Abstract
Autism spectrum disorder (ASD) is characterized by high rates of comorbid internalizing and externalizing disorders. One mechanistic account of these comorbidities is that ASD is characterized by impaired emotion regulation (ER) that results in deficits modulating emotional responses. We assessed neural activation during cognitive reappraisal of faces in high functioning adults with ASD. Groups did not differ in looking time, pupilometry, or subjective ratings of faces during reappraisal. However, instructions to increase positive and negative emotional responses resulted in less increase in nucleus accumbens and amygdala activations (respectively) in the ASD group, and both regulation instructions resulted in less change in dorsolateral prefrontal cortex activation in the ASD group. Results suggest a potential mechanistic account of impaired ER in ASD.
Keywords: Autism spectrum disorder, ER, Dorsolateral Prefrontal Cortex, Amygdala, Nucleus Accumbens, Cognitive Reappraisal, Functional Magnetic Resonance Imaging, Eyetracking, Pupilometry
Although the core features of autism spectrum disorder (ASD) are in the domains of social-communication and restricted and repetitive behaviors (American Psychiatric Association, 2013), ASD is a pervasive neurodevelopmental disorder characterized by impairments in a number of areas. Accumulating evidence suggests that ASD is characterized by broad impairments in affective expression and regulation, including tantrums, aggression, self-injury, anxiety, and irritability (Lecavalier, 2006). Irritability in particular is the primary reason that caregivers seek treatment for ASD (Arnold et al., 2003) and is the strongest predictor of stress in parents of children with ASD (Davis & Carter, 2008). Emotion regulation (ER), the capacity to willfully modulate the intensity of affective reactions is a critical adaptive response to changing environmental demands (Parkinson & Totterdell, 1999; Schore, 2003), and as such, deficits in the capacity to effortfully modulate affective experience may represent an explanatory framework for impaired ER in ASD.
Impaired ER in ASD may also explain the increased rates of comorbid internalizing disorders in ASD given that such disorders are themselves characterized by impaired ER (Bauminger, Solomon, & Rogers, 2010; Jazaieri, Urry, & Gross, 2013; White, Oswald, Ollendick, & Scahill, 2009). As many as four out of five children with ASD are diagnosed with comorbid psychiatric disorders (Simonoff et al., 2008). In particular, prevalence estimates for anxiety disorders in ASD are as high as 84% (Muris, Steerneman, Merckelbach, Holdrinet, & Meesters, 1998), and prevalence estimates of major depressive disorder are as high as 70% in ASD (Lugnegard, Hallerback, & Gillberg, 2011). Although there is evidence that diagnostic practices that are tailored to isolate ASD-specific impairments reveal somewhat lower rates of comorbid disorders in ASD (Mazefsky et al., 2012), individuals with ASD are nevertheless at increased risk of experiencing a range of behavioral and emotional problems related to impaired ER, and are prone to use emotional suppression rather than cognitive reappraisal in the context of potentially threatening negative stimuli (Samson, Hardan, Podell, Phillips, & Gross, 2014). Given the high prevalence of internalizing comorbid psychiatric disorders in ASD, constructs implicated in such disorders are prime targets to investigate as potential contributing factors to ASD etiology. Moreover, the severity of depression symptoms in children with ASD have been found to be unrelated to positive mental coping strategies, suggesting that impaired ER in ASD is not only a reflection of internalizing symptoms but may be characteristic as ASD itself (Rieffe et al., 2011).
Additionally, ER is important not only for understanding associated features of ASD, but is relevant to core symptoms of social communication that define ASD as well (Mazefsky et al., 2013; Weiss, Thomson, & Chan, 2014). For example, emotional awareness, recognition of emotional experience in others, and impaired identification and expression of social gestures may all reflect impaired modulation of social-emotional information processing (Bachevalier & Loveland, 2006; Lecavalier, 2006; Zwaigenbaum et al., 2005) because they require the adjustment of internal affective experiences to changing environmental conditions (Gross, 2013; Ochsner, Bunge, Gross, & Gabrieli, 2002; Ray, Wilhelm, & Gross, 2008). Moreover, ER impairments in ASD have been found to be associated with the overall severity of all core features of ASD (Samson, Phillips, et al., 2014), and ER impairments in ASD may compromise the quality and quantity of early social interactions, and thus may have an adverse impact across development on neural systems critical to social-communicative abilities (White et al., 2014).
The capacity to effectively modulate emotional responses, both automatically and volitionally, is critical for emotional well-being and mental health (Eisenberg & Spinrad, 2004; Fitzsimmons & Bargh, 2004). Emotion regulation is a complex and dynamic process that broadly refers the modification of biological, subjective, and expressive components of emotional experience (Thompson, 1994) and requires flexibility in adapting to changing circumstances (Diamond & Aspinwall, 2003; Gray, Braver, & Raichle, 2002; Keltner & Gross, 1999). Optimal regulation of emotion responses protects against psychopathology, and improving ER is an effective cognitively-based intervention strategy for a range of psychiatric disorders (Keshavan, Vinogradov, Rumsey, Sherrill, & Wagner, 2014). Skills in the domain of cognitive reappraisal are a core developmental acquisition in early and middle childhood (Dennis, 2010) and cognitive reappraisal deficits have been identified in a number of forms of psychopathology (Chambers, Gullone, & Allen, 2009; Koenigsberg et al., 2002; Rottenberg & Gross, 2007).
The purpose of the present study was to examine neural activation during cognitive reappraisal in ASD. Cognitive reappraisal is a form of consciously deployed ER that, in nonclinical samples, effectively modulates subjective responses via a reinterpretation of the meaning of emotional challenges (Butler, Wilhelm, & Gross, 2006; Ochsner et al., 2002; Ray et al., 2008). Reappraisal encompasses both the down-regulation (i.e., attenuation) of negative emotional responses and the up-regulation (i.e., enhancement) of positive emotional responses (Gross, 2013). Effective cognitive reappraisal constrains affective experience to be within a “window of tolerance” between hypo- and hyper-reactivity, maximizing the potential for optimal social-affective functioning (Schore, 2003) and for generating adaptive perspectives (Parkinson & Totterdell, 1999).
Consciously-deployed changes in emotional responses are mediated via modulating effects of dorsolateral, ventrolateral, and medial regions of prefrontal cortex (PFC) involved in cognitive control on brain regions involved in arousal and motivation, including limbic and brainstem regions and medial and orbitofrontal prefrontal cortices (Davidson, 2002; Dolan, 2002; Luu, 2004; Urry et al., 2006). Specifically, cognitive strategies to down-regulate emotional responses to aversive stimuli recruit dorsal and lateral PFC, medial PFC, and anterior cingulate cortex, while simultaneously reducing activation in areas associated with emotion processing, including the amygdala, medial orbitofrontal cortex, lateral orbitofrontal cortex and the nucleus accumbens (NAc; Kalisch, 2009; Kim & Hamann, 2007; Lévesque et al., 2003; Ochsner et al., 2004; Schaefer et al., 2002). Similarly, largely overlapping PFC regions mediate changes in positive emotional responses (Kim & Hamann, 2007), however the corresponding changes in activation of limbic regions, including the NAc, are increased (Heller et al., 2009; Ochsner et al., 2004), suggesting that cognitive control impacts both the up- and down-regulation of emotion.
In the present study, we used functional magnetic resonance imaging (fMRI) combined with eyetracking and pupilometry to examine neural responses during cognitive reappraisal of images of faces in ASD. We selected faces as the target stimulus in this initial study given that ASD is characterized by deficits in social cognition as thus group differences in neural mechanisms of cognitive reappraisal may be most pronounced in the context of social stimuli. Though there are no published studies to date addressing cognitive reappraisal of social information in ASD, Pitskel and colleagues (2014) reported that typically developing children and adolescents showed significant down-regulation of activation in the amygdala and insula when consciously decreasing affective responses to pictures eliciting disgust, whereas children with ASD did not exhibit similar neural patterns during down-regulation. The present study extends this line of research to address cognitive reappraisal of faces specifically as well as to include both positive and negative cognitive reappraisal conditions.
Our hypotheses were shaped by the nonclinical literature highlighting the modulatory influence of cognitive control regions in the lateral prefrontal cortex (see Buhle et al., 2013; Frank et al., 2014 for recent meta-analyses), as well as the ASD fMRI literature that indicates that ASD is characterized by impaired recruitment of brain regions that respond to socio-affective information (including the medial and lateral PFC, orbitofrontal cortex, as well as the amygdala and the NAc) and by impaired recruitment of brain regions involved in cognitive control, including ventral and lateral PFC (see Dichter, 2012 for a review). Thus, we specifically hypothesized that during a task requiring cognitive control of socio-affective information, the ASD group would be characterized by reduced PFC recruitment during cognitive reappraisal and that positive and negative cognitive reappraisal would result in decreased modulation of NAc and amygdala activation, respectively.
