Abstract
BACKGROUND AND AIM:
The prevalence of restless legs syndrome (RLS) in the general population ranges from 5 to 15%; however, locally, such data are scarce. The aim of this study was to estimate the prevalence of RLS in the middle-aged Saudi population.
METHODS:
This was a cross-sectional study that was conducted from February 2013 to June 2013 in Jeddah, Saudi Arabia. The target study population was Saudi school employees. Saudi employees aged 30-60 years were randomly selected and interviewed individually. Trained interviewers completed the Wisconsin Sleep Questionnaire, questions about demographics, the Epworth Sleepiness Scale to measure daytime sleepiness, and questions regarding symptoms of RLS based on the criteria defined by the International Restless Legs Syndrome Study Group (IRLSSG).
RESULTS:
This survey revealed that 8.4% (95% confidence interval (CI): (7.35-9.45)) of the 2,682 participants (62.5% of them were males) had RLS. There was no age effect on the prevalence of RLS. RLS was found to be significantly associated with other sleep disorders, including excessive daytime sleepiness and habitual snoring. A univariate analysis revealed significant correlation of many factors with the RLS, including gender, consanguinity, snoring, diabetes, hypertension, asthma, chronic bronchitis, and smoking. However, when a multivariate logistic regression analysis performed, RLS continued to be associated with male gender, diabetes, asthma, and habitual snoring only.
CONCLUSION:
The prevalence of RLS is 8.4%, which is within the range reported by Western studies. However, unlike findings of most studies, RLS significantly affects males more than females. In addition, snoring, asthma, and consanguinity are potential new risk factors for RLS.
Keywords: Prevalence, restless legs syndrome, risk factors
Restless legs syndrome (RLS), also known as Willis–Ekbom disease, is a common sleep-related, sensorimotor and neurological clinical syndrome that primarily affects the legs.[1] When severe, it can also affect the arms and other parts of the body. RLS is characterized by sore sensations in the legs that are accompanied by an urge to move them, typically in the evening. It is worse at rest and temporarily relieved by activity.[1,2] RLS is idiopathic in nature in most cases, but can be secondary to conditions such as diabetes mellitus (DM), renal failure, and iron deficiency anemia.
Although Dr Karl Ekbom first described RLS in 1945, clinicians and researchers ignored the condition until the late 1980s.[3] The International Restless Legs Syndrome Study Group (IRLSSG) was then formed to create diagnostic criteria.[2] The IRLSSG released guidelines to aid in the clinical diagnosis and determination of RLS severity, in addition to augmenting clinical and epidemiological research on RLS.[4,5]
The restlessness experienced by patients with RLS may lead to other sleep disorders, such as insomnia and excessive daytime sleepiness.[6] In its severe forms, it becomes a chronic and devastating disorder requiring long-term treatment. Although there is no cure for this syndrome, the aim of clinical management is to treat the possible causes and consider different drugs for symptomatic relief. A variety of drugs are available to address symptoms, including dopaminergic agents, opioids, anticonvulsants, and sedative hypnotics.
The prevalence of RLS in the general population ranges from 5 to 15%.[7] Locally, however, prevalence data are scarce. Nevertheless, among primary healthcare patients, the prevalence was reported to be as high as 5.2%, with those affected most often being between 45 and 60 years of age.[8] The aim of this study was to estimate the prevalence of RLS in the middle-aged Saudi population in a community-based survey.
Methods
This was a cross-sectional study that was conducted from February to June 2013 in Jeddah, Saudi Arabia. This study was part of a large, ongoing survey on the prevalence of obstructive sleep apnea among middle-aged people in the western region of Saudi Arabia. The target study population was Saudi school employees because Saudi schools are the best source of national employees with an equal distribution of genders. Stratified random sampling of Saudi school employees was performed in four regions of Jeddah City: South, east, northwest, and central. A list of schools in Jeddah was obtained from the Ministry of Education, and random sampling of schools from each area was then performed. Approval was obtained from the ethical committee of King Abdulaziz University Hospital, Jeddah.
Research sessions for conducting interviews, general health checkups, and anthropometric measurements were organized in each selected school. Saudi employees aged 30-60 years from the selected schools who agreed to participate in the study were recruited. Trained interviewers were assigned to the school research sessions to:
Obtain written informed consent from participants.
