Abstract
Our previous studies showed that anti-β2M monoclonal antibodies (mAbs) have strong and direct apoptotic effects on multiple myeloma (MM) cells, suggesting that anti-β2M mAbs might be developed as a novel therapeutic agent. In this study, we investigated the anti-MM effects of combination treatment with anti-β2M mAbs and bortezomib (BTZ). Our results showed that anti-β2M mAbs enhanced BTZ-induced apoptosis of MM cell lines and primary MM cells. Combination treatment could also induce apoptosis of BTZ-resistant MM cells, and the enhanced effect depended on the surface expression of β2M on MM cells. BTZ up-regulated the expression of autophagy proteins, whereas combination with anti-β2M mAbs inhibited autophagy. Sequence analysis of the promoter region of beclin 1 identified 3 putative NF-κB-binding sites from –615 to –789 bp. BTZ treatment increased, whereas combination with anti-β2M mAbs reduced, NF-κB transcription activities in MM cells, and combination treatment inhibited NF-κB p65 binding to the beclin 1 promoter. Furthermore, anti-β2M mAbs and BTZ combination treatment had anti-MM activities in an established MM mouse model. Thus, our studies provide new insight and support for the clinical development of an anti-β2M mAb and BTZ combination treatment to overcome BTZ drug resistance and improve MM patient survival.
Keywords: multiple myeloma, anti-β2M monoclonal antibody, bortezomib, autophagy, NF-κ p65
INTRODUCTION
Multiple myeloma (MM) is a clonal plasma cell neoplasm that utilizes the bone marrow (BM) microenvironment for survival and proliferation [1–3]. Current MM therapies are rarely curative, and relapse is common. Such failure implies that therapy-resistant, MM-initiating cells exist and that new therapeutics must be developed to target and eradicate these chemoresistant MM cells.
Bortezomib (BTZ) is a proteasome inhibitor used worldwide to treat MM and mantle cell lymphoma [4]. However, adverse effects and drug resistance are emerging as great challenges for its extended application [5]. Cell death and survival are regulated by the crosstalk between apoptosis and autophagy [6], and autophagy activation inhibits apoptosis through reducing caspase cleavage [7, 8]. Recent studies have shown that autophagy activation plays a role in chemotherapy drug resistance in patients with cancer [9]. In particular, BTZ treatment activates autophagy in tumor cells [10, 11]. BTZ-induced autophagy is important in BTZ drug resistance in breast cancer, suggesting that inhibiting autophagy may overcome BTZ-induced drug resistance [9].
Targeted immunotherapy with monoclonal antibodies (mAbs) is an effective and safe cancer treatment. Recent efforts have identified potential therapeutic mAbs by defining alternative or novel MM target antigens, i.e., CD40 [12, 13], interleukin-6 receptor [14], HM1.24 [15, 16], CD74 [17], CD47 [18], TRAIL-R1 [19], CS1 [20], PD-1 [21], as well as by conjugating mAbs with classic or novel drugs to specifically kill MM cells, i.e., CD56-maytansinoid (DM1) [22], CD138-DM1/DM4 [23]. Because most of these antibodies have little activity clinically in myeloma, the development of mAbs with improved cytotoxicity, targeting new and known MM-associated antigens, continues to be an active research area.
β2-microglobulin (β2M) is a part of the major histocompatibility complex (MHC) class I molecule [24]. We recently demonstrated that human β2M is a potential target for MM treatment [25, 26]. Our previous studies showed that anti-β2M mAbs have strong and direct apoptotic effects on MM and other hematological malignancies, with less toxicity to normal tissues and cells [25, 27], suggesting that anti-β2M mAbs might be a novel therapeutic agent for MM. Furthermore, others have reported similar results using an anti-MHC class-1 single-chain Fv diabody or anti-β2M antibodies to induce apoptosis in human MM [28] and other cancers [29, 30].
Here, we examined the anti-MM effects of combination treatment with anti-β2M mAbs and BTZ. Combination treatment inhibited BTZ-induced autophagy and increased MM cell apoptosis to overcome BTZ resistance. These results support the clinical development of anti-β2M mAb and BTZ combination treatment to improve MM patient outcomes.
RESULTS
Anti-β2M mAbs enhance the effects of BTZ on MM cell apoptosis
To investigate the combination effects of anti-β2M mAbs and BTZ, MM cells were cultured in medium with different concentrations of BTZ (0 nM to 40 nM) alone or in combination with anti-β2M mAbs (10 μg/mL) for 24 hours. Annexin-V binding assay showed that BTZ at lower concentrations (5 nM and 10 nM) in combination with the mAbs significantly enhanced apoptosis of ARP-1 (Figure 1A) and MM.1S (Figure 1B) cells. Treatment with high concentrations of BTZ (20 nM and 40 nM) alone had strong anti-MM effects, but combination with the mAbs had no synergistic effects (Figure 1A and 1B; P < 0.01). Next, MM cells were cultured with various anti-β2M mAb concentrations (0 μg/mL to 50 μg/mL), either alone or in combination with a low (5 nM) BTZ concentration for 24 hours. Combination treatment significantly enhanced apoptosis of ARP-1 (Figure 1C) and MM.1S (Figure 1D) cells in an anti-β2M mAb dose-dependent manner (P < 0.01, compared with mAb treatment alone). Combination of anti-β2M mAbs (10 μg/mL) and BTZ (5 nM) was further evaluated in the MM cell lines ARK, ARP-1, MM.1S, and U266 in a 24-hour treatment. Compared to BTZ alone, combination treatment induced enhanced apoptosis by 1.5-fold in all examined MM cell lines (Figure 1E; P < 0.01). In line with these results, after 24-hour treatment, purified primary CD138+ MM cells isolated from 3 patients with MM were more sensitive to the combination treatment than BTZ treatment alone. Two other patients with relapse who had received BTZ were considered as BTZ-resistant. In these MM patient cells, BTZ treatment alone was ineffective whereas combination with anti-β2M mAbs increased apoptosis (Figure 1F, patients 4 and 5). Taken together, these results demonstrate that anti-β2M mAbs combined with BTZ is more effective against MM cells than BTZ treatment alone.
Figure 1. Anti-β2M mAbs and BTZ combination treatment in MM cells.
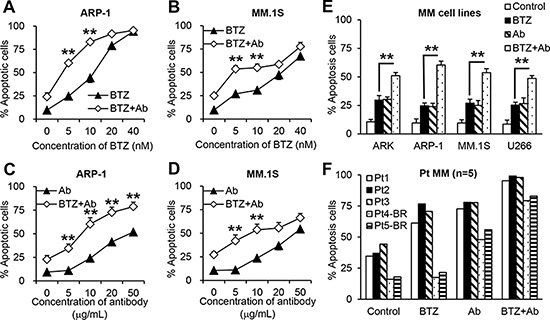
10 μg/mL anti-β2M mAbs were combined with various concentrations of BTZ in ARP-1. (A) and MM.1S (B) cells. 5 nM BTZ combined with various concentrations of anti-β2M mAbs in ARP-1 (C) and MM.1S (D) cells. (E) Anti-β2M mAbs combined with BTZ in different MM cell lines. (F) Anti-β2M mAbs combined with BTZ in CD138+ patient (Pt) MM cells isolated from three BTZ-sensitive MM patients and two BTZ-resistant (BR) MM patients. After 24 hours of treatment, cell apoptosis was monitored by annexin-V binding assay. In E and F, 5 nM BTZ and 10 μg/mL anti-β2M mAbs was used. Summarized data from three independent experiments are shown. **P < 0.01.
