Abstract
Objective
Following traumatic brain injury (TBI), older adults are at increased risk of hemorrhagic and thromboembolic events, but it is unclear whether the increased risk continues after hospital discharge. We estimated incidence rates of hemorrhagic and ischemic stroke following hospital discharge for TBI among adults ≥65 and compared them with pre-TBI rates.
Participants
16,936 Medicare beneficiaries aged ≥65 with a diagnosis of TBI in any position on an inpatient claim between 6/1/2006 and 12/31/2009 who survived to hospital discharge.
Design
Retrospective analysis of a random 5% sample of Medicare claims data
Main Measures
Hemorrhagic stroke was defined as ICD-9 codes 430.xx-432.xx. Ischemic stroke was defined as ICD-9 codes 433.xx-435.xx, 437.0x, and 437.1x.
Results
There was a six-fold increase in the rate of hemorrhagic stroke following TBI compared to the pre-TBI period (adjusted Rate Ratio (RR) 6.5; 95% Confidence Interval (CI) 5.3, 7.8), controlling for age and sex. A smaller increase in the rate of ischemic stroke was observed (adjusted RR 1.3; 95% CI 1.2, 1.4).
Conclusion
Future studies should investigate causes of increased stroke risk post-TBI as well as effective treatments to reduce stroke risk and improve outcomes post-TBI among older adults.
Keywords: Traumatic brain injury, Hemorrhagic stroke, Ischemic stroke, Older adults
Introduction
Traumatic brain injury (TBI) is a significant health problem among older adults that results in 142,000 emergency department visits, 81,500 hospitalizations, and 14,300 deaths annually in the United States.1
Older adults have poor short-term outcomes following TBI including higher in-hospital mortality rates and lower functional abilities at hospital discharge compared to younger patients with similar TBI injury severity.2-4 Mild TBI, which can result in a period of transient confusion, disorientation, or impaired consciousness and accounts for more than 75% of TBI cases, is also associated with higher mortality in older versus younger adults.5,6
Older adults also experience poor long-term outcomes following TBI. Compared to younger patients with TBI, older adults have greater disability in physical and cognitive functioning up to one year after hospital discharge.7-10 This leads to increased hospitalizations and nursing home stays among older adults, and results in high one-year treatment costs.11 One study estimated average per-patient treatment costs in the first year following TBI among adults aged ≥55 to be $80,000, and the lifetime cost of TBI among older adults due to persistent disability and the risk of long-term sequelae is likely much greater.11-16
Stroke can cause increased disability among older adults post-TBI. Older adults are at increased risk of both intracranial hemorrhage and thromboembolic events during hospitalization for TBI.17,18 However, it is unclear whether the increased risk continues during the year after hospital discharge. The aim of this study was to estimate incidence rates of hemorrhagic and ischemic stroke following hospital discharge for TBI among Medicare beneficiaries aged ≥65 and compare them with pre-TBI rates.
Methods
The study population was selected from a 5% random sample of Medicare beneficiaries aged ≥65 years with a diagnosis of TBI (International Classification of Disease, 9th Revision (ICD-9) codes 800.xx, 801.xx, 803.xx, 804.xx, 850.xx- 854.1x, 950.1-950.3, 959.01) in any position on an inpatient claim between 6/1/2006 and 12/31/2009.1 We created episodes of care based on Medicare administrative claims data from the following sources: 2006-2009 Master Beneficiary Summary file, which includes demographic, entitlement, and location information, 2006-2009 5% Chronic Condition Summary file, which contains information on 21 (in our data) chronic conditions, and 2006-2009 5% Inpatient (short and long stay hospitals), Outpatient, Skilled Nursing Facility, and Hospice file, which contains final action fee-for-service claims data from all facilities and includes diagnosis and procedure ICD-9 codes, dates of service, and reimbursement.
New claims for TBI occurring within 24 hours of a previous TBI discharge were combined to form a single hospitalization episode with an admission date reflecting the earliest TBI claim's admission date and a discharge date reflecting the latest TBI claim's discharge date (N=21,155). We included only the first hospitalization for TBI for each beneficiary discharged alive (N=19,351), however we created a counter for the number of TBI claims so we were able to track the number of TBIs/patient. We excluded 334 who died in the hospital. To ensure that we captured indicators for baseline comorbidities, we required a minimum of six months of observation time before the TBI hospitalization (N=16,936). Beneficiaries with Medicare Advantage Plans (Part C) were excluded because their inpatient claims are not captured in the Chronic Condition Data Warehouse (CCW) Medicare database available through the Centers for Medicare & Medicare Services (CMS), which was the source of data used for this study.
