Abstract
The lungs are the most common site of serious infection owing to their large surface area exposed to the external environment and minimum barrier defense. However, this architecture makes the lungs readily available for topical therapy. Therapeutic aerosols include those directed towards improving mucociliary clearance of pathogens, stimulation of innate resistance to microbial infection, cytokine stimulation of immune function and delivery of antibiotics. In our opinion inhaled antimicrobials are underused, especially in patients with difficult-to-treat lung infections. The use of inhaled antimicrobial therapy has become an important part of the treatment of airway infection with Pseudomonas aeruginosa in cystic fibrosis and the prevention of invasive fungal infection in patients undergoing heart and lung transplantation. Cytokine inhaled therapy has also been explored in the treatment of neoplastic and infectious disease. The choice of pulmonary drug delivery systems remains critical as air-jet and ultrasonic nebulizer may deliver sub-optimum drug concentration if not used properly. In future development of this field, we recommend an emphasis on the study of the use of aerosolized hypertonic saline solution to reduce pathogen burden in the airways of subjects infected with microbes of low virulence, stimulation of innate resistance to prevent pneumonia in immunocompromised subjects using cytokines or synthetic pathogen-associated molecular pattern analogues and more opportunities for the use of inhaled antimicrobials. These therapeutics are still in their infancy but show great promise.
Keywords: amikacin, antifungal, antiviral, aspergillosis, cancer, colistin, cytokine, inhaled tobramycin, innate immunity, pneumonia, Pseudomonas, transplantation, vancomycin, ventilator-associated pneumonia, zygomycosis
1. Introduction
Among both healthy and immunosuppressed people, pneumonia remains the leading cause of premature death in the world [1–3]. The susceptibility of the lungs to infection arises from the architectural requirements of gas exchange and frequent inhalation of infectious agents. To support ventilation, humans continuously expose 100 m2 of lung surface area to the external environment. As 5 – 10 L of ambient air are ventilated each minute, particles, droplets and pathogens are also entrained. Further, while even healthy normal volunteers demonstrate nocturnal micro-aspiration of orogastric contents, patients with neurologic, anatomic or iatrogenic impediments to airway protection (e.g., endotracheal or nasogastric tubes) are particularly susceptible to aspiration of infected material into the vast interface of the lower respiratory tract.
Unlike the cutaneous surfaces wrapped in impermeable skin, the stomach with its acidic lumen, or the lower gastrointestinal tract with a thick blanket of adherent mucus, the large environmental interface of the lungs is protected with only a minimal barrier defense. The lung barrier is limited by the demand for unimpeded gaseous diffusion, so this delicate tissue is capillary-thin. Yet, despite this structural vulnerability, the lungs defend themselves successfully against most infectious challenges through a variety of mechanisms [4–9]. Most inhaled or aspirated pathogens fail to reach peripheral airways owing to entrapment in a mobile mucus gel layer lining the proximal conducting airways, followed by expulsion through the mucociliary escalator system [4]. The constitutive presence of antimicrobial peptides and antibodies in the airway lining fluid limits the growth of pathogens that succeed in penetrating to the small airways. Alveolar macrophages ingest organisms that reach the most distal airspaces [6,7]. When baseline defenses are overwhelmed, the lung epithelium responds by increasing its direct antimicrobial capabilities (see Section 3) and signaling the recruitment of leukocytes from the circulation.
While the accessibility and large surface of the lungs contribute to their susceptibility to infection, these features also provide a unique opportunity for topical therapy in the form of respiratory aerosols as follows. First, strategies have recently been developed to increase mucociliary clearance using hypertonic saline aerosols, and these have the potential to reduce pathogen burden within the lungs. Second, recent progress in understanding innate immunity has made it apparent that pathogen resistance of the respiratory epithelium can be markedly stimulated, and implementation of therapies based on this insight has the potential to reduce susceptibility to infection in vulnerable patient populations. Third, redirection of deviated adaptive immunity to augment resistance against specific pathogens by aerosol delivery of cytokines has been validated in small studies in humans. Fourth, antibiotics can be delivered by the respiratory route, maximizing drug concentrations in the area of infection where microbial killing is needed and minimizing systemic drug concentrations that can lead to undesirable side effects. The theoretical basis and practical status of each of these inhalational therapies is reviewed in the following sections.
2. Aerosolized hypertonic saline solution to increase lung mucociliary clearance
The chief impetus to augmentation of mucus clearance from the lungs has been the treatment of cystic fibrosis (CF). Traditionally, postural drainage, percussion and other physical methods have been coupled with cough clearance to mobilize airway mucus and debris. More recently, effective aerosol therapies have been introduced to increase mucociliary clearance. The primary defect in CF is absence of an apical epithelial chloride channel that results in reduced airway surface liquid volume [10,11]. This prevents effective ciliary motion and causes mucus dehydration, which together impair mucociliary clearance and injure the airways. In addition, these changes lead to colonization of the normally sterile airways with bacteria and fungi, causing further inflammation and airway damage. As insight into these underlying mechanisms has grown, therapies have been introduced to increase airway surface liquid volume (Figure 1). These have included nucleotides, amiloride and hypertonic saline solution (HSS), but among these, the strongest evidence supports aerosolized HSS.
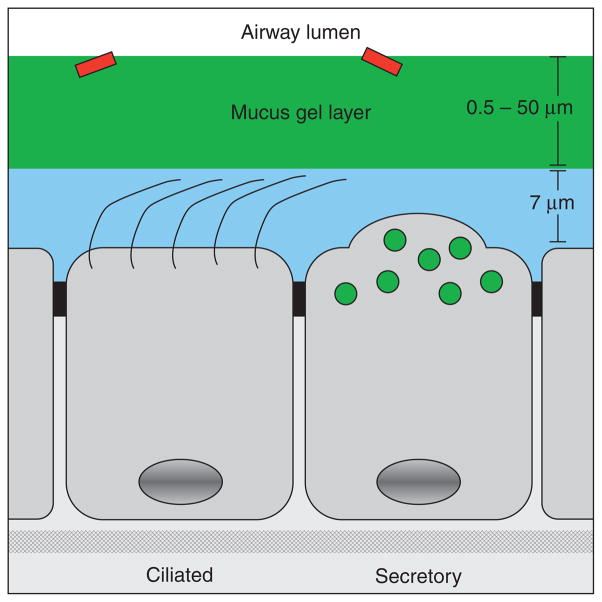
Figure 1. Airway epithelium with overlying surface liquid.
The conducting airways are lined by approximately equal numbers of ciliated and secretory epithelial cells. Secretory cells contain granules that include peptides and mucins (green), although the intracellular mucins may only be detected in small distal airways by sensitive immunohistochemial techniques or during inflammatory metaplasia when their production is increased [15,19]. The airway surface liquid consists of a periciliary layer 7 μm in depth (blue), and an overlying mucus gel layer (green) that varies from < 1 μm in thickness in distal airways to > 50 μm in proximal airways of humans. Cilia beat directionally to propel the mucus gel layer cephalad towards the larynx. The mucin glycoproteins MUC5AC and MUC5B are the principal components of the mucus gel layer, and are exocytically released both from the underlying surface epithelium (shown) and from submucosal glands (not shown). While the mucus gel layer is important in clearance of inhaled pathogens (red), excessive mucin production or airway surface liquid depletion can lead to mucus impaction of the airway lumen, providing a sanctuary for microbial infection.
Early studies in the 1990s indicated that increasing concentrations of aerosolized sodium chloride (saline) solutions result in increasing rates of mucociliary clearance [12–14]. On the basis of these results, HSS aerosols were tested in the short-term treatment of patients with CF and found to improve lung function [12,15]. In 2006, two large studies using 4 ml of 7% saline aerosolized twice daily demonstrated improved lung function and reduced rates of exacerbation [16,17], and this treatment has now become a foundation of the management of CF.
There are several reasons to think that treatment with HSS aerosols would provide benefit to patients besides those with CF. First, the rate of mucociliary clearance is accelerated by increased hydration even in those without airway surface liquid depletion. This has been observed in hyperaldosterone patients who have congenitally decreased sodium absorption and in normal subjects through the use of HSS aerosols [18]. Second, impaction of small airways with lumenal mucus occurs in lung diseases besides CF, such as asthma, chronic obstructive pulmonary disease (COPD) and airway infections with viral, fungal and mycobacterial pathogens [19,20]. Third, airway surface liquid depletion occurs in several disorders of airway inflammation and infection by proteolytic activation of the apical epithelial sodium channel (ENaC) [21]. On the basis of this reasoning, we have begun using aerosolized 7% HSS in subjects with airway mucus impaction and/or persistent airway infection as follows. For virus-induced mucus hypersecretion with cough in patients with asthma, COPD or post-transplantation constrictive bronchiolitis, we use HSS together with the patient’s usual exacerbation treatment regimen, in order to relieve cough and allow delivery of inhaled medications to airways that would otherwise be plugged with mucus. In patients with allergic bronchopulmonary aspergillosis (ABPA), we use HSS together with some combination of inhaled steroids, systemic steroids, a systemic antifungal and systemic anti-IgE therapy. In atypical mycobacterial infection, we use HSS either as monotherapy or together with inhaled and/or oral antibiotics. In patients with an endobronchial stent, we use HSS to prevent accumulation of mucus distal to the stent, which can lead to atelectasis or pneumonia. Occasionally, we have treated patients with HSS who have peripheral lung tree-in-bud radiographic opacities for which we have failed to identify a pathogen. We have anecdotal evidence of symptomatic and radiographic improvements to support all of these uses, but are not aware of data from controlled trials. When several aerosol therapies are used, such as HSS together with inhaled steroids, we administer the HSS first, although there is no objective evidence to support this practice. Studies designed to measure the utility and optimal techniques of aerosolized HSS in diseases other than CF would be valuable.
3. Aerosolized stimulation of lung innate immunity
Though often regarded as passive barriers, the airway and alveolar epithelia supplement baseline lung defenses by undergoing remarkable local structural and functional changes when pathogenic stimuli are encountered. For example, in response to viral, fungal or allergic inflammation, airway epithelial cells rapidly acquire a hypersecretory phenotype by means of a process termed mucous metaplasia [22,23]. The adaptive value of the structural and molecular plasticity of the respiratory epithelium is presumed to be augmented defense against microbial pathogens, and this is supported by the observation of enhanced bacterial clearance following induction of antimicrobial proteins, including defensins, cathelicidins, lysozyme and generators of reactive oxygen species [24–28]. In the presence of pathogens, the airway and alveolar epithelia also elaborate inflammatory cytokines and engage leukocytes in lung protection [29]. Suppression of adaptive immunity and hematopoiesis, as occurs in the setting of hematologic malignancy and/or cytotoxic chemotherapy, do not obviate the lungs’ innate immune response to infection. Rather, profoundly immunosuppressed patients generate remarkable cytokine and chemokine responses to pulmonary infections [30].
In innate immunity, both leukocytes and parenchymal cells identify the presence of pathogens through recognition of pathogen-associated molecular patterns (PAMPs) shared across many pathogen species by germline-encoded pattern recognition receptors (PRRs) [31–35]. Recognition of PAMPs by PRRs activates intracellular signaling cascades, leading to the expression of products involved in microbial defense, inflammation and modulation of adaptive immunity [36]. So far, efforts to induce lung innate immunity have attempted to stimulate PRRs using either natural or synthetic ligands [37]. The most common targets have been Toll-like receptors (TLRs), though NOD-like receptors have been used as vaccine adjuvants for years [37], and other molecules, such as RIG-like receptors and dectin, have been considered potential therapeutic targets [37–42].
