Abstract
Context
This systematic review evaluated the evidence on the impact of family planning reminder systems—interventions intended to remind patients of behaviors to achieve reproductive health goals (e.g., daily text messages reminding oral contraceptive [OC] users to take a pill)—to provide information to guide national recommendations on quality family planning services.
Evidence acquisition
Multiple databases including PubMed were searched during 2010–2011 for peer-reviewed articles published in English from January 1985 through February 2011 describing studies evaluating reminder systems to improve family planning outcomes. Studies were excluded if they focused primarily on HIV or sexually transmitted infection prevention, focused solely on men, or were conducted outside the U.S., Europe, Australia, or New Zealand.
Evidence synthesis
The initial search identified 16,129 articles, five of which met the inclusion criteria. Three studies examined the impact of OC reminder systems; two found a statistically significant positive impact on correct use. Two studies examined the impact of reminder systems among depot medroxyprogesterone acetate (DMPA) users; one found a statistically significant positive impact on correct use.
Conclusions
Although mixed support was found for the effectiveness of reminder system interventions on correct use of OCs and DMPA, the highest-quality evidence yielded null findings. The evidence base would be strengthened by the development of additional studies, especially RCTs, which objectively measure outcomes, examine additional contraceptive methods, and have sufficient sample sizes to detect behavioral outcomes at least 12 months post-intervention.
Introduction
Most unintended pregnancies are preventable with correct and continued contraceptive use, yet nearly half of pregnancies in the U.S. are unintended.1 Contraceptive methods that are user-dependent—for example, hormonal contraceptives including oral contraceptives, injectables (e.g., depot medroxyprogesterone acetate [DMPA]), and condoms—require adherence by users to ensure the method’s effectiveness. Therefore, typical use failure rates for user-dependent methods are substantially higher than perfect-use failure rates.2 It is estimated that approximately 40% of unintended pregnancies occur among women who used their contraceptive method inconsistently or incorrectly.3
Non-adherence with combined hormonal contraceptive regimens (i.e., not taking oral contraceptives as prescribed) increases the risk of ovulation4 as well as side effects such as bleeding irregularities that may lead to discontinuation5 and periods of non-contraceptive coverage. DMPA users must also maintain regular dosing schedules because injections must be given within 14 weeks of a previous injection to ensure effective contraceptive action. Condoms are highly user-dependent and require use during each act of intercourse during fertile periods to protect against unintended pregnancy. Given the importance of correct and continued contraceptive use to prevent unintended pregnancy and reduce the occurrence of side effects and other negative reproductive health outcomes, it is important to identify interventions that can improve family planning behaviors and effectiveness. Family planning reminder systems—interventions intended to remind patients of some behavior to achieve a reproductive health goal, such as taking a pill, attending a clinic visit to receive a DMPA injection, or using a condom—are promising approaches.
The objective of this systematic review was to summarize the evidence on the impact of reminder system interventions in clinical settings to improve family planning outcomes to guide national recommendations on quality family planning services. The information was presented to an expert technical panel in May 2011 at a meeting convened by the Office of Population Affairs and CDC.
