Abstract
Epidemiological studies show that patients with type 2 diabetes (T2DM) and individuals with a diabetes-independent elevation in blood glucose have an increased risk for developing dementia, specifically dementia due to Alzheimer’s disease (AD). These observations suggest that abnormal glucose metabolism likely plays a role in some aspects of AD pathogenesis, leading us to investigate the link between aberrant glucose metabolism, T2DM, and AD in murine models. Here, we combined two techniques — glucose clamps and in vivo microdialysis — as a means to dynamically modulate blood glucose levels in awake, freely moving mice while measuring real-time changes in amyloid-β (Aβ), glucose, and lactate within the hippocampal interstitial fluid (ISF). In a murine model of AD, induction of acute hyperglycemia in young animals increased ISF Aβ production and ISF lactate, which serves as a marker of neuronal activity. These effects were exacerbated in aged AD mice with marked Aβ plaque pathology. Inward rectifying, ATP-sensitive potassium (KATP) channels mediated the response to elevated glucose levels, as pharmacological manipulation of KATP channels in the hippocampus altered both ISF Aβ levels and neuronal activity. Taken together, these results suggest that KATP channel activation mediates the response of hippocampal neurons to hyperglycemia by coupling metabolism with neuronal activity and ISF Aβ levels.
Keywords: Endocrinology, Metabolism, Neuroscience
Introduction
The aggregation and subsequent cerebral accumulation of the amyloid-β (Aβ) peptide is a key initiating factor in Alzheimer’s disease (AD), where Aβ aggregation begins approximately 15 years prior to the onset of cognitive symptoms (1, 2). In addition to extracellular Aβ aggregation and subsequently intraneuronal tau accumulation, decreased glucose metabolism also occurs in regions prone to AD pathology during this presymptomatic period. Although both Aβ and tau are central to AD pathogenesis, it is unclear whether glucose dysregulation is an initiator of AD pathology, a secondary consequence of neuronal dysfunction due to Aβ and tau deposition, or both. Recent epidemiological studies demonstrate that individuals with type 2 diabetes (T2DM) are 2–4 times more likely to develop AD (3–5), individuals with elevated blood glucose levels are at an increased risk to develop dementia (5), and those with elevated blood glucose levels have a more rapid conversion from mild cognitive impairment (MCI) to AD (6), suggesting that disrupted glucose homeostasis could play a more causal role in AD pathogenesis. Although several prominent features of T2DM, including increased insulin resistance and decreased insulin production, are at the forefront of AD research (7–10), questions regarding the effects of elevated blood glucose independent of insulin resistance on AD pathology remain largely unexplored. In order to investigate the potential role of glucose metabolism in AD, we combined glucose clamps and in vivo microdialysis as a method to measure changes in brain metabolites in awake, freely moving mice during a hyperglycemic challenge. Our findings suggest that acute hyperglycemia raises interstitial fluid (ISF) Aβ levels by altering neuronal activity, which increases Aβ production. Since cerebral glucose metabolism is tightly linked to neuronal activity (11, 12) and elevated neuronal activity increases Aβ production (13–15), we explored the role of inward rectifying, ATP-sensitive potassium (KATP) channels as one mechanism linking glucose metabolism, neuronal excitability, and ISF Aβ. Our data suggests that KATP channels can mediate the response of hippocampal neurons to elevated blood glucose levels by coupling changes in metabolism with neuronal activity and ISF Aβ.
