Abstract
There is limited research on the maternal and infant characteristics associated with the timing of solid food introduction. The current study examined how maternal feeding style and infant temperament independently and interactively predicted the age at which infants were introduced to solid food. Data from 115 predominately white, middle-class mothers were collected when infants were 4 and 6 months of age. The timing of solid food introduction was positively correlated with mothers' age, education, breastfeeding at 4 months, self-reported responsiveness to infants' hunger and satiety cues, and negatively correlated with mothers' pre-pregnancy body mass index (BMI), beliefs about feeding infants solid food prior to 6 months of age, and infants' temperamental motor reactivity. When controlling for maternal age, education, pre-pregnancy BMI, and milk feeding method at 4 months, the timing of solid food introduction was negatively predicted by mothers' beliefs about feeding solid food prior to 6 months of age. Exploratory interaction analyses suggested that infant temperament marginally moderated maternal feeding style in predicting the timing of solid food introduction.
Keywords: Solid food introduction, Complementary foods, Feeding style, Infancy, Temperament, Maternal characteristics
Introduction
To support healthy physical and cognitive development, the American Academy of Pediatrics advises exclusive breastfeeding for the first 6 months of life, followed by an additional 6 months or more of breastfeeding while complementary foods (i.e. nutritive substances other than breast milk or formula; hereafter referred to as “solid food”) are introduced (Eidelman & Schanler, 2012). Prior to the 2012 update, solid food introduction was recommended between 4 and 6 months (Gartner & Eidelman, 2005). Despite this recommendation, approximately 40% of infants in the United States are introduced to solid food before 4 months of age (Clayton, Li, Perrine, & Scanlon, 2013; Grummer-Strawn, Scanlon, & Fein, 2008). Even though there are theories and empirical evidence to support a bidirectional relationship between parents and infants (Sameroff, 2009) and that this relationship operates within the feeding context (Birch, 1999; Hughes, Power, Fisher, Mueller, & Nicklas, 2005), few studies have examined how maternal and infant characteristics predict the timing of solid food introduction, either alone or in combination (Jansen, Daniels, & Nicholson, 2012; Patrick, Hennessy, McSpadden, & Oh, 2013). The current study addressed this gap in the literature by examining the influence of maternal feeding style and infant temperament on the age at which infants were introduced to solid food.
Introducing solid food to infants prior to 4 to 6 months of age may be associated with the development of obesity, however the evidence is mixed (Huh, Rifas-Shiman, Taveras, Oken & Gillman, 2011; Moorcroft, Marshall, & McCormick, 2011; Woo et al., 2013). Infants who are introduced to solid foods earlier have been found to consume more energy-dense foods (Robinson et al., 2007), which may promote excess caloric consumption and lead to rapid weight gain (Briefel, Reidy, Karwe, Jankowski, & Hendricks, 2004). Given the high prevalence of infant and childhood obesity (Ogden, Carroll, Kit, & Flegal, 2014), understanding early life factors that may contribute to its development is important (Paul et al., 2009).
One factor shown to be related to the timing of solid food introduction is the type of milk feeding. Previous research has found that mothers who fed formula exclusively or in combination with breast milk were more likely to introduce solid food prior to 4 months than mothers who exclusively breastfed (Armstrong, Abraham, Squair, Brogan, & Merewood, 2014; Clayton et al., 2013; Grummer-Strawn et al., 2008; Kronborg, Foverskov, & Væth, 2014). Maternal feeding style may also influence the timing of solid food introduction and subsequent childhood obesity risk (Faith, Scanlon, Birch, Francis, & Sherry, 2004; Gerards & Kremers, 2015; Ventura & Birch, 2008). Previous studies have found that a responsive feeding style was related to longer breastfeeding duration (Taveras et al., 2004) and later solid food introduction (DiSantis, Hodges, & Orlet Fisher, 2013; Kronborg et al., 2014). Alternatively, controlling feeding styles (e.g., pressuring) have been related to earlier solid food introduction (Brown & Lee, 2013). One purpose of the current study was to extend this research by examining controlling and responsive feeding styles on the timing of solid food introduction beyond that of milk feeding and within the context of maternal demographic and health covariates.
Parent-child relationships are bi-directional, meaning that infant characteristics such as temperament may evoke certain parenting responses and children may respond differently to parenting behaviors (Caspi & Shriner, 2006). In the context of infant feeding, a mother is likely to have pre-existing beliefs about infant feeding (Musher-Eizenman & Kiefner, 2013; Newby, Brodribb, Ware & Davies, 2014), but if her infant responds in a way that is not consistent with those beliefs she may adjust her feeding decisions to meet her child's nutritional needs. Previous research has found that parents of infants who were higher in negative reactivity were less likely to exclusively breastfeed for six months (Niegel, Ystrom, Hagtvet, & Vollrath, 2008) and more likely to respond to infant crying with feeding (Stifter, Anzman-Frasca, Birch, & Voegtline, 2011; McMeekin et al., 2013). Only two studies have specifically considered how infant temperament relates to the timing of solid food introduction and found that parents were more likely to introduce solid foods earlier to infants that were more negative and motorically reactive than infants who were less reactive (Kronborg et al., 2014; Wasser et al., 2011). Mothers of infants who are high in emotional and/or motor reactivity may have more difficulty distinguishing their infants' reactivity from hunger and fullness cues compared to mothers of infants low in these characteristics (McMeekin et al., 2013), but more research is needed to clarify the role of temperament in the decision to begin solid foods (Worobey et al., 2012).
Specific Aims
The first aim of this study was to test the independent effects of maternal feeding style and infant temperament on the timing of solid food introduction above and beyond maternal demographic and health characteristics and milk feeding method at 4 months. The second aim was to explore whether infant temperament moderated the effects of maternal feeding style on the timing of solid food introduction. Based on the previously described literature (Brown & Lee, 2013; DiSantis, et al., 2013; Kronborg et al., 2014) we hypothesized that mothers who endorsed a highly pressuring feeding style would introduce solid food earlier than mothers who reported less pressuring feeding. Our second hypothesis was that mothers who endorsed a highly responsive feeding style would introduce solid food later than mothers who reported less responsive feeding. Lastly, we hypothesized that infants who were higher in negative or motor reactivity would be introduced to solid food earlier than infants lower in these characteristics. Our interaction analyses were exploratory, thus we asked whether the relationship between feeding style and the timing of solid food introduction was moderated by infant temperament.