Methods
Participants
Participants consented to protocols approved by the local Human Investigations Committees at both UNC-Chapel Hill and Duke University Medical Centers and were paid $40 for the imaging portion of the study. Participants completed a mock scan prior to imaging. Fifteen neurotypical control participants (14 right-handed; 13 male; mean (SD) age: 27.4 (8.3)) were recruited from lists of control subjects maintained by the Duke-UNC Brain Imaging and Analysis Center (BIAC). Control participants were not taking any psychotropic medications at the time of scanning. The ASD group was comprised of fifteen right-handed participants (13 male; mean (SD) age: 26.1 (8.1); five diagnosed with Asperger’s Disorder) and were recruited via the Autism Subject Registry maintained through the UNC Carolina Institute for Developmental Disabilities. All participants had normal or corrected-to-normal vision, and exclusion criteria for the ASD group included a history of medical conditions associated with ASD, including Fragile X syndrome, tuberous sclerosis, neurofibromatosis, phenylketonuria, epilepsy and gross brain injury, full-scale intelligence < 80, or MRI contraindications. Six ASD participants were not taking any psychotropic medications; one was taking abilify, one was taking risperidone, and the remaining seven were taking multiple medications (i.e., combinations of aripiprazole, citalopram, lithium, fluvoxamine, buproprion, adderall, and fluoxetine). Diagnoses of ASDs were based on a history of clinical diagnosis confirmed by proband assessment by a research reliable assessor with the Autism Diagnostic Observation Schedule (ADOS-G; Lord et al., 2000) with standard algorithm cutoffs.
Both groups completed the Weschler Abbreviated Scale of Intelligence (WASI, Weschler, 1999), the Social Responsiveness Scale, a continuous measure of ASD symptom severity (Constantino et al., 2003), and the Repetitive Behavior Scale-Revised (RBS-R; Bodfish, Symons, & Lewis, 1999) to assess the severity of repetitive behaviors. Control participants completed the Autism Quotient (Baron-Cohen, Wheelwright, Skinner, Martin, & Clubley, 2001) to verify that they were below the recommended ASD cutoff of 32. Table 1 illustrates demographic data and symptom profiles of study participants.
Table 1.
Means (SDs) of demographic data and symptom profiles.
| Autism (n=15) | Control (n=15) | t (p) | |
|---|---|---|---|
| Age | 26.1 (8.1) | 27.4 (8.3) | 0.43 (0.67) |
| ADOS | |||
| Comm | 6.0 (4.9) | - | - |
| SI | 8.7 (2.2) | - | - |
| SBRI | 2.3 (1.9) | - | - |
| WASI | |||
| Verbal | 108.8 (16.3) | 111.4 (11.2) | 0.51 (0.61) |
| Performance | 115.7 (11.7) | 117.4 (12.5) | 0.39 (0.70) |
| Full | 113.6 (13.8) | 116.3 (11.6) | 0.57 (0.57) |
| SRS | |||
| Aware | 8.5 (4.4) | 4.9 (1.7) | 3.0 (0.006) |
| Cog | 11.1 (6.3) | 4.2 (3.7) | 3.6 (<0.001) |
| Comm | 22.9 (12.5) | 8.7 (7.1) | 3.8 (<0.001) |
| Mot | 13.9 (7.6) | 6.9 (3.5) | 3.2 (0.003) |
| AutMann | 14.1 (7.0) | 4.9 (3.2) | 4.6 (<0.001) |
| Total | 61.7 (35.2) | 29.6 (16.5) | 4.1 (<0.001) |
| RBS-R | |||
| Stereo | 5.4 (3.5) | 2.0 (3.3) | 2.7 (0.01) |
| SIB | 2.7 (2.3) | 0.4 (1.3) | 3.3 (0.002) |
| Comp | 8.1 (5.4) | 2.7 (4.6) | 2.9 (0.006) |
| Rit | 6.1 (5.3) | 1.5 (2.7) | 3.0 (0.005) |
| Same | 10.9 (7.8) | 1.9 (3.0) | 4.2 (<0.001) |
| CI | 4.9 (3.0) | 0.9 (1.4) | 4.7 (<0.001) |
| Total | 38.1 (22.8) | 9.3 (14.4) | 4.1 (<0.001) |
WASI: Wechsler Abbreviated Scale of Intelligence (Weschler, 1999).
ADOS: Autism Diagnostic Observation Scale (Lord et al., 2000); Comm: Communication; SI: Reciprocal Social Interaction; SBRI: Stereotyped Behaviors and Restricted Interests.
SRS: Social Responsiveness Scale (Constantino et al., 2003). Aware: Awareness; Cog: Cognition; Comm: Communition; Mot: Motivation; AutMann: Autistic Mannerisms RBS-R: Repetitive Behavior Scale-Revised (Bodfish et al., 1999); Stereo: Stereotyped Behavior; SIB: Self-Injurious Behavior; Comp: Compulsive Behavior; Rit: Ritualistic Behavior; Same: Sameness Behavior; CI: Circumscribed Interests.
Pre-Scan Cognitive Reappraisal Training Sessions
Care was taken to ensure that participants with ASD who completed the imaging portion of the study implemented cognitive reappraisal appropriately. Prior to scanning, participants completed a cognitive reappraisal training session conducted in a one-on-one format with a clinical psychologist (J.A.R.) using a PowerPoint presentation as a visual aid (a copy of the training materials are available upon request from the corresponding author). Participants were told that they would see pictures of faces and that part-way through the presentation of each image, they would hear a verbal prompt instructing them to either “Think Positive” or “Think Negative” about the image. These terms were chosen in consultation with clinicians at Chapel Hill Division TEACCH to be maximally clear to participants with ASD (for example, terms such as “enhance” or “regulate” were deemed to be too abstract for individuals with ASD).
The cognitive reappraisal training proceeded in three stages. First, the experimenter explained the cognitive reappraisal strategies by displaying several sample images not used in the fMRI task while providing descriptions of cognitive reappraisal strategies. Participants were instructed to reinterpret the meaning of the image in a way that changed their emotional reactions to the picture. Specifically, participants were instructed that to “think positive” about a face, they should imagine the picture is of someone they are interested in, whom they really like, who really likes them, or who is a kind and friendly person. To “think negative” about a face, they were instructed to imagine that the picture is of someone hostile or whom they don’t like. Participants were reminded that they may be asked to “think negative” about pictures that they liked and to “think positive” about pictures that they didn’t like. Both self-focused and situation-focused reappraisal strategies were permitted (c.f. Ochsner et al., 2004). Participants were also told not to look away from images, not to distract themselves, and not to close their eyes as ways to modify the emotional responses.
Second, participants worked collaboratively with the experimenter to practice generating appropriate cognitive reappraisal strategies in the context of several additional images (also not drawn from the fMRI paradigm). During this phase, participants were asked to generate and verbalize a cognitive reappraisal strategy and feedback was provided regarding the appropriateness of each attempt. Examples of correct responses (e.g., describing or interpreting the stimulus in the instructed emotional direction) from individuals with ASD included the following: For “think positive”: “I’ll associate it with someone I like and find good things about their appearance.” For “think negative”: “I’ll think about someone I don’t like who could hurt my feelings.” Conversely, examples of incorrect responses (e.g., using emotional terms inconsistent with the instructed direction) from individuals with ASD included the following: For “think positive”: “He reminds me of someone I know who is an actor.” For “think negative”: “I don’t like the way he looks.” Finally, to verify cognitive reappraisal comprehension, twelve additional practice images were shown and participants were asked to generate and verbalize examples of cognitive reappraisal strategies independently. Two participants with ASD who otherwise met inclusion criteria for the study did not demonstrate adequate comprehension on at least 10/12 practice trials and thus did were not scanned, resulting in a final sample of 15 participants with ASD who participated in the fMRI portion of the study.
fMRI Task
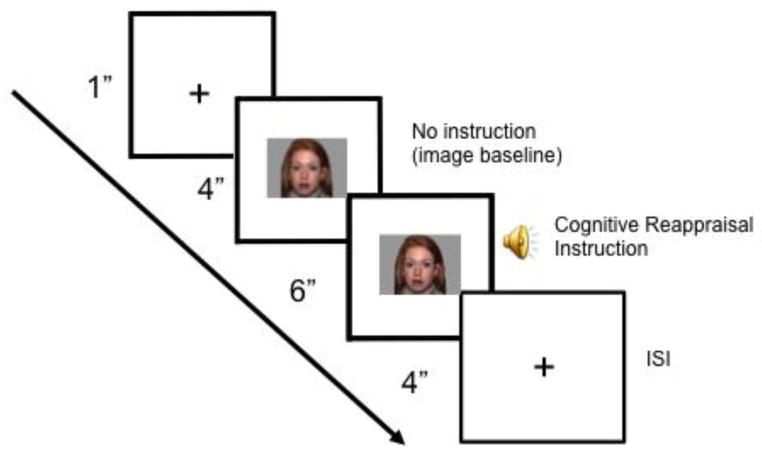
A modified version of a standard cognitive reappraisal task was used, wherein participants viewed a stimulus before and after implementing cognitive reappraisal (e.g., Heller et al., 2009; van Reekum et al., 2007), as depicted in Figure 1. Faces were neutral closed-mouth images from the NimStim set (Tottenham et al., 2009). Stimuli were presented using E-Prime software v. 2.0 (Psychology Software Tools Inc., Pittsburgh, PA). Trials began with a 1-s fixation coupled with an orienting tone, after which a face was presented for 10 s. 4 s after image onset, audio prompts to either “Think Positive” or “Think Negative” signaled the participant to engage a specific cognitive reappraisal strategy. Across four runs that were each 480 seconds in length, 40 faces were presented: 16 were presented with instructions to “Think Positive”; 16 were presented with instructions to “Think Negative”; and eight additional trials were presented with instructions to “Look” at the image to reduce predictability. Not presented here are findings from other trials that presented images of objects instead of faces.
Figure 1.
Cognitive reappraisal fMRI task. On each trial, participants viewed a neutral face for 10 s. 4 s after image onset an audio prompt signaled the participant to engage a specific reappraisal strategy.
Eyetracking and pupilometry acquisition
Eyetracking was collected concurrently with fMRI via an MR-compatible miniature analog video camera (Resonance Technology, Inc.) mounted on the scanner head coil. Although the camera was originally designed to be used with video goggles, a custom-made bracket was made so that the camera was compatible with a video projector system within the scanner. The setup ensured that individuals of various head sizes were suitable for eyetracking and streamlined the set-up and adjustment procedures. Data were collected at 60 Hz with Viewpoint software (Arrington Research ©).
