Abstract
Background
Cosmic radiation and circadian disruption are potential reproductive hazards for flight attendants.
Methods
Flight attendants from 3 US airlines in 3 cities were interviewed for pregnancy histories and lifestyle, medical, and occupational covariates. We assessed cosmic radiation and circadian disruption from company records of 2 million individual flights. Using Cox regression models, we compared respondents (1) by levels of flight exposures and (2) to teachers from the same cities, to evaluate whether these exposures were associated with miscarriage.
Results
Of 2654 women interviewed (2273 flight attendants and 381 teachers), 958 pregnancies among 764 women met study criteria. A hypothetical pregnant flight attendant with median firsttrimester exposures flew 130 hours in 53 flight segments, crossed 34 time zones, and flew 15 hours during her home-base sleep hours (10 pm–8 am), incurring 0.13 mGy absorbed dose (0.36 mSv effective dose) of cosmic radiation. About 2% of flight attendant pregnancies were likely exposed to a solar particle event, but doses varied widely. Analyses suggested that cosmic radiation exposure of 0.1 mGy or more may be associated with increased risk of miscarriage in weeks 9–13 (odds ratio = 1.7 [95% confidence interval = 0.95–3.2]). Risk of a first-trimester miscarriage with 15 hours or more of flying during home-base sleep hours was increased (1.5 [1.1–2.2]), as was risk with high physical job demands (2.5 [1.5–4.2]). Miscarriage risk was not increased among flight attendants compared with teachers.
Conclusions
Miscarriage was associated with flight attendant work during sleep hours and high physical job demands and may be associated with cosmic radiation exposure.
The commercial aircraft cabin environment is the work-place of approximately 168,000 flight personnel in the United States, including pilots, copilots, and 93,100 flight attendants,1 of whom 84% are female.2 The International Agency for Research on Cancer (IARC) estimates 250,000 aircrew worldwide are monitored for radiation exposure3; US airline crew are not currently monitored. Reproductive problems among female flight attendants have been reported since the 1960s, including adverse pregnancy outcomes4–6 and menstrual irregularities.7 Workplace exposures of concern include cosmic ionizing radiation8 and circadian rhythm disruption.9 Galactic cosmic radiation generates secondary and tertiary radiation at aircraft altitudes,10 including neutrons and energetic photons (IARC-known human [group 1] carcinogens).3 Solar particle events (transient solar surface eruptions) are another source of cosmic radiation exposure. Flying across time zones or working during normal sleep hours can affect reproductive hormones with circadian regulation.11 These exposures are different from those of other occupational groups exposed to terrestrial radiation or shift work.12 We evaluated the risk of miscarriage among flight attendants and a comparison group of teachers and assessed whether cosmic radiation, circadian disruption, and other occupational exposures were associated with miscarriage.
METHODS
Questionnaire
The Institutional Review Board of the National Institute for Occupational Safety and Health approved the study; participants provided informed consent. Three US airlines with domiciles (or hubs) in 3 US cities13 provided work histories for female flight attendants employed during the study period (1 August 1992 to 31 July 1996). Teachers were selected as a comparison group because of minimal air travel and few reproductive hazards.14 Local school districts in the same regions provided work histories for teachers. Eligibility was determined as age 18–45 years during the study period; full-time employment as a flight attendant or teacher for at least 1 month during the study period; in a marital relationship anytime during the study period (to increase pregnancy likelihood); and not surgically sterilized before the study period. Women were further considered eligible for the analysis of miscarriage if they had reported 1 or more singleton pregnancies in the study period during which they were employed as a flight attendant or teacher. Medical and reproductive histories were obtained by computer-assisted telephone interviews conducted from 3 November 1999 through 13 April 2001, along with the following variables: occupational exposures during pregnancy (physical job demands, psychosocial stressors, and environmental tobacco smoke); age; use of tobacco, caffeine, alcohol, and recreational drugs; physical activity; paternal occupation; and whether a physician was consulted for a miscarriage. Miscarriage was defined as self-reported involuntary termination of a recognized pregnancy through the 20th gestational week; early miscarriage was considered 13 or fewer weeks. The estimated date of the last menstrual period (LMP) was considered the beginning date of the pregnancy and was calculated during the interview from self-reported gestational age and date at the end of the pregnancy.
Because of the potential for differential recall of pregnancy outcomes, medical records for confirmation of miscarriage were obtained if authorized by the study participant. Vital statistics data were obtained for reported births and fetal deaths. Birth certificates were also used to validate prior fetal losses within the study period if they were indicated on the certificate of a subsequent child and to calculate date of LMP when the mother's report was uncertain.
Exposure Assessment
Weekly exposures were estimated from the LMP through the date the pregnancy ended or was right-censored. Radiation and circadian disruption exposures were assessed from company records of work flights and uncompensated passenger flying and questionnaire report of commuter flying to and from the airline domicile city to work.13,15 Where records permitted, radiation and circadian disruption exposures during the 6 months prior to LMP were also estimated as an indicator of prepregnancy exposures. Teachers’ air travel was estimated from the questionnaires.
For each single nonstop flight between 2 cities (flight segment), data were extracted from records, calculated, or imputed: date flight began, origin and destination cities, block time (airborne plus taxi times), and local departure and arrival times.13 We estimated cosmic radiation dose for more than 99.9% of 1,984,285 flight segments. The Federal Aviation Administration program CARI6P16 (screen version 17 September 2005) was used to estimate galactic cosmic radiation doses for each flight segment.13,15 Dynamic solar particle event dose-rate data from the National Aeronautics and Space Administration's Nowcast of Atmospheric Ionizing Radiation for Aviation Safety model were applied to estimate solar particle event dose to add to galactic cosmic radiation dose for flight segments that possibly traveled through a solar particle event17; solar particle event dose rates are not calculated by CARI6P.18,19 To measure chronic circadian disruption, we used 2 metrics calculated from airline records: cumulative time zones crossed (without regard to travel direction) and Standard Sleep Interval travel, a separate measure of sleep disturbance (time spent flying during the time encompassing 10 pm to 8 am at the flight attendant's domicile).9,15 Both of these metrics are related to a biomarker of chronic circadian disruption in flight attendants, the day-to-day variance in flight attendant overnight melatonin excretion.9
Additional occupational exposures from the questionnaire included workplace exposures to environmental tobacco smoke and psychosocial stressors. High physical job demands was defined as (1) being on your feet (standing and walking) more than 8 hours/day or (2) 2 or more of the following: lifting or carrying objects that weigh at least 15 pounds more than 10 times a day, bending at the waist more than 25 times/day, and pushing or pulling heavy objects requiring at least 15 pounds of force or effort 20 or more times/day.
Statistical Methods
All analyses were performed using SAS software (version 9.3; SAS Institute Inc., Cary, NC). The rate of miscarriage by gestational week was estimated using lifetable methods.20 We used Cox proportional hazards regression models modified for discrete time data to evaluate the risk of miscarriage in flight attendants compared with teachers, adjusting for potential confounders. Additional modeling limited to flight attendants evaluated cosmic ionizing radiation, time zones crossed, and Standard Sleep Interval travel in conjunction with occupational exposure to cigarette smoke and high physical job demands, adjusting for potential confounders. Models were fit using the PHREG procedure with the TIES = DISCRETE option. Discrete Cox model results are reported as odds ratios (ORs), which can be interpreted as relative risks.21 Robust sandwich variance estimates accounted for nonindependent pregnancy outcomes.22 Gestational age (weeks since LMP) was the underlying time variable. Because the risk of miscarriage can vary by gestational week, we evaluated the risk of early miscarriage (ie, in the first trimester, defined as through gestational week 13) but could not evaluate the risk of a late miscarriage (gestational weeks 14–20) or stillbirths due to the small numbers of events (187 early miscarriages vs. only 18 late miscarriages and 5 stillbirths). Because the week the pregnancy became known was not available, we excluded losses occurring in weeks 1–3 and followed pregnancies left-truncated at week 4 until the date the pregnancy ended. All pregnancies were right-censored at 13 weeks.
