Abstract
Fever is a common response to inflammation and infection. The mechanism involves prostaglandin E2 (PGE2)-EP3 receptor signaling in the hypothalamus, which raises the set point of hypothalamic thermostat for body temperature, but the lipid metabolic pathway for pyretic PGE2 production remains unknown. To reveal the molecular basis of fever initiation, we examined lipopolysaccharides (LPS)-induced fever model in monoacylglycerol lipase (MGL)-deficient (Mgll −/−) mice, CB1 receptor-MGL compound-deficient (Cnr1 −/− Mgll −/−) mice, cytosolic phospholipase A2α (cPLA2α)-deficient (Pla2g4a −/−) mice, and diacylglycerol lipase α (DGLα)-deficient (Dagla −/−) mice. Febrile reactions were abolished in Mgll −/− and Cnr1 −/− Mgll −/− mice, whereas Cnr1 −/− Mgll +/+, Pla2g4a −/− and Dagla −/− mice responded normally, demonstrating that MGL is a critical enzyme for fever, which functions independently of endocannabinoid signals. Intracerebroventricular administration of PGE2 caused fever similarly in Mgll −/− and wild-type control mice, suggesting a lack of pyretic PGE2 production in Mgll −/− hypothalamus, which was confirmed by lipidomics analysis. Normal blood cytokine responses after LPS administration suggested that MGL-deficiency does not affect pyretic cytokine productions. Diurnal body temperature profiles were normal in Mgll −/− mice, demonstrating that MGL is unrelated to physiological thermoregulation. In conclusion, MGL-dependent hydrolysis of endocannabinoid 2-arachidonoylglycerol is necessary for pyretic PGE2 production in the hypothalamus.
Introduction
Fever is one of the typical responses to inflammation and infection. It is thought to be an adaptive defense mechanism, as higher body temperature prevents propagation of infectious microorganisms and activates the host's immune system [1]. In homeotherms including mammals, body temperature is regulated by the control of heat production and heat loss to adjust it to a ‘set point’, typically set at around 37°C in mammals [2]. Fever is explained as a ‘resetting’ of the set point to a higher value, which raises the body temperature thresholds for heat production and heat loss mechanisms, causing increased muscle tone, shivering and peripheral vasoconstrictions until the body temperature reaches the new set point [2].
Upon infection of viruses or bacteria, host’s immune cells produce pyretic cytokines including TNFα, IL-1β, and IL-6 [3]. These cytokines via circulation stimulate a production of prostaglandin E2 (PGE2), an arachidonic acid (AA)-derived lipid mediator, in the hypothalamus. PGE2 is considered to be a critical mediator of fever, as genetic ablations of genes for enzymes involved in biosynthesis of PGE2, such as cyclooxygenase-2 (COX-2, encoded by Ptgs2) and microsomal prostaglandin E synthase-1 (mPGES-1, encoded by Ptges), abolish febrile reactions in mice [4, 5]. Among 4 known PGE2 receptor subtypes [6], EP3 receptors (EP3R, encoded by Ptger3) mediate fever, as global Ptger3-knockout [7] and conditional Ptger3-knockout in the medial preoptic nucleus of the hypothalamus [8] prevent fever responses in mice.
A number of previous studies have demonstrated that AA, a precursor for PGE2, is liberated from AA-containing phospholipids by the action of phospholipases A2 (PLA2s) [9]. Among PLA2s, cytosolic PLA2α (cPLA2α, group IVA PLA2) encoded by Pla2g4a gene, has been known as a crucial enzyme for eicosanoid production in inflammatory cells [9]. Although it has been suggested that cPLA2α is involved in PGE2 production during fever [10], this has not been clearly demonstrated. An alternative AA-producing pathway from 2-arachidonoylglycerol (2-AG), an endocannabinoid that functions in the central nervous system through activation of CB1 cannabinoid receptors (CB1R, encoded by Cnr1 gene), was first documented in platelets [11, 12]. A recent study demonstrated that deletion of Mgll, a gene that encodes monoacylglycerol lipase (MGL) which hydrolyzes 2-AG to AA and glycerol, results in accumulation of 2-AG and consequent reductions of AA and eicosanoid levels in the mouse brain [13], suggesting an importance of this pathway.
Here, we address the biosynthetic pathway for pyretic PGE2 in the hypothalamus. Using null mutant mice, we found that lipopolysaccharides (LPS)-induced fever depends on MGL but not on cPLA2α. Mgll −/− mice showed normal cytokine responses after LPS administration, but had reduced hypothalamic PGE2 levels. When injected intracerebroventricularly (ICV), PGE2 caused fever in Mgll −/− mice. These data demonstrate that MGL-dependent hypothalamic PGE2 is required for a febrile response. We also show that diurnal core body temperature changes are normal in MGL-KO mice, demonstrating that MGL is not critical in physiological thermoregulations.
Materials and Methods
Reagents
Lipopolysaccharides (LPS, from Escherichia Coli, serotype 0111:B4) were purchased from Sigma-Aldrich (St. Louis, MO). Organic solvents for liquid chromatography and lipid extraction (methanol, acetonitrile, chloroform) and modifiers (formic acid and ammonium bicarbonate) were purchased from Wako (Osaka, Japan). Phospholipids and eicosanoids were purchased from Avanti Polar Lipids (Alabaster, AL) and Cayman Chemical (Ann Arbor, MI), respectively. Fatty acids and fatty acid methyl esters were purchased from Wako and Sigma-Aldrich, respectively.