Evidence Acquisition
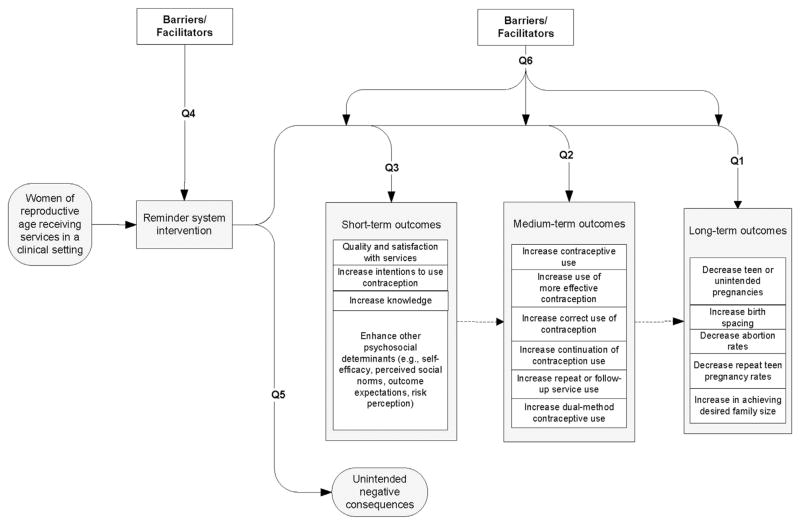
The methods for conducting this systematic review have been described elsewhere.6 In summary, six key questions were developed (Table 1) and an analytic framework applied to show the logical relationships among the population of interest (women of reproductive age receiving services in a clinical setting); the reminder system intervention; and the long-, medium-, and short-term outcomes of interest (Figure 1). Search strategies were then developed that included the identification of key terms (Appendix A), which were used to search multiple electronic databases (Appendix B), including PubMed, during 2010–2011 to identify potential articles. A targeted search was rerun in March 2015 to identify articles published since the initial search. Studies were not considered if they focused primarily on prevention of HIV or sexually transmitted infections (STIs); focused solely on men; or were conducted outside the U.S., Europe, Australia, or New Zealand.
Table 1.
Key Questions for Systematic Review on Impact of Reminder Systems in Clinical Settings
| Key question no. | Question |
|---|---|
| 1 | Is there a relationship between the utilization of reminder systems and improved long-term outcomes of family planning services (e.g., decreased teen or unintended pregnancies, increased birth spacing, decreased abortion rates, decreased repeat teen pregnancy rates, or unintended pregnancy rates)? |
| 2 | Is there a relationship between the utilization of reminder systems and improved medium-term outcomes of family planning services (e.g., increased contraceptive use; increased use of more effective contraception; increased correct use of contraception; increased continuation of contraception use; increased repeat, or follow-up, service use)? |
| 3 | Is there a relationship between the utilization of reminder systems and improved short-term outcomes of family planning services (e.g., improved quality and satisfaction with service, strengthened social norms, improved intentions to use contraception, increased knowledge, enhanced other psychosocial determinants of contraceptive use)? |
| 4 | What are the barriers and facilitators for clinics to offering reminder systems in the family planning setting? |
| 5 | Are there any unintended negative consequences associated with offering reminder systems in the family planning setting? |
| 6 | What are the barriers and facilitators for clients to achieving positive outcomes after utilizing reminder systems in the family planning setting? |
Note: Questions are put into context using the analytic framework presented in Figure 1.
Figure 1.
Analytic framework for systematic review on the impact of reminder systems in clinical settings to improve family planning outcomes.
Note: Numbered lines map to key questions (Q). Dashed lines show logical relationships between outcomes, but these relationships were not assessed in this systematic review.
Selection of Studies
Retrieval and inclusion criteria were developed a priori and applied to the search results. Articles were retrieved if they were published in English from January 1, 1985, through February 28, 2011. These articles were then reviewed to assess if they had evaluated at least one of the six key questions. Articles also must have evaluated a reminder system intervention in a clinic-based setting where family planning services were provided. For Key Questions 1–3, which sought to examine the relationships between utilization of reminder systems and improved long-, medium-, and short-term outcomes, studies had to include a comparison group. For Key Questions 4–6, which sought to examine unintended negative consequences and barriers and facilitators for clinics offering reminder systems, or clients achieving positive outcomes after utilizing reminder systems, articles had to describe a study that examined the impact of a reminder system on at least one outcome of interest and met the inclusion criteria for Key Questions 1–3.