Prior to the start of each scan run, gaze fixations were calibrated by monitoring pupil movements to 16 dynamic fixation points presented at known locations in the visual display. The monitoring of gaze fixations was to ensure that the observed neural effects of cognitive reappraisal were not due to differential patterns of fixations on or off the task images. Thus, areas of interest (AOI) were traced around the external edges of images, and the percentage of time each participant fixated on or off each images was averaged for each participant and each task condition.
Pupilometry represents an index of arousal and of expended cognitive effort (Cabestrero, Crespo, & Quiros, 2009) and covaries with cognitive reappraisal, such that expanded pupil diameter corresponds to greater expended effort (Johnstone, van Reekum, Urry, Kalin, & Davidson, 2007; Urry, 2010; van Reekum et al., 2007). Pupilometry reduction and analysis followed methods outline by Van Reekum and colleagues (2007) and Urry and colleagues (2006). First, blinks were identified and eliminated and missing data points were estimated using linear interpolation. The pupilometry signal was smoothed by a 5-sample rolling average, and slow drifts were removed via linear detrending within each run. Pupilometry values > 4 SDs from the within-subjects mean were discarded. Pupil diameter was aggregated into half-second bins that were range-corrected within subjects. The mean diameters for the half-second picture periods immediately prior to regulation instructions were then subtracted from the mean pupil diameter during each half-second picture periods following cognitive reappraisal instructions, and the proportional change in pupil diameter was then computed for each of the time points following the instruction (i.e., [post–pre]/pre).
fMRI Acquisition
Scanning was performed on a General Electric Health Technologies, 3 Tesla Signa Excite HD scanner system with 50-mT/m gradients (General Electric, Waukesha, Wisconsin, USA). Head movement was restricted using foam cushions. An eight-channel head coil was used for parallel imaging. Two hundred and six high-resolution images were acquired using a 3D fast SPGR pulse sequence (TR = 7.58 ms; TE = 2.936 ms; FOV = 22 cm; image matrix = 2562; voxel size = 1 1 1 mm) and used for coregistration with the functional data. These structural images were aligned in the near axial plane defined by the anterior and posterior commissures. Whole brain functional images consisted of 32 slices parallel to the AC-PC plane using a BOLD-sensitive spiral sequence with sense reconstruction with higher-order shimming, at TR of 1500 ms (TE: 30 ms; FOV: 22 cm; voxel size: 4.00 4.00 3.80; flip angle 60°). Runs began with 4 discarded RF excitations to allow for steady state equilibrium.
fMRI Data Analysis
Preprocessing
Separation of brain tissue from the skull was accomplished using the brain extraction tool (Smith et al., 2004) in FSL version 4.1.4 (Oxford Centre for Functional Magnetic Resonance Imaging of the Brain (FMRIB), Oxford University, U.K.]. Preprocessing of functional data was accomplished in Statistical Parametric Mapping software (SPM8; Wellcome Department of Cognitive Neurology; http://www.fil.ion.ucl.ac.uk/spm) as implemented in Nipype (Gorgolewski et al., 2011), a python-based framework designed for highly pipelined processing of fMRI data from several neuroimaging packages (http://nipy.org/nipype). Our Nipype code is available for download at http://github.com/scanlab-admin/nipype/blob/master/autreg. Preprocessing of fMRI data was conducted in the following steps: (1) slice timing correction temporally aligned the interleaved functional images; (2) correction to the middle functional image was then performed using a six-parameter rigid-body transformation; and (3) functional images were co-registered to structural images in native space. For this co-registration step, functional-to-structural 6 DOF (rigid body) transformations were carried out using brain-boundary based registration (bbregister; Greve & Fischl, 2009) which uses the geometry information of the grey-white matter boundary derived from the automated cortical/subcortical parcellation stream in Freesurfer v5.1 (http://surfer.nmr.mgh.harvard.edu/; Fischl et al., 2004) to conduct cross-modal registration within-subjects. Next, structural images were normalized into a standard stereotaxic space (Montreal Neurological Institute) for intersubject comparison using a diffeomorphic warp as implemented in the Advanced Normalization Tools (ANTS; Avants et al., 2011). The same transformation matrices used for structural-to-standard transformations were then used for functional-to-standard space transformations of co-registered functional images. For GLM analyses, images were smoothed with a 5mm isotropic Gaussian kernel and then high-pass filtered (128s width) in the temporal domain.
General linear model
fMRI data were convolved with the SPM canonical double-gamma hemodynamic response function (HRF). We convolved each condition separately under the assumption that BOLD responses for each condition may be modeled independently despite the lack of a temporal interval between conditions. We initially estimated the following general linear model (GLM) for BOLD responses with an AR(1) structure. The autoregressive (AR) model corrects for temporal autocorrelation of the residuals in fMRI data, thus reducing the potential for false positives in the Restricted Maximum Likelihood (ReML) parameter estimation approach. Onset times and durations of events were used to model a signal response containing a regressor for each response type, which was convolved with a double-γ function to model the hemodynamic response of the entire duration of the pre- and post-instruction phases of the task. Model fitting generated whole brain images of parameter estimates and variances, representing average signal change from baseline. Group-wise activation and deactivation images were calculated by a mixed effects higher level analysis using a whole-brain univariate GLM in which we regressed the preprocessed and spatially smoothed BOLD signal on the pre- and post-instruction period We also included the time series of six head motion parameters as regressors of no interest. The following models were evaluated: (1) Group differences for the contrast of Enhance Positive > Pre- Regulation; (2) Group differences for the contrast of Enhance Negative > Pre- Regulation; and (3) Group differences for the contrast of both regulation conditions (Enhance Negative and Enhance Positive) > Pre- Regulation. Contrasts with the Look condition were evaluated in an exploratory manner even though this condition contained fewer trials than either regulation condition. All results were thresholded at Z>3.3 and were false discovery rate (FDR) corrected at p < .01, with the exception of Enhance Positive > Pre- Regulation, Control > ASD, which was FDR corrected at p < .001 to aid interpretability.
Picture Ratings
After scanning, participants completed a picture rating task outside of the scanner that was identical to the in-scanner task except that after each trial participants provided valence and arousal ratings using the self-assessment mannequin (Bradley & Lang, 1994).
Results
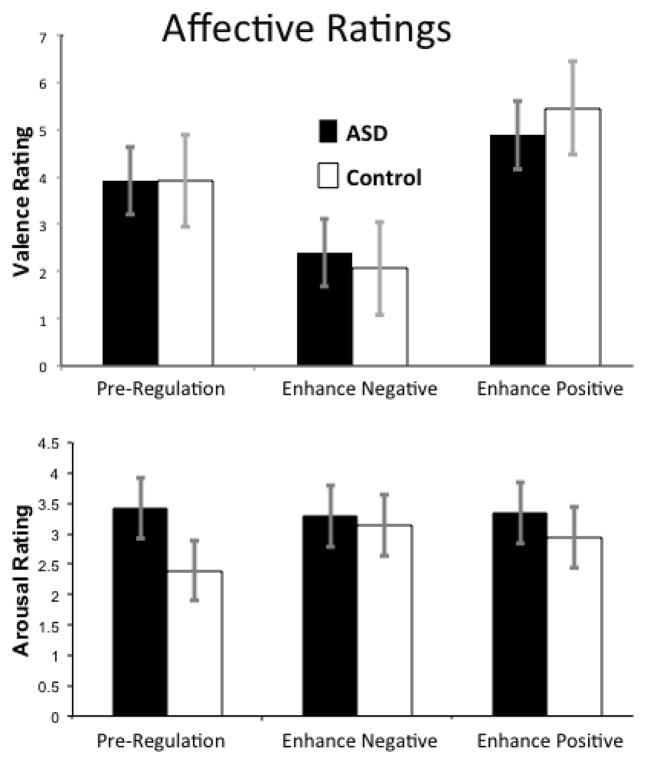
Valence Ratings
A 2 (Group: Control, ASD) x 3 (Condition: “Pre-Regulation”, “Think Negative”, and “Think Positive”) repeated measures MANOVA revealed a main effect of Condition, multivariate F(1,24)= 77.48, p<.0001, reflecting that across groups, valence ratings of faces were conditional on ER condition. There was no significant main effect of Group or Group × Condition interaction, p’s>.16. Between group t-tests detected no significant group differences for any condition, p’s>.20. Within-groups t-tests conducted separately in the ASD and control groups testing for differences between Conditions revealed significant differences between all condition pairs for the ASD group, p’s< .0002, and the Control group, p’s< .0004. Figure 2 (upper panel) illustrates group-averaged valence ratings.
Figure 2.
Subjective ratings. After scanning, participants rated images on the dimensions of valence (top) and arousal (bottom) with and without cognitive reappraisal strategies. Error bars are standard errors of the mean. The range and direction of the ratings are −4 (extremely unpleasant) to +4 (extremely pleasant) and 0 (not at all aroused) to +8 (extremely aroused).
Arousal Ratings
A 2 (Group: Control, ASD) x 3 (Condition: “Pre-Regulation”, “Think Negative”, and “Think Positive”) repeated measures MANOVA revealed no main effects of Condition, Group, or Group × Condition interaction, p’s<.24. Between group t-tests detected no significant group differences for any condition, p’s>.11. Within-groups t-tests conducted separately in the ASD and control groups testing for differences between Conditions revealed no significant differences across all condition pairs for the ASD group, p’s>.70, and the Control group (p’s>.12). Figure 2 (lower panel) illustrates group-averaged arousal ratings.