Methods
Participants
115 mother-infant dyads (54.8% male infants) were recruited through birth announcements and a local community hospital in central Pennsylvania to participate in a longitudinal study on infants' basic needs (e.g., eating, crying, sleeping, and soothing) and emotional and physical development. Inclusion criteria were: Maternal age ≥ 18 years, full-term (≥ 37 weeks) pregnancy that was without complications (e.g., low birth weight), and plans to remain in the area for two years. Self-report survey data and laboratory observation data were collected within two weeks of the infants turning 4, 6, 12, and 18 months of age. At each time point, participants received surveys prior to their scheduled laboratory visits and were instructed to bring the completed questionnaires with them to their laboratory visit. Data for the present study were drawn from the 4- and 6-month maternal self-report surveys with a few noted exceptions. These time points were selected because they were the closest in time to the age at which solid food was introduced to most infants.
The majority of mothers were multiparous (74.8%) and 24.3% of the infants were firstborn children. Participant demographic characteristics reflected the recruitment area. Mothers were an average age of 29.4 years (SD = 4.93; range 19-41) and had an average of 14.67 years of education (SD = 2.05; range 11-20). The most commonly reported race was Caucasian (93.9%), with few others reporting an Asian (3.5%), African American (1.7%) or American Indian/Alaskan Native (0.9%) race. Infant race was similarly distributed. Most mothers (80.9%) were married, some were single (9.6%), or living with a partner (6.1%), and few were divorced or other (3.4%). Family income levels were widely distributed: 10.5% reported earning < $20,000 per year, 25.2% earned $20,000-$40,000, 26.1% earned $40,000-$60,000 per year, 16.5% earned $60,000-$80,000 per year, and 21.7% earned > $80,000 per year.
One extreme outlier was excluded from analyses as the value for the age at which the infant was introduced to solid food was more than four standard deviations above the mean. There were 4 participants without data for the outcome variable, the age at which infants were introduced to solid food. Mothers with incomplete data (4-month infant cry diaries, n = 9; 6-month survey measures, n = 11; maternal pre-pregnancy BMI, n = 14) were not significantly different on any demographic variable or the outcome variable with one exception: Mothers missing BMI data were significantly less educated than mothers for whom we had BMI data (p = .01), but did not differ on the timing of solid food introduction. All other participants had complete data (n = 94). All available data were used in the analyses, with the exception of the hierarchical multiple regression analyses in which only cases with complete data were analyzed.
Measures
Maternal pre-pregnancy BMI
At 4 months, mothers reported their weight in pounds prior to their most recent pregnancy. Trained research assistants collected mothers' heights at the 6-month laboratory visit. BMI was calculated using the standard equation BMI = weight (kg) / (height (m)2).
Baby's Basic Needs Questionnaire (BBNQ)
At 4, 6, and 12 months mothers completed the BBNQ (Stifter, Anzman-Frasca, Birch, & Voegtline, 2011), in which mothers reported their current milk feeding method and the age of their infant if and when mothers had stopped breastfeeding and/or began feeding formula. Mothers' report of milk feeding at 4 months was used to create three dichotomous variables for milk feeding method: breastfeeding, formula feeding, and mixed feeding (i.e. a combination of breast milk and formula). Mothers also reported if and when, in weeks, they had introduced solid food to their infants at each time point, which was the continuous outcome variable (abbreviated as “age introduced solids” in tables and figures). In a few cases where mothers had discrepant reports of the timing of solid food introduction across the 4-, 6-, and/or 12-month time points, mothers' report at the earliest time point was used in the analyses.
Infant/Caregiver Diary
To assess negative reactivity at 4 months, mothers completed diaries of their infants' behavior for three consecutive days (Stifter & Spinrad, 2002) which included soothing grids to indicate what they did to soothe their infants after each cry or fuss episode. To calculate the average number of fussing or crying episodes per day, the total number of soothing grids was summed across days and divided by the number of days for which they completed grids. Mothers who had completed at least two days of grids were used in the analyses. Diaries have a long history of use to assess infant feeding and eating patterns and have been validated by 24-hour audio recordings (Barr, Kramer, Boisjoly, McVey-White, & Pless, 1988; Pinilla & Birch, 1993).
Infant Behavior Questionnaire-Revised (IBQ-R)
At 6 months, mothers completed an infant temperament survey, the IBQ-R (Gartstein & Rothbart, 2003). This widely used 173-item questionnaire asked mothers to rate the relative frequency of specific infant behaviors on a 7-point Likert scale from 1 (“Never”) to 7 (“Always”) in the past 1 to 2 weeks (e.g., “When being dressed or undressed during the last week, how often did the baby smile or laugh?”) Gartstein and Rothbart (2003) demonstrated that the individual items can be grouped into fourteen dimensions of temperament, which can be further grouped into three broad factors. The current study used the dimension Activity Level (Cronbachs's α = .84 in the present sample) as a measure of 6-month motor reactivity and the broad factor Negative Affectivity (Cronbach's α = .72 in the present sample; includes the dimensions: sadness, distress to limitations, fear, and falling reactivity (reversed)) as a measure of 6-month negative reactivity.
Infant Feeding Style Questionnaire (IFSQ)
At 6 months, mothers completed the IFSQ, which is a validated measure of maternal feeding style during infancy (Thompson et al., 2009) that has been used in previous research on infant feeding (DiSantis et al., 2013; Thompson, Adair, & Bentley, 2013). Mothers reported on their infant feeding beliefs and behaviors on a 5-point scale, with beliefs rated from 1 (“Disagree”) to 5 (“Agree”), and behaviors rated from 1 (“Never”) to 5 (“Always”) or non-applicable. The current study included only the maternal feeding style sub-constructs associated with the Pressuring feeding style (i.e. encouraging eating regardless of hunger or satiety cues) and Responsive feeding style (i.e. acknowledging infant hunger and satiety cues and attending to infant during feeding) based on previous research demonstrating that these feeding styles are likely to influence the timing of solid food introduction in combination with infant temperament (Cerniglia et al., 2014; Hagekull et al., 1997; McMeekin et al., 2013; Stifter et al., 2011).
The present study excluded several items that had low response rates in studies of infants less than 6 months of age (Thompson et al., 2009). We calculated the internal consistency of each sub-construct using Cronbach's alpha. Feeding style sub-constructs were eliminated if they were calculated to have a Cronbach's alphas less than .60 in our sample or fewer than two items. The feeding style sub-constructs that met these inclusion criteria were: Pressuring: Finish (seven items; α = .75); Pressuring: Cereal (four items; α = .84; the item “I give/gave my child cereal in the bottle” was excluded to avoid overly inflating the relationship between Pressuring: Cereal and the outcome variable); Pressuring: Soothing (three items; α = .75); and Responsive: Satiety (seven items; α = .67). Pressuring: Finish reflects encouraging infants to consume all of the milk or food served to them, regardless of infants' hunger and satiety cues. Pressuring: Cereal reflects mothers beliefs about whether infants need to eat more than breast milk and/or formula prior to 6 months of age to feel full or sleep through the night, and whether putting cereal in an infant's bottle helps infants feel full or sleep through the night (e.g., “Putting cereal in the bottle is good because it helps an infant feel full.”) Pressuring: Soothing measures the use of food to soothe infant crying. Responsive: Satiety assesses parental awareness and responses to infants' hunger and satiety cues (e.g., “I let my child decide how much to eat.”)
