydney schoolchildren. J Paediatr Child Health. 48, 44–51 (2012). [DOI] [PubMed] [Google Scholar]
- Hernandez B. et al. Factors associated with overweight and obesity in Mexican school-age children: results from the National Nutrition Survey 1999. Salud Publica Mex. 45 Suppl 4, S551–557 (2003). [DOI] [PubMed] [Google Scholar]
- Jiang J. et al. Risk factors for overweight in 2- to 6-year-old children in Beijing, China. Int J Pediatr Obes. 1, 103–108 (2006). [DOI] [PubMed] [Google Scholar]
- Johnson C. A. et al. Socio-demographic and cultural comparison of overweight and obesity risk and prevalence in adolescents in Southern California and Wuhan, China. J Adolesc Health. 39, 925 e921–928 (2006). [DOI] [PubMed] [Google Scholar]
- Keane E., Layte R., Harrington J., Kearney P. M. & Perry I. J. Measured parental weight status and familial socio-economic status correlates with childhood overweight and obesity at age 9. PLoS One. 7, e43503 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimm S. Y. et al. Race, socioeconomic status, and obesity in 9- to 10-year-old girls: the NHLBI Growth and Health Study. Ann Epidemiol. 6, 266–275 (1996). [DOI] [PubMed] [Google Scholar]
- Klein-Platat C. et al. Prevalence and sociodemographic determinants of overweight in young French adolescents. Diabetes Metab Res Rev. 19, 153–158 (2003). [DOI] [PubMed] [Google Scholar]
- Kwon Y., Oh S., Park S. & Park Y. Association between household income and overweight of Korean and American children: trends and differences. Nutr Res. 30, 470–476 (2010). [DOI] [PubMed] [Google Scholar]
- Lamerz A. et al. Social class, parental education, and obesity prevalence in a study of six-year-old children in Germany. Int J Obes (Lond). 29, 373–380 (2005). [DOI] [PubMed] [Google Scholar]
- Maddah M. & Nikooyeh B. Factors associated with overweight in children in Rasht, Iran: gender, maternal education, skipping breakfast and parental obesity. Public Health Nutr. 13, 196–200 (2010). [DOI] [PubMed] [Google Scholar]
- Mamun A. A., Lawlor D. A., O’Callaghan M. J., Williams G. M. & Najman J. M. Positive maternal attitude to the family eating together decreases the risk of adolescent overweight. Obes Res. 13, 1422–1430 (2005). [DOI] [PubMed] [Google Scholar]
- McDonald C. M., Baylin A., Arsenault J. E., Mora-Plazas M. & Villamor E. Overweight is more prevalent than stunting and is associated with socioeconomic status, maternal obesity, and a snacking dietary pattern in school children from Bogota, Colombia. J Nutr. 139, 370–376 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mocanu V. Prevalence of overweight and obesity in urban elementary school children in northeastern Romania: its relationship with socioeconomic status and associated dietary and lifestyle factors. Biomed Res Int. 2013, 537451 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moschonis G. et al. Social, economic and demographic correlates of overweight and obesity in primary-school children: preliminary data from the Healthy Growth Study. Public Health Nutr. 13, 1693–1700 (2010). [DOI] [PubMed] [Google Scholar]
- Mushtaq M. U. et al. Prevalence and socioeconomic correlates of overweight and obesity among Pakistani primary school children. BMC Public Health. 11, 724 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navalpotro L. et al. Area-based socioeconomic environment, obesity risk behaviours, area facilities and childhood overweight and obesity: socioeconomic environment and childhood overweight. Prev Med. 55, 102–107 (2012). [DOI] [PubMed] [Google Scholar]
- Nogueira H. et al. The associations of SES, obesity, sport activity, and perceived neighborhood environments: is there a model of environmental injustice penalizing Portuguese children? Am J Hum Biol. 25, 434–436 (2013). [DOI] [PubMed] [Google Scholar]
- O’Dea J. A., Nguyen Hoang T. D. & Dibley M. J. Plateau in obesity and overweight in a cross sectional study of low, middle and high socioeconomic status schoolchildren between 2004 and 2009. Int J Public Health. 56, 663–667 (2011). [DOI] [PubMed] [Google Scholar]
- Padez C., Mourao I., Moreira P. & Rosado V. Prevalence and risk factors for overweight and obesity in Portuguese children. Acta Paediatr. 94, 1550–1557 (2005). [DOI] [PubMed] [Google Scholar]
- Rivera-Soto W. T., Rodriguez-Figueroa L. & Calderon G. Prevalence of childhood obesity in a representative sample of elementary school children in Puerto Rico by socio-demographic characteristics, 2008. P R Health Sci J. 29, 357–363 (2010). [PubMed] [Google Scholar]
- Rosas L. G. et al. Factors associated with overweight and obesity among children of Mexican descent: results of a binational study. J Immigr Minor Health. 13, 169–180 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Said-Mohamed R., Allirot X., Sobgui M. & Pasquet P. Determinants of overweight associated with stunting in preschool children of Yaounde, Cameroon. Ann Hum Biol. 36, 146–161 (2009). [DOI] [PubMed] [Google Scholar]
- Santiago S., Zazpe I., Cuervo M. & Martinez J. A. Perinatal and parental determinants of childhood overweight in 6-12 years old children. Nutr Hosp. 27, 599–605 (2012). [DOI] [PubMed] [Google Scholar]