Interview candidates individually, including completion of a modified Wisconsin Sleep Questionnaire[9] which included questions on demographics, an assessment of daytime sleepiness using the Epworth Sleepiness Scale,[10] and recording of RLS symptoms based on the criteria defined by the International Restless Legs Syndrome Study Group (IRLSSG).[2] The diagnostic criteria for RLS include the following: An urge to move the legs that is usually associated with uncomfortable sensations in the legs, worsening of these symptoms during rest, at least temporary relief brought on by activity, and worsening of symptoms in the evening.[2,5]
Regarding questionnaires used, the forward backward translation was employed in our study. The focus was on cross-cultural rather than on linguistic/literal equivalence. Discrepancies were discussed with the presence of the principal investigator and within the bilingual expert panel, which composed of four members including the principal investigator. A health professional, familiar with terminology of the questionnaires used and with interview skills, performed forward translation to Arabic. The translator was knowledgeable of the English-speaking culture and her mother tongue was the Arabic language. An independent translator performed the back translation to English who had no knowledge of the questionnaire and had bilingual expertize in English and Arabic.
A pilot study was performed where 21 subjects were interviewed from a single school. Data from the pilot study was not included in the analysis. Pretesting of the questionnaire in the field during the pilot study was focused on items which are difficult and confusing. The study group discussed the conseption, interpretability and suggestions for improvement. Intra- and inter-observer reliability was performed after extensive training and workshops that took 1 month and held for the purpose of lowering the degree of unreliability between interviewers. In all the reliability tests performed, the reliability coefficient ranges from 0.85 to 0.90, which limited the variation in respondents' answers and ensured the uniformity of the interview process being carried out by several interviewers.[11,12]
Statistical methods
The statistical analysis was performed using Statistical Analysis of Social Sciences (SPSS) software. Data are presented as means and standard deviations for continuous variables and as percentages for categorical variables. Comparisons between groups were performed using Student's t-test for continuous variables and the Pearson chi-square test for discrete variables. Results were considered significant at a P - value of 0.05 using two-sided tests. Odds ratios (ORs) and 95% confidence intervals (CIs) were determined. Variables showing association with a P - value < 0.1 in the univariate analysis were included in the multivariate analysis as potential risk factors. Stepwise multiple logistic regression analyses were used to identify significant independent risk factors for RLS.
Results
The survey revealed that 8.4% (95% CI: (7.35-9.45)) of the 2,682 participants (62.5% of them were males) suffer from RLS. Hence, the prevalence of RLS in males is 10.89 (95% CI: (9.20-12.60)) and in females is 6.01 (95% CI: (4.76-7.26)). There was no effect of aging on the prevalence of RLS [Table 1]. Nevertheless, the prevalence of RLS in age group 30-39 is 9.17 (95% CI: (7.55-10.80), 40-49 is 7.54 (95% CI: (6.04-9.04)), and in 50-60 is 8.24 (95% CI: (4.94-11.54)).
Table 1.
Demographic data of the study population
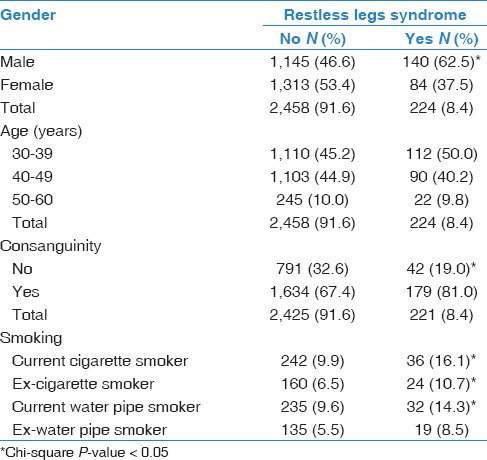
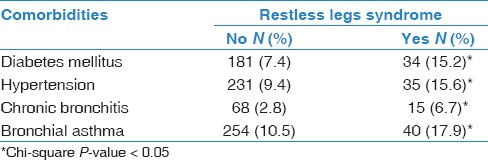
RLS was found to be significantly associated with smoking and consanguinity [Table 1]. Comorbidities (DM, hypertension, chronic bronchitis, and bronchial asthma) were all found to be significantly associated with RLS [Table 2].