Pupilometry
A 2 (Group: control, ASD) x 3 (Condition: “Pre-Regulation”, “Think Positive”, and “Think Negative”) repeated measure MANOVA revealed a main effect of Condition, Multivariate F(2,24)=4.20, p= .027, reflecting that across groups and stimulus types pupil diameter was contingent on condition, but no main effect of Group or Group x Condition interaction, p’s > .10. Paired t-tests examining Condition effects for both groups combined revealed that the main effect of Condition was attributable to all participants having larger pupil diameters for the Positive condition, t(26)=2.80 p=.0094, and Negative condition, t(26)=2.95, p= .0066, relative to the Pre-Regulation Condition. Between-group t-tests detected no group differences for any condition, p’s > .10. Within-groups t-tests conducted separately in the ASD and control groups testing for differences between Conditions revealed that the ASD group demonstrated larger pupil diameters for the Negative face Condition relative to the Pre-Regulation condition, t(14)= 3.30, p<.005, but no other effects were significant, p’s > .15. The left side of Figure 3 illustrates group-averaged changes in pupil diameter for both regulation conditions.
Figure 3.
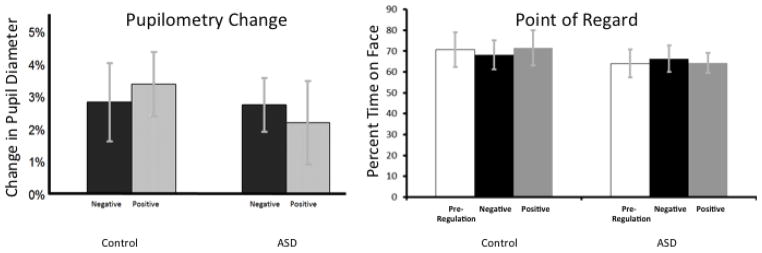
Left: In-scanner change in pupilometry from pre-regulation to negative and positive regulation revealed that both groups were characterized by relatively equivalent increases in pupil diameter during both regulation strategies. Right: In-scanner point-of-regard revealed that both group looked at the face images for relatively equivalent amounts of time before regulation and during both regulation strategies. Not shown is gaze time to eyes and faces separately, which likewise did not differ between groups (p’s>20).
Eyetracking
A 2 (Group: control, ASD) x 3 (Condition: “Pre-Regulation”, “Think Positive”, and “Think Negative”) repeated measure MANOVA revealed no significant effects of Group, Condition, or Group × Condition interaction, p’s > .10, on amount of time spent looking at the face stimuli. When this analysis was repeated for the eyes and mouth regions separately, there were once again no main or interactive effects, p’s>.10. Between groups t-tests detected no significant group differences for any condition, p’s > .10. Within-groups t-tests conducted separately in the ASD and control groups testing for differences between Conditions revealed no significant differences across all condition pairs for both groups for the whole face or for the eyes or mouth regions, p’s > .10. The right side of Figure 3 illustrates group-averaged eyetracking data for time spent looking at faces.
fMRI Results
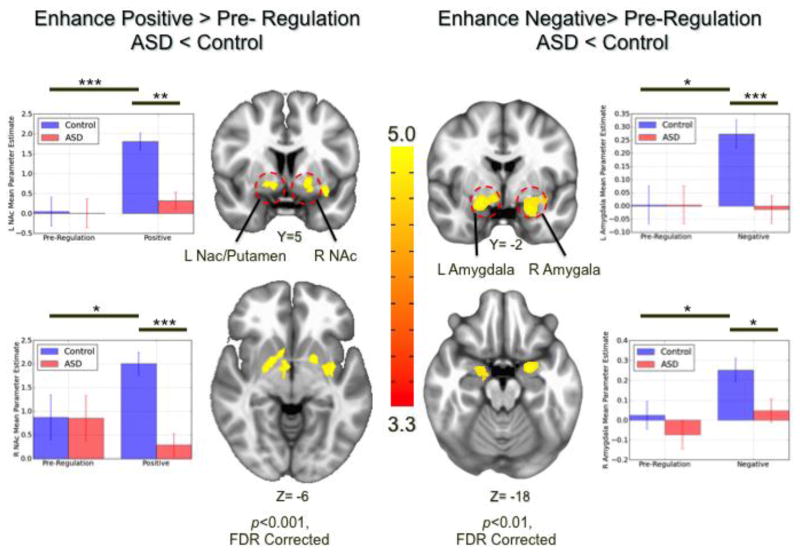
Group differences for the contrast of Enhance Positive > Pre-Regulation
The left of Figure 4 and the top of Table 2 indicates that for the contrast of Enhance Positive > Pre- Regulation, the ASD group was characterized by relatively less increase in activation in the right NAc as well as a left-lateralized cluster that included both the putamen and the NAc than the control group. As can be seen from the bar graphs on the left of Figure 4, this effect was mainly due to an increase in activity during the positive regulation condition in the control group, whereas the ASD group showed minimal change in bilateral NAc activity during the positive regulation condition. There were no clusters with relatively greater increases in activation in the ASD group relative to the control group for this contrast.
Figure 4.
Left: For the contrast of Enhance Positive > Pre- Regulation, the ASD group was characterized by relatively less increase activation in right nucleus accumbens (NAc) and a left-lateralized cluster that included the putamen and NAc than the control group. Right: For the contrast of Enhance Negative > Pre- Regulation, the ASD group was characterized by relatively less increase in left and right amygdala activation than the control group (*** p<0.001; ** p<0.01).
Table 2.
Clusters reflecting significant group differences (Z>3.3).
| (A) Enhance Positive > Pre-Instruction (FDR correction at p<0.001) | |||||||
|---|---|---|---|---|---|---|---|
| Region | Hemi | Size (Nvoxel) | Mean t-value | Peak t-value | MNI Coordinates | ||
| X | Y | Z | |||||
| CON > ASD | |||||||
| Nucleus accumbens | Right | 4022 | 4.49 | 5.04 | 12 | 7 | −9 |
| Nucleus Accumbens/Putamen | Left | 3642 | 4.01 | 5.49 | −23 | 5 | −7 |
| ASD > CON | |||||||
| No Clusters Significant* | -- | -- | -- | -- | -- | -- | -- |
| (B) Enhance Negative > Pre-Instruction (FDR correction at p<0.01) | |||||||
|---|---|---|---|---|---|---|---|
| Region | Hemi | Size (Nvoxel) | Mean t-value | Peak t-value | MNI Coordinates | ||
| X | Y | Z | |||||
| CON > ASD | |||||||
| Amygdala | Left | 3116 | 4.06 | 5.62 | −19 | 1 | −17 |
| Amygdala | Right | 3054 | 3.91 | 5.34 | 25 | 2 | −25 |
| ASD > CON | |||||||
| No Clusters Significant* | -- | -- | -- | -- | -- | -- | -- |
| (C) Any Regulation > Pre-Instruction (FDR correction at p<0.01) | |||||||
|---|---|---|---|---|---|---|---|
| Region | Hemi | Size (Nvoxel) | Mean t-value | Peak t-value | MNI Coordinates | ||
| X | Y | Z | |||||
| CON > ASD | |||||||
| Middle Frontal Gyrus | Left | 7572 | 2.88 | 4.48 | −43 | 22 | 30 |
| Middle Frontal Gyrus | Right | 5193 | 2.78 | 3.94 | 41 | 17 | 33 |
| Superior Frontal Gyrus | Left | 1299 | 2.83 | 3.59 | −23 | 29 | 53 |
| ASD > CON | |||||||
| No Clusters Significant* | -- | -- | -- | -- | -- | -- | -- |
No clusters significant with FDR correction at p< 0.05.
Group differences for the contrast of Enhance Negative > Pre-Regulation
The right of Figure 4 and the middle of Table 2 illustrates that for the contrast of Enhance Negative > Pre-Instruction, the ASD group was characterized by relatively less increase in left and right bilateral amygdala activation than the control group. As can be seen from the bar graphs on the right of Figure 4, this effect was mainly due to an increase in bilateral amygdala activity during the negative regulation condition in the control group, whereas the ASD group showed minimal change in bilateral amygdala activity during the negative regulation condition. There were no clusters with relatively greater increases in activation in the ASD group relative to the control group for this contrast.
Note that, as indicated in Table 2, the effects observed the contrast of Enhance Positive > Pre-Regulation and for the contrast of Enhance Negative > Pre-Regulation were specific to those contrasts. In other words there was no significant Group effect in the NAc for the Enhance Negative > Pre-Regulation contrast, and no significant Group effect in the amygdala for the Enhance Positive > Pre-Regulation contrast.
