Abstract
The aim of the present study was to compare the health outcomes of catheter ablation therapy against those of antiarrhythmic drugs (AADs) in the management of atrial fibrillation (AF). The effects of catheter ablation and AADs on a number of parameters were compared, including AF recurrence, all-cause mortality, stroke/transient ischemic attack (TIA) and quality of life (QoL). A systematic literature search of PubMed, Embase and the Cochrane Central Register of Controlled Trials was conducted to obtain relevant randomized controlled trials. The relative risks (RRs) and 95% confidence intervals (CIs) of AF recurrence, all-cause mortality and stroke/TIA between catheter ablation and AADs were subsequently calculated. Weighted mean differences (WMDs) and 95% CIs were used to evaluate the QoL between the two therapy groups. In total, 11 randomized trials, which included 1,763 AF patients, were eligible for the meta-analysis. Overall, the results indicated that catheter ablation produces superior outcomes compared with AADs in reducing AF recurrence (RR, 0.47; 95% CI, 0.38–0.58; P<0.001) and improving the QoL (physical component summary: WMD, 2.23; 95% CI, 0.24–4.21; P=0.03; mental component summary: WMD, 2.69; 95% CI, 0.04–5.35; P=0.05). However, no statistically significant difference was identified between the two groups with regard to the incidence of all-cause mortality (RR, 0.87; 95% CI, 0.37–2.06; P=0.76) and stroke/TIA (RR, 1.83; 95% CI, 0.73–4.55; P=0.20). In summary, catheter ablation was demonstrated to markedly reduce AF recurrence and improve QoL when compared with AAD therapy. However, the incidence rates of all-cause mortality and stroke/TIA were comparable between catheter ablation and AAD therapy.
Keywords: catheter ablation, antiarrhythmic drugs, atrial fibrillation, meta-analysis
Introduction
Atrial fibrillation (AF) is the most prevalent form of arrhythmia observed in clinical practice, with a high population prevalence in industrial and developing countries (1–3). Furthermore, the prevalence of AF is increasing markedly in elderly populations (4). AF is associated with a three-fold risk of heart failure and a five-fold risk of stroke (5,6). In addition to the significant rate of morbidity, AF is associated with a 1.5–1.9-fold risk of mortality (7). Therefore, AF has become a substantial health burden for patients and societies worldwide.
According to the present guidelines for the management of AF, antiarrhythmic drugs (AADs) are the primary strategy for treating AF (5,6). However, the application of AADs has encountered challenges due to their limited efficacy and potential adverse effects. Thus, catheter ablation therapy has become a generally adopted alternative technique for the treatment of AF, particularly in cases of paroxysmal or/and persistent AF. However, the management recommendations and guidelines have not yet reached a consensus with regard to the use of catheter ablation for the treatment of AF, primarily due to the differences in ablation strategy and technique employed in different centers, in addition to relevant complications (5,6,8). In previous years, a number of small to moderately sized randomized controlled trials (RCTs) have been published that directly compare the efficacy of catheter ablation and AADs for the treatment of AF (9–19). However, the number of patients enrolled in each study was limited. Therefore, a meta-analysis was conducted in the present study to comprehensively evaluate whether catheter ablation is superior to AADs for the treatment of AF. In addition, the quality of the results published by the previous studies was evaluated, as recommended by the Cochrane Collaboration.
Materials and methods
Search strategy and inclusion criteria
MEDLINE, Embase and the Cochrane Central Register of Controlled Trials databases were searched for RCTs that compared catheter ablation with AADs for the treatment of AF, without language restrictions (last search update, May 1, 2014). In addition, reference lists from initially identified articles were retrieved in order to avoid the exclusion of any relevant studies. The following medical subject heading terms were used: ‘Atrial fibrillation’, ‘catheter ablation’ and ‘randomized controlled trials’.
Studies were included if they satisfied the following criteria: i) Study design was a RCT; ii) study population consisted of human participants with paroxysmal, persistent or long-standing persistent AF; iii) interventions included pulmonary vein isolation, no matter which technique was used; and iv) follow-up was ≥12 months.
Quality assessment
The methodological quality of each eligible study (risk of bias) was evaluated as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (version 5.1.0) (20). The risk of bias for each trial was assessed on the basis of the prime endpoint of recurrence of AF. The following criteria were evaluated and assigned a value of ‘high’, ‘low’ or ‘unclear’ by two authors. With regard to selection bias, the authors aimed to determine whether the method of randomization was adequate and whether the treatment allocation was concealed. In addition, performance and detection biases were assessed by determining whether the participants and personnel were blinded to the intervention, and whether the outcome assessor was blinded to the intervention. With regard to attrition bias, the authors determined whether any incomplete outcome data were sufficiently assessed and handled, while reporting bias was assessed by determining whether selective outcome reporting had been identified. Finally, the existence of any additional sources of bias was analyzed.