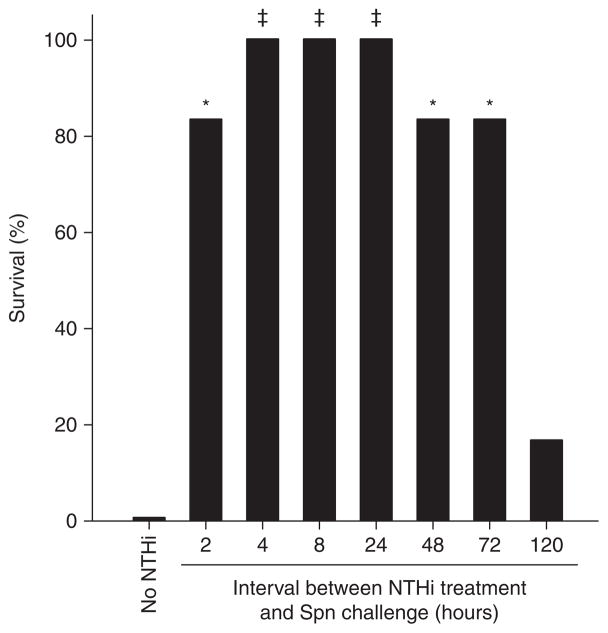
To test whether the functional plasticity of the lungs could be effectively harnessed for protection against pneumonia in vivo, our laboratory strongly stimulated innate immunity before challenge with inhaled respiratory pathogens. To achieve this, mice were exposed to an aerosolized lysate made from non-typeable Haemophilus influenzae, simultaneously stimulating several antimicrobial pathways [42]. A single nebulized treatment resulted in acquisition of high-level resistance to challenge with virulent non-cognate pathogens within 2 h of treatment (Figure 2). We designated this phenomenon stimulated innate resistance (StIR) to reflect several aspects of the protection. It is regarded as ‘stimulated’ insofar as resistance increases greatly following therapeutic application of the lysate. The protection reflects the action of ‘innate’ defenses as demonstrated in several key characteristics: i) protection is achieved in hours, not days to weeks as required for adaptive immunity; ii) protection is achieved in naïve mice following treatment derived from a non-cognate microbe to that used in the challenge; iii) the effect persists despite chemical or genetic depletion of adaptive leukocytes; and iv) protection extends to every microbial pathogen against which it has been tested, indicating a broad, non-selective response. Protection is associated with ‘resistance’ as follows. Faced with a microbial challenge, survival depends on two host strategies: tolerance (the ability to limit the damage caused by the pathogen) and resistance (the ability to limit the pathogen burden) [43,44]. We have found that treatment with the lysate limits the pathogen burden associated with disparate classes of organisms. Consequently, we have identified resistance as the primary means by which the lysate affords protection.
Figure 2. Survival from challenge with Streptococcus pneumoniae (Spn) following treatment with an aerosolized lysate of non-typeable Haemophilus influenze (NTHi).
Mice were pretreated in groups of six with aerosolized NTHi lysate to stimulate innate immunity, then challenged as a single group with a high dose of Spn (6.1 × 1010 CFU/ml). Survival at 7 days is shown as a function of the interval between treatment and challenge (*p = 0.015, ‡p = 0.002, treated versus untreated) [50].
We initially tested the protective benefit of StIR against the most common cause of bacterial pneumonia worldwide, Streptococcus pneumoniae, and found that whereas all untreated mice died following inhalational challenge, all lysate-treated mice survived the challenge. Mechanistic investigations revealed that protection was tightly correlated with the induction of an antimicrobial environment in the lung, demonstrated by rapid reductions in the pathogen burden relative to untreated mice [42]. The protective effect persisted even if the mice were depleted of resident lung leukocytes (alveolar macrophages and mast cells), or depleted of recruited neutrophils. Subsequent studies also indicated that lymphocytes were dispensable in StIR, and in vitro studies revealed that the respiratory epithelium was sufficient to both sense the treatment and effect the antimicrobial response [45].
Stimulated innate resistance extends broadly to other important bacterial respiratory pathogens. Among common causes of nosocomial pneumonia, inhalational treatment with the bacterial lysate protects powerfully against Pseudomonas aeruginosa, Klebsiella pneumoniae and Panton-Valentine leukocidin-producing methicillin-resistant Staphylococcus aureus [45]. The respiratory route is the most likely portal of entry for bioterror agents and the only means by which such pathogens have been successfully delivered in the modern era (i.e., inhalation anthrax) [46–49]. We investigated whether StIR might protect against agents of bioterror, and found that a single aerosolized lysate treatment significantly enhanced mean survival of mice challenged with Bacillus anthracis, Yersinia pestis or Francisella tularensis [45]. For all investigated bacterial pathogens, protection from lethality was associated with significant and immediate reductions in pathogen burden.
Given the breadth of protection against dissimilar bacterial species and the suggestion of even broader antimicrobial activity by analysis of lung gene expression following treatment, protection of mice against a fungal pathogen was also tested. As neither mice nor humans are typically susceptible to Aspergillus pneumonia in the absence of immunocompromise, mice were treated with cyclophosphamide and cortisol before challenge with A. fumigatus. Of the infected mice, > 70% died, unless they received pretreatment with the lysate. Almost all those that did receive the treatment survived (93%). As with the bacterial pathogens, StIR resulted in significant reductions in the intrapulmonary fungal burden [45].
Influenza virus is the leading cause of mortality from lung infection worldwide, and effective pulmonary StIR could provide protection during pandemics. We have found that whereas 100% of control mice died from hemorrhagic pneumonia, > 90% survived following one pretreatment with the bacterial lysate [50]. We also found significant improvement in survival rates if the aerosolized lysate was given 1 day after infection, indicating that innate immune stimulation may be useful in treatment as well as prevention of pneumonia. Furthermore, we found that adding ribavirin to the lysate treatment resulted in synergistic improvements in survival (i.e., better than the additive effects of either treatment alone) when given after the infection [50]. As with all other investigated pathogens, lysate-induced protection against influenza pneumonia was correlated with reductions in lung viral titers.
While treatment with non-typeable Haemophilus influenza (NTHi) lysate results in rapid activation of lung mucosal innate immunity, the protective effect wanes after 4 – 5 days [50,51]. Consequently, repeated treatments would likely be required to prevent pneumonia in patient populations that were at risk beyond this period. We have found repetitive dosing to be both effective and safe in mice. With repetitive lysate treatments, mice have shown persistent resistance to challenges with S. pneumoniae, P. aeruginosa and influenza A [45,50]. Mice exposed weekly for 50 weeks to lysate treatment showed no overt pathology, such as premature death, weight loss or behavioral changes [36]. After 8 weekly exposures, a mononuclear cell infiltration surrounded the airways, although very few alveolar inflammatory cells were observed. After 25 weekly exposures mild airway wall fibrosis was apparent that further progressed after 50 weekly exposures [52]. The prolonged timeline of the airway wall fibrosis and progressive accumulation of lymphocytes suggest the fibrosis occurs owing to an adaptive immune response following chronic exposure to the bacterial lysate, rather than in response to the innate immune stimulation itself. Substitution of macromolecular stimulants of innate immunity with small molecule analogues that do not elicit an adaptive immune response and reduction of the intensity of stimulation may, therefore, avoid this long-term complication. Indeed, the colon of mice is persistently stimulated by the presence of lumenal bacteria, resulting in constitutive activation of StIR that can be revealed as an inducibly reduced capacity for bacterial killing by colonic epithelium after treatment with antibiotics [53], yet the colon does not develop fibrosis.
The data in mice suggest that treatments to induce innate resistance in the lungs should be well tolerated in human patients. We believe the reason that mice can tolerate the highest doses applied (12 times the therapeutic dose) without apparent adverse effects [51] is that the response is contained within the lumen of the lungs. Despite several thousand-fold inductions of inflammatory cytokines in bronchoalveolar lavage fluid over baseline, there is almost no increase in systemic cytokine levels [50]. This is consistent with the recent work of Hoogerwerf and colleagues who induced significant lung inflammatory responses in the airways of human subjects exposed to intrapulmonary application of the TLR ligands lipotechoic acid (TLR2 ligand) and lipopolysaccharide (LPS, TLR4 ligand) yet was not associated with any identifiable clinical signs or symptoms [54].
Our laboratory is not alone in investigating TLR stimulation that may contribute to improved host survival of infections. Several groups have observed the immunomodulatory effects of LPS and have attempted to alter the course of respiratory infections by delivering LPS derivatives [40,41,55] or modifying the LPS structure [39] in pathogens used in experimental pneumonia. All have found some degree of protection through application of a single TLR4 agonist, as have we [51]. Single TLR agonist trials have been successful in human infectious disease, as well. For example, subcutaneous administration of a synthetic TLR9 agonist has induced systemic inflammatory responses and reduced viral loads of hepatitis C [42], and topical imiquimod (TLR7) has shown promise in the treatment of cutaneous leishmaniasis [38]. However, it is likely that synergistic interactions of multiple PRR stimulation will be required to achieve the full efficacy and breadth of activity demonstrated with the bacterial lysate [56–59].
The lysate used to induce StIR has no inherent antibiotic effect [45]. Rather, it induces the host’s native defensive products. The induction of antimicrobial peptide elaboration is consistent both with the time and the breadth of protection and is demonstrated in gene expression microarray [45] and proteomic [51] analyses. In the future, it may be possible to bypass the host-inductive step and directly deliver beneficial antimicrobial peptides or small molecule mimetics [43].
In the near future, stimulating the host’s natural responses to microbial products to prevent and treat pneumonia could provide the basis for development of a novel clinical therapeutic strategy [44,45].
4. Aerosolized delivery of cytokines for targeted immune deviation
IFNα-2a, IFNγ-1b and GM-CSF have been given via the pulmonary route in patients with refractory pulmonary Mycobacterium tuberculosis infection and non-tuberculous mycobacteriosis (NTM) including Mycobacterium avium complex (MAC) lung disease with variable success. These immunologically diverse proteins have also been used for non-infectious pulmonary disorders such as primary lung cancer, metastatic cancer to the lung and alveolar proteinosis, a disease recently associated with antibodies against native GM-CSF [60–62]. A brief description of clinical experience in the use of inhaled cytokine therapy for pulmonary infection follows.
Inhaled IFNα has been tolerated at lower doses (1 – 20 MIU) without systemic adverse events, whereas fever, malaise and headache occurred when doses ranging from 60 to 120 MIU were used and coincided with detectable cytokine in the peripheral circulation [63,64]. Bronchoconstriction poses an impediment in use of this cytokine among patients with chronic bronchitis [65]. Salvage therapy with inhaled IFNα for the treatment of inoperable lung cancer has not been encouraging [66]. Adding IFNα 3 MIU 3 times a week to antituberculous therapy was associated with early resolution of fever and a rapid decline in acid fast bacilli in expectorated sputum compared with antimicrobial therapy alone [67]. Furthermore, in patients with treatment-refractory tuberculosis infection, addition of inhaled IFNα has shown encouraging results although further large randomized studies are needed to validate safety, cost and efficacy [68].