Results and Discussion
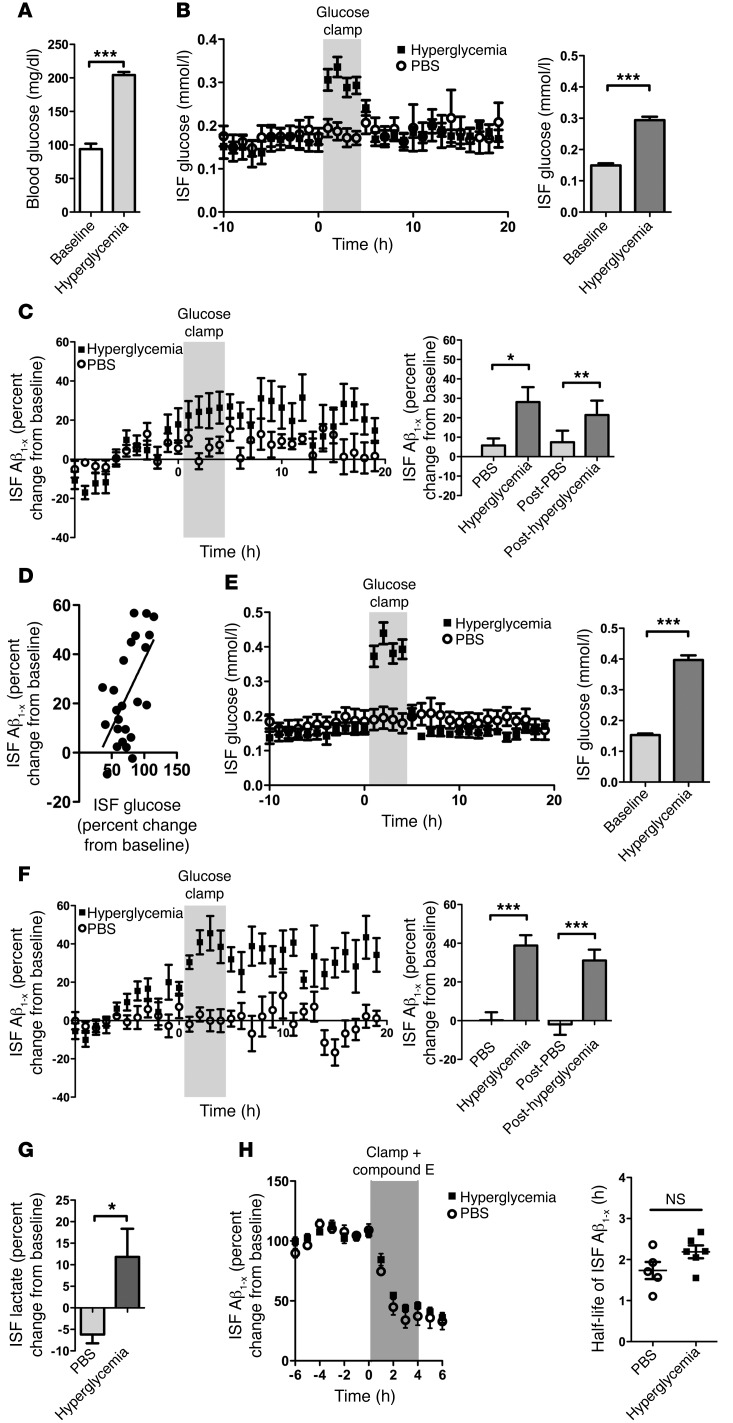
The levels of soluble, monomeric Aβ in the brain determine the likelihood that Aβ will aggregate and lead to toxicity (13, 16). Therefore, we first sought to assess the acute effects of hyperglycemia on the concentration of Aβ within the brain ISF. We coupled glucose clamps (17) with in vivo microdialysis (18) in APPswe/PS1ΔE9 (APP/PS1) mice that were 3 months old, an age prior to the onset of brain Aβ deposition (19). These techniques allowed us to acutely manipulate systemic blood glucose levels in awake, freely moving mice while simultaneously assessing dynamic changes in brain metabolites in hippocampal ISF. During a 4-hour glucose clamp, blood glucose levels were raised from 93.8 ± 8.2 mg/dl to 204.2 ± 4.5 mg/dl, representing a 2.2-fold increase from baseline in 3-month-old APP/PS1 mice (Figure 1A). A comparable effect was seen in WT mice receiving the same metabolic challenge (Supplemental Figure 1; supplemental material available online with this article; doi:10.1172/JCI79742DS1). This elevation in blood glucose resulted in a 1.9-fold increase in hippocampal ISF glucose (Figure 1B). ISF Aβ increased by 24.5% ± 3.8% during the hyperglycemia challenge, an effect that was sustained after euglycemia was restored subsequent to the glucose clamp (Figure 1C). While the effects of glucose on ISF Aβ were variable, ISF glucose correlated with ISF Aβ during hyperglycemia (Pearson’s r = 0.6032; P < 0.01), demonstrating that hippocampal Aβ concentrations are likely modulated by blood glucose levels (Figure 1D).
