Abstract
Background
Information about post-acute coronary syndrome (ACS) survival have been mostly short-term findings or based on specialized, cardiology referral centers.
Objectives
To describe one-year case-fatality rates in the Strategy of Registry of Acute Coronary Syndrome (ERICO) cohort, and to study baseline characteristics as predictors.
Methods
We analyzed data from 964 ERICO participants enrolled from February 2009 to December 2012. We assessed vital status by telephone contact and official death certificate searches. The cause of death was determined according to the official death certificates. We used log-rank tests to compare the probabilities of survival across subgroups. We built crude and adjusted (for age, sex and ACS subtype) Cox regression models to study if the ACS subtype or baseline characteristics were independent predictors of all-cause or cardiovascular mortality.
Results
We identified 110 deaths in the cohort (case-fatality rate, 12.0%). Age [Hazard ratio (HR) = 2.04 per 10 year increase; 95% confidence interval (95%CI) = 1.75–2.38], non-ST elevation myocardial infarction (HR = 3.82 ; 95%CI = 2.21–6.60) or ST elevation myocardial infarction (HR = 2.59; 95%CI = 1.38–4.89) diagnoses, and diabetes (HR = 1.78; 95%CI = 1.20‑2.63) were significant risk factors for all-cause mortality in the adjusted models. We found similar results for cardiovascular mortality. A previous coronary artery disease diagnosis was also an independent predictor of all-cause mortality (HR = 1.61; 95%CI = 1.04–2.50), but not for cardiovascular mortality.
Conclusion
We found an overall one-year mortality rate of 12.0% in a sample of post-ACS patients in a community, non-specialized hospital in São Paulo, Brazil. Age, ACS subtype, and diabetes were independent predictors of poor one‑year survival for overall and cardiovascular-related causes.
Keywords: Acute Coronary Syndrome/mortality, Risk Factors, Prognosis, Lethality, Cohort Studies
Introduction
Acute coronary syndrome (ACS) is a broad term that encompasses ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), and unstable angina (UA). ACS events are frequent conditions in Brazil and worldwide 1. In the past decades, increased aging of the population and increasing trends in the prevalence of some cardiovascular risk factors such as obesity 2 and diabetes 3 have contributed to the elevation in the number of individuals who have suffered an ACS event. In addition, successful system-of-care organization strategies 4, 5, enhanced in-hospital ACS treatment 6, and better options for the control of long-term complications for heart failure 7 and for secondary prevention 8 increased the median survival time of treated ACS patients.
In this scenario, long-term information about survival after an ACS event is of growing interest. Most long-term post-ACS studies focus on patients treated in cardiology referral centers or facilities with specialized cardiology divisions9-14. However, a large number of ACS patients seek treatment in community, non-specialized hospitals15-17. Typically, these locations do not have on-site cardiac catheterization and revascularization, nor do they have a coronary care unit. In one of the few studies to focus on this setting, Aune et al.18 described a one-year mortality rate of 16% in 307 post-MI patients treated in a non-specialized hospital in Norway, after the institution of a reference system for invasive cardiac procedures in a cardiology referral center.
The Strategy of Registry of Acute Coronary Syndrome (ERICO) study is an ongoing cohort of individuals admitted to treat an ACS event in Hospital Universitário da USP (HU-USP), a community hospital in São Paulo, Brazil. The primary aims of this article are as follows: (1) to describe one-year all-cause mortality in the ongoing ERICO cohort, as non-referral hospitals compose a sub-represented scenario in ACS treatment in most post-ACS studies, and (2) to study baseline characteristics that were predictors for a fatal outcome during the first year of follow-up. As a secondary goal, we also described rates and clinical predictors for cardiovascular mortality in this sample.
Methods
Study design and study sample
The ERICO study design has been described in detail elsewhere19. In brief, it is a cohort study of individuals admitted because of an ACS in HU-USP, a 260-bed teaching community regional hospital in the borough of Butantã, São Paulo, in southeastern Brazil. Butantã had an area of 12.5 km2 and a population of 428,000 inhabitants in 201020. This area has marked socioeconomic inequalities; although its mean family income is higher than the city’s average, we have 13.1% of habitants living in favelas or shanty towns (São Paulo city average, 11.1%)21. As with most community, non-specialized hospitals, it is not possible to perform on-site catheterization or revascularization procedures at HU-USP. Most patients who need specialized cardiology care are immediately transferred to Instituto do Coração (InCor), a cardiology referral center with uninterrupted emergency services, eight kilometers away from the community hospital. This co-operation between HU-USP and InCor was established several years before the ERICO cohort enrollment and persists until now. During the in-hospital phase, patients are treated in the emergency ward, internal medicine infirmaries, and/or in the intensive care unit.
ERICO participants must fulfill STEMI, NSTEMI, or UA diagnostic criteria (Table 1). At baseline, trained interviewers obtained data regarding sociodemographics, cardiovascular risk factors, and medications. During this in-hospital phase, all subjects were treated using the discretion of the hospital staff with standard procedures, without influence from the study protocol. Participants were re-evaluated by a physician 30 days after the acute event, with new clinical and laboratory assessments. According to the ERICO study protocol, after 6 months, one year, and yearly thereafter, all participants were contacted by phone to update information about their vital status and non-fatal outcomes. Here we have presented information from 964 ERICO participants who were enrolled from February 2009 to December 2012.
Table 1.
ERICO diagnostic criteria (adapted from Goulart et al19)
| Myocardial infarction: |
|---|
| Both following criteria: |
| •Symptoms consistent with cardiac ischemia within 24 hours of hospital presentation |
| •Troponin I levels above the 99th percentile with a test-specific coefficient of variation < 10%. |
| ST-elevation myocardial infarction: |
| Both following criteria: |
| •Criteria for MI diagnosis |
| •One of the following: (a) persistent ST segment elevation of > 1 mm in two contiguous electrocardiographic leads; (b) presence of a new or presumably new left bundle branch block. |
| Non ST-elevation myocardial infarction: |
| Both following criteria: |
| •Criteria for MI diagnosis |
| •Absence of criteria for ST-elevation MI diagnosis. |
| Unstable angina: |
| All three criteria: |
| •Symptoms consistent with cardiac ischemia 24 hours prior to hospital admission |
| •Absence of MI criteria |
| •At least one of the following: (a) history of coronary artery disease; (b) positive coronary disease stratification test (invasive or noninvasive); (c) transient ST segment changes ≥0.5 mm in two contiguous leads, new T-wave inversion of ≥1 mm and/or pseudo normalization of previously inverted T waves; (d) troponin I > 0.4 ng/mL; or (e) diagnostic concordance of two independent physicians. |
Outcomes
We defined one-year mortality on the basis of the vital status at 360 days after hospital admission. We searched official death records for information about all participants whether (1) we had information that they had died or (2) we could not contact them at the time. Vital status during follow-up was updated through medical registries and death certificates with the collaboration of the municipal and state health offices. On a regular basis, the research team prepared a list of all individuals who had died or with whom contact had been lost. The municipal and state health offices performed a search of their files to obtain death certificates and returned the results of this search to the ERICO research team. Two medical doctors reviewed these data and classified the cause of death for deceased participants according to the information from death certificates. If necessary, a third doctor analyzed the death certificate followed by a consensus meeting. Participants were defined to have died from a cardiovascular cause (cardiovascular mortality) if we identified a cause of death classified in the 10th version of the International Classification of Diseases (ICD-10) chapter IX “Diseases of the circulatory system” or if we identified a cause of death classified with the ICD-10 code R57.0 “Cardiogenic shock.”
