Abstract
Background
Psychological stress is a proposed risk factor for cardiovascular disease (CVD), and posttraumatic stress disorder (PTSD), the sentinel stress-related mental disorder, occurs twice as frequently in women as men. However, whether PTSD contributes to CVD risk in women is not established.
Methods and Results
We examined trauma exposure and PTSD symptoms in relation to incident CVD over a 20-year period in 49,978 women in the Nurses’ Health Study II. Proportional hazards models estimated hazard ratios (HRs) and 95% confidence intervals (CIs) for CVD events confirmed by additional information or medical record review [n=548, including myocardial infarction (n=277) and stroke (n=271)]. Trauma exposure and PTSD symptoms were assessed using the Brief Trauma Questionnaire and a PTSD screen. Compared to no trauma exposure, endorsing 4 or more PTSD symptoms was associated with increased CVD risk after adjusting for age, family history, and childhood factors (HR=1.60 [95% CI, 1.20–2.13]). Being trauma-exposed and endorsing no PTSD symptoms was associated with elevated CVD risk (HR=1.45 [95% CI, 1.15–1.83]), although being trauma-exposed and endorsing 1–3 PTSD symptoms was not. After adjusting for adult health behaviors and medical risk factors, this pattern of findings was maintained. Health behaviors and medical risk factors accounted for 14% of the trauma/no symptoms-CVD association and 47% of the trauma/4+ symptoms-CVD association.
Conclusion
Trauma exposure and elevated PTSD symptoms may increase risk of CVD in this population of women. These findings suggest screening for CVD risk and reducing health risk behaviors in trauma-exposed women may be promising avenues for prevention and intervention.
Keywords: cardiovascular disease, posttraumatic stress disorder, trauma, women, epidemiology
Despite progress in risk factor identification and treatment, cardiovascular disease (CVD) remains the leading cause of death in women,1 and the prevalence of CVD in middle-aged women in particular is on the rise.2 Consequently, there have been calls to expand the scope of research beyond established CVD risk factors in order to improve intervention and prevention efforts.1 Psychological stress has long been hypothesized to be a risk factor for CVD,3 and exposure to extremely stressful or traumatic events, such as childhood adversity4 and combat,5 has been linked to increased CVD risk. Posttraumatic stress disorder (PTSD) occurs in some individuals following trauma exposure and is characterized by re-experiencing the trauma, avoidance of trauma reminders, emotional numbing, and hyperarousal. PTSD, considered the sentinel stress-related mental disorder, is common, with lifetime prevalence rates twice as high in women (10%) as in men (5%).6 Evidence for a PTSD-CVD relation is suggestive,7 and PTSD has been linked to CVD risk-related biomarkers, including elevated inflammatory markers8 and serum lipid concentrations.9 Nevertheless, a systematic literature review indicated a paucity of large, prospective epidemiologic studies of the relations between trauma exposure, PTSD, and CVD, particularly among women.10
Despite emerging findings on stress-related mental disorders and CVD, understanding of whether PTSD increases risk of CVD is limited in important ways. First, the PTSD-CVD relation has been understudied in women. PTSD is more prevalent and associated with greater chronicity and impairment in women than men,6, 11 and CVD manifests in unique ways in women compared to men.12 Thus, studying the PTSD-CVD relation specifically in women is important. To date, of the seven prospective studies of PTSD and incident CVD,5, 13–18 only one has been conducted in women.18 This study by Kubzansky et al., 18 which suggested elevated CVD risk in women with higher PTSD symptoms, relied on self-reported CVD outcomes, necessitating replication with confirmed outcomes. Second, the PTSD-CVD association may be confounded by trauma exposure. It remains unclear whether trauma exposure alone or the mental health consequences of trauma, most typically PTSD, lead to increased CVD risk. Third, although PTSD has been associated with behavioral risk factors for CVD, including cigarette smoking,19 obesity,20 and physical inactivity,21 little research has investigated whether these and other behavioral and medical risk factors mediate the PTSD-CVD relation.
We addressed these under-examined issues using data from a sub-sample of the Nurses’ Health Study II (NHS II), an ongoing cohort study of younger and middle-aged women initiated in 1989. We compared the incidence of CVD events (myocardial infarction [MI] and stroke) confirmed by additional information or medical record review over a 20-year period in women without trauma exposure and with trauma exposure and different PTSD symptom levels. All women were younger than 65 years of age at the end of the study period; thus our investigation addressed the association between trauma, PTSD, and early-onset CVD, an important risk phenotype, particularly in women.12 We also investigated health behaviors and medical risk factors as potential mediators of associations between trauma, PTSD symptoms, and CVD incidence. We hypothesized that trauma exposure and elevated PTSD symptoms would be associated with increased CVD risk compared to no trauma exposure, with women with the highest PTSD symptoms showing the most elevated risk due to greatest behavioral and biological dysregulation.
Methods
Sample
The NHS II includes 116,430 U.S. female nurses, aged 25–42 years at enrollment in 1989 and followed biennially. In 2008, when participants were aged 44–62 years, 60,804 women who completed the 2001 Violence questionnaire and 2007 biennial questionnaire were mailed a supplemental questionnaire assessing trauma exposure and PTSD symptoms.22 To maximize retention, supplemental surveys are only sent to those who return biennial questionnaires. After repeated mailings, 54,282 women returned the questionnaire (89% response rate). This study was approved by the Institutional Review Board of Brigham and Women’s Hospital. Return of the questionnaire via U.S. mail constituted implied consent.
Trauma and PTSD Assessment
Trauma exposure was measured with a 16-item modified version of the Brief Trauma Questionnaire (BTQ).22 The BTQ is considered a reliable and valid measure of trauma exposure that parallels interview measures of trauma exposure.22,23,24 Exposure to 15 traumatic events (e.g., natural disaster exposure, unwanted sexual contact, physical assault), in addition to “a seriously traumatic event not already covered,” was assessed; exposure to each event at any point in one’s lifetime was coded as present or absent. Respondents identified which event occurred first and which event was their worst or most distressing experience. They also reported their ages at the first and worst events. Occurrence of PTSD symptoms in participants’ lifetimes was queried with respect to the worst traumatic event using the 7-item Short Screening Scale for DSM-IV PTSD.25 This scale assesses seven PTSD symptoms (each coded as present or absent). A cutoff score of four has been recommended for identifying probable PTSD;25 this cutoff has been found to define positive cases of PTSD in other samples with a sensitivity of 85% and specificity of 93%.25 Reliability of self-reported age-of-onset of trauma and PTSD has been found to be excellent in this sample (ICC=.95).