Low dose inhaled IFNγ is well tolerated, including in patients with bronchoreactive conditions such as asthma, and a measurable activation of alveolar macrophage has been demonstrated following exposure to this pleiotropic pro-inflammatory cytokine [69,70]. There is considerable clinical experience using inhaled IFNγ in the treatment of pulmonary mycobacterial infections. In combination with antimicrobial therapy, aerosolized IFNγ therapy has resulted in favorable responses for both drug-susceptible and drug-resistant pulmonary tuberculosis, with eradication of organisms and improvement in radiographic measure of disease [71–73]. This benefit, however, did not occur in patients with severe underlying lung disease who had pulmonary tuberculosis [74]. Similarly, no therapeutic benefit was noted in patients with CF treated with high doses (500 or 1,000 μg) of inhaled IFNγ in reducing risk of infection, yet, patients suffered from serious drug toxicity including dyspnea, hemoptysis and hospitalization [75]. IFNγ has also been explored for prevention of ventilator-associated pneumonia (VAP) in critically ill trauma patients [76]. The number of VAP were reduced although there was no improvement in overall mortality in these trauma patients who received 100 μg of aerosolized recombinant IFNγ 3 times a day [76]. This lack of efficacy may be in part owing to low cytokine delivery via standard nebulizer apparatus [77]. Aerosolized recombinant GM-CSF is well tolerated, with doses of 250 μg aerosolized twice daily associated with no serious adverse events, in preliminary trials among patients with pulmonary metastases [78]. Use of aerosolized GM-CSF for the treatment of infections in humans has not been reported. However, animal experiments support pulmonary absorption of aerosolized or intratracheally injected GM-CSF and aerosolized GM-CSF has been effective in eradiation of murine invasive pulmonary aspergillosis in an immunocompromised model [79,80].
Other cytokines used via the aerosolized route include IFNβ in the treatment of lung cancer, IL-2 in renal cell carcinoma and other metastatic cancer to lung, soluble IL-4 receptor for patients with asthma and erythropoietin for treatment of anemia. None of these have been used for the treatment of lung infection.
5. Aerosolized delivery of synthetic antibiotics
In the first subsection we will discuss the use of aminoglycosides in the treatment and prevention of serious lung infection among high-risk patients, followed by a brief introduction to the limited clinical experience with other antimicrobial drugs that have been used for salvage therapy of difficult-to-treat pneumonia. Given that extensive reviews have been performed on inhaled pentamidine in HIV-associated Pneumocystis jiroveci infection, this topic will not be covered herein.
5.1 Aminoglycoside aerosolized therapy
In theory, aminoglycosides have several characteristics that would seem to favor inhalation administration. First, aminoglycosides have concentration dependent killing effects meaning that the high levels achievable in the respiratory tract with inhaled formulations may lead to increased clinical efficacy. Moreover, aminoglycosides have significant dose-limiting toxicity in humans such that the doses that can be given by systemic administration lead to relatively low levels in the pulmonary parenchyma. Finally, because aminoglycosides have been used relatively sparingly over the past few decades, many multidrug resistant organisms that cause nosocomial respiratory infection remain susceptible to at least one, if not many, commonly used aminoglycosides. Indeed, of all classes of antibiotics, data concerning antimicrobial delivery by the inhalation route are most extensive for the aminoglycosides. In this section, we will review pharmacokinetic, clinical and safety information concerning inhalation therapy with aminoglycosides.
The development of broad-spectrum aminoglycosides, such as gentamicin, in the late 1960s and early 1970s held great promise for the treatment of previously recalcitrant respiratory infections owing to antimicrobial resistant Gram-negative rods such as P. aeuroginosa [81]. Investigators soon reported, however, that systemically administered gentamicin often failed to treat pulmonary infections owing to P. aeuroginosa and other Gram-negative rods despite in vitro susceptibility [82]. Low gentamicin levels in respiratory secretions led investigators to postulate that erratic penetration of aminoglycosides into the site of infection might account for therapeutic failures and to suggest that administering gentamicin directly into the lungs might improve the clinical response [83,84]. Preliminary investigations in the 1970s showed that sputum concentrations of gentamicin were often an order of magnitude higher following endotracheal administration compared with systemic treatment [83,85].
Data accumulated in the ensuing 30 years has validated the supposition of these early reports that aminoglycoside penetration into the pulmonary parenchyma is suboptimal following systemic administration [86–93]. The pharmacokinetics of aminoglycoside drug delivery have particular import inasmuch as these agents have concentration-dependent killing effects, meaning that higher drug levels are associated with increased antimicrobial effects [94]. For example, the optimal clinical response to aminoglycoside therapy occurs when the maximum drug concentration (Cmax) to minimum inhibitory concentration (MIC) is > 8:1 [95–98]. Aminoglycoside therapy for pneumonia is usually considered for relatively resistant non-fermentative Gram-negative rods, such as P. aeruginosa, Acinetobacter baumanii and Stenotrophomonas maltophila [99]. Although highly variable depending on the patient population and aminoglycoside being considered, even for susceptible organism, MICs for these organisms are generally in the 1 – 8 μg/mL range [100]. Thus, to maximize the opportunity of clinical response, lung aminoglycoside concentrations of ≥ 10 – 40 μg/mL are needed. Importantly, none of the currently available aminoglycosides have been shown to achieve these kinds of levels when administered systemically even in the setting of an inflammatory process that would be expected to increase entry into the lungs from the circulation [85,86,91,92,101].
In contrast to the difficulties of achieving satisfactory pulmonary levels with systemic aminoglycoside administration, topical aminoglycoside delivery results in concentrations likely to be effective even against relatively resistant organisms [85,86,93,102–104]. Measurements of aminoglycoside levels in the lungs following topical administration are highly dependent on the mechanism used to deliver the drug, the dose and the site sampled. Despite these variabilities, however, investigators have consistently demonstrated aminoglycoside levels > 200 μg/mL in respiratory samples following topical administration [85–87,89,101–107]. The data regarding aminoglycoside concentrations are similar in animal and human studies, in sick and healthy patients and when invasive and non-invasive testing methods are used [85–87,89,101–107]. Therefore, the pharmacokinetic data strongly suggest that topical administration of aminoglycosides is more likely to result in effective drug levels compared with systemic delivery.
5.2 Clinical studies of inhaled aminoglycosides: cystic fibrosis
The control of bronchopulmonary infection has markedly increased the quality of life and life-expectancy of CF patients [108]. The unique endobronchial environment of patients with CF means that the lungs of such patients become colonized with organisms such as S. aureus and H. influenza shortly after birth. However, over time P. aeuroginosa generally becomes the predominant pulmonary pathogen in CF patients, colonizing > 80% of persons by 18 years of age [109]. Host–pathogen interaction between CF patients and P. aeuroginosa is relatively unique in terms of bacterial processes in that once established, endobronchial P. aeuroginosa infection is rarely completely eradicated [110]. Much of the therapeutic advances made over the past decades in the treatment of CF patients have come through decreasing the burden of P. aeuroginosa in the lungs of CF patients, which subsequently ameliorates the inflammatory response responsible for progressive bronchiectasis.
Whereas intravenous antibiotics have long been the gold standard for treating P. aeuroginosa infection in patients with CF, over the past 20 years, a series of increasingly rigorous clinical studies has clearly established a role for inhaled aminoglycosides in suppression of P. aeuroginosa infection in CF patients. Initially, gentamicin was used but investigators shifted towards tobramycin in light of its increased anti-Pseudomonas activity [111–113]. For convenience, early studies nebulized vials of aminoglycosides originally intended for intravenous formulation, which potentially could cause lung irritation owing to the presence of preservatives and antioxidants. An important advance occurred when Smith et al. developed a preservative-free tobramycin preparation for nebulization that at 600 mg delivered a much higher dose than the typical 80 mg intravenous vial [114]. It was the 600-mg dose of tobramycin that was used in a critical 71 person cross-over design study in which patients received t.i.d. dosing. After 1 month of nebulized tobramycin, key pulmonary function parameters and P. aeuroginosa sputum density were significantly improved in the treatment group [107]. The effective, but cumbersome, nature of the treatment led to the development of the next generation of nebulized tobramycin that was subsequently used in the largest randomized, placebo-controlled trial of nebulized aminoglycosides. A total of 520 patients with CF who were colonized with P. aeuroginosa were randomized to nebulized tobramycin 300 mg b.i.d. or placebo administered in 4-week on-off blocks over 24 weeks [115]. Patients receiving active treatment showed improvement in pulmonary function tests, less need for hospitalization and significantly decreased density of P. aeuroginosa in sputum. Importantly, the positive effects of inhaled tobramycin continued for 2 years after treatment initiation [116]. The results of this study led to the US FDA approval of tobramycin solution for inhalation (TSI) (TOBI™, Novartis Corp., East Hanover, NJ), which so far is the only approved antibiotic preparation for airway inhalation in the US.
The effectiveness of TOBI in chronic suppression of P. aeuroginosa in CF patients has led to studies of inhaled aminoglycosides in acute CF exacerbations, but the results have not been nearly as dramatic. Several trials have shown that the addition of inhaled aminoglycosides, such as tobramycin or amikacin, to systemic antipseudomonal therapy increases the proportion of patients that clear P. aeuroginosa from their sputum but does not improve clinical outcomes such as pulmonary function tests [117,118]. A recently completed 17-center international study found no statistical difference in clinical outcomes when inhaled tobramycin was added to systemically administered ciprofloxacin in P. aeuroginosa infected CF patients with an acute exacerbation [119]. Patients receiving inhaled tobramycin had lower P. aeuroginosa sputum density but an increased rate of wheezing with the inhalation therapy that may have offset benefit derived from an augmented antimicrobial effect. Thus, at the present time, inhalation therapy is not considered part of the standard of care for CF patients with acute exacerbations.
5.3 Treatment of non-cystic fibrosis bronchiectasis patients with inhaled aminoglycosides
Although CF is the predominant cause of bronchiectasis in developed countries, there are several other medical conditions that can result in bronchiectasis [120]. The encouraging results of treating CF-related bronchiectasis has increased the long-standing interest in treating patients with non-CF-related bronchiectasis with inhaled aminoglycosides [121]. Unfortunately, similar to the situation in acute exacerbations in CF, the data accumulated so far regarding the effectiveness of inhaled aminoglycosides for non-CF-related bronchiectasis is not as strong as that for maintenance therapy in CF. So far, four published clinical studies have examined the use of inhaled aminoglycosides in non-CF patients with bronchiectasis and chronic P. aeuroginosa infection, all of which used inhaled tobramycin at 300 mg b.i.d. dosing [119,122–124]. Similar to the pivotal CF studies, these trials have consistently found that inhaled tobramycin significantly decreases the respiratory burden of P. aeuroginosa. However, unlike the situation in CF-related bronchiectasis, the decrease in P. aeuroginosa levels in non-CF-related bronchiectasis patients has not led to consistent improvements in objective clinical measures such as pulmonary function tests. One study did find improvement in ‘general health’ among tobramycin-treated patients [123]. The finding that tobramycin-treated patients developed more bronchospasm compared to placebo-treated patients has significantly limited the adoption of aerosolized antibiotics in non-CF bronchiectasis [121]. Thus widespread use of inhaled aminoglycosides in non-CF bronchiectasis patients awaits the development of a formulation that causes less airway irritation while maintaining antipseudomonal efficacy.
