Abstract
Opioid overdose is reversible through the timely administration of naloxone, which has been used by emergency medical services for decades. Law enforcement officers (LEOs) are often the first emergency responders to arrive at an overdose, but they are not typically equipped with naloxone.
This is rapidly changing; more than 220 law enforcement agencies in 24 states now carry naloxone. However, rollout in some departments has been hampered by concerns regarding officer and agency liability.
We systematically examined the legal risk associated with LEO naloxone administration. LEOs can be authorized to administer naloxone through a variety of mechanisms, and liability risks related to naloxone administration are similar to or lower than those of other activities in which LEOs commonly engage.
The number of US lives lost to opioid overdose has been increasing for nearly 2 decades, in an epidemic that affects people of all ages, races, and geographic areas.1–4 This 6-fold rise has been driven mainly by opioid analgesics,5,6 although heroin-involved deaths have recently begun to increase as well.7–12 The most recent data have shown a continued increase in fatal opioid overdoses, with painkiller-linked deaths remaining near their highs and heroin-related fatalities doubling from 2010 to 2012.12,13
Fatal opioid overdose is a solvable public health problem. Whether caused by heroin or prescription painkillers, opioid overdose is reversible through the timely administration of the prescription medication naloxone and, when necessary, the provision of ancillary emergency care.14–17 Opioids kill by depressing respiration to the point that insufficient oxygen is available to brain and other cells, a condition termed hypoxia.18–20 Naloxone displaces opioids from the brain receptors to which they attach, reversing their effects and restoring normal respiration.15,21 It is not a controlled substance, has no abuse potential, and has been used for decades to reverse opioid overdose.14,22,23 The public health challenge is ensuring that it is available when and where it is needed.
Beginning in the 1990s, community programs in several states began distributing naloxone and overdose rescue training to people who use drugs and the friends and family members of people at high risk for overdose.24–28 As of 2010, nearly 200 such community-based naloxone distribution programs were in operation, and participants reported reversing more than 10 000 overdoses.29 Initial results from these efforts have been positive. A community naloxone distribution program in Massachusetts was associated with lower opioid overdose death rates,16 and a simulation model demonstrated that distributing naloxone to heroin users for use at witnessed overdoses is cost-effective.30
Although most early efforts to increase access to naloxone operated without clear legal authorization, many states have recently modified law and policy to encourage the wider prescription, distribution, and administration of naloxone.31,32 By mid-2014, 25 states and the District of Columbia had authorized the prescription of naloxone to friends and family members of those at risk for opioid overdose, and 21 had enacted legal protections for overdose bystanders who summon help in the event of an overdose.33 The goal of these laws is to increase the likelihood that naloxone will be available when and where it is needed and to encourage overdose bystanders to summon emergency responders, who in many areas remain the only source for overdose rescue with naloxone.33
Paramedics have been carrying and administering naloxone for decades, but the first emergency personnel to arrive at the scene of an overdose are often not paramedics but rather emergency medical technicians (EMTs), emergency medical providers with a lower level of training than paramedics, or law enforcement officers (LEOs).34 Nationwide, EMTs outnumber paramedics approximately 3 to 1, and LEOs are approximately 10 times more numerous.35,36 These disparities are typically more pronounced in rural areas and other underserved locations such as tribal lands.37
Equipping EMTs and LEOs with naloxone may therefore reduce the amount of time between the onset of respiratory depression and the administration of naloxone.34,38 Because damage to the brain and other organs generally increases the longer the victim remains hypoxic, the quicker normal respiration is restored, the better outcomes are likely to be.16,39,40 In conjunction with legal changes expanding naloxone access to laypeople, states have also rapidly modified laws and regulations to grant EMTs the authority to administer naloxone. In 2013, only 13 states included naloxone administration in the EMT scope of practice38; by September 2014, this number had risen to 24.41
Because in many jurisdictions LEOs are also dispatched to overdose calls and are often the first on scene, there has been intense interest in equipping them with naloxone as well. The Office of National Drug Control Policy has urged law enforcement agencies to take that step, and its director has declared that naloxone “should be in the patrol cars of every law enforcement professional across the nation.”42(p1) The attorney general of the United States recently announced plans for federal LEOs to explore carrying naloxone, joining the many agencies that have already initiated the intervention and setting the tone for those that have not.43
As of September 2014, more than 220 law enforcement agencies in the United States were carrying naloxone, after a period of rapid scale-up. One of the intervention’s early adopters, the Quincy, Massachusetts, Police Department, launched its law enforcement overdose reversal program in 2010 and has reversed more than 300 overdoses to date.34,44 More recently, New York State allocated $5 million in drug forfeiture funds to purchasing naloxone and funding law enforcement overdose training,45 which has resulted in adoption of naloxone initiatives by more than 150 law enforcement agencies in the state, including the New York City Police Department, in which more than 20 000 street-level personnel will carry the medication.46
Despite this enthusiastic response from many agencies, rollout in some departments has been hampered by concerns regarding officer and agency liability, with officials in several jurisdictions citing liability fears as a reason for not equipping officers with the medication.47–49 We provide here an overview of the current landscape of law enforcement naloxone access and the legal risk environment associated with LEO overdose reversal activities.50 We conclude that LEOs can be authorized to administer naloxone through a variety of mechanisms, and liability risks related to naloxone administration to reverse suspected opioid overdose are similar to or lower than those of other activities in which LEOs commonly engage.