Other variables
Sociodemographic data was obtained by interview, and was complemented with hospital registries. Age was used as a continuous variable (for most analyses) or categorized as < 55, 55–64, 65–74, and ≥ 75 years. Formal education was categorized as no formal education, 1–7 years, and ≥ 8 years. At the baseline assessment, we used self-reported data for smoking status (never, past, or current) and for the diagnosis of hypertension, diabetes, dyslipidemia, physical inactivity, and previous coronary artery disease (CAD).
Ethical considerations
The study protocol was in accordance with the Declaration of Helsinki. The institutional review board of the hospital approved the research protocol (Ethical Committee Approval 866/08). Written informed consent was obtained from all ACS patients admitted to the hospital who agreed to participate in this study, and each subject received a copy of the consent form.
Statistical Analysis
Chi-squared and Wilcoxon rank-sum tests were used to compare individuals with censored data to those with complete vital status information. Continuous variables were presented as mean ± standard deviation and categorical variables were presented as absolute numbers and proportions. We have presented case-fatality rates, with respective 95% confidence intervals, according to ACS subtype, age, sex, years of formal education, smoking status, diagnoses of hypertension, diabetes, and dyslipidemia, physical inactivity, and a previous CAD diagnosis. We have also presented survival data according to ACS subtype at hospital admission and baseline clinical characteristics, using Kaplan–Meier curves. Log-rank tests were used to compare probabilities of survival at 30 days, 180 days, and one year across subgroups.
We built crude and adjusted Cox regression models to study if sex, educational level, smoking status, hypertension, diabetes, dyslipidemia, physical inactivity or previous CAD were independent predictors of all-cause or cardiovascular mortality in our cohort. All adjusted models included sex, age, and ACS subtype as covariates. We built a post hoc model including systolic dysfunction (ejection fraction below 40%) and treatment with percutaneous transluminal coronary angioplasty (PTCA) for the index event as covariates. We also present Cox regression results restricting the dependent variable to the occurrence of deaths because of cardiovascular causes. In this case, we censored participants who died of non-cardiovascular causes at the time of death. Significance level was set at 0.05. We used R software version 2.13.122.
Results
Our sample included 269 (27.9%) individuals with STEMI, 378 (39.2%) with NSTEMI, and 317 (32.9%) with an UA diagnosis in our sample. We found high frequencies of hypertension (77.2%), dyslipidemia (54.9%), and diabetes (39.6%) diagnoses and physical inactivity (71.9%). Table 2 shows the baseline characteristics of the study sample. Median in-hospital stay duration was 4 days for individuals with UA and 8 days for individuals with STEMI or NSTEMI, with an in-hospital mortality rate of 3.0%. Preliminary data about in-hospital medical treatment revealed that aspirin was administered to 98.3% of the patients, clopidogrel to 95.9%, heparin to 96.0%, statins to 91.9%, beta blockers to 83.6%, and either angiotensin-converting enzyme inhibitors and/or angiotensin-receptor blockers to 84.0% (Table 3). Regarding stratification strategies, 69.9%, 82.0%, and 48.3% of patients with NSTEMI, STEMI, and UA in ERICO underwent coronary angiography for the index event. Angioplasty was performed in 58.2% of ERICO participants from whom a coronary angiography was obtained, with a success rate of 96.3%. Reperfusion therapy for the index event was performed in 72.2% of STEMI cases. Thrombolysis was the selected strategy in 79.9% of STEMI patients for whom a reperfusion strategy was indicated. The most frequent cause that contraindicated reperfusion treatment in STEMI patients was late patient presentation to emergency care (69.2% of STEMI participants without reperfusion treatment). No studied baseline characteristics were associated with the decision for reperfusion or strategy selection. Although not defined by the study protocol, echocardiograms were performed in 66.4% and 77.3% of ERICO participants with NSTEMI and STEMI, respectively. On the basis of this data, an ejection fraction below 50% was found in 35.9% and 36.5% and an ejection fraction below 40% in 14.3% and 7.2% of ERICO participants with NSTEMI and STEMI, respectively.
Table 2.
Baseline characteristics of study participants
| STEMI n = 269 | NSTEMI n = 378 | UA n = 317 | Total n = 964 | |
|---|---|---|---|---|
| Age (years) | ||||
| Median | 59.0 | 64.5 | 62.0 | 62.0 |
| Interquartile range | 51.0-68.0 | 55.0-75.0 | 54.0-73.0 | 53.0-73.0 |
| Male sex (%) | 181 (67.3%) | 223 (59.0%) | 166 (52.4%) | 570 (59.1%) |
| Formal education (%) | ||||
| No formal education | 27 (10.1%) | 50 (13.3%) | 49 (15.5%) | 126 (13.1%) |
| 1-7 years | 113 (42.2%) | 169 (44.8%) | 132 (41.6%) | 414 (43.0%) |
| ≥8 years | 128 (47.8%) | 158 (41.9%) | 136 (42.9%) | 422 (43.9%) |
| Smoking status (%) | ||||
| Never | 68 (26.4%) | 120 (34.0%) | 100 (34.0%) | 288 (31.8%) |
| Past | 88 (34.1%) | 121 (34.3%) | 130 (44.2%) | 339 (37.5%) |
| Current | 102 (39.5%) | 112 (31.7%) | 64 (21.8%) | 278 (30.7%) |
| Hypertension (%) | 164 (63.3%) | 291 (78.0%) | 272 (87.7%) | 727 (77.2%) |
| Diabetes (%) | 77 (30.1%) | 165 (44.5%) | 127 (41.6%) | 369 (39.6%) |
| Dyslipidemia (%) | 102 (46.6%) | 187 (55.0%) | 166 (61.5%) | 455 (54.9%) |
| Physical inactivity (%) | 173 (69.8%) | 261 (72.5%) | 210 (72.9%) | 644 (71.9%) |
| Previous CAD (%) | 37 (14.9%) | 83 (24.1%) | 129 (45.4%) | 249 (28.4%) |
CAD: Coronary artery disease; STEMI: ST elevation myocardial infarction; NSTEMI: Non-ST elevation myocardial infarction; UA: Unstable angina.