Cumulative absorbed dose, time zones crossed, and hours of Standard Sleep Interval travel were considered time dependent and evaluated from LMP through the cutoff week (ie, the week of miscarriage within risk sets). Although other exposure approaches and cutpoints were considered, these exposures were dichotomized at the median cumulative exposure using static cutpoints based on all pregnancies ending in miscarriage in weeks 4–13. The use of dichotomous variables for exposure was intended to reduce the effects of collinearity and limited sample size in combined exposure models. Cigarette smoke and high physical job demands were treated as fixed exposures.
Because radiation dose and time zones crossed were highly correlated (Pearson correlation = 0.89) but less correlated with Standard Sleep Interval travel (Pearson correlations = 0.67 and 0.66, respectively), we evaluated the flying exposures one at a time and in combined models that considered 2 exposures simultaneously using 4 categories (low in both exposures, low in one but high in the other, and high in both exposures).
We evaluated confounding by demographic characteristics (race, Hispanic ethnicity, education, and income), physical variables (maternal age at LMP and body mass index), reproductive history (parity), lifestyle characteristics (cigarette smoking, alcohol consumption, home stress, use of very hot baths/hot tub/sauna, and high vigorous physical activity), medical history (thyroid condition, benign tumors of the reproductive organs, pelvic inflammatory disease, sexually transmitted infections, cervical procedures, fibroid procedures, infections, fever, injury, and x-rays to the torso), and workplace psychosocial stressors. First, associations of covariates with miscarriage and exposures were evaluated using log-binomial regression, t tests, chi-square tests, and nonparametric tests, as appropriate. Potential confounders that were associated with both the outcome and the exposure at a 20% significance level were identified and included in multivariate modeling. In models, confounding was evaluated by comparing crude and adjusted model estimates using a 15% change-in-estimate rule. The span of maternal age at the LMP among study pregnancies was less than 15 years; departures from linearity were not observed when higher order terms were included in the model.
A requirement of the study was that participants reported working as a flight attendant or school teacher during the pregnancy; however, for some flight attendant pregnancies, company flight records did not indicate any flying (working flights or uncompensated passenger flights) during the pregnancy (n = 79 pregnancies). Flight attendants have some control over which flights they choose to fly, which typically increases with seniority at commercial airlines. Because a flight attendant who elected to not fly during the pregnancy might be different from flight attendants who did fly during the pregnancy, we separated nonflyers from the low-exposed comparison group when we modeled the flying exposures.
We evaluated the proportional odds assumption for the occupational exposures by including a time-dependent interaction term in the model and performing a likelihood ratio test for interaction. We report separate estimates for gestational weeks 4–8 and 9–13; we do not report estimates for the combined period 4–13 weeks when the proportional odds assumption was not met. Note that models of the 4- to 8-week time period include losses that occur in weeks 9–13 but censor them at week 8.
Sensitivity analyses included omitting miscarriages for which the pregnancy was not reported to a doctor and the miscarriage was not diagnosed or treated by a doctor or in a hospital (n = 5); omitting women diagnosed with certain immune disorders (arthritis, Crohn's disease, fibromyalgia, and eosinophilia-myalgia syndrome; n = 5); changing the starting week of pregnancy analysis to weeks 5, 6, or 7; analyzing with a log-binomial model (reanalyzing with time-varying covariates treated as fixed average values, ignoring proportional hazards assumptions); modeling exposures with time-dependent median cutpoints (rather than fixed median cutpoints); excluding nonflying flight attendants from models rather than categorizing them in a different group than the flight attendants with low exposures; and modeling solar particle events as time-dependent dichotomous exposures.
RESULTS
Study Population
Of 2595 eligible flight attendants among 5096 successfully contacted, 2273 (88%) agreed to be interviewed; after exclusions, 673 flight attendants had 1 or more eligible pregnancies for a total of 840 study pregnancies analyzed. Of 466 eligible teachers among 1582 successfully contacted, 381 (82%) agreed to be interviewed; 91 teachers had 1 or more eligible pregnancies for a total of 118 study pregnancies analyzed (eTable 1; http://links.lww.com/EDE/A862).
The miscarriage rate among study pregnancies by gestational week is shown in the Figure. We obtained 43% of flight attendants’ birth and medical records and 30% of teachers’ for the study of miscarriages or stillbirths. Of those, we confirmed the outcome for 82% of flight attendants and 100% of teachers. Of the 14 flight attendant miscarriages not confirmed, 13 were not reported on the birth or medical record and 1 birth certificate included an additional outcome (induced abortion) that could not be distinguished from the reported miscarriage.
FIGURE.
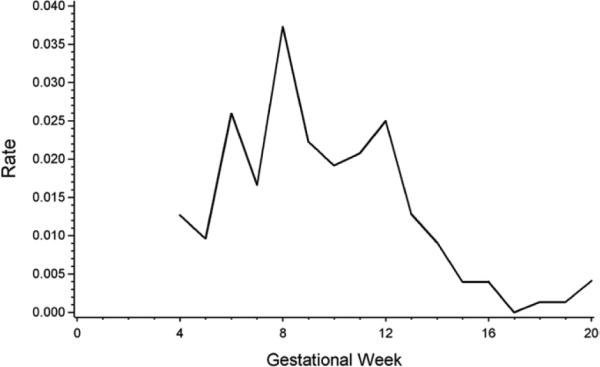
Miscarriage rate among study pregnancies by gestational week from the last menstrual period.
Flight attendants were more likely to be white and of higher family income than teachers, who were more likely to be college graduates than flight attendants. Flight attendants were more likely to have had cervical procedures before or during pregnancy (11% vs. 4%). The 2 groups were similar in gravidity, parity, and number of previous miscarriages at the time of each pregnancy (Table 1). At work, flight attendants were more likely than teachers to be exposed to tobacco smoke (18% vs. 3%), incur high physical job demands (80% vs. 21%), and score higher on several workplace psychosocial stressors.
TABLE 1.