The Chou-Talalay combination index (CI) offers quantitative definitions for additive effect (CI = 1), synergism (CI < 1), and antagonism (CI > 1) in drug combinations. We applied the CI-isobol equation to study drug interactions between BTZ and anti-β2M mAbs. As shown in Supplementary Figure S1, combining BTZ and anti-β2M mAb has a synergistic effect (CI < 1) at a low concentration (fraction affected (fa) < 0.45). Therefore, we used low concentrations of BTZ (5 nM) and anti-β2M mAbs (10 μg/mL) in the following experiments.
The combination of anti-β2M mAbs and BTZ overcomes BTZ resistance
To investigate whether combining anti-β2M mAbs and BTZ enhances the anti-MM effects of BTZ in BTZ-resistant MM cells, we used BTZ-sensitive (KAS-6.wt and OPM-2.wt) and BTZ-resistant (KAS-6.BR and OPM-2.BR) MM cells [31]. First, we confirmed cell sensitivity to BTZ treatment, observing that BTZ treatment induced apoptosis of BTZ-sensitive cells in a dose-dependent manner, but did not induce apoptosis of BTZ-resistant cells (Figure 2A and 2C; P < 0.01). Next, we analyzed apoptosis of BTZ-sensitive and BTZ-resistant MM cells treated with BTZ or anti-β2M mAbs, alone or in combination. After 24-hour treatment, BTZ was effective in BTZ-sensitive cells but not in BTZ-resistant cells, whereas combining BTZ with anti-β2M mAbs induced apoptosis in both BTZ-sensitive and BTZ-resistant cells, and was more efficacious than BTZ treatment alone (Figure 2B and 2D; P < 0.01). These results indicate that combining anti-β2M mAbs with BTZ overcomes BTZ resistance in MM.
Figure 2. Combination of anti-β2M mAbs and BTZ restores the sensitivity of BTZ-resistant MM cells to BTZ treatment.
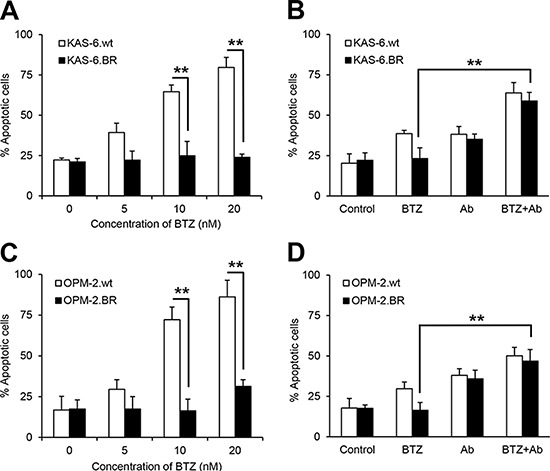
Wild type (wt) or BTZ-resistant (BR) KAS-6 (A and B) and OPM-2 (C and D) cells were cultured in medium with the addition of BTZ or anti-β2M mAbs, singly or in combination, for 24 hours. MM cell apoptosis was monitored by annexin-V binding assay. The percentage of cells undergoing apoptosis increased in a dose-dependent manner in the BTZ-sensitive cells, with no change in the percentage undergoing apoptosis in BTZ-resistant KAS-6 cells (A) and OPM-2 cells (C), treated with various BTZ concentrations. Also shown is the increase in the percentage of cells undergoing apoptosis in either wild type or BTZ-resistant KAS-6 (B) and OPM-2 (D) cells, treated with the combination of BTZ (5 nM) and anti-β2M mAbs (10 μg/mL), compared with cells treated with BTZ only. Summarized data from three independent experiments are shown. **P < 0.01.
Effects of combination treatment depends on MM cell β2M expression
To evaluate the significance of MM cell β2M expression in anti-β2M mAb and BTZ combination treatment-induced MM apoptosis, we used β2M short-hairpin RNA (shRNA)-lentiviral or β2M open reading frame (ORF)-lentiviral systems to knockdown or overexpress β2M, respectively, in MM cells. β2M expression was evaluated by Western blotting, quantitative real-time polymerase chain reaction (qPCR), enzyme-linked immunosorbent assay (ELISA), and flow cytometry. Significant reductions or increases in β2M protein (Supplementary Figure S2A and S2B) and mRNA (Supplementary Figure S2C and S2D) were observed in β2M shRNA- or β2M ORF-expressing ARP-1 and MM.1S cells compared with non-specific shRNA or control vector cells (P < 0.01). In addition, β2M shRNA-expressing ARP-1 cells secreted significantly less soluble β2M whereas β2M ORF-expressing ARP-1 cells secreted more compared with control cells (Supplementary Figure S2E; P < 0.01). Flow cytometry analysis showed a 70% reduction inβ2M shRNA-ARP-1 cells whereas β2M ORF-ARP-1 cells had a 2-fold increase in surface expression of β2M (Supplementary Figure S2F) and HLA-ABC (Supplementary Figure S2G) compared with control cells (P < 0.01).
Next, the effects of anti-β2M mAb or BTZ treatment, singly or in combination, on MM cell apoptosis were examined in β2M-knockdown and β2M-overexpressing MM cells. After 24-hour treatment, anti-β2M mAb treatment alone induced apoptosis of control cells and enhanced apoptosis ofβ2M-overexpressing cells, but reduced apoptosis in β2M-knockdown cells; BTZ treatment alone induced apoptosis in all tested cells (Figure 3). Combination treatment did not enhance apoptosis in β2M-knockdown cells (Figure 3A and 3C) but did in β2M-overexpressing cells (Figure 3B and 3D), as compared with BTZ treated-only cells (P < 0.01). These results indicate that the enhanced effects of combination treatment depend on MM cell β2M expression.
Figure 3. The efficacy of anti-β2M mAbs and BTZ combination treatment in β2M-knockdown and β2M-overexpression MM cells.
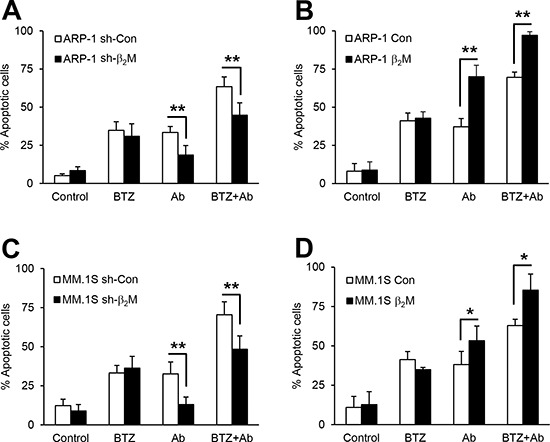
Non-specific (sh-con) or β2M shRNA (sh-β2M)-expressing, and stable control vector (con) or human β2M cDNA (β2M)-expressing ARP-1 (A and B) and MM.1S (C and D) cells were cultured in medium with or without addition of BTZ (5 nM) or anti-β2M mAbs (10 μg/mL), singly or in combination for 24 hours. Apoptosis was reduced in β2M shRNA-expressing ARP-1 (A) and MM.1S (C) cells receiving combination treatment compared with cells treated with BTZ only. Apoptosis was enhanced in β2M-overexpressing ARP-1 (B) and MM.1S (D) cells receiving combination treatment, compared with cells treated with BTZ only. Summarized data from three independent experiments are shown. *P < 0.05, **P < 0.01.