Assessment of Study Quality and Synthesis of Data
The quality of each piece of evidence identified by the initial search was assessed by two investigators independently using the grading system developed by the U.S. Preventive Services Task Force.7 Each reminder system intervention was evaluated on its level of intensity using a definition developed for this review. Interventions that took place once were classified as low intensity, those that occurred more than once but less frequently than weekly were classified as moderate intensity, and those that occurred weekly were classified as high intensity. As different types of reminder systems are appropriate for different contraceptive methods, findings are reported by contraceptive method. Findings are also stratified by outcome of interest; as such, studies that examined multiple outcomes may be discussed more than once. Summary measures of association were not computed across studies because of the diversity of the interventions, study designs, and populations. Articles published since the initial search were not incorporated into the evidence table because we wanted to only include information considered during the May 2011 expert technical panel to guide national recommendations on quality family planning services.
Evidence Synthesis
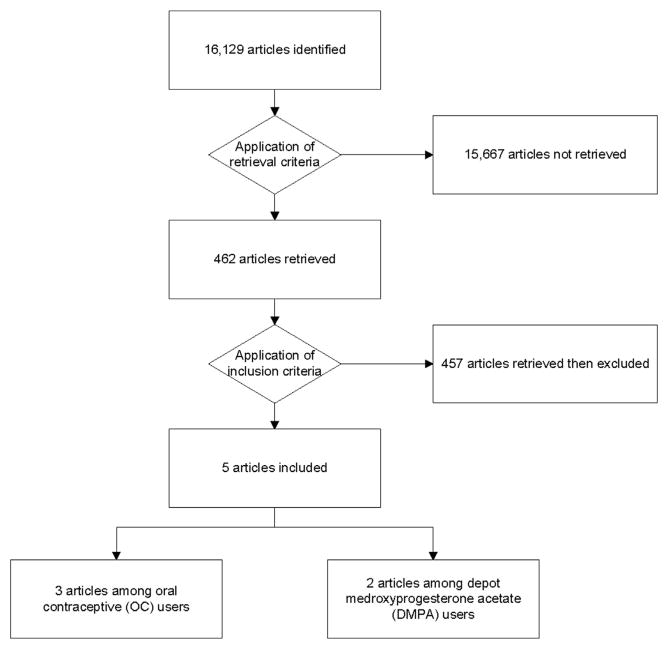
The initial search strategy identified 16,129 articles (Figure 2). After applying the retrieval criteria, 462 articles were retrieved for closer review. Of these, five articles8–12 met the inclusion criteria (Appendix C). Excluded studies were mainly those not relevant to the six key questions. Of the five studies included in this review, three8,9,11 examined the impact of reminder systems among oral contraceptive users and two10,12 examined the impact among DMPA users.
Figure 2.
Flow chart of study selection.
Oral Contraceptive Users
Of the three studies that examined the impact of reminder systems among oral contraceptive users, one was an RCT9 rated as having moderate risk for bias, one was a retrospective, historic, non-randomized controlled trial8 rated as having high risk for bias, and one was a cohort study11 rated as having high risk for bias. All three studies8,9,11 examined medium-term outcomes, and two studies8,9 also examined barriers facing clients. None of the studies examined long-term outcomes, short-term outcomes, or unintended negative consequences associated with offering reminder system interventions.
Sample sizes in the three studies were 82,9 153,8 and 975.11 Two studies8,9 reported the ages of participants, which ranged from 18 to 37 years. Two studies9,11 recruited participants from health clinics, and one study8 recruited participants through flyer and newspaper advertisements. A different reminder system intervention was used in each of the three studies. One used daily e-mail messages,8 one used daily text messages,9 and one distributed a credit card–sized device that emitted an audible beep to aid in establishing a daily pill-taking routine.11 All three reminder system interventions were rated as high intensity.8,9,11 Appendix C describes the details of each study.