Data extraction
Two authors independently extracted relevant data from the included trials, and disagreements were resolved by discussion and consensus. The following data were extracted from each RCT: Name of the first author, year of publication, number of patients (intervention vs. control), age of populations, composition of gender, time of follow-up, definition of primary outcome and other important clinical information. In the case of a trial being reported in multiple publications, the most complete study or the article with the longest follow-up time was selected. The primary endpoint was the recurrence of AF. Secondary endpoints included all-cause mortality, stroke/transient ischemic attack (TIA) and quality of life (QoL).
Statistical analysis
Data analysis was performed based on an intention-to-treat analysis. Relative risks (RRs) with 95% confidence intervals (CIs) were selected to compare the differences for dichotomous outcomes, while weighted mean differences (WMDs) with 95% CIs were used to compare continuous outcomes. Heterogeneity among studies was analyzed using a χ2-based Q test and I2 statistic. If significant heterogeneity was identified (P<0.05 and I2 >50%), a random-effects model was selected, whilst a fixed-effects model was selected in all other cases.
Begg's funnel plot and Egger's test were used to evaluate the significance of the publication bias. The meta-analysis was performed using Stata software, version 11.0 (StataCorp, College Station, TX, USA) and Revman 5.1 software (The Cochrane Collaboration). A two-tailed P-value of <0.05 was considered to indicate a statistically significant difference. Finally, the quality of the evidence was evaluated using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) system (21).
Results
Literature search and selection
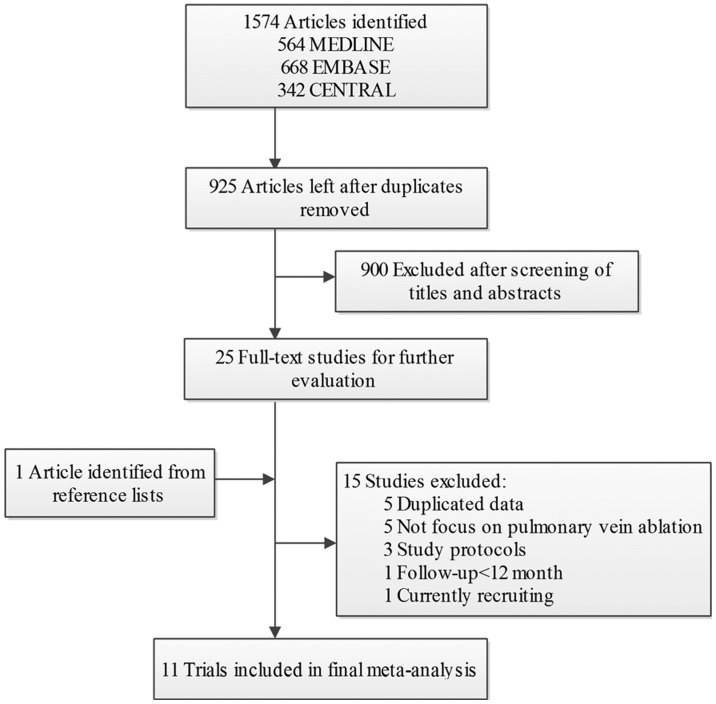
A flow diagram of the literature search is presented in Fig. 1. Briefly, 1,917 potentially relevant articles were identified following electronic and additional manual searches. Among the 1,917 publications yielded, 900 articles were excluded following screening of the titles and abstracts. Subsequently, 26 full-text articles were assessed for eligibility. Among these, 15 articles were further excluded for a variety of reasons, as described in Fig. 1. Finally, 11 RCTs involving 1,763 patients with AF were included in the meta-analysis (9–19).
Figure 1.
Flow diagram of the included studies in the meta-analysis
Study characteristics and risk of bias assessment
Primary characteristics of the 11 RCTs included in the meta-analysis are shown in Table I. The 11 trials were published between 2003 and 2013. Among them, four trials enrolled only patients with paroxysmal AF (13,15,16,18), two trials enrolled patients with only persistent AF (11,19), and the remaining five trials enrolled patients with paroxysmal and persistent AF (9,10,12,14,17). Three trials enrolled patients to receive pulmonary vein ablation as the first-line therapy (10,17,18), whereas the remaining studies included patients that had failed at least one AAD treatment protocol or were intolerant of AADs. The majority of the trials compared catheter ablation with AADs, with the exception of one trial that compared catheter ablation plus AADs with single AAD administration (12). All the AF patients assigned to catheter ablation underwent a single ablation procedure in four of the studies (9,10,12,14). In the other trials, patients that received catheter ablation therapy underwent two or more ablation procedures in the blanking period when required.