Table 2.
Distribution of comorbidities based on the diagnosis of restless legs syndrome
RLS was also found to be significantly associated with other sleep disorders, including daytime sleepiness and habitual snoring [Tables 3 and 4]. No association was detected with any of the parameters of obesity [Table 5].
Table 3.
Snoring habits in subjects with and without restless legs syndrome
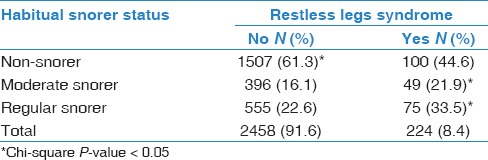
Table 4.
Daytime sleepiness in restless leg syndrome (RLS) subjects compared to RLS-free subjects
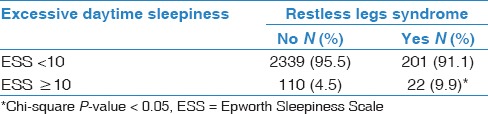
Table 5.
Parameters of obesity in RLS subjects compared to RLS-free subjects

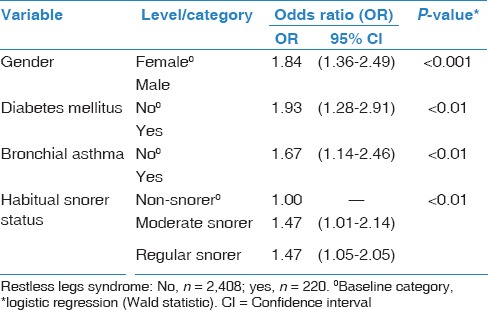
A bivariate analysis of RLS with selected risk factors revealed significant associations with gender, consanguinity, snoring, excessive day time sleepiness, DM, hypertension, asthma, chronic bronchitis, current and past smoking, current water pipe smoking, and a family history of sleep disorders [Table 6]. The multivariate analysis confirmed the association between RLS and being male, having DM, having asthma, and being a habitual snorer only [Table 7].
Table 6.
Univariate analysis of restless legs syndrome status and risk factors
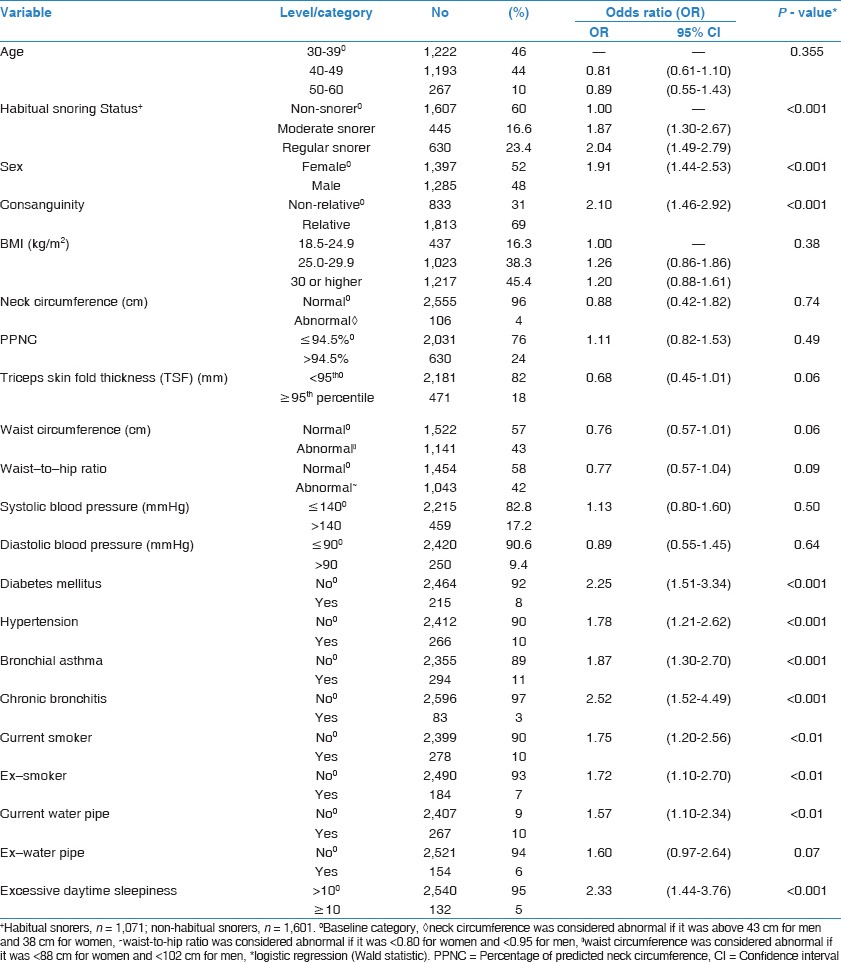
Table 7.