Data analytic plan
Preliminary analyses, including descriptive statistics and correlations, were conducted to describe the relationships among the demographic, maternal, and infant characteristics and the timing of solid food introduction. Additionally, a one-way ANOVA and follow-up contrasts were run to examine whether the timing of solid food introduction differed by milk feeding method (i.e. breastfeeding, formula feeding, or mixed feeding).
To test whether maternal feeding style and infant temperament independently predicted the timing of solid food introduction above and beyond maternal demographic and health characteristics (i.e. maternal pre-pregnancy BMI, age, and education) and milk feeding method, a hierarchical multiple regression was run. Maternal demographic and health characteristics and milk feeding method at 4 months (breastfeeding or formula feeding; mixed feeding was redundant) were entered in Step 1, maternal feeding style variables were entered in Step 2 (Pressuring: Soothing, Pressuring: Finish, Pressuring: Cereal, and Responsive: Satiety), and infant temperament variables were entered in Step 3 (4-month negative reactivity, 6-month negative reactivity, and 6-month motor reactivity). Continuous predictor variables were centered.
Exploratory regression analyses were conducted to examine whether infant temperament moderated the effects of maternal feeding style in predicting the timing of solid food introduction, above and beyond maternal demographic and health characteristics and milk feeding method. First, we tested three full models that included the covariates of maternal pre-pregnancy BMI, age, and education level, milk feeding method at 4 months, four maternal feeding style variables (Pressuring: Soothing, Pressuring: Finish, Pressuring: Cereal, and Responsive: Satiety), one infant temperament variable (4-month negative reactivity, 6-month negative reactivity, or 6-month motor reactivity) and interaction terms between each of the four feeding style variables and the single temperament variable; thus, four interaction terms were tested per model. All covariates and predictors were centered prior to the analyses.
Consistent with an exploratory approach, we then tested three reduced models that excluded any interaction terms that were not significant at the p < .10 level in the full models. After testing the reduced models, we probed interactions that were significant at the p < .10 level. The values from the reduced model tests were used to plot any significant or marginally significant interactions using the standard cutoff of one standard deviation above (i.e. high) and below (i.e. low) the mean of the variables included in the interaction (Aiken & West, 1991; Dawson, 2014). Simple slopes analyses were also performed to test which, if any, slopes of the moderator variables were significantly different from zero (Dawson, 2014). Including the full and reduced models, a total of six models were tested.
Results
Descriptive statistics for study variables can be found in Table 1. The average age at which parents introduced solid food was 17.36 weeks. 25.5% of infants were introduced to solid food between 0 and 15 weeks of age, 61.8% between 16 and 23 weeks, and 12.7% at or after 24 weeks.
Table 1. Descriptive statistics on study variables.
| Characteristic | Mean (SD) | %, n |
|---|---|---|
| Age introduced solids | 17.36 (4.62) | |
| Maternal age (at birth), years | 29.40 (4.93) | |
| Maternal pre-pregnancy BMI | 27.76 (7.25) | |
| Maternal education, years | 14.67 (2.05) | |
| Breastfeeding at 4M | 37.4%, 43 | |
| Formula feeding at 4M | 38.3%, 44 | |
| Mixed feeding at 4M | 23.5%, 27 | |
| 6M Pressuring: Cereal (IFSQ) | 1.92 (0.87) | |
| 6M Pressuring: Finish (IFSQ) | 2.07 (0.61) | |
| 6M Pressuring: Soothing (IFSQ) | 2.21 (0.83) | |
| 6M Responsive: Satiety (IFSQ) | 4.54 (0.45) | |
| 4M Negative reactivity (Diary) | 7.64 (3.28) | |
| 6M Negative reactivity (IBQ-R) | 3.34 (0.67) | |
| 6M Motor reactivity (IBQ-R) | 4.36 (0.93) |
Direct effects of maternal and infant characteristics on introduction to solid food
Pearson correlations among the study variables can be found in Table 2. Relevant to our aims, younger, less educated, and heavier mothers introduced solids earlier than older, more educated, and leaner mothers. Of the maternal feeding styles, mothers who endorsed statements that infants less than 6 months old need more to eat than breast milk or formula (higher Pressuring: Cereal feeding style) introduced solid food earlier, while mothers who said they paid more attention to their infants' hunger and fullness cues (higher Responsive: Satiety feeding style) introduced solid food later. The only infant temperament variable correlated with the timing of solid food introduction was 6-month motor reactivity. Infants who were rated higher in motor reactivity were introduced to solid food earlier than infants rated lower in motor reactivity. Infant sex, birth order, and birth weight were not significantly associated with the timing of solid food introduction or maternal feeding style (data not shown).
Table 2. Correlations among the timing of solid food introduction, maternal characteristics, and infant temperament.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age introduced solids | --- | .20* | .32** | -.26** | .12 | -.09 | -.22* | -.48** | -.15 | -.04 | .21* |
| 2. Maternal age | --- | .24** | -.07 | .12 | .00 | .06 | -.16 | -.05 | -.05 | -.14 | |
| 3. Maternal education | --- | -.29** | .11 | -.11 | -.13 | -.34** | -.02 | -.03 | .20* | ||
| 4. Maternal pre-pregnancy BMI | --- | .03 | .17 | .28** | .09 | -.05 | .07 | -.11 | |||
| 5. 4M Negative reactivity (Diary) | --- | .21* | .02 | -.21* | -.20* | -.09 | -.14 | ||||
| 6. 6M Negative reactivity (IBQ-R) | --- | .43** | .09 | .27** | -.02 | -.08 | |||||
| 7. 6M Motor reactivity (IBQ-R) | --- | .23* | .18 | -.12 | .03 | ||||||
| 8. Pressuring: Cereal (IFSQ) | --- | .14 | .22* | -.10 | |||||||
| 9. Pressuring: Finish (IFSQ) | --- | -.01 | -.12 | ||||||||
| 10. Pressuring: Soothing (IFSQ) | --- | .13 | |||||||||
| 11. Responsive: Satiety (IFSQ) | --- |
p < .05,
p < .01
The results of a one-way ANOVA and follow-up contrasts on the three milk feeding methods revealed significant differences in the timing of solid food introduction, F(2, 107) = 8.51, p <.001. Mothers who were exclusively breastfeeding at 4 months introduced solid food to their infants significantly later (M = 19.43 weeks, SD = 4.08) than mothers who were formula feeding (M = 15.57 SD = 4.50; p < .001) and marginally significantly later than mothers who were mixed feeding (M = 16.92, SD = 4.44; p < .07). Mothers who were formula feeding at 4 months did not significantly differ from mothers who were mixed feeding on the timing of solid food introduction.