For each year of the study, participants were categorized into four groups based on the year of their first trauma and the year of their worst trauma: 1) no trauma exposure, 2) trauma-exposed and endorsed no PTSD symptoms on the screen (referred to as trauma/no symptoms), 3) trauma-exposed and endorsed 1–3 PTSD symptoms (referred to as trauma/1–3 symptoms), and 4) trauma-exposed and endorsed 4 or more PTSD symptoms (referred to as trauma/4+ symptoms). Prior to their first trauma (if one was reported), women were categorized as having no trauma exposure. After their first trauma, women were classified as trauma/no symptoms. Following their worst trauma, women were classified as trauma/no symptoms, trauma/1–3 symptoms, or trauma/4+ symptoms based on the number of PTSD symptoms reported with respect to the worst event. If women reported only one event, then the years of the first trauma and worst trauma were the same.
Cardiovascular Endpoint Assessment
At baseline, participants reported whether they ever experienced physician-diagnosed “MI or angina” or “stroke (CVA [cerebrovascular accident]) or TIA [transient ischemic attack]).” A positive response to any of these CVD endpoints at baseline resulted in exclusion from analyses. At each biennial follow-up, participants indicated whether they had a physician-diagnosed “MI” or “stroke (CVA) or TIA” in the past 2 years. Consistent with prior research,4 we defined CVD events based on MI and stroke. TIA alone (n=39) was excluded. All CVD events were nonfatal. Physicians blind to participants’ trauma/PTSD status reviewed medical records to confirm reported CVD events after obtaining participants’ permission. MI was confirmed if it met World Health Organization criteria based on symptoms plus diagnostic ECG changes or elevated cardiac-specific enzyme concentrations.26 Stroke was confirmed based on National Survey of Stroke criteria as a neurological deficit with sudden or rapid onset that persisted for >24 hours or until death.27 Cases confirmed by record review were considered “definite cases.” CVD events were classified as “probable cases” if a participant or relative acknowledged the reported diagnosis as correct but access to medical records was denied or unable to be attained. Trauma exposure and PTSD symptoms were not associated with differential rates of record refusal (χ2(df=3)=1.57, P=.67). In this study, we considered probable or definite CVD events based on the 1991–2009 questionnaires (n=548).
Covariates
Family history and childhood factors were included as potential confounders, specifically race/ethnicity (African American, Latina, Asian, Caucasian, other), maximum parental education at the participant’s birth (high school or less, some college, 4+ years of college), maternal and paternal history of MI or stroke, and somatotype at age five based on a somatogram scale (to estimate childhood adiposity).
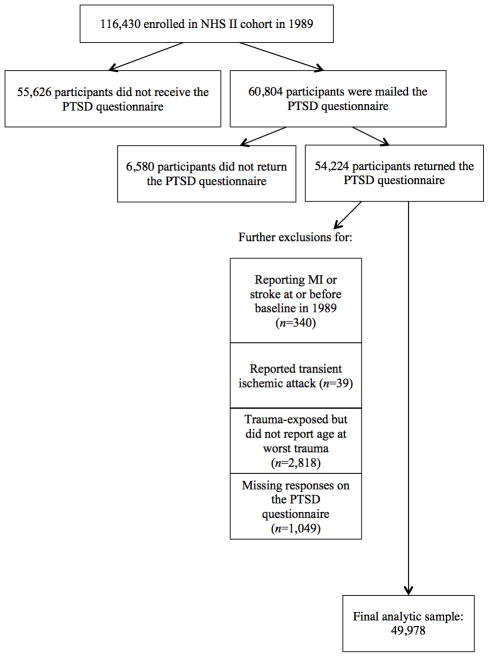
Adult health behaviors and medical risk factors were examined as possible mediators of the PTSD-CVD association. These time-varying covariates were assessed at baseline via self-report and updated biennially, unless otherwise noted (see Figure 1 for study timeline). Adult body mass index (BMI) in kg/m2 was computed from self-reported height and weight and coded continuously.28 In addition, participants were classified as nonsmokers, former smokers, or current smokers of 1–14, 15–24, or 25+ cigarettes/day. Alcohol consumption was assessed in 1989, 1991, 1995, 1999, 2003, and 2007, and categorized as 0, 1–4, 5–9, 10–19, or 20+ grams/day. Physical activity was measured in 1989, 1991, 1997, 2001, and 2005, and categorized as less than 3, 3–8.9, 9–17.9, 18–26.9, or 27+ metabolic equivalent hours/week. Diet quality was assessed every 4 years beginning in 1991 and quantified based on the Alternative Healthy Eating Index, which has been linked to CVD risk.29 Alternative Healthy Eating Index scores were divided into quintiles; the highest quintile represented the healthiest diet. Time-varying indicators for presence or absence of physician-diagnosed hypertension and type 2 diabetes mellitus, along with use of hormone therapy (HT; never used/premenopausal, current user, former user), were included as covariates given evidence for associations with MI or stroke.30–32 We also examined use of antidepressant medication (ADM), which is often prescribed for PTSD33 and has been linked to increased CVD risk.34 Lifetime ADM use was assessed in 1993, and regular past two-year ADM use was assessed in 1997, 2001, 2003, 2005, and 2007. We created a single time-varying ADM use variable. Women who endorsed lifetime ADM use in 1993 were coded as having used ADM from 1989–1993, and use was updated as available.
Figure 1.
Timeline of variables collected at biennial assessments. CVD=cardiovascular disease. BMI=body mass index. T2D=type 2 diabetes mellitus. HTN=hypertension. HT=hormone therapy. ADM=antidepressant medication. Response rates for the analytic sample are listed for each time point. Trauma/PTSD status was assigned for each year of the study and updated based on reported age of worst trauma (assessed with a supplemental questionnaire in 2008).