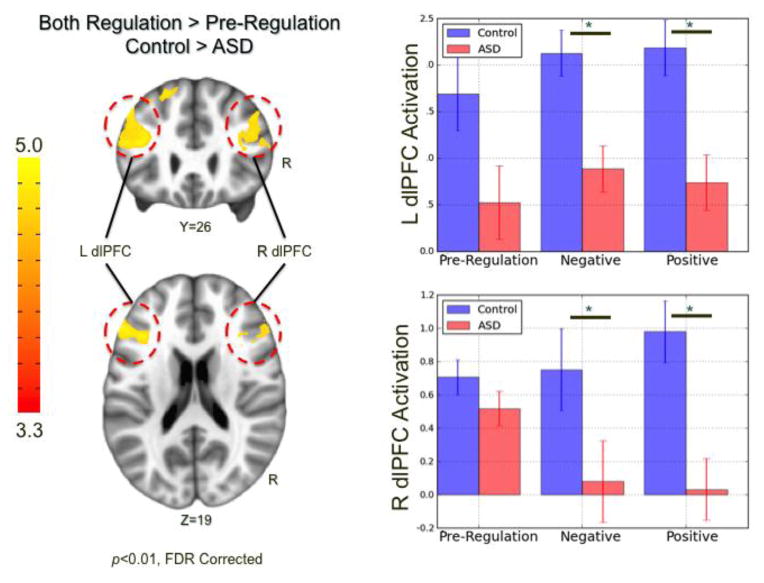
Group differences for the contrast of both regulation conditions (Enhance Negative and Enhance Positive) > Pre- Regulation
The left of Figure 5 and the bottom of Table 2 illustrate that for the contrast of Either Regulation > Pre-Instruction, the ASD group was characterized by relatively less increase in left and right dorsolateral prefrontal cortex activation (indicated as Middle Frontal Gyrus in Table 2) and left superior frontal gyrus than the control group. As can be seen from the bar graphs on the right of Figure 5, this effect was driven by moderately increased activation in both regulation conditions relative to the pre-instruction condition in the control group, whereas the ASD group showed decreased dorsolateral prefrontal cortex activation in three of four conditions. There were no clusters with relatively greater increases in activation in the ASD group relative to the control group for this contrast.
Figure 5.
For the contrast of Either Regulation > Pre- Regulation, the ASD group was characterized by relatively less increase in left and right dorsolateral prefrontal cortex (DLPFC) activation than the control group. Solid lines in the bar graph indicate significant between groups effects (*p<.05).
Exploratory analyses contrasting both regulation conditions with the Look condition did not yield any significant interactions with Group.
Although there were no group differences in the percentage of time both groups looked at faces during the fMRI task, fMRI models were analyzed including average looking time at faces during the regulations conditions as an additional regressor. These results were highly similar, and are presented as Supplementary Material.
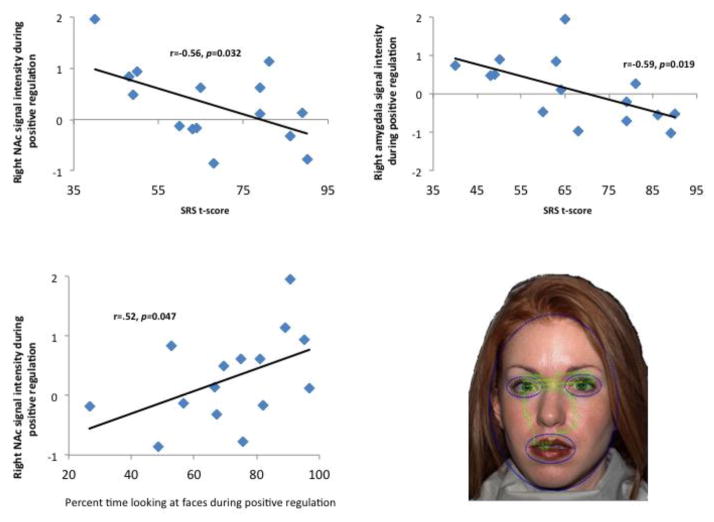
Associations between fMRI, Symptom, and Gaze Time
Relations between regional brain activation magnitudes and symptom severity within the ASD group as well as Gaze Time were evaluated via correlational analyses between average condition-specific signal intensities in clusters listed in Table 2 that differentiated groups, total scores on the SRS and RBS-R, and the percent of time participants spent looking at the face during each condition during scanning. Because of the exploratory nature of these analyses, results were not corrected for multiple comparisons. As can be seen in Figure 6, within the ASD group, there was a negative association between right NAc activation and SRS scores, reflecting that participants with more severe symptoms showed less modulation of this region during positive ER. Within the ASD group, there was also a negative association between right amygdala activation and SRS scores, reflecting that participants with more severe symptoms showed less modulation of this region during positive ER. Finally, within the ASD group there was a positive association between right NAc activation and the percentage of time participants spent looking at the face during positive ER, reflecting that participants who looked at faces more showed greater modulation of this region during positive ER. Within the control group, there was a trend towards an inverse relation between right amygdala activation and the percent of time looking at the face during negative ER (p<.10). No other correlations were significant.
Figure 6.
Top Left Relations between right nucleus accumbens (NAc) activation and SRS scores in the ASD group. Top Right: Relations between right amygdala activation and SRS scores in the ASD group. Bottom Left: Relations between right nucleus accumbens (NAc) activation and the percentage of time participants spend looking at the face during positive ER in the ASD group. Bottom Right: The scan paths from a single trial demarking point-of-regard (in green) as well as face, eyes, and mouth areas of interest (in blue).
Discussion
Although there is a wide range of initial concerns reported by parents of children with ASD, a high proportion report extremes of temperament and marked irritability during the first year of life, worries that may precede concerns related to core ASD symptoms (Gillberg et al., 1990; Hoshino et al., 1987). Additionally, prospective studies of high-risk infants indicate that behavioral reactivity, intense distress reactions, higher negative affect, lower positive affect, and difficulty controlling behavior differentiate high-risk from low-risk siblings and uniquely predict future ASD diagnoses (Brian et al., 2008; Garon et al., 2009; Zwaigenbaum et al., 2005). Moreover, tantrums and aggression are among the behaviors that most commonly lead parents to seek treatment (Arnold et al., 2003), and irritability and negative emotionality uniquely predict parental stress above other ASD symptoms (Davis & Carter, 2008; Owen et al., 2009). Finally, up to 60% of individuals with pervasive developmental disorder are characterized by moderate to severe irritability (Lecavalier, 2006). These temperamental profiles suggest that an ER framework may be useful for understanding the emergence of ASD early in life.
The purpose of this study was to evaluate the neural mechanisms of impaired ER in ASD using a task that evaluated cognitive reappraisal, a form of consciously deployed ER that, in nonclinical samples, effectively modulates subjective responses via a reinterpretation of the meaning of emotional challenges (Davidson, 2002; Gross, 2013; Ochsner et al., 2002; Ray et al., 2008). Cognitive reappraisal is mediated by modulating effects of dorsolateral, ventrolateral, and medial regions of prefrontal cortex (PFC) involved in cognitive control on ventral regions involved in arousal and motivation, including limbic and brainstem regions and medial and orbitofrontal prefrontal cortices (Critchley, 2005; Eippert et al., 2007; Urry et al., 2006). This functional neuranatomy suggests the relevance of investigating cognitive reappraisal in ASD, given that ASD is characterized both by impaired recruitment of brain regions that respond to socio-affective information (including the amygdala and the NAc) as well as by impaired recruitment of brain regions involved in cognitive control, including ventral and lateral PFC (see Dichter, 2012 for a review).
We used a training procedure to ensure that participants with ASD who were scanned understood how to implement the cognitive reappraisal strategies. We found that two out of seventeen participants with ASD who otherwise met inclusion criteria for the study were not able to implement the cognitive reappraisal strategies. Methodologically, this suggests that the majority of high functioning adults with ASD can learn cognitive reappraisal, highlighting the utility of cognitive reappraisal paradigms to study ASD. Substantively, we found no group differences in corollary measures meant to confirm the cognitive reappraisal manipulation in both groups. Specifically, there were no group differences in changes in pupil dilation during cognitive reappraisal, indicating that both groups were expending equivalent degrees of cognitive effort during cognitive reappraisal. Likewise, groups did not differ in subjective ratings of faces during cognitive reappraisal, further highlighting the ability of high functioning adults with ASD to implement cognitive reappraisal strategies. Finally, groups did not differ in time spent looking at faces or the eyes or mouth regions of faces, indicated that differences in neural activation were not caused by differences in looking behavior (cf. Dalton et al., 2005), confirmed by activation maps that included average looking time at the face region of stimuli as an additional regressor (see Supplementary Materials).
Functional neuroimaging results revealed group differences in predicted regions of interest. Specifically, consistent with hypotheses, the ASD group demonstrated decreased capacity to up-regulate NAc activity during instructions to think more positively about faces (this effect included portions of the left putamen as well). The NAc increases activity during cognitive control of goal directed behaviors and specifically during conscious increases in positive affect (Grace, Floresco, Goto, & Lodge, 2007). The decreased capacity to increase activity in this region, a central hub of the brain’s dopaminergic mesolimbic reward system (Berridge, Robinson, & Aldridge, 2009), may contribute to the decreases motivational salience of social information for individuals with ASD (Chevallier, Kohls, Troiani, Brodkin, & Schultz, 2012) and also indicates specific deficits in consciously changing the activity of a brain region that codes for the positive affective impact of social stimuli. Additionally, ASD symptom severity, indexed by SRS scores, predicted the magnitude of right NAc activity during positive cognitive reappraisal in the ASD group, suggesting that the capacity to up-regulate neural responses to social stimuli may impact the expression of ASD symptom severity.
Also consistent with hypotheses, the ASD group demonstrated decreased capacity to down-regulate amygdala activity during instructions to think negatively about faces. There is a rich literature addressing the role of the amygdala in suppression of negative emotional responses (Kim & Hamann, 2007; Lévesque et al., 2003; Ochsner et al., 2002), and the diminished capacity to decrease amygdala responses in social contexts may play a causal mechanistic role in the expression of a range of behavioral problems associated with negative affect that are commonly seen in ASD, including tantrums, aggression, self-injury, and irritability (Lecavalier, 2006). This finding is consistent with the recent results of Pitskel and colleagues (2014) who reported that children and adolescents with ASD were characterized by relatively decreased modulation of amygdala activation when consciously decreasing affective responses to pictures eliciting disgust. (Danial & Wood, 2013; Sukhodolsky, Bloch, Panza, & Reichow, 2013). That study also found group differences in insula activation, perhaps due to the use of more emotionally evocative disgust pictures rather than neutral faces. Pitskel and colleagues (2014) also reported group equivalence on subjective ratings during cognitive reappraisal despite differences in functional brain activity, and noted that this pattern of findings in consistent with clinical reports of effective cognitive behavioral therapy for ASD. We also found that ASD symptom severity, indicated by SRS scores, predicted the magnitude right amygdala activity during negative cognitive reappraisal in the ASD group. Combined with the significant relation between SRS scores and NAc activity during positive reappraisal, these findings suggest that the capacity to both up-regulate and down-regulate positive and negative emotional responses to faces are relevant to the expression of ASD symptom severity.