The three studies8,9,11 among oral contraceptive users that examined the impact of reminder systems on medium-term outcomes investigated correct use (i.e., no missed hormonal pills), with two8,11 finding a statistically significant impact. In one of these studies,8 a retrospective, historic, non-randomized controlled trial of 153 sexually active women, perfect oral contraceptive adherence (assessed using diary cards) was significantly (p<0.05) higher during three cycles of pill use among intervention participants (n=50) who received daily reminder e-mail messages on adherence than among women in a historic reference group (n=103) who received no reminders (78% vs 58% during Cycle 1, 80% vs 59% during Cycle 2, and 72% vs 53% during Cycle 3). In the second study,11 a cohort study of 975 women, intervention participants (n=485) received a credit card–sized reminder device that emitted a daily audible beep to establish a pill-taking routine and were compared with control participants (n=490) who received no reminder device. Perfect oral contraceptive adherence during the preceding 3 months was significantly (p<0.005) higher among intervention (41%) versus control (19%) participants; adherence was assessed using a survey completed at 3- to 6-month follow-up. The third study, an RCT of 82 women that used electronic monitoring devices to assess adherence, found no statistically significant effect of daily reminder text messages on the number of missed pills per cycle over 4 months of follow-up.9
Two studies examined barriers for clients to achieving positive outcomes after utilizing reminder systems in family planning settings.8,9 The first—a retrospective, historic, non-randomized controlled trial that included 50 intervention women who received daily reminder e-mail messages at approximately 8:30AM each day to promote oral contraceptive adherence—reported that participants noted that the reminders would have been more helpful if the timing that the e-mail messages were sent could have been individualized to their preferred pill-taking schedule.8 Furthermore, although the majority (64%) of intervention participants wished to continue receiving the daily e-mail reminders, only 25% were willing to pay $5.00–$10.00 per month for the service. In the second study,9 an RCT that included 37 intervention women who received daily text messages on oral contraceptive adherence, cost of the service was also a barrier for continuing to use the reminder system. Although >85% of participants expressed that they would continue or consider continuing to use the reminder system, 43% would not pay for the service and 57% stated that they would pay a median acceptable cost of $5.00 per month for the service.
Depot Medroxyprogesterone Acetate Users
Of the two studies that examined the impact of reminder systems among DMPA users, one was an RCT10 rated as having moderate risk for bias and the other was a retrospective cohort study12 rated as having high risk for bias. Both studies10,12 examined medium-term outcomes, and one study10 also examined barriers facing clinics. None of the studies examined long-term outcomes, short-term outcomes, or unintended negative consequences associated with offering reminder system interventions.
Sample sizes in the two studies were 18412 and 207,10 with the mean age of participants being 21 and 23 years, respectively. One study10 recruited participants from a health clinic, and the other12 conducted a chart review to identify DMPA users before and after implementation of a clinic-level intervention. A different reminder system was used in each of the studies. One10 sent a reminder letter 2 weeks before an upcoming injection appointment and made repeated phone calls to participants if they missed the appointment. The other12 distributed a wallet-sized reminder card with the date of the next DMPA injection and sent a reminder postcard shortly before an upcoming injection appointment. One study10 was rated as having variable intensity, and the other12 was rated as moderate intensity. Appendix C describes the details of each study.
The two studies10,12 among DMPA users that examined the impact of reminder systems on medium-term outcomes investigated correct use (i.e., timely DMPA injections), and one10 also examined continuation of DMPA use over time. Of the two studies that examined correct use, one12 found a statistically significant positive impact of receiving a wallet-sized reminder card with the date of the next DMPA injection and a reminder postcard shortly before the next injection appointment on timely DMPA injections. In this retrospective cohort study conducted via chart review of 184 DMPA users aged 13–50 years, women were compared before and after clinic implementation of the reminder system intervention (the number of women in the intervention and control groups was not stated). The intervention was significantly (p<0.05) associated with improvement in timeliness of the next DMPA injection, with 64% of injections received on time before the intervention versus 76% after the intervention. Furthermore, the mean number of days late for an injection significantly (p<0.05) decreased from 20 days late to 8 days late before versus after the intervention. The other study was an RCT of 207 DMPA users, some of whom received a reminder letter 2 weeks prior to the upcoming injection appointment and repeated phone calls if an appointment was missed; rates of late and missed injections over 12 months of follow-up were similar between groups (data not shown).10 This study also examined continuation of DMPA use over time and did not find a statistically significant effect; forty-three percent of intervention participants continued DMPA use through 12-month follow-up versus 45% of control participants who received only a written appointment card at initial visit and no reminder letter or phone calls. Although DMPA side effects were thought to be a main reason for discontinuation, the percentage of women reporting side effects did not differ between those who chose to continue DMPA (82%) and those who did not (84%).