Beneficiaries contributed follow-up time to our study if they were enrolled in Medicare Parts A and B, with no Part C enrollment, at any time between 6/1/2006 and 12/31/2009 and were selected as part of the 5% random sample. Once entered into the cohort, beneficiaries continued to contribute follow-up time until 12/31/2009 unless they 1) were deceased, or 2) enrolled in a Medicare Advantage (Part C) plan. Therefore, depending on age and enrollment status, each beneficiary could contribute between a minimum of 6 months and a maximum of 48 months follow-up time. Finally, TBI events occurred throughout the study period. Thus, a beneficiary could have more pre-TBI than post-TBI follow-up time depending on the timing of the TBI event.
We searched inpatient, outpatient, skilled nursing, hospice, home health, and durable medical equipment claims to capture new hemorrhagic and ischemic stroke events. To ensure that we were capturing only new events post-TBI, we required that there be an interval of at least two weeks between discharge from the index TBI hospitalization and a subsequent hospitalization for hemorrhagic or ischemic stroke. Patients whose first hemorrhagic or ischemic stroke occurred within two weeks of admission for/discharge from TBI are not included in these analyses. Hemorrhagic stroke following hospital discharge for TBI was defined as ICD-9 codes 430.xx-432.xx in any position on a claim with an admission date at least 14 days after the discharge date for the first TBI hospitalization during the study period. Ischemic stroke was defined as ICD-9 codes 433.xx-435.xx, 437.0x, 437.1x in any position on a claim with an admission date at least 14 days after the discharge date for the first TBI hospitalization during the study period.
Baseline comorbidities at TBI hospitalization were determined using CMS's CCW flagged comorbid conditions in conjunction with date of first diagnosis.19 Only 21 of the 27 chronic conditions identified based on the presence of ICD-9 codes on inpatient, skilled nursing, home health, or outpatient claims using algorithms defined by CMS were available in these data because they weren't available on the date of the initial data request. We are missing indicator variables for hypertension, hyperlipidemia, benign prostatic hyperplasia, acquired hypothyroidism, anemia, and asthma. If the date of first diagnosis of a particular chronic condition was prior to the date of TBI hospitalization, the patient was considered to have that chronic condition at baseline. We used the date of first stroke to determine comorbidities at baseline for beneficiaries who experienced a hemorrhagic or ischemic stroke prior to TBI for our regression analyses. We created a variable indicating the number of chronic conditions present. For this variable, we included the following chronic conditions: Alzheimer's disease and related dementias, heart failure, chronic obstructive pulmonary disease, diabetes, chronic kidney disease, depression, and atrial fibrillation. Three age categories were created: 65 to ≤74, 75 to ≤85 and ≥85.
Beneficiaries had different lengths of follow-up time post-TBI. We did not require a minimum follow-up time but rather calculated annual incidence rates of hemorrhagic and ischemic stroke using the number of months of coverage for Medicare Parts A and B with no Part C (Medicare Advantage Plans) following hospital discharge for TBI as the denominator. Annual incidence rates per 1,000 and ninety-five percent confidence intervals are reported by sex and overall.
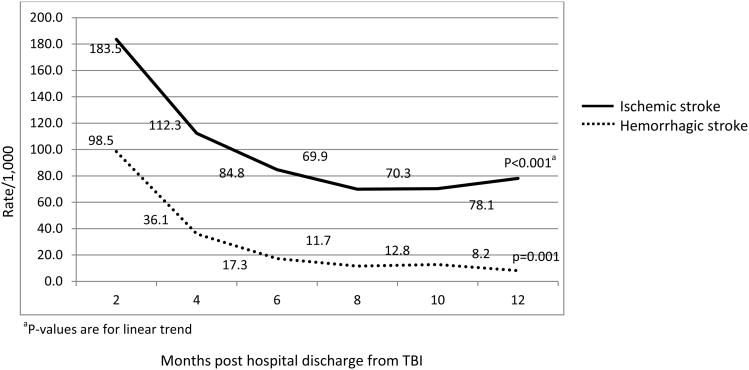
To examine how quickly incidence rates were approaching baseline values, we calculated incidence rates within each time interval (>0 to ≤ 2 months, >2 to ≤4 months, >4 to ≤ 6 months, >6 to ≤8 months, >8 to ≤10 months and >10 to ≤12 months). We tested for trends in the rates over time using linear regression with quadratic time terms as necessary to achieve the best model fit.
To determine if TBI increased the risk of hemorrhagic and ischemic stroke we compared incidence rates among patients who experienced a stroke before TBI with incidence rates among patients who experienced a stroke after TBI. Hemorrhagic and ischemic stroke are rare events and no patients experienced the same type of stroke (hemorrhagic or ischemic) both before and after TBI. For events occurring before the TBI hospitalization, we required a two-week period between discharge from hospitalization for a hemorrhagic or ischemic stroke and admission for a TBI. Incidence rates of hemorrhagic and ischemic stroke occurring before the TBI hospitalization were calculated using the number of pre-TBI months of coverage for Medicare Parts A and B with no Part C as the denominator.
We used generalized linear models with a Poisson distribution and log link to generate rate ratios comparing the rate of either hemorrhagic or ischemic stroke post-TBI with rates pre-TBI, accounting for the correlation between beneficiaries pre/post-TBI while controlling for important confounders. We assessed the associations between pre- and post-TBI hemorrhagic and ischemic stroke with the following baseline comorbidities that were available in our data: Alzheimer's disease and related dementias, acute myocardial infarction, cataract, heart failure, chronic kidney disease, cancer, chronic obstructive pulmonary disease, depression, diabetes, glaucoma, hip/pelvic fracture, ischemic heart disease, osteoporosis, osteoarthritis, stroke/transient ischemic attack. We also examined sex, age and race. Potential confounders were included in our regression models if they were significantly associated with pre- and post-TBI hemorrhagic or ischemic stroke. Our adjusted model for hemorrhagic stroke included age, sex, atrial fibrillation, Alzheimer's disease and related dementias, depression, hip fracture, heart failure, osteoarthritis, and rheumatoid arthritis. Our adjusted model for ischemic stroke included age, race, atrial fibrillation, Alzheimer's disease and related dementias, depression, hip fracture, heart failure, acute myocardial infarction, diabetes, glaucoma, cataracts, chronic kidney disease, prostate cancer, chronic obstructive pulmonary disease, stroke/transient ischemic attack, and rheumatoid arthritis.
Statistical significance was defined as p<0.05. All analysis was performed with SAS version 9.2 (Cary, NC). This study was approved by the Institutional Review Board of the University of Maryland, Baltimore.
Results
In our 5% sample of Medicare beneficiaries aged ≥65, there were 20,984 TBI hospitalizations between 2006 and 2009. The number of TBI hospitalizations per beneficiary ranged from 1 to 7, with 89% experiencing one TBI, 9% experiencing two TBIs, and 2% experiencing three or more TBIs. The TBI cohort included 16,936 unique beneficiaries who survived to hospital discharge with at least 6 months of Medicare Parts A and B and no Part C coverage prior to the first TBI.
Average age was 81.0 (standard deviation (s.d.) 7.9) years, 62% were female, and 90% were white (Table 1). The prevalence of the comorbidities included in our comorbidity count variable (i.e. Alzheimer's disease and related dementias, heart failure, chronic obstructive pulmonary disease, diabetes, chronic kidney disease, depression, and atrial fibrillation) was high, with 46% having three or more comorbidities and 15% with no comorbidity. The most common comorbidities were heart failure (46%) and history of depression (41%). Patients who experienced either a hemorrhagic or ischemic stroke pre-TBI differed significantly from those who experienced a hemorrhagic or ischemic stroke post-TBI (data not shown). They were significantly older (82.2 (s.d.8.0) years vs. 80.2 (s.d.7.5) years, p=0.009) and had a greater mean number of comorbidities (3.1 (s.d.1.7) vs. 2.4 (s.d.1.7), p<0.001).
Table 1. Characteristics of 5% sample of Medicare beneficiaries aged ≥65 hospitalized with traumatic brain injury in 2006-2009, n=16,936.
| Characteristic | |
|---|---|
| Mean age (years) (standard deviation) | 81.0 (7.9) |
| Age group (years), n (%) | |
| 65-75 | 3,889 (23) |
| 75-84 | 6,906 (41) |
| ≥85 | 6,141 (36) |
| Sex, n (%) | |
| Female | 10,557 (62) |
| Male | 6,379 (38) |
| Race, n (%) | |
| White | 15,175 (90) |
| Black | 876 (5) |
| Other | 885 (5) |
| Comorbid disease at TBI hospitalization, n (%) | |
| Alzheimer's disease and related dementias | 5,706 (34) |
| Heart failure | 7,869 (46) |
| Chronic obstructive pulmonary disease | 5,308 (31) |
| Diabetes | 6,535 (39) |
| Atrial fibrillation | 4,664 (28) |
| Rheumatoid arthritis | 8,844 (52) |
| History of depression | 6,877 (41) |
The incidence rate of hemorrhagic stroke decreased significantly over the 12 months following discharge from TBI hospitalization (p=0.001). (Figure 1) The incidence rate of ischemic stroke also decreased significantly over the year following hospital discharge (p<0.001). Both curves display a steeply decreasing slope over the first 4 months post hospital discharge.
Figure 1. Annualized incidence rates per 1,000 within time intervals over the year following hospital discharge for traumatic brain injury among Medicare beneficiaries aged ≥65, n=16,936.
aP-values are for linear trend
The annualized incidence rate per 1,000 for hemorrhagic stroke following TBI was 23.9 (95% confidence interval (CI) 21.8, 26.3) (Table 2). Rates for men and women were similar. There was a six-fold higher rate of hemorrhagic stroke post-TBI compared to pre-TBI (23.9 versus 3.7 per 1,000, respectively) (adjusted RR 6.5; 95% CI 5.3, 7.8). We also investigated whether the increase in incidence was similar for both intra-cerebral hemorrhage and sub-arachnoid hemorrhage. The rate ratio of intra-cerebral hemorrhage comparing post-TBI to pre-TBI indicated a seven-fold increase (adjusted RR 6.8; 95% CI 5.5, 8.3) while the rate ratio for sub-arachnoid hemorrhage was even higher (RR 10.1; 95% CI 7.4, 13.7).
Table 2. Unadjusted (95% confidence intervals) annualized incidence rates per 1,000, before and after hospitalization for traumatic brain injury among Medicare beneficiaries aged ≥65, n=16,936.
| Outcome | Overall | Women | Men |
|---|---|---|---|
| Pre-TBI hospitalization | |||
| Hemorrhagic stroke, N=131 | 3.7 (3.1,4.4) | 3.6 (2.9, 4.5) | 3.7 (2.8, 5.0) |
| Ischemic stroke, N=2,508 | 70.5 (67.8, 73.4) | 70.9 (67.5, 74.5) | 69.9 (65.6, 74.6) |
| Post-TBI hospitalization | |||
| Hemorrhagic stroke, N=447 | 23.9 (21.8, 26.3) | 23.2 (20.6, 26.1) | 25.3 (21.7, 29.4) |
| Ischemic stroke, N=1,576 | 84.4 (80.3, 88.6) | 84.6 (79.6, 90.0) | 83.9 (77.2, 91.2) |
The annualized incidence rate per 1,000 for ischemic stroke following TBI was 84.4 (95% CI 80.3, 88.6). (Table 2) Rates for men and women were similar. The rate of ischemic stroke was higher post-TBI than pre-TBI (84.4 versus 70.5 per 1,000, respectively) (adjusted RR 1.3; 95% CI 1.2, 1.4).
Discussion
In this national sample of Medicare beneficiaries aged ≥65 hospitalized for TBI, we observed elevated rates of both hemorrhagic and ischemic stroke following hospital discharge compared to pre-TBI rates. Incidence rates of hemorrhagic and ischemic stroke were highest in the month after discharge from TBI hospitalization and decreased over time. To our knowledge, this is the first study that provides estimates of hemorrhagic and thrombotic events following TBI among older adults using nationally representative data.
Overall annualized rates of hemorrhagic stroke (includes both intra-cerebral hemorrhage and sub-arachnoid hemorrhage) were over six times higher following hospital discharge for TBI than pre-TBI rates. This increase is similar to results reported by Chen et al. (2011) for intra-cerebral hemorrhage using data from a large retrospective cohort study conducted in Taiwan.12 In that study, 23,199 TBI cases were matched 2:1 with non-TBI controls and followed for up to five years to determine stroke incidence. Patients with TBI had an increased hazard of intra-cerebral hemorrhage compared to non-TBI controls (hazard ratio(HR) 6.3; 95% CI 5.6, 7.8).
The hazard ratio of sub-arachnoid stroke reported in Chen's study was lower (HR 4.9; 95% CI 3.8, 7.2), and contrasts with the results of our study in which the rate of sub-arachnoid stroke post-TBI was ten times higher than pre-TBI rates. The difference in sub-arachnoid hemorrhage rate ratios between this study and Chen's is likely due to the older age of our study participants, who may be more likely to suffer from sub-arachnoid hemorrhage due to unreported head injury.
TBI can result in cerebral hemorrhage; therefore, elevated rates of hemorrhagic stroke immediately following TBI are not unexpected. Incidence rates of hemorrhagic stroke were highest in the two months following hospital discharge for TBI and decreased over time. Nonetheless, the rate of hemorrhagic stroke in the 10-12 month time interval post-TBI was double the pre-TBI rate, suggesting that the increased risk of hemorrhagic stroke persists for at least one year post-TBI.
Annualized rates of ischemic stroke following TBI were 30% higher compared to pre-TBI rates. This is consistent with estimates from the study conducted in Taiwan (HR 1.4; 95% CI 1.3, 1.6) as well as a more recent retrospective study conducted in the United States that examined ischemic stroke risk after TBI in adults aged 18 and older (HR 1.31; 95% CI 1.25–1.36).12,20 Incidence rates of ischemic stroke were highest in the two months following hospital discharge and rapidly approached pre-TBI rates.
This study had certain limitations. Claims data are designed for reimbursement, not research, and can have missing information and coding errors. Head trauma in older adults could be recorded as hemorrhagic stroke rather than as a traumatic brain injury. This would likely result in higher observed rates of stroke pre-TBI due to the increase in detection of TBI after the event, and would bias results toward the null. Although we had information on many risk factors for stroke (e.g.atrial fibrillation, prior stroke, diabetes, and heart failure for ischemic stroke, and prior hemorrhagic stroke and hypertension for hemorrhagic stroke), we were missing information on anemia, a known risk factor for hemorrhagic stroke, and hypertension, a risk factor for both hemorrhagic and ischemic stroke.
The increased risk of both hemorrhagic and ischemic stroke following TBI among patients aged ≥65 raises concerns because prophylactic treatments for ischemic stroke include anticoagulation therapy which could increase hemorrhagic stroke risk and may be contraindicated post-TBI. There are currently no national guidelines regarding stroke prophylaxis following hospital discharge from TBI. Future studies should investigate causes of increased stroke risk post-TBI as well as effective treatments to reduce stroke risk and improve outcomes post-TBI among older adults.
Acknowledgments
This work was supported by National Institutes of Health grant R21 AG042768-01 (Zuckerman, PI). Dr. Albrecht is supported by National Institutes of Health grant T32AG000262-14 (Magaziner, PI)
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
References
- 1.Faul M, Xu L, Wald MM, Coronado V. Atlanta, Georgia: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. [Accessed 5/3/13]. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths, 2002-2006. Available at: http://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf. [Google Scholar]
- 2.Thompson HJ, McCormick WC, Kagan SH. Traumatic Brain Injury in Older Adults: Epidemiology, Outcomes, and Future Implications. J Am Geriatr Soc. 2006;54:1590–1595. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harvey LA, Close JCT. Traumatic brain injury in older adults: characteristics, causes and consequences. Injury, Int J Care Injured. 2012;43:1821–1826. doi: 10.1016/j.injury.2012.07.188. [DOI] [PubMed] [Google Scholar]