Sensitivity Analyses
Childhood abuse and depression have been associated with increased CVD risk in this cohort,4, 35 and we examined potential confounding by childhood abuse and depression prior to PTSD onset. Childhood sexual abuse (CSA) before age 18 was measured in 2001 with four questions regarding unwanted sexual touching or forced or coerced sexual contact by an adult or older child.36 Responses were coded as no sexual abuse, sexual touch only, or forced sex.4 Childhood physical abuse was assessed in 2001 with the revised Conflict Tactics Scale,37 and classified as none, mild, moderate, or severe.4 Depressive symptoms were assessed in 1993 with the 5-item Short Form-36 Mental Health scale, a mental health status measure found to be valid in screening for depression.38
Exclusions
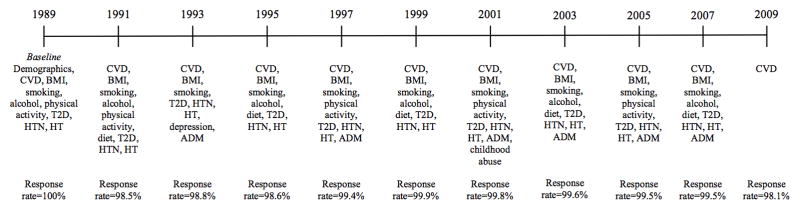
A flowchart of participant exclusions used to derive the analytic sample (N=49,978) is depicted in Figure 2. Women excluded from analyses were similar to those included in terms of childhood adiposity (highest somatotype at age five: 6.9% vs. 6.9%), age at baseline (34.1 vs. 34.7 years), BMI at baseline (24.3 vs. 23.8), and cumulative incidence of CVD events from 1989–2009 (1.2% vs. 1.1%), although they reported somewhat lower rates of family history of CVD: maternal history of MI (9.6% vs. 11.0%), maternal history of stroke (6.1% vs. 8.8%), paternal history of MI (26.1% vs. 29.6%), paternal history of stroke (8.9% vs. 13.1%).
Figure 2.
Flowchart of exclusions for deriving the final analytic sample.
Statistical Analysis
We investigated whether trauma exposure and PTSD symptoms were associated with CVD incidence by using Cox proportional hazards models to calculate hazard ratios (HRs) and 95% confidence intervals (CIs). Participants contributed person-time from baseline in 1989 until their last returned questionnaire, CVD onset, or the end of follow-up based on the 2009 questionnaire. Trauma exposure and PTSD symptoms at baseline were updated over the study period based on participants’ reported age at the worst trauma. Models were constructed such that, for each time period of prediction (e.g., CVD from the 1993 questionnaire), proposed mediators were lagged by one period (e.g., data from the 1991 questionnaire) and trauma/PTSD status was lagged such that it represented the year prior to the period for the mediators (e.g., trauma/PTSD status in 1990).
We tested a series of models that sequentially adjusted for potential confounders and mediators. Model 1 adjusted for age and included dummy variables representing trauma/no symptoms, trauma/1–3 symptoms, and trauma/4+ symptoms. Model 2 adjusted for family history and childhood factors considered potential confounders (race/ethnicity, parental education, maternal and paternal history of MI or stroke, age five somatotype). Model 3 adjusted for adult health behaviors that might serve as mediators of the PTSD-CVD association (BMI, cigarette smoking, alcohol intake, physical activity, diet quality). Model 4 adjusted for all factors included in Model 3 plus medical risk factors that have been directly or indirectly linked with trauma exposure or PTSD as well as CVD (hypertension, type 2 diabetes mellitus, HT use, ADM use). We investigated the extent to which health behaviors and medical risk factors in Model 4 might account for increased CVD risk in women with trauma exposure and PTSD symptoms using the SAS mediate macro.39,40 This macro calculates point estimates (and 95% CIs) of the percent of exposure effect explained by one or more intermediate variables, and is estimated on the coefficient scale.
To test potential confounding by childhood abuse, we re-estimated Model 2 adjusting for childhood abuse. We also investigated potential confounding by depression prior to PTSD onset by adjusting for depressive symptoms assessed in 1993 (the earliest depression measure in the NHS II). Depression can be triggered by PTSD41 and could mediate the PTSD-CVD association. We were most concerned with investigating whether depression prior to PTSD accounted for our results. To ensure depression occurred prior to PTSD, we began our prediction period after 1993 and excluded PTSD cases with onset in or prior to 1993, resulting in a sample size of 40,356. We also examined potential effect modification by testing interactions between trauma/PTSD status with childhood abuse and early depression as these variables might potentiate the association between trauma/PTSD status and CVD. Additionally, we addressed the possible impact of recall bias in the retrospective reporting of trauma and PTSD given that most CVD events occurred prior to the trauma and PTSD assessment in 2008. We conducted an analysis that included only CVD events occurring after trauma and PTSD assessment (i.e., 163 CVD events reported on the 2009 biennial questionnaire), adjusting for Model 2 covariates.
Results
Participant characteristics as a function of trauma exposure and PTSD symptoms at baseline are presented in Table 1. Approximately 30% of participants did not report any traumatic events at or prior to baseline. Just over 50% of women were classified as trauma/no symptoms at baseline, 9.5% of women were classified as trauma/1–3 symptoms, and 9.5% of women were classified as trauma/4+ symptoms. Compared to no trauma exposure, trauma exposure and PTSD symptoms were associated with higher rates of cigarette smoking and family history of MI and stroke, in addition to a greater likelihood of reporting the highest somatotype at age five. Over follow-up, an additional 4,372 women reported trauma exposure. In the final period for predicting CVD incidence, approximately 21% of women were classified as having no trauma exposure, 47% as trauma/no symptoms, and 16% each as trauma/1–3 symptoms and trauma/4+ symptoms, respectively.
Table 1.