5.4 Prevention and treatment of ventilator-associated pneumonia with inhaled aminoglycosides
Although vital for management of critically ill patients, mechanical ventilation is often complicated by the development of respiratory infections that cause substantial morbidity and mortality [125]. Given the ease of access afforded by endotracheal intubation, there is a long history of instilling antimicrobials directly into the respiratory tract to treat and prevent ventilator associated respiratory infections [83]. The most systematically researched area in this regard has been the use of topical antibiotics to prevent ventilator associated pneumonia (VAP) [126]. Although the largest trials have been done with non-aminoglycoside antibiotics, both tobramycin and gentamicin have shown some efficacy in preventing VAP [127,128]. A recent meta-analysis found that topical antimicrobial administration significantly decreases VAP rates in mechanically ventilated patients [126]. These data are in conflict with the recommendation of The Centers for Disease Control and Prevention against using nebulized antibiotics to prevent VAP because of concern for development of antimicrobial resistance and administration side effects [129].
Compared to VAP prevention, there is less systemic data regarding the use of inhaled aminoglycosides for VAP therapy [130]. However, given the rising rates of VAP owing to multidrug or even pan-resistant Gram-negative pathogens, the use of inhaled aminoglycosides or other antimicrobials may become increasingly common in an effort to increase local drug concentrations to overcome relatively resistant pathogens. Of note, a recent retrospective study in cancer patients with Gram-negative rod VAP found that those patients who received inhaled aminoglycosides, mainly tobramycin or inhaled colistin, had significantly better clinical outcomes compared to patients receiving systemic aminoglycoside or colistin therapy [131]. Finally, Palmer et al. recently reported the results of a trial in which patients with ventilator-associated tracheobronchitis (VAT) were randomized to inhaled antimicrobials, tobramycin and/or vancomcyin, or placebo [132]. Patients receiving inhaled antimicrobials had marked improvement in objective respiratory scores and were significantly less likely to progress to VAP compared to patients receiving placebo. Taken together, the combination of increasing drug resistance and accumulating data regarding the efficacy of inhalation therapy indicates that topical aminoglycoside therapy may have a multifaceted role in the prevention and treatment of respiratory infection in mechanically ventilated patients although multicenter, prospective studies are needed.
5.5 Safety of inhaled aminoglycosides
Two chief concerns regarding topical aminoglycoside therapy are the development of drug resistance and side effects of the medication or medication delivery system. Given that topical administration results in a gradient of antimicrobial drug concentration from the central to the peripheral airways, there is substantial concern for the induction of antimicrobial resistance [121]. Moreover, topical therapy is often given for prolonged periods of time, even years, thereby maximizing the opportunity for drug resistance. Whereas case reports and case series have confirmed that resistant organisms can emerge during therapy, careful examination during randomized clinical trials have not found that the emergence of drug-resistant organisms in treated patients is a particularly significant issue [100,110,126]. In light of the extremely high levels of aminoglycosides achievable with nebulized therapy, some countries have suggested developing inhalation specific MIC breakpoints under which very few organisms would actually be aminoglycoside resistant [133]. Whether environmental contamination of nosocomial nebulized therapy would lead to increased aminoglycoside resistance in health-care settings remains a theoretical but unproven concern. The elicitation of bronchospasm by topical therapy is another main safety issue especially when nebulized antibiotics are being used for symptomatic relief such as in bronchiectasis [121]. Although usually readily responsive to bronchodilators, airway irritation by nebulized aminoglycosides is limiting to numerous patients and continuing research to develop better tolerated therapies is critical to more widespread use.
5.6 Other aerosolized antibacterial therapies
Clinical experience with aerosolization of antibacterial agents other than aminoglycosides is limited but growing. The marked increase in multidrug-resistant Gram-negative pathogens has led to increased use of polymyxins, antimicrobials that were developed in the 1950s but whose use rapidly decreased in the 1970s and 1980s owing to concerns over nephrotoxicity [134]. Use of colistin (polymyxin E) has markedly increased recently as strains of P. aeruginosa and A. bauamnnii that are resistant to all other classes of commercially available anitmicrobials have remained susceptible to colistin [134]. Similar to the aminoglycosides, inhalation is a potentially attractive route of colistin administration given the toxicities observed with systemic administration. Retrospective and non-randomized studies have shown encouraging results with inhaled colistin although the studies are confounded by patient heterogeneity and administration of additional antimicrobials in conjunction with inhaled colistin [130,131,134–138]. So far, minimal toxicity has been reported with inhaled colistin although systematic data are lacking. Inhaled aztreonam appears to be a safe and effective alternative to inhaled tobramycin in cystic fibrosis [139]. Finally, a recent study has shown that inhaled vancomycin was effective in preventing ventilator-associated tracheobronchitis from progressing to ventilator-associated pneumonia [132]. The relentless increase in drug resistance among respiratory pathogens gives added urgency to continuing studies designed to better define the role of inhaled antimicrobials in pulmonary infections.
5.7 Antifungal aerosolized therapy
Despite recent advances in antifungal drug therapy, invasive fungal infections (IFIs) remain a serious threat for immunosuppressed cancer patients and recipients of organ or hematopoietic transplantation [140,141]. Response to systemic immune enhancement cytokine therapy such as recombinant GM-CSF, IFNγ and donor granulocyte transfusions is fraught with a lack of cost and utility validation studies and compounded by uncertain clinical efficacy data [142]. Invasive aspergillosis is a life-threatening infection often seen during the first 3 years after heart–lung transplantation [143], whereas in recipients of allogeneic stem cell transplantation, this infection occurs during the pre-engraftment neutropenic period, during acute graft-versus-host disease (GVHD) and during a late risk period that includes treatment of chronic GVHD [144]. In patients with cancer, those with acute myelogenous leukemia are especially susceptible to IFIs, and the risk period may be prolonged in patients with refractory or relapsed cancer [145]. Inhaled amphotericin B has been explored for prevention of IFI in susceptible patients during high-risk periods and for salvage therapy in patients with difficult-to-treat invasive pulmonary fungal disease.
In lung transplant recipients, Aspergillus species infections leads to colonization that often precedes invasive disease manifested as tracheobronchitis or anastomotic infections, and/or invasive pulmonary disease; fungal dissemination in these non-neutropenic patients without cancer is uncommon. Most of these fungal infections occur in non-neutropenic solid-organ transplant recipients during the period of early graft rejection and rejection immunosuppressive therapy [143]. It is interesting to note that Aspergillus species colonization 3 months after transplantation is more common in patients with human leukocyte antigen (HLA) A1; however, in these patients who are prone to late fungal colonization the risk of invasive fungal disease was not substantially increased [143]. In contrast, several fungal infections have recently been reported in heart transplant recipients with refractory rejection treated with sirolimus in conjunction with tacrolimus and patients with cardiac allograft vasculopathy [146].
Inhaled amphotericin B was the first drug used for the treatment of systemic mycosis, and earlier animal experiments using aerosolized amphotericin B showed favorable efficacy in the treatment of pulmonary aspergillosis [147]. The lipid preparations of amphotericin B, such as amphotericin B lipid complex (ABLC), have also been effectively delivered through the aerosolized route. Pre-infection ABLC treatment with 0.4 – 1.6 mg/kg given 2 days before infection provided a 63 – 100% survival benefit in animal experiments [148]. The peak concentration of amphotericin B in bronchioalveolar lavage after a single dose occurs 30 min after inhalation, and it is slowly cleared from the lungs over the next 24 h [149].
The drug delivery apparatus remains critical in predicting the concentration of drug being aerosolized. In clinical distribution kinetics studies, 10% of the inhaled ABLC was deposited in the lungs when given via specialized delivery systems such as an AeroEclipse Nebulizer driven by 7 – 8 L/min compressed air, and this lung deposition was twofold higher compared to levels achieved using standard aerosol delivery systems for bronchodilator therapy [150]. Formulation is also important, with a sixfold higher drug concentration with aerosolized ABLC compared with amphotericin B deoxycholate in animal experiments [148]. Furthermore, inhaled ABLC was well tolerated in a study of lung transplant recipients, whereas conventional amophotericin B deoxycholate resulted in a twofold higher rate of treatment-related adverse events [151].
A significant reduction in cases of invasive pulmonary aspergillosis was reported in patients given inhaled amphotericin B during and after surgery for heart and heart–lung transplantation [152]. Similarly, a lipid-based preparation of amphotericin B (ABLC) has also been successfully used in prevention of Aspergillus tracheobronchitis, anastomotic and invasive lung disease in heart and lung transplant recipients [143,153].
The paucity of clinical data for aerosolized amphotericin B treatment in patients with established fungal lung infection makes it difficult to recommend this intervention even in refractory cases. The two examples of such cases are as follows: a non-immunosuppressed patient with post-viral Aspergillus tracheobronchitis that failed to respond to prolonged liposomal amphotericin B therapy had a favorable response to extended treatment with inhaled amphotericin B deoxycholate plus GM-CSF and IFNγ immune enhancement [154]. Second, a severely immunosuppressed patient with Rhizomucor lung infection that evolved to include Pseudalescheria boydii had a complete resolution of infection with inhaled ABLC, which was continued for 5 months and on long-term follow up no infection recurrence was observed [155]. These cases underline the potential role inhaled amphotericin B may play in the treatment of established disease; however, no recommendations can be made with the current clinical information.
5.8 Antiviral aerosolized therapy
Respiratory tract viral infections are generally mild and often respond to supportive care. In immunosuppressed patients with cancer or transplantation, however, these infections can be associated with devastating complications that require early diagnosis and prompt therapy [137]. Paramyxoviruses such as respiratory syncytial virus (RSV) and parainfluenza virus (PIV), influenzavirus A and B, adenovirus and the recently recognized human metapneumovirus (hMPV) are of concern. Ribavirin, a purine nucleoside analogue, has been used for the treatment of chronic hepatitis C virus infection by oral administration, and for hemorrhagic fever and disseminated hMPV by intravenous administration. Aerosolized ribavirin was approved by the FDA for the treatment of RSV infections in hospitalized children. The conventional continuous treatment of 60 mg of ribavirin/ml for 18 h is effective with or without intravenous immunoglobulin; however, patients feel severely isolated, which may interfere with patient care [138]. Intermittent aerosolized ribavirin 20 mg/ml for 2 h 3 times daily has also been effective in adult cancer and stem cell transplant patients with RSV infection [140]. In immunosuppressed children with RSV infection, intermittent high doses (60 mg) of ribavirin/ml for 2 h given 3 times daily were well tolerated, associated with clinical response comparable to standard continuous therapy and associated with significantly less environmental contamination and exposure to health-care workers, and with greater accessibility to patients [141,142].
Parainfluenzavirus is associated with potentially serious complications in heart–lung transplant recipients, with possible roles in acute allograft rejection and post-viral bronchiolitis obliterans [143]. Inhaled ribavirin in this population has been associated with clinical improvement, albeit clinical experience is limited [144]. In hematopoietic stem cell transplant recipients, parainfluenzavirus infection is serious in the presence of other copathogens and in patients with respiratory failure, and treatment with aerosolized ribavirin has not been associated with decreased duration of viral shedding or pneumonia-associated mortality [145].