Figure 1. Hyperglycemia increases ISF glucose and Aβ levels in the APP/PS1 hippocampus in vivo.
(A) Blood glucose levels in 3-month-old APP/PS1 mice (n = 6–8 mice/group) during fasted baseline and hyperglycemic clamp. (B) ISF glucose levels increased from 0.158 ± 0.004 to 0.306 ± 0.011 mmol/l during hyperglycemia in 3-month-old APP/PS1 mice (n = 6–8 mice/group). (C) Hyperglycemia increased ISF Aβ levels by 24.5% ± 3.8% in 3-month-old APP/PS1 mice during and after clamp (n = 6–7 mice/group). (D) ISF Aβ correlates with ISF glucose during hyperglycemia (n = 6 mice, Pearson’s r = 0.6032; P < 0.01). (E) ISF glucose levels increased from 0.153 ± 0.003 to 0.397 ± 0.0149 mmol/l during hyperglycemia in 18-month-old APP/PS1 mice (n = 6–7 mice/group). (F) Hyperglycemia increased ISF Aβ levels by 38.8% ± 5.3% in 18-month-old APP/PS1 mice, during and after glucose clamps (n = 6–7 mice/group). (G) Hyperglycemia increases ISF lactate, a marker of neuronal activity (n = 7 mice/group). (H) Compound E decreases ISF Aβ during hyperglycemia and does not alter ISF Aβ half-life, demonstrating hyperglycemia alters Aβ production, not Aβ clearance. Data represent mean ± SEM. Significance denoted *P < 0.05, **P < 0.01, and ***P < 0.001 using 2-way ANOVA (C and F) or Student’s t tests (A, B, E, G, and H).
Hypothesizing that the presence of Aβ aggregation into amyloid plaques and oligomers promotes localized injury and affects the brain’s response to hyperglycemia, we altered blood glucose levels in mice with significant Aβ plaque burden (Supplemental Figure 2). Using the same approach in 18-month-old APP/PS1 mice where blood glucose was clamped between 150–200 mg/dl, increases in blood glucose raised ISF glucose 2.6-fold from baseline (Figure 1E). Hyperglycemia significantly increased hippocampal ISF Aβ by 38.8% ± 5.3%, with a maximal effect of 45.6% ± 9.0%, which persisted after euglycemia was restored (Figure 1F). The hyperglycemia-dependent increase in ISF Aβ levels was 1.6-fold higher in 18-month-old mice compared with 3-month-old mice, demonstrating that older mice with significant plaque pathology respond differentially to a hyperglycemic insult. Previous studies demonstrated that increased synaptic activity drives Aβ release from an endocytic pool in vivo, resulting in an increase in ISF Aβ but not total tissue Aβ (14, 15, 18). We found that hyperglycemia increased ISF Aβ specifically, while the total amount of Aβ40 and Aβ42 within the brain did not change (Supplemental Figure 3). Due to the astrocyte neuron lactate shuttle, extracellular lactate can be used as a marker of neuronal activity, and previous work shows that it increases in concert with ISF Aβ (13, 20–22). ISF lactate increased during glucose clamps, suggesting hyperglycemia increases both neuronal activity and ISF Aβ (Figure 1G and Supplemental Figure 4). To determine whether elevations in ISF Aβ were due to increased production or decreased clearance of Aβ, we administered compound E, a potent gamma secretase inhibitor, concurrently with hyperglycemia as a means to abolish Aβ production and to measure the rate of ISF Aβ clearance. This showed that the rate of ISF Aβ clearance did not differ in the presence versus the absence of hyperglycemia, illustrating that the hyperglycemia-induced increase in ISF Aβ levels is not due to a significant slowing of Aβ clearance (Figure 1H). Since both T2DM and AD are diseases of aging and Aβ deposition begins about 15 years prior to the onset of dementia due to AD, these findings suggest that poor glycemic control during a presymptomatic period could increase basal neuronal activity, drive Aβ production/release, and instigate or exacerbate Aβ deposition.