Participant characteristics as a function of trauma exposure and PTSD symptoms at the NHS II 1989 baseline assessment (N=49978)
| No trauma (n=15005) | Trauma-exposed (n=34973)
|
|||
|---|---|---|---|---|
| No PTSD symptoms (n=25471) | 1–3 symptoms (n=4751) | 4+ symptoms (n=4751) | ||
| Age in 1989 | 34 years | 35 years | 35 years | 35 years |
| Parents’ education at birth, ≥ college | 23.7% (3555) | 22.4% (5702) | 22.9% (1089) | 23.3% (1105) |
| Maternal history of MI* | 9.4% (1413) | 11.4% (2901) | 11.8% (562) | 13.4% (635) |
| Paternal history of MI | 27.9% (4179) | 30.1% (7662) | 30.4% (1443) | 31.3% (1489) |
| Maternal history of stroke | 7.5% (1118) | 9.4% (2397) | 8.3% (395) | 10.7% (510) |
| Paternal history of stroke | 11.8% (1766) | 13.5% (3444) | 13.1% (622) | 14.8% (701) |
| Highest somatotype, age 5 | 6.2% (928) | 7.0% (1795) | 6.7% (319) | 8.0% (379) |
| Race | ||||
| African American | 0.7% (111) | 1.0% (265) | 1.1% (51) | 0.8% (37) |
| Asian | 1.6% (234) | 1.2% (299) | 0.9% (43) | 0.8% (38) |
| Caucasian | 93.5% (14030) | 93.8% (23894) | 94.2% (4474) | 94.6% (4496) |
| Latina | 0.9% (139) | 1.4% (347) | 1.5% (70) | 1.3% (62) |
| Other | 3.3% (491) | 2.6% (666) | 2.4% (113) | 2.5% (118) |
| Body mass index (kg/m2) | 23.5 | 23.9 | 24.0 | 24.2 |
| Cigarette Smoking | ||||
| Never | 72.3% (10851) | 65.8% (16749) | 62.1% (2949) | 58.7% (2788) |
| Former smoker | 18.1% (2718) | 22.4% (5708) | 25.0% (1187) | 27.3% (1295) |
| Current, 1–14 cigs/day | 4.1% (612) | 4.6% (1176) | 5.0% (236) | 5.1% (244) |
| Current, 15–24 cigs/day | 3.6% (542) | 4.7% (1206) | 5.0% (239) | 5.9% (278) |
| Current, 25+ cigs/day | 1.6% (236) | 2.2% (552) | 2.5% (121) | 2.7% (126) |
| Missing | 0.3% (46) | 0.3% (80) | 0.4% (19) | 0.4% (20) |
| Alcohol Intake | ||||
| 0 grams/day | 35.9% (5392) | 36.3% (9248) | 36.2% (1722) | 39.2% (1860) |
| 1–<5 grams/day | 43.1% (6470) | 42.7% (10875) | 41.5% (1972) | 40.1% (1906) |
| 5–<10 grams/day | 11.2% (1675) | 11.1% (2815) | 11.2% (530) | 10.2% (483) |
| 10–<20 grams/day | 7.7% (1156) | 7.5% (1921) | 8.6% (409) | 7.9% (377) |
| 20+ grams/day | 1.3% (198) | 1.6% (413) | 1.9% (91) | 1.8% (87) |
| Missing | 0.8% (114) | 0.8% (199) | 0.6% (27) | 0.8% (38) |
| Physical Activity | ||||
| <3 MET hrs/wk† | 14.6% (2194) | 13.9% (3543) | 15.2% (722) | 14.4% (683) |
| 3–8.9 MET hrs/wk | 23.3% (3498) | 23.1% (5882) | 23.5% (1115) | 22.4% (1065) |
| 9–17.9 MET hrs/wk | 21.0% (3156) | 21.5% (5487) | 21.3% (1011) | 20.5% (976) |
| 18–26.9 MET hrs/wk | 13.3% (1993) | 13.3% (3391) | 14.0% (665) | 14.3% (677) |
| 27+ MET hrs/wk | 27.8% (4164) | 28.1% (7168) | 26.1% (1238) | 28.4% (1350) |
| Alternative Health Eating Index | ||||
| 1st quintile (worst diet) | 20.4% (3063) | 18.0% (4593) | 16.8% (799) | 16.3% (774) |
| 2nd quintile | 19.0% (2845) | 18.4% (4692) | 18.8% (891) | 17.0% (806) |
| 3rd quintile | 26.0% (3906) | 25.9% (6586) | 25.5% (1210) | 25.4% (1205) |
| 4th quintile | 17.5% (2619) | 18.9% (4817) | 18.0% (855) | 18.9% (896) |
| 5th quintile (best diet) | 16.7% (2510) | 18.3% (4670) | 20.6% (977) | 22.0% (1047) |
| Missing | 0.4% (62) | 0.4% (113) | 0.4% (19) | 0.5% (23) |
MI=myocardial infarction.
MET hrs/wk=metabolic equivalent hours per week.
There were 548 probable or definite CVD events (277 MI and 271 stroke events) between 1989 and 2009. Compared to no trauma exposure, both trauma/no symptoms and trauma/4+ symptoms were associated with increased risk of CVD incidence after adjusting for demographic, family history, and childhood factors (Table 2, Model 2). Women with 4 or more PTSD symptoms had the highest risk of a CVD event, followed by trauma-exposed women endorsing no symptoms, although the HRs for these two groups were not significantly different, P=.42. Endorsing 1–3 PTSD symptoms was not significantly associated with risk of CVD incidence, and the HRs for the trauma/no symptoms and trauma/4+ symptoms groups were significantly greater than the HR for the trauma/1–3 symptoms group, Ps<.01. The associations between trauma/no symptoms and trauma/4+ symptoms with CVD incidence remained statistically significant, albeit somewhat attenuated, after adjusting for adult health behaviors (Table 2, Model 3). Adjusting for health conditions and CVD-associated medication use further attenuated the associations, although trauma/no symptoms remained significantly associated with elevated CVD risk (Table 2, Model 4). Trauma/PTSD status was significantly associated with all proposed health behavior and medical risk factor mediators, Ps<.05. Based on the SAS mediate macro and assuming their actions were fully those of mediation (and not confounding), adult health behaviors and medical risk factors accounted for 14% (95% CI, 3–25%) of the association of trauma/no symptoms with CVD and 47% (95% CI, 23–70%) of the association of trauma/4+ symptoms with CVD. There were no significant exposure-mediator interactions (Ps>.05), and confounding of mediator-outcome associations was minimized by statistically controlling for relevant variables, including demographics, family history, and childhood adiposity. Moreover, the effect estimates of the mediators were highly similar in models with and without these potential confounders, suggesting that confounding was minimal.
