Abstract
BACKGROUND:
The morbidity and mortality associated with COPD exacts a considerable economic burden. Comorbidities in COPD are associated with poor health outcomes and increased costs. Our objective was to assess the impact of comorbidities on COPD-associated costs in a large administrative claims dataset.
METHODS:
This was a retrospective observational study of data from the Truven Health MarketScan Commercial Claims and Encounters and the MarketScan Medicare Supplemental Databases from January 1, 2009, to September 30, 2012. Resource consumption was measured from the index date (date of first occurrence of non-rule-out COPD diagnosis) to 360 days after the index date. Resource use (all-cause and disease-specific [ie, COPD- or asthma-related] ED visits, hospitalizations, office visits, other outpatient visits, and total length of hospital stay) and health-care costs (all-cause and disease-specific costs for ED visits, hospitalizations, office visits, and other outpatient visits and medical, prescription, and total health-care costs) were assessed. Generalized linear models were used to evaluate the impact of comorbidities on total health-care costs, adjusting for age, sex, geographic location, baseline health-care use, employment status, and index COPD medication.
RESULTS:
Among 183,681 patients with COPD, the most common comorbidities were cardiovascular disease (34.8%), diabetes (22.8%), asthma (14.7%), and anemia (14.2%). Most patients (52.8%) had one or two comorbidities of interest. The average all-cause total health-care costs from the index date to 360 days after the index date were highest for patients with chronic kidney disease ($41,288) and anemia ($38,870). The impact on total health-care costs was greatest for anemia ($10,762 more, on average, than a patient with COPD without anemia).
CONCLUSIONS:
Our analysis demonstrated that high resource use and costs were associated with COPD and multiple comorbidities.
COPD is defined by GOLD (Global Initiative for Chronic Obstructive Lung Disease) as a common, preventable, and treatable airflow limitation disease that is usually progressive and is associated with enhanced inflammation in the airways and lungs.1 COPD results in substantial economic burden and mortality. In 2010, the projected annual cost of COPD in the United States, as determined by the National Heart, Lung, and Blood Institute, was $49.9 billion, which included $29.5 billion in direct medical costs, $8.0 billion in indirect morbidity costs (eg, lost productivity because of illness), and $12.4 billion in indirect mortality costs (eg, lost productivity because of early death).2 COPD, together with other chronic lower respiratory diseases, is the third leading cause of death in the United States.3
Comorbidities are a major determinant of health status, health expenditure, and prognosis in patients with COPD.1,4 Patients with COPD with comorbidities have poorer health outcomes than those without comorbidities. In an analysis of 20,296 patients, poorer lung function was associated with having comorbid diseases, and those with poorer lung function and comorbid diseases had higher risks of morbidity and mortality.4 Worsening of comorbid diseases may be related to the airflow limitation associated with COPD, which can affect cardiac function and gas exchange.1,5 Proinflammatory molecules associated with COPD may also contribute to skeletal muscle wasting and cachexia and may trigger or exacerbate comorbid heart disease, osteoporosis, anemia, diabetes and metabolic syndrome, normocytic anemia, and depression.1,5 Comorbidities in patients with COPD impose a substantial economic burden; data across seven countries showed that annual societal costs were higher in patients with COPD who reported comorbidities than in those who did not.6
The presence of comorbidities is one of the components of the evaluation of a patient with new or suspected COPD.1 Management of patients with COPD includes the diagnosis and treatment of comorbidities; however, treatment of COPD is generally not affected by comorbidities, and comorbidities should be treated as if the patient did not have COPD.1 The objectives of this study were to assess and quantify the impact of comorbidities on the costs associated with COPD in a large administrative claims dataset.
Materials and Methods
Study Design
This was a retrospective observational study. Data sources were the Truven Health MarketScan Commercial Claims and Encounters and the MarketScan Medicare Supplemental Databases from January 1, 2009, to September 30, 2012. Records of patients with a COPD diagnosis at any diagnosis position within the intake period from July 1, 2009, through September 30, 2011, were included. Claims for laboratory, pathology, or radiology services were not used to identify individuals with a specific condition, because their use could incorrectly identify individuals as having that condition based on the reason for testing (eg, screening) rather than the test results; therefore, those claims were ignored during patient selection, and diagnoses were termed non-rule-out COPD. The first occurrence of non-rule-out COPD diagnosis (International Classification of Diseases, Ninth Revision, Clinical Modification codes 490.xx, 491.xx, 492.xx, 494.xx, or 496.xx) (e-Table 1 (93.4KB, pdf) ) was defined as the index event, and the date of the index event was defined as the index date. None of the source databases contained any personal identifiers. Institutional review board approval was not required for this study. The study proposal was presented to and accepted by the Novartis Outcomes Research Review Forum.
Patients
Eligible patients were aged 40 to 90 years (inclusive), had COPD, and used at least one long-acting muscarinic antagonist (LAMA), long-acting β2-adrenergic agonist (LABA), inhaled corticosteroid (ICS)/LABA, or LAMA + ICS + LABA from 180 days before the index date through 180 days after the index date. Patients were enrolled continuously in the medical, pharmacy benefit, and fee-for-service plan from 180 days before the index date to 360 days after the index date. Patients were excluded if region information was missing.
Variables
Comorbidities were defined as any occurrence of a specific diagnosis code from 180 days before the index date through 180 days after the index date. This time period, which does not fall completely within the baseline period or the 360-day follow-up period, was chosen to establish and solidify the baseline patient comorbidities being evaluated. Comorbidities of interest were identified prospectively and consisted of chronic kidney disease (CKD); cardiovascular disease (CVD), including heart failure, stroke, acute myocardial infarction (MI), and peripheral vascular disease; asthma; depression; diabetes; osteoporosis; and anemia. Resource consumption was measured from 180 days prior to the index date to the index date (for baseline assessments) and from the index date through 360 days after the index date (for outcomes assessments). Resource use assessments included all-cause and disease-specific ED visits, hospitalizations, office visits (defined as any office visit to any doctor), outpatient visits, and total length of hospital stay; in this instance, disease-specific means COPD- or asthma-related. The health-care costs assessed included all-cause and disease-specific costs for ED visits, hospitalizations, office visits, and other outpatient visits, as well as medical, prescription drug, and total health-care costs. All costs were adjusted to 2012 US dollars. Other covariate variables included age, sex, region, employment status, and index medication (the first drug class used during the period).