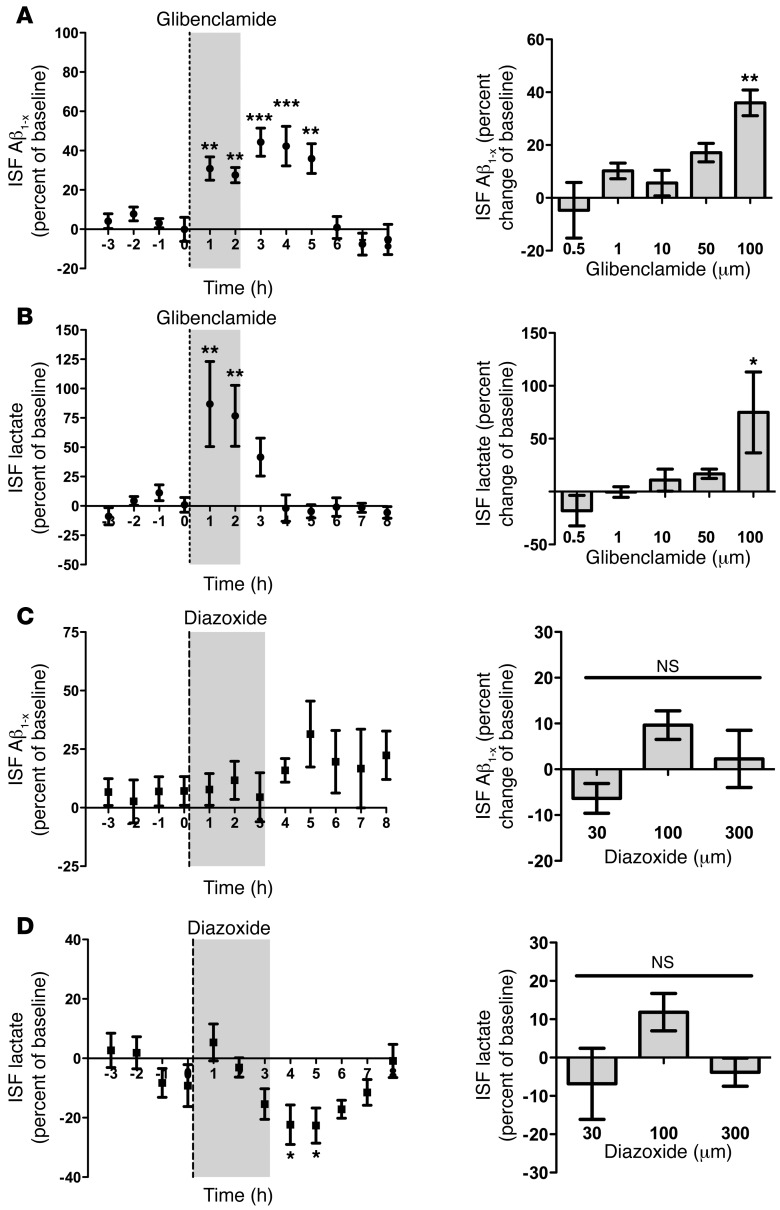
Elevated extracellular glucose levels can evoke rapid changes in neuronal excitability through KATP channels (23, 24). KATP channels are hetero-octameric proteins composed of 4 inner pore-forming subunits (Kir6.1 or Kir6.2) and 4 sulfonylurea receptor (SUR) subunits. Increased glucose concentrations lead to elevations in intracellular ATP, causing KATP channel closure, membrane depolarization, and increased cellular excitability. Although best described for their role in insulin secretion in pancreatic β cells, KATP channels are found on both neurons and astrocytes (25) and can couple cellular metabolism with neuronal activity. To investigate the role of KATP channel activity on glucose-dependent increases in ISF Aβ, we pharmacologically manipulated hippocampal KATP channels under euglycemic and hyperglycemic conditions. We delivered glibenclamide, a KATP channel antagonist, to the APP/PS1 hippocampus via reverse microdialysis and found that it increased ISF Aβ and lactate levels in a dose-dependent manner, with a maximal effect of 36.2% ± 3.2% and 73.3% ± 19.8%, respectively (Figure 2, A and B). These findings illustrate that closure of KATP channels leads to both increased neuronal activity and extracellular concentrations of Aβ (Figure 2, A andB). Conversely, we investigated whether the KATP channel agonists, diazoxide and pinacidil, affect ISF Aβ and lactate levels by opening KATP channels and hyperpolarizing cells (Figure 2, C and D, and Supplemental Figure 5). Although no overall change in ISF Aβ was observed (Figure 2C and Supplemental Figure 5A), diazoxide decreased ISF lactate by 22.5% ± 4.3%, suggesting an inhibitory effect on neuronal activity (Figure 2D). This finding is consistent with previous work, demonstrating that diazoxide decreased action-potential frequency and calcium influx in cultured cortical neurons (26). Together, our findings suggest that KATP channels alter cellular excitability within the hippocampus and that increased cellular excitability via KATP channel activation leads to increased ISF Aβ.