Results of the hierarchical multiple regression analysis predicting the timing of solid food introduction showed some support for our hypotheses and are shown in Table 3. Maternal demographic and health characteristics and milk feeding method were included in Step 1. This model was significant, F(5, 88) = 5.79, p < .001, and explained 25% of the variance. Adding the maternal feeding style variables in Step 2 explained an additional 19% of the variance in the timing of solid food introduction and increased the total variance explained by the model to 44%, F(9, 84) = 7.18, p < .001. Adding the infant temperament variables in Step 3 did not explain any additional variance. Thus, the total variance explained by the final model was 44%, F(12, 81) = 5.24, p < .001). The only variable that was a significant predictor of the timing of solid food introduction in the context of all other study variables was the Pressuring: Cereal feeding style.
Table 3. Hierarchical multiple regression predicting timing of solid food introduction (n = 94).
| Variables | B | SE(B) | β | F | R2 |
|---|---|---|---|---|---|
| Step 1. Maternal characteristics and milk feeding method | 16.79 | .84 | -.18 | 5.79** | .25 |
| Maternal pre-pregnancy BMI | -0.11 | 0.06 | -0.18+ | ||
| Maternal age | 0.13 | 0.09 | 0.14 | ||
| Maternal education | 0.39 | 0.23 | 0.16 | ||
| Breastfeeding at 4M | 2.19 | 1.08 | 0.23* | ||
| Formula feeding at 4M | -1.15 | 1.13 | -0.12 | ||
| Step 2. Maternal feeding style | 16.52 | 0.75 | 7.18** | .44 | |
| Maternal pre-pregnancy BMI | -0.11 | 0.05 | -0.18* | ||
| Maternal age | 0.14 | 0.08 | 0.14 | ||
| Maternal education | 0.08 | 0.22 | 0.03 | ||
| Breastfeeding at 4M | 2.04 | 0.96 | 0.22* | ||
| Formula feeding at 4M | -0.16 | 1.03 | -0.12 | ||
| Pressuring: Finish (IFSQ) | -0.10 | 0.64 | -0.01 | ||
| Pressuring: Cereal (IFSQ) | -2.25 | 0.49 | -0.42** | ||
| Pressuring: Soothing (IFSQ) | 0.15 | 0.47 | 0.03 | ||
| Responsive: Satiety (IFSQ) | 1.74 | 0.92 | 0.17+ | ||
| Step 3. Infant temperament | 16.52 | 0.77 | 5.24** | .44 | |
| Maternal pre-pregnancy BMI | -0.10 | 0.06 | -0.17+ | ||
| Maternal age | 0.14 | 0.09 | 0.15 | ||
| Maternal education | 0.07 | 0.22 | 0.03 | ||
| Breastfeeding at 4M | 1.99 | 0.99 | 0.21+ | ||
| Formula feeding at 4M | -0.11 | 1.05 | -0.01 | ||
| Pressuring: Cereal (IFSQ) | -2.20 | 0.51 | -0.41** | ||
| Pressuring: Finish (IFSQ) | 0.04 | 0.70 | 0.01 | ||
| Pressuring: Soothing (IFSQ) | 0.14 | 0.49 | 0.03 | ||
| Responsive: Satiety (IFSQ) | 1.85 | 0.97 | 0.18+ | ||
| Infant 4M negativity (Diary) | 0.06 | 0.13 | 0.04 | ||
| Infant 6M negativity (IBQ-R) | -0.18 | 0.68 | -0.03 | ||
| Infant 6M activity (IBQ-R) | -0.12 | 0.51 | -0.02 |
p < .10;
p < .05;
p < .01
Exploratory results from interaction analyses
Multiple regression analyses were used to explore whether infant temperament moderated the effects of maternal feeding style on the timing of solid food introduction. The results of the full and reduced models are described next, and results of the full models are shown in Table 4.
Table 4. Multiple regressions predicting the timing of solid food introduction: Full models with interactions.
| Variables | B | SE(B) | β | F | R2 |
|---|---|---|---|---|---|
| I. Infant 4M negative reactivity (n = 94) | 16.30 | 0.76 | 5.21** | .48 | |
| Maternal pre-pregnancy BMI | -0.10 | 0.05 | -0.17+ | ||
| Maternal age | 0.15 | 0.08 | 0.16+ | ||
| Maternal education | 0.14 | 0.22 | 0.06 | ||
| Breastfeeding at 4M | 2.21 | 0.96 | 0.24* | ||
| Formula feeding at 4M | 0.06 | 1.02 | 0.01 | ||
| Pressuring: Cereal | -2.32 | 0.53 | -0.43** | ||
| Pressuring: Finish | -0.35 | 0.65 | -0.05 | ||
| Pressuring: Soothing | -0.09 | 0.48 | -0.02 | ||
| Responsive: Satiety | 0.59 | 1.11 | 0.06 | ||
| 4M Negativity (4M Neg) | 0.00 | 0.12 | 0.00 | ||
| Pressuring: Cereal × 4M Neg | -0.27 | 0.14 | -0.18+ | ||
| Pressuring: Finish × 4M Neg | -0.01 | 0.22 | 0.00 | ||
| Pressuring: Soothing × 4M Neg | 0.25 | 0.16 | 0.15 | ||
| Responsive: Satiety × 4M Neg | 0.16 | 0.24 | 0.07 | ||
| II. Infant 6M negative reactivity (n = 98) | 16.89 | 0.76 | 4.62** | .44 | |
| Maternal pre-pregnancy BMI | -0.10 | 0.06 | -0.16+ | ||
| Maternal age | 0.14 | 0.09 | 0.14 | ||
| Maternal education | 0.15 | 0.22 | 0.06 | ||
| Breastfeeding at 4M | 1.46 | 1.01 | 0.16 | ||
| Formula feeding at 4M | -0.34 | 1.05 | -0.04 | ||
| Pressuring: Cereal | -2.02 | 0.50 | -0.38** | ||
| Pressuring: Finish | -0.35 | 0.67 | -0.05 | ||
| Pressuring: Soothing | 0.10 | 0.50 | 0.02 | ||
| Responsive: Satiety | 1.17 | 0.96 | 0.12 | ||
| 6M Negativity (6M Neg) | -0.14 | 0.64 | -0.02 | ||
| Pressuring: Cereal × 6M Neg | 0.45 | 0.67 | 0.06 | ||
| Pressuring: Finish × 6M Neg | -0.20 | 1.20 | -0.02 | ||
| Pressuring: Soothing × 6M Neg | -0.60 | 0.89 | -0.07 | ||
| Responsive: Satiety × 6M Neg | -2.59 | 1.40 | -0.18+ | ||
| III. Infant 6M motor reactivity (n = 98) | 16.66 | 0.76 | 5.05** | .46 | |
| Maternal pre-pregnancy BMI | -0.09 | 0.06 | -0.14 | ||
| Maternal age | 0.12 | 0.09 | 0.12 | ||
| Maternal education | 0.22 | 0.22 | 0.10 | ||
| Breastfeeding at 4M | 1.76 | 1.02 | 0.19+ | ||
| Formula feeding at 4M | -0.45 | 1.05 | -0.05 | ||
| Pressuring: Cereal | -2.23 | 0.52 | -0.42** | ||
| Pressuring: Finish | -0.12 | 0.64 | -0.02 | ||
| Pressuring: Soothing | 0.13 | 0.49 | 0.02 | ||
| Responsive: Satiety | 1.20 | 0.03 | 0.12 | ||
| 6M motor reactivity (6M Act) | -0.05 | 0.49 | -0.01 | ||
| Pressuring: Cereal × 6M Act | 0.04 | 0.55 | 0.16+ | ||
| Pressuring: Finish × 6M Act | 0.47 | 0.67 | 0.07 | ||
| Pressuring: Soothing × 6M Act | 0.47 | 0.64 | 0.70 | ||
| Responsive: Satiety × 6M Act | -1.21 | 1.01 | -0.11 |
p < .10;
p < .05;
p < .01
The full model testing whether 4-month negative reactivity moderated the effects of maternal feeding style on the timing of introduction to solid food was significant (p < .001), and significant main effects for breastfeeding at 4 months and the Pressuring: Cereal feeding style emerged. The main effect of the Pressuring: Cereal feeding style was qualified by its inclusion in an interaction term. The interaction between the Pressuring: Cereal feeding style and 4-month negative reactivity was marginally significant (p < .07).