Data Analysis
Patient characteristics, comorbidities of interest, health-care use, and costs were summarized descriptively. Data were analyzed descriptively by the type and number of comorbidities of interest.
A generalized linear model (GLM) was used to evaluate which comorbidities drive total costs after accounting for patient characteristics in the total population. After examining the data, we selected GLMs with a log-link and γ distribution to evaluate the incremental all-cause costs, adjusting for baseline demographics, resource use, and comorbidities.7 To better understand total costs that are potentially attributable to comorbidities, the average treatment effect (change in the response by a change in a covariate) of each comorbidity was calculated by using the recycled prediction method.8 The predicted costs for patients with CVD were calculated based on the estimated GLM (with costs as the dependent variable) by assuming all patients had CVD (regardless of whether they had CVD) while keeping other covariates as they were. The predicted costs, for which every observation is treated as if it represents patients without CVD, were obtained in the same manner. The average treatment effect was the mean difference in the predicted costs for the two groups. Thus, we compared two hypothetical populations (one with CVD and one without CVD) that had the exact same values for the other independent variables in the model. CIs were generated with the percentile method (the 95% lower bound CI is the 2.5th percentile of the bootstrap distribution, and the 95% upper bound CI is the 97.5th percentile of the bootstrap distribution). Analyses were carried out using SAS version 9.2 (SAS Institute).
Results
Patients
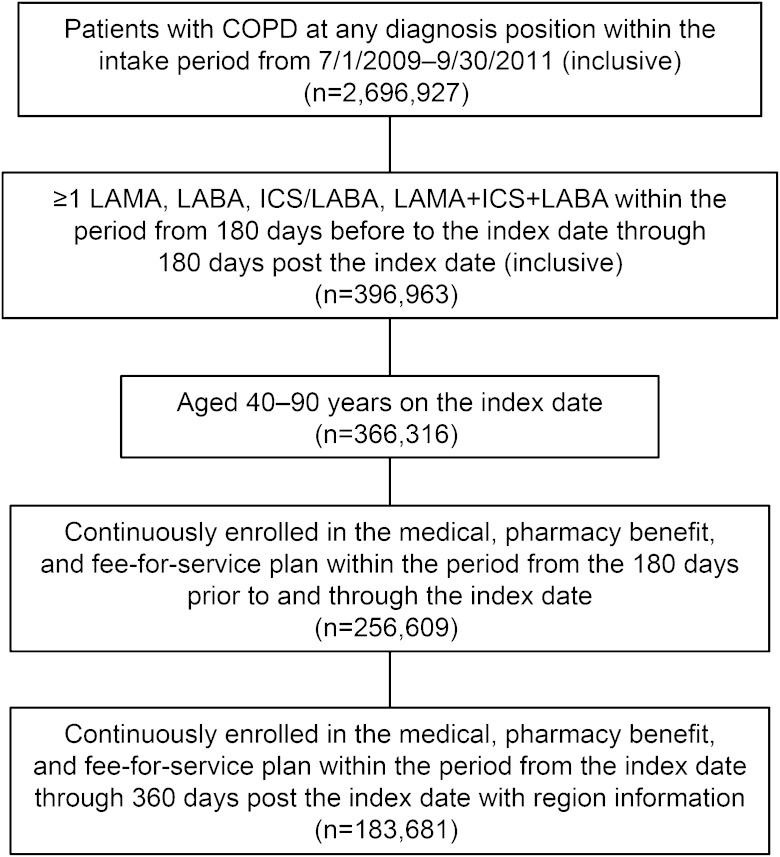
This analysis included 183,681 patients (Fig 1). Patient characteristics on the index date are summarized in Table 1, and health-care use and costs from the 180 days preceding the index date through the index date are summarized in Table 2. The most common comorbidity was CVD (34.8%), followed by diabetes (22.8%), asthma (14.7%), anemia (14.2%), CKD (9.9%), depression (9.9%), and osteoporosis (6.9%). Most patients (52.8%) had one or two comorbidities of interest. Patients with CKD and anemia experienced the highest incidence of all-cause ED visits leading to hospitalizations (23.2% and 20.4%, respectively) and all-cause hospitalizations (38.0% and 33.8%, respectively). The percentages of all-cause office visits and of all-cause other outpatient visits were generally similar across the various comorbidity groups (all-cause office visits, 93.8%-95.4%; all-cause other outpatient visits, 95.1%-97.7%) and were higher than those for patients with no baseline comorbidities of interest (83.9% and 84.6%, respectively).
Figure 1 –
Patient selection. ICS = inhaled corticosteroid; LABA = long-acting β2-adrenergic agonist; LAMA = long-acting muscarinic antagonist.
TABLE 1 ] .