Figure 2. Modulation of hippocampal KATP channels affects ISF Aβ and lactate in vivo.
(A) Glibenclamide, a KATP antagonist, was given via reverse microdialysis and increased ISF Aβ in a dose-dependent manner, with a maximal increase of 36.2% ± 3.2% at 100 μM. The left panel represents a time course of the 100 μM dose, while the right demonstrates the dose-dependent effects of glibenclamide. (B) ISF lactate increased in a dose-dependent manner, with a maximal increase of 73.3-5% ± 19.8%. The left panel represents a time course of the 100 μM dose, while the right illustrates the dose-dependent effects of glibenclamide. (C) Diazoxide, a KATP agonist, did not alter ISF Aβ levels. The left panel demonstrates a time course of the 300 μM dose of diazoxide, where the right shows that diazoxide does not affect ISF Aβ at any dose. (D) Diazoxide (300 μM) decreased ISF lactate by 22.5% ± 4.3% after administration. The left panel demonstrates the time course of the 300 μM dose of diazoxide, while the right shows a dose response of diazoxide. Data represent mean ± SEM. For all analyses, n = 5–7 mice/group per glibenclamide dose and n = 4–5 mice/group per diazoxide dose. *P < 0.05, **P < 0.01, ***P < 0.001 using a 1-way ANOVA.
To determine whether increases in ISF Aβ during hyperglycemia were due to KATP channels, we investigated whether opening KATP channels prevented increases in ISF Aβ during hyperglycemia. Diazoxide was infused into the hippocampus via reverse microdialysis prior to and during hyperglycemia in 18-month-old APP/PS1 mice. ISF Aβ levels did not significantly change prior to and during hyperglycemia in the presence of diazoxide (Figure 3A). In contrast, hyperglycemia alone resulted in a 38.8% ± 5.3% elevation in ISF Aβ, demonstrating that diazoxide blocks the increase in ISF Aβ during hyperglycemia (Figure 3A). Using ISF lactate levels as a measure of neuronal activity, diazoxide treatment blocked the hyperglycemia-dependent increase in ISF lactate levels (Figure 3B). Taken together, these findings demonstrate that KATP channel activation mediates the response of hippocampal neurons to elevated glucose levels by coupling metabolism with neuronal activity and ISF Aβ.
Figure 3. Pharmacological manipulation of KATP channels blocks hyperglycemia-induced increases in ISF Aβ.
(A) In 18-month-old APP/PS1 mice, glucose clamps increase ISF Aβ. However, when diazoxide, a KATP agonist, is given via reverse microdialysis during hyperglycemia, the increase in ISF Aβ is blocked (38.84% ± 3.5% vs. 9.33% ± 2.1% increase). (B) Treatment with diazoxide decreased hippocampal ISF lactate in 18-month-old APP/PS1 mouse brains during hyperglycemia, suggesting decreased neuronal activity coincides with decreased ISF Aβ (11.8% ± 3.6% vs. –4.043% ± 3.4%). Data represent mean ± SEM. For all analyses, n = 6–7 mice/group, *P < 0.05, ***P < 0.001 using 2-way ANOVA.