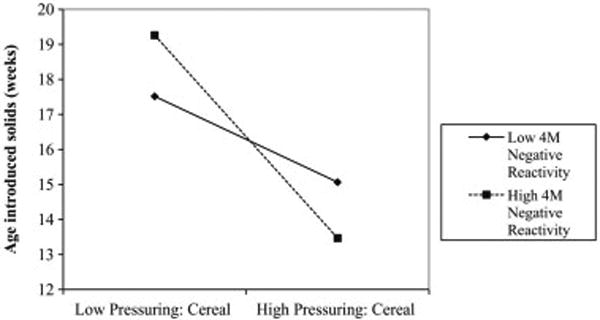
After removing the non-significant interaction terms the reduced model was still significant (R2 = .48, F(12, 81) = 6.16, p < .001), as were the previously described main effects. The interaction between the Pressuring: Cereal feeding style and 4-month negative reactivity became significant (β = -0.29, p < .05). Probing the interaction between the Pressuring: Cereal feeding style and 4-month negative reactivity revealed that the slopes for both high 4-month negative reactivity (t = -4.14, p < .001) and low 4-month negative reactivity (t = -2.39, p < .02) were significant. As can be seen in Figure 1, infants who were rated as high in 4-month negative reactivity were introduced to solid food earlier if their mothers also highly endorsed feeding cereal or other complementary food to infants less than 6 months old, compared to infants high in 4-month negative reactivity whose mothers were low in endorsing feeding cereal or other complementary food to infants less than 6 months old. Similarly, infants who were rated as low in 4-month negative reactivity were introduced to solid food earlier if their mothers also highly endorsed the Pressuring: Cereal feeding style, compared to infants low in 4-month negative reactivity whose mothers were low in endorsing the Pressuring: Cereal feeding style.
Figure 1. Interaction between Pressuring: Cereal and 4-month negative reactivity.
The full model testing whether 6-month negative reactivity moderated the effects of maternal feeding style on the timing of introduction to solid food was significant (p < .001), and revealed a significant main effect of the Pressuring: Cereal feeding style. There were no other significant main effects. One interaction term, the Responsive: Satiety feeding style by 6-month negative reactivity, was marginally significant (p < .07).
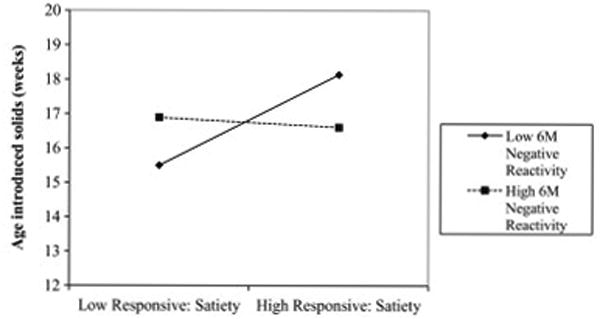
After removing the non-significant interaction terms, the reduced model was still significant (R2 = .43, F(11, 86) = 5.97, p < .001), as was the significant main effect of the Pressuring: Cereal feeding style (β =-2.03, t = -4.16, p < .001). The interaction term, Responsive: Satiety by 6-month negative reactivity, maintained marginal significance (β = -2.38, t = -1.87, p < .07). After probing the interaction, only the slope for low 6-month negative reactivity was significant (t = 2.55, p = .01). As seen in Figure 2, infants who were low in 6-month negative reactivity were introduced to solid food later if their mothers highly endorsed responsiveness to their infants' hunger and satiety cues, compared to infants who were low in 6-month negative reactivity whose mothers reported low levels of responsiveness.
Figure 2. Interaction between Responsive: Satiety 6-month negative reactivity.
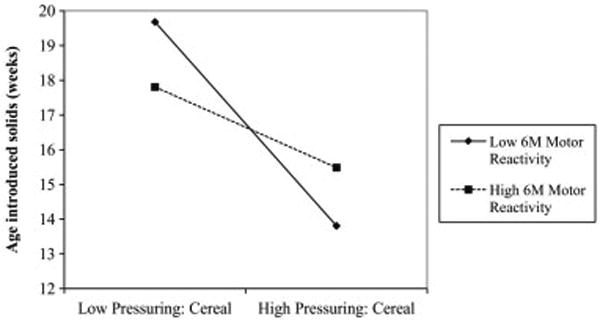
The full model testing whether 6-month motor reactivity moderated the effects of maternal feeding style on the timing of solid food introduction was significant (p < .001), and revealed a significant main effect for the Pressuring: Cereal feeding style. One interaction term, Pressuring: Cereal by 6-month motor reactivity was marginally significant (p < .10).