Table I.
Characteristics of the studies included in meta-analysis.
| Study | Ablation/AAD patients, n | Gender (M/F), n | Age, years | Type of AF | Ablation strategy | Follow-up, months (success rate, %) | Primary outcome |
|---|---|---|---|---|---|---|---|
| Krittayaphong et al (2003) | 15/15 | T:11/4 | T: 55.3±10.5 | Paroxysmal (70%) and persistent AF | CPVA | 12 (100%) | AF |
| C: 8/7 | C: 48.6±15.4 | ||||||
| Wazni et al (2005) | 33/37 | NA | T: 53±8 | Paroxysmal (96%) and persistent AF | PVI | 12 | AF |
| C: 54±8 | (95.6) | ||||||
| Oral et al (2006) | 77/69 | T: 67/10 | T: 55±9 | Chronic AF | CPVA | 12 | AT |
| C: 62/7 | C: 58±8 | (100) | |||||
| Stabile et al (2006) | 68/69 | T: 37/31 | T: 62.2±9 | Paroxysmal (67%) and persistent AF | CPVA | 12 | AT |
| C: 44/25 | C: 62.3±10.7 | (97.1) | |||||
| Jais et al (2008) | 53/59 | T: 45/8 | T: 49.7±10.7 | Paroxysmal AF | PVI | 12 | AF |
| C: 49/10 | C: 52.4±11.4 | (96.4) | |||||
| Forleo et al (2009) | 35/35 | T: 20/15 | T: 63.2±8.6 | Paroxysmal (41%) and persistent AF | PVI | 12 | AF |
| C: 23/12 | C: 64.8±6.5 | (100) | |||||
| Wilber et al (2010) | 106/61 | T: 73/33 | T: 55.5 (53.7–57.3) | Paroxysmal AF | PVI | 12 | Protocol-defined treatment failure AT |
| C: 38/23 | C: 56.1 (52.9–59.4) | (95.2) | |||||
| Pappone et al (2011) | 99/99 | T: 69/30 | T: 55±10 | Paroxysmal AF | CPVA | 48 | AT |
| C: 64/35 | C: 57±10 | (100) | |||||
| Nielsen et al (2012) | 146/148 | T: 100/46 | T: 56±9 | Paroxysmal AF | CPVA | 24 | Burden of AF AT |
| C: 106/42 | C: 54±10 | (95.9) | |||||
| Morillo et al (2012) | 66/61 | T: 51/15 | 55.3±10.5 | Paroxysmal (87.5%) and persistent AF | PVI | 24 | |
| C: 45/16 | (82.7) | ||||||
| Blandino et al (2013) | 153/258 | T: 109/44 | T: 75±5 | Persistent AF | PVI | 60 | AF/AT |
| C: 186/72 | C: 76±5 | (100) |
AAD, antiarrhythmic drugs; AF, atrial fibrillation; NA, not available; CPVA, circumferential pulmonary vein ablation; PVI, pulmonary vein isolation; AT, atrial tachycardia; M, male; F, female; T, treatment group; C, control group.
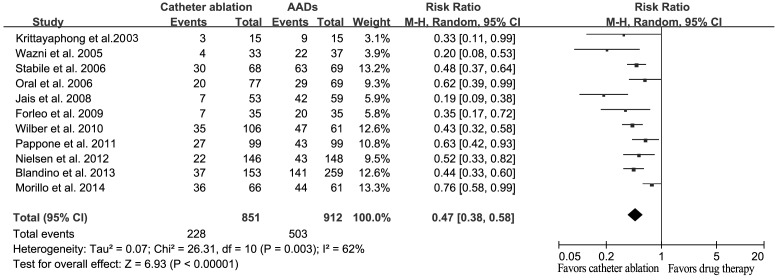
A risk of bias assessment was performed for each trial, and the results are presented in Fig. 2A. Of the 11 trials, six trials adopted appropriate methods to generate the random sequence (10–12,14,15,18). One study reported allocation concealment using sealed envelopes (15); however, the methods of concealment in other trials were not mentioned. Blinding of the outcome assessors was reported in three trials (11,12,18). The overall risk of bias is presented in Fig. 2B.
Figure 2.
Risk of bias assessment for the included trials. (A) Summary of the risk of bias for each individual trial. (B) Overall risk of bias.