AUTHORIZATION
Because naloxone is a prescription medication, it can only be administered by a person operating under a valid prescription order.51 Both EMS and LEO responders who administer naloxone typically do so under what is termed a protocol or standing order, whereby a medical professional who is authorized to prescribe the medication empowers authorized individuals to administer it to a person who meets specified criteria.17
Although most law enforcement agencies that carry naloxone are located in states that have directly or indirectly permitted that practice via law or regulation, as of September 2014 LEOs in 2 states (Pennsylvania and Michigan) administer the medication under the authority of medical orders issued by the local emergency medical services agency’s medical director (Daniel Schwartz, MD, personal communication, August 26, 2014; Sheriff Ted Schendel, personal communication, August 13, 2014) without any additional authorization.
Through a systematic legal analysis, we identified 11 states that have added naloxone administration to the scope of practice of law enforcement personnel, which explicitly permits them to administer the medication under a standing medication order. Of those 11, this authority has been granted via statute in 10 (Delaware, Georgia, Indiana, Louisiana, Maine, Minnesota, Missouri, Ohio, Oklahoma, and Wisconsin) and by regulation in 1 (Massachusetts). An additional 10 states in which officers carry naloxone (California, Illinois, Maryland, New Jersey, New Mexico, New York, North Carolina, Utah, Tennessee, and Vermont) have passed laws that permit the medication to be prescribed to and administered by a variety of individuals but do not specifically mention law enforcement. In Rhode Island, officers carry naloxone under the authority of regulations promulgated by the state Department of Health (Figure 1).
FIGURE 1—
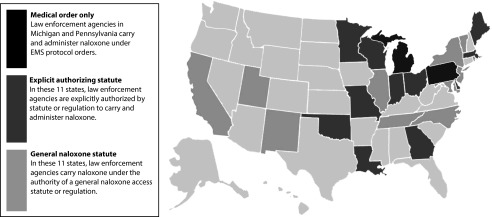
Law enforcement naloxone administration authority as of September 2014.
Note. EMS = emergency medical services.
IMMUNITY
Using standard legal research methods, we systematically searched the Westlaw legal database to determine whether and to what extent naloxone administration in the out-of-hospital setting has been the grounds for a lawsuit. We discovered no cases brought as a result of naloxone administration by LEOs, which is perhaps not surprising because that practice is relatively new. However, we also did not find any cases regarding the prescription, distribution, or administration of naloxone via community distribution programs, which have been operating for more than a decade and have been involved in more than 10 000 reversals.29 Although a few cases in the emergency medical services context have involved naloxone administration, they all center on otherwise tortious acts by emergency medical services personnel rather than the administration of the medication itself.
Some law enforcement officials may find these results surprising. Surveys demonstrate that LEOs, like physicians, consistently overestimate their likelihood of being found legally liable for their on-the-job actions.52–54 In reality, however, the legal risk to any person who acts in good faith to rescue another is very low.51 In nearly all cases, it is reduced further when the individual involved is an LEO acting in the course of his or her professional duties.
As a general matter, to succeed in a suit claiming damages attributable to the administration of naloxone, the aggrieved party would be required to show that he or she suffered an injury that was caused by the negligence of the person administering the medication. Such negligence can generally be shown by proving that the administrator acted in a way other than how a reasonable person in the same circumstance would have acted.