Combination of anti-β2M mAbs and BTZ reduces BTZ-induced autophagy
To further determine the enhanced effects of combination treatment on MM cell apoptosis, we evaluated caspase cascades in MM cells treated for 24 hours. In ARP-1 and MM.1S cells, BTZ or anti-β2M mAb treatment alone resulted in an accumulation of cleaved caspase 9, caspase 3, and PARP, and the combination treatment enhanced the caspase cleavage (Figure 4A). These findings were in line with the annexin-V binding assay results (Figure 1) and suggest that anti-β2M mAbs plus BTZ enhances caspase activation in MM cells.
Figure 4. Anti-β2M mAbs and BTZ combination treatment reduces BTZ-induced autophagy activation.
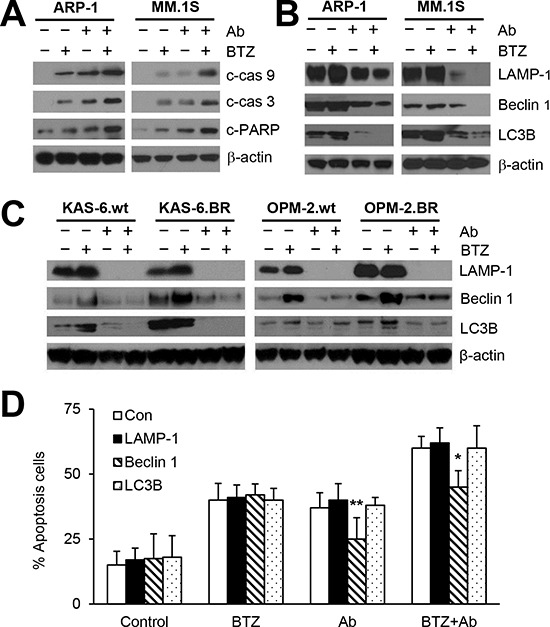
MM cells were cultured in medium with or without addition of BTZ (5 nM) or anti-β2M mAbs (10 μg/mL), singly or in combination for 24 hours. Representative images of Western blot analysis (A) showing the levels of cleaved caspase 9 (c-cas9), caspase 3 (c-cas3), and PARP (c-PARP) in ARP-1 and MM.1S cells. Representative images of Western blot analysis showing the levels of the autophagy proteins LAMP-1, Beclin-1, and LC3B in (B) ARP-1 and MM.1S cells and (C) KAS-6.wt, KAS-6.BR, OPM-2.wt, and OPM-2.BR cells. (D) Annexin-V binding assay showing that rescuing Beclin 1 but not LC3B or LAMP-1 reduced apoptosis in ARP-1 cells treated with anti-β2M mAbs alone or with mAbs plus BTZ. The experiments were carried out in triplicate. β-actin served as protein loading control. *P < 0.05, **P < 0.01.
Cell death and survival are regulated by the crosstalk between apoptosis and autophagy [32]. Recent studies have shown that autophagy activation plays a role in BTZ drug resistance in patients with cancer [11]. We therefore determined the effects of 24-hour anti-β2M mAb and BTZ combination treatment on autophagy activation. Treatment with BTZ alone up-regulated the expression of autophagy proteins LAMP-1, Beclin 1, and LC3B, whereas treatment with anti-β2M mAbs alone or in combination with BTZ decreased expression in ARP-1 and MM.1S cells (Figure 4B). Next, the effects of anti-β2M mAb or BTZ treatment, singly or in combination for 24 hours, on the expression of autophagy proteins in KAS-6.wt, KAS-6.BR, OPM2.wt, and OPM2.BR cells were examined. As shown in Figure 4C, autophagy protein expression was higher in BTZ-resistant cell lines compared with BTZ-sensitive cell lines. BTZ treatment alone up-regulated the expression of LAMP-1, Beclin 1, and LC3B whereas anti-β2M mAb treatment alone or combined with BZT down-regulated the expression in both BTZ-resistant and -sensitive cell lines. These results indicated that combining anti-β2M mAbs and BTZ overcomes BTZ-induced autophagy in both BTZ-resistant and -sensitive MM cells.
To determine which autophagy proteins mediate BTZ resistance, we rescued LAMP-1, Beclin 1, and LC3B expression in ARP-1 cells by infection with lentivirus containing human LAMP1, Beclin-1, or LC3B ORFs, respectively. After 24-hour treatment, rescuing Beclin 1, but not LC3B or LAMP-1, reduced apoptosis in ARP-1 cells treated with anti-β2M mAbs alone or in combination with BTZ (Figure 4D), indicating that Beclin 1 is responsible for the anti-β2M mAb-induced inhibition of autophagy.
Combination treatment down-regulates autophagy by inhibiting BTZ-activated NF-κB p65 signaling
Constitutive NF-κB activity in cancer cells can induce BTZ resistance [33, 34]. Therefore, we wondered whether anti-β2M mAbs inhibited BTZ-induced autophagy by inhibiting NF-κB signaling. After 24-hour treatment, cytoplasmic and nuclear protein fractions of ARP-1 and MM.1S cells were extracted and detected by Western blotting. As shown in Figure 5A, BTZ treatment alone induced the translocation of NF-κB p65 into nuclei, whereas anti-β2M mAb treatment alone or in combination with BTZ had no such effect. In addition, BTZ treatment alone increased the phosphorylation levels of p65 and IκB-α in ARP-1, MM.1S, OPM-2.wt, and OPM-2.BR cells after 24-hour treatment, whereas anti-β2M mAb treatment alone or in combination with BTZ reduced the levels of phosphorylated p65 and IκB-α (Figure 5B). These results indicate that BTZ alone activates NF-κB signaling, whereas anti-β2M mAb and BTZ combination treatment reduces the signaling.
Figure 5. Anti-β2M mAbs and BTZ combination treatment down-regulates BTZ-induced NF-κB p65 activity.