Finally, we found that during both cognitive reappraisal conditions, the ASD group was characterized by blunted activation, relative to the pre-regulation baseline, in bilateral dorsolateral prefrontal cortex. Dorsal and lateral aspects of the prefrontal cortex are critically involved in cognitive control of goal-directed processes (Duncan & Owen, 2000), and a large literature has investigated atypical recruitment of dorsolateral prefrontal cortex in ASD during tasks that require cognitive control, including tasks that require interference inhibition (Dichter & Belger, 2007; Gomot, Belmonte, Bullmore, Bernard, & Baron-Cohen, 2008; Solomon et al., 2009) and response monitoring (Thakkar et al., 2008). The present study extends this line of research to indicate that ASD is also characterized by decreased dorsolateral prefrontal cortex activation during the cognitive control of emotional responses.
Despite evidence of differences in neural activation during cognitive reappraisal, it is noteworthy that participants with ASD reported that cognitive reappraisal altered their affective responses to images, though the demand characteristics of the ratings procedure may have influenced affective ratings data. It is thus possible that the observed neural deficits did not completely interfere with cognitive reappraisal capacity in the laboratory setting, though correlations between neural responses and SRS scores suggest that the observed neural deficits may have impacted ASD symptom severity in this sample. We also highlight the general disconnect between subjective affective responses and pupilometry results on the one hand, which essentially reflected no differences in the ASD group, and group differences during cognitive reappraisal. This pattern suggests that individuals with ASD may achieve effective ER via alternative functional brain mechanisms. Alternatively, it is possible that more emotionally evocative social stimuli may have yielded group differences in self-reports and pupilometry as well.
Interpretive cautions include the fact that this study involved the presentation of visual stimuli accompanied by brief auditory instructional prompts. ASD is characterized by deficits in sensory integration (Iarocci & McDonald, 2006), and processing auditory and visual information simultaneously has potentially complex effects on neural activation (Anderson, Ferguson, Lopez-Larson, & Yurgelun-Todd, 2010). Although we highlight the ubiquity of variations of the current paradigm in the cognitive reappraisal literature (Bernat, Patrick, Benning, & Tellegen, 2006; Heller et al., 2009; Johnstone et al., 2007), the potential effects of multisensory processing on our results are unknown. We also note that collecting emotion ratings outside the scanner may have resulted in emotion ratings that may not fully reflect emotions experienced in the scanner. Furthermore, we also acknowledge that given the fact that task stimuli were neutral, instructions to “think positive” may have included not only increases in positive emotions but also decreases in negative emotions (similarly, instructions to “think negative” may have included not only increases in negative emotions but also decreases in positive emotions). Future studies using positive or negative stimuli will be needed to more conclusively link “think positive” findings to attempts to increase positive emotions only and “think negative” finding to attempts to decrease negative emotions only.
Additionally, there are individual differences in the ability to implement cognitive reappraisal strategies even amongst participants with adequate comprehension of cognitive reappraisal strategies, and future studies should assess relations between neural indices of cognitive reappraisal in ASD and dimensions known to moderate cognitive reappraisal effectiveness, including irritability, anxiousness, and depressive symptoms (Aman, Singh, Stewart, & C.J., 1985; Esbensen, Rojahn, Aman, & Ruedrich, 2003). ASD is also frequently comorbid with other Axis I disorders, including anxiety disorders (van Steensel, Bogels, & Perrin, 2011) and depression (Gotham, Unruh, & Lord, 2014), both of which themselves are characterized by impaired ER (Jazaieri et al., 2013). Future studies will be needed to tease apart the contributing influence of anxiety and depression, measured both as categorical disorders and as dimensional symptom states, on ER in ASD. Finally, ER includes both automatic and volitional forms of emotional control, and future research should address the capacity of individuals with ASD to exhibit automatic forms of allostatic emotional control. In summary, the present study is the first report of the neural mechanisms of positive and negative cognitive reappraisal of social information in ASD, and highlights the utility of investigating ER as an important construct relevant to the expression of core and associated features of ASD.
Supplementary Material
Acknowledgments
We thank the clinicians at Chapel Hill Division TEACCH for consultation on the cognitive reappraisal training instructions. Portions of these findings were presented at the 2014 Society for Biological Psychiatry in New York City. We thank BIAC MRI technologists Susan Music, Natalie Goutkin, and Luke Poole for assistance with data acquisition, and BIAC Director Allen Song for assistance with various aspects of this project. This research was supported by MH081285, MH085254, MH073402, HD079124, HD40127, H325D070011, and a UNC-CH Graduate School Dissertation Completion Fellowship (CRD). Assistance with participant recruitment was provided by the Clinical Translational Core of the Carolina Institute for Developmental Disabilities (HD079124).
References
- Aman MG, Singh NN, Stewart AW, CJF The Aberrant Behavior Checklist: A behavior rating scale for the assessment of treatment effects. Am J Ment Defic. 1985;89:485–491. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-V. 4. Washington, DC: 2013. [Google Scholar]
- Anderson JS, Ferguson MA, Lopez-Larson M, Yurgelun-Todd D. Topographic maps of multisensory attention. Proc Natl Acad Sci U S A. 2010;107(46):20110–20114. doi: 10.1073/pnas.1011616107. 1011616107 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold LE, Vitiello B, McDougle C, Scahill L, Shah B, Gonzalez NM, Tierney E. Parent-defined target symptoms respond to risperidone in RUPP autism study: customer approach to clinical trials. J Am Acad Child Adolesc Psychiatry. 2003;42(12):1443–1450. doi: 10.1097/00004583-200312000-00011. [DOI] [PubMed] [Google Scholar]
- Avants BB, Tustison NJ, Song G, Cook PA, Klein A, Gee JC. A reproducible evaluation of ANTs similarity metric performance in brain image registration. Neuroimage. 2011;54(3):2033–2044. doi: 10.1016/j.neuroimage.2010.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachevalier J, Loveland KA. The orbitofrontal–amygdala circuit and self-regulation of social–emotional behavior in autism. Neuroscience and Biobehavioral Reviews. 2006;30:97–117. doi: 10.1016/j.neubiorev.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S, Wheelwright S, Skinner R, Martin J, Clubley E. The autism-spectrum quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J Autism Dev Disord. 2001;31(1):5–17. doi: 10.1023/a:1005653411471. [DOI] [PubMed] [Google Scholar]
- Bauminger N, Solomon M, Rogers SJ. Externalizing and internalizing behaviors in ASD. Autism Research. 2010;3(3):101–112. doi: 10.1002/aur.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernat E, Patrick CJ, Benning SD, Tellegen A. Effects of picture content and intensity on affective physiological response. Psychophysiology. 2006;43(1):93–103. doi: 10.1111/j.1469-8986.2006.00380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge KC, Robinson TE, Aldridge JW. Dissecting components of reward: ‘liking’, ‘wanting’, and learning. Curr Opin Pharmacol. 2009;9(1):65–73. doi: 10.1016/j.coph.2008.12.014. S1471-4892(08)00212-9 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodfish JW, Symons FW, Lewis MH. The Repetitive Behavior Scale-Revised. Western Carolina Center Research Reports 1999 [Google Scholar]
- Bradley MM, Lang PJ. Measuring emotion: the Self-Assessment Manikin and the Semantic Differential. J Behav Ther Exp Psychiatry. 1994;25(1):49–59. doi: 10.1016/0005-7916(94)90063-9. [DOI] [PubMed] [Google Scholar]
- Brian J, Bryson SE, Garon N, Roberts W, Smith IM, Szatmari P, Zwaigenbaum L. Clinical assessment of autism in high-risk 18-month-olds. Autism. 2008;12(5):433–456. doi: 10.1177/1362361308094500. 12/5/433 [pii] [DOI] [PubMed] [Google Scholar]
- Buhle JT, Silvers JA, Wager TD, Lopez R, Onyemekwu C, Kober H, Ochsner KN. Cognitive Reappraisal of Emotion: A Meta-Analysis of Human Neuroimaging Studies. Cereb Cortex. 2013 doi: 10.1093/cercor/bht154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler EA, Wilhelm FH, Gross JJ. Respiratory sinus arrhythmia, emotion, and emotion regulation during social interaction. Psychophysiology. 2006;43(6):612–622. doi: 10.1111/j.1469-8986.2006.00467.x. [DOI] [PubMed] [Google Scholar]