One study,10 the RCT that examined correct and continued use of DMPA among women receiving a reminder letter 2 weeks prior to the upcoming injection appointment and repeated phone calls if an appointment was missed, examined barriers for clinics to offering reminder systems in family planning settings. In this study, the authors reported that the reminder system was intensive, often involving multiple phone calls and facilitation of appointment scheduling, and would not easily be incorporated into most office settings.
Discussion
This systematic review identified five studies that examined the impact of reminder system interventions in clinical settings on family planning outcomes and met the inclusion criteria.8–12 Three studies8,9,11 examined the impact of daily reminder systems on correct use of oral contraceptives and found inconsistent findings. Two of the studies (both rated as having high risk for bias)—a retrospective, historic, non-randomized controlled trial that examined daily e-mail messages8 and a cohort study that examined use of a small reminder device that emitted a daily audible beep11—found a statistically significant positive impact of the reminder system on perfect oral contraceptive adherence (assessed via self-report) during three cycles of pill use. However, the third study,9 which had a stronger design (RCT), was rated as having moderate risk for bias and used a more objective measure of adherence—an electronic monitoring device that sent a wireless signal each time participants opened the device to remove a pill—found no significant impact of daily text messages on oral contraceptive adherence over 3 months. Evidence suggests that women’s self-reported pill-taking behavior lacks validity and overestimates perfect adherence compared with electronic monitoring devices.9,13
Two studies10,12 examined the impact of reminder systems on correct use of DMPA and found inconsistent findings. One study12 rated as having high risk for bias found a statistically significant impact of receiving a wallet-sized reminder card with the date of the next DMPA injection and a reminder postcard shortly before the next injection appointment. However, the other study,10 which had a stronger design (RCT), was rated as having moderate risk for bias, and assessed timeliness of DMPA injections over a longer period of follow-up (12 versus 3 months), found no significant effect of receiving a reminder letter 2 weeks prior to the upcoming injection appointment and repeated phone calls if an appointment was missed. The one study10 that examined the impact of a reminder system on continued use of DMPA did not find a statistically significant positive effect of the intervention on DMPA continuation rates at a 12-month follow-up.
Three studies8–10 included in this systematic review examined either barriers for clients to achieving positive outcomes after utilizing reminder systems or barriers for clinics to offering reminder systems. Barriers for clients included costs associated with using the reminder system8,9 and not being able to individualize the time the reminder message was received.8 However, one study9 in this systematic review that did allow participants to choose the time the reminder message was received did not find a significant positive impact of the intervention. Barriers for clinics included reminder systems that were too intensive to easily be incorporated into most office settings (e.g., repeated phone calls).10
The effect of reminder systems in other areas of health behavior has been reported. Personal reminders such as telephone calls or e-mails from healthcare providers to patients have been shown to improve medication adherence rates for chronic disorders (e.g., hypertension),14,15 as have electronic reminders automatically sent without personal contact between the healthcare provider and patient.16 Several studies17–20 from the HIV literature have found reminder systems to significantly improve medication adherence among HIV-infected individuals. Evidence also suggests that text message reminders significantly improve attendance at upcoming healthcare appointments for ongoing care21 and pediatric and adolescent immunizations.22
It may be that reminder systems to improve adherence with taking medications for health conditions that pose a risk to life may be more effective. Women often have ambivalent feelings or conflicted desire toward pregnancy and having a baby,23 which may influence correct and continued contraceptive use irrespective of reminder systems. Whereas forgetfulness is a common reason reported for non-adherence to medications being used to treat medical disorders,16 contraceptive behaviors are influenced by a complex host of factors, including personal feeling and beliefs, concerns about side effects, partner influences, cultural values and norms, and healthcare system issues.3