Table 2.
Adjusted hazard ratios (95% confidence intervals) for the association of trauma exposure and PTSD symptoms with risk of incident cardiovascular events, 1989 to 2009
| Hazard Ratio (95% Confidence Interval)
|
|||||
|---|---|---|---|---|---|
| Cases, n (person-y) | Model 1: Adjusted for Age | Model 2: Adjusted for Age, Family History, and Childhood Factors* | Model 3: Model 2 Plus Health Behaviors† | Model 4: Model 3 Plus Medical Risk Factors‡ | |
| No trauma exposure | 94 (261 315) | 1.00 | 1.00 | 1.00 | 1.00 |
| Trauma/No symptoms | 300 (538 609) | 1.46 (1.16–1.84) | 1.45 (1.15–1.83) | 1.42 (1.12–1.79) | 1.38 (1.09–1.75) |
| Trauma/1–3 symptoms | 58 (134 319) | 1.00 (0.72–1.39) | 0.99 (0.71–1.38) | 0.94 (0.68–1.31) | 0.90 (0.65–1.25) |
| Trauma/4+ symptoms | 96 (137 340) | 1.64 (1.23–2.18) | 1.60 (1.20–2.13) | 1.43 (1.07–1.91) | 1.30 (0.97–1.74) |
Adjusted for age, race/ethnicity, parental education, maternal and paternal history of MI or stroke, and age 5 somatotype.
Adjusted for variables in Model 2 plus BMI, cigarette smoking, alcohol intake, physical activity, and diet quality.
Adjusted for variables in Model 3 plus hypertension, type 2 diabetes mellitus, hormone therapy, and antidepressant use.
Prior research in this population has demonstrated an association of childhood abuse with CVD incidence.4 In the current sample (which overlapped somewhat, but not completely, with the sample used in the previous study4), CSA was associated with increased CVD risk (HR=1.23 [95% CI, 1.00–1.50] for sexual touching only and HR=1.62 [95% CI, 1.27–2.07] for forced sex) over and above age, family history, and childhood factors. Childhood physical abuse was not significantly associated with CVD incidence, Ps>.14. To investigate whether current findings were confounded by CSA, we conducted a sensitivity analysis adjusting for CSA. Trauma/no symptoms and trauma/4+ symptoms were still associated with increased risk of CVD (adjusting for covariates in Model 2; HR=1.37 [95% CI, 1.08–1.73] for trauma/no symptoms; HR=0.91 [95% CI, 0.65–1.27] for trauma/1–3 symptoms; HR=1.39 [95% CI, 1.03–1.87] for trauma/4+ symptoms). Moreover, there was no significant interaction between CSA and trauma/PTSD status for CVD incidence, P=.28.
We also considered whether depressive symptoms might confound our findings. When covarying depressive symptoms in 1993 along with the covariates in Model 2, trauma/no symptoms and trauma/4+ symptoms were associated with elevated CVD risk; the HRs were close in magnitude to those in the original analyses, although the trauma/4+ symptoms-CVD association fell short of statistical significance (HR=1.48 [95% CI, 1.15–1.91] for trauma/no symptoms; HR=1.07 [95% CI, 0.75–1.51] for trauma/1–3 symptoms; HR=1.53 [95% CI, 0.90–2.61] for trauma/4+ symptoms). There was no significant interaction between depression and trauma/PTSD status for risk of incident CVD, P=.997.
In the prospective analysis predicting incident CVD based on the 2009 questionnaire (adjusted for covariates in Model 2), trauma/no symptoms and trauma/4+ symptoms were associated with increased risk of CVD incidence (HR=1.27 [95% CI, 0.83–1.94] for trauma/no symptoms; HR=0.79 [95% CI, 0.44–1.42] for trauma/1–3 symptoms; HR=1.42 [95% CI, 0.86–2.34] for trauma/4+ symptoms). These findings did not reach statistical significance, likely given limited statistical power in this short follow-up period.
We also examined associations of trauma exposure and PTSD symptoms separately with incidence of probable or definite MI (n=277) and stroke (n=271) over the entire study period (Table 3). Results for MI were similar to those for overall CVD, with trauma/no symptoms and trauma/4+ symptoms associated with increased risk of MI incidence compared to no trauma exposure. Only trauma/4+ symptoms was significantly related to stroke incidence.
Table 3.
Adjusted* hazard ratios (95% confidence intervals) for the association of trauma exposure and PTSD symptoms with risk of incident MI and stroke, 1989 to 2009
| MI (n=277) | Stroke (n=271) | |
|---|---|---|
| No trauma exposure | 1.00 | 1.00 |
| Trauma/No symptoms | 1.96 (1.38–2.78) | 1.09 (0.80–1.50) |
| Trauma/1–3 symptoms | 1.11 (0.68–1.81) | 0.93 (0.59–1.44) |
| Trauma/4+ symptoms | 1.58 (1.02–2.46) | 1.64 (1.12–2.39) |
Adjusted for age, race/ethnicity, parental education, maternal and paternal history of MI or stroke, and age 5 somatotype.
Discussion
We examined whether trauma exposure and PTSD symptoms were associated with risk of early-onset CVD (MI and stroke) over 20 years in a large, population-based cohort of female nurses. We have three key findings. First, higher PTSD symptoms (i.e., endorsing four or more symptoms on the PTSD screen) were associated with increased risk of CVD incidence. Second, trauma exposure alone (endorsing no PTSD symptoms on the screen) was associated with elevated CVD risk. Third, adult health behaviors and medical risk factors accounted for an estimated 14% of the association of trauma/no symptoms with CVD and an estimated 47% of the association of trauma/4+ symptoms with CVD. Our findings suggest that elevated PTSD symptoms and trauma exposure may each be associated with poor cardiovascular health. To our knowledge, this is the first study in women to 1) predict CVD events confirmed by additional information or record review, 2) consider the effects of trauma exposure separately from PTSD, and 3) examine health behaviors and medical risk factors as potential mediators of the associations between trauma exposure, PTSD symptoms, and CVD incidence.