Table 3.
Medication use during in-hospital treatment in the sample
| Medication | STEMI | NSTEMI | UA |
|---|---|---|---|
| Aspirin | 99.2% | 98.6% | 97.8% |
| Clopidogrel | 99.2% | 97.7% | 95.6% |
| Heparin | 95.9% | 97.7% | 96.3% |
| Statins | 95.5% | 92.6% | 89.7% |
| Betablockers | 87.2% | 80.9% | 84.6% |
| ACE inhibitors and/or ARB | 86.4% | 85.1% | 81.0% |
ACE: Angiotensin-converting enzyme; ARB: Angiotensin receptor blocker
During the first year of follow-up, we had complete vital status information from 918 (95.2%) study participants in this sample. Individuals with censored vital status data during follow-up were more prone to be male and younger (p < 0.001 for both), compared with those with complete vital status information.
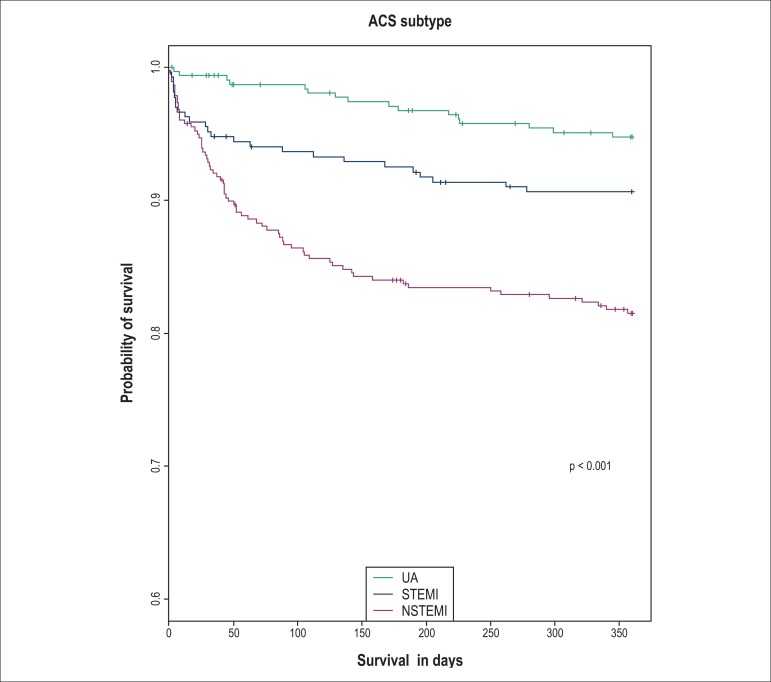
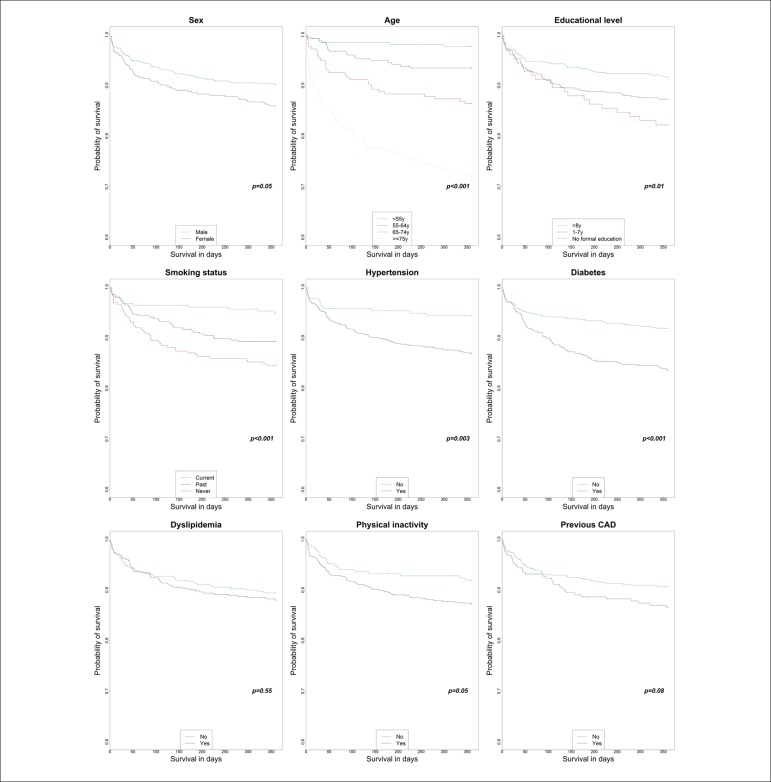
We identified 42 (case-fatality rate, 4.4%), 90 (case-fatality rate, 9.6%), and 110 (case-fatality rate, 12.0%) deaths at 30 days, 180 days, and one year, respectively. Case-fatality rates by subgroups (with respective 95% confidence intervals) at 30 days, 180 days, and one year are presented in Table 4. The survival analysis using Kaplan–Meier curves according to ACS subtype at presentation (Figure 1) and baseline characteristics (Figure 2) are also shown. Analyzing survival rates at 30 days, 180 days, and one year, we found age and ACS subtypes to be predictors for 30-day mortality (p < 0.001 for both). Age, NSTEMI diagnosis, less education, never smoking, hypertension, and diabetes were significantly associated with poorer survival at 180 days and one year of follow-up. In addition, we found that female sex and physical inactivity had an association with poorer one-year prognosis with borderline significance (p = 0.05 for both).
Table 4.