Study Demographic Variables and Other Covariates for the Miscarriage Analysis
| Characteristic | Flight Attendants | Teachers |
|---|---|---|
| Study women; no.a | 673 | 91 |
| Demographic variables | ||
| Age at interview (years); median (range) | 38 (26–19) | 37 (29–49) |
| Nonwhite race; no. (%) | 47 (7) | 15 (16) |
| Hispanic ethnicity; no. (%) | 48 (7) | 3 (3) |
| Body mass index at interview (kg/m2); median (range) | 21 (17–38) | 23 (17–45) |
| Education; no. (%) | ||
| No collegeb | 89 (13) | 0 (0) |
| Some college | 292 (43) | 1 (1) |
| College graduate or higher | 292 (43) | 90 (99) |
| Annual family income; no. (%) | ||
| Unknown | 13 | 0 |
| <$50,000 | 92 (14) | 21 (23) |
| $50,000–$74,999 | 166 (25) | 26 (29) |
| $75,000 or higher | 402 (61) | 44 (48) |
| Study pregnancies; no.c | 840 | 118 |
| Time from end of pregnancy to interview (years); median (range) | 5.5 (3.0–8.1) | 5.6 (3.4–8.0) |
| Reproductive factors during pregnancy | ||
| Age at last menstrual period (years); median (range) | 32 (20–43) | 31 (24–42) |
| Gravidity (no. previous pregnancies); no. (%) | ||
| Unknown | 30 | 0 |
| 0 | 298 (37) | 49 (42) |
| 1 | 272 (34) | 28 (24) |
| 2+ | 240 (30) | 41 (35) |
| Parity (no. previous live births); no. (%) | ||
| Unknown | 16 | 0 |
| No prior pregnancies | 298 | 49 |
| 0 | 199 (38) | 20 (29) |
| 1 | 243 (46) | 39 (57) |
| 2+ | 84 (16) | 10 (14) |
| No. previous miscarriages; no. (%) | ||
| Unknown | 23 | 0 |
| No prior pregnancies | 298 | 49 |
| 0 | 312 (60) | 37 (54) |
| 1 | 160 (31) | 25 (36) |
| 2+ | 47 (9) | 7 (10) |
| Years since last pregnancy; median (range) | 1.8 (0–19) | 1.9 (0.3–14) |
| Occupational factors during pregnancy | ||
| Job tenure at last menstrual period (years); median (range)d | 6.3 (0.1–23) | NA |
| Exposed to coworkers’, customers’, or clients’ smoke in pregnancy | 152 (18) | 4 (3) |
| Low job control at work in pregnancye | 216 (26) | 18 (15) |
| Low supervisor support in pregnancyf | 651 (79) | 61 (53) |
| Somewhat hard or very hard physical effort at work in pregnancy | 441 (53) | 19 (16) |
| High physical job demands in pregnancyg | 665 (80) | 24 (21) |
| Lifting/carrying at least 15 pounds more than 10 times/day at work in pregnancy | 433 (52) | 12 (10) |
| Being on feet more than 8 hours/day at work in pregnancy | 474 (57) | 16 (14) |
| Bending at the waist more than 25 times/day at work in pregnancy | 675 (82) | 44 (38) |
| Pushing/pulling at least 15 pounds 20 or more times/day at work in pregnancy | 521 (63) | 8 (7) |
| Husband's occupation; no. (%) | ||
| Reproductive hazard exposure possibleh | 159 (20) | 19 (17) |
| Reproductive hazard exposure not likely | 485 (61) | 91 (83) |
| Flight crew | 148 (19) | 0 (0) |
| Lifestyle factors during pregnancy | ||
| Smoked during first trimester | 31 (4) | 3 (3) |
| Lived with a smoker during pregnancy | 47 (6) | 10 (8) |
| Smoked or lived with a smoker during pregnancy | 71 (9) | 11 (9) |
| Caffeine use in first trimesteri | ||
| None | 320 (39) | 54 (46) |
| Low | 330 (40) | 41 (35) |
| High | 179 (22) | 23 (19) |
| Alcohol use in first trimester | 208 (25) | 26 (22) |
| Home stress in pregnancyj | 230 (28) | 34 (29) |
| Any children at home under age 4 years in pregnancy | 278 (34) | 36 (31) |
| Any use of very hot baths or hot tubs/sauna in pregnancy | 199 (24) | 38 (32) |
| High use (>4/month) of very hot baths or hot tubs/sauna in pregnancy | 69 (8) | 14 (12) |
| High vigorous physical activity (>120 minutes/week) in pregnancy | 271 (33) | 32 (27) |
| Medical factors during pregnancy | ||
| Bladder, kidney, urinary tract infection in first trimester | 20 (2) | 1 (1) |
| Illness with fever in first trimester | 13 (2) | 1 (1) |
| Injury in first trimesterk | 8 (1) | 0 (0) |
| Selected injury in first trimesterl | 7 (1) | 0 (0) |
| X-rays or radiotherapy during first trimester or in 3 months before pregnancy | 17 (2) | 2 (2) |
| Thyroid condition prior to pregnancy or during first trimester | 16 (2) | 2 (2) |
| Benign tumor of the reproductive organs before or during pregnancy | 52 (6) | 7 (6) |
| Pelvic inflammatory disease before or during pregnancy | 23 (3) | 0 (0) |
| Chlamydia before or during pregnancy | 36 (4) | 5 (4) |
| Herpes, human papillomavirus, gonorrhea before or during pregnancy | 46 (6) | 7 (6) |
| Cervical procedures before or during pregnancy | 89 (11) | 5 (4) |
| Fibroid procedures before or during pregnancy | 15 (2) | 1 (1) |
Due to missing values, sample size varies (660–673 for flight attendants; 90–91 for teachers).
Percentages may not sum to 100 due to rounding.
Summary statistics assume independence among the study pregnancies and are not adjusted for other variables. Due to missing values, sample size varies (792–840 for flight attendant pregnancies; 110–118 for teacher pregnancies).
Job tenure at last menstrual period is based on company-provided hire dates for flight attendant pregnancies and not available for teacher pregnancies.
Low job control defined as “your job allowed you to make a lot of decisions on your own”: never, seldom, or sometimes.
Low supervisor support defined as “management was concerned about the welfare of employees”: never, seldom, or sometimes.
High physical job demands defined as (1) being on your feet (including standing and walking) more than 8 hours/day or (2) 2 or more of the following: lifting or carrying objects that weigh at least 15 pounds more than 10 times a day, bending at the waist more than 25 times/day, and pushing or pulling heavy objects requiring at least 15 pounds of force or effort 20 or more times/day.
Job title, business, and main duties data for husbands during the pregnancy were categorized by expert judgment and consultation with National Institute for Occupational Safety and Health industrial hygienists, based on understanding of reproductive hazards in a variety of workplaces.
Caffeine use defined as any consumption of caffeinated coffee, tea, or soft drinks during the relevant time period. High caffeine use defined as daily caffeine consumption exceeding 85 mg computed from the usual number of drinks/day of caffeinated coffee (~85 mg/drink), tea (~40 mg/drink), and soft drinks (~36 mg/drink) during the relevant time period.
Home stress during pregnancy defined as 2 or more of the following: (1) responsibilities at home were shared with others never, seldom, or sometimes, (2) exposed to hostility or conflict at home sometimes, often, or all the time, and (3) having a close friend or family member with whom I could talk about my true feelings when I needed to never, seldom, or sometimes; or 1 or more of the following: (1) responsibilities at home were shared with others never or seldom, (2) exposed to hostility or conflict at home sometimes, often, or all the time, or (3) having a close friend or family member with whom I could talk about my true feelings when I needed to never or seldom.
Includes all injuries reported for the question “during this pregnancy, did you have any serious injury or an accident with injury that required a visit to a doctor?”
Limited to self-reported falls, auto accidents, or shock reported for the question “during this pregnancy, did you have any serious injury or an accident with injury that required a visit to a doctor?”
NA indicates not available.