Overall, our results are consistent with the broader PTSD-CVD literature, including the only other study conducted in women.18 In the present study, CVD risk was highest for women endorsing 4 or more symptoms on the PTSD screen, a commonly-used cutoff for probable PTSD diagnosis.25 Effect sizes remained elevated and similar in magnitude in sensitivity analyses adjusting for CSA and depression before PTSD onset, suggesting that these results were not simply reflecting previously demonstrated effects of CSA or depression. Elevated PTSD symptoms were also associated with increased risk of MI and stroke incidence when we examined these outcomes separately. Trauma-exposed women endorsing 1–3 PTSD symptoms on the screen did not have significantly elevated risk of CVD compared to women with no trauma. This result was unexpected because some research has found subthreshold PTSD to be associated with physical health problems.42 The 95% CI for the HR for the trauma/1–3 symptoms group was wide, however, and included values greater than 1. Further research that assesses all PTSD symptom criteria using a clinical interview is needed to better understand associations of full and partial PTSD diagnoses with CVD.
Unlike most studies of PTSD and CVD, we examined associations of both trauma exposure and PTSD symptoms with CVD risk in a single investigation. Preliminary evidence in the literature suggests that trauma exposure is associated with physical health independent of psychopathology.43 Our finding that trauma exposure in women endorsing no PTSD symptoms was related to increased CVD risk is consistent with the notion that trauma exposure per se has negative health consequences, although additional risk factors are also likely at play. Furthermore, some researchers have suggested that trauma-exposed individuals who do not endorse any PTSD symptoms may engage in coping strategies (e.g., emotional suppression) that may generate physical distress and lead to negative physical health consequences,44 and our findings are congruent with this account. Although the NHS II data do not permit a detailed examination of this hypothesis, this would be of interest for further study. Overall, these results suggest that the effects of trauma on physical health may impact more than just those who develop PTSD symptoms. Nevertheless, more research is needed, particularly studies that assess multiple manifestations of posttraumatic psychopathology in order to account for alternative psychopathological responses to trauma that are not captured by PTSD.
Adult health behaviors and medical risk factors (including ADM use) accounted for an estimated 14% and 47% of the associations of trauma/no symptoms and trauma/4+ symptoms with CVD, respectively. Comprehensive investigations of the mechanisms linking PTSD to CVD are lacking,45 but previously we found that health behaviors and medical risk factors accounted for 60–80% of associations between childhood abuse and CVD incidence.4 Our findings suggest that health behavioral correlates explained some, but not all, of the trauma/no symptoms-CVD and trauma/4+ symptoms-CVD relations. Although measurement error could have attenuated these associations, additional mechanisms of risk are of interest for future study. Trauma exposure and PTSD are associated with dysregulation of the autonomic nervous system, hypothalamic-pituitary-adrenal axis, and inflammatory response, and subsequent changes in catecholamines, cortisol, and inflammatory cytokines may increase CVD risk.45 Research measuring changes in CVD-related biomarkers from before to after trauma exposure and PTSD onset will help elucidate biological mechanisms. Furthermore, although we accounted for several health behaviors, data were unavailable on additional behavioral correlates of PTSD that may contribute to CVD. For example, insomnia and poor sleep quality (e.g., due to nightmares) are common in PTSD, and sleep problems (e.g., daytime sleepiness) have been associated with CVD risk.46
This study has several limitations. We used retrospective assessment of trauma and PTSD symptoms, and the precision of reports—particularly regarding dating of traumatic experiences—may have been reduced. Furthermore, trauma history and PTSD symptoms were measured in 2008, after many CVD events occurred. Nevertheless, trauma exposure and PTSD symptoms were associated with elevated CVD risk when we analyzed CVD events occurring only after trauma/PTSD assessment. Another limitation is that PTSD symptoms were assessed with a screen that did not measure all diagnostic criteria. Thus, our results are not generalizable to clinical diagnoses. Additionally, because we twice lagged the primary exposure of trauma/PTSD in models to avoid effect-cause artifacts, some results might be underestimates if some of the effects of trauma and PTSD appear within a few years after trauma/PTSD onset. Further research examining the effects of time since trauma and PTSD duration with respect to CVD risk is needed.
Survivor bias is another concern because women needed to remain in the NHS II until 2008 to provide data on trauma and PTSD. Given that PTSD has been associated with increased mortality risk,5 our findings may underestimate the PTSD-CVD relation if those with (vs. without) PTSD were more likely to die prior to PTSD assessment. However, the death rate in the NHS II is low and unlikely to substantially influence estimates; 1.6% of the original sample (n=1,826) was deceased by the trauma and PTSD assessment in 2008. Nevertheless, results should be considered in light of this limitation. Additionally, the NHS II cohort is predominantly white and highly educated, which may limit the generalizability of findings. Furthermore, because women were aged 44–64 years at the end of follow-up, our results pertain to nonfatal early-onset CVD. Additional research on trauma, PTSD, and later onset CVD (including fatal events) is needed.
The current study also has several strengths that make it unlike previous investigations. It is based on a large-scale long-running cohort that is well-characterized with regard to CVD risk and risk-related factors. We also considered the effects of PTSD in community-dwelling women exposed to a range of traumas. Additionally, we 1) evaluated trauma and PTSD in relation to validated CVD events as confirmed by additional information or record review; 2) contrasted a no-trauma group with a trauma-exposed group endorsing no PTSD symptoms; and 3) incorporated longitudinal, repeated-measures data to estimate the impact of potential mediators. Thus, we believe that our findings have potential implications for treatment and prevention. Currently, neither the American Heart Association nor the American Stroke Association recognizes trauma or PTSD as risk factors for CVD,47 and there is no systematic approach for addressing CVD risk factors in trauma-exposed individuals with or without PTSD. Our findings, together with those in the literature, suggest that PTSD may be a modifiable risk factor for CVD. Additional research on the mechanisms underlying the relations between trauma, PTSD, and CVD will help to elucidate understanding of these associations. If research continues to demonstrate associations between trauma exposure, PTSD, and CVD incidence (particularly evidence for causal links), then assessing and monitoring cardiovascular function in trauma-exposed individuals and those with PTSD may have a positive public health impact and help to detect pre-clinical markers of cardiovascular dysfunction. Furthermore, it will be important to examine whether successful PTSD treatment has a positive impact on cardiovascular health. In sum, broadly recognizing that trauma and PTSD, which are public health concerns in their own right, have more far-reaching effects on physical health than previously thought may begin to inform public health interventions aimed at reducing risk of CVD, the leading cause of morbidity and mortality.