Case-fatality rates according to baseline clinical characteristics at 30 days, 180 days, and one-year of follow-up
| Case-fatality rates (95% confidence interval) | |||
|---|---|---|---|
| 30 days | 180 days | One year | |
| ACS subtype | |||
| STEMI | 4.9% (2.7% - 8.3%) | 7.5% (4.8% - 11.6%) | 9.6% (6.4% - 14.0%) |
| NSTEMI | 7.2% (4.9% - 10.4%) | 16.2% (12.7% - 20.5%) | 19.2% (15.3% - 23.7%) |
| UA | 0.6% (0.1% - 2.5%) | 3.3% (1.7% - 6.1%) | 5.4% (3.2% - 8.8%) |
| Age | |||
| < 55 years | 1.5% (0.5% - 4.1%) | 1.6% (0.5% - 4.2%) | 2.4% (1.0% - 5.5%) |
| 55-64 years | 1.1% (0.3% - 3.4%) | 5.5% (3.2% - 9.2%) | 6.8% (4.2% - 10.7%) |
| 65-74 years | 4.7% (2.4% - 8.6%) | 11.8% (7.9% - 17.1%) | 13.8% (9.6% - 19.4%) |
| > 75 years | 12.4% (8.3% - 17.9%) | 22.9% (17.4% - 29.4%) | 28.6% (22.6% - 35.5%) |
| Sex | |||
| Male | 3.9% (2.5% - 5.9%) | 8.2% (6.1% - 10.9%) | 10.4% (8.0% - 13.3%) |
| Female | 5.1% (3.2% - 7.9%) | 11.5% (8.6% - 15.2%) | 14.2% (11.0% - 18.2%) |
| Formal education | |||
| No formal education | 4.8% (2.0% - 10.5%) | 13.1% (7.9% - 20.7%) | 18.3% (12.1% - 26.7%) |
| 1-7 years | 4.9% (3.1% - 7.5%) | 11.1% (8.3% - 14.6%) | 13.1% (10.0% - 17.0%) |
| ≥8 years | 3.6% (2.1% - 6.0%) | 6.8% (4.7% - 9.9%) | 8.8% (6.3% - 12.1%) |
| Smoking status | |||
| Never | 4.9% (2.8% - 8.2%) | 13.2% (9.6% - 17.9%) | 16.1% (12.1% - 21.1%) |
| Past | 3.3% (1.7% - 5.9%) | 8.7% (6.0% - 12.4%) | 11.0% (8.0% - 15.1%) |
| Current | 3.3% (1.6% - 6.3%) | 4.1% (2.2% - 7.4%) | 5.3% (3.0% - 8.9%) |
| Hypertension | |||
| Yes | 4.4% (3.1% - 6.3%) | 10.7% (8.6% - 13.3%) | 13.5% (11.1% - 16.3%) |
| No | 2.8% (1.1% - 6.3%) | 4.8% (2.4% - 8.9%) | 6.0% (3.3% - 10.5%) |
| Diabetes | |||
| Yes | 4.9% (3.0% - 7.7%) | 13.7% (10.4% - 17.8%) | 16.8% (13.1% - 21.1%) |
| No | 3.8% (2.4% - 5.8%) | 6.6% (4.7% - 9.1%) | 8.5% (6.3% - 11.3%) |
| Dyslipidemia | |||
| Yes | 3.8% (2.3% - 6.1%) | 10% (7.5% - 13.3%) | 12.4% (9.5% - 15.9%) |
| No | 4.6% (2.8% - 7.3%) | 8.5% (6.0% - 12.0%) | 11.0% (8.0% - 14.8%) |
| Physical inactivity | |||
| Yes | 4.8% (3.4% - 6.9%) | 10.6% (8.4% - 13.4%) | 13.1% (10.6% - 16.1%) |
| No | 3.2% (1.5% - 6.4%) | 7.0% (4.2% - 11.1%) | 8.4% (5.3% - 12.9%) |
| Previous CAD | |||
| Yes | 5.2% (2.9% - 9.0%) | 11.4% (7.9% - 16.3%) | 13.9% (9.9% - 19.1%) |
| No | 3.5% (2.3% - 5.4%) | 8.0% (6.1% - 10.6%) | 9.8% (7.6% - 12.5%) |
ACS: acute coronary syndrome; CAD: Coronary artery disease; STEMI: ST elevation myocardial infarction; NSTEMI: Non-ST elevation myocardial infarction; UA: Unstable angina.
Figure 1.
Kaplan–Meier curves according to ACS subtype at presentation.
Figure 2.
Kaplan–Meier curves according to clinical baseline characteristics.
We could identify the cause of death, using official information from available death certificates, for 102 (99%) of the 103 participants who died during the first year of follow-up, with only one undefined cause of death. Table 5 presents the causes and time of death using the 10th revision of the International Classification of Diseases (ICD-10) version 2015 chapters. Table 6 presents the crude and adjusted hazard ratios (HR) for all-cause mortality and cardiovascular mortality according to the ACS subtypes and baseline characteristics. Age, NSTEMI or STEMI diagnosis, and diabetes were associated with both outcomes in the adjusted models. Previous CAD was also an independent predictor of all-cause mortality, although only a non-significant trend was observed for cardiovascular mortality (p = 0.066) in adjusted models, probably because of a smaller number of events. After further adjustment for systolic dysfunction and treatment with PTCA for the index event, diabetes (p = 0.013), and age (p = 0.010) remained as significant risk factors for all-cause mortality. An NSTEMI diagnosis (p = 0.047) remained as a significant risk factor for cardiovascular mortality.
Table 5.
Causes of death (ICD-10 chapters) during follow-up according to death certificate
| Cause of death | 0 to 30 days n = 42 | 31 to 180 days n = 43 | 180 days to one year n = 18 | Total n = 103 |
|---|---|---|---|---|
| IX. Diseases of the circulatory system | 36 (85.7%) | 31 (72.1%) | 8 (44.4%) | 75 (72.8%) |
| II. Neoplasms | 2 (4.8%) | 4 (9.3%) | 2 (11.1%) | 8 (7.8%) |
| X. Diseases of the respiratory system | 1 (2.4%) | 2 (4.7%) | 3 (16.7%) | 6 (5.8%) |
| I. Certain infectious and parasitic diseases | 3 (7.1%) | 1 (2.3%) | 0 | 4 (3.9%) |
| XX. External causes of morbidity and mortality | 0 | 1(2.3%) | 2 (11.1%) | 3 (2.9%) |
| XI. Diseases of the digestive system | 0 | 3 (7.0%) | 0 | 3 (2.9%) |
| XII. Diseases of the skin and subcutaneous tissue | 0 | 1(2.3%) | 1 (5.6%) | 2 (1.9%) |
| XIV. Diseases of the genitourinary system | 0 | 0 | 1 (5.6%) | 1 (1.0%) |
| Undefined | 0 | 0 | 1 (5.6%) | 1 (1.0%) |
Table 6.