A hypothetical pregnant flight attendant with median first-trimester exposures flew 130 block hours in 53 flight segments, crossed 34 time zones, and flew 15 hours in the Standard Sleep Interval (Table 2). From these flights, she incurred an absorbed radiation dose of 0.13 mGy (effective dose = 0.36 mSv [proton radiation weighting factor (wR) = 5]). In the same 3-month period, a teacher or nonflying flight attendant would receive an average of 0.14 mSv effective dose due to external irradiation from natural background: 0.083 mSv from space and 0.053 mSv from terrestrial radiation,23 compared with the flying flight attendant who received an average of 0.49 mSv, including both occupational exposure and exposure to background radiation while not flying. Based on records from 6 months before pregnancy, flight attendants incurred estimated median annual estimates of 700 block hours in 280 flight segments, crossed 184 time zones, and flew 76 hours in the Standard Sleep Interval. They incurred a median absorbed dose of 0.68 mGy (effective dose = 1.8 mSv, range = 0–5.8 mSv). Cumulative total absorbed dose from galactic cosmic radiation was highly correlated with cumulative absorbed dose from particle-specific components (electromagnetic showers, muons, neutrons, pions, and protons) and with cumulative effective dose (results not shown). Only 2 solar particle events of potential dose significance occurred during the study period (30 October to 4 November 1992 and 20–22 February 1994). About 2% of flight attendant pregnancies were likely exposed to a solar particle event during the pregnancy, but solar particle event doses varied widely. The 2 highest estimated solar particle event doses were 0.29 and 0.44 mGy (0.81 and 1.2 mSv) from single flights flown by flight attendants when they were not pregnant.
TABLE 2.
Occupational Radiation and Circadian Disruption Exposures Among 840 Flight Attendant Study Pregnancies and 118 Teacher Study Pregnanciesa
| Cumulative Exposurea |
|||||
|---|---|---|---|---|---|
| First Trimesterb |
Cumulative Weeks
1–20c |
Prior 6 Monthsd |
|||
| Flight Attendants |
Teachers |
Flight Attendants |
Teachers |
Flight Attendants |
|
| Metric | Median (Max) | Median (Max) | Median (Max) | Median (Max) | Median (Max) |
| Flight characteristics | |||||
| No. flight segments | 53 (140) | 0 (4.1) | 68.0 (210) | 0 (4.7) | 140 (390) |
| Block time (hours) | 130 (310) | 0 (5.9) | 180 (430) | 0 (6.4) | 350 (700) |
| No. time zones crossed | 34 (190) | 0 (4.1) | 41 (250) | 0 (6.00) | 92 (400) |
| Standard Sleep Interval travel (hours)e | 15 (220) | 0 (0) | 19 (270) | 0 (0) | 38 (320) |
| Travel through solar particle event (%) | 1.8 | NA | 2.0 | NA | 2.6 |
| Absorbed dose (mGy) | |||||
| Electromagnetic showers | 0.073 (0.27) | 0 (0.0037) | 0.095 (0.36) | 0 (0.0039) | 0.19 (0.56) |
| Muon | 0.014 (0.046) | 0 (0.00068) | 0.019 (0.060) | 0 (0.00072) | 0.036 (0.093) |
| Neutron | 0.029 (0.12) | 0 (0.0014) | 0.037 (0.16) | 0 (0.0015) | 0.073 (0.24) |
| Pion | 0.0011 (0.0039) | 0 (0.000056) | 0.0015 (0.0052) | 0 (0.000060) | 0.0029 (0.0082) |
| Proton | 0.015 (0.064) | 0 (0.00077) | 0.020 (0.084) | 0 (0.00081) | 0.039 (0.12) |
| Total | 0.13 (0.51) | 0 (0.0067) | 0.17 (0.68) | 0 (0.0071) | 0.34 (1.0) |
| Total including solar particle events | 0.13 (0.51) | NA | 0.17 (0.68) | NA | 0.34 (1.0) |
| Effective dose (mSv) | |||||
| Proton wR = 2 | 0.31 (1.30) | 0 (0.015) | 0.39 (1.7) | 0 (0.016) | 0.77 (2.4) |
| Proton wR = 5 | 0.36 (1.5) | 0 (0.018) | 0.46 (2.0) | 0 (0.019) | 0.90 (2.9) |
| Total including solar particle events, proton wR = 5 | 0.36 (1.5) | NA | 0.46 (2.0) | NA | 0.91 (2.9) |
Results reported to 2 significant figures. Minimum exposures were zero for all metrics. All statistics assume independence among the study pregnancies and are not adjusted for other variables. Although all study models used absorbed dose, we also present effective dose, a radiation protection metric. Median (maximum), except where indicated.
Exposures during the first trimester were assessed for 840 flight attendant and 118 teacher pregnancies. Exposures were summed from week 1 through the earlier of week 13 and the week the pregnancy ended. For flight attendant pregnancies, Standard Sleep Interval travel was set to missing for 37 flight attendant pregnancies because they had only uncompensated passenger travel during the first trimester, and Standard Sleep Interval travel could not be estimated for these flights. For teacher pregnancies, metrics involving solar particle events could not be assessed and were set to missing; all exposure metrics are zero for 88 teacher pregnancies because they reported no air travel during the pregnancy; and for the remaining 30 teacher pregnancies, Standard Sleep Interval travel could not be assessed and was set to missing.
Exposures during the first 20 weeks of pregnancy were assessed for 814 flight attendant pregnancies and 116 teacher pregnancies. Exposures were summed from week 1 through the earlier of week 20 and the week the pregnancy ended. Exposures are missing for 26 flight attendant and 2 teacher study pregnancies that contained time after the first-trimester outside of the window for which flight exposures were assessed.
Cumulative exposures during the 6 months prior to the pregnancy were not available for any teacher pregnancies and not available for 82 flight attendants pregnancies because airline records were not provided for this time period.
Estimated time spent flying during the Standard Sleep Interval defined from 10:00 pm to 8:00 am at the flight attendant's domicile (home base).
NA indicates not available; wR, radiation weighting factor.
Occupational Exposures and Miscarriage
Flight attendants were not more likely than teachers to experience a miscarriage (OR = 0.85 [95% confidence interval (CI) = 0.53–1.4], adjusted for first-trimester maternal age, parity, home stress, physical activity, and alcohol). Although adjustment for parity had little impact on the point estimates of our models (results not shown), it was included as a means to address the presence or absence of young children in a household, which could in turn affect several of our exposures, including stress and lifting.
Occupational exposures among flight attendants were first considered one at a time (Table 3). Model 8 provided evidence of an association between higher levels of absorbed radiation dose (≥0.1 mGy) and miscarriage in weeks 9–13 (OR = 1.7 [95% CI = 0.95–3.2]). Higher Standard Sleep Interval travel (≥15 hours) was associated with miscarriage during the first trimester (model 15 = 1.5 [1.1–2.2]). Associations were not observed for higher numbers of time zones crossed and miscarriage. When exposure metrics were evaluated 2 at a time (models 16–24), we observed increased odds of miscarriage for Standard Sleep Interval travel ≥15 hours (models 21 and 24). The models also show a modest cosmic radiation–miscarriage association (models 18 and 21). Flight attendants who did not fly during the pregnancy had higher odds of miscarriage compared with actively flying flight attendants with low occupational exposures.
TABLE 3.