Influenza A virus is a major cause of morbidity and mortality, and infections are often severe in patients with defective adaptive T-cell response. Drug resistance to neuraminidase inhibitors poses a serious treatment challenge in the setting of poor response to conventional vaccines in the high-risk cancer and transplant population [146]. Aerosolized ribavirin 60 mg/ml for three daily dose of 15 min duration was effective against influenza A and B infections of mice [147]. Recently, megadose ribavirin (100mg/ml) was shown to be effective in mice infected with lethal influenza A H3N2 virus. This mega-dose therapy for only 4 days resulted in > 90% survival when given within 24 – 48 h after infection [148]. Further clinical studies are needed to evaluate appropriate dose and efficacy of ribavirin for the treatment of drug-resistant or drug-refractory virulent influenzavirus infection.
Human metapneumovirus has emerged as a common respiratory tract viral pathogen associated with subclinical or mild disease. Occasionally, in patients with T-cell immune defects hMPV has been show to cause disseminated fatal disease [149]. In patients with stem cell or solid-organ transplantation these infection, even with limited pulmonary disease, are life threatening and increase risk for post-viral invasive fungal pneumonia [150]. Intravenous ribavirin is considered the best available treatment for these serious disseminated or pulmonary hMPV infections, reflecting anti-viral effect of the drug and possible drug-mediated immunomodulatory properties that may further enhance viral clearance, and aid in resolution of infection, especially in an immunocompromised host [151].
In patients intolerant to intravenous ribavirin owing to hemolytic anemia and other serious complications, aerosolized treatment for pulmonary hMPV disease has been used with some success [152]. Similarly, in the treatment of pneumotropic human adenovirus, aerosolized ribavirin is preferred to intravenous owing to the high drug concentration achieved in the alveoli, compared with intravenous ribavirin therapy that may not lead to cytotoxic concentrations in lung tissue [153]. However, this may not be the only determinant in clinical efficacy of ribavirin therapy as drug-induced enhancement of the Th1 helper T-cell activity needs to be further evaluated in clinical trials [151].
6. Nebulizer systems
A critical consideration for all inhaled therapeutics is the characteristics of the delivery system. For all of the therapies discussed herein, liquid aerosols were used, most commonly generated by air-jet nebulizers, though additional technologies are being increasingly used [156]. The air-jet and ultrasonic nebulizers generate aerosol under high pressure and vibration of piezo-electric crystal, respectively. These commonly used delivery systems yield adequate pulmonary deposition of antimicrobial drugs in ambulatory patients, whereas drug delivery is lower in critically ill patients receiving assisted ventilation [157,158]. The new aerosol electric generators use a vibrating mesh or plate with multiple apertures that increase pulmonary drug deposition by 2 – 3 times and significantly higher drug output compared with air-jet nebulizers. These should be considered for aerosol drug delivery in mechanically ventilated patients with pneumonia [159].
Similarly, cytokine inhalation therapy seems attractive for various difficult-to-treat mycobacterial infections involving the lung, albeit delivery of these agents to the site of infection poses a daunting task. In standard nebulizer systems such as Respirgard or Misty-neb, only 5 – 7% of the total administered dose reaches the lung tissue [74,160]. This difficulty can be mitigated by using highly efficient air-jet or ultrasonic nebulizers, or specialized delivery systems using the new generation of electric aerosol generators to achieve therapeutic concentrations of immune modulatory cytokines to the site of pulmonary infection. The reader is referred to recent review articles for further information [161].
7. Summary
The lungs are the most common site of serious infection owing to their large surface area exposed to the external environment and minimum barrier defense. However, this architecture makes the lungs readily available for topical therapy. Therapeutic aerosols include those directed towards improving mucociliary clearance pf pathogens, stimulation of innate resistance to microbial infection, cytokine stimulation of immune function and delivery of antibiotics. These therapeutics are still in their infancy, but show great promise.
8. Expert opinion.
In our opinion inhaled antimicrobials are underused, especially in patients with difficult-to-treat lung infections of low acuity.
The use of inhaled antimicrobial therapy has become an important part of the treatment of airway infection with P. aeruginosa in cystic fibrosis and the prevention of invasive fungal infection in patients undergoing heart and lung transplantation.
In future development of this field, we recommend an emphasis on the study of the use of aerosolized hypertonic saline solution to reduce pathogen-induced disorders in the airways of subjects infected with microbes of low virulence, stimulation of innate resistance to prevent pneumonia in immunocompromised subjects using cytokines or synthetic PAMP analogues and more opportunities for the use of inhaled antimicrobials.
Footnotes
Declaration of interest
This research was supported in part by Cancer Center Support Grant CA16672 from the National Institutes of Health.
Bibliography
- 1.The World Health Report 2004 – Changing History. Geneva: World Health Organization; 2004. [Google Scholar]
- 2.File TM. Community-acquired pneumonia. Lancet. 2003;362(9400):1991–2001. doi: 10.1016/S0140-6736(03)15021-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joos L, Tamm M. Breakdown of pulmonary host defense in the immunocompromised host: cancer chemotherapy. Proc Am Thorac Soc. 2005;2(5):445–8. doi: 10.1513/pats.200508-097JS. [DOI] [PubMed] [Google Scholar]
- 4.Knowles MR, Boucher RC. Mucus clearance as a primary innate defense mechanism for mammalian airways. J Clin Invest. 2002;109(5):571–7. doi: 10.1172/JCI15217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin TR, Frevert CW. Innate immunity in the lungs. Proc Am Thorac Soc. 2005;2(5):403–11. doi: 10.1513/pats.200508-090JS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rogan MP, Geraghty P, Greene CM, et al. Antimicrobial proteins and polypeptides in pulmonary innate defence. Respir Res. 2006;7:29. doi: 10.1186/1465-9921-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Travis SM, Singh PK, Welsh MJ. Antimicrobial peptides and proteins in the innate defense of the airway surface. Curr Opin Immunol. 2001;13(1):89–95. doi: 10.1016/s0952-7915(00)00187-4. [DOI] [PubMed] [Google Scholar]
- 8.Flanders SACH, Saint S. Nosocomial pneumonia: state of the science. Am J Infect Control. 2006;(34):84–93. doi: 10.1016/j.ajic.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Knowles MR, Boucher RC. Mucus clearance as a primary innate defense mechanism for mammalian airways. J Clin Invest. 2002;109(5):571–7. doi: 10.1172/JCI15217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ratjen F. Restoring airway surface liquid in cystic fibrosis. N Engl J Med. 2006;354(3):291–3. doi: 10.1056/NEJMe058293. [DOI] [PubMed] [Google Scholar]
- 11.Tarran R, Donaldson S, Boucher RC. Rationale for hypertonic saline therapy for cystic fibrosis lung disease. Semin Respir Crit Care Med. 2007;28(3):295–302. doi: 10.1055/s-2007-981650. [DOI] [PubMed] [Google Scholar]
- 12.Eng PA, Morton J, Douglass JA, et al. Short-term efficacy of ultrasonically nebulized hypertonic saline in cystic fibrosis. Pediatr Pulmonol. 1996;21(2):77–83. doi: 10.1002/(SICI)1099-0496(199602)21:2<77::AID-PPUL3>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 13.Robinson M, Regnis JA, Bailey DL, et al. Effect of hypertonic saline, amiloride, and cough on mucociliary clearance in patients with cystic fibrosis. Am J Respir Crit Care Med. 1996;153(5):1503–9. doi: 10.1164/ajrccm.153.5.8630593. [DOI] [PubMed] [Google Scholar]
- 14.Sood N, Bennett WD, Zeman K, et al. Increasing concentration of inhaled saline with or without amiloride: effect on mucociliary clearance in normal subjects. Am J Respir Crit Care Med. 2003;167(2):158–63. doi: 10.1164/rccm.200204-293OC. [DOI] [PubMed] [Google Scholar]
- 15.Wark PA, McDonald V. Nebulised hypertonic saline for cystic fibrosis. Cochrane Database Syst Rev. 2003;(1):CD001506. doi: 10.1002/14651858.CD001506. [DOI] [PubMed] [Google Scholar]
- 16.Donaldson SH, Bennett WD, Zeman KL, et al. Mucus clearance and lung function in cystic fibrosis with hypertonic saline. N Engl J Med. 2006;354(3):241–50. doi: 10.1056/NEJMoa043891. [DOI] [PubMed] [Google Scholar]
- 17.Elkins MR, Robinson M, Rose BR, et al. A controlled trial of long-term inhaled hypertonic saline in patients with cystic fibrosis. N Engl J Med. 2006;354(3):229–40. doi: 10.1056/NEJMoa043900. [DOI] [PubMed] [Google Scholar]
- 18.Kerem E, Bistritzer T, Hanukoglu A, et al. Pulmonary epithelial sodium-channel dysfunction and excess airway liquid in pseudohypoaldosteronism. N Engl J Med. 1999;341(3):156–62. doi: 10.1056/NEJM199907153410304. [DOI] [PubMed] [Google Scholar]
- 19.Williams OW, Sharafkhaneh A, Kim V, et al. Airway mucus: from production to secretion. Am J Respir Cell Mol Biol. 2006;34(5):527–36. doi: 10.1165/rcmb.2005-0436SF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Evans CM, Kim K, Tuvim MJ, et al. Mucus hypersecretion in asthma: causes and effects. Curr Opin Pulm Med. 2009;15(1):4–11. doi: 10.1097/MCP.0b013e32831da8d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boucher RC. Airway surface dehydration in cystic fibrosis: pathogenesis and therapy. Annu Rev Med. 2007;58:157–70. doi: 10.1146/annurev.med.58.071905.105316. [DOI] [PubMed] [Google Scholar]