Crude and adjusted hazard ratios (95% confidence intervals) for all-cause and cardiovascular mortality, according to ACS classification and patient baseline characteristics
| All-cause mortality | Cardiovascular mortality | |||
|---|---|---|---|---|
| Crude hazard ratio (95%CI) | Multivariate hazard ratio (95%CI) | Crude hazard ratio (95%CI) | Multivariate hazard ratio (95%CI) | |
| Age (per 10-year increase) | 2.09 (1.79 - 2.43) | 2.04 (1.75 - 2.38) | 2.06 (1.71 - 2.48) | 1.98 (1.65 - 2.39) |
| ACS subtype | ||||
| STEMI | 1.89 (1.01 - 3.54) | 2.59 (1.38 - 4.89) | 1.69 (0.75 - 3.81) | 2.28 (1.004 - 5.16) |
| NSTEMI | 3.90 (2.27 - 6.72) | 3.82 (2.21 - 6.60) | 4.56 (2.32 - 8.99) | 4.39 (2.22 - 8.67) |
| UA | Reference | Reference | Reference | Reference |
| Sex | ||||
| Female | 1.45 (1.00 - 2.11) | 1.33 (0.91 - 1.94) | 1.49 (0.95 - 2.34) | 1.33 (0.84 - 2.10) |
| Male | Reference | Reference | Reference | Reference |
| Formal education | ||||
| No formal education | 2.16 (1.27 - 3.69) | 1.31 (0.75 - 2.28) | 1.64 (0.85 - 3.18) | 0.96 (0.48 - 1.91) |
| 1-7 years | 1.54 (1.00 - 2.36) | 1.16 (0.75 - 1.79) | 1.30 (0.78 - 2.16) | 0.96 (0.57 - 1.60) |
| ≥8 years | Reference | Reference | Reference | Reference |
| Smoking status | ||||
| Current | 0.31 (0.17 - 0.57) | 0.55 (0.29 - 1.04) | 0.37 (0.18 - 0.73) | 0.65 (0.31 - 1.35) |
| Past | 0.67 (0.43 - 1.05) | 0.81 (0.51 - 1.29) | 0.61 (0.35 - 1.05) | 0.75 (0.42 - 1.33) |
| Never | Reference | Reference | Reference | Reference |
| Hypertension | 2.38 (1.31 - 4.34) | 1.84 (1.00 - 3.37) | 2.15 (1.07 - 4.32) | 1.63 (0.80 - 3.29) |
| Diabetes | 2.08 (1.41 - 3.06) | 1.78 (1.20 - 2.63) | 2.35 (1.47 - 3.75) | 1.97 (1.23 - 3.16) |
| Dyslipidemia | 1.13 (0.75 - 1.71) | 1.10 (0.72 - 1.67) | 1.53 (0.91 - 2.56) | 1.47 (0.87 - 2.49) |
| Physical inactivity | 1.62 (0.99 - 2.65) | 1.37 (0.84 - 2.25) | 1.46 (0.83 - 2.59) | 1.22 (0.69 - 2.17) |
| Previous CAD | 1.45 (0.95 - 2.23) | 1.61 (1.04 - 2.50) | 1.50 (0.90 - 2.52) | 1.64 (0.97 - 2.78) |
Multivariate adjustment included age, sex, and ACS subtype, except itself; ACS: acute coronary syndrome; CAD: Coronary artery disease; STEMI: ST elevation myocardial infarction; NSTEMI: Non-ST elevation myocardial infarction; UA: Unstable angina.
Discussion
In the present study, we have observed an overall one-year case-fatality rate of 12.0% for patients admitted to a community hospital with a diagnosis of ACS. A significant difference in the mortality rate was noted when the results were stratified by ACS type (5.4%, 9.6%, and 19.2% for participants with UA, STEMI, and NSTEMI diagnoses, respectively). The earliest predictors of poor survival (at 30 days of follow-up) were age and ACS subtype. Age, ACS subtype, diabetes, and a previous CAD diagnosis were independent risk factors for one-year all-cause mortality in our cohort. Restricting mortality data to deaths because of cardiovascular specific causes, we found that age, ACS subtype, and diabetes remained significant independent predictors of poor long-term survival.
Other authors have also studied post-ACS mortality. The Swedish Register of Cardiac Intensive Care was a prospective observational study in coronary care units of 58 hospitals in Sweden. In an analysis of 19,599 participants of that cohort, Stenestrand et al.9 found a one-year post-MI mortality rate of 7.8%. The Gulf Registry of Acute Coronary Events was a cohort study of 7,930 post-ACS patients from 65 hospitals (71% with a coronary care unit, 43% with on-site catheterization) in six Middle East countries. AlHabib et al.10 analyzed data from that cohort and found a one-year mortality rate of 11.5% for STEMI patients and 7.7% for patients with a non-ST elevation ACS (UA or NSTEMI). Skelding et al.11 analyzed observational data from a single specialized center in Pennsylvania, and found a one-year mortality rate of 8% in 2,066 patients who underwent invasive evaluation. Kleopatra et al.23 similarly analyzed data from 1,986 women with NSTEMI in 155 hospitals from the German Acute Coronary Syndromes registry and found a one-year mortality rate of 8.1% in those who underwent invasive stratification and 24.0% in those who did not. Ruano-Ravina et al.12 recently analyzed a cohort of 1,461 individuals presenting with STEMI who underwent primary angioplasty in two hospitals in Spain, and found a one-year mortality rate of 9.3%. In Brazil, the Acute Coronary Care Evaluation of Practice Registry (ACCEPT study), a multicenter post-ACS Brazilian study with 2,485 patients, found a 30-day mortality rate of 1.8%, 3.0%, and 3.4% in individuals with UA, NSTEMI, and STEMI, respectively13. A study of 1,027 patients with NSTEMI from a single cardiology referral center in the city of São Paulo14 found that 5.3% of the participants died or had a new infarction within 30 days.
The comparison of mortality rates across the post-ACS cohorts must be interpreted with caution. Differences in patient selection and treatment options, including fast-paced advances in treatment in the past years may be partially responsible for unequal results. Compared with results from the recently published ACCEPT study, a Brazilian follow-up study of post-ACS patients, we had higher 30-day mortality rates for NSTEMI patients (7.2% vs. 3.0%) and lower for UA patients (0.6% vs. 1.8%). Both ACCEPT (up to 30 days) and ERICO (up to one year) trial had a very small loss of vital status information during follow-up, and they were conducted almost simultaneously. In this case, patient selection may be a major contribution for these unequal results. First, inclusion criteria were not the same in these two cohorts. In the ACCEPT study, UA diagnosis relied on remarkable ECG changes (ST depression of at least 1.0 mm or transient ST elevation or ST elevation of 1.0 mm or less, or T-wave inversion of more than 3.0 mm)24. Although this allowed a more homogeneous UA subgroup, some lower-risk UA patients may be missed with this strategy. We opted for less restrictive criteria, similar to those adopted for the GRACE study25. Thus, differences in a 30-day mortality rates for UA patients in ERICO and ACCEPT studies may have occurred because of the inclusion of less severe UA patients in our sample. Moreover, as the cut-off troponin I values vary according to the diagnostic kit utilized and the criteria for normality, NSTEMI definition may have varied from center to center. We opted for a cut-off troponin level that fulfilled the criteria of the American Heart Association / European Society of Cardiology26 and the Committee on Standardization of Markers of Cardiac Damage of the International Federation of Clinical Chemistry and Laboratory Medicine27. Thus, it is possible that some patients, who were included in the NSTEMI group in ACCEPT, would not be included as such in the ERICO trial. Therefore, the lower NSTEMI mortality in ACCEPT may be because of the inclusion of less severe cases, which may partially explain these differences in mortality rates. Finally, as with most ACS registry and post-ACS follow-up studies, tertiary centers and other cardiology referral hospitals may be overrepresented in ACCEPT. For example, a CAD diagnosis before study entry was more frequent in ACCEPT than in ERICO for all ACS subtypes. It is important to highlight that treatment in referral centers only occurs in a minority of patients in many areas of the world, including Brazil. This underlines the need for high-quality data from other non-cardiology specific centers, which will allow for a better understanding of the whole post-ACS population.