Supplementary Material
Acknowledgments
We acknowledge the Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital, and Harvard Medical School for managing the NHS II.
Funding Sources: This study was supported by the National Institutes of Health grants R01MH101269-01A1 (to KCK, LDK) and UM1CA176726 (for NHS II infrastructure).
Footnotes
Disclosures: None.
References
- 1.Mozaffarian D, Wilson PW, Kannel WB. Beyond established and novel risk factors lifestyle risk factors for cardiovascular disease. Circulation. 2008;117:3031–3038. doi: 10.1161/CIRCULATIONAHA.107.738732. [DOI] [PubMed] [Google Scholar]
- 2.Towfighi A, Zheng L, Ovbiagele B. Sex-specific trends in midlife coronary heart disease risk and prevalence. Arch Intern Med. 2009;169:1762–1766. doi: 10.1001/archinternmed.2009.318. [DOI] [PubMed] [Google Scholar]
- 3.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Rich-Edwards JW, Mason S, Rexrode K, Spiegelman D, Hibert E, Kawachi I, Jun HJ, Wright RJ. Physical and sexual abuse in childhood as predictors of early-onset cardiovascular events in women. Circulation. 2012;126:920–927. doi: 10.1161/CIRCULATIONAHA.111.076877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boscarino JA. A prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: implications for surveillance and prevention. Psychosom Med. 2008;70:668–676. doi: 10.1097/PSY.0b013e31817bccaf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 7.Pacella ML, Hruska B, Delahanty DL. The physical health consequences of PTSD and PTSD symptoms: a meta-analytic review. J Anxiety Disord. 2013;27:33–46. doi: 10.1016/j.janxdis.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Heath NM, Chesney SA, Gerhart JI, Goldsmith RE, Luborsky JL, Stevens NR, Hobfoll SE. Interpersonal violence, PTSD, and inflammation: potential psychogenic pathways to higher C-reactive protein levels. Cytokine. 2013;63:172–178. doi: 10.1016/j.cyto.2013.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maia DB, Marmar CR, Mendlowicz MV, Metzler T, Nóbrega A, Peres MC, Coutinho ES, Volchan E, Figueira I. Abnormal serum lipid profile in Brazilian police officers with post-traumatic stress disorder. J Affect Disord. 2008;107:259–263. doi: 10.1016/j.jad.2007.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qureshi SU, Pyne JM, Magruder KM, Schulz PE, Kunik ME. The link between post-traumatic stress disorder and physical comorbidities: a systematic review. Psychiat Quart. 2009;80:87–97. doi: 10.1007/s11126-009-9096-4. [DOI] [PubMed] [Google Scholar]
- 11.Pratchett LC, Pelcovitz MR, Yehuda R. Trauma and violence: are women the weaker sex? Psychiat Clin N Am. 2010;33:465–474. doi: 10.1016/j.psc.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Papakonstantinou NA, Stamou MI, Baikoussis NG, Goudevenos J, Apostolakis E. Sex differentiation with regard to coronary artery disease. J Cardiol. 2013;62:4–11. doi: 10.1016/j.jjcc.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Jordan HT, Miller-Archie SA, Cone JE, Morabia A, Stellman SD. Heart disease among adults exposed to the September 11, 2001 World Trade Center disaster: results from the World Trade Center Health Registry. Prev Med. 2011;53:370–376. doi: 10.1016/j.ypmed.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 14.Jordan HT, Stellman SD, Morabia A, Miller-Archie SA, Alper H, Laskaris Z, Brackbill RM, Cone JE. Cardiovascular disease hospitalizations in relation to exposure to the September 11, 2001 World Trade Center disaster and posttraumatic stress disorder. J Am Heart Assoc. 2013;2:e000431. doi: 10.1161/JAHA.113.000431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kubzansky LD, Koenen KC, Spiro A, III, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Arch Gen Psychiatry. 2007;64:109–116. doi: 10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- 16.Scherrer JF, Chrusciel T, Zeringue A, Garfield LD, Hauptman PJ, Lustman PJ, Freedland KE, Carney RM, Bucholz KK, Owen R. Anxiety disorders increase risk for incident myocardial infarction in depressed and nondepressed Veterans Administration patients. Am Heart J. 2010;159:772–779. doi: 10.1016/j.ahj.2010.02.033. [DOI] [PubMed] [Google Scholar]
- 17.Vaccarino V, Goldberg J, Rooks C, Shah AJ, Veledar E, Faber TL, Votaw JR, Forsberg CW, Bremner JD. Post-traumatic stress disorder and incidence of coronary heart disease: a twin study. J Am Coll Cardiol. 2013;62:970–978. doi: 10.1016/j.jacc.2013.04.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kubzansky LD, Koenen KC, Jones C, Eaton WW. A prospective study of posttraumatic stress disorder symptoms and coronary heart disease in women. Health Psychol. 2009;28:125–130. doi: 10.1037/0278-6133.28.1.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koenen KC, Stellman SD, Sommer JF, Stellman JM. Persisting posttraumatic stress disorder symptoms and their relationship to functioning in vietnam veterans: a 14-year follow-up. J Trauma Stress. 2008;21:49–57. doi: 10.1002/jts.20304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perkonigg A, Owashi T, Stein MB, Kirschbaum C, Wittchen H-U. Posttraumatic stress disorder and obesity: evidence for a risk association. Am J Prev Med. 2009;36:1–8. doi: 10.1016/j.amepre.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 21.Zen AL, Whooley MA, Zhao S, Cohen BE. Post-traumatic stress disorder is associated with poor health behaviors: findings from the heart and soul study. Health Psychol. 2012;31:194–201. doi: 10.1037/a0025989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morgan CA, Hazlett G, Wang S, Richardson EG, Schnurr P, Southwick SM. Symptoms of dissociation in humans experiencing acute, uncontrollable stress: a prospective investigation. Am J Psychiat. 2001;158:1239–1247. doi: 10.1176/appi.ajp.158.8.1239. [DOI] [PubMed] [Google Scholar]