Limitations
The evidence summarizing the impact of reminder systems in clinical settings to improve family planning outcomes has several limitations, which should be considered when interpreting the evidence. Of the five studies included in this review, none were determined to have a low risk for bias (i.e., high quality), and three8,11,12 were determined to have a high risk for bias (i.e., low quality). Studies were considered to be at risk for bias because of selection bias,8–11 self-report bias,8,11 recall bias,11 or short follow-up times for behavioral outcomes.8,9,11,12 Participation rates were not reported in two studies.10,11 Some studies failed to report comparability between study groups8,12 and one11 included study groups that appeared to differ related to important background and reproductive health characteristics, limiting the ability to definitely attribute outcomes to the reminder system. Attrition bias was also an issue for some studies; one11 did not report the percentage of participants completing the study, and two8,12 did not report the comparability between participants who completed and did not complete the study. Among the included trials, primary weaknesses included not reporting investigator blinding10 and possible study reactivity,8–10 a type of information bias in trials where the outcome under investigation improves in participants who are aware of being observed.24
Despite these limitations, the evidence base for the impact of reminder system interventions in clinical settings on family planning outcomes also has several strengths. Two of five studies in this review were RCTs,9,10 both of which used computer-generated randomization for group assignment9,10; investigators were also blinded to group assignment in one RCT.9 One study10 followed participants for 12 months. Other strengths included high participation and completion rates,9 small differences in follow-up rates between study groups,9 and study groups with similar baseline characteristics.9,10 One study9 used an objective measurement of oral contraceptive adherence (i.e., electronic monitoring devices), and two studies10,12 validated information on continuation of DMPA using clinic records.
Additional articles meeting the inclusion criteria for this systematic review have been published since our initial search of the literature. A targeted search was rerun in PubMed in March 2015 and identified two newly published articles25,26 from one RCT that examined the effect of 180 daily educational text messages on knowledge about oral contraceptives and continuation of use at 6 months. This RCT found modest positive effects of the intervention on mean knowledge scores26 and self-reported continuation rates at 6 months.25
Conclusions
Although this review found mixed support for the effectiveness of reminder system interventions on correct use of oral contraceptives and DMPA, the highest-quality evidence yielded null findings and did not support the effectiveness of such interventions. There was no evidence to support the effectiveness of reminder systems on DMPA continuation rates, and no included studies (from the initial search) examined the effect of reminder systems on oral contraceptive continuation rates. There is such limited evidence available on the impact of reminder systems that it is difficult to draw conclusions about when and for whom they might be effective. Along with expert feedback and findings from two other complementary systematic reviews on the impact of contraceptive counseling27 and education28 in family planning programs, the information was used to develop recommendations for providing quality contraceptive counseling in the 2014 “Providing Quality Family Planning Services.”29 The evidence base on the impact of reminder systems in clinical settings to improve family planning outcomes would be strengthened by the development of additional studies, especially RCTs, which objectively measure outcomes, examine additional contraceptive methods, and have sample sizes that are large enough to detect behavioral outcomes at least 12 months post-intervention.
Supplementary Material
Acknowledgments
Publication of this article was supported by the U.S. Centers for Disease Control and Prevention (CDC) and the Office of Population Affairs (OPA).
Appendix. Supplementary data
Supplementary data associated with this article can be found at http://dx.doi.org/10.1016/j.amepre.2015.03.018.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC or the Office of Population Affairs.
No financial disclosures were reported by the authors of this paper.