Multivariate analysis of restless legs syndrome status and risk factors
Discussion
This study revealed an RLS prevalence of 8.4% in the middle-aged Saudi population, with a male predominance and no association with aging. As expected, excessive daytime sleepiness was significantly higher among RLS subjects. To our knowledge, this is the first community-based study in Saudi Arabia to examine the prevalence of RLS using the four minimum diagnostic criteria as described by the IRLSSG.
The prevalence of RLS among the general population depends on many factors, including the criteria used to define the syndrome and the design of the study. Ohayon et al., in their review of the English literature regarding epidemiological studies on the prevalence of RLS worldwide, reported prevalence values ranging from 1.9 to 4.6% when using strict diagnostic criteria of RLS. However, when focusing on studies similar to our own, the prevalence of RLS in the general adult population ranged from 3.9 to 14.3%, as is seen in studies performed in Europe and North America.[7] These studies, like our study, were community-based and used the same four minimum diagnostic criteria described by the IRLSSG to diagnose RLS.[7] Therefore, the prevalence of RLS of 8.4% reported in our study is within the range observed in Western studies of similar design. In contrast, RLS seems to be less common in Asian populations, with a prevalence ranging from 1 to 4% in most studies.[7] An Indian community-based study that used diagnostic criteria similar to ours demonstrated an RLS prevalence of 2.1%.[13]
Although the prevalence reported in our study is in concordance with the prevalence values reported by European and North American studies, some of our findings were not consistent with those studies. Studies from North America and Europe demonstrated a linear trend of an increase in age with increasing RLS frequencies, an observation that was not found in our study and the studies from Asia. Furthermore, unlike most studies, our study showed that more males than females were affected by RLS. Most studies have reported the prevalence of RLS to be approximately twice as high in women as in men.[7] However, it is consistent with a Japanese study that reported a male predominance in individuals aged 40-49 years.[33] A previous study from Saudi Arabia demonstrated an overall prevalence of RLS that was approximately equal between males and females.[8] However, this survey did not have a community-based design since it was performed in primary care practices. It is tempting to attribute the male predominance in our study to the relatively higher prevalence of smoking, which is linked to RLS,[14] among males compared with females in Saudi Arabia.[15] However, this hypothesis no longer appeared valid when the multivariate analysis was applied. Another possible explanation is the higher prevalence of diabetes in male patients. However, although the prevalence of DM was higher in males than in females (10.4 vs 5.9%, respectively); it did not explain the higher prevalence of RLS in males. This is because the multivariate analysis with RLS as the outcome variable controlling for DM in the model still showed that males had significantly higher RLS than females, therefore this gender discrepancy should be investigated further [Table 7].
In the Middle East, only scarce data are available regarding the prevalence of RLS. In Turkey, a population-based survey was conducted using diagnostic criteria similar to that used in our study to determine the prevalence of RLS among people aged 40 years and above.[16] The prevalence of RLS was estimated to be 9.7%, which is in accordance with the prevalence of 8.4% reported in the present study. Similar to other studies but unlike ours, that study also revealed a female predominance among patients with RLS.[16] More recent studies from Turkey used more strict criteria to define RLS and, consequently, reported a low prevalence of 3.4%.[17,18] In Saudi Arabia, however, the only study addressing this issue was conducted in a primary healthcare services setting.[8] Direct questioning of 1,303 consecutive patients was performed.[8] Participants who responded positively to all four questions defined by the IRLSSG were diagnosed as having RLS. Based on these diagnostic criteria, the prevalence of RLS among Saudis was 5.2%.[8] The prevalence was highest among participants aged 45-60 years. The overall prevalence was approximately equal between males and females.[8] Nevertheless, we believe that our study may be more representative of the prevalence of RLS in the Saudi population, as it was a community-based survey conducted in large study population.