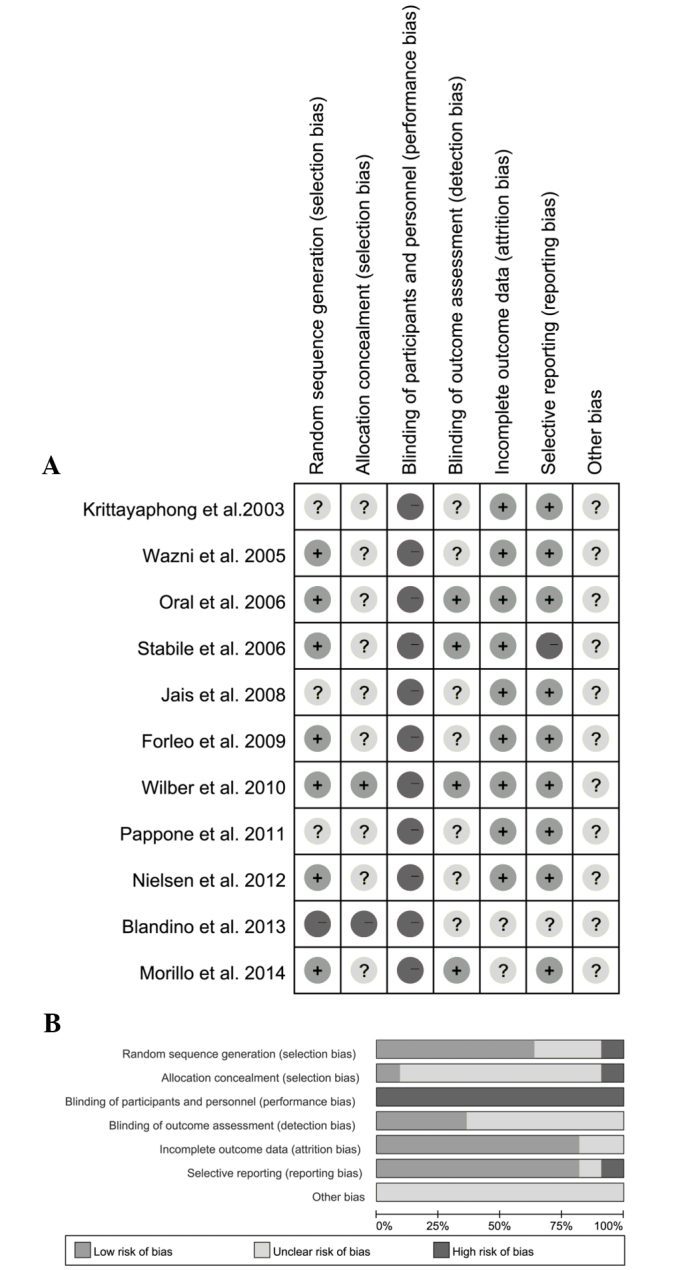
Analysis of the primary outcome, recurrence of AF
The majority of the included trials considered the recurrence of AF and/or atrial tachyarrhythmia as their primary end point. Therefore, the overall effect of catheter ablation against AADs for the recurrence of AF was assessed. The results indicated that catheter ablation was able to significantly reduce the recurrence of AF, as compared with AADs (RR, 0.47; 95% CI, 0.38–0.58; P<0.001; Fig. 3). Significant heterogeneity was detected among the trials (Q=26.31; I2=62%; P=0.003).
Figure 3.
Forest plot of the effects of catheter ablation vs. AADs on the recurrence of atrial fibrillation. AAD, antiarrhythmic drug; CI, confidence interval.
Three trials enrolled drug-naive patients and the result was similar to the overall effect (RR, 0.50; 95% CI, 0.27–0.92; P=0.03). Sensitivity analysis indicated that no single study significantly altered the combined effect, which ranged between 0.45 (95% CI, 0.37–0.55) and 0.41 (95% CI, 0.43–0.62).
Analysis of the secondary outcomes, all-cause mortality, stroke and/or TIA, and QoL
A total of 18 mortalities were reported in six studies, among which eight cases had received catheter ablation and 10 cases had received AADs. No statistically significant difference in the mortality rate was detected between the catheter ablation and AAD treatment groups (RR, 0.87; 95% CI, 0.37–2.06; P=0.76; Fig. 4), with no evidence for significant heterogeneity (Q=2.12, I2=0%, P=0.83).
Figure 4.
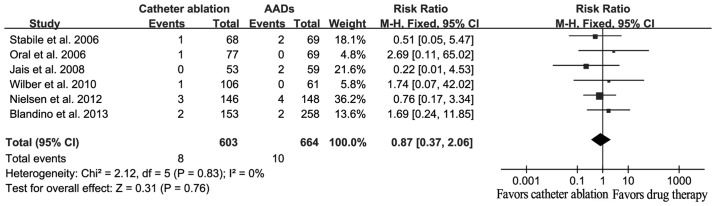
Forest plot of the effects of catheter ablation vs. AADs on all-cause mortality. AAD, antiarrhythmic drugs; CI, confidence interval.