Animals
MGL-deficient (Mgll −/−) mice [14], DGLα-deficient (Dagla −/−) mice [15], CB1R-MGL compound-deficient (Cnr1 −/− Mgll −/−) mice, cytosolic phospholipase A2α-deficient (Pla2g4a −/−) mice [16], and their control mice as specified in each experiment, were prepared by mating respective heterozygous mice. Female mice were used for all the studies. All mouse strains had a C57BL/6 genetic background and were maintained in a specific-pathogen-free facility (ambient temperature 23°C, light-dark cycle with lights on from 0700 to 2000 h), and fed ad libitum with a standard laboratory diet (MF; Oriental Yeast, Tokyo, Japan) and water.
LPS-induced fever model
Adult female mice (8–10 wk-old) were isolated and habituated to an ambient temperature of 30°C before the experiment. LPS (20 μg dissolved in 100 μL saline) or saline was injected intraperitoneally, and core body temperatures were monitored every 30 min using a RET-3 rectal probe (AD instruments, Dunedin, New Zealand) and a MR2041 thermo-logger (Chino, Tokyo, Japan). Mice were habituated to the insertion of rectal probe 3–4 h before LPS injection. We observed relatively unstable body temperature readings at 30 min, 60 min, and 90 min timepoints, which can be attributed to injection and/or restraint stress, and therefore, we did not evaluate these datapoints. Fever typically manifested ~2h after LPS injection.
ICV administration of PGE2
For intracerebroventricular injection, mice were anesthetized with isoflurane using a Univentor 400 anesthesia unit (Univentor, Zejtun, Malta). Using a Hamilton Gastight micro syringe (Reno, NV) with a 27-gauge needle (Terumo, Tokyo, Japan), PGE2 (4 nmol in 2 μL of saline) or equal volume of saline was injected to the left lateral ventricle (coordinates: 1 mm lateral and 0.5 mm caudal to bregma, depth 2.5 mm). After injection, mice were recovered from anesthesia and core body temperatures were monitored every 15 min using a rectal probe. Ambient temperature was set at 25°C.
Measurement of diurnal core body temperature changes
A miniature temperature data logger device was prepared according to the method reported previously [17], with modifications. In brief, the circuit board of DS1921H-F5# iButton device (Maxim Integrated Products, San-Jose, CA) was removed, reassembled with a new lithium coin battery (CR1216, Panasonic, Osaka, Japan), programmed to record the temperature every 5 min, and then potted with paraffin (m.p. 68–70°C, Wako) to make it water-proof. Mice were intra-abdominally implanted with the thermo-loggers and maintained under a light-dark cycle with lights on from 0800 to 2000 h. Ambient temperature was set at 25°C. Ten days after surgery, the loggers were removed from mice and incubated at 37°C for 30 min for post-calibration purpose. The data were retrieved using OneWireViewer software (Maxim). Data points for 3 consecutive light-dark cycles (day 8–day 10 after surgery) were used to determine the diurnal core body temperature changes for each mouse.
Lipid analysis
Hypothalamus block and liver samples were collected from mice 2 h after intraperitoneal injection of LPS or saline. Lipids were extracted from tissues stored frozen under liquid nitrogen, by methanol (for eicosanoids), acetonitrile (for 2-AG and AEA), or chloroform-methanol (1:1, for total fatty acids). Eicosanoids, 2-AG, and AEA were measured using liquid chromatography mass spectrometry (LC-MS) as previously described [15, 18]. Total fatty acids were analyzed by a gas chromatograph with a flame ionization detector (GC-2010 Plus, Shimadzu, Kyoto, Japan) using a Supelco SP-2560 column (100 m × 0.25 mm I.D., 0.20 μm, Sigma-Aldrich). Total lipid samples were spiked with C21:0 fatty acid internal standard, and derivatized to fatty acid methyl esters (FAMEs) using a FAME derivatization and purification kit (Nacalai Tesque, Kyoto, Japan). The samples were quantified using peak areas of known amounts of FAMEs and C21:0 FAME. Phospholipid profiling analysis was conducted with a Nexera liquid chromatograph connected to an LCMS-8040 triple quadrupole mass spectrometer with electrospray-ionization source (Shimadzu).
Serum cytokines
Serum samples were collected from mice 2 h after intraperitoneal injection of LPS or saline. TNFα, IL-1β, and IL-6 were determined by enzyme-linked immunosorbent assay kits (Thermo Scientific, Waltham, MA).
Statistics
GraphPad Prism 5 (GraphPad Software, San Diego, CA) was used for statistical calculations. P-values < 0.05 were considered statistically significant.
Ethics statement
All procedures in the present study were conducted in accordance with the Guidelines for Animal Care of The University of Tokyo, approved by the animal experimentation committee of Faculty of Medicine, The University of Tokyo (approval no. M-P12-124).