Although LEO naloxone administration is a relatively new practice, the use of the medication to reverse overdose in the prehospital setting is well established,17,22 and the number of law enforcement agencies adopting it is rapidly expanding. Whether a particular LEO’s actions were reasonable as a legal matter would depend on the particular circumstances of each situation, but the long-standing use of naloxone for emergency overdose reversal combined with explicit support from both federal and state governments strongly weighs in favor of a determination that the general practice of LEO naloxone administration is reasonable. Once the administrator shows that his or her actions were reasonable, the plaintiff cannot prevail.51
Even if a claimant is able to successfully argue that the administration was unreasonable and therefore negligent, he or she must still show that it was the cause of harm that the claimant suffered.55 Although no medication is without some risk, naloxone administration has a low risk of serious side effects.56–61 In addition, most states permit the LEO to argue that the actions of the person who overdosed must be taken into account in assigning legal responsibility.55,62
Several additional immunities are also available to LEOs. In general, officers cannot be held legally accountable for any acts or omissions undertaken in good faith and within the scope of their employment.63 This broad immunity stems from several sources. First, LEOs are generally immune from liability for civil claims arising from what are termed discretionary acts or omissions.64 Discretionary acts are any in which the LEO must exercise his or her professional judgment by considering the specific factual circumstances of a situation and making a subjective determination based on these circumstances, as in deciding whether naloxone administration is indicated in a particular situation.65,66
Moreover, the law in most states either permits or requires governmental entities to indemnify an officer against lawsuits arising out of an alleged act or omission made in the performance of the officer’s duties.67 In these states, an individual officer will not be personally liable for any monetary damages that might be assessed.68 In addition, in most instances an LEO is entitled to be defended by an attorney either working for or paid for by the government or the union representing the officer.69 A recent survey of federal civil rights claims found that even when LEOs are not explicitly covered by such a law they are almost never required to personally cover lawsuit costs, even when their conduct was so egregious that it led to them being disciplined, terminated, or criminally prosecuted.70
In the same vein, LEOs would generally not be liable for failing to provide overdose rescue, and equipping them with naloxone does not, in general, expose them to liability for failure to deploy it in an overdose emergency. In nearly all states, LEOs have no legal duty to assist others, even when they are in a position to do so.67 An LEO, of course, may face administrative discipline for violating the standard operating procedures of his or her employing agency if such procedures mandate particular actions.
Other immunity may also apply in some states. For example, all states have enacted at least 1 law that provides civil immunity to good Samaritans who provide aid in the event of an emergency.32 These laws vary from state to state, with little consistency in the classes of people to whom protection is extended, whether and to what extent training is required for their protections to apply, and the extent of the protection.71 Although these laws are intended to encourage laypeople and others who would not otherwise provide emergency care to do so, some also extend full or partial immunity to professional rescuers.72,73 In some states off-duty LEOs may be covered by these laws to the same extent as an ordinary citizen, and off-duty officers acting under the auspices of a nonprofit organization or governmental agency would likely be covered by the federal Volunteer Protection Act.74
These protections, particularly when layered atop the low baseline liability risk associated with good-faith naloxone administration, would make it extremely difficult for a lawsuit against an LEO, employing agency, or overarching governmental entity to succeed.
Governmental Immunity
In general, states may be sued only with their consent, a doctrine known as sovereign immunity.67 Although nearly every state has partially waived this immunity, these waivers generally retain immunity for the discretionary acts of or omissions by officers made in good faith and within the scope of their employment. Also, state laws often prohibit punitive damages or otherwise cap the amount of money the government can be required to pay should it lose a suit, often to the amount covered by insurance.62,69,75
In at least 11 states, claims against the state are heard by special boards on which administrative judges, appointed and employed by the government, have exclusive jurisdiction to hear and determine claims.69 In many of these states, the administrative board’s decision can be appealed to a traditional court only with permission of a state agency.
At the local level, municipalities and other political subdivisions such as counties and towns generally enjoy similar protections as those available to state governmental entities.67 In more than three quarters of states, the same or substantially similar provisions apply to both state and local governmental entities. Illinois and Oregon permit local government liability only if the employees themselves are not immune, and West Virginia excludes localities from immunity only if the acts result in injury, death, or loss to persons or property.76 Of the remaining states, at least 8 place monetary limits on amounts a plaintiff can recover.
Naloxone-Specific Immunity Laws
As of September 2014, 25 states and the District of Columbia had enacted laws to encourage the prescription, dispensing, and administration of naloxone.32 Although these laws have some variation, most permit prescribers acting in good faith to prescribe the medication to people who are likely to have the opportunity to use it to reverse overdose and permit those people to administer the medication. Most also provide all parties with immunity from civil liability and criminal charges, and some provide protection from administrative charges such as practicing medicine without a license.33
LEOs in 11 such states carried naloxone as of September 2014. Nine of these states provide civil immunity for people who administer naloxone as long as the person does so in good faith. Several states add additional requirements, such as that the administrator exercise reasonable care or act without gross negligence or willful misconduct. Two require that the administrator have received training or relevant information (Table 1). Although many of these laws were aimed mainly at increasing access among family members, friends, and other laypeople likely to witness an overdose, their language is typically broad enough that they can reasonably be read to include LEOs.