After removing the non-significant interaction terms, the reduced model was still significant (R2 = .44, F(11, 86) =6.09, p < .001). The main effect of the Pressuring: Cereal feeding style remained significant, and the interaction between Pressuring: Cereal and 6-month motor reactivity became significant (β =1.09, t = 2.04, p < .05). After probing the interaction, the simple slopes analysis showed that the slopes for both high 6-month motor reactivity (t = -2.21, p < .05) and low 6-month motor reactivity (t = -4.25, p < .001) were significant. As seen in Figure 3, infants who were high in 6-month motor reactivity were introduced to solid food earlier if their mothers highly endorsed feeding cereal or other complementary food prior to 6 months of age, compared to infants who were high in 6-month motor reactivity whose mothers did not endorse this practice. Similarly, infants who were low in 6-month motor reactivity were introduced to solid food earlier if their mothers were high in Pressuring: Cereal compared to infants who were low in 6-month motor reactivity whose mothers were low in the Pressuring: Cereal feeding style.
Figure 3. Interaction between Pressuring: Cereal and 6-month motor reactivity.
Discussion
The results of this study revealed that most infants were introduced to solid food at around 17 weeks of age, which indicates that on average mothers were following the guideline that was in place at the time of measurement. However, that one in four mothers introduced solid food prior to 4 months suggests that guideline adherence could be improved, particularly now that the recommended age has increased to 6 months. Demographic correlates of earlier solid food introduction were similar to those found in other samples and included younger maternal age at birth, fewer years of education, and higher pre-pregnancy BMI (Gibbs & Forste, 2014; Wijndaele et al., 2009). Breastfeeding at 4 months was associated with later timing of solid food introduction compared to formula feeding at 4 months, which is also consistent with existing literature (Armstrong et al., 2014; Clayton et al., 2013; Grummer-Strawn et al., 2008; Kronborg, Foverskov, & Væth, 2014).
Regarding the independent effects of maternal feeding style, mothers who endorsed that infants younger than 6 months of age need more to eat than breast milk or formula, including the practice of adding cereal to an infant's bottle (Pressuring: Cereal feeding style), were more likely to introduce solid food earlier than mothers who did not endorse this feeding style. Higher reports of responding to infant cues in the feeding context (the Responsive: Satiety feeding style) were associated with later timing of solid food introduction. These findings are consistent with our hypotheses and previous research that has shown that mothers introduce solid foods prior to the recommended guidelines because of their beliefs about infant feeding (Clayton et al., 2013; Heinig et al., 2006). Our results suggest that if mothers believe that infants less than 6 months old need more than breast milk or formula to sleep through the night or feel full, they may disregard the recommended guideline and introduce solid food early.
Infant negative and motor reactivity were not directly related to when infants were introduced to solid food, but rather our exploratory interaction analyses suggested that infant temperament modestly influenced the effects of maternal feeding style on the timing of solid food introduction. Four-month negative reactivity moderated the Pressuring: Cereal feeding style such that infants who were high in 4-month negative reactivity were introduced to solid food earlier if their mothers were high in Pressuring: Cereal. Excessive infant crying may reinforce a mother's beliefs and encourage her to consider solid food as a method of calming the infant, even though an early study on the use of cereal in the bottle to reduce infant crying demonstrated that this practice was ineffective (Barr, Kramer, Pless, Boisjoly, & Leduc, 1989).
Six-month motor reactivity also moderated the relationship between the Pressuring: Cereal feeding style and the timing of solid food introduction. Mothers of highly active infants who endorsed the practice of feeding solid food to young infants introduced to solid food earlier to their infants than mothers did not highly endorse the Pressuring: Cereal feeding style. Mothers may perceive motor activity as infant fussiness (Barr et al., 1988) and use solid food to manage behavior. Indeed, mothers in this study that rated their 6-month-old infants as high in negative reactivity also rated their infants high in motor reactivity (r = .43, p < .001). Additional research is necessary to confirm this explanation.
The finding that low negative reactivity as well as low motor activity moderated the Pressuring: Cereal feeding style was somewhat counterintuitive. It may be that mothers of infants who are low in affective or motor reactivity who also strongly believe that infants need to consume more than breast milk or formula perceive their infants' lack of reactivity as a sign of lethargy and the need for more energy, and thus introduce solid food earlier for added nutrition. Future research should explore this hypothesis.
Six-month negative reactivity moderated the effects of the Responsive: Satiety feeding style such that infants who were low in 6-month negative reactivity were introduced to solid food later if their mothers reported high levels of responsiveness to infant hunger and fullness cues. Mothers of highly reactive infants have been reported to have lower awareness of infant cues (McMeekin et al., 2013), but it may be that infants who are low in reactivity are also difficult to take cues from in a feeding context. Highly responsive mothers, even of infants who are not very reactive, may be more likely to look for infant cues in the feeding context. Low responsive mothers who have low reactive infants may be attending to other influences in deciding when to introduce solid food (e.g., listening to the advice of a friend). Additional research on the feeding behaviors of low responsive mothers with low reactive infants could test this hypothesis.
Taken together, our findings suggest that maternal characteristics primarily drive the decision of when to introduce solid food. Mothers may have underlying beliefs about how to respond to infants in a feeding context that directly impact their feeding behavior. Even though infant negative and motor reactivity had an effect on the relationship between maternal feeding style and her decision to begin solid feeding, the findings were modest indicating limited influence of infant characteristics on the decision to begin solid foods.
The results of this study must be interpreted alongside its limitations. First, maternal self-report was used for both maternal feeding style and infant temperament. Observed measures of maternal feeding style would be more valid and are recommended for future studies on this topic (Musher-Eizenman & Kiefner, 2013). Additionally, maternal feeding style and infant temperament were assessed at 6 months, which is after many of the mothers had introduced solid food. Mothers' feeding style may have been influenced by her infants' response to solid food. However, there is evidence to suggest that maternal feeding style, specifically control in feeding, is already established at birth (Brown & Lee, 2013), and is somewhat stable across the first two years of life (Blissett & Farrow, 2007; Thompson et al., 2013). Temperament is a relatively stable construct and in this sample the average number of fussing or crying episodes per day at 4-months was significantly associated with 6-month negative reactivity (r = .21, p < .04).
Conclusions
Our study suggests that within a predominately white, middle-class sample, both maternal feeding style and infant temperament contribute to the timing of solid food introduction, but that this early feeding decision is primarily determined by mothers. As such, mothers may benefit from additional guidance on infants' basic nutrition needs prior to 6 months of age and on how to respond to infant crying and motor reactivity levels without resorting to the earlier introduction of solid food to manage infant behavior.
The current guidelines recommend parents introduce solid food around 6 months of age (Eidelman & Schanler, 2012) and future studies are needed to assess whether parents are meeting this new recommendation. To promote adherence to the recommended guidelines for the timing of solid food introduction, health care professionals may need to directly assess and address maternal beliefs about feeding cereal or other nutritive substances outside of breast milk or formula to infants less than 6 months old. Clinician guidance may need to include alternative soothing and sleeping strategies to deter the use of cereal in the bottle or early introduction to solid food (Paul et al., 2011).
Highlights.