- Cabestrero R, Crespo A, Quiros P. Pupillary dilation as an index of task demands. Percept Mot Skills. 2009;109(3):664–678. doi: 10.2466/pms.109.3.664-678. [DOI] [PubMed] [Google Scholar]
- Chambers R, Gullone E, Allen NB. Mindful emotion regulation: An integrative review. Clin Psychol Rev. 2009;29(6):560–572. doi: 10.1016/j.cpr.2009.06.005. S0272-7358(09)00086-5 [pii] [DOI] [PubMed] [Google Scholar]
- Chevallier C, Kohls G, Troiani V, Brodkin ES, Schultz RT. The social motivation theory of autism. Trends Cogn Sci. 2012;16(4):231–239. doi: 10.1016/j.tics.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, Davis SA, Todd RD, Schindler MK, Gross MM, Brophy SL, Reich W. Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J Autism Dev Disord. 2003;33(4):427–433. doi: 10.1023/a:1025014929212. [DOI] [PubMed] [Google Scholar]
- Critchley HD. Neural mechanisms of autonomic, affective, and cognitive integration. J Comp Neurol. 2005;493(1):154–166. doi: 10.1002/cne.20749. [DOI] [PubMed] [Google Scholar]
- Dalton KM, Nacewicz BM, Johnstone T, Schaefer HS, Gernsbacher MA, Goldsmith HH, Davidson RJ. Gaze fixation and the neural circuitry of face processing in autism. Nat Neurosci. 2005;8(4):519–526. doi: 10.1038/nn1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danial JT, Wood JJ. Cognitive behavioral therapy for children with autism: review and considerations for future research. J Dev Behav Pediatr. 2013;34(9):702–715. doi: 10.1097/DBP.0b013e31829f676c. [DOI] [PubMed] [Google Scholar]
- Davidson RJ. Anxiety and affective style: role of prefrontal cortex and amygdala. Biol Psychiatry. 2002;51(1):68–80. doi: 10.1016/s0006-3223(01)01328-2. [DOI] [PubMed] [Google Scholar]
- Davis NO, Carter AS. Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: associations with child characteristics. J Autism Dev Disord. 2008;38(7):1278–1291. doi: 10.1007/s10803-007-0512-z. [DOI] [PubMed] [Google Scholar]
- Dennis TA. Neurophysiological markers for child emotion regulation from the perspective of emotion-cognition integration: current directions and future challenges. Dev Neuropsychol. 2010;35(2):212–230. doi: 10.1080/87565640903526579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond LM, Aspinwall LG. Emotion regulation across the life span:An integrative perspective emphasizing self-regulation, positive affect, and dyadic processes. Motivation and Emotion. 2003;27(2):125–156. [Google Scholar]
- Dichter GS. Functional magnetic resonance imaging of autism spectrum disorders. Dialogues Clin Neurosci. 2012;14(3):319–351. doi: 10.31887/DCNS.2012.14.3/gdichter. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dichter GS, Belger A. Social stimuli interfere with cognitive control in autism. Neuroimage. 2007;35(3):1219–1230. doi: 10.1016/j.neuroimage.2006.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan RJ. Emotion, cognition, and behavior. Science. 2002;298(5596):1191–1194. doi: 10.1126/science.1076358. 298/5596/1191 [pii] [DOI] [PubMed] [Google Scholar]
- Duncan J, Owen AM. Common regions of the human frontal lobe recruited by diverse cognitive demands. Trends Neurosci. 2000;23(10):475–483. doi: 10.1016/s0166-2236(00)01633-7. [DOI] [PubMed] [Google Scholar]
- Eippert F, Veit R, Weiskopf N, Erb M, Birbaumer N, Anders S. Regulation of emotional responses elicited by threat-related stimuli. Hum Brain Mapp. 2007;28(5):409–423. doi: 10.1002/hbm.20291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Spinrad TL. Emotion-related regulation: sharpening the definition. Child Dev. 2004;75(2):334–339. doi: 10.1111/j.1467-8624.2004.00674.x. CDEV674 [pii] [DOI] [PubMed] [Google Scholar]
- Esbensen AJ, Rojahn J, Aman MG, Ruedrich S. Reliability and validity of an assessment instrument for anxiety, depression, and mood among individuals with mental retardation. J Autism Dev Disord. 2003;33(6):617–629. doi: 10.1023/b:jadd.0000005999.27178.55. [DOI] [PubMed] [Google Scholar]
- Fischl B, van der Kouwe A, Destrieux C, Halgren E, Segonne F, Salat DH, Dale AM. Automatically parcellating the human cerebral cortex. Cereb Cortex. 2004;14(1):11–22. doi: 10.1093/cercor/bhg087. [DOI] [PubMed] [Google Scholar]
- Fitzsimmons G, Bargh JA. Automatic self-regulation. In: Baumeister R, Vohs K, editors. Handbook of self-regulation: Research, theory, and applications. New York: The Guilford Press; 2004. pp. 151–170. [Google Scholar]
- Frank DW, Dewitt M, Hudgens-Haney M, Schaeffer DJ, Ball BH, Schwarz NF, Sabatinelli D. Emotion regulation: Quantitative meta-analysis of functional activation and deactivation. Neurosci Biobehav Rev. 2014;45C:202–211. doi: 10.1016/j.neubiorev.2014.06.010. [DOI] [PubMed] [Google Scholar]
- Garon N, Bryson SE, Zwaigenbaum L, Smith IM, Brian J, Roberts W, Szatmari P. Temperament and its relationship to autistic symptoms in a high-risk infant sib cohort. J Abnorm Child Psychol. 2009;37(1):59–78. doi: 10.1007/s10802-008-9258-0. [DOI] [PubMed] [Google Scholar]
- Gillberg C, Ehlers S, Schaumann H, Jakobsson G, Dahlgren SO, Lindblom R, Blidner E. Autism under age 3 years: a clinical study of 28 cases referred for autistic symptoms in infancy. J Child Psychol Psychiatry. 1990;31(6):921–934. doi: 10.1111/j.1469-7610.1990.tb00834.x. [DOI] [PubMed] [Google Scholar]
- Gomot M, Belmonte MK, Bullmore ET, Bernard FA, Baron-Cohen S. Brain hyper-reactivity to auditory novel targets in children with high-functioning autism. Brain. 2008;131(Pt 9):2479–2488. doi: 10.1093/brain/awn172. [DOI] [PubMed] [Google Scholar]
- Gorgolewski K, Burns CD, Madison C, Clark D, Halchenko YO, Waskom ML, Ghosh SS. Nipype: a flexible, lightweight and extensible neuroimaging data processing framework in python. Front Neuroinform. 2011;5:13. doi: 10.3389/fninf.2011.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Unruh K, Lord C. Depression and its measurement in verbal adolescents and adults with autism spectrum disorder. Autism. 2014 doi: 10.1177/1362361314536625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace AA, Floresco SB, Goto Y, Lodge DJ. Regulation of firing of dopaminergic neurons and control of goal-directed behaviors. Trends Neurosci. 2007;30(5):220–227. doi: 10.1016/j.tins.2007.03.003. [DOI] [PubMed] [Google Scholar]
- Gray JR, Braver TS, Raichle ME. Integration of emotion and cognition in the lateral prefrontal cortex. Proc Natl Acad Sci U S A, 99. 2002;(6):4115–4120. doi: 10.1073/pnas.062381899. 99/6/4115 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greve DN, Fischl B. Accurate and robust brain image alignment using boundary-based registration. Neuroimage. 2009;48(1):63–72. doi: 10.1016/j.neuroimage.2009.06.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ. Emotion regulation: taking stock and moving forward. Emotion. 2013;13(3):359–365. doi: 10.1037/a0032135. [DOI] [PubMed] [Google Scholar]
- Heller AS, Johnstone T, Shackman AJ, Light SN, Peterson MJ, Kolden GG, Davidson RJ. Reduced capacity to sustain positive emotion in major depression reflects diminished maintenance of fronto-striatal brain activation. Proc Natl Acad Sci U S A. 2009;106(52):22445–22450. doi: 10.1073/pnas.0910651106. 0910651106 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoshino Y, Kaneko M, Yashima Y, Kumashiro H, Volkmar FR, Cohen DJ. Clinical features of autistic children with setback course in their infancy. Jpn J Psychiatry Neurol. 1987;41(2):237–245. doi: 10.1111/j.1440-1819.1987.tb00407.x. [DOI] [PubMed] [Google Scholar]
- Iarocci G, McDonald J. Sensory integration and the perceptual experience of persons with autism. J Autism Dev Disord. 2006;36(1):77–90. doi: 10.1007/s10803-005-0044-3. [DOI] [PubMed] [Google Scholar]
- Jazaieri H, Urry HL, Gross JJ. Affective Disturbance and Psychopathology: An Emotion Regulation Perspective. Journal of Experimental Psychopathology. 2013;5(6):584–599. [Google Scholar]
- Johnstone T, van Reekum CM, Urry HL, Kalin NH, Davidson RJ. Failure to regulate: counterproductive recruitment of top-down prefrontal-subcortical circuitry in major depression. Journal of Neuroscience. 2007;27(33):8877–8884. doi: 10.1523/JNEUROSCI.2063-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalisch R. The functional neuroanatomy of reappraisal: time matters. Neurosci Biobehav Rev. 2009;33(8):1215–1226. doi: 10.1016/j.neubiorev.2009.06.003. S0149-7634(09)00083-9 [pii] [DOI] [PubMed] [Google Scholar]
- Keltner D, Gross JJ. Functional accounts of emotions. Cognition & Emotion. 1999;13(5):467–480. [Google Scholar]
- Keshavan MS, Vinogradov S, Rumsey J, Sherrill J, Wagner A. Cognitive training in mental disorders: update and future directions. Am J Psychiatry. 2014;171(5):510–522. doi: 10.1176/appi.ajp.2013.13081075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH, Hamann S. Neural correlates of positive and negative emotion regulation. Journal of Cognitive Neuroscience. 2007;19(5):776–798. doi: 10.1162/jocn.2007.19.5.776. [DOI] [PubMed] [Google Scholar]