Results
MGL mediates LPS-induced febrile response
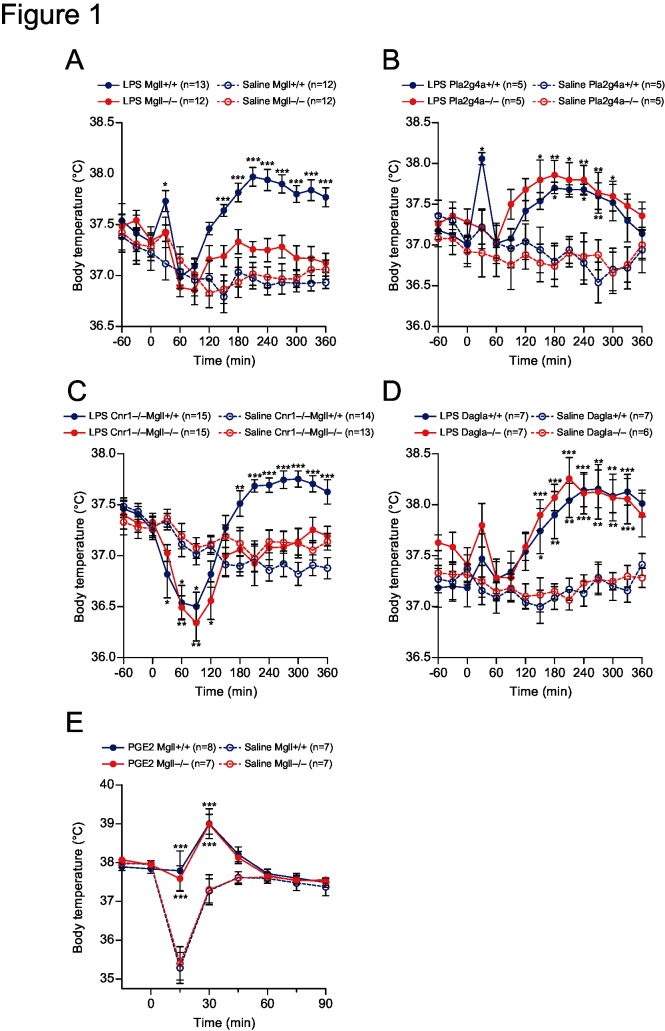
We first examined LPS-induced fever in mice lacking MGL or cPLA2α to identify which enzyme mediates PGE2 production during fever. Bacterial endotoxin LPS activates TLR4 receptors expressed on immune cells, causing various inflammatory responses including immediate release of proinflammatory cytokines [19]. Intraperitoneal administration of LPS (20 μg dissolved in 100 μL saline; from Escherichia Coli, serotype 0111:B4) caused a transient increase in core body temperature, which was typically observed in wild-type mice 2–6 h after LPS administration (Fig 1A and 1B ). The febrile responses were largely attenuated in Mgll −/− mice (Fig 1A ), while remaining unchanged in Pla2g4a −/− mice (Fig 1B ). Ablation of MGL is reported to increase 2-AG levels, which reportedly results in downregulation and desensitization of CB1R in the brain [20]. To examine if the attenuated febrile responses in Mgll −/− mice were due to altered CB1R signals, compound knockout mice for Cnr1 and Mgll genes (Cnr1 −/− Mgll −/−) were examined. LPS-induced fever was blocked in Cnr1 −/− Mgll −/− mice, while control Cnr1 −/− Mgll +/+ mice showed normal febrile responses (Fig 1C ). These results demonstrated that the impaired febrile responses in Mgll −/− mice are not due to altered CB1R signaling in these mice. We also examined the possible involvement of diacylglycerol lipase α (DGLα), a major 2-AG-producing enzyme in the brain [15]. LPS-induced febrile responses in diacylglycerol lipase α-deficient (Dagla −/−) mice were normal (Fig 1D ), suggesting that this enzyme is not involved in fever mechanism.
Fig 1. LPS- and PGE2-induced febrile responses.
(A-D) MGL-knockout (Mgll −/−) mice (A), cPLA2α-knockout (Pla2g4a −/−) mice (B), CB1R-MGL compound-knockout (Cnr1 −/− Mgll −/−) mice (C), DGL-knockout (Dagla −/−) mice (D), and their respective WT control mice were intraperitoneally injected with 20 μg of LPS or saline (n = 5–15 as indicated on the panels). Core body temperatures were monitored by insertion of a rectal probe every 30 min. Mice were kept at thermo-neutral conditions (30°C). (E) Mgll +/+ and Mgll −/− mice were intracerebroventricularly injected with 4 nmol of PGE2 or saline (n = 7–8 for each group). Core body temperatures were monitored by a rectal probe every 15 min. Mice were kept at 23°C. Data are expressed as means ± SEM. *p<0.05, ** p< 0.01, ***p<0.001 vs. saline-treated wild-type controls, by Bonferroni post-test after two-way repeated measures ANOVA.
ICV administration of PGE2 elicits fever in MGL-deficient mice
We next performed ICV administration of PGE2 (4 nmol in 2 μL of saline) to Mgll −/− and control WT mice. PGE2 caused transient fever that reached a peak around 30 min after its administration similarly in Mgll −/− and control WT mice (Fig 1E ). Vehicle injection (2 μL of saline) caused transient hypothermia in the early (~15 min) phase, which was not evident in PGE2-injected mice and was similarly observed in both genotypes (Fig 1E ). The result demonstrated that fever mechanisms downstream of PGE2 are intact in Mgll −/− mice.