References
- 1.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478–485. doi: 10.1016/j.contraception.2011.07.013. http://dx.doi.org/10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404. doi: 10.1016/j.contraception.2011.01.021. http://dx.doi.org/10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frost JJ, Darroch JE, Remez L. Improving contraceptive use in the United States. Issues Brief (Alan Guttmacher Inst) 2008;(1):1–8. [PubMed] [Google Scholar]
- 4.Zapata LB, Steenland MW, Brahmi D, Marchbanks PA, Curtis KM. Effect of missed combined hormonal contraceptives on contraceptive effectiveness: a systematic review. Contraception. 2013;87(5):685–700. doi: 10.1016/j.contraception.2012.08.035. http://dx.doi.org/10.1016/j.contraception.2012.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: a prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998;179(3 pt 1):577–582. doi: 10.1016/s0002-9378(98)70047-x. http://dx.doi.org/10.1016/S0002-9378(98)70047-X. [DOI] [PubMed] [Google Scholar]
- 6.Tregear SJ, Gavin LE, Williams JR. Systematic review evidence methodology: providing quality family planning services. Am J Prev Med. 2015;49(2S1):S23–S30. doi: 10.1016/j.amepre.2015.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris RP, Helfand M, Woolf SH, et al. Current methods of the U.S. Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(suppl 3):21–35. doi: 10.1016/s0749-3797(01)00261-6. http://dx.doi.org/10.1016/S0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 8.Fox MC, Creinin MD, Murthy AS, Harwood B, Reid LM. Feasibility study of the use of a daily electronic mail reminder to improve oral contraceptive compliance. Contraception. 2003;68(5):365–371. doi: 10.1016/j.contraception.2003.08.013. http://dx.doi.org/10.1016/j.contraception.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Hou MY, Hurwitz S, Kavanagh E, Fortin J, Goldberg AB. Using daily text-message reminders to improve adherence with oral contraceptives: a randomized controlled trial. Obstet Gynecol. 2010;116(3):633–640. doi: 10.1097/AOG.0b013e3181eb6b0f. http://dx.doi.org/10.1097/AOG.0b013e3181eb6b0f. [DOI] [PubMed] [Google Scholar]
- 10.Keder LM, Rulin MC, Gruss J. Compliance with depot medroxyprogesterone acetate: a randomized, controlled trial of intensive reminders. Am J Obstet Gynecol. 1998;179(3 pt 1):583–585. doi: 10.1016/s0002-9378(98)70048-1. http://dx.doi.org/10.1016/S0002-9378(98)70048-1. [DOI] [PubMed] [Google Scholar]
- 11.Lachowsky M, Levy-Toledano R. Improving compliance in oral contraception: “the reminder card”. Eur J Contracept Reprod Health Care. 2002;7(4):210–215. http://dx.doi.org/10.1080/ejc.7.4.210.215. [PubMed] [Google Scholar]
- 12.Madlon-Kay DJ. The effectiveness of a mail reminder system for depot medroxyprogesterone injections. Arch Fam Med. 1996;5(4):234–236. doi: 10.1001/archfami.5.4.234. http://dx.doi.org/10.1001/archfami.5.4.234. [DOI] [PubMed] [Google Scholar]
- 13.Potter L, Oakley D, de Leon-Wong E, Canamar R. Measuring compliance among oral contraceptive users. Fam Plann Perspect. 1996;28(4):154–158. http://dx.doi.org/10.2307/2136191. [PubMed] [Google Scholar]
- 14.Marquez Contreras E, Vegazo Garcia O, Martel Claros N, et al. Efficacy of telephone and mail intervention in patient compliance with antihypertensive drugs in hypertension. ETECUM-HTA study. Blood Press. 2005;14(3):151–158. doi: 10.1080/08037050510008977. http://dx.doi.org/10.1080/08037050510008977. [DOI] [PubMed] [Google Scholar]
- 15.Waalen J, Bruning AL, Peters MJ, Blau EM. A telephone-based intervention for increasing the use of osteoporosis medication: a randomized controlled trial. Am J Manag Care. 2009;15(8):e60–e70. [PubMed] [Google Scholar]