RLS can be idiopathic in nature but may also occur secondary to diseases such as DM, renal failure, iron deficiency anemia, Parkinson's disease, and multiple sclerosis. It may also occur as a side effect of some medications and can accompany or be aggravated by pregnancy. In our survey, no investigation or clinical analysis was performed. However, as expected, RLS was found to be significantly associated with DM. In addition, asthma was unexpectedly found to be associated with RLS. Therefore, our study suggests that RLS in Saudis may be associated with different conditions than those associated with RLS in other populations. However, it is not clear whether this association between asthma and RLS in the Saudi population is related to medications such as antihistamines.
Although most studies have not been able to determine a causality relationship between RLS and cardiovascular disease,[19,20] one large population-based study reported that multiple cardiovascular risk factors, including obesity, diabetes, and hypertension were independent predictors of incident RLS.[21] Of these risk factors, only diabetes was found to have significant value as a risk factor for RLS in both the univariate and multivariate analyses in our study. The present study also demonstrated that hypertension was a significant risk factor, but this association was no longer present in the multivariate analysis. In addition, our survey failed to demonstrate a significant association between obesity and RLS. This result is in contrast to findings in previous epidemiological studies that indicated that body mass index (BMI), independent of all other confounders, was associated with a higher risk of RLS.[22,23,24] This relationship may be due to a decrease in the number of dopamine receptors in the brains of obese subjects. The lack of a role of obesity as a risk factor for RLS in the Saudi population may be related to the fact that obesity is very common in our community, affecting more than 50% of the population,[25] thus making it difficult to identify differences between individuals who are and are not affected by RLS. Nevertheless, this absence of the role of obesity in RLS was in agreement with other studies.[26,27] Similarly, habitual snoring (a possible risk factor for coronary artery disease) was identified in our survey as another independent risk factor for RLS, a finding that was not reported previously. Results from a relatively recent study suggested that snoring was independently associated with carotid artery atherosclerosis.[28] Nevertheless, snoring is a cardinal sign of obstructive sleep apnea, which is a potential risk factor for ischemic heart disease.[29,30,31,32] In this study, RLS patients were also found to be predominantly male, which is a well-known independent risk factor for coronary artery disease. Another significant risk factor for cardiovascular diseases is smoking, which was identified as a factor that may also aggravate RLS symptoms.[14] Although our study also showed a significant link between smoking and RLS, this association was no longer present in the multivariate analysis.
Interestingly, consanguinity (defined as a possible marriage between first-degree cousins) was significantly associated with RLS in our study population. This risk factor, which is a practice common in certain Saudi families, had not been previously investigated. The significant association between this new potential risk factor and RLS was shown in the univariate analysis (OR: 2.10; 95% CI: (1.46-2.92); P < 0.001) [Table 6]. This finding is further supported by the previously reported family history of RLS in more than 40% of patients with primary RLS.[34,35] However, this significant link disappeared with the multivariate analysis, and hence, further studies are needed to further endorse this potential risk factor.
Because the diagnosis of RLS in the present study was based on the four minimum IRLSSG diagnostic criteria regardless of frequency, severity, or differential diagnosis; the prevalence rate likely encompasses both primary and secondary RLS. In addition, cases that mimic RLS may have also been included, leading to an exaggerated prevalence rate. Therefore, this study had some limitations, including lack of clinical assessments, failure to utilize procedures as well as blood tests in order to confirm the diagnosis of RLS, and differentiate primary from secondary types.
In summary, the present study was a population-based study with a large sample size conducted in Saudi Arabia that demonstrated that RLS is a common problem in the Saudi population. It suggested that the prevalence rate, patient presentation, and associated risk factors of RLS might be different than in other countries. Although the prevalence of this condition in the Saudi population was within the range reported by Western studies, it was higher than that reported by Asian studies. In addition, unlike most studies from Europe and North America, our study showed that RLS mainly affects males. DM was found to be associated with RLS, which is consistent with previous studies. Interestingly, habitual snoring, asthma, and consanguinity were introduced in this study as new potential risk factors. These findings, however, require a further evaluation.