- 23.Schnurr PP, Vieilhauer MJ, Weathers F, Findler M. The Brief Trauma Questionnaire. White River Junction, VT: National Center for PTSD; 1999. [Google Scholar]
- 24.Schnurr PP, Spiro A, III, Vielhauer MJ, Findler MN, Hamblen JL. Trauma in the lives of older men: findings from the Normative Aging Study. J Clin Geropsych. 2002;8:175–187. [Google Scholar]
- 25.Breslau N, Peterson EL, Kessler RC, Schultz LR. Short screening scale for DSM-IV posttraumatic stress disorder. Am J Psychiat. 1999;156:908–911. doi: 10.1176/ajp.156.6.908. [DOI] [PubMed] [Google Scholar]
- 26.Rose GA, Blackburn H. Cardiovascular Survey Methods. Geneva, Switzerland: World Health Organization; 2002. [PubMed] [Google Scholar]
- 27.Walker A, Robins M, Weinfeld F. The National Survey of Stroke: clinical findings. Stroke. 1981;12(suppl):I-13–I-44. [PubMed] [Google Scholar]
- 28.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–473. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142:1009–1018. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kothari V, Stevens RJ, Adler AI, Stratton IM, Manley SE, Neil HA, Holman RR. UKPDS 60: risk of stroke in type 2 diabetes estimated by the UK Prospective Diabetes Study risk engine. Stroke. 2002;33:1776–1781. doi: 10.1161/01.str.0000020091.07144.c7. [DOI] [PubMed] [Google Scholar]
- 31.Nelson HD, Humphrey LL, Nygren P, Teutsch SM, Allan JD. Postmenopausal hormone replacement therapy. JAMA. 2002;288:872–881. doi: 10.1001/jama.288.7.872. [DOI] [PubMed] [Google Scholar]
- 32.Psaty BM, Furberg CD, Kuller LH, Cushman M, Savage PJ, Levine D, O’Leary DH, Bryan RN, Anderson M, Lumley T. Association between blood pressure level and the risk of myocardial infarction, stroke, and total mortality: the cardiovascular health study. Arch Intern Med. 2001;161:1183–1192. doi: 10.1001/archinte.161.9.1183. [DOI] [PubMed] [Google Scholar]
- 33.Friedman MJ, Davidson JRT. Pharmacotherapy for PTSD. In: Friedman MJ, Keane TM, Resisk PA, editors. Handbook of PTSD: Science and Practicei. New York, NY: Guilford Press; 2007. pp. 376–405. [Google Scholar]
- 34.Smoller JW, Allison M, Cochrane BB, Curb JD, Perlis RH, Robinson JG, Rosal MC, Wenger NK, Wassertheil-Smoller S. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women’s Health Initiative study. JAMA. 2009;169:2128–2139. doi: 10.1001/archinternmed.2009.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whang W, Kubzansky LD, Kawachi I, Rexrode KM, Kroenke CH, Glynn RJ, Garan H, Albert CM. Depression and risk of sudden cardiac death and coronary heart disease in women: Results from the Nurses’ Health Study. J Am Coll Cardiol. 2009;53:950–958. doi: 10.1016/j.jacc.2008.10.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gallup G, Moore D, Schussel R. Disciplining Children in America: A Gallup Poll Report. Princeton, NJ: The Gallup Organization; 1995. [Google Scholar]
- 37.Straus MA, Gelles RG. Physical violence in American families: Risk factors and adaptations to violence in 8.145 families. New Brunswick, NJ: Transaction Publishers; 1990. [Google Scholar]
- 38.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 39.The SAS mediate macro [computer program] Boston: Brigham and Women’s Hospital, Channing Laboratory; 2009. [Google Scholar]
- 40.Lin DY, Fleming TR, De Gruttola V. Estimating the proportion of treatment effect explained by surrogate marker. Stat Med. 1997;16:1515–1527. doi: 10.1002/(sici)1097-0258(19970715)16:13<1515::aid-sim572>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 41.Erickson DJ, Wolfe J, King DW, King LA, Sharkansky EJ. Posttraumatic stress disorder and depression symptomatology in a sample of Gulf War veterans: a prospective analysis. J Consult Clin Psych. 2001;69:41–49. doi: 10.1037//0022-006x.69.1.41. [DOI] [PubMed] [Google Scholar]
- 42.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Medical comorbidity of full and partial posttraumatic stress disorder in US adults: Results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom Med. 2011;73:697–707. doi: 10.1097/PSY.0b013e3182303775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Scott KM, Koenen KC, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, Caldas-de-Almeida JM, de Girolamo G, Florescu S. Associations between lifetime traumatic events and subsequent chronic physical conditions: a cross-national, cross-sectional study. PLoS One. 2013;8:e80573. doi: 10.1371/journal.pone.0080573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.D’Andrea W, Sharma R, Zelechoski AD, Spinazzola J. Physical health problems after single trauma exposure: When stress takes root in the body. J Am Psychiatr Nurses Assoc. 2011;17:378–392. doi: 10.1177/1078390311425187. [DOI] [PubMed] [Google Scholar]
- 45.Edmondson D, Cohen BE. Posttraumatic stress disorder and cardiovascular disease. Prog Cardiovasc Dis. 2013;55:548–556. doi: 10.1016/j.pcad.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boden-Albala B, Roberts ET, Bazil C, Moon Y, Elkind MS, Rundek T, Paik MC, Sacco RL. Daytime sleepiness and risk of stroke and vascular disease findings from the Northern Manhattan Study (NOMAS) Circ Cardiovasc Qual Outcomes. 2012;5:500–507. doi: 10.1161/CIRCOUTCOMES.111.963801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.American Stroke Association. [Accessed April 20, 2015];Converging risk factors for stroke. 2014 http://www.strokeassociation.org/STROKEORG/LifeAfterStroke/HealthyLivingAfterStroke/UnderstandingRiskyConditions/Converging-Risk-Factors-for-Stroke_UCM_310319_Article.jsp.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.