- 22.Evans CM, Williams OW, Tuvim MJ, et al. Mucin is produced by clara cells in the proximal airways of antigen-challenged mice. Am J Respir Cell Mol Biol. 2004;31(4):382–94. doi: 10.1165/rcmb.2004-0060OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Williams OW, Sharafkhaneh A, Kim V, et al. Airway mucus: from production to secretion. Am J Respir Cell Mol Biol. 2006;34(5):527–36. doi: 10.1165/rcmb.2005-0436SF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akinbi HT, Epaud R, Bhatt H, et al. Bacterial killing is enhanced by expression of lysozyme in the lungs of transgenic mice. J Immunol. 2000;165(10):5760–6. doi: 10.4049/jimmunol.165.10.5760. [DOI] [PubMed] [Google Scholar]
- 25.Bals R, Weiner DJ, Moscioni AD, et al. Augmentation of innate host defense by expression of a cathelicidin antimicrobial peptide. Infect Immun. 1999;67(11):6084–9. doi: 10.1128/iai.67.11.6084-6089.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cole AM, Liao HI, Stuchlik O, et al. Cationic polypeptides are required for antibacterial activity of human airway fluid. J Immunol. 2002;169(12):6985–91. doi: 10.4049/jimmunol.169.12.6985. [DOI] [PubMed] [Google Scholar]
- 27.Cole AM, Thapa DR, Gabayan V, et al. Decreased clearance of Pseudomonas aeruginosa from airways of mice deficient in lysozyme M. J Leukoc Biol. 2005;78(5):1081–5. doi: 10.1189/jlb.0205073. [DOI] [PubMed] [Google Scholar]
- 28.Moser C, Weiner DJ, Lysenko E, et al. beta-Defensin 1 contributes to pulmonary innate immunity in mice. Infect Immun. 2002;70(6):3068–72. doi: 10.1128/IAI.70.6.3068-3072.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Evans SE, Hahn PY, McCann F, et al. Pneumocystis cell wall beta-glucans stimulate alveolar epithelial cell chemokine generation through nuclear factor-kappaB-dependent mechanisms. Am J Respir Cell Mol Biol. 2005;32(6):490–7. doi: 10.1165/rcmb.2004-0300OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agusti C, Rano A, Rovira M, et al. Inflammatory response associated with pulmonary complications in non-HIV immunocompromised patients. Thorax. 2004;59(12):1081–8. doi: 10.1136/thx.2004.030551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barton GM, Medzhitov R. Toll-like receptor signaling pathways. Science. 2003;300(5625):1524–5. doi: 10.1126/science.1085536. [DOI] [PubMed] [Google Scholar]
- 32.Boldrick JC, Alizadeh AA, Diehn M, et al. Stereotyped and specific gene expression programs in human innate immune responses to bacteria. Proc Natl Acad Sci USA. 2002;99(2):972–7. doi: 10.1073/pnas.231625398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kapetanovic R, Cavaillon JM. Early events in innate immunity in the recognition of microbial pathogens. Expert Opin Biol Ther. 2007;7(6):907–18. doi: 10.1517/14712598.7.6.907. [DOI] [PubMed] [Google Scholar]
- 34.Kawai T, Akira S. TLR signaling. Cell Death Differ. 2006;13(5):816–25. doi: 10.1038/sj.cdd.4401850. [DOI] [PubMed] [Google Scholar]
- 35.Kopp E, Medzhitov R. Recognition of microbial infection by Toll-like receptors. Curr Opin Immunol. 2003;15(4):396–401. doi: 10.1016/s0952-7915(03)00080-3. [DOI] [PubMed] [Google Scholar]
- 36.Zhang G, Ghosh S. Toll-like receptor-mediated NF-kappaB activation: a phylogenetically conserved paradigm in innate immunity. J Clin Invest. 2001;107(1):13–9. doi: 10.1172/JCI11837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ulevitch RJ. Therapeutics targeting the innate immune system. Nat Rev Immunol. 2004;4(7):512–20. doi: 10.1038/nri1396. [DOI] [PubMed] [Google Scholar]
- 38.Arevalo I, Tulliano G, Quispe A, et al. Role of imiquimod and parenteral meglumine antimoniate in the initial treatment of cutaneous leishmaniasis. Clin Infect Dis. 2007;44(12):1549–54. doi: 10.1086/518172. [DOI] [PubMed] [Google Scholar]
- 39.Kanistanon D, Hajjar AM, Pelletier MR, et al. A Francisella mutant in lipid A carbohydrate modification elicits protective immunity. PLoS Pathog. 2008;4(2):e24. doi: 10.1371/journal.ppat.0040024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lembo A, Pelletier M, Iyer R, et al. Administration of a synthetic TLR4 agonist protects mice from pneumonic tularemia. J Immunol. 2008;180(11):7574–81. doi: 10.4049/jimmunol.180.11.7574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Luhrmann A, Deiters U, Skokowa J, et al. In vivo effects of a synthetic 2-kilodalton macrophage-activating lipopeptide of Mycoplasma fermentans after pulmonary application. Infect Immun. 2002;70(7):3785–92. doi: 10.1128/IAI.70.7.3785-3792.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McHutchison JG, Bacon BR, Gordon SC, et al. Phase 1B, randomized, double-blind, dose-escalation trial of CPG 10101 in patients with chronic hepatitis C virus. Hepatology. 2007;46(5):1341–9. doi: 10.1002/hep.21773. [DOI] [PubMed] [Google Scholar]
- 43.Raberg L, Sim D, Read AF. Disentangling genetic variation for resistance and tolerance to infectious diseases in animals. Science. 2007;318(5851):812–4. doi: 10.1126/science.1148526. [DOI] [PubMed] [Google Scholar]
- 44.Williams TN, Mwangi TW, Wambua S, et al. Negative epistasis between the malaria-protective effects of alpha +-thalassemia and the sickle cell trait. Nat Genet. 2005;37(11):1253–7. doi: 10.1038/ng1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Evans SE, Scott BL, Clement CG, et al. Stimulated innate resistance of lung epithelium protects mice broadly against bacteria and fungi. Am J Respir Cell Mol Biol. 2009 Mar 27; doi: 10.1165/rcmb.2008-0260OC. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dennis DT, Inglesby TV, Henderson DA, et al. Tularemia as a biological weapon: medical and public health management. JAMA. 2001;285(21):2763–73. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- 47.Hilleman MR. Overview: cause and prevention in biowarfare and bioterrorism. Vaccine. 2002;20(25–26):3055–67. doi: 10.1016/s0264-410x(02)00300-6. [DOI] [PubMed] [Google Scholar]
- 48.Wayne Conlan J, Shen H, Kuolee R, et al. Aerosol-, but not intradermal-immunization with the live vaccine strain of Francisella tularensis protects mice against subsequent aerosol challenge with a highly virulent type A strain of the pathogen by an alphabeta T cell- and interferon gamma-dependent mechanism. Vaccine. 2005;23(19):2477–85. doi: 10.1016/j.vaccine.2004.10.034. [DOI] [PubMed] [Google Scholar]
- 49.Wilkening DA. Sverdlovsk revisited: modeling human inhalation anthrax. Proc Natl Acad Sci USA. 2006;103(20):7589–94. doi: 10.1073/pnas.0509551103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tuvim MJ, Evans SE, Clement CG, et al. Augmented lung inflammation protects against influenza A pneumonia. PLoS ONE. 2009;4(1):e4176. doi: 10.1371/journal.pone.0004176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clement CG, Evans SE, Evans CM, et al. Stimulation of lung innate immunity protects against lethal pneumococcal pneumonia in mice. Am J Respir Crit Care Med. 2008;177(12):1322–30. doi: 10.1164/rccm.200607-1038OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moghaddam SJ, Clement CG, De la Garza MM, et al. Haemophilus influenzae lysate induces aspects of the chronic obstructive pulmonary disease phenotype. Am J Respir Cell Mol Biol. 2008;38(6):629–38. doi: 10.1165/rcmb.2007-0366OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brandl K, Plitas G, Mihu CN, et al. Vancomycin-resistant enterococci exploit antibiotic-induced innate immune deficits. Nature. 2008;455(7214):804–7. doi: 10.1038/nature07250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hoogerwerf JJ, de Vos AF, Bresser P, et al. Lung inflammation induced by lipoteichoic acid or lipopolysaccharide in humans. Am J Respir Crit Care Med. 2008;178(1):34–41. doi: 10.1164/rccm.200708-1261OC. [DOI] [PubMed] [Google Scholar]
- 55.Reppe K, Tschernig T, Luhrmann A, et al. Immunostimulation with macrophage-activating lipopeptide-2 increased survival in murine pneumonia. Am J Respir Cell Mol Biol. 2009;40(4):474–81. doi: 10.1165/rcmb.2008-0071OC. [DOI] [PubMed] [Google Scholar]
- 56.Bagchi A, Herrup EA, Warren HS, et al. MyD88-dependent and MyD88-independent pathways in synergy, priming, and tolerance between TLR agonists. J Immunol. 2007;178(2):1164–71. doi: 10.4049/jimmunol.178.2.1164. [DOI] [PubMed] [Google Scholar]
- 57.Trinchieri G, Sher A. Cooperation of Toll-like receptor signals in innate immune defence. Nat Rev Immunol. 2007;7(3):179–90. doi: 10.1038/nri2038. [DOI] [PubMed] [Google Scholar]
- 58.Medzhitov R. Recognition of microorganisms and activation of the immune response. Nature. 2007;449(7164):819–26. doi: 10.1038/nature06246. [DOI] [PubMed] [Google Scholar]
- 59.Foster SL, Hargreaves DC, Medzhitov R. Gene-specific control of inflammation by TLR-induced chromatin modifications. Nature. 2007;447(7147):972–8. doi: 10.1038/nature05836. [DOI] [PubMed] [Google Scholar]
- 60.Tazawa R, Hamano E, Arai T, et al. Granulocyte-macrophage colony-stimulating factor and lung immunity in pulmonary alveolar proteinosis. Am J Respir Crit Care Med. 2005;171(10):1142–9. doi: 10.1164/rccm.200406-716OC. [DOI] [PubMed] [Google Scholar]
- 61.Anderson PM, Markovic SN, Sloan JA, et al. Aerosol granulocyte macrophage-colony stimulating factor: a low toxicity, lung-specific biological therapy in patients with lung metastases. Clin Cancer Res. 1999;5(9):2316–23. [PubMed] [Google Scholar]
- 62.Trapnell BC, Whitsett JA, Nakata K. Pulmonary alveolar proteinosis. N Engl J Med. 2003;349(26):2527–39. doi: 10.1056/NEJMra023226. [DOI] [PubMed] [Google Scholar]
- 63.Kinnula V, Mattson K, Cantell K. Pharmacokinetics and toxicity of inhaled human interferon-alpha in patients with lung cancer. J Interferon Res. 1989;9(4):419–23. doi: 10.1089/jir.1989.9.419. [DOI] [PubMed] [Google Scholar]
- 64.Maasilta P, Halme M, Mattson K, et al. Pharmacokinetics of inhaled recombinant and natural alpha interferon. Lancet. 1991;337(8737):371. doi: 10.1016/0140-6736(91)91009-j. [DOI] [PubMed] [Google Scholar]
- 65.Kinnula V, Cantell K, Mattson K. Effect of inhaled natural interferon-alpha on diffuse bronchioalveolar carcinoma. Eur J Cancer. 1990;26(6):740–1. doi: 10.1016/0277-5379(90)90132-d. [DOI] [PubMed] [Google Scholar]