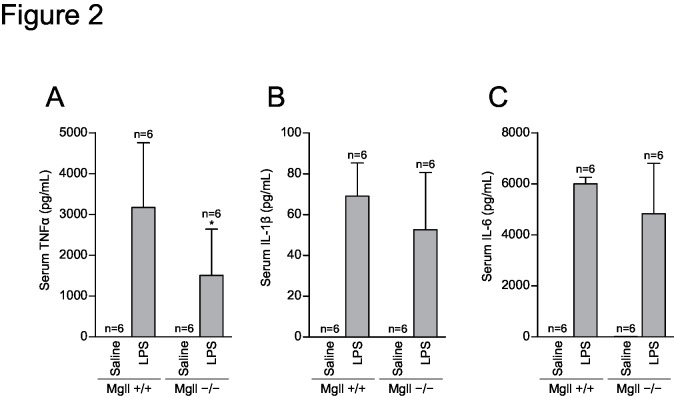
Systemic cytokine response to LPS administration is normal in MGL-deficient mice
A previous report demonstrated that MGL-deficient mice are protected from LPS-induced neuroinflammation by a decrease in inflammatory cytokines observed 6 h after LPS administration [13]. It is possible that the immediate cytokine responses are also lost in Mgll −/− mice. To test this, we examined cytokine responses in Mgll −/− mice. Blood levels of TNFα, IL-1β, and IL-6 were elevated 2 h after systemic LPS administration in both Mgll −/− and WT control mice (Fig 2). A modest attenuation of TNFα levels was noted in Mgll −/− mice (Fig 2A ) but was unlikely to explain the loss of febrile responses in these mice. Thus, the immediate cytokine responses (~2 h after LPS) that precede the febrile response remained intact in Mgll −/− mice.
Fig 2. Serum cytokines after LPS administration.
Mgll +/+ and Mgll −/− mice (n = 6 for each group) were intraperitoneally injected with 20 μg of LPS or saline, and serum were collected 2 h after injection. Serum levels of TNFα (A), IL-1β (B), and IL-6 (C) were determined by enzyme-linked immunosorbent assay. Data are expressed as mean ± SD. *p<0.05 vs. Mgll +/+, by Bonferroni post-test after two-way ANOVA.
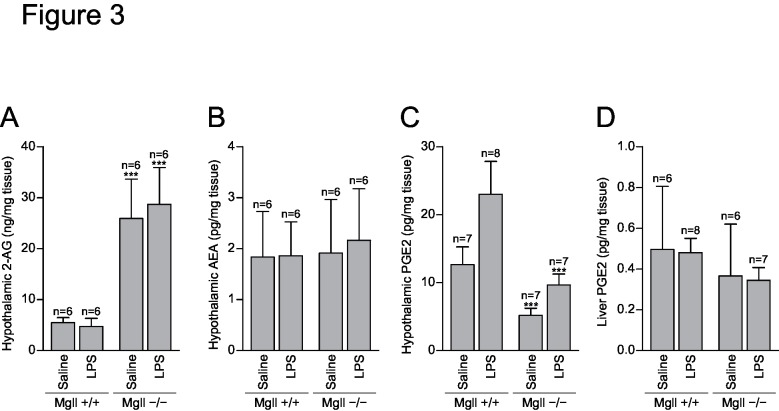
Hypothalamic PGE2 is decreased in MGL-deficient mice
Next, we performed lipidomics analysis to determine the changes in lipid mediators and related lipids in Mgll −/− mice. Total fatty acid analysis of hypothalamic tissue demonstrated no difference between the genotypes, suggesting that the tissue AA pool is not affected by MGL-deficiency (S1 Fig). Phospholipid profiling analysis reveals no significant difference between the genotypes, suggesting PLA2 substrates are unaltered in the Mgll −/− hypothalamus (S2 Fig). Levels of hypothalamic 2-AG levels were substantially increased by the deletion of MGL (Fig 3A ), while those of anandamide (arachidonoyl ethanolamide, AEA) were not altered (Fig 3B ). These results confirmed that MGL is the major 2-AG hydrolyzing enzyme in the hypothalamus. Both 2-AG and AEA levels were unaltered by LPS administration in both genotypes (Fig 3A and 3B ), which can be understood either by unchanged 2-AG and AEA production or by possible changes in their metabolic flux, which are undetectable in a snapshot analysis. Hypothalamic PGE2 and other several eicosanoids were decreased in Mgll −/− mice to levels no greater than those of saline-treated control WT mice even after LPS administration (Fig 3C and S3 Fig). Reports suggest that the liver is an important source of PGE2 during LPS-induced fever, as liver Kupffer cells can be activated by LPS [10, 21]. A previous report demonstrated an increase in liver PGE2 levels 6 h after LPS administration, which was abolished in MGL-deficient mice [13]. We measured the liver eicosanoids 2 h after LPS administration (Fig 3D and S4 Fig). LPS did not increase liver PGE2 by 2 h and there were no differences between genotypes, suggesting that MGL-dependent hypothalamic PGE2 production is important for febrile response.
Fig 3. Lipid mediator levels after LPS administration.
Mgll +/+ and Mgll −/− mice were intraperitoneally injected with 20 μg of LPS or saline (n = 6–8 for each group). Two hours later, hypothalamus and liver tissues were collected. Lipids were extracted and analyzed by liquid chromatography-tandem mass spectrometry. (A) Hypothalamic 2-AG levels. (B) Hypothalamic anandamide levels. (C) Hypothalamic PGE2 levels. (D) Liver PGE2 levels. Data are expressed as means ± SD. ***p<0.001 vs. Mgll +/+, by Bonferroni post-test after two-way ANOVA.