By combining glucose clamps with in vivo microdialysis, we were able to modulate blood glucose levels in awake, freely moving APP/PS1 mice while simultaneously investigating changes in Aβ, glucose, and lactate within the hippocampal ISF. Our data demonstrate that elevated blood glucose levels affect hippocampal metabolism, neuronal activity, and ISF Aβ concentrations in young mice, lacking any appreciable Aβ plaque load. However, in aged mice with marked Aβ deposition, the effect of hyperglycemia on ISF Aβ is exacerbated, suggesting that age- or pathology-dependent changes result in an alteration of the brain’s response to a metabolic insult. Since extracellular Aβ, and subsequently tau, aggregate in a concentration-dependent manner during the preclinical period of AD while individuals are cognitively normal (27), our findings suggest that repeated episodes of transient hyperglycemia, such as those found in T2DM, could both initiate and accelerate plaque accumulation. Thus, the correlation between hyperglycemia and increased ISF Aβ provides one potential explanation for the increased risk of AD and dementia in T2DM patients or individuals with elevated blood glucose levels. In addition, our work suggests that KATP channels within the hippocampus act as metabolic sensors and couple alterations in glucose concentrations with changes in electrical activity and extracellular Aβ levels. Not only does this offer one mechanistic explanation for the epidemiological link between T2DM and AD, but it also provides a potential therapeutic target for AD. Given that FDA-approved drugs already exist for the modulation of KATP channels and previous work demonstrates the benefits of sulfonylureas for treating animal models of AD (26), the identification of these channels as a link between hyperglycemia and AD pathology creates an avenue for translational research in AD.
Methods
Detailed information can be found in Supplemental Methods.
Statistics.
Statistical analysis using Student’s t tests, 1-way ANOVAs, and 2-way ANOVAs and the appropriate post hoc tests were performed as described in each experiment above. P values ≤ 0.05 were considered significant.
Study approval.
All procedures were carried out in accordance with an approved IACUC protocol from Washington University School of Medicine.
Supplementary Material
Acknowledgments
This work was supported by the following grants, NIH F32 NS080320 (to S.L. Macauley), P01 NS080675 (to M.E. Raichle and D.M. Holtzman), NSF DGE-1143954 (to M. Stanley), and JPB Foundation (to D.M. Holtzman). We would like to thank Eli Lilly for their gift of m266 and 3D6 antibodies.
Footnotes
Conflict of interest: David M. Holtzman cofounded and is on the scientific advisory board of C2N Diagnostics. David M. Holtzman consults for Genentech, AstraZeneca, Neurophage, and Eli Lilly.
Reference information:J Clin Invest. 2015;125(6):2463–2467. doi:10.1172/JCI79742.
References
- 1.Holtzman DM, Morris JC, Goate AM. Alzheimer’s disease: the challenge of the second century. Sci Transl Med. 2011;3(77):77sr1. doi: 10.1126/scitranslmed.3002369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297(5580):353–356. doi: 10.1126/science.1072994. [DOI] [PubMed] [Google Scholar]
- 3.Ott A, Stolk RP, van Harskamp F, Pols HA, Hofman A, Breteler MM. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology. 1999;53(9):1937–1942. doi: 10.1212/WNL.53.9.1937. [DOI] [PubMed] [Google Scholar]
- 4.Huang CC, et al. Diabetes mellitus and the risk of Alzheimer’s disease: a nationwide population-based study. PLoS One. 2014;9(1):e87095. doi: 10.1371/journal.pone.0087095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crane PK, et al. Glucose levels and risk of dementia. N Engl J Med. 2013;369(6):540–548. doi: 10.1056/NEJMoa1215740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morris JK, Vidoni ED, Honea RA, Burns JM, Alzheimer’s Disease Neuroimaging Initiative. Impaired glycemia increases disease progression in mild cognitive impairment. Neurobiol Aging. 2014;35(3):585–589. doi: 10.1016/j.neurobiolaging.2013.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263–S275. doi: 10.3233/JAD-2012-129042. [DOI] [PubMed] [Google Scholar]
- 8.Craft S. Alzheimer disease: Insulin resistance and AD — extending the translational path. Nat Rev Neurol. 2012;8(7):360–362. doi: 10.1038/nrneurol.2012.112. [DOI] [PubMed] [Google Scholar]