Patient Characteristics
| Characteristics at Index Date | All Patients (N = 183,681) | Comorbidities | |||||||
| CKD (n = 18,181) | CVD (n = 64,011) | Asthma (n = 27,046) | Depression (n = 18,102) | Diabetes (n = 41,922) | Osteoporosis (n = 12,644) | Anemia (n = 26,033) | No Comorbidity (n = 64,232) | ||
| Age, mean (SD), y | 65.9 (11.7) | 71.4 (10.7) | 69.9 (11.0) | 62.5 (12.0) | 61.8 (11.3) | 67.2 (10.7) | 70.0 (10.5) | 68.7 (11.7) | 63.8 (11.4) |
| Men | 83,559 (45.5) | 9,825 (54.0) | 31,940 (49.9) | 9,048 (33.5) | 5,451 (30.1) | 21,307 (50.8) | 1,973 (15.6) | 11,238 (43.2) | 30,622 (47.7) |
| Region | |||||||||
| Northeast | 29,638 (16.1) | 2,905 (16.0) | 10,672 (16.7) | 4,429 (16.4) | 2,882 (15.9) | 6,705 (16.0) | 2,279 (18.0) | 4,523 (17.4) | 10,019 (15.6) |
| Midwest | 63,734 (34.7) | 6,524 (35.9) | 23,027 (36.0) | 8,147 (30.1) | 6,332 (35.0) | 15,673 (37.4) | 3,716 (29.4) | 8,979 (34.5) | 22,201 (34.6) |
| South | 64,335 (35.0) | 6,018 (33.1) | 21,278 (33.2) | 9,553 (35.3) | 6,096 (33.7) | 14,298 (34.1) | 4,165 (32.9) | 8,576 (32.9) | 23,397 (36.4) |
| West | 25,974 (14.1) | 2,734 (15.0) | 9,034 (14.1) | 4,917 (18.2) | 2,792 (15.4) | 5,246 (12.5) | 2,484 (19.6) | 3,955 (15.2) | 8,615 (13.4) |
| Employment status | |||||||||
| Employee | 130,072 (70.8) | 13,608 (74.8) | 47,088 (73.6) | 18,371 (67.9) | 11,750 (64.9) | 30,042 (71.7) | 8,460 (66.9) | 18,629 (71.6) | 45,261 (70.5) |
| Othera | 53,609 (29.2) | 4,573 (25.2) | 16,923 (26.4) | 8,675 (32.1) | 6,352 (35.1) | 11,880 (28.3) | 4,184 (33.1) | 7,404 (28.4) | 18,971 (29.5) |
| Index COPD medication | |||||||||
| LABAs | 3,719 (2.0) | 360 (2.0) | 1,277 (2.0) | 520 (1.9) | 266 (1.5) | 806 (1.9) | 299 (2.4) | 511 (2.0) | 1,368 (2.1) |
| LAMAs | 49,258 (26.8) | 5,301 (29.2) | 18,974 (29.6) | 3,949 (14.6) | 4,522 (25.0) | 11,197 (26.7) | 3,704 (29.3) | 7,149 (27.5) | 17,557 (27.3) |
| ICS/LABA fixed or loose-dose combination | 111,587 (60.8) | 10,406 (57.2) | 36,206 (56.6) | 20,337 (75.2) | 11,543 (63.8) | 25,503 (60.8) | 7,274 (57.5) | 15,448 (59.3) | 38,813 (60.4) |
| ICS/LABA fixed or loose-dose combination and LAMA | 19,117 (10.4) | 2,114 (11.6) | 7,554 (11.8) | 2,240 (8.3) | 1,771 (9.8) | 4,416 (10.5) | 1,367 (10.8) | 2,925 (11.2) | 6,494 (10.1) |
| Comorbidities of interestb | |||||||||
| CKD | 18,181 (9.9) | 18,181 (100.0) | 12,333 (19.3) | 2,564 (9.5) | 2,057 (11.4) | 8,069 (19.2) | 1,317 (10.4) | 6,872 (26.4) | … |
| CVDc | 64,011 (34.8) | 12,333 (67.8) | 64,011 (100.0) | 9,162 (33.9) | 7,203 (39.8) | 20,187 (48.2) | 5,116 (40.5) | 14,716 (56.5) | … |
| Asthma | 27,046 (14.7) | 2,564 (14.1) | 9,162 (14.3) | 27,046 (100.0) | 3,596 (19.9) | 6,762 (16.1) | 2,046 (16.2) | 4,176 (16.0) | … |
| Depression | 18,102 (9.9) | 2,057 (11.3) | 7,203 (11.3) | 3,596 (13.3) | 18,102 (100.0) | 4,448 (10.6) | 1,605 (12.7) | 3,712 (14.3) | … |
| Diabetes | 41,922 (22.8) | 8,069 (44.4) | 20,187 (31.5) | 6,762 (25.0) | 4,448 (24.6) | 41,922 (100.0) | 2,346 (18.6) | 8,986 (34.5) | … |
| Osteoporosis | 12,644 (6.9) | 1,317 (7.2) | 5,116 (8.0) | 2,046 (7.6) | 1,605 (8.9) | 2,346 (5.6) | 12,644 (100.0) | 2,608 (10.0) | … |
| Anemia | 26,033 (14.2) | 6,872 (37.8) | 14,716 (23.0) | 4,176 (15.4) | 3,712 (20.5) | 8,986 (21.4) | 2,608 (20.6) | 26,033 (100.0) | … |
| Number of comorbidities of interestb | |||||||||
| 0 | 64,232 (35.0) | … | … | … | … | … | … | … | 64,232 (100.0) |
| 1 | 61,990 (33.7) | 2,033 (11.2) | 22,494 (35.1) | 10,325 (38.2) | 5,605 (31.0) | 12,646 (30.2) | 4,096 (32.4) | 4,791 (18.4) | … |
| 2 | 34,995 (19.1) | 5,234 (28.8) | 22,356 (34.9) | 9,017 (33.3) | 6,028 (33.3) | 14,662 (35.0) | 4,308 (34.1) | 8,385 (32.2) | … |
| 3 | 15,498 (8.4) | 6,097 (33.5) | 12,681 (19.8) | 4,837 (17.9) | 3,822 (21.1) | 9,112 (21.7) | 2,588 (20.5) | 7,357 (28.3) | … |
| 4 | 5,551 (3.0) | 3,645 (20.0) | 5,104 (8.0) | 2,009 (7.4) | 1,802 (10.0) | 4,268 (10.2) | 1,166 (9.2) | 4,210 (16.2) | … |
| 5 | 1,235 (0.7) | 1,017 (5.6) | 1,199 (1.9) | 708 (2.6) | 688 (3.8) | 1,068 (2.5) | 380 (3.0) | 1,115 (4.3) | … |
| 6 | 174 (0.1) | 149 (0.8) | 171 (0.3) | 144 (0.5) | 151 (0.8) | 160 (0.4) | 100 (0.8) | 169 (0.6) | … |
| 7 | 6 (0.0) | 6 (0.0) | 6 (0.0) | 6 (0.0) | 6 (0.0) | 6 (0.0) | 6 (0.0) | 6 (0.0) | … |
Data are given as No. (%) unless otherwise indicated. CKD = chronic kidney disease; CVD = cardiovascular disease; ICS = inhaled corticosteroid; LABA = long-acting β2-adrenergic agonist; LAMA = long-acting muscarinic agonist; MI = myocardial infarction.
Spouse/child/dependent relation.
Within the period from 180 d before the index date through 180 d after the index date (inclusive).
Includes heart failure, stroke, acute MI, and peripheral vascular disease.