- 16.Vervloet M, Linn AJ, van Weert JC, de Bakker DH, Bouvy ML, van Dijk L. The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literature. J Am Med Inform Assoc. 2012;19(5):696–704. doi: 10.1136/amiajnl-2011-000748. http://dx.doi.org/10.1136/amiajnl-2011-000748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dowshen N, Kuhns LM, Johnson A, Holoyda BJ, Garofalo R. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: a pilot study using personalized, interactive, daily text message reminders. J Med Internet Res. 2012;14(2):e51. doi: 10.2196/jmir.2015. http://dx.doi.org/10.2196/jmir.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.da Costa TM, Barbosa BJ, Gomes e Costa DA, et al. Results of a randomized controlled trial to assess the effects of a mobile SMS-based intervention on treatment adherence in HIV/AIDS-infected Brazilian women and impressions and satisfaction with respect to incoming messages. Int J Med Inform. 2012;81(4):257–269. doi: 10.1016/j.ijmedinf.2011.10.002. http://dx.doi.org/10.1016/j.ijmedinf.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardy H, Kumar V, Doros G, et al. Randomized controlled trial of a personalized cellular phone reminder system to enhance adherence to antiretroviral therapy. AIDS Patient Care STDS. 2011;25(3):153–161. doi: 10.1089/apc.2010.0006. http://dx.doi.org/10.1089/apc.2010.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodrigues R, Shet A, Antony J, et al. Supporting adherence to antiretroviral therapy with mobile phone reminders: results from a cohort in South India. PLoS One. 2012;7(8):e40723. doi: 10.1371/journal.pone.0040723. http://dx.doi.org/10.1371/journal.pone.0040723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R, Car J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev. 2013;12:Cd007458. doi: 10.1002/14651858.CD007458.pub3. http://dx.doi.org/10.1002/14651858.CD007458.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stockwell MS, Kharbanda EO, Martinez RA, Lara M, Vawdrey D, Natarajan K, et al. Text4Health: impact of text message reminder-recalls for pediatric and adolescent immunizations. Am J Public Health. 2012;102(2):e15–e21. doi: 10.2105/AJPH.2011.300331. http://dx.doi.org/10.2105/AJPH.2011.300331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins JA, Popkin RA, Santelli JS. Pregnancy ambivalence and contraceptive use among young adults in the United States. Perspect Sex Reprod Health. 2012;44(4):236–243. doi: 10.1363/4423612. http://dx.doi.org/10.1363/4423612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Delgado-Rodriguez M, Llorca J. Bias. J Epidemiol Community Health. 2004;58(8):635–641. doi: 10.1136/jech.2003.008466. http://dx.doi.org/10.1136/jech.2003.008466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Castano PM, Bynum JY, Andres R, Lara M, Westhoff C. Effect of daily text messages on oral contraceptive continuation: a randomized controlled trial. Obstet Gynecol. 2012;119(1):14–20. doi: 10.1097/AOG.0b013e31823d4167. http://dx.doi.org/10.1097/AOG.0b013e31823d4167. [DOI] [PubMed] [Google Scholar]
- 26.Hall KS, Westhoff CL, Castano PM. The impact of an educational text message intervention on young urban women’s knowledge of oral contraception. Contraception. 2013;87(4):449–454. doi: 10.1016/j.contraception.2012.09.004. http://dx.doi.org/10.1016/j.contraception.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zapata LB, Tregear SJ, Curtis KM, et al. Impact of contraceptive counseling in clinical settings: a systematic review. Am J Prev Med. 2015;49(2S1):S31–S45. doi: 10.1016/j.amepre.2015.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pazol K, Zapata LB, Tregear SJ, et al. Impact of contraceptive education on contraceptive knowledge and decision making: a systematic review. Am J Prev Med. 2015;49(2S1):S46–S56. doi: 10.1016/j.amepre.2015.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.CDC. Providing quality family planning services: recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep. 2014;63(4):1–54. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.