Feeding style predicts solid food introduction beyond demographic characteristics
Believing infants need solid foods < 6mo predicts earlier solid food introduction
Infant temperament may marginally influence the timing of solid food introduction
To promote guideline adherence, clinicians should address maternal feeding beliefs
Acknowledgments
The authors want to thank the families who participated in the study and all members of the research team who contributed to the collection of this data.
Sources of funding: This study was supported by a grant to the third author (CAS) from the National Institutes of Digestive Diseases and Kidney (DK081512). Manuscript preparation support for the first (AED) and second (KJM) authors was provided by Agriculture and Food Research Initiative Grant no. 2011-67001-30117 from the USDA National Institute of Food and Agriculture, Childhood Obesity Prevention Challenge Area – A2121. Support to AED during the revision period came from the National Science Foundation under Grant No. DGE1255832. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the NIDDK, USDA, or the National Science Foundation.
Footnotes
Conflict of interest statement: The authors declare that they have no conflicts of interest.
Contributions: AED was primarily responsible for the research questions, data analyses, interpretation, and drafting and revising of this manuscript. KJM contributed to the data analyses and interpretation. CAS was responsible for the conception and design of the larger research study from which the data for the current study were drawn, and contributed extensively to the interpretation of the analyses, drafting, and revising of this manuscript. All authors read and approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Allison E. Doub, 315 Health and Human Development-East Building, The Pennsylvania State University, University Park, PA 16802, United States
Kameron J. Moding, Email: kjm5444@psu.edu, 315 Health and Human Development-East Building, The Pennsylvania State University, University Park, PA 16802, United States.
Cynthia A. Stifter, Email: tvr@psu.edu, 308 Health & Human Development-East Building, The Pennsylvania State University, University Park PA 16802, United States.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, Calif.: SAGE Publications, Inc; 1991. [Google Scholar]
- Armstrong J, Abraham EC, Squair M, Brogan Y, Merewood A. Exclusive breastfeeding, complementary feeding, and food choices in UK infants. Journal of Human Lactation. 2014;30(2):201–208. doi: 10.1177/0890334413516383. [DOI] [PubMed] [Google Scholar]
- Barr RG, Kramer MS, Boisjoly C, McVey-White L, Pless IB. Parental diary of infant cry and fuss behaviour. Archives of Disease in Childhood. 1988;63(4):380–387. doi: 10.1136/adc.63.4.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr RG, Kramer MS, Pless IB, Boisjoly C, Leduc D. Feeding and temperament as determinants of early infant crying/fussing behavior. Pediatrics. 1989;84(3):514–521. [PubMed] [Google Scholar]
- Birch LL. Development of food preferences. Annual Review of Nutrition. 1999;19(1):41–62. doi: 10.1146/annurev.nutr.19.1.41. [DOI] [PubMed] [Google Scholar]
- Blissett J, Farrow C. Predictors of maternal control of feeding at 1 and 2 years of age. International Journal of Obesity. 2007;31(10):1520–1526. doi: 10.1038/sj.ijo.0803661. [DOI] [PubMed] [Google Scholar]
- Briefel RR, Reidy K, Karwe V, Jankowski L, Hendricks K. Toddlers' transition to table foods: Impact on nutrient intakes and food patterns. Journal of the American Dietetic Association. 2004;104(1 Suppl 1):s38–44. doi: 10.1016/j.jada.2003.10.025. [DOI] [PubMed] [Google Scholar]
- Brown A, Lee M. Breastfeeding is associated with a maternal feeding style low in control from birth. PLoS ONE. 2013;8(1) doi: 10.1371/journal.pone.0054229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Shriner RL. Personality development. In: Damon W, Lerner RM, Eisenberg N, editors. Handbook of Child Psychology, Vol 3: Social, Emotional, and Personality Development. 6th. Hoboken, N.J: Wiley; 2006. [Google Scholar]
- Cerniglia L, Cimino S, Ballarotto G. Mother–child and father–child interaction with their 24-month-old children during feeding, considering paternal involvement and the child's temperament in a community sample. Infant Mental Health Journal. 2014;35(5):473–481. doi: 10.1002/imhj.21466. [DOI] [PubMed] [Google Scholar]
- Clayton HB, Li R, Perrine CG, Scanlon KS. Prevalence and reasons for introducing infants early to solid foods: Variations by milk feeding type. Pediatrics. 2013;131(4):e1108–1114. doi: 10.1542/peds.2012-2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson JF. Moderation in management research: What, why, when, and how. Journal of Business and Psychology. 2014;29(1):1–19. doi: 10.1007/s10869-013-9308-7. [DOI] [Google Scholar]
- DiSantis KI, Hodges EA, Fisher JO. The association of breastfeeding duration with later maternal feeding styles in infancy and toddlerhood: A cross-sectional analysis. International Journal of Behavioral Nutrition and Physical Activity. 2013;10 doi: 10.1186/1479-5868-10-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eidelman AI, Schanler RJ. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827–e841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- Faith MS, Scanlon KS, Birch LL, Francis LA, Sherry B. Parent-child feeding strategies and their relationships to child eating and weight status. Obesity Research. 2004;12(11):1711–1722. doi: 10.1038/oby.2004.212. [DOI] [PubMed] [Google Scholar]
- Gartner L, Eidelman A. Breastfeeding and the use of human milk. Pediatrics. 2005;115(2):496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Rothbart MK. Studying infant temperament via the Revised Infant Behavior Questionnaire. Infant Behavior and Development. 2003;26(1):64–86. doi: 10.1016/S0163-6383(02)00169-8. [DOI] [Google Scholar]
- Gerards SMPL, Kremers SPJ. The role of food parenting skills and the home food environment in children's weight gain and obesity. Current Obesity Reports. 2015:1–7. doi: 10.1007/s13679-015-0139-x. http://doi.org/10.1007/s13679-015-0139-x. [DOI] [PMC free article] [PubMed]
- Gibbs BG, Forste R. Socioeconomic status, infant feeding practices and early childhood obesity. Pediatric Obesity. 2014;9(2):135–146. doi: 10.1111/j.2047-6310.2013.00155.x. [DOI] [PubMed] [Google Scholar]
- Grummer-Strawn LM, Scanlon KS, Fein SB. Infant feeding and feeding transitions during the first year of life. Pediatrics. 2008;122(Suppl 2):S36–42. doi: 10.1542/peds.2008-1315d. [DOI] [PubMed] [Google Scholar]
- Hagekull B, Bohlin G, Rydell AM. Maternal sensitivity, infant temperament, and the development of early feeding problems. Infant Mental Health Journal. 1997;18(1):92–106. doi: 10.1002/(SICI)1097-0355(199721)18:1<92∷AID-IMHJ7>3.0.CO;2-2. [DOI] [Google Scholar]