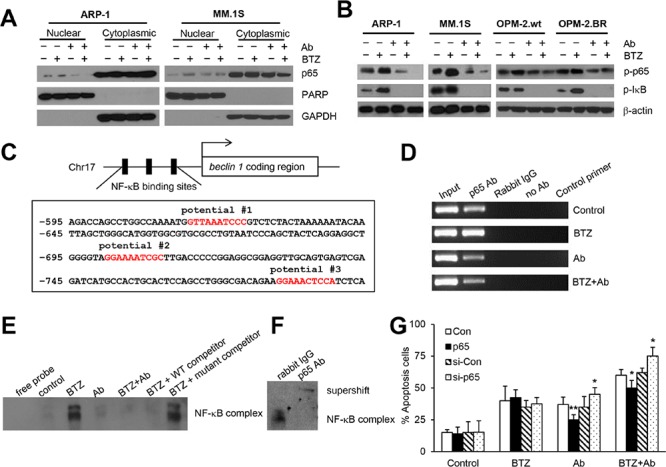
After 24 hours of treatment with BTZ or anti-β2M mAbs, singly or in a combination, MM cells were harvested and the cytoplasmic and nuclear proteins were extracted. (A) Representative images of Western blot analysis showing nuclear and cytoplasmic NF-κB p65 in ARP-1 and MM.1S cells. PARP and GAPDH served as nuclear and cytoplasmic loading controls, respectively. (B) Representative images of Western blot analysis showing phosphorylated NF-κB p65 and phosphorylated IκB-α in ARP-1, MM.1S, OPM-2wt, and OPM-2.BR cells. β-actin served as a protein loading control. (C) Schematic diagram of NF-κB binding sites in the beclin 1 promoter region. The locations of three potential NF-κB binding sites are indicated. (D) Representative ChIP assay images showing the ability of NF-κB p65 to bind to the beclin 1 promoter in BTZ-, mAb- or mAb plus BTZ-treated ARP-1 cells. Chromatin was extracted from the treated cells, and the DNA was precipitated with p65 antibody, then analyzed by qPCR. The input served as an internal control, and samples treated with rabbit IgG, or no antibody, or control primer of non-transcribed region served as negative controls. Nuclear proteins were extracted from ARP-1 cells after 24-hour treatment for EMSA assay. (E) Binding of potential #2 probe was presented after BTZ treatment and reduced in the mAb- or combination treatment. Cold competition was performed using unlabeled probes as indicated. (F) Supershift assay performed with p65 antibody to investigate the BTZ-induced p65 binding complex to beclin 1 promoter. Rabbit IgG served as a negative control. (G) Rescuing or knocking down p65 in ARP-1 cells showing reduced or enhanced apoptosis by annexin-V binding assay. All experiments were carried out in triplicate. *P < 0.05, **P < 0.01.
Combination treatment inhibits BTZ-induced NF-κB p65 binding to the beclin 1 promoter
Sequence analysis of the beclin 1 promoter region showed 3 putative NF-κB binding sites from –615 to –789 bp (Figure 5C). Chromatin immunoprecipitation (ChIP) assay verified that 24-hour treatment with BTZ treatment alone up-regulated p65 binding to the beclin 1 promoter in ARP-1 cells, but anti-β2M mAb treatment alone or in combination with BTZ reduced the binding (Figure 5D). To further confirm that BTZ induced p65 binding to the beclin 1 promoter, electrophoretic mobility shift assay (EMSA) was performed. As shown in Supplementary Figure S3, after 24-hour treatment, potential #2 probe could bind to ARP-1 nuclear proteins, but potential #1 and potential #3 probes could not. Further analysis of the potential #2 probe confirmed an intense band in the BTZ treatment group, but only faint bands in the anti-β2M mAb and combination treatment groups (Figure 5E and Supplementary Figure S3), indicating that BTZ treatment enhanced protein binding to the beclin 1 promoter but anti-β2M mAbs or combination treatment inhibited the binding. For DNA competition experiments, the inducible band could be shifted off completely by unlabeled potential #2 probe, but not by unlabeled mutant potential #2 probe (Figure 5E). After BTZ treatment, p65 antibody supershifted the identified band, indicating that BTZ presence leads to p65 binding of the beclin 1 promoter (Figure 5F). These results indicate that anti-β2M mAbs reduce BTZ-induced autophagy by inhibiting NF-κB p65 binding to the beclin 1 promoter.
In addition, rescuing p65 by lentiviral infection of human p65 ORF treated with anti-β2M mAbs alone or combined with BTZ for 24 hours reduced apoptosis, whereas knocking down p65 by lentiviral infection with human p65 shRNA increased apoptosis of ARP-1 cells (Figure 5G). Taken together, these results indicate that anti-β2M mAbs enhanced BTZ treatment efficacy via an NF-κB–Beclin 1 signaling pathway.
Anti-β2M mAbs enhance the anti-MM effects of BTZ in vivo
We examined the therapeutic effects of anti-β2M mAb and BTZ combination treatment in vivo in a xenograft MM SCID mouse model. To detect the effects of combination treatment, low and nontherapeutic doses of BTZ and anti-β2M mAbs were chosen based on our previous studies [25, 35]. Although treatment with anti-β2M mAbs or BTZ reduced tumor volume (P < 0.05, versus control mice), combination treatment was more efficacious than BTZ alone (Figure 6A and 6B; P < 0.01). Tumor burden was further assessed by measuring serum M-protein levels by ELISA (Figure 6C and 6D; P < 0.01). No change in body weight was found in treated groups (data not shown), suggesting that the combination treatment probably had no toxic effect.
Figure 6. Anti-β2M mAbs enhance anti-MM effects of BTZ in vivo.
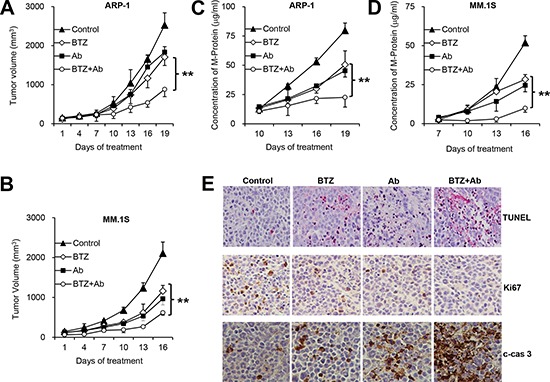
Shown are tumor volumes (A, B) and M-protein levels (C, D) in ARP-1 or MM.1S tumor-bearing mice, respectively (n = 4), treated with mouse IgG1 or DMSO (control), BTZ, anti-β2M mAbs (Ab), or the combination of BTZ and anti-β2M mAbs (BTZ+Ab). ARP-1 or MM.1S cells were subcutaneously injected into SCID mice. At 3 to 4 weeks after MM cell injection, mice were intraperitoneally injected with BTZ (0.1 mg/kg) or subcutaneously around tumors with anti-β2M mAbs (0.6 mg/kg), singly or in combination, every 3 days for 3 weeks. Tumor volumes were measured every 3 days after treatment. The level of circulating human kappa or lambda chain in mouse serum was measured by ELISA. (E) Representative images of in situ TUNEL assay and immunohistochemistry of Ki67 and cleaved caspase 3 (c-cas 3) showing MM tumor cell apoptosis and proliferation. **P < 0.01.
Greater numbers of apoptotic tumor cells were detected by TdT-mediated dUTP nick-end labeling (TUNEL) assay in ARP-1 tumor-bearing mice treated with BTZ or anti-β2M mAbs, compared with mice treated with DMSO or mouse IgG1. Anti-β2M mAb and BTZ combination treatment showed additive effects on induction of MM cell apoptosis compared with treatment with BTZ alone (Figure 6E). Immunohistochemistry in ARP-1 tumor-bearing mice revealed that cells positive for Ki67 decreased after combination treatment, and cells positive for cleaved caspase 3 increased after combination treatment, compared with BTZ treatment alone (Figure 6E). These data indicate that combination of anti-β2M mAbs and BTZ enhances BTZ's therapeutic effects against MM in vivo.