TABLE 2 ] .
Baseline Resource Use and Costs
| Parameter | All Patients (N = 183,681) | Comorbidities | |||||||
| CKD (n = 18,181) | CVD (n = 64,011) | Asthma (n = 27,046) | Depression (n = 18,102) | Diabetes (n = 41,922) | Osteoporosis (n = 12,644) | Anemia (n = 26,033) | No Comorbidity (n = 64,232) | ||
| Resource use,a No. (%) | |||||||||
| All-cause ED visits | |||||||||
| Leading to hospitalizations | 16,767 (9.1) | 4,216 (23.2) | 11,056 (17.3) | 3,749 (13.9) | 2,813 (15.5) | 5,874 (14.0) | 1,419 (11.2) | 5,299 (20.4) | 1,616 (2.5) |
| Not leading to hospitalizations | 40,151 (21.9) | 6,938 (38.2) | 21,202 (33.1) | 8,181 (30.2) | 6,005 (33.2) | 11,918 (28.4) | 3,180 (25.2) | 9,155 (35.2) | 7,562 (11.8) |
| All-cause hospitalizations | 28,963 (15.8) | 6,905 (38.0) | 18,772 (29.3) | 5,762 (21.3) | 4,468 (24.7) | 9,860 (23.5) | 2,357 (18.6) | 8,794 (33.8) | 3,196 (5.0) |
| All-cause office visits | 165,533 (90.1) | 17,349 (95.4) | 60,074 (93.8) | 25,573 (94.6) | 17,061 (94.2) | 39,762 (94.8) | 11,990 (94.8) | 24,712 (94.9) | 53,865 (83.9) |
| All-cause other outpatient visits | 168,291 (91.6) | 17,766 (97.7) | 61,611 (96.3) | 25,730 (95.1) | 17,464 (96.5) | 40,589 (96.8) | 12,198 (96.5) | 25,318 (97.3) | 54,336 (84.6) |
| COPD- or asthma-related ED visits | |||||||||
| Leading to hospitalizations | 3,071 (1.7) | 437 (2.4) | 1,598 (2.5) | 1,552 (5.7) | 499 (2.8) | 1,014 (2.4) | 279 (2.2) | 621 (2.4) | 338 (0.5) |
| Not leading to hospitalizations | 6,074 (3.3) | 821 (4.5) | 2,967 (4.6) | 2,469 (9.1) | 959 (5.3) | 1,642 (3.9) | 523 (4.1) | 1,197 (4.6) | 923 (1.4) |
| COPD- or asthma-related hospitalizations | 4,645 (2.5) | 663 (3.6) | 2,430 (3.8) | 2,236 (8.3) | 704 (3.9) | 1,500 (3.6) | 424 (3.4) | 952 (3.7) | 548 (0.9) |
| COPD- or asthma-related office visits | 43,501 (23.7) | 4,448 (24.5) | 16,714 (26.1) | 12,601 (46.6) | 4,497 (24.8) | 9,913 (23.6) | 3,998 (31.6) | 6,715 (25.8) | 11,282 (17.6) |
| COPD- or asthma-related other outpatient visits | 50,468 (27.5) | 5,806 (31.9) | 20,744 (32.4) | 12,390 (45.8) | 5,241 (29.0) | 12,385 (29.5) | 4,565 (36.1) | 8,578 (33.0) | 13,003 (20.2) |
| Costs, mean (SD),b $ | |||||||||
| All-cause ED visit costs | |||||||||
| Leading to hospitalization | 78.6 (633.9) | 228.6 (1,394.1) | 154.8 (949.8) | 120.3 (640.0) | 148.4 (780.2) | 123.1 (677.4) | 96.2 (570.7) | 195.9 (1,206.4) | 18.8 (197.4) |
| Not leading to hospitalization | 193.2 (964.5) | 342.9 (1,628.5) | 294.1 (1,300.8) | 311.8 (1,157.7) | 384.2 (1,582.0) | 261.2 (1,293.2) | 221.4 (1,251.2) | 334.9 (1,503.8) | 94.3 (552.1) |
| All-cause hospitalization costs | 2,113.1 (15,096.5) | 7,816.1 (35,849.2) | 4,615.2 (23,415.6) | 2,866.2 (17,705.3) | 4,543.2 (28,269.4) | 3,655.4 (21,835.7) | 2,558.7 (18,003.4) | 6,570.4 (31,749.0) | 352.3 (3,660.7) |
| All-cause office visit costs | 482.4 (500.3) | 731.4 (647.4) | 628.8 (586.4) | 609.5 (588.3) | 639.1 (605.9) | 608.8 (561.6) | 643.7 (651.4) | 726.4 (699.5) | 316.4 (356.3) |
| All-cause other outpatient visit costs | 3,841.8 (10,751.5) | 8,321.2 (22,228.3) | 5,954.2 (14,748.3) | 4,090.3 (9,535.7) | 5,882.9 (12,775.2) | 5,170.4 (13,700.9) | 4,957.6 (10,600.9) | 8,058.6 (20,230.9) | 2,045.1 (6,386.2) |
| All-cause medical costs (ED + hospitalization + office visits + other outpatient) | 6,709.1 (20,155.3) | 17,440.1 (44,852.1) | 11,647.1 (29,860.0) | 7,998.1 (21,673.3) | 11,597.8 (33,604.4) | 9,818.8 (27,875.8) | 8,477.5 (23,265.1) | 15,886.2 (40,247.2) | 2,826.9 (7,823.3) |
| All-cause prescription drug costs | 2,636.5 (3,705.4) | 3,678.1 (4,288.3) | 3,118.3 (4,549.5) | 2,843.7 (3,595.1) | 3,422.4 (6,040.7) | 3,554.6 (4,711.9) | 3,287.5 (4,545.1) | 3,442.8 (4,687.0) | 1,976.8 (2,828.0) |
| All-cause total health-care costs (medical costs + prescription drug costs) | 9,094.5 (16,330.1) | 19,405.5 (29,521.0) | 14,125.4 (22,539.5) | 10,583.2 (17,066.6) | 14,200.2 (22,676.7) | 12,827.1 (20,527.3) | 11,437.6 (17,798.1) | 18,010.9 (28,059.2) | 4,789.9 (8,237.6) |
| COPD- or asthma-related ED visit costs | |||||||||
| Leading to hospitalization | 11.5 (163.5) | 16.0 (161.9) | 17.2 (194.0) | 40.7 (323.4) | 18.3 (162.2) | 15.4 (148.3) | 15.6 (169.4) | 16.9 (226.4) | 3.2 (61.7) |
| Not leading to hospitalization | 20.0 (222.2) | 22.2 (202.0) | 25.3 (239.1) | 65.9 (418.2) | 35.7 (286.3) | 21.9 (214.9) | 21.6 (191.8) | 26.8 (282.5) | 8.0 (132.9) |