- Koenigsberg HW, Harvey PD, Mitropoulou V, Schmeidler J, New AS, Goodman M, Siever LJ. Characterizing affective instability in borderline personality disorder. Am J Psychiatry. 2002;159(5):784–788. doi: 10.1176/appi.ajp.159.5.784. [DOI] [PubMed] [Google Scholar]
- Lecavalier L. Behavioral and emotional problems in young people with pervasive developmental disorders: relative prevalence, effects of subject characteristics, and empirical classification. J Autism Dev Disord. 2006;36(8):1101–1114. doi: 10.1007/s10803-006-0147-5. [DOI] [PubMed] [Google Scholar]
- Lévesque J, Eugene F, Joanette Y, Paquette V, Mensour B, Beaudoin G, Beauregard M. Neural circuitry underlying voluntary suppression of sadness. Biological Psychiatry. 2003;53(6):502–510. doi: 10.1016/s0006-3223(02)01817-6. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, Rutter M. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism & Developmental Disorders. 2000;30(3):205–223. [PubMed] [Google Scholar]
- Lugnegard T, Hallerback MU, Gillberg C. Psychiatric comorbidity in young adults with a clinical diagnosis of Asperger syndrome. Res Dev Disabil. 2011;32(5):1910–1917. doi: 10.1016/j.ridd.2011.03.025. [DOI] [PubMed] [Google Scholar]
- Luu P, Tucker DM. Self-regulation by the medial frontal cortex: Limbic representation of motive set-points. In: Beauregard M, editor. Consciousness, emotional self-regulation and the brain. Amsterdam, Netherlands: John Benjamins Publishing Company; 2004. pp. 123–161. [Google Scholar]
- Mazefsky CA, Herrington J, Siegel M, Scarpa A, Maddox BB, Scahill L, White SW. The role of emotion regulation in autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2013;52(7):679–688. doi: 10.1016/j.jaac.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Oswald DP, Day TN, Eack SM, Minshew NJ, Lainhart JE. ASD, a psychiatric disorder, or both? Psychiatric diagnoses in adolescents with high-functioning ASD. J Clin Child Adolesc Psychol. 2012;41(4):516–523. doi: 10.1080/15374416.2012.686102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Steerneman P, Merckelbach H, Holdrinet I, Meesters C. Comorbid anxiety symptoms in children with pervasive developmental disorders. J Anxiety Disord. 1998;12(4):387–393. doi: 10.1016/s0887-6185(98)00022-x. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, Bunge SA, Gross JJ, Gabrieli JD. Rethinking feelings: an FMRI study of the cognitive regulation of emotion. J Cogn Neurosci. 2002;14(8):1215–1229. doi: 10.1162/089892902760807212. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, Ray RD, Cooper JC, Robertson ER, Chopra S, Gabrieli JD, Gross JJ. For better or for worse: neural systems supporting the cognitive down- and up-regulation of negative emotion. Neuroimage. 2004;23(2):483–499. doi: 10.1016/j.neuroimage.2004.06.030. [DOI] [PubMed] [Google Scholar]
- Owen R, Sikich L, Marcus RN, Corey-Lisle P, Manos G, McQuade RD, Findling RL. Aripiprazole in the treatment of irritability in children and adolescents with autistic disorder. Pediatrics. 2009;124(6):1533–1540. doi: 10.1542/peds.2008-3782. [DOI] [PubMed] [Google Scholar]
- Parkinson B, Totterdell P. Classifying affect-regulation strategies. Cognition and Emotion. 1999;13:277–303. [Google Scholar]
- Pitskel NB, Bolling DZ, Kaiser MD, Pelphrey KA, Crowley MJ. Neural systems for cognitive reappraisal in children and adolescents with autism spectrum disorder. Dev Cogn Neurosci. 2014;10:117–128. doi: 10.1016/j.dcn.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray R, Wilhelm FH, Gross JJ. All in the mind’s eye: Anger rumination and reappraisal. Journal of Personality and Social Psychology. 2008;94:133–145. doi: 10.1037/0022-3514.94.1.133. [DOI] [PubMed] [Google Scholar]
- Rieffe C, Oosterveld P, Meerum Terwogt M, Mootz S, Van Leeuwen E, Stockmann L. Emotion regulation and internalizing symptoms in children with autism spectrum disorders. [1362361310366571 [pii] 10.1177/1362361310366571];Autism. 2011 doi: 10.1177/1362361310366571. [DOI] [PubMed] [Google Scholar]
- Rottenberg J, Gross JJ. Emotion and emotion regulation: A map for psychotherapy researchers. Clinical Psychology: Science and Practice. 2007;14:323–328. [Google Scholar]
- Samson AC, Hardan AY, Podell RW, Phillips JM, Gross JJ. Emotion Regulation in Children and Adolescents With Autism Spectrum Disorder. Autism Res. 2014 doi: 10.1002/aur.1387. [DOI] [PubMed] [Google Scholar]
- Samson AC, Phillips JM, Parker KJ, Shah S, Gross JJ, Hardan AY. Emotion dysregulation and the core features of autism spectrum disorder. J Autism Dev Disord. 2014;44(7):1766–1772. doi: 10.1007/s10803-013-2022-5. [DOI] [PubMed] [Google Scholar]
- Schaefer SM, Jackson DC, Davidson RJ, Aguirre GK, Kimberg DY, Thompson-Schill SL. Modulation of amygdalar activity by the conscious regulation of negative emotion. J Cogn Neurosci. 2002;14(6):913–921. doi: 10.1162/089892902760191135. [DOI] [PubMed] [Google Scholar]
- Schore AN. Affect dysregulation and disorders of the self/affect regulation and the repair of the self. New York: W. W. Norton & Company, Inc; 2003. [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Smith SM, Jenkinson M, Woolrich MW, Beckmann CF, Behrens TEJ, Johansen-Berg H, Matthews PM. Advances in functional and structural MR image analysis and implementation as FSL. NeuroImage. 2004;23(Suppl 1):S208–219. doi: 10.1016/j.neuroimage.2004.07.051. [DOI] [PubMed] [Google Scholar]
- Solomon M, Ozonoff SJ, Ursu S, Ravizza S, Cummings N, Ly S, Carter CS. The neural substrates of cognitive control deficits in autism spectrum disorders. Neuropsychologia. 2009;47(12):2515–2526. doi: 10.1016/j.neuropsychologia.2009.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukhodolsky DG, Bloch MH, Panza KE, Reichow B. Cognitive-behavioral therapy for anxiety in children with high-functioning autism: a meta-analysis. Pediatrics. 2013;132(5):e1341–1350. doi: 10.1542/peds.2013-1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakkar KN, Polli FE, Joseph RM, Tuch DS, Hadjikhani N, Barton JJ, Manoach DS. Response monitoring, repetitive behaviour and anterior cingulate abnormalities in autism spectrum disorders (ASD) Brain. 2008;131(Pt 9):2464–2478. doi: 10.1093/brain/awn099. awn099 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RA. Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev. 1994;59(2–3):25–52. [PubMed] [Google Scholar]
- Tottenham N, Tanaka JW, Leon AC, McCarry T, Nurse M, Hare TA, Nelson C. The NimStim set of facial expressions: judgments from untrained research participants. Psychiatry Res. 2009;168(3):242–249. doi: 10.1016/j.psychres.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urry HL. Seeing, thinking, and feeling: emotion-regulating effects of gaze-directed cognitive reappraisal. Emotion. 2010;10(1):125–135. doi: 10.1037/a0017434. 2010-01983-005 [pii] [DOI] [PubMed] [Google Scholar]
- Urry HL, van Reekum CM, Johnstone T, Kalin NH, Thurow ME, Schaefer HS, Davidson RJ. Amygdala and ventromedial prefrontal cortex are inversely coupled during regulation of negative affect and predict the diurnal pattern of cortisol secretion among older adults. J Neurosci. 2006;26(16):4415–4425. doi: 10.1523/JNEUROSCI.3215-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Reekum CM, Johnstone T, Urry HL, Thurow ME, Schaefer HS, Alexander AL, Davidson RJ. Gaze fixations predict brain activation during the voluntary regulation of picture-induced negative affect. Neuroimage. 2007;36(3):1041–1055. doi: 10.1016/j.neuroimage.2007.03.052. [DOI] [PubMed] [Google Scholar]
- van Steensel FJA, Bogels SM, Perrin S. Anxiety Disorders in Children and Adolescents with Autistic Spectrum Disorders: A Meta-Analysis. Clinical Child and Family Psychology Review. 2011;14(3):302–317. doi: 10.1007/s10567-011-0097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss JA, Thomson K, Chan L. A Systematic Literature Review of Emotion Regulation Measurement in Individuals With Autism Spectrum Disorder. Autism Res. 2014 doi: 10.1002/aur.1426. [DOI] [PubMed] [Google Scholar]
- Weschler D. Weschler Abbreviated Scale of Intelligence (WASI) San Antonio, TX: Harcourt Assessment; 1999. [Google Scholar]
- White SW, Mazefsky CA, Dichter GS, Chiu PH, Richey JA, Ollendick TH. Social-cognitive, physiological, and neural mechanisms underlying emotion regulation impairments: understanding anxiety in autism spectrum disorder. Int J Dev Neurosci. 2014 doi: 10.1016/j.ijdevneu.2014.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clin Psychol Rev. 2009;29(3):216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwaigenbaum L, Bryson S, Rogers T, Roberts W, Brian J, Szatmari P. Behavioral manifestations of autism in the first year of life. Int J Dev Neurosci. 2005;23(2–3):143–152. doi: 10.1016/j.ijdevneu.2004.05.001. S0736574804000553 [pii] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.