Association of Occupational Exposures Among Flight Attendants with Early Miscarriage (Gestational Weeks 4–13) According to Time Period During Pregnancya
| Weeks 4–8 |
Weeks 9–13 |
Weeks 4–13 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variableb | No. Pregnancies | No. Miscarriages | OR (95% CI) | No. Pregnancies | No. Miscarriages | OR (95% CI) | No. Pregnancies | No. Miscarriages | OR (95% CI) |
| Any work flightsc | Model 1 | Model 2 | Model 3 | ||||||
| Yesd | 722 | 63 | 1.0 | 659 | 64 | 1.0 | 722 | 127 | 1.0 |
| No | 75 | 15 | 2.2 (1.3–3.7) | 60 | 5 | 0.78 (0.33–1.9) | 75 | 20 | 1.5 (0.97–2.5) |
| Coworkers or passengers smoked in pregnancy | |||||||||
| Nod | 651 | 55 | 1.0 | 596 | 51 | 1.0 | 651 | 106 | 1.0 |
| Yes | 146 | 23 | 1.7 (1.0–2.9) | 123 | 18 | 1.8 (1.0–3.0) | 146 | 41 | 1.8 (1.2–2.6) |
| Any work flightsc | Model 4 | Model 5 | Model 6 | ||||||
| Yesd | 722 | 63 | 1.0 | 659 | 64 | 1.0 | 722 | 127 | 1.0 |
| No | 75 | 15 | 2.4 (1.4–4.1) | 60 | 5 | 0.90 (0.37–2.2) | 75 | 20 | 1.7 (1.1–2.8) |
| Physical job demands in pregnancye | |||||||||
| Lowd | 157 | 8 | 1.0 | 149 | 6 | 1.0 | 157 | 14 | 1.0 |
| High | 640 | 70 | 2.2 (1.1–4.4) | 570 | 63 | 2.8 (1.3–6.4) | 640 | 133 | 2.5 (1.5–4.2) |
| Cumulative absorbed dose (mGy)f | Model 7 | Model 8 | Model 9 | ||||||
| No work flightsc | 75 | 15 | 2.3 (1.3–4.1) | 60 | 5 | 1.3 (0.46–3.6) | 75 | 20 | |
| <0.1 | 191 | 36 | 1.0 | 155 | 12 | 1.0 | 191 | 48 | NR |
| 0.1+ | 531 | 27 | 0.95 (0.55–1.6) | 504 | 52 | 1.7 (0.95–3.2) | 531 | 79 | |
| Cumulative time zones crossed | Model 10 | Model 11 | Model 12 | ||||||
| No work flightsc | 75 | 15 | 2.3 (1.3–4.1) | 60 | 5 | 0.92 (0.35–2.4) | 75 | 20 | 1.7 (1.0–2.9) |
| <30d | 281 | 38 | 1.0 | 243 | 23 | 1.0 | 281 | 61 | 1.0 |
| 30+ | 441 | 25 | 0.90 (0.54–1.5) | 416 | 41 | 1.2 (0.70–2.0) | 441 | 66 | 1.1 (0.75–1.6) |
| Cumulative Standard Sleep Interval travel (hours) | Model 13 | Model 14 | Model 15 | ||||||
| No work flightsc | 75 | 15 | 2.5 (1.4–4.5) | 60 | 5 | 1.2 (0.45–3.0) | 75 | 20 | 2.0 (1.2–3.4) |
| <15d | 342 | 39 | 1.0 | 303 | 24 | 1.0 | 342 | 63 | 1.0 |
| 15+ | 380 | 24 | 1.2 (0.70–2.0) | 356 | 40 | 1.8 (1.1–3.0) | 380 | 64 | 1.5 (1.1–2.2) |
| Absorbed dose and time zones crossed | Model 16 | Model 17 | Model 18 | ||||||
| No work flightsc | 75 | 15 | 2.3 (1.2–4.2) | 60 | 5 | 1.2 (0.42–3.4) | 75 | 20 | 1.9 (1.1–3.3) |
| Low–low (<0.1 mGy and <30 zones)d | 165 | 33 | 1.0 | 132 | 11 | 1.0 | 165 | 44 | 1.0 |
| Low–high (<0.1 mGy and ≥30 zones) | 26 | 3 | 0.91 (0.36–2.3) | 23 | 1 | 0.55 (0.07–4.2) | 26 | 4 | 0.84 (0.36–2.0) |
| High–low (≥0.1 mGy and <30 zones) | 116 | 5 | 1.1 (0.41–2.9) | 111 | 12 | 1.7 (0.79–3.9) | 116 | 17 | 1.4 (0.79–2.5) |
| High–high (≥0.1 mGy and ≥30 zones) | 415 | 22 | 0.90 (0.51–1.6) | 393 | 40 | 1.6 (0.83–3.1) | 415 | 62 | 1.3 (0.84–1.9) |
| Absorbed dose and Standard Sleep Interval travel | Model 19 | Model 20 | Model 21 | ||||||
| No work flightsc | 75 | 15 | 2.6 (1.4–4.8) | 60 | 5 | 1.5 (0.51–4.4) | 75 | 20 | 2.2 (1.2–3.9) |
| Low–low(<0.1 mGy and <15 hours)d | 164 | 28 | 1.0 | 136 | 9 | 1.0 | 164 | 37 | 1.0 |
| Low–high (<0.1 mGy and ≥15 hours) | 27 | 8 | 1.8 (0.86–3.9) | 19 | 3 | 2.5 (0.65–9.4) | 27 | 11 | 2.0 (1.0–3.9) |
| High–low (≥0.1 mGy and <15 hours) | 178 | 11 | 1.1 (0.55–2.4) | 167 | 15 | 1.6 (0.71–3.5) | 178 | 26 | 1.3 (0.78–2.2) |
| High–high (≥0.1 mGy and ≥15 hours) | 353 | 16 | 1.0 (0.52–1.9) | 337 | 37 | 2.3 (1.2–4.7) | 353 | 53 | 1.6 (1.1–2.5) |
| Time zones crossed and Standard Sleep Interval travel | Model 22 | Model 23 | Model 24 | ||||||
| No work flightsc | 75 | 15 | 2.6 (1.4–4.8) | 60 | 5 | 1.0 (0.38–2.8) | 75 | 20 | 1.9 (1.1–3.4) |
| Low–low (<30 zones and <15 hours)d | 221 | 30 | 1.0 | 191 | 17 | 1.0 | 221 | 47 | 1.0 |
| Low–high (<30 zones and ≥15 hours) | 60 | 8 | 2.0 (0.97–4.3) | 52 | 6 | 1.6 (0.61–4.1) | 60 | 14 | 1.8 (1.0–3.4) |
| High–low (≥30 zones and <15 hours) | 121 | 9 | 1.1 (0.55–2.3) | 112 | 7 | 0.68 (0.28–1.7) | 121 | 16 | 0.91 (0.52–1.6) |
| High–high (≥30 zones and ≥15 hours) | 320 | 16 | 0.96 (0.51–1.8) | 304 | 34 | 1.6 (0.88–2.9) | 320 | 50 | 1.4 (0.91–2.2) |
NR indicates not reported as the likelihood ratio test of proportional odds was statistically significant (P = 0.037).
Models of pregnancies in weeks 4–13 included 797 flight attendant study pregnancies (11 miscarriages in gestational weeks 1–3 and 32 pregnancies with 1 or more missing covariates were excluded).
All models additionally adjusted for age at the last menstrual period and parity.
Some employed flight attendants did not incur work flights during the first trimester.
Reference category.
High physical job demands defined as (1) being on your feet (including standing and walking) more than 8 hours/day or (2) 2 or more of the following: lifting or carrying objects that weigh at least 15 pounds more than 10 times a day, bending at the waist more than 25 times/day, and pushing or pulling heavy objects requiring at least 15 pounds of force or effort 20 or more times/day.