A total of 17 strokes/TIA were reported, among which 10 events occurred in catheter ablation patients and seven events occurred in AAD patients. However, no statistically significant difference was detected between the catheter ablation and AAD therapies (RR, 1.83; 95% CI, 0.73–4.55; P=0.20; Fig. 5), and there was no evident heterogeneity (Q=0.39; I2=0%; P=0.98).
Figure 5.
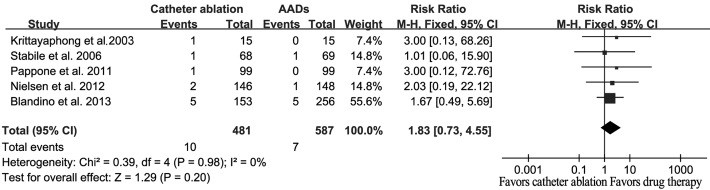
Forest plot of the effects of catheter ablation vs. AADs on stroke/transient ischemic attack. AAD, antiarrhythmic drug; CI, confidence interval.
Four studies included results with regard to the differences in the QoL outcome, including the physical component summary (PCS) and the mental component summary (MCS). When compared with the baseline observations, the catheter ablation and AAD treatment groups exhibited a significantly improved QoL at the end of the study. However, catheter ablation was shown to result in improved QoL outcomes compared with AADs (PCS: WMD, 2.23; 95% CI, 0.24–4.21; P=0.03; MCS: WMD, 2.69; 95% CI, 0.04–5.35; P=0.05; Fig. 6).
Figure 6.
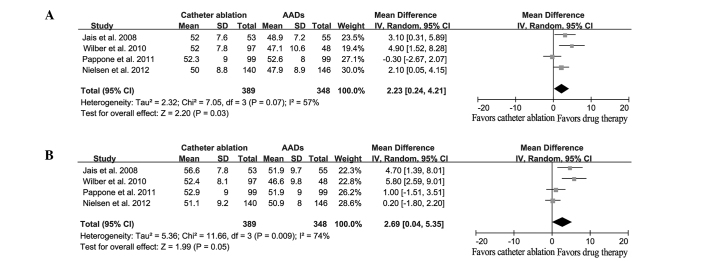
Forest plot of the effects of catheter ablation vs. AADs on the quality of life. (A) Physical component summary and (B) mental component summary. AAD, antiarrhythmic drug; SD, standard deviation; IV, independent variable; CI, confidence interval.
Quality assessment and publications bias
The quality of the evidence was evaluated using the GRADE system. As shown in Table II, the evidence quality of the outcomes ranged between low and high. Potential publication bias was assessed using Begg's funnel plot and Egger's test, and the results indicated that there was no potential publication bias (Fig. 7; Egger's test, P=0.066).
Table II.
Summary of findings with regard to the quality of the evidence of outcomes.
| Illustrative comparative risks (95% CI) | |||||
|---|---|---|---|---|---|
| Outcomes | Assumed risk of AADs | Corresponding risk catheter ablation | RR (95% CI) | Participants (studies), n | Quality of the evidence (GRADE) |
| AF recurrence | 552 per 1,000 | 259 per 1,000 (210–320) | 0.47 (0.38–0.58) | 1,763 (11) | ++++High |
| All-causes mortality | 15 per 1,000 | 13 per 1,000 (6–31) | 0.87 (0.37–2.06) | 1,267 (6) | +++−Moderatea |
| Stroke/TIA | 12 per 1,000 | 22 per 1,000 (9–54) | 1.83 (0.73–4.55) | 1,068 (5) | +++−Moderatea |
| QoL PCS | – | – | 2.23 (0.24–4.21) | 737 (4) | ++−−Lowb,c |
| QoL MCS | – | – | 2.69 (0.04–5.35) | 737 (4) | ++−−Lowb,c |
Assumed risk of AADs is presented as the mean baseline risk of the studies included in the meta-analysis.
Number of events was small.
Blinding of assessment was impossible.
95% CI range was large. CI, confidence interval; GRADE, Grading of Recommendations, Assessment, Development and Evaluations; AF, atrial fibrillation; RR, relative risk; TIA, transient ischemic attack; AADs, antiarrhythmic drugs; QoL, quality of life; PCS, physical component summary; MCS, mental component summary.
Figure 7.