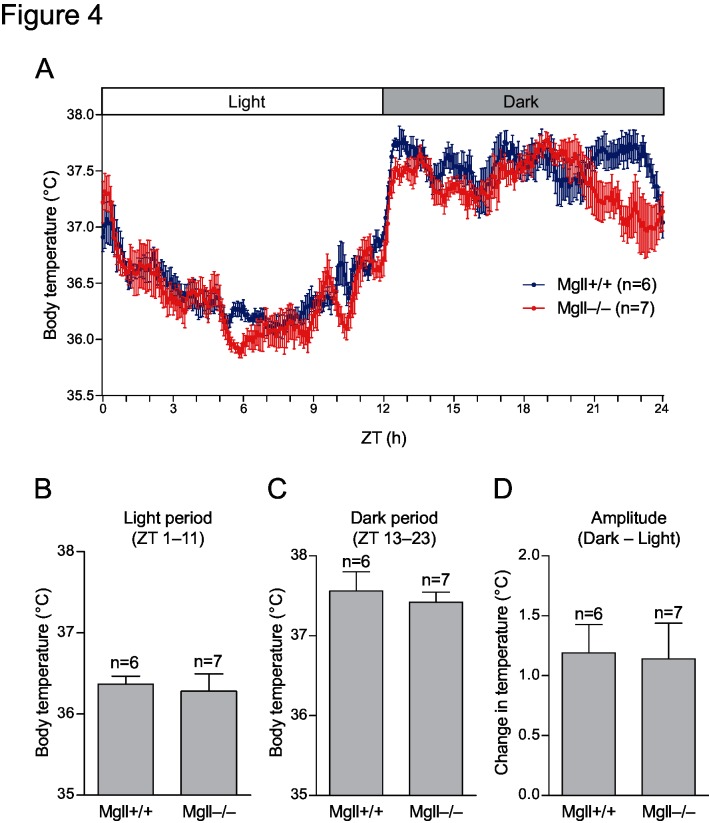
Diurnal core body temperature rhythmicity is normal in MGL-deficient mice
To examine if MGL is involved in physiological thermoregulatory mechanisms, diurnal core body temperature changes of Mgll −/− and control WT mice were recorded by intra-abdominal thermo-logger implants. No significant differences in the profile (Fig 4A ), average core body temperatures in the light and dark periods (Fig 4B and 4C ), and the amplitude of body temperature changes (Fig 4D ) were found between the genotypes, suggesting that MGL is not involved in the regulation of daily core body temperature rhythms.
Fig 4. Diurnal core body temperature changes.
(A) Mgll +/+ (n = 6) and Mgll −/− mice (n = 7) were intra-abdominally implanted with thermo-logger and placed in a thermostat chamber with a light-dark cycle (L:D = 12h:12h). Core body temperatures of 3 consecutive light-dark cycles were averaged for each mice. Data are expressed as means ± SEM, for indicated numbers of mice. No statistically significant differences were found between genotypes (Bonferroni post-test after two-way repeated measures ANOVA). (B-D) Averaged body temperature for light period (ZT 1–10) (B) and dark period (ZT 13–23) (C), and the difference in body temperatures between light and dark periods (D) were calculated using the data shown in (A). No statistically significant differences were found between genotypes (Student’s t-test).
Discussion
Management and medication of fever are clinically important. Non-steroidal anti-inflammatory drugs (NSAIDs) that target COXs, as well as acetaminophen, are widely used for fever treatment and are effective, but safer antipyretics are anticipated since adverse effects are known for these drugs [22]. To this end, detailed understanding of fever mechanism at biochemical levels is essential. In the present study, we demonstrated that MGL-dependent 2-AG degradation is the underlying mechanism for hypothalamic PGE2 production in LPS-induced fever. Despite the fact that cPLA2α has been regarded as a crucial enzyme for the AA cascade and its involvement has been demonstrated in many inflammatory disease models [9], febrile reaction mediated by hypothalamic PGE2-EP3R pathway was an apparent exception; it depends on MGL and does not require cPLA2α (Fig 1A and 1B ). Our result suggests that drug(s) that target cPLA2α, which is currently not available, would be ineffective against fever. Instead, endocannabinoid metabolism can be a potential target for fever treatment.
Genetic ablation as well as pharmacological inactivation of MGL result in an accumulation of 2-AG in vivo, as shown by previous studies [13, 20], and in the present study (Fig 3A ). It is, therefore, plausible that accumulated 2-AG activates CB1R in the brain to decrease core body temperature (one of the well-known effects of marijuana), which counteracts febrile responses triggered by PGE2-EP3R signaling. Although such a hypothesis seems unlikely, as a previous report demonstrated a downregulation of CB1R in MGL-deficient mice due to its persistent activation [20], it is critical to eliminate CB1R signaling to examine the role for MGL in pyretic PGE2 production. Our results using compound deficient mice for CB1R and MGL clearly demonstrated MGL-dependent- and CB1R-independent nature of febrile reactions (Fig 1C ). Moreover, results that ICV injection of PGE2 elicited fever in MGL-deficient mice (Fig 1E ), and that hypothalamic PGE2 levels after LPS injection were suppressed by MGL deficiency (Fig 3C ), further support our concept that MGL mediates pyretic PGE2 production in the hypothalamus.
The results for blood levels of TNFα, IL-1β and IL-6 2h after LPS administration demonstrated that pyretic cytokine productions are normal in MGL-deficient mice (Fig 2). A recent report describes that neuroinflammation after LPS administration is suppressed in MGL-deficient mice, with decreased cytokines as well as eicosanoid levels [13]. This discrepancy in cytokine response may be explained by the difference in time points chosen. In the early phase, LPS stimulates a transient increase in blood cytokine levels that reach a peak 1–2 h after LPS administration. This activates hypothalamic PGE2-EP3R pathway to cause febrile response. In the later phase, 6–8 h after LPS administration, PGE2 (or other MGL-dependent metabolites) on the contrary may enhance cytokine productions in the tissue and exacerbate inflammation. Similar difference was observed for tissue lipid mediators. Previous report describes that LPS-induced elevations in liver prostaglandin E2 determined at 6h after LPS administration were blocked by genetic or pharmacological inactivation of MGL [13]. In our experiment, when measured at 2h after injection, LPS did not alter liver PGE2 levels in both MGL-deficient and wild-type mice (Fig 3D ). Meanwhile, levels of TXB2, PGD2, LTD4 and PAF were increased (S4 Fig), demonstrating that LPS do stimulate some lipid mediators at this time point. From the results, we concluded that liver PGE2 is not the MGL-dependent factor that mediates febrile responses.