Acknowledgment
We would like to thank all Sleep Medicine and Research Center staff at KAUH; specially Ms. Haneen Almutairi, Ms. Walaa Abubzahra and Dr. Ibrahim Zakaria for their unlimited cooperation with data collection and data entry.
Footnotes
Source of Support: King Abdulaziz University for Science and Technology (KACST)
Conflicts of interest: None declared.
References
- 1.Diagnostic and Coding Manual. 2nd ed. 2005. American academy of sleep medicine. The international classification of sleep disorders; pp. 178–181. [Google Scholar]
- 2.Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisi J. Restless Legs Syndrome Diagnosis and Epidemiology workshop at the National Institutes of Health, International Restless Legs Syndrome Study Group. Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–19. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 3.Walters AS, Henling W. Clinical presentation and neuropharmacology of restless legs syndrome. Clin Neuropharmacol. 1987;10:225–37. doi: 10.1097/00002826-198706000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Walters AS, LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP, et al. International Restless Legs Syndrome Study Group. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003;4:121–32. doi: 10.1016/s1389-9457(02)00258-7. [DOI] [PubMed] [Google Scholar]
- 5.Abetz L, Arbuckle R, Allen RP, Garcia-Borreguero D, Hening W, Walters AS, et al. The reliability, validity and responsiveness of the International Restless Legs Syndrome Study Group rating scale and subscales in a clinical-trial setting. Sleep Med. 2006;7:340–9. doi: 10.1016/j.sleep.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 6.Allen RP, Walters AS, Montplaisir J, Hening W, Myers A, Bell TJ, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165:1286–92. doi: 10.1001/archinte.165.11.1286. [DOI] [PubMed] [Google Scholar]
- 7.Ohayon MM, O'Hara R, Vitiello MV. Epidemiology of restless legs syndrome: A synthesis of the literature. Sleep Med Rev. 2012;16:283–95. doi: 10.1016/j.smrv.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.BaHammam A, Al-shahrani K, Al-zahrani S, Al-shammari A, Al-amri N, Sharif M. The prevalence of restless legs syndrome in adult Saudis attending primary health care. Gen Hosp Psychiatry. 2011;33:102–6. doi: 10.1016/j.genhosppsych.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The Occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 10.Johns MW. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 11.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine; 2000;25:3186–91. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 12.Harkness J, Pennell BE, Schoua-Glusberg A. Survey questionnaire translation and assessment. In: Presser S, Rothgeb J, Couper M, Lessler J, Martin E, Martin J, editors. Methods for Testing and Evaluating Survey Questionnaires. Vol. 68. Hoboken: John Wiley and Sons; 2004. pp. 453–73. doi:10.1093/poq/nfh008. [Google Scholar]
- 13.Rangarajan S, Rangarajan S, D'Souza GA. Restless legs syndrome in an Indian urban population. Sleep Med. 2007;9:88–93. doi: 10.1016/j.sleep.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Bayard M, Avonda T, Wadzinski J. Restless legs syndrome. Am Fam Physician. 2008;78:235–40. [PubMed] [Google Scholar]
- 15.Wali SO, Idrees MM, Alamoudi OS, Aboulfarag AM, Salem AD, Aljohaney AA, et al. Prevalence of chronic obstructive pulmonary disease in Saudi Arabia. Saudi Med J. 2014;35:684–90. [PubMed] [Google Scholar]
- 16.Sevim S, Dogu O, Camdeviren H, Bugdayci R, Sasmaz T, Kaleagasi H, et al. Unexpectedly low prevalence and unusual characteristics of RLS in Mersin, Turkey. Neurology. 2003;61:1562–9. doi: 10.1212/01.wnl.0000096173.91554.b7. [DOI] [PubMed] [Google Scholar]
- 17.Erer S, Karli N, Zarifoglu M, Ozcakir A, Yildiz D. The prevalence and clinical features of restless legs syndrome: A door to door population study in Orhangazi, Bursa in Turkey. Neurol India. 2009;57:729–33. doi: 10.4103/0028-3886.59467. [DOI] [PubMed] [Google Scholar]