Cumulative occupational exposure metrics were evaluated from the estimated date of last menstrual period through the cutoff week; cutpoints reflect the median exposure among cases.
High physical job demands were a risk factor for miscarriage (OR = 2.5 [95% CI = 1.5–4.2]). We performed additional modeling adjusted for age and parity with the components of the composite metric: standing/walking, bending at the waist, lifting, and pushing/pulling, as defined in eTable 2 (http://links.lww.com/EDE/A862). Among these job-demand components, standing and walking for more than 8 hours/day (1.8 [1.2–2.8]) and bending at the waist more than 25 times/day (2.0 [1.1–3.5]) were risk factors for miscarriage.
In Table 4, we combine occupational exposures absorbed dose, Standard Sleep Interval travel, and physical demands together in the same set of models, adjusted for age and parity. Associations of individual exposures and other covariates with miscarriage were generally consistent with those in Table 3. The 5 high- and low-exposure categories were modeled with 4 degrees of freedom, which is equivalent to inclusion of a product term in these models. Inclusion or exclusion of a product term for radiation and Standard Sleep Interval travel did not meaningfully change the analysis results. Exposure to smoking by coworkers or passengers during the pregnancy was a risk factor for miscarriage in single-exposure analyses (OR = 1.8 [95% CI = 1.2–2.6]). When added to Table 4 combined occupational exposure models, there was reduced evidence of its association with miscarriage (eg, OR = 1.4 [95% CI = 0.78–2.4] in weeks 9–13; data not shown). Additional sensitivity analyses (results not shown) did not meaningfully change the analysis results.
TABLE 4.
Association of Age, Parity, Physical Job Demands, Absorbed Dose, and Standard Sleep Interval Time (Analyzed Simultaneously) with Early Miscarriage (Gestational Weeks 4–13) According to Time Perioda
| Weeks 4–8 |
Weeks 9–13 |
Weeks 4–13 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variableb | No. Pregnancies | No. Miscarriages | OR (95% CI) | No. Pregnancies | No. Miscarriages | OR (95% CI) | No. Pregnancies | No. Miscarriages | OR (95% CI) |
| Model 1 | Model 2 | Model 3 | |||||||
| Age at last menstrual period (1 year) | 797 | 78 | 1.1 (1.1–1.2) | 719 | 69 | 1.0 (0.96–1.1) | 797 | 147 | 1.1 (1.0–1.1) |
| Parity | |||||||||
| Nulliparousc | 478 | 45 | 1.0 | 433 | 47 | 1.0 | 478 | 92 | 1.0 |
| Parous | 319 | 33 | 0.91 (0.56–1.5) | 286 | 22 | 0.70 (0.43–1.2) | 319 | 55 | 0.81 (0.57–1.2) |
| Physical job demands in pregnancyd | |||||||||
| Lowc | 157 | 8 | 1.0 | 149 | 6 | 1.0 | 157 | 14 | 1.0 |
| High | 640 | 70 | 2.2 (1.1–4.5) | 570 | 63 | 2.8 (1.2–6.4) | 640 | 133 | 2.5 (1.5–4.1) |
| Absorbed dose and Standard Sleep Interval travele | |||||||||
| No work flightsf | 75 | 15 | 2.6 (1.4–4.9) | 60 | 5 | 1.6 (0.54–4.6) | 75 | 20 | 2.3 (1.3–4.0) |
| Low–low (<0.1 mGy and <15 hours)c | 164 | 28 | 1.0 | 136 | 9 | 1.0 | 164 | 37 | 1.0 |
| Low–high (<0.1 mGy and ≥15 hours) | 27 | 8 | 1.8 (0.86–3.9) | 19 | 3 | 2.4 (0.64–9.3) | 27 | 11 | 2.0 (1.0–3.9) |
| High–low (≥0.1 mGy and <15 hours) | 178 | 11 | 1.2 (0.55–2.4) | 167 | 15 | 1.5 (0.69–3.4) | 178 | 26 | 1.3 (0.76–2.1) |
| High–high (≥0.1 mGy and ≥15 hours) | 353 | 16 | 0.97 (0.50–1.9) | 337 | 37 | 2.3 (1.1–4.6) | 353 | 53 | 1.6 (1.0–2.5) |
Models of pregnancies in weeks 4–13 included 797 flight attendant study pregnancies (11 miscarriages in gestational weeks 1–3 and 32 pregnancies with 1 or more missing covariates were excluded).
All variables were included in each model; however, estimates for age and parity are not necessarily interpretable as total effects.24
Reference category.
High physical job demands defined as (1) being on your feet (including standing and walking) more than 8 hours/day or (2) 2 or more of the following: lifting or carrying objects that weigh at least 15 pounds more than 10 times a day, bending at the waist more than 25 times/day, and pushing or pulling heavy objects requiring at least 15 pounds of force or effort 20 or more times/day.
Cumulative occupational exposure metrics were evaluated from the estimated date of last menstrual period through the cutoff week; cutpoints reflect the median exposure among cases.
Some employed flight attendants did not incur work flights during the first trimester.
DISCUSSION
In this study, we found associations between miscarriage in flight attendants and occupational exposure to circadian disruption and physical job demands. We also found evidence of an association between cosmic ionizing radiation during pregnancy and miscarriage among flight attendants, although the association was modest and may have been affected by multicollinearity with circadian disruption metrics. We initially evaluated other approaches to exposure metrics, including continuous and quartile cutpoint metrics for radiation and circadian disruption. Many of these earlier models exhibited strong signs of collinearity and diminished evidence of association between the metrics and miscarriage. The analyses we present with “high–low” exposure metrics, especially Standard Sleep Interval travel, were the least influenced by multicollinearity between radiation and circadian disruption metrics and best able to describe the effects of separate metrics.
Evidence from atomic bomb survivor studies suggested a 50 mGy threshold for adverse reproductive outcomes in humans25; however, lower x-ray exposures have been associated with miscarriage in nurses (1 or more hours a day self-reported exposure)26 and veterinarians (more than 5 self-reported films/week).27 Flight attendants’ prepregnancy exposure rates were also low compared with the 50 mGy threshold, but generally higher than during their first trimester; half had estimated annual doses between 0.7 and 2.0 mGy (effective dose = 1.8–5.8 mSv) prior to pregnancy. These studies suggest that the most highly exposed flight attendants, nurses, and veterinarians may be at increased risk for reproductive and other health effects.
The International Commission on Radiological Protection28,29 recommends effective dose limits of 20 mSv/year averaged over 5 years (100 mSv in 5 years) for radiation workers and 1 mSv/year for the public. The International Commission on Radiological Protection considers flight crew occupationally exposed to cosmic radiation. European Union Member States require airlines to educate workers about their radiation risks, assess exposure when dose is likely to exceed 1 mSv/year, and adjust work schedules so that no individual worker exceeds 6 mSv/year.30 There are no official dose limits for US flight crew, although the National Council on Radiation Protection and Measurements reported that flight crew incur the largest average annual effective dose of all US radiation-exposed workers (3.07 mSv, 2006).23 By comparison, the average annual dose for US Department of Energy workers was 0.59 mSv in 2006.23 In our study, the highest solar particle event doses came from single flight segments (rather than from several flight segments flown during a solar particle event). If a pregnant flight attendant flew one of these segments during a solar particle event, she could easily approach or surpass the International Commission on Radiological Protection 1-mSv prenatal guideline18 or the National Council on Radiation Protection and Measurements 0.5-mSv recommended monthly limit during pregnancy.31 Resources are being developed to provide real-time and predictive information on solar particle events to flight crew and the public.32–34
We found an increased risk of miscarriage in flight attendants who flew 15+ hours during their home-base sleep hours. This is a new finding; however, it is consistent with reports of adverse reproductive outcomes associated with night or rotating shift work.35,36 Time zones crossed and radiation metrics were highly correlated, but we attempted to separate the etiologic contributions of circadian disruption and radiation by including our other circadian metric, Standard Sleep Interval travel, in a 2-exposure model with simplified exposure levels. Both time zones crossed and Standard Sleep Interval travel are related to a circadian biomarker, the day-to-day variance in overnight melatonin excretion.9 Standard Sleep Interval travel may be the better circadian metric for flight crew studies, but it considers only flight time and not commuter or other personal time, and it, therefore, probably underestimates disrupted sleep.