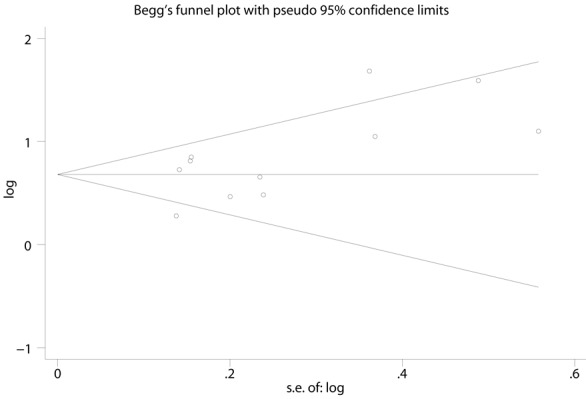
Beggs funnel plot for assessment of potential publication bias.
Discussion
The primary finding of the present meta-analysis was that the recurrence of AF was notably reduced in patients that received catheter ablation therapy, as compared with those that received AADs. Furthermore, catheter ablation treatment was shown to result in an improved QoL when compared with AADs. However, no statistically significant difference was identified between two groups with regard to the incidence of all-cause mortality and stroke/TIA.
In the present study, a significant reduction in recurrent AF was observed in the patients who underwent catheter ablation therapy, as compared with the patients that received AADs. Restoration of a sinus rhythm is considered to improve the long-term survival rates and reduce the incidence of stroke/TIA in general AF patients (22,23). In addition, a previous observational study indicated that catheter ablation is superior to AADs in reducing the all-cause mortality rate (24). However, in the present meta-analysis, no statistically significant difference was detected between the catheter ablation and AAD therapy with regard to the rates of mortality and stroke/TIA, for which there are a number of possible explanations. Firstly, the current study design was different to that of the aforementioned observational study, with only RCTs included in the current meta-analysis. RCTs are considered to provide the most robust evidence for clinical practice; however, the number of participants enrolled may be insufficient to obtain statistical differences. Secondly, the duration of the follow-up period in the majority of the trials was only 12 months, which may be too short to detect a representative quantity of adverse events, particularly considering that patients in RCTs are typically younger and exhibit a low prevalence of structural heart disease. These factors limited the value of the studies for the evaluation of the long-term efficacy of catheter ablation. However, the ongoing multicenter, randomized Catheter Ablation versus Antiarrhythmic Drug Therapy for Atrial Fibrillation (CABANA) trial (no. NCT00911508), which plans to enroll >3,000 patients, may resolve this problem.
QoL is a key factor to consider when selecting a method of AF management. Theoretically, early catheter ablation is able to avoid the requirement for long-term drug employment and the subsequent side effects. The present study indicated that patients who underwent catheter ablation therapy had an improved QoL compared with patients that received AADs. However, the assessment of QoL is subjective, and as catheter ablation is distinct from drug therapy, blinding of the assessment is impossible. Furthermore, according to the GRADE system, the quality of evidence of QoL as a parameter is assessed as ‘low’. Therefore, further studies may be required to elucidate this issue.
Cost-effectiveness is an additional key factor to take into consideration when comparing treatments for AF. However, was the ablation technique and duration differed between study centers, it is difficult to precisely evaluate the cost-effectiveness of catheter ablation compared with AADs for AF therapy. The limited information available did not permit a consensus on the cost-effectiveness of catheter ablation for AF (25–28). Thus, the cost comparison of catheter ablation and AADs requires further investigation in future RCTs.
Prior to the present study, a number of previous meta-analyses were published that compared catheter ablation with AADs for the treatment of AF (29–31). However, the present study possesses a number of advantages compared with the previous studies. Firstly, the present meta-analysis included more recently published trials, and the number of AF patients included in this meta-analysis was twice the number reported in previous studies. Furthermore, the present study analyzed a number of outcome markers, in addition to the primary endpoint (recurrent AF), including all-cause mortality, stroke/TIA and the change of QoL. In addition, in the present study, the quality of evidence was assessed using the GRADE system, as proposed by the Cochrane Collaboration.
However, the current meta-analysis contains a number of limitations, and the present results require cautious interpretation. Firstly, the trials included in the meta-analysis used different ablation techniques and different methods to monitor the recurrence of AF. These variations are consistent with the current status in clinical practice. Secondly, unlike real clinical practice, AF patients included in the present analysis were relatively young, with no serious structural heart diseases, and only one study (11) enrolled elderly patients (≥70 years). Thus, when appraising the results of the present study in the real clinical practice setting, the aforementioned limitations should be considered.
In conclusion, the results of the present study demonstrated that catheter ablation therapy is superior to AADs in reducing the recurrence of AF and improving the QoL. However, there is insufficient evidence to suggest that catheter ablation is superior to AADs in reducing the long-term severe adverse events, including all-cause mortality and stroke/TIA. This issue may be clarified by the future CABANA trial (no. NCT00911508).