In our experiments using global knockout mice, the cell type(s) producing PGE2 in the hypothalamus were not elucidated, thus warranting further studies using conditional knockout mice [23]. A recent study demonstrated that LPS-induced fever depends on PGE2 production in the brain endothelial cells [24, 25]. Thus, it is likely that hypothalamic endothelial cells are the candidate cell type also for 2-AG degradation by MGL; however, it is possible that AA released from other cell types leads to endothelial PGE2 production by a transcellular mechanism. Observations that COX-2 and mPGES-1 are induced in the endothelial cells during LPS-induced fever [24, 25] indicate that these enzymes seem to be rate-limiting for pyretic PGE2 production. It remains elusive whether MGL is also rate-limiting; we did not observe changes in hypothalamic 2-AG levels by LPS (Fig 3A ), but this does not necessarily mean that MGL activity was unaltered, as concentrations do not reflect possible changes in metabolic flux.
It is of interest that the LPS-induced febrile response was normal in DGLα-deficient mice (Fig 1D ). We have shown that DGLα expressed in neuronal cells serves as the major 2-AG source in the brain [15] and others have demonstrated MGL as a major 2-AG-degrading enzyme [26], suggesting a functional coupling of DGLα and MGL that regulates 2-AG levels in the brain. However, our results suggest that 2-AG produced independently of DGLα is the precursor for hypothalamic PGE2 during fever. Other enzymes with DGL activity (e.g., DGLβ [15]) may be involved; this possibility requires further investigation.
From a physiological point of view, whether PGE2 serves as a factor that determines the primary body temperature set point and its diurnal rhythmicity, has been a question. A previous report demonstrates that RANKL-RANK pathway affect diurnal female body temperature changes via PGE2-EP3R pathway [27]. In our experiment, MGL-deficient female mice were normothermic, and were similar in both amplitude and rhythmicity of body temperature changes as compared with wild-type mice (Fig 4). The result points that MGL-dependent PGE2 production is not involved in such a normal physiology. Thus, hypothalamic PGE2 caused by RANKL-RANK signaling in females may involve MGL-independent mechanism(s) in part, which awaits further studies.
Supporting Information
Hypothalamic tissues were collected from Mgll +/+ and Mgll −/− mice (n = 6 for each group). Total lipids were extracted and fatty acid methyl esters (FAMEs) were prepared for total fatty acids, including free and esterified fatty acids. FAMEs were quantified using gas chromatography with flame ionization detector (GC-FID). Data are expressed as means ± SD. No statistically significant differences were found between genotypes (Bonferroni post-test after two-way ANOVA).
(PDF)
Hypothalamic tissues were collected from Mgll +/+ and Mgll −/− mice (n = 5 for each group). Phospholipids were extracted from cryomilled samples by methanol and analyzed by liquid chromatography-tandem mass spectrometry. Data are expressed as normalized mean values ± SD, using the total sum of the signals for diradyl-phospholipids or lyso-phospholipids. No statistically significant differences were found between genotypes (Bonferroni post-test after two-way ANOVA). (L)PC, (lyso)phosphatidylcholine; SM, sphingomyelin; (L)PE, (lyso)phosphatidylethanolamine; PS, phosphatidylserine; PI, phosphatidylinositol; LPA, lysophosphatidic acid. Numbers after phospholipid names indicate total carbon and double bond numbers for radyl group(s). ‘o’ and ‘p’ indicate O-alkyl and O-alkenyl group, respectively.
(PDF)
Mgll +/+ and Mgll −/− mice were intraperitoneally injected with 20 μg of LPS or saline. Two h later, hypothalamic tissues were collected and analyzed for lipid mediator levels by liquid chromatography-tandem mass spectrometry (n = 6–8 for each group). Data are expressed as means ± SD. ***p<0.001 vs. Mgll +/+, by Bonferroni post-test after two-way ANOVA.
(PDF)
Mgll +/+ and Mgll −/− mice were intraperitoneally injected with 20 μg of LPS or saline. Two h later, liver tissues were collected and analyzed for lipid mediator levels by liquid chromatography-tandem mass spectrometry (n = 2–8 for each group). Data are expressed as means ± SD. *p<0.05 vs. Mgll +/+, by Bonferroni post-test after two-way ANOVA.