- 9.Craft S. Insulin resistance and Alzheimer’s disease pathogenesis: potential mechanisms and implications for treatment. Curr Alzheimer Res. 2007;4(2):147–152. doi: 10.2174/156720507780362137. [DOI] [PubMed] [Google Scholar]
- 10.de la Monte SM. Brain insulin resistance and deficiency as therapeutic targets in Alzheimer’s disease. Curr Alzheimer Res. 2012;9(1):35–66. doi: 10.2174/156720512799015037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sibson NR, Dhankhar A, Mason GF, Rothman DL, Behar KL, Shulman RG. Stoichiometric coupling of brain glucose metabolism and glutamatergic neuronal activity. Proc Natl Acad Sci U S A. 1998;95(1):316–321. doi: 10.1073/pnas.95.1.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belanger M, Allaman I, Magistretti PJ. Brain energy metabolism: focus on astrocyte-neuron metabolic cooperation. Cell Metab. 2011;14(6):724–738. doi: 10.1016/j.cmet.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 13.Bero AW, et al. Neuronal activity regulates the regional vulnerability to amyloid-beta deposition. Nat Neurosci. 2011;14(6):750–756. doi: 10.1038/nn.2801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cirrito JR, et al. Endocytosis is required for synaptic activity-dependent release of amyloid-beta in vivo. Neuron. 2008;58(1):42–51. doi: 10.1016/j.neuron.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cirrito JR, et al. Synaptic activity regulates interstitial fluid amyloid-β levels in vivo. Neuron. 2005;48(6):913–922. doi: 10.1016/j.neuron.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 16.Yan P, et al. Characterizing the appearance and growth of amyloid plaques in APP/PS1 mice. J Neurosci. 2009;29(34):10706–10714. doi: 10.1523/JNEUROSCI.2637-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237(3):E214–E223. doi: 10.1152/ajpendo.1979.237.3.E214. [DOI] [PubMed] [Google Scholar]
- 18.Cirrito JR, et al. In vivo assessment of brain interstitial fluid with microdialysis reveals plaque-associated changes in amyloid-β metabolism and half-life. J Neurosci. 2003;23(26):8844–8853. doi: 10.1523/JNEUROSCI.23-26-08844.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jankowsky JL, et al. Mutant presenilins specifically elevate the levels of the 42 residue β-amyloid peptide in vivo: evidence for augmentation of a 42-specific gamma secretase. Hum Mol Genet. 2004;13(2):159–170. doi: 10.1093/hmg/ddh019. [DOI] [PubMed] [Google Scholar]
- 20.Pellerin L, Magistretti PJ. Glutamate uptake into astrocytes stimulates aerobic glycolysis: a mechanism coupling neuronal activity to glucose utilization. Proc Natl Acad Sci U S A. 1994;91(22):10625–10629. doi: 10.1073/pnas.91.22.10625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uehara T1, Sumiyoshi T, Itoh H, Kurata K. Lactate production and neurotransmitters; evidence from microdialysis studies. Pharmacol Biochem Behav. 2008;90(2):273–281. doi: 10.1016/j.pbb.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 22.Roh JH, et al. Disruption of the sleep-wake cycle and diurnal fluctuation of β-amyloid in mice with Alzheimer’s disease pathology. Sci Transl Med. 2012;4(150):150ra122. doi: 10.1126/scitranslmed.3004291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nichols CG. KATP channels as molecular sensors of cellular metabolism. Nature. 2006;440(7083):470–476. doi: 10.1038/nature04711. [DOI] [PubMed] [Google Scholar]
- 24.Huang CW, Huang CC, Cheng JT, Tsai JJ, Wu SN. Glucose and hippocampal neuronal excitability: role of ATP-sensitive potassium channels. J Neurosci Res. 2007;85(7):1468–1477. doi: 10.1002/jnr.21284. [DOI] [PubMed] [Google Scholar]
- 25.Dunn-Meynell AA, Rawson NE, Levin BE. Distribution and phenotype of neurons containing the ATP-sensitive K+ channel in rat brain. Brain Res. 1998;814(1):41–54. doi: 10.1016/s0006-8993(98)00956-1. [DOI] [PubMed] [Google Scholar]
- 26.Liu D, et al. The KATP channel activator diazoxide ameliorates amyloid-beta and tau pathologies and improves memory in the 3xTgAD mouse model of Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):443–457. doi: 10.3233/JAD-2010-101017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sperling RA, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.