Diabetes was an independent risk factor for one-year mortality in our cohort. This is consistent with the findings of others. In our country, the previously cited study by Santos et al.14 found that a diabetes diagnosis was significantly associated to all-cause mortality or re-infarction in 30 days. AlFaleh et al.28 analyzed 6,362 patients from the Gulf Registry of Acute Coronary Events-2 (Gulf RACE-2), and found that a history of diabetes or new-onset hyperglycemia at admission was associated with higher in-hospital, 30 day, and one-year mortality rates. A retrospective cohort study by Kaul et al.29 with 25,324 ACS patients in Canada also found diabetes to be an independent risk factor for one-year mortality (HR 1.41; 95%CI 1.24–1.61). A recent study by Savonitto et al.30 analyzed 645 individuals aged 75 years or older with a non-ST-elevation ACS diagnosis. In that sample, diabetes and admission hyperglycemia were associated with higher one-year mortality rates. A study of 2,027 patients with MI by Nicolau et al.31 also found that hyperglycemia was associated with in-hospital mortality, with a more pronounced effect in younger individuals. However, this is still subject of debate in the literature. The Global Registry of Acute Coronary Events (GRACE) study investigators built a risk predictor model for six-month mortality. Although diabetes was associated with higher mortality in their cohort, a model with eight other clinical predictors (age, congestive heart failure, systolic blood pressure, Killip class, initial serum creatinine concentration, positive initial cardiac markers, cardiac arrest on admission, and ST-segment deviation) contained more than 90% of the predictive information32. This suggested that the impact of diabetes diagnosis on long-term mortality was probably mediated by its association with one of the risk factors in the model. In addition, in Aune et al.’s study18, based on two cohorts of patients from a hospital without catheterization capabilities in Norway, diabetes was not a predictor of higher one-year mortality (HR 1.01; 95%CI 0.64–1.59). Differences in study populations may explain conflicting results between Aune et al.’s study and ours. For example, their cohorts had higher median ages but lower frequency of hypertension, diabetes, and previous CAD prevalence compared with ours. Lower diabetes prevalence, interaction among these factors on mortality risk, and the impact of selection or survival bias may be partially responsible for this difference.
Our data pointed to a non-significant trend for higher one-year mortality risk in non-smokers compared with current and past smokers. Other authors have also described similar findings33. Some explanations have been raised to explain this apparent paradox. First, post-ACS studies only include individuals who actually reached the hospital alive. As some studies associate smoking with sudden coronary death34, it is possible that these results may be partially explained by survival bias. Second, non-smokers who had an ACS event usually have more other cardiovascular risk factors compared with non-smokers. However, there have been conflicts in the data regarding the profile for other cardiovascular risk factors if they were sufficient to explain the worse prognosis observed in non-smokers. Robertson et al.35 evaluated 13,819 patients with non-ST elevation ACS from the Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial. They found smoking to be associated to lower one-year mortality compared with non-smokers in crude models (HR 0.80; 95%CI 0.65–0.98). After adjustment for other cardiovascular risk factors, they described higher one-year mortality risk in smokers (HR 1.37; 95%CI 1.07–1.75). On the other hand, Lee et al.36, using data from 41,025 participants from the GUSTO-I trial, found that current smoking was associated to lower 30-day mortality after an ACS event and this protective effect persisted even after adjustment for other cardiovascular risk factors (p < 0.0001). In our cohort, the association between smoking and lower one-year mortality risk vanished after adjustment for age, sex, and ACS subtype. In addition, the frequency of diabetes, a strong risk factor for mortality in our sample, was higher in non-smokers compared with smokers (48.2% vs. 25.5%; p < 0.001), which may at least partially explain the trend towards a higher risk in non-smokers. This negative association between diabetes and smoking is expected, as others have demonstrated that the body-mass index is usually higher in non-smokers37.
At HU-USP, emergencists, intensive care and internal medicine professionals provided treatment during the index event for all ERICO participants. It must be noted that some cardiology procedures as coronary tomography, echocardiogram, and treadmill exercise tests are available onsite. In addition, several cardiologists are on the hospital staff and actively participated in the discussion of ACS cases in the emergency room, although they were not specifically responsible for the treatment of all ACS patients.
Although one could raise concerns that treatment in community hospitals could induce potential biases mediated by inequalities in treatment compared with specialized centers, we did not observe it in the present study. Comparing our treatment strategies with data from the Brazilian Registry on Acute Coronary Syndromes (BRACE) study, we found that rates of pharmacological treatment in the ERICO cohort were similar or slightly higher compared with the Brazilian southeastern hospitals that were included in BRACE study. We believe that the higher rates in ERICO may be associated with a low frequency of medical treatment contraindications, as we can speculate that the patients in a community hospital often have a lower number of comorbidities compared with those treated in tertiary hospitals. In addition, rates for reperfusion treatment in STEMI patients were also very similar compared with the findings of the BRACE study. The main reason for contraindications (late patient presentation to emergency care) was the same in both studies.
Some important features of the present study should be highlighted. This was a long-term cohort of post-ACS patients treated in a community, non-cardiology hospital, which has been a scenario that has been frequently neglected. As a community hospital, most patients who sought treatment (including the emergency department) lived in the Butantã borough. Although ERICO was not a population-based study, it had a community basis and its results could be generalized to similar areas. We had very small loss of vital status information or refusals during the follow-up period, which allowed us to adequately calculate mortality rates. Death official records could confirm death causes for more than 90% of the participants who died during follow-up. Thus, we could also study the prognostic role of the clinical variables focusing specifically on cardiovascular mortality. Our study had some limitations. First, this was a single-center study, so its findings cannot be directly extended to all Brazilian population, or compared directly with other populations. However, we do believe that these results from this ongoing cohort, although still described with a follow-up time shorter than in other studies, added novel information on the understanding of ACS patients treated in non-referral centers, who typically had a different risk factor profile compared with those treated in specialized centers19,38,39. Second, we did not include information about the influence of pharmacological and non-pharmacological treatment on results. Nevertheless, we do not believe that inequalities in treatment would invalidate, as confounding factors, the associations presented in this paper. Third, for some variables we probably did not have enough power to conclude for significant risk. As ERICO was a long-term cohort, we can re-evaluate the prognostic role of these variables in the future. Fourth, although the number of lost vital status information during follow-up was small, the predominance of men and younger individuals in the group with censored data may have had some influence on our results. Fifth, we could not retrieve death certificate information from 6.4% of the occurred deaths. In addition, we could not add systematic information for causes of death from chart reviews or interviews with patients’ families and doctors. In both cases, these may also have had an impact in the analyses for cardiovascular mortality.