(PDF)
Acknowledgments
We thank Dr. A. Tanimura for the kind assistance in mouse preparation. We also thank A. Kobayashi for technical assistance and other laboratory members for valuable discussions. This work was supported by MEXT KAKENHI Grant Numbers 23790356, 25116707 (to Y.K.), 21220006, 25000015 (to M.K.), and 24229003 (to T.S.), a grant from the Tokyo Society of Medical Sciences, Japan (to Y.K.), and Takeda Science Foundation (to T.S.). Cnr1 −/− mice were kindly provided by Dr. Andreas Zimmer at University of Bonn, Germany.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by MEXT KAKENHI Grant Numbers 23790356, 25116707 (to Y.K.), 21220006, 25000015 (to M.K.), and 24229003 (to T.S.), a grant from the Tokyo Society of Medical Sciences, Japan (to Y.K.), and Takeda Science Foundation (to T.S.). Department of Lipidomics, Graduate School of Medicine, The University of Tokyo, is funded in part by Ono Pharmaceutical Co., LTD. (Osaka, Japan) and Shimadzu Corp. (Kyoto, Japan). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Kluger MJ, Kozak W, Conn CA, Leon LR, Soszynski D. Role of fever in disease. Ann N Y Acad Sci. 1998;856:224–33. Epub 1999/01/26. . [DOI] [PubMed] [Google Scholar]
- 2. Cabanac M. Adjustable set point: to honor Harold T. Hammel. J Appl Physiol (1985). 2006;100(4):1338–46. Epub 2006/03/17. 10.1152/japplphysiol.01021.2005 . [DOI] [PubMed] [Google Scholar]
- 3. Netea MG, Kullberg BJ, Van der Meer JW. Circulating cytokines as mediators of fever. Clin Infect Dis. 2000;31 Suppl 5:S178–84. Epub 2000/12/13. 10.1086/317513 . [DOI] [PubMed] [Google Scholar]
- 4. Engblom D, Saha S, Engstrom L, Westman M, Audoly LP, Jakobsson PJ, et al. Microsomal prostaglandin E synthase-1 is the central switch during immune-induced pyresis. Nat Neurosci. 2003;6(11):1137–8. Epub 2003/10/21. 10.1038/nn1137 . [DOI] [PubMed] [Google Scholar]
- 5. Li S, Wang Y, Matsumura K, Ballou LR, Morham SG, Blatteis CM. The febrile response to lipopolysaccharide is blocked in cyclooxygenase-2(-/-), but not in cyclooxygenase-1(-/-) mice. Brain Res. 1999;825(1–2):86–94. Epub 1999/04/27. . [DOI] [PubMed] [Google Scholar]
- 6. Sugimoto Y, Narumiya S. Prostaglandin E receptors. J Biol Chem. 2007;282(16):11613–7. Epub 2007/03/03. 10.1074/jbc.R600038200 . [DOI] [PubMed] [Google Scholar]
- 7. Ushikubi F, Segi E, Sugimoto Y, Murata T, Matsuoka T, Kobayashi T, et al. Impaired febrile response in mice lacking the prostaglandin E receptor subtype EP3. Nature. 1998;395(6699):281–4. Epub 1998/09/29. 10.1038/26233 . [DOI] [PubMed] [Google Scholar]
- 8. Lazarus M, Yoshida K, Coppari R, Bass CE, Mochizuki T, Lowell BB, et al. EP3 prostaglandin receptors in the median preoptic nucleus are critical for fever responses. Nat Neurosci. 2007;10(9):1131–3. Epub 2007/08/07. 10.1038/nn1949 . [DOI] [PubMed] [Google Scholar]
- 9. Shimizu T, Ohto T, Kita Y. Cytosolic phospholipase A2: biochemical properties and physiological roles. IUBMB Life. 2006;58(5–6):328–33. Epub 2006/06/07. 10.1080/15216540600702289 . [DOI] [PubMed] [Google Scholar]
- 10. Steiner AA, Ivanov AI, Serrats J, Hosokawa H, Phayre AN, Robbins JR, et al. Cellular and molecular bases of the initiation of fever. PLoS Biol. 2006;4(9):e284 Epub 2006/08/29. 10.1371/journal.pbio.0040284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Prescott SM, Majerus PW. Characterization of 1,2-diacylglycerol hydrolysis in human platelets. Demonstration of an arachidonoyl-monoacylglycerol intermediate. J Biol Chem. 1983;258(2):764–9. Epub 1983/01/25. . [PubMed] [Google Scholar]
- 12. Bell RL, Kennerly DA, Stanford N, Majerus PW. Diglyceride lipase: a pathway for arachidonate release from human platelets. Proc Natl Acad Sci U S A. 1979;76(7):3238–41. Epub 1979/07/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nomura DK, Morrison BE, Blankman JL, Long JZ, Kinsey SG, Marcondes MC, et al. Endocannabinoid hydrolysis generates brain prostaglandins that promote neuroinflammation. Science. 2011;334(6057):809–13. Epub 2011/10/25. 10.1126/science.1209200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Uchigashima M, Yamazaki M, Yamasaki M, Tanimura A, Sakimura K, Kano M, et al. Molecular and morphological configuration for 2-arachidonoylglycerol-mediated retrograde signaling at mossy cell-granule cell synapses in the dentate gyrus. J Neurosci. 2011;31(21):7700–14. Epub 2011/05/27. 10.1523/JNEUROSCI.5665-10.2011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tanimura A, Yamazaki M, Hashimotodani Y, Uchigashima M, Kawata S, Abe M, et al. The endocannabinoid 2-arachidonoylglycerol produced by diacylglycerol lipase alpha mediates retrograde suppression of synaptic transmission. Neuron. 2010;65(3):320–7. Epub 2010/02/18. 10.1016/j.neuron.2010.01.021 . [DOI] [PubMed] [Google Scholar]
- 16. Uozumi N, Kume K, Nagase T, Nakatani N, Ishii S, Tashiro F, et al. Role of cytosolic phospholipase A2 in allergic response and parturition. Nature. 1997;390(6660):618–22. Epub 1997/12/24. 10.1038/37622 . [DOI] [PubMed] [Google Scholar]