References
- 1.Naccarelli GV, Varker H, Lin J, Schulman KL. Increasing prevalence of atrial fibrillation and flutter in the United States. Am J Cardiol. 2009;104:1534–1539. doi: 10.1016/j.amjcard.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 2.Wilke T, Groth A, Mueller S, et al. Incidence and prevalence of atrial fibrillation: An analysis based on 8.3 million patients. Europace. 2013;15:486–493. doi: 10.1093/europace/eus333. [DOI] [PubMed] [Google Scholar]
- 3.Zhou ZQ, Hu DY. An epidemiological study on the prevalence of atrial fibrillation in the Chinese population of mainland China. J Epidemiol. 2008;18:209–216. doi: 10.2188/jea.JE2008021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Piccini JP, Hammill BG, Sinner MF, et al. Incidence and prevalence of atrial fibrillation and associated mortality among Medicare beneficiaries, 1993–2007. Circ Cardiovasc Qual Outcomes. 2012;5:85–93. doi: 10.1161/CIRCOUTCOMES.111.962688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Camm AJ, Lip GY, De Caterina R, et al. ESC Committee for Practice Guidelines (CPG): 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: An update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33:2719–2747. doi: 10.1093/eurheartj/ehs253. [DOI] [PubMed] [Google Scholar]
- 6.Wann LS, Curtis AB, January CT, et al. 2006 Writing Committee Members; ACCF/AHA Task Force Members: 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (updating the 2006 guideline): A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;123:104–123. doi: 10.1161/CIR.0b013e3181fa3cf4. [DOI] [PubMed] [Google Scholar]
- 7.Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: The Framingham Heart Study. Circulation. 1998;98:946–952. doi: 10.1161/01.CIR.98.10.946. [DOI] [PubMed] [Google Scholar]
- 8.Verma A, Macle L, Cox J, Skanes AC. (CCS Atrial Fibrillation Guidelines Committee). Canadian Cardiovascular Society atrial fibrillation guidelines 2010: Catheter ablation for atrial fibrillation/atrial flutter. Can J Cardiol. 2011;27:60–66. doi: 10.1016/j.cjca.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Krittayaphong R, Raungrattanaamporn O, Bhuripanyo K, et al. A randomized clinical trial of the efficacy of radiofrequency catheter ablation and amiodarone in the treatment of symptomatic atrial fibrillation. J Med Assoc Thai. 2003;86(Suppl 1):8–16. [PubMed] [Google Scholar]
- 10.Wazni OM, Marrouche NF, Martin DO, et al. Radiofrequency ablation vs. antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: A randomized trial. JAMA. 2005;293:2634–2640. doi: 10.1001/jama.293.21.2634. [DOI] [PubMed] [Google Scholar]
- 11.Oral H, Pappone C, Chugh A, et al. Circumferential pulmonary-vein ablation for chronic atrial fibrillation. N Engl J Med. 2006;354:934–941. doi: 10.1056/NEJMoa050955. [DOI] [PubMed] [Google Scholar]
- 12.Stabile G, Bertaglia E, Senatore G, et al. Catheter ablation treatment in patients with drug-refractory atrial fibrillation: A prospective, multi-centre, randomized, controlled study (Catheter Ablation For The Cure Of Atrial Fibrillation Study) Eur Heart J. 2006;27:216–221. doi: 10.1093/eurheartj/ehi583. [DOI] [PubMed] [Google Scholar]
- 13.Jais P, Cauchemez B, Macle L, et al. Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: Rhe A4 study. Circulation. 2008;118:2498–2505. doi: 10.1161/CIRCULATIONAHA.108.772582. [DOI] [PubMed] [Google Scholar]
- 14.Forleo GB, Mantica M, De Luca L, et al. Catheter ablation of atrial fibrillation in patients with diabetes mellitus type 2: Results from a randomized study comparing pulmonary vein isolation versus antiarrhythmic drug therapy. J Cardiovasc Electrophysiol. 2009;20:22–28. doi: 10.1111/j.1540-8167.2008.01275.x. [DOI] [PubMed] [Google Scholar]
- 15.Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: A randomized controlled trial. JAMA. 2010;303:333–340. doi: 10.1001/jama.2009.2029. [DOI] [PubMed] [Google Scholar]
- 16.Pappone C, Vicedomini G, Augello G, et al. Radiofrequency catheter ablation and antiarrhythmic drug therapy: A prospective, randomized, 4-year follow-up trial: The APAF study. Circ Arrhythm Electrophysiol. 2011;4:808–814. doi: 10.1161/CIRCEP.111.966408. [DOI] [PubMed] [Google Scholar]
- 17.Morillo CA, Verma A, Connolly SJ, Kuck KH, Nair GM, Champagne J, Sterns LD, Beresh H, Healey JS, Natale A. (RAAFT-2 Investigators). Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation (RAAFT 2): A randomized trial. JAMA. 2014;311:692–700. doi: 10.1001/jama.2014.467. [DOI] [PubMed] [Google Scholar]
- 18.Cosedis Nielsen J, Johannessen A, Raatikainen P, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med. 2012;367:1587–1595. doi: 10.1056/NEJMoa1113566. [DOI] [PubMed] [Google Scholar]
- 19.Blandino A, Toso E, Scaglione M, et al. Long-term efficacy and safety of two different rhythm control strategies in elderly patients with symptomatic persistent atrial fibrillation. J Cardiovasc Electrophysiol. 2013;24:731–738. doi: 10.1111/jce.12126. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration. [Mar;2011 ]. 2011. www.cochrane-handbook.org www.cochrane-handbook.org updated. Available from.