| COPD- or asthma-related hospitalization costs | 193.5 (2,602.1) | 345.3 (4,690.5) | 315.6 (3,724.5) | 690.3 (5,052.3) | 338.9 (3,288.7) | 294.1 (3,458.8) | 285.5 (2,721.3) | 347.7 (4,475.8) | 50.1 (963.6) |
| COPD- or asthma-related office visit costs | 43.2 (122.5) | 47.9 (144.9) | 51.5 (146.9) | 89.0 (193.2) | 52.1 (137.3) | 44.4 (155.6) | 68.3 (177.2) | 53.3 (187.4) | 28.5 (85.4) |
| COPD- or asthma-related other outpatient visit costs | 281.5 (1,710.5) | 431.4 (2,443.7) | 399.3 (2,173.8) | 387.9 (2,094.4) | 416.7 (2,633.2) | 327.5 (1,860.5) | 497.6 (2,674.8) | 438.0 (2,308.1) | 179.1 (1,269.1) |
| COPD- or asthma-related medical costs (ED + hospitalization + office visits + other outpatient) | 549.7 (3,334.8) | 862.7 (5,495.9) | 808.9 (4,580.3) | 1,273.8 (5,775.2) | 861.7 (4,523.4) | 703.3 (4,195.8) | 888.4 (4,181.6) | 882.7 (5,315.2) | 269.0 (1,712.9) |
| COPD- or asthma-related prescription drug costs | 591.7 (669.0) | 575.6 (659.3) | 590.1 (669.4) | 582.6 (646.3) | 498.3 (620.3) | 570.8 (656.5) | 678.0 (704.5) | 570.0 (657.0) | 601.7 (677.6) |
| COPD- or asthma-related total health-care costs (medical costs + prescription drug costs)c | 1,138.6 (3,185.3) | 1,421.3 (4,476.5) | 1,391.0 (4,113.6) | 1,845.1 (5,191.1) | 1,359.2 (4,578.9) | 1,267.1 (3,708.9) | 1,566.5 (4,302.5) | 1,441.0 (4,641.2) | 870.7 (1,906.3) |
See Table 1 legend for expansion of abbreviations.
Resource use from the index date (exclusive) through 180 d before the index date (inclusive).
2012 US dollars.
Those with > $181,066.56 in total costs have been capped at $181,066.56.
The prevalence of COPD- or asthma-related hospitalizations was highest among patients with asthma at baseline (8.3%); for the other baseline comorbidities, the frequencies of COPD- or asthma-related hospitalizations were similar, ranging from 3.4% (osteoporosis) to 3.9% (depression). Mean all-cause total health-care costs from the 180 days before the index date through the index date were highest among patients with CKD ($19,405) and anemia ($18,011) and lowest among those with asthma ($10,583) and osteoporosis ($11,438). Mean COPD- or asthma-related total health-care costs were highest among patients with asthma ($1,845) and osteoporosis ($1,566).
In addition to those shown in Table 2, analyses were conducted based on the number of comorbidities present. Patients with four or more comorbidities experienced the highest incidence of ED visits leading to hospitalizations (33.1%), compared with 22.2% in those with three comorbidities, 13.8% in those with two comorbidities, 7.4% in those with one comorbidity, and 2.5% in those with no comorbidities. Similarly, the rate of all-cause hospitalizations was highest in patients with four or more comorbidities (50.4%) and lowest in those with no comorbidities (5.0%). All-cause total health-care costs increased as the number of comorbidities increased (zero comorbidities of interest, $4,790; four or more comorbidities of interest, $27,895), as did COPD- or asthma-related total health-care costs (zero comorbidity of interest, $871; four or more comorbidities of interest, $2,216).
Postindex Resource Use and Costs by Comorbidities
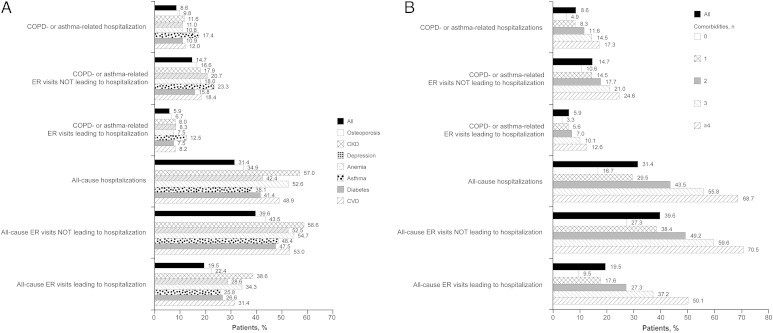
During the time period from the index date through 360 days after the index date, 38.6% of patients with COPD and CKD and 34.3% of patients with COPD and anemia had all-cause ED visits leading to hospitalizations (Fig 2A). The percentage of patients experiencing all-cause hospitalizations was highest among those with CKD (57.0%) and anemia (52.6%) (Fig 2A). The percentage of patients with COPD- or asthma-related hospitalizations was highest among those with asthma (17.4%) and CVD (12.0%) (Fig 2A). All-cause total health-care costs during the time period from the index date through 360 days following the index date were highest among patients with COPD and CKD ($41,288) and patients with COPD and anemia ($38,870) (Table 3). COPD- or asthma-related total health-care costs were highest among patients with COPD and asthma ($5,389) and those with COPD and CKD ($5,117).
Figure 2 –
A, B, Resource use from index date through 360 d after the index date for each outcome. A, By comorbidity. B, By number of comorbidities. CKD = chronic kidney disease; CVD = cardiovascular disease; ER = emergency room.
TABLE 3 ] .