Future research of this occupational group should consider employed nonflying flight attendants as a separate exposure group. Records-based identification of these workers was critical to our analysis, because their risk of miscarriage was found to be considerably higher than for flight attendants with low exposures. These participants maintained flight attendant employed status without flying by trading flights with other flight attendants, using state- or company-based benefits, performing another airline job while keeping flight attendant credentials, or having a doctor's order not to fly. They were more likely than those who did fly to have had 2 or more previous pregnancies, and the data suggested that they were more likely to have 2 or more previous miscarriages (10% vs. 5%). Thus, they may have avoided flying during pregnancy due to their previous miscarriages, which may also have been caused by earlier occupational exposures.
High physical job demands—specifically, prolonged standing/walking or bending at the waist—were also associated with increased miscarriage, congruent with prior studies.37 The negative findings for occupational lifting contrast with results from a large Danish cohort, possibly due to our use of a relatively low-exposure threshold and dichotomous classification.38
Although occupational environmental tobacco smoke exposure was a risk factor in single-exposure analyses (OR = 1.8 [95% CI = 1.2–2.6]), we did not adjust for it when evaluating the association of miscarriage with radiation and circadian rhythm disruption (Table 4). Environmental tobacco smoke was a likely proxy exposure for Standard Sleep Interval travel prior to the airlines’ comprehensive smoking ban on long international overnight routes. Further, active smoking during the pregnancy was rare (4%) and did not meet criteria for confounding in our study because the rates of miscarriage among active smokers (26%) were comparable to those among nonsmokers (21%) (likelihood ratio P = 0.55). Environmental tobacco smoke exposure has generally been associated with later adverse reproductive outcomes rather than with miscarriage.39
This study's limitations include potential differential recall bias from self-report of outcome and gestational age information, although this information was verified/validated where possible; estimation rather than direct measurement of exposures; and possible multicollinearity of radiation and circadian disruption metrics. Occupational exposures estimated from the questionnaire were not trimester specific; physical job demands and other exposures may change throughout pregnancy. Finally, there is no ideal comparison group for flight attendants. Based on the differences we identified and other potential differences between these 2 occupational groups, our finding of no difference in flight attendants’ risk of miscarriage compared with teachers would benefit from further examination.
The strengths of this study include the first assessment of flight attendant radiation and circadian disruption exposures from individual flight segments that allowed us to contrast correlated exposures in analyses and the first direct estimation of solar particle event doses in flight attendants. Pregnant flight attendants share circadian disruption and ergonomic concerns with pregnant workers on the ground who may also be on their feet, bend from the waist, or work the night shift. Ergonomic guidelines being developed for pregnant workers40 should be adapted for pregnant flight crew, and guidelines need to be developed for pregnant shift workers on the ground and in the air. Unlike pregnant women on the ground, however, pregnant flight crew are occupationally exposed to cosmic radiation. Communication of the potential risk from exposure to cosmic radiation would allow them to make informed decisions about flying during pregnancy.
Supplementary Material
ACKNOWLEDGMENTS
We thank the women who participated in this study. We appreciate the assistance of the study airlines and the school districts; Airlines for America; the late Jerry Hordinsky of the Federal Aviation Administration (FAA); the Association of Flight Attendants, its Seattle Local 19, and Judith Anderson of the Air Safety, Health and Security Department for consultation; the Association of Professional Flight Attendants and its Miami representatives; the International Brotherhood of Teamsters, Airline Division, and its Detroit representatives; and the American Federation of Teachers and National Education Association and their local affiliates (Seattle Education Association, Grand Rapids Education Association, United Teachers of Dade, and Pinellas Classroom Teachers Association). The late Wallace Friedberg and Kyle Copeland of the FAA provided CARI software and consultation. Pamela Stratton (Eunice Kennedy Shriver National Institute of Child Health and Human Development) consulted with us on gynecologic treatment and diagnoses. Donna Baird and Clarice Weinberg improved our article with their thoughtful reviews. We thank National Institute for Occupational Safety and Health (NIOSH) contributors James Deddens for assistance with the CARI input algorithm; Patricia Laber for data management; and the NIOSH statistical assistants and programmers who brought order to approximately 2 million medical and work history records: Faith Armstrong, William Ehling, Kim Jenkins, Denise Giglio, Christine Gersic, and Zachary Zivkovich.
Footnotes
The authors report no conflicts of interest. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention (CDC). Mention of any company or product does not constitute endorsement by the CDC.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com). This content is not peer-reviewed or copy-edited; it is the sole responsibility of the authors.