- 21.Guyatt GH, Oxman AD, Vist GE, et al. (GRADE Working Group). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ionescu-Ittu R, Abrahamowicz M, Jackevicius CA, et al. Comparative effectiveness of rhythm control vs rate control drug treatment effect on mortality in patients with atrial fibrillation. Arch Intern Med. 2012;172:997–1004. doi: 10.1001/archinternmed.2012.2266. [DOI] [PubMed] [Google Scholar]
- 23.Tsadok MA, Jackevicius CA, Essebag V, et al. Rhythm versus rate control therapy and subsequent stroke or transient ischemic attack in patients with atrial fibrillation. Circulation. 2012;126:2680–2687. doi: 10.1161/CIRCULATIONAHA.112.092494. [DOI] [PubMed] [Google Scholar]
- 24.Pappone C, Rosanio S, Augello G, et al. Mortality, morbidity and quality of life after circumferential pulmonary vein ablation for atrial fibrillation: Outcomes from a controlled nonrandomized long-term study. J Am Coll Cardiol. 2003;42:185–197. doi: 10.1016/S0735-1097(03)00577-1. [DOI] [PubMed] [Google Scholar]
- 25.Khaykin Y, Wang X, Natale A, et al. Cost comparison of ablation versus antiarrhythmic drugs as first-line therapy for atrial fibrillation: An economic evaluation of the RAAFT pilot study. J Cardiovasc Electrophysiol. 2009;20:7–12. doi: 10.1111/j.1540-8167.2008.01303.x. [DOI] [PubMed] [Google Scholar]
- 26.McKenna C, Palmer S, Rodgers M, et al. Cost-effectiveness of radiofrequency catheter ablation for the treatment of atrial fibrillation in the United Kingdom. Heart. 2009;95:542–549. doi: 10.1136/hrt.2008.147165. [DOI] [PubMed] [Google Scholar]
- 27.Reynolds MR, Zimetbaum P, Josephson ME, Ellis E, Danilov T, Cohen DJ. Cost-effectiveness of radiofrequency catheter ablation compared with antiarrhythmic drug therapy for paroxysmal atrial fibrillation. Circ Arrhythm Electrophysiol. 2009;2:362–369. doi: 10.1161/CIRCEP.108.837294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Noro M, Kujime S, Ito N, et al. Cost effectiveness of radiofrequency catheter ablation vs. medical treatment for atrial fibrillation in Japan. Cost performance for atrial fibrillation. Circ J. 2011;75:1860–1866. doi: 10.1253/circj.CJ-10-0793. [DOI] [PubMed] [Google Scholar]
- 29.Noheria A, Kumar A, Wylie JV, Jr, Josephson ME. Catheter ablation vs. antiarrhythmic drug therapy for atrial fibrillation: A systematic review. Arch Intern Med. 2008;168:581–586. doi: 10.1001/archinte.168.6.581. [DOI] [PubMed] [Google Scholar]
- 30.Piccini JP, Lopes RD, Kong MH, Hasselblad V, Jackson K, Al-Khatib SM. Pulmonary vein isolation for the maintenance of sinus rhythm in patients with atrial fibrillation: A meta-analysis of randomized, controlled trials. Circ Arrhythm Electrophysiol. 2009;2:626–633. doi: 10.1161/CIRCEP.109.856633. [DOI] [PubMed] [Google Scholar]
- 31.Bonanno C, Paccanaro M, La Vecchia L, Ometto R, Fontanelli A. Efficacy and safety of catheter ablation versus antiarrhythmic drugs for atrial fibrillation: A meta-analysis of randomized trials. J Cardiovasc Med (Hagerstown) 2010;11:408–418. doi: 10.2459/JCM.0b013e328332e926. [DOI] [PubMed] [Google Scholar]