TABLE 1—
Summary of Liability Protections for Law Enforcement Naloxone Administration: September 2014
| States with Explicit Authorization (n = 11) |
States with General Authorization (n = 11) |
||||
| Protection | No. (%) | States | No. (%) | States | Total (n = 22), No. (%) |
| Immunity provided | |||||
| Civil | 7 (64) | DE, GA, IN, LA, MN, OK, WI | 9 (82) | CA, NJ, NM, NY, NC, UT, RI, TN, VT | 16 (73) |
| Administrative/other | 3 (27) | DE, LA, OH | 7 (64) | CA, NJ, NM, NY, NC, TN, VT | 10 (45) |
| Conditions | |||||
| Must act in good faith | 5 (45) | DE, GA, MN, OH, OK | 9 (82) | CA, NJ, NM, NY, NC, UT, RI, TN, VT | 14 (64) |
| Must have been trained or received information | 2 (18) | DE, WI | 2 (18) | CA, NJ | 4 (18) |
| Absent gross negligence or willful/wanton misconduct | 3 (27) | GA, IN, LA | 2 (18) | TN, VTa | 5 (23) |
| Must act reasonably | 1 (9) | WI | 4 (36) | CA, NM, NY, NC | 5 (23) |
Vermont also requires lack of recklessness.
Of the 11 states that directly authorize LEOs to administer naloxone, 7 (Delaware, Georgia, Indiana, Louisiana, Minnesota, Oklahoma, and Wisconsin) provide officers with civil immunity as long as the LEO meets certain standards. Five require that the officer act in good faith. Georgia law requires that the LEO act in good faith, without gross negligence or intent to harm, or as an ordinary reasonably prudent person would act. Indiana and Louisiana require the absence of gross negligence or willful misconduct. Although the Oklahoma law does not contain an explicit immunity provision, it dictates that LEOs acting as authorized are covered under the state’s broad Good Samaritan act (Table 1).
In Delaware, the immunity applies only if the LEO has completed a training course approved by the Department of Health, and Wisconsin officers are provided immunity only if they act in accordance with an agreement entered with an ambulance provider or physician. By contrast, Georgia law explicitly notes that civil immunity applies even if the LEO administers naloxone without being trained in its use. In all cases, the immunity granted by these laws is in addition to the immunity described earlier.
CONCLUSIONS AND RECOMMENDATIONS
The opioid overdose epidemic in the United States shows no signs of abating. Naloxone has been used for more than 40 years to reverse opioid overdose, and many states and the federal government are acting quickly to expand access to the medication. We conclude that LEOs can be authorized to administer naloxone through a variety of means, that adding the administration of naloxone to an LEO’s duties is unlikely to meaningfully affect liability risk for either officers or agencies, and that the passage of laws explicitly permitting LEOs to administer naloxone in the event of an overdose emergency greatly increases the chances that they will do so.
Although the expansion of naloxone administration authority to LEOs shows promise as an overdose reduction measure, research is needed to identify best practices and to determine whether LEO naloxone programs are a good use of scarce public resources in all jurisdictions. In areas in which LEOs are typically the first emergency responders to arrive at an overdose, equipping them with naloxone can reduce time to overdose rescue, possibly lowering morbidity and mortality by decreasing the amount of time the victim remains in respiratory depression.34 This research demonstrates that many of the states in which this is most likely to be the case (generally those with large rural regions) have not modified state law to encourage or explicitly permit LEOs to administer naloxone (Figure 1). Adoption of such measures by those states should be a high priority.
Although cost-effectiveness studies on law enforcement overdose reversal initiatives are not yet available, the price of the medication is relatively low, at approximately $60 to $80 per 2-dose rescue kit—a relatively small price when weighed against potential reductions in fatal overdose and nonfatal morbidity. In addition, law enforcement naloxone initiatives may have benefits beyond overdose rescue. Initial evidence has suggested that training officers in evidence-based public health initiatives can improve their receptiveness to those initiatives,77,78 and officers report that participating in naloxone programs improves public perception of law enforcement and LEOs.34
The training that accompanies LEO naloxone initiatives may be an opportune time to educate officers regarding addiction and overdose risk, possibly increasing their understanding of and support for overdose-related public health initiatives and strengthening relations between LEOs and the communities they serve. Encouraging LEOs to view individuals suffering from overdose as patients in need of care instead of criminals in need of arrest may, in time, discourage the use of policing policies and practices that increase the risk of overdose and other drug-related harms.77–80
In closing, we note that increased naloxone access is by no means the only tool to address the epidemic of opioid overdose. LEO naloxone initiatives should not come at the cost of scaling up or initiating community-based naloxone programs, which have a demonstrated record of success,16 and should be paired with laws that encourage bystanders to summon emergency responders by providing meaningful immunity for those that do.32 Although the rapidly expanding efforts to reduce time to overdose rescue are long overdue, they are unlikely to have much lasting effect in the absence of a comprehensive strategy to scale up evidence-based drug treatment and counseling, modify punitive drug policies, and reduce inappropriate opioid prescribing. The question is not whether these interventions work, but how to most effectively bring them to scale as part of a comprehensive, cross-sectoral effort to reduce the epidemic of drug overdose.