DISCUSSION
Chemotherapy is the most effective treatment for MM currently. Several new drugs have been developed to prolong patient survival [36, 37]. However, the application of these drugs, such as BTZ, usually induces drug resistance, and quick relapse is common [38, 39]. mAbs are emerging as a major new treatment that confers great benefits [40]. In this study, we determined that the combination of anti-β2M mAbs and BTZ was more effective against MM than either agent alone. More importantly, we found that anti-β2M mAbs overcome BTZ resistance by inhibiting BTZ-induced autophagy.
Anti-β2M mAbs enhanced the anti-MM effects of BTZ in a panel of established human MM cell lines and primary MM cells from patients. These findings indicate the potential of anti-β2M mAbs and BTZ combination treatment as a therapeutic strategy against MM. Moreover, anti-β2M mAbs re-sensitized BTZ-resistant MM cells to BTZ treatment, and the enhanced effects of the combination treatment correlated with the expression of surface β2M on MM cells. Therefore, combination treatment with anti-β2M mAbs and BTZ has the potential to impact a larger and heterogeneous patient population with β2M-expression, and to be effective in patients with relapse or who develop tumors resistant to conventional treatment with BTZ.
Mechanistic studies showed that the combination of anti-β2M mAbs and BTZ resulted in an accumulation of cleaved caspase 9, caspase 3 and PARP, and inhibition of the autophagy proteins LAMP-1, Beclin 1, and LC3B. Treatment with a low concentration of BTZ had only a minor effect on caspase cleavage but could induce autophagy. Notably, we found that anti-β2M mAbs inhibited BTZ-induced autophagy in a dose-dependent manner (data not shown). Thus, the combination of anti-β2M mAbs and BTZ may provide an approach to overcome BTZ drug resistance through the inhibition of BTZ-induced autophagy.
Recent research demonstrated that BTZ can induce canonical NF-κB activation by down-regulating constitutive IκB-α expression in MM cells [41]. Other studies found that BTZ treatment of primary effusion lymphoma cells failed to inhibit NF-κB activation [42]. In line with these reports, our data showed that BTZ activated NF-κB transcription activity by increasing NF-κB p65 nuclear translocation and p65 phosphorylation in MM cells. The combination of anti-β2M mAbs and BTZ significantly reduced both the NF-κB p65 nuclear translocation and p65 phosphorylation. Other groups have reported novel NF-κB p65 consensus sites in the beclin 1 promoter and demonstrated that NF-κB p65 positively modulated canonical autophagy in various human tumor cell lines [43]. Our ChIP and EMSA assays verified that anti-β2M mAb treatment inhibited BTZ-induced NF-κB p65 binding to the beclin 1 promoter.
The enhanced anti-MM effect of the combination therapy was also found in vivo. Combination treatment with anti-β2M mAbs and BTZ inhibited tumor growth and serum M-protein level compared with either agent alone. These results underscore a potential clinical development strategy by combining anti-β2M mAbs and BTZ to treat MM patients, which could lower the doses of BTZ and anti-β2M mAbs needed while enhancing their anti-tumor effects, and more importantly, reduce BTZ- and anti-β2M mAb-induced toxicity.
As shown in our schematic diagram of signaling pathways (Supplementary Figure S4), BTZ induces caspase cleavage and apoptosis of MM cells, resulting in drug sensitivity to BTZ treatment. However, BTZ could also enhance beclin 1 transcription by increasing NF-κB p65 binding to the beclin 1 promoter, leading to autophagy activation. Activated autophagy inhibits MM cell apoptosis and promotes cell survival, resulting in drug resistance to BTZ treatment (Supplementary Figure S4A). When BTZ is combined with anti-β2M mAbs, NF-κB p65 transcription activities and BTZ-induced autophagy are inhibited, while caspase cleavage and MM cell apoptosis are increased, resulting in re-sensitization of MM cells to BTZ treatment (Supplementary Figure S4B). Thus, our study strongly suggests that anti-β2M mAbs can overcome BTZ drug resistance in patients.
In conclusion, we for the first time demonstrate that anti-β2M mAbs prevent BTZ drug resistance and enhance BTZ anti-MM efficacy by reducing autophagy protein expression via NF-κB signaling, which provides a rationale for combining these drugs to improve patient outcomes in MM. Thus, our studies provide new insight for the clinical development of anti-β2M mAbs to overcome chemotherapy drug resistance and improve MM patient survival.
MATERIALS AND METHODS
Reagents, MM cell lines, and primary MM cells
Anti-β2M mAbs (clone D1) were generated as previously described [25]. Mouse IgG1 (BioLegend) was used as an isotype control. BTZ (PS-341; Millennium) was dissolved in DMSO at 10 mM as a stock solution. Human ARP-1 and ARK cells were established at the University of Arkansas for Medical Sciences from BM aspirates of patients with MM [44], MM.1S was kindly provided by Dr. Steven Rosen of Northwestern University (Chicago, IL), and U266 cells were purchased from the American Type Culture Collection (ATCC). The BTZ-sensitive (wild-type, wt) and BTZ-resistant (BR) MM cell lines KAS-6.wt, KAS-6.BR, OPM-2.wt, and OPM-2.BR were generated by Dr. Robert Z. Orlowski as previously described [31]. Primary CD138+ MM cells were isolated from BM aspirates of MM patients according to approved IRB protocols of The University of Texas MD Anderson Cancer Center and Cleveland Clinic. All cells were cultured in RPMI-1640 medium supplemented with 10% fetal bovine serum and maintained at 37°C with 5% CO2.
Lentiviral infection of MM cells with shRNA and ORF expression clone transfection
MM cells were infected with lentivirus containing human β2M or p65 shRNAs or lentivirus containing human β2M, LAMP1, Beclin-1, LC3B, or p65 ORFs (Genecopoeia) according to the manufacturer's protocol to knockdown or overexpress specific gene, respectively. Non-specific shRNA or control vector was used as controls. Stable cell line screening was performed with 800 μg/mL neomycin (Sigma) for 4 weeks, and positive cells were selected.
Extraction of cytoplasmic and nuclear proteins
MM cell cytoplasmic and nuclear protein fractions were extracted using NE-PER extraction reagents according to the manufacturer's protocol (Pierce Biotechnology). Nuclear protein extracts were used for EMSA. Cytoplasmic and nuclear protein extracts were used for detecting NF-κB p65 by Western blotting. PARP or GAPDH served as a nuclear or cytoplasmic internal control, respectively.
Western blotting
Western blotting was conducted as previously described [25]. Mouse anti-β2M mAbs (Santa Cruz Biotech) were used to detect β2M protein. Rabbit polyclonal antibodies against cleaved caspase 9, cleaved caspase 3, cleaved PARP, LAMP-1, Beclin 1, LC3B, non-phosphorylated p65, phosphorylated p65, phosphorylated IκB-α, GAPDH, PARP, and β-actin were obtained from Cell Signaling Technology.
qPCR
Total RNA was isolated using an RNeasy kit (Qiagen). Total RNA (1 μg) was reverse transcribed using a SuperScript II (Invitrogen) reverse transcriptase PCR kit; 1 μL of the final cDNA was used for qPCR amplification with SYBRGreen using a StepOnePlus real-time PCR system (Applied Biosciences). The primers for amplification were: β2M-F 5′-AAT TGA AAA AGT GGA GCA TTC AGA-3′; β2M-R 5′-GGC TGT GAC AAA GTC ACA TGG TT-3′; GAPDH-F 5′-CAC TCC TCC ACC TTT GAC G-3′; and GAPDH-R 5′-ACC ACC CTG TTG CTG TAG C-3′. Gene expression levels were normalized to GAPDH levels.