- 66.Maasilta P, Holsti LR, Halme M, et al. Natural alpha-interferon in combination with hyperfractionated radiotherapy in the treatment of non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 1992;23(4):863–8. doi: 10.1016/0360-3016(92)90660-a. [DOI] [PubMed] [Google Scholar]
- 67.Giosue S, Casarini M, Alemanno L, et al. Effects of aerosolized interferon-alpha in patients with pulmonary tuberculosis. Am J Respir Crit Care Med. 1998;158(4):1156–62. doi: 10.1164/ajrccm.158.4.9803065. [DOI] [PubMed] [Google Scholar]
- 68.Giosue S, Casarini M, Ameglio F, et al. Aerosolized interferon-alpha treatment in patients with multi-drug-resistant pulmonary tuberculosis. Eur Cytokine Netw. 2000;11(1):99–104. [PubMed] [Google Scholar]
- 69.Martin RJ, Boguniewicz M, Henson JE, et al. The effects of inhaled interferon gamma in normal human airways. Am Rev Respir Dis. 1993;148(6 Pt 1):1677–82. doi: 10.1164/ajrccm/148.6_Pt_1.1677. [DOI] [PubMed] [Google Scholar]
- 70.Boguniewicz M, Martin RJ, Martin D, et al. The effects of nebulized recombinant interferon-gamma in asthmatic airways. J Allergy Clin Immunol. 1995;95(1 Pt 1):133–5. doi: 10.1016/s0091-6749(95)70162-1. [DOI] [PubMed] [Google Scholar]
- 71.Condos R, Raju B, Canova A, et al. Recombinant gamma interferon stimulates signal transduction and gene expression in alveolar macrophages in vitro and in tuberculosis patients. Infect Immun. 2003;71(4):2058–64. doi: 10.1128/IAI.71.4.2058-2064.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Raju B, Hoshino Y, Kuwabara K, et al. Aerosolized gamma interferon (IFN-gamma) induces expression of the genes encoding the IFN-gamma-inducible 10-kilodalton protein but not inducible nitric oxide synthase in the lung during tuberculosis. Infect Immun. 2004;72(3):1275–83. doi: 10.1128/IAI.72.3.1275-1283.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Condos R, Rom WN, Schluger NW. Treatment of multidrug-resistant pulmonary tuberculosis with interferon-gamma via aerosol. Lancet. 1997;349(9064):1513–5. doi: 10.1016/S0140-6736(96)12273-X. [DOI] [PubMed] [Google Scholar]
- 74.Condos R, Hull FP, Schluger NW, et al. Regional deposition of aerosolized interferon-gamma in pulmonary tuberculosis. Chest. 2004;125(6):2146–55. doi: 10.1378/chest.125.6.2146. [DOI] [PubMed] [Google Scholar]
- 75.Moss RB, Mayer-Hamblett N, Wagener J, et al. Randomized, double-blind, placebo-controlled, dose-escalating study of aerosolized interferon gamma-1b in patients with mild to moderate cystic fibrosis lung disease. Pediatr Pulmonol. 2005;39(3):209–18. doi: 10.1002/ppul.20152. [DOI] [PubMed] [Google Scholar]
- 76.Nakos G, Malamou-Mitsi VD, Lachana A, et al. Immunoparalysis in patients with severe trauma and the effect of inhaled interferon-gamma. Crit Care Med. 2002;30(7):1488–94. doi: 10.1097/00003246-200207000-00015. [DOI] [PubMed] [Google Scholar]
- 77.Virgolini I, Kurtaran A, Leimer M, et al. Inhalation scintigraphy with iodine-123-labeled interferon gamma-1b: pulmonary deposition and dose escalation study in healthy volunteers. J Nucl Med. 1997;38(9):1475–81. [PubMed] [Google Scholar]
- 78.Rao RD, Anderson PM, Arndt CA, et al. Aerosolized granulocyte macrophage colony-stimulating factor (GM-CSF) therapy in metastatic cancer. Am J Clin Oncol. 2003;26(5):493–8. doi: 10.1097/01.coc.0000037664.04141.D0. [DOI] [PubMed] [Google Scholar]
- 79.Niven RW, Whitcomb KL, Shaner L, et al. The pulmonary absorption of aerosolized and intratracheally instilled rhG-CSF and monoPEGylated rhG-CSF. Pharm Res. 1995;12(9):1343–9. doi: 10.1023/a:1016281925554. [DOI] [PubMed] [Google Scholar]
- 80.Machida M, Hayashi M, Awazu S. Pulmonary absorption of recombinant human granulocyte colony-stimulating factor (rhG-CSF) after intratracheal administration to rats. Biol Pharm Bull. 1996;19(2):259–62. doi: 10.1248/bpb.19.259. [DOI] [PubMed] [Google Scholar]
- 81.Gatmaitan BG, Carruthers MM, Lerner AM. Gentamicin in treatment of primary Gram-negative pneumonias. Am J Med Sci. 1970;260(2):90–4. doi: 10.1097/00000441-197008000-00003. [DOI] [PubMed] [Google Scholar]
- 82.Pines A, Raafat H, Plucinski K. Gentamicin and colistin in chronic purulent bronchial infections. Br Med J. 1967;2(5551):543–5. doi: 10.1136/bmj.2.5551.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Klastersky J, Geuning C, Mouawad E, et al. Endotracheal gentamicin in bronchial infections in patients with tracheostomy. Chest. 1972;61(2):117–20. doi: 10.1378/chest.61.2.117. [DOI] [PubMed] [Google Scholar]
- 84.Pines A, Raafat H, Siddiqui GM, et al. Treatment of severe pseudomonas infections of the bronchi. Br Med J. 1970;1(5697):663–5. doi: 10.1136/bmj.1.5697.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Odio W, Van Laer E, Klastersky J. Concentrations of gentamicin in bronchial secretions after intramuscular and endotracheal administration. J Clin Pharmacol. 1975;15(7):518–24. doi: 10.1002/j.1552-4604.1975.tb01474.x. [DOI] [PubMed] [Google Scholar]
- 86.Panidis D, Markantonis SL, Boutzouka E, et al. Penetration of gentamicin into the alveolar lining fluid of critically ill patients with ventilator-associated pneumonia. Chest. 2005;128(2):545–52. doi: 10.1378/chest.128.2.545. [DOI] [PubMed] [Google Scholar]
- 87.Carcas AJ, Garcia-Satue JL, Zapater P, et al. Tobramycin penetration into epithelial lining fluid of patients with pneumonia. Clin Pharmacol Ther. 1999;65(3):245–50. doi: 10.1016/S0009-9236(99)70103-7. [DOI] [PubMed] [Google Scholar]
- 88.Valcke YJ, Vogelaers DP, Colardyn FA, et al. Penetration of netilmicin in the lower respiratory tract after once-daily dosing. Chest. 1992;101(4):1028–32. doi: 10.1378/chest.101.4.1028. [DOI] [PubMed] [Google Scholar]
- 89.Braude AC, Hornstein A, Klein M, et al. Pulmonary disposition of tobramycin. Am Rev Respir Dis. 1983;127(5):563–5. doi: 10.1164/arrd.1983.127.5.563. [DOI] [PubMed] [Google Scholar]
- 90.Kuhn RJ. Pharmaceutical considerations in aerosol drug delivery. Pharmacotherapy. 2002;22(3 Pt 2):80S–5S. doi: 10.1592/phco.22.6.80s.33907. [DOI] [PubMed] [Google Scholar]
- 91.Goldstein I, Wallet F, Nicolas-Robin A, et al. Lung deposition and efficiency of nebulized amikacin during Escherichia coli pneumonia in ventilated piglets. Am J Respir Crit Care Med. 2002;166(10):1375–81. doi: 10.1164/rccm.200204-363OC. [DOI] [PubMed] [Google Scholar]
- 92.Goldstein I, Wallet F, Robert J, et al. Lung tissue concentrations of nebulized amikacin during mechanical ventilation in piglets with healthy lungs. Am J Respir Crit Care Med. 2002;165(2):171–5. doi: 10.1164/ajrccm.165.2.2107025. [DOI] [PubMed] [Google Scholar]
- 93.Klastersky J, Carpentier-Meunier F, Kahan-Coppens L, et al. Endotracheally administered antibiotics for gram-negative bronchopneumonia. Chest. 1979;75(5):586–91. doi: 10.1378/chest.75.5.586. [DOI] [PubMed] [Google Scholar]
- 94.Flume P, Klepser ME. The rationale for aerosolized antibiotics. Pharmacotherapy. 2002;22(3 Pt 2):71S–9S. doi: 10.1592/phco.22.6.71s.33909. [DOI] [PubMed] [Google Scholar]
- 95.Moore RD, Lietman PS, Smith CR. Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis. 1987;155(1):93–9. doi: 10.1093/infdis/155.1.93. [DOI] [PubMed] [Google Scholar]
- 96.Moore RD, Smith CR, Lietman PS. The association of aminoglycoside plasma levels with mortality in patients with gram-negative bacteremia. J Infect Dis. 1984;149(3):443–8. doi: 10.1093/infdis/149.3.443. [DOI] [PubMed] [Google Scholar]
- 97.Schentag JJ. Correlation of pharmacokinetic parameters to efficacy of antibiotics: relationships between serum concentrations, MIC values, and bacterial eradication in patients with gram-negative pneumonia. Scand J Infect Dis Suppl. 1990;74:218–34. [PubMed] [Google Scholar]
- 98.Deziel-Evans LM, Murphy JE, Job ML. Correlation of pharmacokinetic indices with therapeutic outcome in patients receiving aminoglycosides. Clin Pharm. 1986;5(4):319–24. [PubMed] [Google Scholar]
- 99.Collins T, Gerding DN. Aminoglycosides versus beta-lactams in gram-negative pneumonia. Semin Respir Infect. 1991;6(3):136–46. [PubMed] [Google Scholar]
- 100.Burns JL, Van Dalfsen JM, Shawar RM, et al. Effect of chronic intermittent administration of inhaled tobramycin on respiratory microbial flora in patients with cystic fibrosis. J Infect Dis. 1999;179(5):1190–6. doi: 10.1086/314727. [DOI] [PubMed] [Google Scholar]
- 101.Valcke Y, Pauwels R, Van der Straeten M. The penetration of aminoglycosides into the alveolar lining fluid of rats. The effect of airway inflammation. Am Rev Respir Dis. 1990;142(5):1099–103. doi: 10.1164/ajrccm/142.5.1099. [DOI] [PubMed] [Google Scholar]
- 102.Meers P, Neville M, Malinin V, et al. Biofilm penetration, triggered release and in vivo activity of inhaled liposomal amikacin in chronic Pseudomonas aeruginosa lung infections. J Antimicrob Chemother. 2008;61(4):859–68. doi: 10.1093/jac/dkn059. [DOI] [PubMed] [Google Scholar]
- 103.Davis KK, Kao PN, Jacobs SS, et al. Aerosolized amikacin for treatment of pulmonary Mycobacterium avium infections: an observational case series. BMC Pulm Med. 2007;7:2. doi: 10.1186/1471-2466-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.McCall CY, Spruill WJ, Wade WE. The use of aerosolized tobramycin in the treatment of a resistant pseudomonal pneumonitis. Ther Drug Monit. 1989;11(6):692–5. doi: 10.1097/00007691-198911000-00014. [DOI] [PubMed] [Google Scholar]
- 105.Dopfer R, Brand P, Mullinger B, et al. Inhalation of tobramycin in patients with cystic fibrosis: comparison of two methods. J Physiol Pharmacol. 2007;58(Suppl 5)(Pt 1):141–54. [PubMed] [Google Scholar]
- 106.Lenoir G, Antypkin YG, Miano A, et al. Efficacy, safety, and local pharmacokinetics of highly concentrated nebulized tobramycin in patients with cystic fibrosis colonized with Pseudomonas aeruginosa. Paediatr Drugs. 2007;9(Suppl 1):11–20. doi: 10.2165/00148581-200709001-00003. [DOI] [PubMed] [Google Scholar]
- 107.Ramsey BW, Dorkin HL, Eisenberg JD, et al. Efficacy of aerosolized tobramycin in patients with cystic fibrosis. N Engl J Med. 1993;328(24):1740–6. doi: 10.1056/NEJM199306173282403. [DOI] [PubMed] [Google Scholar]