Acknowledgments
The work of C. S. Davis, J. K. Southwell, and D. Carr was partially supported by the Robert Wood Johnson Foundation’s Network for Public Health Law program.
Note. All opinions are those of the authors and not necessarily those of the funders.
Human Participant Protection
Institutional review board approval was not needed for this research, which did not involve human participants.
References
- 1.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers and other drugs among women–United States, 1999-2010. MMWR Morb Mortal Wkly Rep. 2013;62(26):537–542. [PMC free article] [PubMed] [Google Scholar]
- 2.Rossen LM, Khan D, Warner M. Trends and geographic patterns in drug-poisoning death rates in the US, 1999–2009. Am J Prev Med. 2013;45(6):e19–e25. doi: 10.1016/j.amepre.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chien LH, Hedegaard H, Warner M. Drug-poisoning deaths involving opioid analgesics: United States, 1999–2011. NCHS Data Brief. 2014;(166):1–8. [PubMed] [Google Scholar]
- 4.Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011;(81):1–8. [PubMed] [Google Scholar]
- 5.Okie S. A flood of opioids, a rising tide of deaths. N Engl J Med. 2010;363(21):1981–1985. doi: 10.1056/NEJMp1011512. [DOI] [PubMed] [Google Scholar]
- 6.Modarai F, Mack K, Hicks P et al. Relationship of opioid prescription sales and overdoses, North Carolina. Drug Alcohol Depend. 2013;132(1–2):81–86. doi: 10.1016/j.drugalcdep.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Peavy KM, Banta-Green CJ, Kingston S, Hanrahan M, Merrill JO, Coffin PO. “Hooked on” prescription-type opiates prior to using heroin: results from a survey of syringe exchange clients. J Psychoactive Drugs. 2012;44(3):259–265. doi: 10.1080/02791072.2012.704591. [DOI] [PubMed] [Google Scholar]
- 8.Pollini RA, Banta-Green CJ, Cuevas-Mota J, Metzner M, Teshale E, Garfein RS. Problematic use of prescription-type opioids prior to heroin use among young heroin injectors. Subst Abuse Rehabil. 2011;2(1):173–180. doi: 10.2147/SAR.S24800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers—United States, 2002-2004 and 2008-2010. Drug Alcohol Depend. 2013;132(1-2):95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 10.New York City Department of Health and Mental Hygiene. Unintentional drug poisoning (overdose) deaths in New York City, 2000-2012. Epi Data Brief. 2013;(33):1–4. [Google Scholar]
- 11.Markon J. Holder calls deaths from heroin overdoses an “urgent and growing public health crisis.”. Washington Post. March 10, 2014. Available at: http://www.washingtonpost.com/politics/holder-calls-deaths-from-heroin-overdoses-an-urgent-and-growing-public-health-crisis/2014/03/10/1a99720a-a7cf-11e3-b61e-8051b8b52d06_story.html. Accessed October 25, 2014.
- 12.Rudd RA, Paulozzi LJ, Bauer MJ et al. Increases in heroin overdose deaths—28 States, 2010 to 2012. MMWR Morb Mortal Wkly Rep. 2014;63(39):849–854. [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention. 2013 drug overdose mortality data announced [press release]. Atlanta, GA: January 12, 2015.