Total Medical Costs by Comorbidity and Number of Comorbidities
| Comorbidity | Total All-Cause Health-care Costs | Total All-Cause Hospitalization Costs | Total COPD- or Asthma-Related Health-care Costs |
| All Patients | 21,752.8 (28,846.3) | 5,523.4 (26,365.2) | 3,993.5 (7,283.1) |
| CKD | 41,288.4 (43,468.0) | 15,817.1 (50,265.7) | 5,117.0 (9,467.0) |
| CVD | 31,734.3 (36,115.8) | 10,508.1 (38,004.4) | 4,996.9 (9,191.6) |
| Asthma | 25,092.5 (30,739.5) | 7,314.5 (29,846.2) | 5,389.3 (10,379.6) |
| Depression | 31,661.8 (36,407.5) | 10,171.5 (39,321.6) | 4,802.1 (9,649.0) |
| Diabetes | 29,245.7 (33,987.8) | 8,797.6 (35,505.2) | 4,304.6 (8,020.2) |
| Osteoporosis | 26,084.1 (30,715.4) | 6,283.6 (26,798.3) | 4,995.5 (9,195.7) |
| Anemia | 38,870.3 (42,916.3) | 14,101.7 (48,623.3) | 4,987.0 (9,565.7) |
| No. of comorbidities | |||
| 0 | 12,978.3 (18,544.5) | 1,834.9 (12,398.5) | 3,169.2 (5,254.8) |
| 1 | 19,535.8 (24,511.6) | 4,077.2 (19,861.6) | 3,837.1 (6,658.8) |
| 2 | 27,648.7 (31,173.8) | 7,607.7 (29,582.7) | 4,527.2 (7,937.8) |
| 3 | 37,991.4 (38,451.0) | 12,681.3 (40,038.7) | 5,485.0 (9,962.4) |
| ≥ 4 | 56,641.9 (50,207.4) | 26,006.7 (68,846.1) | 6,987.6 (13,797.4) |
Data are presented as mean (SD). Costs are from index date through 360 d after the index date and are in 2012 US dollars. See Table 1 legend for expansion of abbreviations.
Patients with four or more comorbidities of interest experienced the highest incidence of ED visits leading to hospitalizations (50.1% vs 9.5% with no comorbidities) and all-cause hospitalizations (68.7% vs 16.7% with no comorbidities) (Fig 2B). All-cause total health-care costs and COPD- or asthma-related total health-care costs both increased as the number of comorbidities increased (Table 3).
Model Results
The reference group selected for the GLM was female patients with COPD aged 40 to 64 years, living in the South, employed, having an index medication of ICS/LABA fixed or loose-dose combination with no ED visits or hospitalizations regardless of relationship to asthma or COPD, and who did not have CKD, CVD, asthma, depression, diabetes, osteoporosis, or anemia. In this group, the average total health-care cost was $12,408. A ratio, based on the impact on total health-care costs, was estimated for each variable in the model (Table 4) and represents multiplicative effects.
TABLE 4 ] .
Ratios for Variables Included in the Generalized Linear Model
| Variable | Ratio (95% CI) |
| Age group | |
| 40-64 ya | … |
| 65-90 y | 0.95 (0.94-0.97) |
| Sex | |
| Femalea | … |
| Male | 1.04 (1.03-1.06) |
| Region | |
| Southa | … |
| Northeast | 1 (0.99-1.02) |
| North central (Midwest) | 0.91 (0.90-0.92) |
| West | 1.02 (1.01-1.04) |
| Employment status | |
| Employeea | … |
| Other (spouse/child/dependent relation) | 1.08 (1.07-1.09) |
| Index medication class | |
| ICS/LABA fixed or loose-dose combinationa | … |
| LABAs | 1.08 (1.04-1.13) |
| LAMAs | 1.08 (1.06-1.09) |
| ICS/LABA fixed or loose-dose combination and LAMA | 1.22 (1.20-1.25) |
| Within the period from the index date (exclusive) through 180 d before the index date (inclusive) | |
| No COPD- or asthma-related ED visitsa | … |
| Any COPD- or asthma-related ED visits | 1.07 (1.04-1.11) |
| No COPD- or asthma-related hospitalizationsa | … |
| Any COPD- or asthma-related hospitalizations | 1.15 (1.10-1.20) |
| No COPD- or asthma-related ED visitsa | … |
| Any non COPD- or asthma-related ED visits | 1.19 (1.17-1.12) |
| No COPD- or asthma-related hospitalizationsa | … |
| Any non COPD- or asthma-related hospitalizations | 1.15 (1.13-1.17) |
| Comorbidities of interest | |
| CKD | 1.43 (1.40-1.46) |
| CVD (stroke, acute MI, peripheral vascular disease) | 1.55 (1.53-1.57) |
| Asthma | 1.15 (1.13-1.17) |
| Depression | 1.35 (1.33-1.38) |
| Diabetes | 1.23 (1.22-1.25) |
| Osteoporosis | 1.18 (1.15-1.20) |
| Anemia | 1.54 (1.52-1.57) |
Arithmetic mean cost for the reference group was $12,408. See Table 1 legend for expansion of abbreviations.
Reference group.
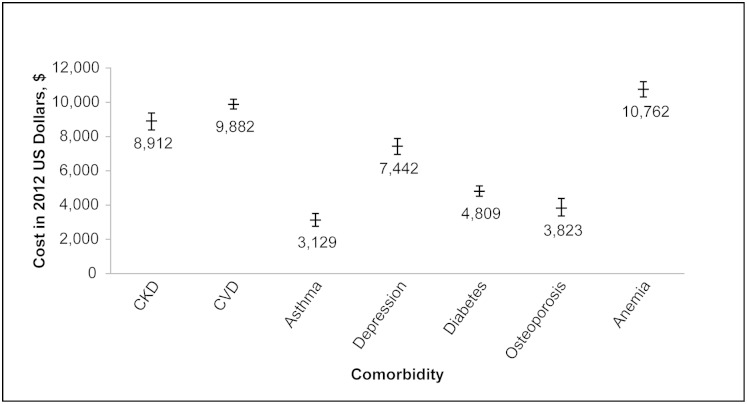
Characteristics with the greatest impact on costs included depression (ratio, 1.35), CKD (ratio, 1.43), anemia (ratio, 1.54), and CVD (ratio, 1.55) comorbidities (Table 4). The average treatment effect for each comorbidity after adjusting for age, sex, geographic location, baseline health-care use, employment status, and index COPD medication is shown in Figure 3. For the time period from the index date through 360 days following the index date, a patient with COPD and anemia had, on average, $10,762 more in total health-care costs than a patient with COPD but without anemia. CVD and CKD increased total health-care costs by $9,882 and $8,912, respectively.