- Heinig MJ, Follett JR, Ishii KD, Kavanagh-Prochaska K, Cohen R, Panchula J. Barriers to compliance with infant-feeding recommendations among low-income women. Journal of Human Lactation. 2006;22(1):27–38. doi: 10.1177/0890334405284333. [DOI] [PubMed] [Google Scholar]
- Hughes SO, Power TG, Orlet Fisher J, Mueller S, Nicklas TA. Revisiting a neglected construct: Parenting styles in a child-feeding context. Appetite. 2005;44(1):83–92. doi: 10.1016/j.appet.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Huh SY, Rifas-Shiman SL, Taveras EM, Oken E, Gillman MW. Timing of solid food introduction and risk of obesity in preschool-aged children. Pediatrics. 2011;127(3):e544–e551. doi: 10.1542/peds.2010-0740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen E, Daniels LA, Nicholson JM. The dynamics of parenting and early feeding – constructs and controversies: A viewpoint. Early Child Development and Care. 2012;182(8):967–981. doi: 10.1080/03004430.2012.678593. [DOI] [Google Scholar]
- Kronborg H, Foverskov E, Væth M. Predictors for early introduction of solid food among Danish mothers and infants: an observational study. BMC Pediatrics. 2014;14(1):243. doi: 10.1186/1471-2431-14-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMeekin S, Jansen E, Mallan K, Nicholson J, Magarey A, Daniels L. Associations between infant temperament and early feeding practices. A cross-sectional study of Australian mother-infant dyads from the NOURISH randomised controlled trial. Appetite. 2013;60(1):239–245. doi: 10.1016/j.appet.2012.10.005. [DOI] [PubMed] [Google Scholar]
- Moorcroft KE, Marshall JL, McCormick FM. Association between timing of introducing solid foods and obesity in infancy and childhood: A systematic review. Maternal & Child Nutrition. 2011;7(1):3–26. doi: 10.1111/j.1740-8709.2010.00284.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musher-Eizenman DR, Kiefner A. Food parenting: A selective review of current measurement and an empirical examination to inform future measurement. Childhood Obesity. 2013;9(s1):S–32. doi: 10.1089/chi.2013.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby R, Brodribb W, Ware RS, Davies PSW. Infant feeding knowledge, attitudes, and beliefs predict antenatal intention among first-time mothers in Queensland. Breastfeeding Medicine. 2014;9(5):266–272. doi: 10.1089/bfm.2014.0012. [DOI] [PubMed] [Google Scholar]
- Niegel S, Ystrom E, Hagtvet KA, Vollrath ME. Difficult temperament, breastfeeding, and their mutual prospective effects: the Norwegian Mother and Child Cohort Study. Journal of Developmental and Behavioral Pediatrics. 2008;29(6):458–462. doi: 10.1097/dbp.0b013e3181877a88. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick H, Hennessy E, McSpadden K, Oh A. Parenting styles and practices in children's obesogenic behaviors: Scientific gaps and future research directions. Childhood Obesity. 2013;9s1:S73–86. doi: 10.1089/chi.2013.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul IM, Bartok CJ, Downs DS, Stifter CA, Ventura AK, Birch LL. Opportunities for the primary prevention of obesity during infancy. Advances in Pediatrics. 2009;56:107–133. doi: 10.1016/j.yapd.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul IM, Savage JS, Anzman SL, Beiler JS, Marini ME, Stokes JL, Birch LL. Preventing obesity during infancy: A pilot study. Obesity. 2011;19(2):353–361. doi: 10.1038/oby.2010.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinilla T, Birch LL. Help me make it through the night: behavioral entrainment of breast-fed infants' sleep patterns. Pediatrics. 1993;91(2):436–444. [PubMed] [Google Scholar]
- Robinson S, Marriott L, Poole J, Crozier S, Borland S, Lawrence W, et al. Southampton Women's Survey Study G. Dietary patterns in infancy: The importance of maternal and family influences on feeding practice. British Journal of Nutrition. 2007;98(5):1029–1037. doi: 10.1017/S0007114507750936. [DOI] [PubMed] [Google Scholar]
- Sameroff A. The transactional model of development: How children and contexts shape each other. Washington, DC, US: American Psychological Association; 2009. The transactional model; pp. 3–21. [Google Scholar]
- Stifter CA, Anzman-Frasca S, Birch LL, Voegtline K. Parent use of food to soothe infant/toddler distress and child weight status. An exploratory study. Appetite. 2011;57(3):693–699. doi: 10.1016/j.appet.2011.08.013. [DOI] [PubMed] [Google Scholar]
- Stifter CA, Spinrad TL. The effect of excessive crying on the development of emotion regulation. Infancy. 2002;3(2):133–152. doi: 10.1207/S15327078IN0302_2. [DOI] [PubMed] [Google Scholar]
- Taveras EM, Scanlon KS, Birch L, Rifas-Shiman SL, Rich-Edwards JW, Gillman MW. Association of breastfeeding with maternal control of infant feeding at age 1 year. Pediatrics. 2004;114(5):e577–583. doi: 10.1542/peds.2004-0801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson AL, Adair LS, Bentley ME. Pressuring and restrictive feeding styles influence infant feeding and size among a low-income African-American sample. Obesity. 2013;21(3):562–571. doi: 10.1002/oby.20091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson AL, Mendez MA, Borja JB, Adair LS, Zimmer CR, Bentley ME. Development and validation of the Infant Feeding Style Questionnaire. Appetite. 2009;53(2):210–221. doi: 10.1016/j.appet.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? International Journal of Behavioral Nutrition and Physical Activity. 2008;5:15. doi: 10.1186/1479-5868-5-15. http://doi.org/10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasser H, Bentley M, Borja J, Davis Goldman B, Thompson A, Slining M, Adair L. Infants perceived as “fussy” are more likely to receive complementary foods before 4 months. Pediatrics. 2011;127(2):229–237. doi: 10.1542/peds.2010-0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijndaele K, Lakshman R, Landsbaugh JR, Ong KK, Ogilvie D. Determinants of early weaning and use of unmodified cow's milk in infants: A systematic review. Journal of the American Dietetic Association. 2009;109(12):2017–2028. doi: 10.1016/j.jada.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Woo JG, Guerrero ML, Ruiz-Palacios GM, Peng Ym, Herbers PM, Yao W, et al. Morrow AL. Specific infant feeding practices do not consistently explain variation in anthropometry at age 1 year in urban United States, Mexico, and China cohorts. Journal of Nutrition. 2013;143(2):166–174. doi: 10.3945/jn.112.163857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worobey J, Peña J, Ramos I, Espinosa C. Infant difficulty and early weight gain: Does fussing promote overfeeding? Maternal & Child Nutrition. 2012 doi: 10.1111/j.1740-8709.2012.00410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