- 14.Chamberlain JM, Klein BL. A comprehensive review of naloxone for the emergency physician. Am J Emerg Med. 1994;12(6):650–660. doi: 10.1016/0735-6757(94)90033-7. [DOI] [PubMed] [Google Scholar]
- 15.Kim D, Irwin KS, Khoshnood K. Expanded access to naloxone: options for critical response to the epidemic of opioid overdose mortality. Am J Public Health. 2009;99(3):402–407. doi: 10.2105/AJPH.2008.136937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walley AY, Xuan Z, Hackman HH et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346 doi: 10.1136/bmj.f174. f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ashton H, Hassan Z. Best evidence topic report. Intranasal naloxone in suspected opioid overdose. Emerg Med J. 2006;23(3):221–223. doi: 10.1136/emj.2005.034322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leino K, Mildh L, Lertola K, Seppala T, Kirvela O. Time course of changes in breathing pattern in morphine- and oxycodone-induced respiratory depression. Anaesthesia. 1999;54(9):835–840. doi: 10.1046/j.1365-2044.1999.00946.x. [DOI] [PubMed] [Google Scholar]
- 19.Bouillon T, Bruhn J, Roepcke H, Hoeft A. Opioid-induced respiratory depression is associated with increased tidal volume variability. Eur J Anaesthesiol. 2003;20(2):127–133. doi: 10.1017/s0265021503000243. [DOI] [PubMed] [Google Scholar]
- 20.Pattinson KT. Opioids and the control of respiration. Br J Anaesth. 2008;100(6):747–758. doi: 10.1093/bja/aen094. [DOI] [PubMed] [Google Scholar]
- 21.Lewanowitsch T, Irvine RJ. Naloxone methiodide reverses opioid-induced respiratory depression and analgesia without withdrawal. Eur J Pharmacol. 2002;445(1-2):61–67. doi: 10.1016/s0014-2999(02)01715-6. [DOI] [PubMed] [Google Scholar]
- 22.Barton ED, Ramos J, Colwell C, Benson J, Baily J, Dunn W. Intranasal administration of naloxone by paramedics. Prehosp Emerg Care. 2002;6(1):54–58. doi: 10.1080/10903120290938797. [DOI] [PubMed] [Google Scholar]
- 23.Davis CS, Banta-Green CJ, Coffin P, Dailey MW, Walley AY. Intranasal naloxone for opioid overdose reversal. Prehosp Emerg Care. 2015;19(1):135–137. doi: 10.3109/10903127.2014.942484. [DOI] [PubMed] [Google Scholar]
- 24.Maxwell S, Bigg D, Stanczykiewicz K, Carlberg-Racich S. Prescribing naloxone to actively injecting heroin users: a program to reduce heroin overdose deaths. J Addict Dis. 2006;25(3):89–96. doi: 10.1300/J069v25n03_11. [DOI] [PubMed] [Google Scholar]
- 25.Galea S, Worthington N, Piper TM, Nandi VV, Curtis M, Rosenthal DM. Provision of naloxone to injection drug users as an overdose prevention strategy: early evidence from a pilot study in New York City. Addict Behav. 2006;31(5):907–912. doi: 10.1016/j.addbeh.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 26.Clark AK, Wilder CM, Winstanley EL. A systematic review of community opioid overdose prevention and naloxone distribution programs. J Addict Med. 2014;8(3):153–163. doi: 10.1097/ADM.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 27.Piper TM, Stancliff S, Rudenstine S et al. Evaluation of a naloxone distribution and administration program in New York City. Subst Use Misuse. 2008;43(7):858–870. doi: 10.1080/10826080701801261. [DOI] [PubMed] [Google Scholar]
- 28.Doe-Simkins M, Walley AY, Epstein A, Moyer P. Saved by the nose: bystander-administered intranasal naloxone hydrochloride for opioid overdose. Am J Public Health. 2009;99(5):788–791. doi: 10.2105/AJPH.2008.146647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Community-based opioid overdose prevention programs providing naloxone—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(6):101–105. [PMC free article] [PubMed] [Google Scholar]
- 30.Coffin PO, Sullivan SD. Cost-effectiveness of distributing naloxone to heroin users for lay overdose reversal. Ann Intern Med. 2013;158(1):1–9. doi: 10.7326/0003-4819-158-1-201301010-00003. [DOI] [PubMed] [Google Scholar]
- 31.Beletsky L, Rich JD, Walley AY. Prevention of fatal opioid overdose. JAMA. 2012;308(18):1863–1864. doi: 10.1001/jama.2012.14205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davis C, Webb D, Burris S. Changing law from barrier to facilitator of opioid overdose prevention. J Law Med Ethics. 2013;41(suppl 1):33–36. doi: 10.1111/jlme.12035. [DOI] [PubMed] [Google Scholar]
- 33.Davis CS. Legal Interventions to Reduce Overdose Mortality: Naloxone Access and Overdose Good Samaritan Laws. St. Paul, MN: Network for Public Health Law; 2014. [Google Scholar]
- 34.Davis CS, Ruiz S, Glynn P, Picariello G, Walley AY. Expanded access to naloxone among firefighters, police officers, and emergency medical technicians in Massachusetts. Am J Public Health. 2014;104(8):e7–e9. doi: 10.2105/AJPH.2014.302062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.US Department of Transportation Federal Interagency Committee on Emergency Medical Services. National EMS Assessment. Washington, DC: US Department of Transportation; 2012. [Google Scholar]
- 36.National Highway Traffic Safety Administration. EMS Workforce for the 21st Century: A National Assessment. Washington, DC: National Highway Traffic Safety Administration; 2008. [Google Scholar]
- 37.Rawlinson C, Crews P. Access to Quality Health Services in Rural Areas Emergency Medical Services: A Literature Review. College Station, TX: Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003. [Google Scholar]
- 38.Davis CS, Southwell JK, Niehaus VR, Walley AY, Dailey MW. Emergency medical services naloxone access: a national systematic legal review. Acad Emerg Med. 2014;21(10):1173–1177. doi: 10.1111/acem.12485. [DOI] [PubMed] [Google Scholar]
- 39.Strachan L, Noble DW. Hypoxia and surgical patients—prevention and treatment of an unnecessary cause of morbidity and mortality. J R Coll Surg Edinb. 2001;46(5):297–302. [PubMed] [Google Scholar]
- 40.Sporer KA. Strategies for preventing heroin overdose. BMJ. 2003;326(7386):442–444. doi: 10.1136/bmj.326.7386.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davis C. Legal Interventions to Reduce Overdose Mortality: Emergency Medical Services Naloxone Access. St. Paul, MN: Network for Public Health Law; 2014. [Google Scholar]
- 42. Office of National Drug Control Policy. Announcing the opioid overdose toolkit [press release]. Washington, DC: August 28, 2013.