Analysis of surface β2M and HLA-ABC and cell apoptosis by flow cytometry
APC-conjugated mAbs against human β2M, HLA-ABC, and isotype control were obtained from BioLegend. An apoptosis assay was performed as previously described [25]. FITC-labeled annexin-V antibody and propidium iodide (PI) were purchased from Life Technologies. Data were acquired with a flow cytometer (FACSCalibur; BD Biosciences).
ELISA
Cell culture supernatants were collected, and secreted β2M was quantified with a human β2M Quantikine IVD ELISA Kit (R&D Systems). Serum M-protein levels were measured in SCID mice injected with ARP-1 by using the Human Kappa ELISA Kit or MM.1S cells using the Human Lambda ELISA Kit (Bethyl Laboratories).
ChIP assay
ChIP assay was performed with a ChIP assay kit (Millipore) according to the manufacturer's instructions. Chromatin was extracted from ARP-1 cells. Anti-NF-κB p65 antibody and isotype control (Cell Signaling Technology) were used for the chromatin immunoprecipitation. The precipitated DNA was analyzed by qPCR with the following primer sets for the region surrounding the NF-κB binding sites at the beclin 1 promoter: F 5′-AGA CCA GCC TGG CCA AAA TGG T-3′ and R 5′-TGA GAT GGA GTT TCC TTC TGT CG-3′. Values were subtracted from control IgG values and normalized to corresponding input control.
EMSA
Probes were labeled at the 3′ end with biotin (Biotin 3′ End DNA Labeling Kit; Pierce Biotechnology), following the manufacturer's instructions. Oligonucleotides used as probe or competitor were synthesized as: potential #1, 5′-AAA TGG TTA AAT CCC GTC TCT A-3′; potential #2, 5′-GGG TAG GAA AAT CGC TTG ACC C-3′; potential #2 mutant, 5′-GGG TAG CAA AAT CCC TTG ACC C-3′; potential #3, 5′-GAC AGA AGG AAA CTC CAT CTC A-3′. EMSA was performed using the LightShift Chemiluminescent EMSA Kit (Pierce Biotechnology). The DNA-protein complexes were separated on 6% native polyacrylamide gels in 0.5% Tris-borate buffer. For DNA competition experiments, a 100-fold molar excess of unlabeled oligonucleotide was added before incubation. For supershift experiments, 2 μL of anti-NF-′B p65 antibody or isotype control was added to the completed binding reaction mixture [45].
In vivo tumor xenograft mouse models
Six-week-old male SCID mice (Jackson Laboratory) were injected subcutaneously in the right flank with 1 × 106 ARP-1 or MM.1S cells. At 3 to 4 weeks later when palpable tumors (5 mm in diameter) developed, mice (n = 4 per group) were intraperitoneally injected with BTZ (0.1 mg/kg), subcutaneously injected around tumors with anti-β2M mAbs (0.6 mg/kg), either singly or in combination every 3 days for 3 weeks. Control mice were injected with equal amounts of mouse IgG1 or DMSO. Tumors were measured every 3 days with calipers, and tumor volumes (mm3) were calculated as (width2 × length)/2. Mice were humanely sacrificed when moribund or when subcutaneous tumors reached 15 mm in diameter. All mice were maintained in facilities accredited by the American Association of Laboratory Animal Care, and the studies were approved by the Institutional Animal Care and Use Committees of The University of Texas MD Anderson Cancer Center and Cleveland Clinic.
In situ apoptosis assay and immunohistochemistry
In situ tumor cell apoptosis was determined by using a TUNEL assay kit (Boehringer–Mannheim). Immunohistochemistry was conducted as previously described [46]. Ki67 and cleaved caspase 3 expression were detected using specific antibodies (Cell Signaling Technology). Sectioned tumor tissue was embedded in paraffin. Three slides from each treatment group were evaluated. Six fields were arbitrarily selected for examination, using a defined rectangular field area at × 200 magnification, and positive staining cells were counted in each field.
Statistical analysis
The Student's t-test was used to compare various experimental groups. A P value < 0.05 was considered statistically significant. Unless otherwise indicated, the values provided are means and standard deviations (SD).
SUPPLEMENTARY FIGURES
Acknowledgments
We thank The University of Texas MD Anderson Cancer Center and Cleveland Clinic Myeloma Tissue Bank for providing patient samples. This work was supported by funds from the Center for Targeted Therapy at The University of Texas MD Anderson Cancer Center (Q. Yi), grants from the National Cancer Institute R01 CA138402, R01 CA138398, R01 CA163881, and P50 CA142509 (Q. Yi), and K99/R00 CA137158 (J. Yang), the Leukemia and Lymphoma Society (Q. Yi), the Multiple Myeloma Research Foundation (Q. Yi), the Commonwealth Foundation for Cancer Research (Q. Yi), American Society of Hematology (J. Yang), and the National Natural Science Foundation of China Grant No. 81470356 (J. Yang).
Footnotes
Authorship
Contribution: MZ, QY, and JY initiated the work, designed the experiments, and wrote the paper. MZ, JH, ZL, YL, YZ, and HLi performed the experiments and statistical analyses. JX, HLiu, JQ, RO, and LK provided samples and critical suggestions.
CONFLICT OF INTEREST
The authors declare no competing financial interests.