- 17. Lovegrove BG. Modification and miniaturization of Thermochron iButtons for surgical implantation into small animals. J Comp Physiol B. 2009;179(4):451–8. Epub 2008/12/31. 10.1007/s00360-008-0329-x . [DOI] [PubMed] [Google Scholar]
- 18. Kita Y, Takahashi T, Uozumi N, Shimizu T. A multiplex quantitation method for eicosanoids and platelet-activating factor using column-switching reversed-phase liquid chromatography-tandem mass spectrometry. Anal Biochem. 2005;342(1):134–43. Epub 2005/06/17. 10.1016/j.ab.2005.03.048 . [DOI] [PubMed] [Google Scholar]
- 19. Kawai T, Akira S. Toll-like receptors and their crosstalk with other innate receptors in infection and immunity. Immunity. 2011;34(5):637–50. Epub 2011/05/28. 10.1016/j.immuni.2011.05.006 . [DOI] [PubMed] [Google Scholar]
- 20. Schlosburg JE, Blankman JL, Long JZ, Nomura DK, Pan B, Kinsey SG, et al. Chronic monoacylglycerol lipase blockade causes functional antagonism of the endocannabinoid system. Nat Neurosci. 2010;13(9):1113–9. Epub 2010/08/24. 10.1038/nn.2616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li Z, Perlik V, Feleder C, Tang Y, Blatteis CM. Kupffer cell-generated PGE2 triggers the febrile response of guinea pigs to intravenously injected LPS. Am J Physiol Regul Integr Comp Physiol. 2006;290(5):R1262–70. Epub 2006/01/18. 10.1152/ajpregu.00724.2005 . [DOI] [PubMed] [Google Scholar]
- 22. Plaisance KI. Toxicities of drugs used in the management of fever. Clin Infect Dis. 2000;31 Suppl 5:S219–23. Epub 2000/12/13. 10.1086/317518 . [DOI] [PubMed] [Google Scholar]
- 23. Tanimura A, Uchigashima M, Yamazaki M, Uesaka N, Mikuni T, Abe M, et al. Synapse type-independent degradation of the endocannabinoid 2-arachidonoylglycerol after retrograde synaptic suppression. Proc Natl Acad Sci U S A. 2012;109(30):12195–200. Epub 2012/07/12. 10.1073/pnas.1204404109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Engstrom L, Ruud J, Eskilsson A, Larsson A, Mackerlova L, Kugelberg U, et al. Lipopolysaccharide-induced fever depends on prostaglandin E2 production specifically in brain endothelial cells. Endocrinology. 2012;153(10):4849–61. Epub 2012/08/09. 10.1210/en.2012-1375 . [DOI] [PubMed] [Google Scholar]
- 25. Ridder DA, Lang MF, Salinin S, Roderer JP, Struss M, Maser-Gluth C, et al. TAK1 in brain endothelial cells mediates fever and lethargy. J Exp Med. 2011;208(13):2615–23. Epub 2011/12/07. 10.1084/jem.20110398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Savinainen JR, Saario SM, Laitinen JT. The serine hydrolases MAGL, ABHD6 and ABHD12 as guardians of 2-arachidonoylglycerol signalling through cannabinoid receptors. Acta Physiol (Oxf). 2012;204(2):267–76. Epub 2011/03/23. 10.1111/j.1748-1716.2011.02280.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hanada R, Leibbrandt A, Hanada T, Kitaoka S, Furuyashiki T, Fujihara H, et al. Central control of fever and female body temperature by RANKL/RANK. Nature. 2009;462(7272):505–9. Epub 2009/11/27. 10.1038/nature08596 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hypothalamic tissues were collected from Mgll +/+ and Mgll −/− mice (n = 6 for each group). Total lipids were extracted and fatty acid methyl esters (FAMEs) were prepared for total fatty acids, including free and esterified fatty acids. FAMEs were quantified using gas chromatography with flame ionization detector (GC-FID). Data are expressed as means ± SD. No statistically significant differences were found between genotypes (Bonferroni post-test after two-way ANOVA).
(PDF)
Hypothalamic tissues were collected from Mgll +/+ and Mgll −/− mice (n = 5 for each group). Phospholipids were extracted from cryomilled samples by methanol and analyzed by liquid chromatography-tandem mass spectrometry. Data are expressed as normalized mean values ± SD, using the total sum of the signals for diradyl-phospholipids or lyso-phospholipids. No statistically significant differences were found between genotypes (Bonferroni post-test after two-way ANOVA). (L)PC, (lyso)phosphatidylcholine; SM, sphingomyelin; (L)PE, (lyso)phosphatidylethanolamine; PS, phosphatidylserine; PI, phosphatidylinositol; LPA, lysophosphatidic acid. Numbers after phospholipid names indicate total carbon and double bond numbers for radyl group(s). ‘o’ and ‘p’ indicate O-alkyl and O-alkenyl group, respectively.
(PDF)
Mgll +/+ and Mgll −/− mice were intraperitoneally injected with 20 μg of LPS or saline. Two h later, hypothalamic tissues were collected and analyzed for lipid mediator levels by liquid chromatography-tandem mass spectrometry (n = 6–8 for each group). Data are expressed as means ± SD. ***p<0.001 vs. Mgll +/+, by Bonferroni post-test after two-way ANOVA.
(PDF)
Mgll +/+ and Mgll −/− mice were intraperitoneally injected with 20 μg of LPS or saline. Two h later, liver tissues were collected and analyzed for lipid mediator levels by liquid chromatography-tandem mass spectrometry (n = 2–8 for each group). Data are expressed as means ± SD. *p<0.05 vs. Mgll +/+, by Bonferroni post-test after two-way ANOVA.
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.