- 43. Department of Justice Office of Public Affairs. Attorney General Holder announces plans for federal law enforcement personnel to begin carrying naloxone [press release]. Washington, DC: July 31, 2014.
- 44.Ronan P. Quincy police successfully use Narcan for 300th time. Patriot Ledger. October 8, 2014. Available at: http://www.patriotledger.com/article/20141008/News/141006435. Accessed October 23, 2014.
- 45.Letter from Eric T. Schneiderman, Attorney General of New York, to Law Enforcement Agencies, April 3, 2014. Available at: http://www.ag.ny.gov/sites/default/files/pdfs/features/cop/COP_Letter.pdf. Accessed October 23, 2014.
- 46.Goodman D. In expanded program, officers across New York City will carry antidote for heroin overdoses. New York Times. May 27, 2014. Available at: http://www.nytimes.com/2014/05/27/nyregion/in-expanded-program-officers-across-new-york-city-will-carry-antidote-for-heroin-overdoses.html. Accessed October 23, 2014.
- 47.Ortega O. Police union, Somerville at odds on Narcan. Boston Globe. September 22, 2014. Available at: http://www.bostonglobe.com/metro/2014/09/21/required-carry-narcan-somerville-police-union-argues-for-new-contract/ATzxFwi8VYDy3NV1I7nWfI/story.html. Accessed October 20, 2014.
- 48.Terry N. Join the conversation: should Asbury Park cops and firefighters be allowed to give opiate antidote Narcan? Asbury Park Press. March 10, 2014. Available at: http://www.app.com/article/20140309/NJNEWS/303090028/-1/UPDATE/Asbury-Park-won-t-allow-cops-firefighters-to-give-opiate-antidote-Narcan. Accessed October 23, 2014. [Google Scholar]
- 49.Dinan E. Pols, first responders debate letting officers give overdose antidote. Seacoast Online. May 6, 2014. Available at: http://www.seacoastonline.com/article/20140506/News/405060407. Accessed October 23, 2014. [Google Scholar]
- 50.Rhodes T. The “risk environment”: a framework for understanding and reducing drug-related harm. Int J Drug Policy. 2002;13(2):85–94. [Google Scholar]
- 51.Burris S, Norland J, Edlin BR. Legal aspects of providing naloxone to heroin users in the United States. Int J Drug Policy. 2001;12(3):237–248. [Google Scholar]
- 52.Lawthers AG, Laird NM, Lipsitz S, Hebert L, Brennan TA, Localio AR. Physicians’ perceptions of the risk of being sued. J Health Polit Policy Law. 1992;17(3):463–482. doi: 10.1215/03616878-17-3-463. [DOI] [PubMed] [Google Scholar]
- 53.Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assuaged by tort reforms. Health Aff (Millwood) 2010;29(9):1585–1592. doi: 10.1377/hlthaff.2010.0135. [DOI] [PubMed] [Google Scholar]
- 54.Hughes T. Police officers and civil liability: “the ties that bind”? Policing. 2001;24(2):240–262. [Google Scholar]
- 55.Burris S, Beletsky L, Castagna C, Coyle C, Crowe C, McLaughlin JM. Stopping an invisible epidemic: legal issues in the provision of naloxone to prevent opioid overdose. Drexel Law Review. 2009;1(2):273–339. [Google Scholar]
- 56.Yealy DM, Paris PM, Kaplan RM, Heller MB, Marini SE. The safety of prehospital naloxone administration by paramedics. Ann Emerg Med. 1990;19(8):902–905. doi: 10.1016/s0196-0644(05)81566-5. [DOI] [PubMed] [Google Scholar]
- 57.Hsu W, Rao RB, Nelson LS. Naloxone hazards overstated. J Toxicol Clin Toxicol. 1997;35(2):215–217. doi: 10.3109/15563659709001198. 219–220. [DOI] [PubMed] [Google Scholar]
- 58.Buajordet I, Naess AC, Jacobsen D, Brors O. Adverse events after naloxone treatment of episodes of suspected acute opioid overdose. Eur J Emerg Med. 2004;11(1):19–23. doi: 10.1097/00063110-200402000-00004. [DOI] [PubMed] [Google Scholar]