REFERENCES
- 1.Yaccoby S, Barlogie B, Epstein J. Primary myeloma cells growing in SCID-hu mice: a model for studying the biology and treatment of myeloma and its manifestations. Blood. 1998;92:2908–2913. [PubMed] [Google Scholar]
- 2.Kirshner J, Thulien KJ, Martin LD, Debes Marun C, Reiman T, Belch AR, Pilarski LM. A unique three-dimensional model for evaluating the impact of therapy on multiple myeloma. Blood. 2008;112:2935–2945. doi: 10.1182/blood-2008-02-142430. [DOI] [PubMed] [Google Scholar]
- 3.Kyle RA, Rajkumar SV. Multiple myeloma. N Engl J Med. 2004;351:1860–1873. doi: 10.1056/NEJMra041875. [DOI] [PubMed] [Google Scholar]
- 4.Cao B, Li J, Mao X. Dissecting bortezomib: development, application, adverse effects and future direction. Curr Pharm Des. 2013;19:3190–3200. doi: 10.2174/13816128113199990338. [DOI] [PubMed] [Google Scholar]
- 5.Chen D, Frezza M, Schmitt S, Kanwar J, Dou QP. Bortezomib as the first proteasome inhibitor anticancer drug: current status and future perspectives. Curr Cancer Drug Targets. 2011;11:239–253. doi: 10.2174/156800911794519752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rubinstein AD, Kimchi A. Life in the balance—a mechanistic view of the crosstalk between autophagy and apoptosis. J Cell Sci. 2012;125:5259–5268. doi: 10.1242/jcs.115865. [DOI] [PubMed] [Google Scholar]
- 7.Gordy C, He YW. The crosstalk between autophagy and apoptosis: where does this lead? Protein Cell. 2012;3:17–27. doi: 10.1007/s13238-011-1127-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Djavaheri-Mergny M, Maiuri MC, Kroemer G. Cross talk between apoptosis and autophagy by caspase-mediated cleavage of Beclin 1. Oncogene. 2010;29:1717–1719. doi: 10.1038/onc.2009.519. [DOI] [PubMed] [Google Scholar]
- 9.Rzymski T, Milani M, Singleton DC, Harris AL. Role of ATF4 in regulation of autophagy and resistance to drugs and hypoxia. Cell Cycle. 2009;8:3838–3847. doi: 10.4161/cc.8.23.10086. [DOI] [PubMed] [Google Scholar]
- 10.Selimovic D, Porzig BB, El-Khattouti A, Badura HE, Ahmad M, Ghanjati F, Santourlidis S, Haikel Y, Hassan M. Bortezomib/proteasome inhibitor triggers both apoptosis and autophagy-dependent pathways in melanoma cells. Cell Signal. 2013;25:308–318. doi: 10.1016/j.cellsig.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Jia L, Gopinathan G, Sukumar JT, Gribben JG. Blocking autophagy prevents bortezomib-induced NF-kappaB activation by reducing I-kappaBalpha degradation in lymphoma cells. PloS One. 2012;7:e32584. doi: 10.1371/journal.pone.0032584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tai YT, Li X, Tong X, Santos D, Otsuki T, Catley L, Tournilhac O, Podar K, Hideshima T, Schlossman R, Richardson P, Munshi NC, Luqman M, Anderson KC. Human anti-CD40 antagonist antibody triggers significant antitumor activity against human multiple myeloma. Cancer Res. 2005;65:5898–5906. doi: 10.1158/0008-5472.CAN-04-4125. [DOI] [PubMed] [Google Scholar]
- 13.Tai YT, Li XF, Catley L, Coffey R, Breitkreutz I, Bae J, Song W, Podar K, Hideshima T, Chauhan D, Schlossman R, Richardson P, Treon SP, Grewal IS, Munshi NC, Anderson KC. Immunomodulatory drug lenalidomide (CC-5013, IMiD3) augments anti-CD40 SGN-40-induced cytotoxicity in human multiple myeloma: clinical implications. Cancer Res. 2005;65:11712–11720. doi: 10.1158/0008-5472.CAN-05-1657. [DOI] [PubMed] [Google Scholar]
- 14.Tassone P, Galea E, Forciniti S, Tagliaferri P, Venuta S. The IL-6 receptor super-antagonist Sant7 enhances antiproliferative and apoptotic effects induced by dexamethasone and zoledronic acid on multiple myeloma cells. Int J Oncol. 2002;21:867–873. [PubMed] [Google Scholar]
- 15.Ozaki S, Kosaka M, Wakahara Y, Ozaki Y, Tsuchiya M, Koishihara Y, Goto T, Matsumoto T. Humanized anti-HM1.24 antibody mediates myeloma cell cytotoxicity that is enhanced by cytokine stimulation of effector cells. Blood. 1999;93:3922–3930. [PubMed] [Google Scholar]
- 16.Tai YT, Horton HM, Kong SY, Pong E, Chen H, Cemerski S, Bernett MJ, Nguyen DH, Karki S, Chu SY, Lazar GA, Munshi NC, Desjarlais JR, Anderson KC, Muchhal US. Potent in vitro and in vivo activity of an Fc-engineered humanized anti-HM1.24 antibody against multiple myeloma via augmented effector function. Blood. 2012;119:2074–2082. doi: 10.1182/blood-2011-06-364521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stein R, Mattes MJ, Cardillo TM, Hansen HJ, Chang CH, Burton J, Govindan S, Goldenberg DM. CD74: a new candidate target for the immunotherapy of B-cell neoplasms. Clin Cancer Res. 2007;13:5556s–5563s. doi: 10.1158/1078-0432.CCR-07-1167. [DOI] [PubMed] [Google Scholar]
- 18.Kim D, Wang J, Willingham SB, Martin R, Wernig G, Weissman IL. Anti-CD47 antibodies promote phagocytosis and inhibit the growth of human myeloma cells. Leukemia. 2012;26:2538–2545. doi: 10.1038/leu.2012.141. [DOI] [PubMed] [Google Scholar]
- 19.Menoret E, Gomez-Bougie P, Geffroy-Luseau A, Daniels S, Moreau P, Le Gouill S, Harousseau JL, Bataille R, Amiot M, Pellat-Deceunynck C. Mcl-1L cleavage is involved in TRAIL-R1- and TRAIL-R2-mediated apoptosis induced by HGS-ETR1 and HGS-ETR2 human mAbs in myeloma cells. Blood. 2006;108:1346–1352. doi: 10.1182/blood-2005-12-007971. [DOI] [PubMed] [Google Scholar]
- 20.Tai YT, Dillon M, Song W, Leiba M, Li XF, Burger P, Lee AI, Podar K, Hideshima T, Rice AG, van Abbema A, Jesaitis L, Caras I, Law D, Weller E, Xie W, et al. Anti-CS1 humanized monoclonal antibody HuLuc63 inhibits myeloma cell adhesion and induces antibody-dependent cellular cytotoxicity in the bone marrow milieu. Blood. 2008;112:1329–1337. doi: 10.1182/blood-2007-08-107292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenblatt J, Glotzbecker B, Mills H, Vasir B, Tzachanis D, Levine JD, Joyce RM, Wellenstein K, Keefe W, Schickler M, Rotem-Yehudar R, Kufe D, Avigan D. PD-1 blockade by CT-011, anti-PD-1 antibody, enhances ex vivo T-cell responses to autologous dendritic cell/myeloma fusion vaccine. J Immunother. 2011;34:409–418. doi: 10.1097/CJI.0b013e31821ca6ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tassone P, Gozzini A, Goldmacher V, Shammas MA, Whiteman KR, Carrasco DR, Li C, Allam CK, Venuta S, Anderson KC, Munshi NC. In vitro and in vivo activity of the maytansinoid immunoconjugate huN901-N2′-deacetyl- N2′-(3-mercapto-1-oxopropyl)-maytansine against CD56+ multiple myeloma cells. Cancer Res. 2004;64:4629–4636. doi: 10.1158/0008-5472.CAN-04-0142. [DOI] [PubMed] [Google Scholar]