Conclusion
We found an overall one-year mortality rate of 12.0% in a sample of post-ACS patients in HU-USP, a community, non-cardiology hospital in São Paulo, Brazil. Age, ACS subtype, and diabetes were independent predictors of poor one-year survival for overall and cardiovascular-related causes.
Footnotes
Author contributions
Conception and design of the research:Santos IS, Goulart AC, Bittencourt MS, Sitnik D, Pereira AC, Lotufo PA, Bensenor IM. Acquisition of data:Santos IS, Goulart AC, Brandão RM, Santos RCO, Bittencourt MS, Sitnik D, Pastore CA, Samesima N. Analysis and interpretation of the data: Santos IS, Goulart AC, Brandão RM, Santos RCO, Bittencourt MS, Sitnik D, Pereira AC, Pastore CA, Samesima N, Lotufo PA, Bensenor IM. Statistical analysis: Santos IS, Goulart AC. Obtaining financing: Santos IS, Bensenor IM. Writing of the manuscript:Santos IS, Bensenor IM. Critical revision of the manuscript for intellectual content: Goulart AC, Brandão RM, Santos RCO, Bittencourt MS, Sitnik D, Pereira AC, Pastore CA, Samesima N, Lotufo PA.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
This study was funded by FAPESP
Study Association
This study is not associated with any thesis or dissertation work.
References
- 1.Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Murray CJ, et al. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the Global Burden of Disease 2010 study. Circulation. 2014;129(14):1483–1492. doi: 10.1161/CIRCULATIONAHA.113.004042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–781. doi: 10.1016/S0140-6736(14)60460-8. Erratum in: Lancet. 2014;384(9945):746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Marcolino MS, Brant LC, Araujo JG, Nascimento BR, Castro LR, Martins P, et al. Implementation of the myocardial infarction system of care in city of Belo Horizonte, Brazil. Arq Bras Cardiol. 2013;100(4):307–314. Erratum in: Arq Bras Cardiol. 2013;100(4):313. [PubMed] [Google Scholar]
- 5.DelliFraine J, Langabeer J, 2nd, Segrest W, Fowler R, King R, Moyer P, et al. Developing an ST-elevation myocardial infarction system of care in Dallas County. Am Heart J. 2013;165(6):926–931. doi: 10.1016/j.ahj.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Piegas LS, Feitosa G, Mattos LA, Nicolau JC, Rossi JM, Neto, Timerman A, et al. Sociedade Brasileira de Cardiologia Diretriz da Sociedade Brasileira de Cardiologia sobre tratamento do infarto agudo do miocárdio com supradesnível do segmento ST. Arq Bras Cardiol. 2009;93(6) Suppl 2:e179–e264. [PubMed] [Google Scholar]
- 7.McMurray JJ. Clinical practice: systolic heart failure. N Engl J Med. 2010;362(3):228–238. doi: 10.1056/NEJMcp0909392. [DOI] [PubMed] [Google Scholar]
- 8.Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143(9):659–672. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- 9.Stenestrand U, Wallentin L, Swedish Register of Cardiac Intensive Care Early statin treatment following acute myocardial infarction and 1-year survival. JAMA. 2001;285(4):430–436. doi: 10.1001/jama.285.4.430. [DOI] [PubMed] [Google Scholar]
- 10.Alhabib KF, Sulaiman K, Al-Motarreb A, Almahmeed W, Asaad N, Amin H, et al. Baseline characteristics, management practices, and long-term outcomes of Middle Eastern patients in the Second Gulf Registry of Acute Coronary Events (Gulf RACE-2) Ann Saudi Med. 2012;32(1):9–18. doi: 10.5144/0256-4947.2012.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skelding KA, Boga G, Sartorius J, Wood GC, Berger PB, Mascarenhas VH, et al. Frequency of coronary angiography and revascularization among men and women with myocardial infarction and their relationship to mortality at one year: an analysis of the Geisinger myocardial infarction cohort. J Interv Cardiol. 2013;26(1):14–21. doi: 10.1111/joic.12009. [DOI] [PubMed] [Google Scholar]
- 12.Ruano-Ravina A, Aldama-López G, Cid-Álvarez B, Piñón-Esteban P, López-Otero D, Calviño-Santos R, et al. Radial vs femoral access after percutaneous coronary intervention for ST-segment elevation myocardial infarction: thirty-day and one-year mortality results. Rev Esp Cardiol (End Ed) 2013;66(11):871–878. doi: 10.1016/j.rec.2013.05.029. [DOI] [PubMed] [Google Scholar]
- 13.Piva e Mattos LA, Berwanger O, Santos ES, Reis HJ, Romano ER, Petriz JL, et al. Clinical outcomes at 30 days in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT) Arq Bras Cardiol. 2013;100(1):6–13. doi: 10.1590/s0066-782x2013000100003. [DOI] [PubMed] [Google Scholar]
- 14.Santos ES, Timerman A, Baltar VT, Castillo MT, Pereira MP, Minuzzo L, et al. Dante Pazzanese risk score for non-st-segment elevation acute coronary syndrome. Arq Bras Cardiol. 2009;93(4):343-51, 336-44. doi: 10.1590/s0066-782x2009001000006. [DOI] [PubMed] [Google Scholar]
- 15.Ting HH, Rihal CS, Gersh BJ, Haro LH, Bjerke CM, Lennon RJ, et al. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: the Mayo Clinic STEMI Protocol. Circulation. 2007;116(7):729–736. doi: 10.1161/CIRCULATIONAHA.107.699934. [DOI] [PubMed] [Google Scholar]
- 16.Alter DA, Austin PC, Tu JV, Canadian Cardiovascular Outcomes Research Team Community factors, hospital characteristics and inter-regional outcome variations following acute myocardial infarction in Canada. Can J Cardiol. 2005;21(3):247–255. [PubMed] [Google Scholar]
- 17.Prefeitura de São Paulo. Secretaria Municipal de Saúde Informações em saúde: produção hospitalar. [Acesso em 2014 jul 10]. Disponível em: http://www.prefeitura.sp.gov.br.