- 59.Wermeling DP. Review of naloxone safety for opioid overdose: practical considerations for new technology and expanded public access. Ther Adv Drug Saf. 2015;6(1):20–31. doi: 10.1177/2042098614564776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Belz D, Lieb J, Rea T, Eisenberg MS. Naloxone use in a tiered-response emergency medical services system. Prehosp Emerg Care. 2006;10(4):468–471. doi: 10.1080/10903120600885134. [DOI] [PubMed] [Google Scholar]
- 61.Osterwalder JJ. Naloxone—for intoxications with intravenous heroin and heroin mixtures—harmless or hazardous? A prospective clinical study. J Toxicol Clin Toxicol. 1996;34(4):409–416. doi: 10.3109/15563659609013811. [DOI] [PubMed] [Google Scholar]
- 62.American Law Institute. Philadelphia, PA: American Law Institute; 1979. Restatement (Second) of Torts. [Google Scholar]
- 63. City of Lancaster v. Chambers, 883 SW 2d 650. (TX 1994).
- 64. Everitt v. General Elec. Co., 932 A. 2d 831 (NH 2007).
- 65.De Geest G. Who should be immune from tort liability? J Legal Stud. 2012;41(2):291–319. [Google Scholar]
- 66. Harlow v. Fitzgerald, 457 US 800 (1982).
- 67.Dobbs D, Hayden T, Bublick E. Dobbs’ Law of Torts. 2nd ed. Eagan, MN: Thomson West; 2011. [Google Scholar]
- 68.Jeffries JC., Jr In praise of the Eleventh Amendment and Section 1983. Va Law Rev. 1998;84(1):47–82. [Google Scholar]
- 69.Shepard’s Editorial Staff. Civil Actions Against State and Local Government: Its Divisions, Agencies and Officers. 2nd ed. Eagan, MN: Thomson West; 2002. [Google Scholar]
- 70.Schwartz JC. Police indemnification. New York Univ Law Rev. 2014;89(3):885–1005. [Google Scholar]
- 71.Sutton V. Is there a doctor (and a lawyer) in the house? Why our Good Samaritan laws are doing more harm than good for a national public health security strategy: a fifty-state survey. J Health Biomed Law. 2010;6:261–300. [Google Scholar]
- 72.Waisman DA. Negligence, responsibility, and the clumsy Samaritan: is there a fairness rationale for the Good Samaritan immunity? Ga State Univ Law Rev. 2013;29(Spring):609–683. [Google Scholar]
- 73.Reuter SR. Physicians as good Samaritans. Should they receive immunity for their negligence when responding to hospital emergencies? J Leg Med. 1999;20(2):157–193. doi: 10.1080/01947649909511086. [DOI] [PubMed] [Google Scholar]
- 74. Volunteer Protection Act of 1997, 42 U.S.C. 14501–14505.
- 75. City of Newport v. Fact Concerts, Inc., 453 U.S. 247 (1981).
- 76. W. Va. Code Ann. § 29-12A-4(c)(2).
- 77.Davis CS, Beletsky L. Bundling occupational safety with harm reduction information as a feasible method for improving police receptiveness to syringe access programs: evidence from three US cities. Harm Reduct J. 2009;6:16. doi: 10.1186/1477-7517-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Silverman B, Davis CS, Graff J, Bhatti U, Santos M, Beletsky L. Harmonizing disease prevention and police practice in the implementation of HIV prevention programs: up-stream strategies from Wilmington, Delaware. Harm Reduct J. 2012;9(1):17. doi: 10.1186/1477-7517-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Strathdee SA, Beletsky L, Kerr T. HIV, drugs and the legal environment. Int J Drug Policy. 2015;26(suppl 1):S27–S32. doi: 10.1016/j.drugpo.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Davis CS, Burris S, Kraut-Becher J, Lynch KG, Metzger D. Effects of an intensive street-level police intervention on syringe exchange program use in Philadelphia, PA. Am J Public Health. 2005;95(2):233–236. doi: 10.2105/AJPH.2003.033563. [DOI] [PMC free article] [PubMed] [Google Scholar]