- Stamatakis E., Primatesta P., Chinn S., Rona R. & Falascheti E. Overweight and obesity trends from 1974 to 2003 in English children: what is the role of socioeconomic factors? Arch Dis Child. 90, 999–1004 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steyn N. P., Labadarios D., Maunder E., Nel J. & Lombard C. Secondary anthropometric data analysis of the National Food Consumption Survey in South Africa: the double burden. Nutrition. 21, 4–13 (2005). [DOI] [PubMed] [Google Scholar]
- Timperio A., Salmon J., Telford A. & Crawford D. Perceptions of local neighbourhood environments and their relationship to childhood overweight and obesity. Int J Obes (Lond). 29, 170–175 (2005). [DOI] [PubMed] [Google Scholar]
- Toschke A. M., Montgomery S. M., Pfeiffer U. & von Kries R. Early intrauterine exposure to tobacco-inhaled products and obesity. Am J Epidemiol. 158, 1068–1074 (2003). [DOI] [PubMed] [Google Scholar]
- Veugelers P. J. & Fitzgerald A. L. Prevalence of and risk factors for childhood overweight and obesity. CMAJ. 173, 607–613 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Kries R. et al. Breast feeding and obesity: cross sectional study. BMJ. 319, 147–150 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Kries R., Toschke A. M., Koletzko B. & Slikker W. Jr. Maternal smoking during pregnancy and childhood obesity. Am J Epidemiol. 156, 954–961 (2002). [DOI] [PubMed] [Google Scholar]
- Wang Z., Patterson C. M. & Hills A. P. Association between overweight or obesity and household income and parental body mass index in Australian youth: analysis of the Australian National Nutrition Survey, 1995. Asia Pac J Clin Nutr. 11, 200–205 (2002). [DOI] [PubMed] [Google Scholar]
- Xie B. et al. Socio-demographic and economic correlates of overweight status in Chinese adolescents. Am J Health Behav. 31, 339–352 (2007). [DOI] [PubMed] [Google Scholar]
- Langnase K., Mast M. & Muller M. J. Social class differences in overweight of prepubertal children in northwest Germany. Int J Obes Relat Metab Disord. 26, 566–572 (2002). [DOI] [PubMed] [Google Scholar]
- Parsons T. J., Power C., Logan S. & Summerbell C. D. Childhood predictors of adult obesity: a systematic review. Int J Obes Relat Metab Disord. 23 Suppl 8, S1–107 (1999). [PubMed] [Google Scholar]
- Reidpath D. D., Burns C., Garrard J., Mahoney M. & Townsend M. An ecological study of the relationship between social and environmental determinants of obesity. Health Place. 8, 141–145 (2002). [DOI] [PubMed] [Google Scholar]
- Sobal J. & Stunkard A. J. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 105, 260–275 (1989). [DOI] [PubMed] [Google Scholar]
- McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 29, 29–48 (2007). [DOI] [PubMed] [Google Scholar]
- Fezeu L. et al. Association between socioeconomic status and adiposity in urban Cameroon. Int J Epidemiol. 35, 105–111 (2006). [DOI] [PubMed] [Google Scholar]
- Kaplan G. A. & Keil J. E. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 88, 1973–1998 (1993). [DOI] [PubMed] [Google Scholar]
- Gortmaker S. L., Must A., Perrin J. M., Sobol A. M. & Dietz W. H. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 329, 1008–1012 (1993). [DOI] [PubMed] [Google Scholar]
- Braddon F. E., Rodgers B., Wadsworth M. E. & Davies J. M. Onset of obesity in a 36 year birth cohort study. Br Med J (Clin Res Ed). 293, 299–303 (1986). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maty S.C., Everson-Rose S.A., Haan M.N., Raghunathan T.E. & Kaplan G.A. Education, income, occupation, and the 34-year incidence (1965-99) of Type 2 diabetes in the Alameda County Study. Int J Epidemiol. 34, 1274–1281 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A. & Specter, S. E. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 79, 6–16 (2004). [DOI] [PubMed] [Google Scholar]
- Lu N., Samuels M. E. & Huang K. C. Dietary behavior in relation to socioeconomic characteristics and self-perceived health status. J Health Care Poor Underserved. 13, 241–257 (2002). [DOI] [PubMed] [Google Scholar]
- Winkleby M. A., Kraemer H. C., Ahn D. K. & Varady A. N. Ethnic and socioeconomic differences in cardiovascular disease risk factors: findings for women from the Third National Health and Nutrition Examination Survey, 1988-1994. JAMA. 280, 356–362 (1998). [DOI] [PubMed] [Google Scholar]
- Wardle J. & Griffith J. Socioeconomic status and weight control practices in British adults. J Epidemiol Community Health. 55, 185–190 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agardh E., Allebeck P., Hallqvist J., Moradi T. & Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 40, 804–818 (2011). [DOI] [PubMed] [Google Scholar]
- Stroup D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 283, 2008–2012 (2000). [DOI] [PubMed] [Google Scholar]
- Wells G. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, 3–4 (Ottawa: University of Ottawa, 2011). [Google Scholar]
- Egger M., Davey Smith G., Schneider M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 315, 629–634 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg C. B. & Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 50, 1088–1101 (1994). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.