Figure 3 –
Difference in average total health-care cost by comorbidity from index date through 360 d after the index date in 2012 US dollars. See Figure 2 legend for expansion of abbreviations.
Discussion
Our results were consistent with those of previously published work, in that a significant burden of comorbidity was associated with COPD,9 and comorbid conditions were associated with incremental increases in resource use and health-care costs.10,11 Total health-care costs during the period from the index date through 360 days following the index date were greatest among patients with COPD and CKD or anemia; COPD- or asthma-related total health-care costs were greatest among patients with COPD and asthma and CKD. These results were driven, in part, by high incidences of all-cause ED visits leading to hospitalizations among patients with COPD and CKD or anemia, and a high incidence of COPD- or asthma-related hospitalization among patients with COPD and asthma.
Multivariable analyses adjusted for age, sex, geographic location, baseline health-care use, employment status, and index COPD medication showed that the effect of comorbidities on total health-care costs was greatest for anemia. This finding is consistent with the high incidences of all-cause ED visits leading to hospitalizations and all-cause hospitalizations among patients with COPD and anemia. Substantial treatment effects of CVD and CKD (about $9,000) are likely attributable, in part, to the high incidence (about 50%) of all-cause hospitalization in both groups.
Cavailles et al12 reviewed the pathophysiologic and epidemiologic links between COPD and the comorbidities studied here, and concluded that shared risk factors and the influence of chronic systemic inflammation are likely contributors to these relationships. Smoking is a major risk factor for both COPD and CVD, and CVD was the most common comorbidity in the COPD population; thus, the frequent coexistence of these two conditions is unsurprising. However, the literature also suggests that the systemic inflammation associated with COPD produces a “procoagulant state” and endothelial dysfunction that may contribute to thromboembolic events.12 In fact, at least one study13 has shown that the link between cardiovascular events (including death) and COPD is independent of smoking status and other confounding coronary risk factors.
There is no evidence of a direct role for COPD-related inflammation in anemia,12 which was identified as the most costly of the comorbidities in this study. However, older age, malnutrition, and CVD frequently accompany COPD and are believed to play a role in the development of anemia in patients with COPD.12 Consistent with our findings, Ornek et al14 determined that anemia significantly increased the cost of COPD treatment in patients hospitalized for acute exacerbation of COPD. Furthermore, anemia was independently prognostic for premature mortality, hospital admissions, and cumulative duration of hospitalization in patients with severe COPD receiving long-term oxygen therapy.15
Our results support CKD as a key driver of total health-care costs as well as COPD- and asthma-related health-care costs in patients with COPD, although it was not as prevalent as other comorbidities studied. Epidemiologic studies have confirmed COPD as a risk factor for CKD,9,16,17 and the literature suggests that renal function is sensitive to hypoxemia and hypercarbia.18 Additionally, arterial stiffness associated with COPD may damage glomeruli,18 and some COPD medications may have nephrotoxic effects.16 The presence of chronic renal failure significantly increased the cost of care in patients hospitalized for acute exacerbation of COPD.14
Finally, COPD- or asthma-related total health-care costs were higher among patients with COPD and asthma than among those with any other comorbidity. “Overlap syndrome” refers to patients who have components of both conditions, and it is often used to describe elderly individuals in whom the distinction between asthma and COPD is difficult to make.19 In a study of nearly 25,000 insured adults with COPD, those with asthma had 1.6 times greater odds of having respiratory-related ED visits, hospitalizations, or both than did those with COPD alone and demonstrated an approximately 50% increase in respiratory-related health-care costs.20
Hospital cost use for COPD or bronchiectasis was also evaluated in a recent analysis of the Nationwide Inpatient Sample and the Nationwide Emergency Department Sample database of the Healthcare Cost and Utilization Project. Although significant trends were not found in age-adjusted rates of hospital discharges from 2001 to 2012, ED visits from 2006 to 2011, or 30-day readmissions from 2009 to 2012, the mean charges and costs of all discharges increased considerably from 2001 to 2012, with aggregate charges for inpatient stays increasing from $8,023,983,422 in 2001 to $18,112,392,566 in 2012.21
This study was subject to several limitations. Because it was restricted to patients who were on long-acting therapies, patients with the mildest form of COPD and patients with more advanced disease who were not appropriately prescribed long-acting therapies were likely excluded. Inherent to claims data research, the clinical accuracy of the coding could not be assessed. In addition, patients with health maintenance organizations or full or partial capitated point-of-service insurance coverage were excluded from this study because the financial information for this population was incomplete. Further, this analysis did not include patients on Medicaid and it contained < 8% of patients with managed Medicare. No information was available regarding the severity of disease and the level of treatment adherence. Finally, the study lacked data regarding indirect costs related to COPD and comorbidities. An analysis in the younger, working-age COPD population (45-64 years of age) showed that these costs (which include the costs of impaired productivity at work, lost productivity because of early retirement, disability pensions paid, and tax revenue lost) are considerably higher than the direct medical cost of COPD.22
Conclusions
In conclusion, these results show that a high prevalence of patients with COPD and multiple comorbidities have associated high resource use and costs, especially within the all-cause use category. Optimizing treatment among patients with COPD and comorbidities is a challenge. Further research on comorbid conditions affecting the treatment adherence of patients with COPD, COPD pathogenic pathways, and worsening overall prognosis is necessary to elucidate the role of comorbidities in COPD.