- 18.Aune E, Endresen K, Fox KA, Steen-Hansen JE, Roislien J, Hjelmesaeth J, et al. Effect of implementing routine early invasive strategy on one-year mortality in patients with acute myocardial infarction. Am J Cardiol. 2010;105(1):36–42. doi: 10.1016/j.amjcard.2009.08.641. [DOI] [PubMed] [Google Scholar]
- 19.Goulart AC, Santos IS, Sitnik D, Staniak HL, Fedeli LM, Pastore CA, et al. Design and baseline characteristics of a coronary heart disease prospective cohort: two-year experience from the strategy of registry of acute coronary syndrome study (ERICO study) Clinics (Sao Paulo) 2013;68(3):431–434. doi: 10.6061/clinics/2013(03)RC02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prefeitura de São Paulo Dados demográficos dos distritos pertencentes às subprefeituras. [Acesso em 2014 jul 14]. Disponível em: http://www.prefeitura.sp.gov.br/cidade/secretarias/subprefeituras/subprefeituras/dados_demograficos/index.php?p=12758.
- 21.Prefeitura de São Paulo Butantã , Região Oeste, Sumário de dados 2004. [Acesso em 2014 jul 11]. Disponível em http://ww2.prefeitura.sp.gov.br/arquivos/secretarias/governo/sumario_dados/ZO_BUTANTA_Caderno29.pdf.
- 22.R Core Team . R: a language and environment for statistical computing. Version 3.0.1 (20B-05-16). Vienna (Austria) The R Foundation for Statistical Computing; 2012. [Google Scholar]
- 23.Kleopatra K, Muth K, Zahn R, Bauer T, Koeth O, Jünger C, et al. Acute Coronary Syndromes Registry investigators. Effect of an invasive strategy on in-hospital outcome and one-year mortality in women with non-ST-elevation myocardial infarction. Int J Cardiol. 2011;153(3):291–295. doi: 10.1016/j.ijcard.2010.08.050. [DOI] [PubMed] [Google Scholar]
- 24.Mattos LA. Rationality and methods of ACCEPT registry - Brazilian registry of clinical practice in acute coronary syndromes of the Brazilian Society of Cardiology. Arq Bras Cardiol. 2011;97(2):94–99. doi: 10.1590/s0066-782x2011005000064. [DOI] [PubMed] [Google Scholar]
- 25.Goodman SG, Huang W, Yan AT, Budaj A, Kennelly BM, Gore JM, et al. Expanded Global Registry of Acute Coronary Events (GRACE2) Investigators The expanded Global Registry of Acute Coronary Events: baseline characteristics, management practices, and hospital outcomes of patients with acute coronary syndromes. Am Heart J. 2009;158(2):193–201. doi: 10.1016/j.ahj.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 26.Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. Eur Heart J. 2007;28(20):2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 27.Panteghini M. Recommendations on use of biochemical markers in acute coronary syndrome: IFCC proposals. eJIFCC. 2003;13(2):1–5. http://www,ifcc.org/ejifcc [PMC free article] [PubMed] [Google Scholar]
- 28.AlFaleh HF, Alhabib KF, Kashour T, Ullah A, Alsheikhali AA, Al Suwaidi J, et al. Short-term and long-term adverse cardiovascular events across the glycaemic spectrum in patients with acute coronary syndrome: the Gulf Registry of Acute Coronary Events-2. Coron Artery Dis. 2014;25(4):330–338. doi: 10.1097/MCA.0000000000000090. [DOI] [PubMed] [Google Scholar]
- 29.Kaul P, Ezekowitz JA, Armstrong PW, Leung BK, Savu A, Welsh RC, et al. Incidence of heart failure and mortality after acute coronary syndromes. Am Heart J. 2013;165(3):379–385. doi: 10.1016/j.ahj.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 30.Savonitto S, Morici N, Cavallini C, Antonicelli R, Petronio AS, Murena E, et al. One-year mortality in elderly adults with non-ST-elevation acute coronary syndrome: effect of diabetic status and admission hyperglycemia. J Am Geriatr Soc. 2014;62(7):1297–1303. doi: 10.1111/jgs.12900. [DOI] [PubMed] [Google Scholar]
- 31.Nicolau JC, Serrano CV, Jr, Giraldez RR, Baracioli LM, Moreira HG, Lima F, et al. In patients with acute myocardial infarction, the impact of hyperglycemia as a risk factor for mortality is not homogeneous across age-groups. Diabetes Care. 2012;35(1):150–152. doi: 10.2337/dc11-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fox KA, Dabbous OH, Goldberg RJ, Pieper KS, Eagle KA, Van de Werf F, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE) BMJ. 2006;333(7578):1091. doi: 10.1136/bmj.38985.646481.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ishihara M, Sato H, Tateishi H, Kawagoe T, Shimatani Y, Kurisu S, et al. Clinical implications of cigarette smoking in acute myocardial infarction: acute angiographic findings and long-term prognosis. Pt 1Am Heart J. 1997;134(5):955–960. doi: 10.1016/s0002-8703(97)80020-8. [DOI] [PubMed] [Google Scholar]
- 34.Burke AP, Farb A, Malcom GT, Liang YH, Smialek J, Virmani R. Coronary risk factors and plaque morphology in men with coronary disease who died suddenly. N Engl J Med. 1997;336(18):1276–1282. doi: 10.1056/NEJM199705013361802. [DOI] [PubMed] [Google Scholar]
- 35.Robertson JO, Ebrahimi R, Lansky AJ, Mehran R, Stone GW, Lincoff AM. Impact of cigarette smoking on extent of coronary artery disease and prognosis of patients with non-ST-segment elevation acute coronary syndromes: an analysis from the ACUITY Trial (Acute Catheterization and Urgent Intervention Triage Strategy) JACC Cardiovasc Interv. 2014;7(4):372–379. doi: 10.1016/j.jcin.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 36.Lee KL, Woodlief LH, Topol EJ, Weaver WD, Betriu A, Col J, et al. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction. Results from an international trial of 41,021 patients. GUSTO-I Investigators. Circulation. 1995;91(6):1659–1668. doi: 10.1161/01.cir.91.6.1659. [DOI] [PubMed] [Google Scholar]
- 37.Manson JE, Stampfer MJ, Hennekens CH, Willett WC. Body weight and longevity: a reassessment. JAMA. 1987;257(3):353–358. [PubMed] [Google Scholar]
- 38.Santos ES, Minuzzo L, Pereira MP, Castillo MT, Palácio MA, Ramos RF, et al. Acute coronary syndrome registry at a cardiology emergency center. Arq Bras Cardiol. 2006;87(5):597–602. doi: 10.1590/s0066-782x2006001800008. [DOI] [PubMed] [Google Scholar]
- 39.Nicolau JC, Franken M, Lotufo PA, Carvalho AC, Marin JA, Neto, Lima FG, et al. Use of demonstrably effective therapies in the treatment of acute coronary syndromes: comparison between different Brazilian regions. Analysis of the Brazilian Registry on Acute Coronary Syndromes (BRACE) Arq Bras Cardiol. 2012;98(4):282–289. doi: 10.1590/s0066-782x2012000400001. [DOI] [PubMed] [Google Scholar]