- 18.Taºdemir M, Erdoğan H, Börü UT, Dilaver E, Kumaº A. Epidemiology of restless legs syndrome in Turkish adults on the western Black Sea coast of Turkey: A door-to-door study in a rural area. Sleep Med. 2010;11:82–6. doi: 10.1016/j.sleep.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Walters AS, Rye DB. Review of the relationship of restless legs syndrome and periodic limb movements in sleep to hypertension, heart disease, and stroke. Sleep. 2009;32:589–97. doi: 10.1093/sleep/32.5.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Winkelman JW, Shahar E, Sharief I, Gottlieb DJ. Association of restless legs syndrome and cardiovascular disease in the Sleep Heart Health Study. Neurology. 2008;70:35–42. doi: 10.1212/01.wnl.0000287072.93277.c9. [DOI] [PubMed] [Google Scholar]
- 21.Szentkirályi A, Völzke H, Hoffmann W, Happe S, Berger K. A time sequence analysis of the relationship between cardiovascular risk factors, vascular diseases and restless legs syndrome in the general population. J Sleep Res. 2013;22:434–42. doi: 10.1111/jsr.12040. [DOI] [PubMed] [Google Scholar]
- 22.Gao X, Schwarzschild MA, Wang H, Ascherio A. Obesity and restless legs syndrome in men and women. Neurology. 2009;72:1255–61. doi: 10.1212/01.wnl.0000345673.35676.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res. 2002;53:547–54. doi: 10.1016/s0022-3999(02)00443-9. [DOI] [PubMed] [Google Scholar]
- 24.Kim J, Choi C, Shin K, Yi H, Park M, Cho N, et al. Prevalence of restless legs syndrome and associated factors in the Korean adult population: The Korean Health and Genome Study. Psychiatry Clin Neurosci. 2005;59:350–3. doi: 10.1111/j.1440-1819.2005.01381.x. [DOI] [PubMed] [Google Scholar]
- 25.Al-Othaimeen AI, Al-Nozha M, Osman AK. Obesity: An emerging problem in Saudi Arabia. Analysis of data from the National Nutrition Survey. East Mediterr Health J. 2007;13:441–8. [PubMed] [Google Scholar]
- 26.Celle S, Roche F, Kerleroux J, Thomas-Anterion C, Laurent B, Rouch I, et al. Prevalence and clinical correlates of restless legs syndrome in an elderly French population: The synapse study. J Gerontol A Biol Sci Med Sci. 2010;65:167–73. doi: 10.1093/gerona/glp161. [DOI] [PubMed] [Google Scholar]
- 27.Winkelman JW, Redline S, Baldwin CM, Resnick HE, Newman AB, Gottlieb DJ. Polysomnographic and health-related quality of life correlates of restless legs syndrome in the Sleep Heart Health Study. Sleep. 2009;32:772–8. doi: 10.1093/sleep/32.6.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee SA, Amis TC, Byth K, Larcos G, Kairaitis K, Robinson TD, et al. Heavy snoring as a cause of carotid artery atherosclerosis. Sleep. 2008;31:1207–13. [PMC free article] [PubMed] [Google Scholar]
- 29.Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM. Burden of sleep apnea: Rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ. 2009;108:246–9. [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Shawwa BA, Badi AN, Goldberg AN, Woodson BT. Defining common outcome metrics used in obstructive sleep apnea. Sleep Med Rev. 2008;12:449–61. doi: 10.1016/j.smrv.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 31.Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O'Connor GT, et al. Sleep-disordered breathing and mortality: A prospective cohort study. PLoS Med. 2009;6:e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 33.Kageyama T, Kabuto M, Nitta H, Kurokawa Y, Taira K, Suzuki S, et al. Prevalences of periodic limb movement-like and restless legs-like symptoms among Japanese adults. Psychiatry Clin Neurosci. 2000;54:296–8. doi: 10.1046/j.1440-1819.2000.00685.x. [DOI] [PubMed] [Google Scholar]
- 34.Hening W, Allen R, Earley C, Kushida C, Picchietti D, Silber M. The treatment of restless legs syndrome and periodic limb movement disorder. An American Academy of Sleep Medicine Review. Sleep. 1999;22:970–99. [PubMed] [Google Scholar]
- 35.Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lespérance P. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: A study of 133 patients diagnosed with new standard criteria. Mov Disord. 1997;12:61–5. doi: 10.1002/mds.870120111. [DOI] [PubMed] [Google Scholar]