Supplementary Material
Online Supplement
Acknowledgments
Author contributions: D. M. M. and K. H. take responsibility for the integrity and content of the manuscript, including the data and analysis. D. M. M., K. H., T.-C. Y., H. Z., Y. L., H. T., and K. S. contributed to the study design, data analysis and interpretation, and writing and review of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Mannino has received honoraria/consulting fees from and served on speaker bureaus for GlaxoSmithKline; Novartis Pharmaceuticals Corporation; Pfizer, Inc; Boehringer-Ingelheim GmbH; AstraZeneca; Forest Laboratories, Inc; Merck & Co; and Amgen. Furthermore, he has received royalties from UpToDate and is on the board of directors of the COPD Foundation. Ms Higuchi is an employee of Novartis Pharmaceuticals Corporation. Dr Yu is an employee and stockholder of Novartis Pharmaceuticals Corporation. Ms Zhou is an employee of KMK Consulting Inc and provides services to Novartis Pharmaceuticals Corporation. Ms Li was a contractor for Novartis Pharmaceuticals Corporation from Beijing Foreign Enterprises Human Resources Services Co, Ltd when the study was conducted. Dr Tian is an employee and stockholder of Novartis Pharmaceuticals Corporation. Dr Suh was an outcomes research fellow of Novartis Pharmaceuticals Corporation when the study was conducted.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: Medical writing services were provided by Anny Wu, PharmD, and Erica Wehner, RPh, at Complete Healthcare Communications, Inc (Chadds Ford, PA), with funding from Novartis Pharmaceuticals Corporation (East Hanover, NJ).
Additional information: The e-Table can be found in the Supplemental Materials section of the online article.
ABBREVIATIONS
- CKD
chronic kidney disease
- CVD
cardiovascular disease
- GLM
generalized linear model
- ICS
inhaled corticosteroid
- LABA
long-acting β2-adrenergic agonist
- LAMA
long-acting muscarinic antagonist
- MI
myocardial infarction
Footnotes
Partial results from this study have been presented at the International Society for Pharmacoeconomics and Outcomes Research 16th Annual European Congress, November 2-6, 2013, Dublin, Ireland.
FUNDING/SUPPORT: This study was supported by Novartis Pharmaceuticals Corporation, East Hanover, NJ.
References
- 1.Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Global Initiative for Chronic Obstructive Lung Disease website. http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html. Published 2013. Accessed September 26, 2013.
- 2.Trends in COPD (chronic bronchitis and emphysema): morbidity and mortality. American Lung Association website. http://www.lung.org/finding-cures/our-research/trend-reports/copd-trend-report.pdf. Published 2013. Accessed September 26, 2013.
- 3.Hoyert DL, Xu J. Deaths: preliminary data for 2011. Natl Vital Stat Rep. 2012;61(6):1-51. [PubMed] [Google Scholar]
- 4.Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32(4):962-969. [DOI] [PubMed] [Google Scholar]
- 5.Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33(5):1165-1185. [DOI] [PubMed] [Google Scholar]
- 6.Wouters EF. Economic analysis of the Confronting COPD survey: an overview of results. Respir Med. 2003;97(suppl C):S3-S14. [DOI] [PubMed] [Google Scholar]
- 7.Deb P, Manning WG, Norton EC. Modeling health care costs and counts. Paper presented at: iHEA World Congress; July 7-10, 2013; Sidney, Australia. http://harrisschool.uchicago.edu/sites/default/files/iHEA_Sydney_minicourse.pdf. Accessed August 1, 2013.
- 8.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12(2):308-331. [Google Scholar]
- 9.Baty F, Putora PM, Isenring B, Blum T, Brutsche M. Comorbidities and burden of COPD: a population based case-control study. PLoS One. 2013;8(5):e63285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin PJ, Shaya FT, Scharf SM. Economic implications of comorbid conditions among Medicaid beneficiaries with COPD. Respir Med. 2010;104(5):697-704. [DOI] [PubMed] [Google Scholar]
- 11.Simon-Tuval T, Scharf SM, Maimon N, Bernhard-Scharf BJ, Reuveni H, Tarasiuk A. Determinants of elevated healthcare utilization in patients with COPD. Respir Res. 2011;12:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavailles A, Brinchault-Rabin G, Dixmier A, et al. Comorbidities of COPD. Eur Respir Rev. 2013;22(130):454-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sin DD, Man SF. Chronic obstructive pulmonary disease as a risk factor for cardiovascular morbidity and mortality. Proc Am Thorac Soc. 2005;2(1):8-11. [DOI] [PubMed] [Google Scholar]
- 14.Ornek T, Tor M, Altın R, et al. Clinical factors affecting the direct cost of patients hospitalized with acute exacerbation of chronic obstructive pulmonary disease. Int J Med Sci. 2012;9(4):285-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chambellan A, Chailleux E, Similowski T; ANTADIR Observatory Group. Prognostic value of the hematocrit in patients with severe COPD receiving long-term oxygen therapy. Chest. 2005;128(3):1201-1208. [DOI] [PubMed] [Google Scholar]
- 16.Mapel DW, Marton JP. Prevalence of renal and hepatobiliary disease, laboratory abnormalities, and potentially toxic medication exposures among persons with COPD. Int J Chron Obstruct Pulmon Dis. 2013;8:127-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Gestel YR, Chonchol M, Hoeks SE, et al. Association between chronic obstructive pulmonary disease and chronic kidney disease in vascular surgery patients. Nephrol Dial Transplant. 2009;24(9):2763-2767. [DOI] [PubMed] [Google Scholar]
- 18.Mapel D. Renal and hepatobiliary dysfunction in chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2014;20(2):186-193. [DOI] [PubMed] [Google Scholar]
- 19.Nakawah MO, Hawkins C, Barbandi F. Asthma, chronic obstructive pulmonary disease (COPD), and the overlap syndrome. J Am Board Fam Med. 2013;26(4):470-477. [DOI] [PubMed] [Google Scholar]
- 20.Blanchette CM, Broder M, Ory C, Chang E, Akazawa M, Dalal AA. Cost and utilization of COPD and asthma among insured adults in the US. Curr Med Res Opin. 2009;25(6):1385-1392. [DOI] [PubMed] [Google Scholar]
- 21.Ford ES. Hospital discharges, readmissions, and ED visits for COPD or bronchiectasis among US adults: findings from the Nationwide Inpatient Sample 2001-2012 and Nationwide Emergency Department Sample 2006-2011. Chest. 2015;147(4):989-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Boven JF, Vegter S, van der Molen T, Postma MJ. COPD in the working age population: the economic impact on both patients and government. COPD. 2013;10(6):629-639. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplement