Abstract
Background and objectives
Patients with ESRD on dialysis live in a complex sociomedical situation and are dependent on technology and infrastructure, such as transportation, electricity, and water, to sustain their lives. Interruptions of this infrastructure by natural disasters can result in devastating outcomes.
Design, setting, participants, & measurements
Between November of 2013 and April of 2014, a cross-sectional survey was conducted of patients who received maintenance hemodialysis before and after the landfall of Hurricane Sandy on October 29, 2012 in lower Manhattan, New York. The primary outcome was the number of missed dialysis sessions after the storm. Dialysis-specific and general disaster preparedness were assessed using checklists prepared by the National Kidney Foundation and US Homeland Security, respectively.
Results
In total, 598 patients were approached, and 357 (59.7%) patients completed the survey. Participants were 60.2% men and 30.0% black, with a median age of 60 years old; 94 (26.3%) participants missed dialysis (median of two sessions [quartile 1 to quartile 3 =1–3]), and 236 (66.1%) participants received dialysis at nonregular dialysis unit(s): 209 (58.5%) at affiliated dialysis unit(s) and 27 (7.6%) at emergency rooms. The percentages of participants who carried their insurance information and detailed medication list were 75.9% and 44.3%, respectively. Enhancement of the dialysis emergency packet after the hurricane was associated with a significantly higher cache of medical records at home at follow-up survey (P<0.001, Fisher’s exact test). Multivariate Poisson regression analysis showed that dialysis-specific preparedness (incidence rate ratio, 0.91; 95% confidence interval, 0.87 to 0.98), other racial ethnicity (incidence rate ratio, 0.34; 95% confidence interval, 0.20 to 0.57), dialysis treatment in affiliated units (incidence rate ratio, 0.69; 95% confidence interval, 0.51 to 0.94), and older age (incidence rate ratio, 0.98; 95% confidence interval, 0.97 to 0.99) were associated with a significantly lower incidence rate ratio of missed dialysis.
Conclusions
There is still room to improve the preparedness for natural disasters of patients with ESRD. Provider- or facility-oriented enhancement of awareness of the disease and preparedness should be a priority.
Keywords: dialysis, ESRD, epidemiology and outcomes
Introduction
Patients with ESRD on dialysis live in a complex sociomedical situation and are dependent on technology and infrastructure, such as transportation, electricity, and water supply, for dialysis apparatus to sustain their lives. Although infrequent, natural disasters, such as hurricanes, tornados, or earthquakes, readily disrupt this infrastructure and can result in devastating outcomes (1–6).
Hurricane Sandy, which hit greater New York on October 29, 2012, caused a storm surge with flooding followed by an explosion at the East River ConEdison power plant. The interruption of the electric supply to lower Manhattan (below 39th Street) for an entire week was a disaster for patients with ESRD (7). Many patients lost elevator access, motor transportation, and telephonic communication to regular dialysis units or backup facilities. Only one unit was equipped with electric generators on landfall. Other dialysis facilities were unable to resume regular operation for days to several months because of the electricity loss, unavailability of water, flood damage, or sanitation problems. Beth Israel Medical Center (now Mount Sinai Beth Israel [MSBI]) was the only large medical center in lower Manhattan to provide continuous care during the storm through the use of in situ electric generators and a multidisciplinary effort to triage patients on dialysis (8,9). MSBI accepted >70 patients on hemodialysis who presented to the Emergency Department for dialysis (Gotanda, H. et al., personal communications); they were triaged on the basis of serum potassium level on venous blood gas estimation to either emergent dialysis with admission (>30 patients) or relocated to other dialysis facilities or their home with instructions on emergency diet and oral potassium ion exchange resin (sodium polystyrene sulfonate) use.
The Department of Health and Human Services released data on “Hospital Emergency Preparedness and Response during Superstorm Sandy” on the basis of a survey of 174 Medicare-certified hospitals located in 40 counties declared as disaster areas in Connecticut, New Jersey, and New York and site visits to 10 select hospitals located in areas most affected by the storm (10). Their survey found that 89% of hospitals reported experiencing critical challenges during the storm, including hospital infrastructure (electrical utilities, backup generator, structural damage, and flooding), patient surge (from other hospitals, home care, nursing homes, etc.), communication, and staffing.
Similar challenges were likely evident in hemodialysis units. An evaluation of the effect of Hurricane Sandy on kidney care by the Kidney Community Emergency Response is in process (11). Kelman et al. (12) recently published data on the adverse outcomes of the storm using the Centers for Medicare and Medicaid Services (CMS) claims data for patients on dialysis in the State of New Jersey and the five New York City boroughs (Brooklyn, Manhattan, Queens, Staten Island, and the Bronx). Among 13,264 patients with ESRD, Kelman et al. (12) found increased emergency room (ER) visits and hospitalizations as well as an increased 30-day mortality rate compared with a similarly sized comparison group.
The effect on the lives of patients on dialysis that we witnessed firsthand as the only functioning medical center during the storm motivated us to conduct a cross-sectional 1-year follow-up survey of disaster preparedness of patients on hemodialysis in the wake of Hurricane Sandy.
Materials and Methods
Study Design
We conducted a systematic cross-sectional follow-up study of patients on hemodialysis in lower Manhattan who received maintenance hemodialysis at the time of Hurricane Sandy.
Setting and Population
Patients receiving dialysis care at five of eight dialysis facilities located in lower Manhattan, where electricity was deprived during the storm, were included in the study. One unit had not reopened, and patients had dispersed (Veterans Affairs Medical Center Dialysis Unit); also, we could not reach an agreement with two units to participate in the study (Fresenius Medical Care Southern Manhattan [chair number =24] and New York Downtown Hospital Dialysis Unit [chair number =7]). The included dialysis units (chair number in parentheses) are River Renal Services (Bellevue Hospital Dialysis Unit; 18; two shifts), Lower Manhattan Dialysis Center (30; four shifts), Lower Manhattan Dialysis Center II (14; three shifts), Avantus Irving Place Dialysis Center (26; four shifts), and Chinatown Dialysis Center Inc. (36; three shifts). The chair numbers and lists of dialysis centers were obtained from the Medicare homepage. The survey was conducted between November of 2013 and April of 2014. Of a potential 820 slots calculated from chair and shift numbers, 598 participants were selected and approached as a convenience sample. Participants <18 years of age or unable to comprehend the informed consent process (including history of dementia) were excluded from this convenience sample in advance (Figure 1). After the data collection, personally identifiable information was deleted from the datasets, and each participant was assigned to one random numeric number as an identifier to secure anonymity. This anonymous dataset was used for additional statistical analyses. Ethical considerations, including Health Insurance Portability and Accountability Act compliance during patient information gathering, were addressed in the submission to the Institutional Review Board. The study protocol was approved by the Institutional Review Board of the Beth Israel Medical Center (approval number 072–13).
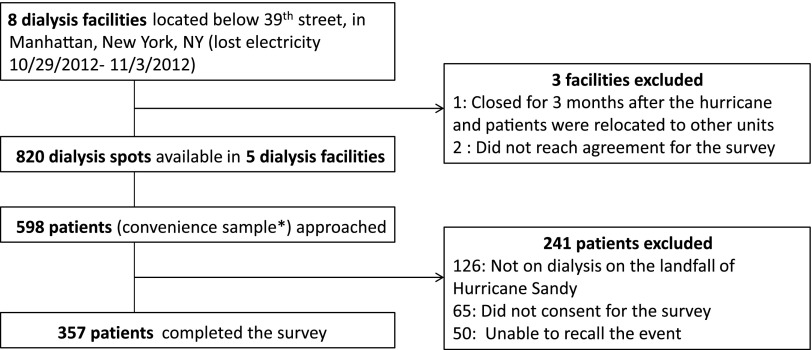
Figure 1.
Outline of the survey. Of a potential 820 slots calculated from chair and shift numbers, 598 participants were selected and approached as a convenience sample. *Participants younger than 18 years of age or unable to comprehend the informed consent process (including history of dementia) were excluded from this convenience sample in advance.
Study Protocol
Study participants were interviewed during their dialysis sessions, were informed of the study purpose, and provided written informed consent for interviews and review of medical records. The survey was completed by the participant or read to them by a researcher. Non-English–speaking participants were interviewed by an on-site interpreter.
Distribution of the Dialysis Emergency Packet
After Hurricane Sandy, three of five facilities reinforced the emergency plan by distributing a dialysis emergency packet. The contents included (1) contact number for their regular dialysis unit, (2) contact number for the Island Peer Review Organization ESRD Network of New York (Network 2), (3) contact number for an alternative dialysis center, (4) medical problem list, (5) dialysis prescriptions, (6) home medication list, (7) infection status (viral hepatitis and HIV), (8) emergency kit checklist (on the basis of the National Kidney Foundation [NKF] recommendations), and (9) emergency diet planner (low potassium and fluid restriction). We assessed how this enhancement was associated with participants’ emergency preparedness at 1-year follow-up by comparing two groups (with and without enhancement of the packet) on the cache of medical records at home and knowledge of other dialysis facilities.
Study Instruments
The survey consisted of three parts: (1) dialysis-specific disaster preparedness, (2) general disaster preparedness, and (3) demographics. Dialysis-specific disaster preparedness was assessed using the NKF-recommended dialysis-specific disaster preparedness checklist (13) (Table 1, dialysis-specific preparedness). The participants were asked if their disaster preparedness had changed from before to after the storm (referring to the 13-item NKF checklist). If the answer was no, then the participants were asked to check all of the items that they had prepared at the time of interview. If the answer was yes, then they were asked to provide items that they newly prepared after the storm as well as items that they had before the storm. General disaster preparedness was assessed using the 15-item checklist proposed by the Department of Homeland Security (14) (Table 1, general disaster preparedness). Participants’ demographic information and early dialysis treatment logs were obtained from medical records.
Table 1.
Instruments of the survey: Dialysis-specific preparedness checklist and the Department of Homeland Security 15-item checklist
| Dialysis-Specific Preparedness (National Kidney Foundation) | General Disaster Preparedness; Department of Homeland Security 15-Item Checklist |
|---|---|
| (1) Insurance information | (1) First aid kit |
| (2) Detailed list of medicines to bring with you | (2) Working flashlight |
| (3) Friend or relative with whom to stay | (3) Working battery-powered portable radio |
| (4) Plans to get to safety if disaster is imminent | (4) Spare batteries |
| (5) Knowledge of other dialysis centers | (5) Mess kit or paper cups, plates, and plastic utensils |
| (6) Medical records at home | (6) Cash or traveler’s check |
| (7) Discussed with relative | (7) Nonelectric can opener or utility knife |
| (8) Necklace/bracelet identifier | (8) Antibacterial wipes or gel |
| (9) Extra medicines (2-wk supply) | (9) Personal hygiene items |
| (10) Knowledge of renal emergency diet | (10) Toilet paper or towelettes |
| (11) Stored extra food | (11) One change of clothes per person |
| (12) Knowledge of polystyrene sulfonate | (12) Blanket or sleeping bag per person |
| (13) Polystyrene sulfonate at home | (13) Essential medications |
| (14) Extra keys for house and car | |
| (15) List of emergency phone numbers |
Data Analyses
To evaluate the association between the distribution of the emergency packet and the endorsed dialysis-specific preparedness items at the survey period (1–1.5 years after the hurricane), a Fisher’s exact test was used for cross-tabulated data (Supplemental Table 1).
The effect of factors on the number of missed dialysis sessions was assessed by means of stepwise Poisson regression analyses. Dialysis-specific preparedness score and general preparedness score were defined as the numbers of checklist items fulfilled on the basis of the NKF and the Department of Homeland Security, respectively. Analyzed as candidate covariates in the initial step were dialysis-specific preparedness score, general preparedness score, age, sex, ethnicity, body mass index, vintage of dialysis, comorbidities (hypertension, diabetes, coronary artery diseases, atrial fibrillation, and chronic heart failure), dialysis in other units (ER or affiliated units), knowledge of other dialysis centers, living with family, dialysis access (arteriovenous fistula, arteriovenous graft, or catheter), and evacuation requirement. Thereafter, significant covariates (dialysis-specific preparedness score, age, ethnicity, dialysis in other units, and evacuation requirement) were used to calculate incidence rate ratios (IRRs). All statistical analyses were conducted using Stata Statistical Software: Release 13 (StataCorp LP).
Results
Effect of Hurricane Sandy on Patients on Dialysis
Of 598 participants approached, 357 (59.7%) completed the survey; 126 (21.1%) were not on dialysis on the landfall, 65 (10.9%) did not provide consent, and 50 (8.4%) failed to recall the event precisely and did not complete the survey (Figure 1). Demographic data were retrieved from medical records (Table 2). Participants were 60.2% men, median age was 60 years old (first to third quartile [Q1–Q3]=50–70 years old), and they had widely distributed racial ethnicity, with 30.0% black. Most participants had multiple comorbidities, including hypertension (89.9%), diabetes mellitus (40.6%), dyslipidemia (40.3%), and coronary artery disease (31.1%); 77.0% had arteriovenous fistulas as dialysis access, and the median length of hemodialysis on landfall was 2.8 years (Q1–Q3=1.2–5.7 years).
Table 2.
Demographics of participants
| n (Total =357) | Percentage | |
|---|---|---|
| Sex | ||
| Men | 215 | 60.2 |
| Women | 142 | 39.8 |
| Age (yr), median | 60 | Interquartile range =50–70 |
| ≤50 | 93 | 26.1 |
| 51–60 | 87 | 24.4 |
| 61–70 | 90 | 25.2 |
| >70 | 87 | 24.4 |
| Racial identity | ||
| Black | 107 | 30.0 |
| White | 53 | 14.8 |
| Hispanic/Latino | 104 | 29.1 |
| Other | 93 | 26.1 |
| Comorbidity | ||
| Hypertension | 321 | 89.9 |
| Diabetes | 145 | 40.6 |
| Dyslipidemia | 144 | 40.3 |
| Coronary artery disease | 111 | 31.1 |
| Systolic heart failure | 50 | 14.0 |
| Atrial fibrillation | 45 | 12.6 |
| Dialysis access | ||
| Arteriovenous fistula | 275 | 77.0 |
| Arteriovenous graft | 53 | 14.8 |
| Catheter | 29 | 8.1 |
| Body mass index | 26.1±6.1 | |
| Length of time on dialysis (yr), median | 2.8 | Interquartile range =1.2–5.7 |
| <1 | 77 | 21.6 |
| 1 to <3 | 102 | 28.6 |
| 3 to <5 | 79 | 22.1 |
| 5 to <10 | 60 | 16.8 |
| ≥10 | 39 | 10.9 |
| Living place | ||
| Apartment | 274 | 76.8 |
| House | 60 | 16.8 |
| Single-room occupancy | 3 | 0.8 |
| Institution (nursing or group home) | 20 | 5.6 |
| Home health aide | ||
| Yes | 106 | 29.7 |
| Living with family | ||
| Yes | 205 | 57.4 |
| Living situation affected by Hurricane Sandy | 123 | 34.4 |
| Required evacuation | 46 | 12.9 |
Racial identity, living situations, and evacuation status were self-reported by participants. Home health aide was defined as somebody who helps with living activities other than a family member. Information on comorbidities, dialysis access, body mass index, and length of time on dialysis was obtained from medical records. Median and interquartile range of age and length of time on dialysis and mean±SD of body mass index are also reported.
Ninety-four (26.3%) participants missed dialysis sessions during the storm, with a median of missed dialysis session of two (Q1–Q3=1–3); 65 (69.1%) participants missed one to two sessions, 27 (28.7%) participants missed three to five sessions, and two (2.1%) participants missed more than five sessions. The reasons for missing dialysis were transportation (14; 14.9%), unit closure (38; 40.4%), and both transportation and unit closure (42; 44.7%; multiple answers allowed).
Before the landfall, 221 (61.9%) participants received early dialysis, 57 of which still missed dialysis (Supplemental Figure 1A). Early dialysis did not change the proportion of participants who missed dialysis (P=0.81, Fisher’s exact test) but was associated with a significantly smaller number of missed dialysis sessions compared with no early dialysis (Supplemental Figure 1B).
In total, 236 (66.1%) participants received dialysis in a unit other than their regular unit: 209 (58.5%) at affiliated dialysis unit(s) and 27 (7.6%) at ERs. Of those who received dialysis at other unit(s) or ERs, 68 (28.8%) participants had shorter treatment times than usual, leading to overt symptoms (chest pain, dyspnea, or nausea) in 11 participants.
Disaster Preparedness of Patients on Hemodialysis
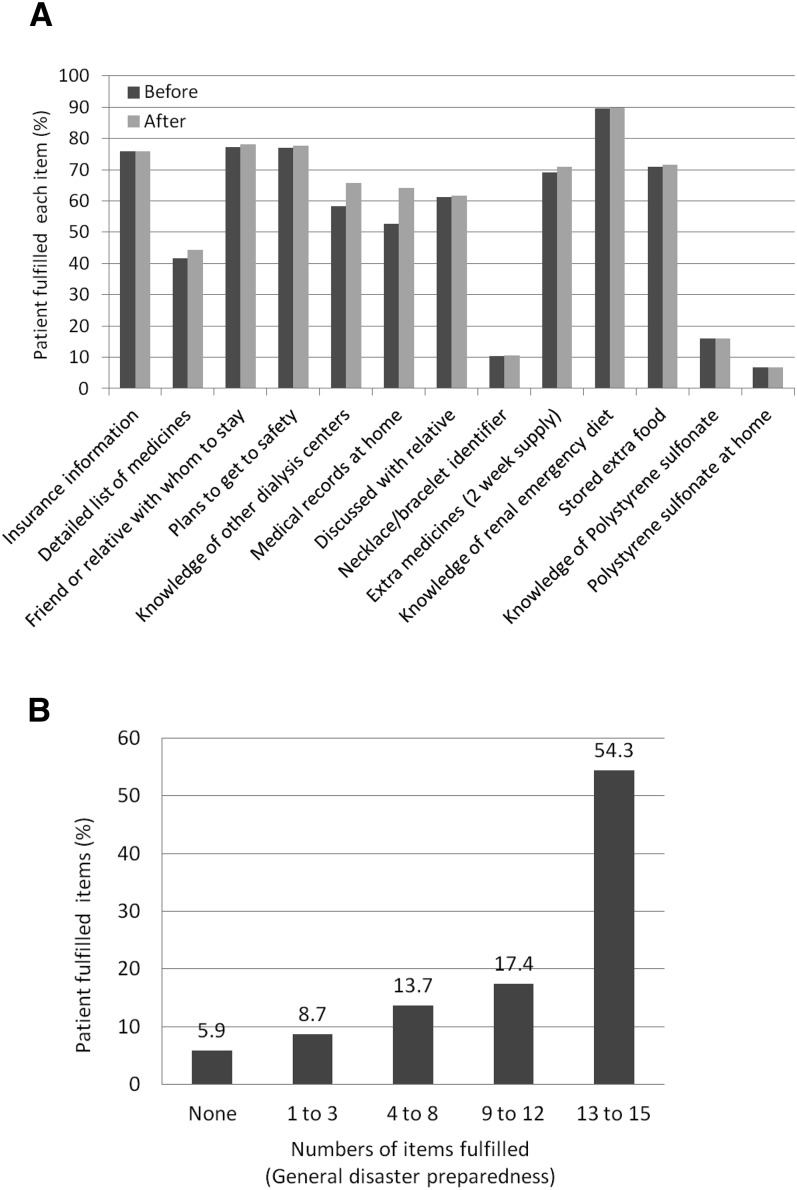
For dialysis-specific disaster preparedness, of 13 essential items from the NKF recommendations (Table 1, dialysis-specific preparedness), participants fulfilled a median of eight recommended items (Q1–Q3=6–9 items); 271 (75.9%) participants had their insurance information, but only 158 (44.3%) participants carried a detailed medication list. The percentages of participants understanding the role of and possessing sodium polystyrene sulfonate at home were very low (16% and 6.7%, respectively) (Figure 2A).
Figure 2.
Natural disaster preparedness. (A) Dialysis-specific disaster preparedness on the basis of the 13-item checklist of the National Kidney Foundation. The dark gray and light gray bars refer to the percentages before and after the storm, respectively. The percentage of those with knowledge of other dialysis centers increased from 58.2% to 65.8%. The percentage of those who had their medical records at home increased from 52.7% to 64.1%. (B) General disaster preparedness on the basis of the 15-item checklist of the Department of Homeland Security; 54.3% of participants fulfilled 13–15 items. In contrast, 5.9% of participants did not have any recommended items prepared.
Sixty-one (17.1%) participants had higher dialysis-specific preparedness when we compared it before and after the storm. Of those, 41 participants retained medical records at home, 27 participants had knowledge of their optional dialysis centers, and nine participants started to carry their detailed medication list with them.
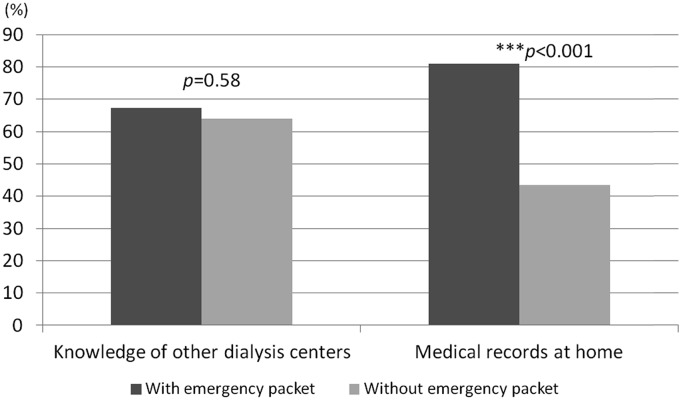
The association of the dialysis emergency packet distribution after the hurricane and the dialysis-specific preparedness at the study period (1–1.5 years after the hurricane) was assessed. The cache of medical records at home was significantly higher for the facilities that distributed the emergency packet to the participants compared with those that did not (P<0.001, Fisher’s exact test), but the number of participants having knowledge of other dialysis centers was not different between these two groups (P=0.58, Fisher’s exact test) (Figure 3, Supplemental Table 1).
Figure 3.
Dialysis emergency packet distribution and disaster preparedness. The percentages of participants who had knowledge of other dialysis centers with or without the dialysis emergency packet (67.3% and 64%, respectively). Similarly, 81.1% and 43.5% of participants had medical records at home with or without intervention, respectively. With the dialysis emergency packet distribution, the cache of medical records at home was significantly higher (P<0.001, Fisher’s exact test).
General Disaster Preparedness
On the basis of the 15-item checklist of the Department of Homeland Security, the participants fulfilled a median of 11 items (Q1–Q3=8–15 items) (Figure 2B).
Characteristics Associated with Missed Dialysis Sessions during Emergency
We performed a multivariate Poisson regression analysis to assess the incidence of missed dialysis as a function of independent measures. The analysis revealed that dialysis-specific preparedness (IRR, 0.91; 95% confidence interval [95% CI], 0.87 to 0.98), nonclassified (i.e., not black, white, or Hispanic) racial ethnicity (IRR, 0.34; 95% CI, 0.20 to 0.57), dialysis treatment in other affiliated unit(s) (IRR, 0.69; 95% CI, 0.51 to 0.94), and older age (IRR, 0.98; 95% CI, 0.97 to 0.99) were associated with a lower incidence of missed dialysis sessions after the storm. However, requirement of evacuation (IRR, 1.6; 95% CI, 1.1 to 2.3) and disturbed living situation (IRR, 2.3; 95% CI, 1.6 to 3.2) were associated with a higher number of missed dialysis sessions after the storm (Table 3). Other candidate covariates described in Materials and Methods were not significantly associated with the number of missed dialysis sessions.
Table 3.
Poisson regression analysis on the number of missed dialysis sessions
| Incidence Rate Ratio | 95% Confidence Interval | P Value | |
|---|---|---|---|
| Dialysis-specific preparedness | 0.91 | 0.87 to 0.98 | 0.001 |
| Racial ethnicity (compared with black) | |||
| White | 0.67 | 0.40 to 1.12 | 0.13 |
| Hispanic/Latino | 0.81 | 0.58 to 1.12 | 0.20 |
| Other | 0.34 | 0.20 to 0.57 | <0.001 |
| Hemodialysis in other units (compared with none received) | |||
| Emergency room | 1.14 | 0.73 to 1.78 | 0.57 |
| Other affiliated units | 0.69 | 0.51 to 0.94 | 0.02 |
| Evacuation | |||
| Yes | 1.57 | 1.08 to 2.29 | 0.02 |
| Living situation affected | |||
| Yes | 2.25 | 1.60 to 3.18 | <0.001 |
| Age | 0.98 | 0.97 to 0.99 | <0.001 |
Multivariate Poisson regression analysis assessing the incidence rate ratio of missed dialysis as a function of independent patient characteristics. For dialysis-specific preparedness and age, incidence rate ratio was calculated as a function of numeric variants. Ethnicity, supplemental hemodialysis facilities, evacuation, and living situations were analyzed as categorical (or binary) data. The control group is shown in parentheses. For example, white is associated with 33% lower incidence rate ratio compared with black.
To further address if non-English speakers or patients with visual impairment had similar outcomes, we performed the chi-squared test for each parameter, because these two parameters were not analyzable as independent variables in the multivariate regression analysis because of strong interaction with other parameters. Non-English speakers were defined as those who do not understand basic English words. Interestingly, non-English speakers missed significantly fewer dialysis sessions (P<0.01), but visual impairment did not affect the outcomes (P=0.61) (Supplemental Table 1).
Discussion
This is the first systematic follow-up survey of the effect of Hurricane Sandy on patients with ESRD with granular individual data, including closure of specific facilities and precise patient demographics.
Our survey showed that 94 (26.3%) participants missed at least one dialysis session after the storm, and 29 (8.1%) participants missed more than three sessions; these findings are less severe than those from Hurricane Katrina, in which these missed dialysis proportions were 44% and 17%, respectively (15). This difference is likely because of the geographic scale of Hurricane Katrina and the higher availability of nearby resources in the aftermath of Hurricane Sandy. In our urban setting, 14.9% of patients missed dialysis because of Pre-center issues/failures, including elevator access and transportation. Most of the dialysis units and patient residences are located above ground level, requiring electricity for water supply and elevators to transport patients and providers. In addition, although early dialysis before the landfall successfully decreased missed dialysis sessions for 61.9% of participants, one quarter of the patients still missed dialysis. Our data have highlighted the need to improve patient, facility, and system-based disaster preparedness.
Our analysis indicated that older age and ethnicity (not black, white, or Hispanic/Latino) were associated with lower numbers of missed dialysis sessions (Table 3), consistent with previous studies performed on nonadherence to dialysis treatment in nondisaster settings (16–18). Self-reported other ethnicity, mainly a Chinese/Asian population, was associated with fewer missed dialysis sessions, whereas non-English–speaking patients (again, mainly Chinese) had a decreased risk of missed dialysis. Although these subgroups were mainly centered at Chinatown Dialysis Center, which did not close after Hurricane Sandy, this illustrates that strong cultural or social supports might have helped coordinate care in an emergency situation.
We observed that participants who were relocated to another affiliated dialysis center for treatment missed 30% fewer dialysis sessions. In practice, the dialysis facilities operated as a local network, highlighting the importance of communication and information sharing among dialysis facilities. In fact, large dialysis providers are mandated to provide a unique medical record number for patients on dialysis, generated by the CMS, to facilitate information sharing. We are aware of the ongoing Medicare Blue Button System (19), which enables health care providers and patients to share vital medical information. However, in a large-scale disaster, which disrupts communication tools among providers, information sharing would be limited, and other retrieval methods will be needed.
We also found that individual dialysis-specific disaster preparedness contributed to fewer missed dialysis sessions, consistent with previous reports (15). Our data indicate that, although a 1-point change in dialysis-specific preparedness was associated with a 9% decrease in missed dialysis sessions, there is still room to improve disaster preparedness: patients filled a median of only eight suggested items (Q1–Q3=6–9 items), comparable with the previous study by Foster et al. (20).
Furthermore, distribution of the dialysis emergency packet was associated with a higher cache of medical records at home, suggesting that distribution of information is a potentially efficient way to improve patient outcomes in a disaster setting. However, this study is a cross-sectional observational study, and additional studies are needed to show if facility to patient information distribution is directly associated with improved outcomes; indeed, patients did not routinely carry this information to ERs or other affiliated units. Intervention to enhance portable personal record carriage is still needed.
Currently, the CMS recommends that dialysis facilities fulfill certain criteria for disaster preparation (21), and the NKF and local ESRD networks have largely adopted these recommendations. The CMS conditions for coverage (22) (ART 494.60 Subpart B, Patient Safety) include standard emergency preparedness, such as exits, floor plans, utilities, water, gas, electricity, and evacuation kits (V408); emergency staff and patient training (V409 and V412); annual review of emergency and disaster plans (V415); and recommendations for contact with the local disaster agency (V416). Dialysis facilities are also required by the CMS to have an agreement with a nearby hospital to provide both emergency care for patients on dialysis and backup dialysis services in the event of an interruption of care at the facility (V770). All of the above are potentially important factors to improve patient outcomes in the setting of natural disasters.
There are limitations to our study. First, this was a retrospective cross-sectional study on the basis of questionnaires, and there is inevitable recall bias. Second, we excluded patients with cognitive impairment, who may need more support and, probably, are more vulnerable to the effects of missed dialysis. Although we did not find a significant effect of family support, it is of great importance to encourage familial and institutional support in an emergency. Third, this study was done in an urban setting in lower Manhattan, and the results in other settings might be different. Fourth, although Hurricane Sandy had substantial effects on patient treatment, the disaster was predictable and different from devastating, catastrophic, and unpredictable disasters, such as earthquakes and tsunamis.
Although patients on dialysis have different abilities to tolerate missed treatments, interrupted access to hemodialysis can be life threatening. We observed a single death and a single severe cardiac dysrhythmia. We support the practice of facilities providing early or prophylactic treatments whenever forewarned of significant disasters. Facilities should regularly review their disaster preparedness and update dialysis emergency packets. To minimize precenter failures that contribute to missed dialysis, we also suggest individualized disaster plans, including transportation and residential building contingencies, particularly for the most vulnerable patients with ESRD.
Disclosures
None.
Supplementary Material
Acknowledgments
We thank all of the care providers, including facility managers, technicians, physicians, nurse practitioners, nurses, social workers, and on-site translators, as well as the patients who participated in the study.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Preparing for Disasters for Patients on Dialysis,” on pages 1316–1317.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.10181014/-/DCSupplemental.
References
- 1.Kopp JB, Ball LK, Cohen A, Kenney RJ, Lempert KD, Miller PE, Muntner P, Qureshi N, Yelton SA: Kidney patient care in disasters: Lessons from the hurricanes and earthquake of 2005. Clin J Am Soc Nephrol 2: 814–824, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Kopp JB, Ball LK, Cohen A, Kenney RJ, Lempert KD, Miller PE, Muntner P, Qureshi N, Yelton SA: Kidney patient care in disasters: Emergency planning for patients and dialysis facilities. Clin J Am Soc Nephrol 2: 825–838, 2007 [DOI] [PubMed] [Google Scholar]
- 3.Bonomini M, Stuard S, Dal Canton A: Dialysis practice and patient outcome in the aftermath of the earthquake at L’Aquila, Italy, April 2009. Nephrol Dial Transplant 26: 2595–2603, 2011 [DOI] [PubMed] [Google Scholar]
- 4.Portilla D, Shaffer RN, Okusa MD, Mehrotra R, Molitoris BA, Bunchman TE, Ibrahim T: Lessons from Haiti on disaster relief. Clin J Am Soc Nephrol 5: 2122–2129, 2010 [DOI] [PubMed] [Google Scholar]
- 5.Johnson DW, Hayes B, Gray NA, Hawley C, Hole J, Mantha M: Renal services disaster planning: Lessons learnt from the 2011 Queensland floods and North Queensland cyclone experiences. Nephrology (Carlton) 18: 41–46, 2013 [DOI] [PubMed] [Google Scholar]
- 6.Kamei D, Kuno T, Sato S, Nitta K, Akiba T: Impact of the Fukushima Daiichi Nuclear Power Plant accident on hemodialysis facilities: An evaluation of radioactive contaminants in water used for hemodialysis. Ther Apher Dial 16: 87–90, 2012 [DOI] [PubMed] [Google Scholar]
- 7.Lempert KD, Kopp JB: Hurricane Sandy as a kidney failure disaster. Am J Kidney Dis 61: 865–868, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jangi S: Facing uncertainty—dispatch from Beth Israel Medical Center, Manhattan. N Engl J Med 367: 2267–2269, 2012 [DOI] [PubMed] [Google Scholar]
- 9.Redlener I, Reilly MJ: Lessons from Sandy—preparing health systems for future disasters. N Engl J Med 367: 2269–2271, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Department of Health and Human Services: Hospital Emergency Preparedness and Response during Superstorm Sandy. Available at: http://oig.hhs.gov/oei/reports/oei-06-13-00260.asp. Accessed September 15, 2014
- 11.Kidney Community Emergency Response: Kidney Community Emergency Response Coaliation (KCER) Hurricane Sandy after Action Report. Available at: http://www.nephrologynews.com/ext/resources/files/Reports/KCER_Hurricane_Sandy_After_Action_Report_12-28-12_508.pdf. Accessed August 20, 2014
- 12.Kelman J, Finne K, Bogdanov A, Worrall C, Margolis G, Rising K, MaCurdy TE, Lurie N: Dialysis care and death following Hurricane Sandy. Am J Kidney Dis 65: 109–115, 2015 [DOI] [PubMed] [Google Scholar]
- 13.National Kidney Foundation: Planning for Emergencies. Available at: http://www.kidney.org/atoz/content/disasterbrochurefacilities. Accessed September 15, 2014
- 14.Federal Emergency Management Agency: Department of Homeland Security: Ready. Prepare. Plan. Stay informed. Available at: http://www.ready.gov/build-a-kit. Accessed August 20, 2014
- 15.Anderson AH, Cohen AJ, Kutner NG, Kopp JB, Kimmel PL, Muntner P: Missed dialysis sessions and hospitalization in hemodialysis patients after Hurricane Katrina. Kidney Int 75: 1202–1208, 2009 [DOI] [PubMed] [Google Scholar]
- 16.Saran R, Bragg-Gresham JL, Rayner HC, Goodkin DA, Keen ML, Van Dijk PC, Kurokawa K, Piera L, Saito A, Fukuhara S, Young EW, Held PJ, Port FK: Nonadherence in hemodialysis: Associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int 64: 254–262, 2003 [DOI] [PubMed] [Google Scholar]
- 17.Patel SS, Peterson RA, Kimmel PL: The impact of social support on end-stage renal disease. Semin Dial 18: 98–102, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Leggat JE, Jr., Orzol SM, Hulbert-Shearon TE, Golper TA, Jones CA, Held PJ, Port FK: Noncompliance in hemodialysis: Predictors and survival analysis. Am J Kidney Dis 32: 139–145, 1998 [DOI] [PubMed] [Google Scholar]
- 19.The Official US Government Site of Medicare: Manage Your Health: Medicare's Blue Button. Available at: http://www.medicare.gov/manage-your-health/blue-button/medicare-blue-button.html. Accessed January 21, 2015
- 20.Foster M, Brice JH, Shofer F, Principe S, Dewalt D, Falk R, Ferris M: Personal disaster preparedness of dialysis patients in North Carolina. Clin J Am Soc Nephrol 6: 2478–2484, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers of Medicare and Medicaid Services: Medicare and Medicaid Programs; Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers. Available at: http://www.cms.gov/Medicare/End-Stage-Renal-Disease/ESRDNetworkOrganizations/downloads/emergencypreparednessforfacilities2.pdf. Accessed August 15, 2014
- 22.Centers of Medicare and Medicaid Services: Medicare and Medicaid Programs; Conditions for Coverage for End-Stage Renal Disease Facilities; Final Rule. Available at: http://www.cms.gov/Regulations-and-Guidance/Legislation/CFCsAndCoPs/Downloads/ESRDfinalrule0415.pdf. Accessed December 26, 2014 [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.