- 4.Mosenthal AC, Lavery RF, Addis M, Kaul S, Ross S, Marburger R, Deitch EA, Livingston DH. Isolated Traumatic Brain Injury: Age Is an Independent Predictor of Mortality and Early Outcome. J Trauma. 2002;52:907–911. doi: 10.1097/00005373-200205000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Susman M, DiRusso SM, Sullivan T, Risucci D, Nealon P, Cuff S, Haider A, Benzil D. Traumatic Brain Injury in the Elderly: Increased Mortality and Worse Functional Outcome At Discharge Despite Lower Injury Severity. J Trauma. 2002:53, 219–224. doi: 10.1097/00005373-200208000-00004. [DOI] [PubMed] [Google Scholar]
- 6.National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 7.Livingston DH, Lavery RF, Mosenthal AC, Knudson MM, Lee S, Morabito D, Manley GT, Nathens A, Jurkovich G, Hoyt DB, Coimbra R. Recovery at One Year Following Isolated Traumatic Brain Injury: A Western Trauma Association Prospective Multicenter Trial. J Trauma. 2005:59, 1298–1304. doi: 10.1097/01.ta.0000196002.03681.18. [DOI] [PubMed] [Google Scholar]
- 8.Utomo WK, Gabbe BJ, Simpson PM, Cameron PA. Predictors of In-Hospital Mortality and 6-month Functional Outcomes in Older Adults after Moderate to Severe Traumatic Brain Injury. Injury, Int J Care Injured. 2009;4:973–977. doi: 10.1016/j.injury.2009.05.034. [DOI] [PubMed] [Google Scholar]
- 9.Selassie AW, Zaloshnja E, Langlois JA, Miller T, Jones P, Steiner C. Incidence of Long-term Disability Following Traumatic Brain Injury Hospitalization, United States, 2003. J Head Trauma Rehabil. 2008:23, 123–131. doi: 10.1097/01.HTR.0000314531.30401.39. [DOI] [PubMed] [Google Scholar]
- 10.Gubler KD, Davis R, Koepsell T, Soderberg R, Maier RV, Rivara FP. Long-term Survival of Elderly Trauma Patients. Arch Surg. 1997:132, 1010–1014. doi: 10.1001/archsurg.1997.01430330076013. [DOI] [PubMed] [Google Scholar]
- 11.Thompson HJ, Weir S, Rivara FP, Wang J, Sullivan SD, Salkever D, MacKenzie EJ. Utilization and Costs of Health Care after Geriatric Traumatic Brain Injury. J Neurotrauma. 2012;29:1864–1871. doi: 10.1089/neu.2011.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen YH, Kang JH, Lin HC. Patients With Traumatic Brain Injury Population-Based Study Suggests Increased Risk of Stroke. Stroke. 2011:42, 2733–2739. doi: 10.1161/STROKEAHA.111.620112. [DOI] [PubMed] [Google Scholar]
- 13.Yeh CC, Chen TL, Hu CH, Chiu WT, Liao CC. Risk of epilepsy after traumatic brain injury: a retrospective population-based cohort study. J Neurol Neurosurg Psychiatry. 2013;84:441–445. doi: 10.1136/jnnp-2012-302547. [DOI] [PubMed] [Google Scholar]
- 14.Masel BE, DeWitt DS. Traumatic Brain Injury: A Disease Process, Not an Event. J Neurotrauma. 2010;27:1529–1540. doi: 10.1089/neu.2010.1358. [DOI] [PubMed] [Google Scholar]
- 15.Moretti L, Cristofori I, Weaver SM, Chau A, Portelli JN, Grafman J. Cognitive decline in older adults with a history of traumatic brain injury. Lancet Neurol. 2012:11, 1103–1112. doi: 10.1016/S1474-4422(12)70226-0. [DOI] [PubMed] [Google Scholar]
- 16.Zaloshnja E, Miller T, Langlois JA, Selassie AW. Prevalence of Long-Term Disability From Traumatic Brain Injury in the Civilian Population of the United States, 2005. J Head Trauma Rehabil. 2008:23, 394–400. doi: 10.1097/01.HTR.0000341435.52004.ac. [DOI] [PubMed] [Google Scholar]
- 17.Knudson MM, Ikossi DG, Khaw L, Morabito D, Speetzen LS. Ann Surg. 2004. Thromboembolism After Trauma:An Analysis of 1602 Episodes From the American College of Surgeons National Trauma Data Bank; pp. 240pp. 490–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Subaiya S, Roberts I, Komolafe E, Pablo P. Predicting intracranial hemorrhage after traumatic brain injury in low and middle-income countries: A prognostic model based on a large, multi-center, international cohort. BMC Emergency Medicine. 2012;12:17. doi: 10.1186/1471-227X-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Medicare and Medicaid Services Chronic Condition Data Warehouse. [Accessed 5/3/13]; Available at: http://www.ccwdata.org/web/guest/condition-categories.
- 20.Burke JF, Stulc JL, Skolarus LE, Sears ED, Zahuranec DB, Morgenstern LB. Traumatic brain injury may be an independent risk factor for stroke. Neurology. 2013;81:33–39. doi: 10.1212/WNL.0b013e318297eecf. [DOI] [PMC free article] [PubMed] [Google Scholar]