- 23.Ikeda H, Hideshima T, Fulciniti M, Lutz RJ, Yasui H, Okawa Y, Kiziltepe T, Vallet S, Pozzi S, Santo L, Perrone G, Tai YT, Cirstea D, Raje NS, Uherek C, Dalken B, et al. The monoclonal antibody nBT062 conjugated to cytotoxic Maytansinoids has selective cytotoxicity against CD138-positive multiple myeloma cells in vitro and in vivo. Clin Cancer Res. 2009;15:4028–4037. doi: 10.1158/1078-0432.CCR-08-2867. [DOI] [PubMed] [Google Scholar]
- 24.Bjorkman PJ, Burmeister WP. Structures of two classes of MHC molecules elucidated: crucial differences and similarities. Curr Opin Struct Biol. 1994;4:852–856. doi: 10.1016/0959-440x(94)90266-6. [DOI] [PubMed] [Google Scholar]
- 25.Yang J, Qian J, Wezeman M, Wang S, Lin P, Wang M, Yaccoby S, Kwak LW, Barlogie B, Yi Q. Targeting beta2-microglobulin for induction of tumor apoptosis in human hematological malignancies. Cancer Cell. 2006;10:295–307. doi: 10.1016/j.ccr.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 26.Zhang M, Qian J, Lan Y, Lu Y, Li H, Hong B, Zheng Y, He J, Yang J, Yi Q. Anti-beta(2)M monoclonal antibodies kill myeloma cells via cell- and complement-mediated cytotoxicity. Int J Cancer. 2014;135:1132–1141. doi: 10.1002/ijc.28745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang J, Cao Y, Hong S, Li H, Qian J, Kwak LW, Yi Q. Human-like mouse models for testing the efficacy and safety of anti-beta2-microglobulin monoclonal antibodies to treat myeloma. Clin Cancer Res. 2009;15:951–959. doi: 10.1158/1078-0432.CCR-08-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sekimoto E, Ozaki S, Ohshima T, Shibata H, Hashimoto T, Abe M, Kimura N, Hattori K, Kawai S, Kinoshita Y, Yamada-Okabe H, Tsuchiya M, Matsumoto T. A single-chain Fv diabody against human leukocyte antigen-A molecules specifically induces myeloma cell death in the bone marrow environment. Cancer Res. 2007;67:1184–1192. doi: 10.1158/0008-5472.CAN-06-2236. [DOI] [PubMed] [Google Scholar]
- 29.Nomura T, Huang WC, Seo S, Zhau HE, Mimata H, Chung LW. Targeting beta2-microglobulin mediated signaling as a novel therapeutic approach for human renal cell carcinoma. J Urol. 2007;178:292–300. doi: 10.1016/j.juro.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Huang WC, Wu D, Xie Z, Zhau HE, Nomura T, Zayzafoon M, Pohl J, Hsieh CL, Weitzmann MN, Farach-Carson MC, Chung LW. beta2-microglobulin is a signaling and growth-promoting factor for human prostate cancer bone metastasis. Cancer Res. 2006;66:9108–9116. doi: 10.1158/0008-5472.CAN-06-1996. [DOI] [PubMed] [Google Scholar]
- 31.Kuhn DJ, Berkova Z, Jones RJ, Woessner R, Bjorklund CC, Ma W, Davis RE, Lin P, Wang H, Madden TL, Wei C, Baladandayuthapani V, Wang M, Thomas SK, Shah JJ, Weber DM, et al. Targeting the insulin-like growth factor-1 receptor to overcome bortezomib resistance in preclinical models of multiple myeloma. Blood. 2012;120:3260–3270. doi: 10.1182/blood-2011-10-386789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Driscoll JJ, Chowdhury RD. Molecular crosstalk between the proteasome, aggresomes and autophagy: translational potential and clinical implications. Cancer Lett. 2012;325:147–154. doi: 10.1016/j.canlet.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 33.Markovina S, Callander NS, O’Connor SL, Kim J, Werndli JE, Raschko M, Leith CP, Kahl BS, Kim K, Miyamoto S. Bortezomib-resistant nuclear factor-kappaB activity in multiple myeloma cells. Mol Cancer Res. 2008;6:1356–1364. doi: 10.1158/1541-7786.MCR-08-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang DT, Young KH, Kahl BS, Markovina S, Miyamoto S. Prevalence of bortezomib-resistant constitutive NF-kappaB activity in mantle cell lymphoma. Mol Cancer. 2008;7:40. doi: 10.1186/1476-4598-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zheng Y, Yang J, Qian J, Zhang L, Lu Y, Li H, Lin H, Lan Y, Liu Z, He J, Hong S, Thomas S, Shah J, Baladandayuthapani V, Kwak LW, Yi Q. Novel phosphatidylinositol 3-kinase inhibitor NVP-BKM120 induces apoptosis in myeloma cells and shows synergistic anti-myeloma activity with dexamethasone. J Mol Med. 2012;90:695–706. doi: 10.1007/s00109-011-0849-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Suzuki K. Current therapeutic strategy for multiple myeloma. Jap J Clin Oncol. 2013;43:116–124. doi: 10.1093/jjco/hys215. [DOI] [PubMed] [Google Scholar]
- 37.Chou T. Multiple myeloma: recent progress in diagnosis and treatment. J Clin Exp Hematopathol. 2012;52:149–159. doi: 10.3960/jslrt.52.149. [DOI] [PubMed] [Google Scholar]
- 38.Romano A, Conticello C, Di Raimondo F. Bortezomib for the treatment of previously untreated multiple myeloma. Immunotherapy. 2013;5:327–352. doi: 10.2217/imt.13.14. [DOI] [PubMed] [Google Scholar]
- 39.Lawasut P, Chauhan D, Laubach J, Hayes C, Fabre C, Maglio M, Mitsiades C, Hideshima T, Anderson KC, Richardson PG. New proteasome inhibitors in myeloma. Curr Hematol Malig Rep. 2012;7:258–266. doi: 10.1007/s11899-012-0141-2. [DOI] [PubMed] [Google Scholar]
- 40.Allegra A, Penna G, Alonci A, Russo S, Greve B, Innao V, Minardi V, Musolino C. Monoclonal antibodies: potential new therapeutic treatment against multiple myeloma. Eur J Haematol. 2013;90:441–468. doi: 10.1111/ejh.12107. [DOI] [PubMed] [Google Scholar]
- 41.Hideshima T, Ikeda H, Chauhan D, Okawa Y, Raje N, Podar K, Mitsiades C, Munshi NC, Richardson PG, Carrasco RD, Anderson KC. Bortezomib induces canonical nuclear factor-kappaB activation in multiple myeloma cells. Blood. 2009;114:1046–1052. doi: 10.1182/blood-2009-01-199604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sarosiek KA, Cavallin LE, Bhatt S, Toomey NL, Natkunam Y, Blasini W, Gentles AJ, Ramos JC, Mesri EA, Lossos IS. Efficacy of bortezomib in a direct xenograft model of primary effusion lymphoma. Proc Natl Acad Sci U S A. 2010;107:13069–13074. doi: 10.1073/pnas.1002985107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Copetti T, Demarchi F, Schneider C. p6/RelA binds and activates the beclin 1 promoter. Autophagy. 2009;5:858–859. doi: 10.4161/auto.8822. [DOI] [PubMed] [Google Scholar]
- 44.Hardin J, MacLeod S, Grigorieva I, Chang R, Barlogie B, Xiao H, Epstein J. Interleukin-6 prevents dexamethasone-induced myeloma cell death. Blood. 1994;84:3063–3070. [PubMed] [Google Scholar]
- 45.Huang CJ, Bi EG, Hu Y, Deng WW, Tian ZG, Dong C, Hu YJ, Sun B. A novel NF-kappa B binding site controls human granzyme B gene transcription. J Immunol. 2006;176:4173–4181. doi: 10.4049/jimmunol.176.7.4173. [DOI] [PubMed] [Google Scholar]
- 46.Chen S, Zhang M, Ma H, Saiyin H, Shen S, Xi J, Wan B, Yu L. Oligo-microarray analysis reveals the role of cyclophilin A in drug resistance. Cancer Chemother Pharmacol. 2008;61:459–469. doi: 10.1007/s00280-007-0491-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