REFERENCES
- 1.Air Transport Association . When America Flies, It Works: 2010 Economic Report. Air Transport Association; Washington, DC: 2010. [Google Scholar]
- 2.Association of Flight Attendants . Member Survey. AFA; Washington, DC: 1995. [Google Scholar]
- 3.International Agency for Research on Cancer . IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. 100D. International Agency for Research on Cancer (IARC), World Health Organization (WHO); Lyon, France: 2012. A Review of Human Carcinogens. [Google Scholar]
- 4.Shmidova VF. [The effect of high-altitude and high-speed flights on the function of the reproductive organs of stewardesses]. Gig Tr Prof Zabol. 1966;10:55–57. [PubMed] [Google Scholar]
- 5.Daniell WE, Vaughan TL, Millies BA. Pregnancy outcomes among female flight attendants. Aviat Space Environ Med. 1990;61:840–844. [PubMed] [Google Scholar]
- 6.Aspholm R, Lindbohm ML, Paakkulainen H, Taskinen H, Nurminen T, Tiitinen A. Spontaneous abortions among Finnish flight attendants. J Occup Environ Med. 1999;41:486–491. doi: 10.1097/00043764-199906000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Lauria L, Ballard TJ, Caldora M, Mazzanti C, Verdecchia A. Reproductive disorders and pregnancy outcomes among female flight attendants. Aviat Space Environ Med. 2006;77:533–539. [PubMed] [Google Scholar]
- 8.Waters M, Bloom TF, Grajewski B. The NIOSH/FAA Working Women's Health Study: evaluation of the cosmic-radiation exposures of flight attendants. Health Phys. 2000;79:553–559. doi: 10.1097/00004032-200011000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Grajewski B, Nguyen MM, Whelan EA, Cole RJ, Hein MJ. Measuring and identifying large-study metrics for circadian rhythm disruption in female flight attendants. Scand J Work Environ Health. 2003;29:337–346. doi: 10.5271/sjweh.740. [DOI] [PubMed] [Google Scholar]
- 10.Goldhagen P. Overview of aircraft radiation exposure and recent ER-2 measurements. Health Phys. 2000;79:526–544. doi: 10.1097/00004032-200011000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Baker FC, Driver HS. Circadian rhythms, sleep, and the menstrual cycle. Sleep Med. 2007;8:613–622. doi: 10.1016/j.sleep.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 12.Hammer GP, Blettner M, Zeeb H. Epidemiological studies of cancer in aircrew. Radiat Prot Dosimetry. 2009;136:232–239. doi: 10.1093/rpd/ncp125. [DOI] [PubMed] [Google Scholar]
- 13.Grajewski B, Waters MA, Whelan EA, Bloom TF. Radiation dose estimation for epidemiologic studies of flight attendants. Am J Ind Med. 2002;41:27–37. doi: 10.1002/ajim.10018. [DOI] [PubMed] [Google Scholar]
- 14.Whelan EA, Grajewski B, Wood E, et al. Feasibility issues in reproductive biomonitoring of female flight attendants and teachers. J Occup Environ Med. 2002;44:947–955. doi: 10.1097/00043764-200210000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Grajewski B, Waters MA, Yong LC, Tseng CY, Zivkovich Z, Cassinelli RT., 2nd. Airline pilot cosmic radiation and circadian disruption exposure assessment from logbooks and company records. Ann Occup Hyg. 2011;55:465–475. doi: 10.1093/annhyg/mer024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Friedberg W, Copeland K. What Aircrews Should Know About Their Occupational Exposure to Ionizing Radiation. Federal Aviation Administration, Civil Aerospace Medical Institute; Oklahoma City: 2003. [Google Scholar]
- 17.Anderson JL, Mertens CJ, Grajewski B, Luo L, Tseng CY, Cassinelli RT., 2nd. Flight attendant radiation dose from solar particle events. Aviat Space Environ Med. 2014;85:828–832. doi: 10.3357/ASEM.3989.2014. [DOI] [PubMed] [Google Scholar]
- 18.Mertens CJ, Kress BT, Wiltberger M, Tobiska WK, Grajewski B, Xu X. Atmospheric ionizing radiation from galactic and solar cosmic rays. In: Nenoi M, editor. Current Topics in Ionizing Radiation Research. InTech; Rijeka, Croatia: 2012. pp. 683–738. [Google Scholar]
- 19.Mertens CJ, Meier MM, Brown S, Norman RB, Xu X. NAIRAS aircraft radiation model development, dose climatology, and initial validation. Space Weather. 2013;11:1–33. doi: 10.1002/swe.20100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ammon Avalos L, Galindo C, Li DK. A systematic review to calculate background miscarriage rates using life table analysis. Birth Defects Res A Clin Mol Teratol. 2012;94:417–423. doi: 10.1002/bdra.23014. [DOI] [PubMed] [Google Scholar]
- 21.Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. John Wiley and Sons; New York: 1980. [Google Scholar]
- 22.Lin DY, Wei LJ. The robust inference for the proportional hazards model. J Am Stat Assoc. 1989;84:1074–1078. [Google Scholar]
- 23.National Council on Radiation Protection and Measurements . Ionizing Radiation Exposure of the Population of the United States. Report No. 160. Recommendations of the National Council on Radiation Protection and Measurements (NCRP) National Council on Radiation Protection and Measurements; Bethesda, MD: 2009. [Google Scholar]
- 24.Westreich D, Greenland S. The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. Am J Epidemiol. 2013;177:292–298. doi: 10.1093/aje/kws412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Santis M, Cesari E, Nobili E, Straface G, Cavaliere AF, Caruso A. Radiation effects on development. Birth Defects Res C Embryo Today. 2007;81:177–182. doi: 10.1002/bdrc.20099. [DOI] [PubMed] [Google Scholar]
- 26.Lawson CC, Rocheleau CM, Whelan EA, et al. Occupational exposures among nurses and risk of spontaneous abortion. Am J Obstet Gynecol. 2012;206:327.e1–327.e8. doi: 10.1016/j.ajog.2011.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shirangi A, Fritschi L, Holman CDJ. Maternal occupational exposures and risk of spontaneous abortion in veterinary practice. Occup Environ Med. 2008;65:719–725. doi: 10.1136/oem.2007.035246. [DOI] [PubMed] [Google Scholar]
- 28.International Commission on Radiological Protection (ICRP) 1990 Recommendations of the International Commission on Radiological Protection. Pergamon; New York: 1991. [Google Scholar]
- 29.International Commission on Radiological Protection ICRP Publication 103: recommendations of the International Commission on Radiological Protection. Radiat Prot Dosimetry. 2008;129:500–507. [Google Scholar]
- 30.EURADOS . Exposure of Air Crew to Cosmic Radiation. A Report of EURADOS Working Group 11, EURADOS Report 1996.01. Office for Official Publications of the European Communities; Luxembourg: 1996. European Commission Report Radiation Protection 85. [Google Scholar]
- 31.Copeland K, Sauer HH, Duke FE, Friedberg W. Cosmic radiation exposure of aircraft occupants on simulated high-latitude flights during solar proton events from 1 January 1986 through 1 January 2008. Adv Space Res. 2008;42:1008–1029. [Google Scholar]
- 32.National Aeronautics and Space Administration (NASA) [15 January 2014];NAIRAS (Nowcast of Atmospheric Ionizing Radiation System) Available at: http://sol.spacenvironment.net/~nairas/index.html.
- 33.National Oceanic and Atmospheric Administration (NOAA) SWPC [15 January 2014];Today's Space Weather. Available at: http://www.swpc.noaa.gov/today.html.
- 34.Technologies SE. [15 January 2014];Space Weather on the iPhone/iPod/iPad (Space Wx App) Available at: http://www.spacewx.com/iPhone.html.
- 35.Lawson CC, Whelan EA, Lividoti Hibert EN, Spiegelman D, Schernhammer ES, Rich-Edwards JW. Rotating shift work and menstrual cycle characteristics. Epidemiology. 2011;22:305–312. doi: 10.1097/EDE.0b013e3182130016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Whelan EA, Lawson CC, Grajewski B, Hibert EN, Spiegelman D, Rich-Edwards JW. Work schedule during pregnancy and spontaneous abortion. Epidemiology. 2007;18:350–355. doi: 10.1097/01.ede.0000259988.77314.a4. [DOI] [PubMed] [Google Scholar]
- 37.Florack EI, Zielhuis GA, Pellegrino JE, Rolland R. Occupational physical activity and the occurrence of spontaneous abortion. Int J Epidemiol. 1993;22:878–884. doi: 10.1093/ije/22.5.878. [DOI] [PubMed] [Google Scholar]
- 38.Juhl M, Strandberg-Larsen K, Larsen PS, et al. Occupational lifting during pregnancy and risk of fetal death in a large national cohort study. Scand J Work Environ Health. 2013;39:335–342. doi: 10.5271/sjweh.3335. [DOI] [PubMed] [Google Scholar]
- 39.Leonardi-Bee J, Britton J, Venn A. Secondhand smoke and adverse fetal outcomes in nonsmoking pregnant women: a meta-analysis. Pediatrics. 2011;127:734–741. doi: 10.1542/peds.2010-3041. [DOI] [PubMed] [Google Scholar]
- 40.MacDonald LA, Waters TR, Napolitano PG, et al. Clinical guidelines for occupational lifting in pregnancy: evidence summary and provisional recommendations. Am J Obstet Gynecol. 2013;209:80–88. doi: 10.1016/j.ajog.2013.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