- 108.Ratjen F, Doring G. Cystic fibrosis. Lancet. 2003;361(9358):681–9. doi: 10.1016/S0140-6736(03)12567-6. [DOI] [PubMed] [Google Scholar]
- 109.Canton R, Cobos N, de Gracia J, et al. Antimicrobial therapy for pulmonary pathogenic colonisation and infection by Pseudomonas aeruginosa in cystic fibrosis patients. Clin Microbiol Infect. 2005;11(9):690–703. doi: 10.1111/j.1469-0691.2005.01217.x. [DOI] [PubMed] [Google Scholar]
- 110.Sexauer WP, Fiel SB. Aerosolized antibiotics in cystic fibrosis. Semin Respir Crit Care Med. 2003;24(6):717–26. doi: 10.1055/s-2004-815667. [DOI] [PubMed] [Google Scholar]
- 111.Kun P, Landau LI, Phelan PD. Nebulized gentamicin in children and adolescents with cystic fibrosis. Aust Paediatr J. 1984;20(1):43–5. doi: 10.1111/j.1440-1754.1984.tb00035.x. [DOI] [PubMed] [Google Scholar]
- 112.Wall MA, Terry AB, Eisenberg J, et al. Inhaled antibiotics in cystic fibrosis. Lancet. 1983;1(8337):1325. doi: 10.1016/s0140-6736(83)92428-5. [DOI] [PubMed] [Google Scholar]
- 113.Steinkamp G, Tummler B, Gappa M, et al. Long-term tobramycin aerosol therapy in cystic fibrosis. Pediatr Pulmonol. 1989;6(2):91–8. doi: 10.1002/ppul.1950060207. [DOI] [PubMed] [Google Scholar]
- 114.Smith AL, Ramsey BW, Hedges DL, et al. Safety of aerosol tobramycin administration for 3 months to patients with cystic fibrosis. Pediatr Pulmonol. 1989;7(4):265–71. doi: 10.1002/ppul.1950070413. [DOI] [PubMed] [Google Scholar]
- 115.Ramsey BW, Pepe MS, Quan JM, et al. Intermittent administration of inhaled tobramycin in patients with cystic fibrosis. Cystic Fibrosis Inhaled Tobramycin Study Group. N Engl J Med. 1999;340(1):23–30. doi: 10.1056/NEJM199901073400104. [DOI] [PubMed] [Google Scholar]
- 116.Moss RB. Long-term benefits of inhaled tobramycin in adolescent patients with cystic fibrosis. Chest. 2002;121(1):55–63. doi: 10.1378/chest.121.1.55. [DOI] [PubMed] [Google Scholar]
- 117.Stephens D, Garey N, Isles A, et al. Efficacy of inhaled tobramycin in the treatment of pulmonary exacerbations in children with cystic fibrosis. Pediatr Infect Dis. 1983;2(3):209–11. doi: 10.1097/00006454-198305000-00007. [DOI] [PubMed] [Google Scholar]
- 118.Schaad UB, Wedgwood-Krucko J, Suter S, et al. Efficacy of inhaled amikacin as adjunct to intravenous combination therapy (ceftazidime and amikacin) in cystic fibrosis. J Pediatr. 1987;111(4):599–605. doi: 10.1016/s0022-3476(87)80130-0. [DOI] [PubMed] [Google Scholar]
- 119.Bilton D, Henig N, Morrissey B, et al. Addition of inhaled tobramycin to ciprofloxacin for acute exacerbations of Pseudomonas aeruginosa infection in adult bronchiectasis. Chest. 2006;130(5):1503–10. doi: 10.1378/chest.130.5.1503. [DOI] [PubMed] [Google Scholar]
- 120.Barker AF. Bronchiectasis. N Engl J Med. 2002;346(18):1383–93. doi: 10.1056/NEJMra012519. [DOI] [PubMed] [Google Scholar]
- 121.Rubin BK. Aerosolized antibiotics for non-cystic fibrosis bronchiectasis. J Aerosol Med Pulm Drug Deliv. 2008;21(1):71–6. doi: 10.1089/jamp.2007.0652. [DOI] [PubMed] [Google Scholar]
- 122.Drobnic ME, Sune P, Montoro JB, et al. Inhaled tobramycin in non-cystic fibrosis patients with bronchiectasis and chronic bronchial infection with Pseudomonas aeruginosa. Ann Pharmacother. 2005;39(1):39–44. doi: 10.1345/aph.1E099. [DOI] [PubMed] [Google Scholar]
- 123.Barker AF, Couch L, Fiel SB, et al. Tobramycin solution for inhalation reduces sputum Pseudomonas aeruginosa density in bronchiectasis. Am J Respir Crit Care Med. 2000;162(2 Pt 1):481–5. doi: 10.1164/ajrccm.162.2.9910086. [DOI] [PubMed] [Google Scholar]
- 124.Scheinberg P, Shore E. A pilot study of the safety and efficacy of tobramycin solution for inhalation in patients with severe bronchiectasis. Chest. 2005;127(4):1420–6. doi: 10.1378/chest.127.4.1420. [DOI] [PubMed] [Google Scholar]
- 125.Dodek P, Keenan S, Cook D, et al. Evidence-based clinical practice guideline for the prevention of ventilator-associated pneumonia. Ann Intern Med. 2004;141(4):305–13. doi: 10.7326/0003-4819-141-4-200408170-00011. [DOI] [PubMed] [Google Scholar]
- 126.Falagas ME, Siempos II, Bliziotis IA, et al. Administration of antibiotics via the respiratory tract for the prevention of ICU-acquired pneumonia: a meta-analysis of comparative trials. Crit Care. 2006;10(4):R123. doi: 10.1186/cc5032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rathgeber J, Zielmann S, Panzer C, et al. Prevention of pneumonia by endotracheal micronebulization of tobramycin. Anasthesiol Intensivmed Notfallmed Schmerzther. 1993;28(1):23–9. doi: 10.1055/s-2007-998870. [DOI] [PubMed] [Google Scholar]
- 128.Klastersky J, Huysmans E, Weerts D, et al. Endotracheally administered gentamicin for the prevention of infections of the respiratory tract in patients with tracheostomy: a double-blind study. Chest. 1974;65(6):650–4. doi: 10.1378/chest.65.6.650. [DOI] [PubMed] [Google Scholar]
- 129.Tablan OC, Anderson LJ, Besser R, et al. Guidelines for preventing health-care–associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep. 2004;53(RR-3):1–36. [PubMed] [Google Scholar]
- 130.Falagas ME, Agrafiotis M, Athanassa Z, et al. Administration of antibiotics via the respiratory tract as monotherapy for pneumonia. Expert Rev Anti Infect Ther. 2008;6(4):447–52. doi: 10.1586/14787210.6.4.447. [DOI] [PubMed] [Google Scholar]
- 131.Ghannam DE, Rodriguez GH, Raad II, et al. Inhaled aminoglycosides in cancer patients with ventilator-associated gram-negative bacterial pneumonia: safety and feasibility in the era of escalating drug resistance. Eur J Clin Microbiol Infect Dis. 2009;28(3):253–9. doi: 10.1007/s10096-008-0620-5. [DOI] [PubMed] [Google Scholar]
- 132.Palmer LB, Smaldone GC, Chen JJ, et al. Aerosolized antibiotics and ventilator-associated tracheobronchitis in the intensive care unit. Crit Care Med. 2008;36(7):2008–13. doi: 10.1097/CCM.0b013e31817c0f9e. [DOI] [PubMed] [Google Scholar]
- 133.Morosini MI, Garcia-Castillo M, Loza E, et al. Breakpoints for predicting Pseudomonas aeruginosa susceptibility to inhaled tobramycin in cystic fibrosis patients: use of high-range Etest strips. J Clin Microbiol. 2005;43(9):4480–5. doi: 10.1128/JCM.43.9.4480-4485.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Linden PK, Paterson DL. Parenteral and inhaled colistin for treatment of ventilator-associated pneumonia. Clin Infect Dis. 2006;43(Suppl 2):S89–S4. doi: 10.1086/504485. [DOI] [PubMed] [Google Scholar]
- 135.Michalopoulos A, Fotakis D, Virtzili S, et al. Aerosolized colistin as adjunctive treatment of ventilator-associated pneumonia due to multidrug-resistant gram-negative bacteria: a prospective study. Respir Med. 2008;102(3):407–12. doi: 10.1016/j.rmed.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 136.Kwa AL, Loh C, Low JG, et al. Nebulized colistin in the treatment of pneumonia due to multidrug-resistant Acinetobacter baumannii and Pseudomonas aeruginosa. Clin Infect Dis. 2005;41(5):754–7. doi: 10.1086/432583. [DOI] [PubMed] [Google Scholar]
- 137.Berlana D, Llop JM, Fort E, et al. Use of colistin in the treatment of multiple-drug-resistant gram-negative infections. Am J Health Syst Pharm. 2005;62(1):39–47. doi: 10.1093/ajhp/62.1.39. [DOI] [PubMed] [Google Scholar]
- 138.Hamer DH. Treatment of nosocomial pneumonia and tracheobronchitis caused by multidrug-resistant Pseudomonas aeruginosa with aerosolized colistin. Am J Respir Crit Care Med. 2000;162(1):328–30. doi: 10.1164/ajrccm.162.1.9910071. [DOI] [PubMed] [Google Scholar]
- 139.McCoy KS, Quittner AL, Oermann CM, et al. Inhaled aztreonam lysine for chronic airway Pseudomonas aeruginosa in cystic fibrosis. Am J Respir Crit Care Med. 2008;178(9):921–8. doi: 10.1164/rccm.200712-1804OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Safdar A. Strategies to enhance immune function in hematopoietic transplantation recipients who have fungal infections. Bone Marrow Transplant. 2006;38(5):327–37. doi: 10.1038/sj.bmt.1705439. [DOI] [PubMed] [Google Scholar]
- 141.Safdar A. Difficulties with fungal infections in acute myelogenous leukemia patients: immune enhancement strategies. Oncologist. 2007;12(Suppl 2):2–6. doi: 10.1634/theoncologist.12-S2-2. [DOI] [PubMed] [Google Scholar]
- 142.Safdar ARG, Lichtiger B, Dickey BF, et al. Recombinant interferon gamma 1 b immune enhancement in 20 patients with hematologic malignancies and systemic opportunistic infections treated with donor granulocyte transfusions. Cancer. 2006;106(12):2664–71. doi: 10.1002/cncr.21929. [DOI] [PubMed] [Google Scholar]
- 143.Montoya JG, Chaparro SV, Celis D, et al. Invasive aspergillosis in the setting of cardiac transplantation. Clin Infect Dis. 2003;37(Suppl 3):S281–92. doi: 10.1086/376527. [DOI] [PubMed] [Google Scholar]
- 144.Garcia-Vidal CUA, Kirby KA, Marr KA. Epidemiology of invasive mold infections in allogeneic stem cell transplant recipients: biological risk factors for infection according to time after transplantation. Clin Infect Dis. 2008;47(8):1041–50. doi: 10.1086/591969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mattiuzzi GN, Kantarjian H, Faderl S, et al. Amphotericin B lipid complex as prophylaxis of invasive fungal infections in patients with acute myelogenous leukemia and myelodysplastic syndrome undergoing induction chemotherapy. Cancer. 2004;100(3):581–9. doi: 10.1002/cncr.11936. [DOI] [PubMed] [Google Scholar]
- 146.Singh N, Limaye AP, Forrest G, et al. Late-onset invasive aspergillosis in organ transplant recipients in the current era. Med Mycol. 2006;44(5):445–9. doi: 10.1080/13693780600684494. [DOI] [PubMed] [Google Scholar]
- 147.Schmitt HJ, Bernard EM, Hauser M, et al. Aerosol amphotericin B is effective for prophylaxis and therapy in a rat model of pulmonary aspergillosis. Antimicrob Agents Chemother. 1988;32(11):1676–9. doi: 10.1128/aac.32.11.1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Cicogna CE, White MH, Bernard EM, et al. Efficacy of prophylactic aerosol amphotericin B lipid complex in a rat model of pulmonary aspergillosis. Antimicrob Agents Chemother. 1997;41(2):259–61. doi: 10.1128/aac.41.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Koizumi T, Kubo K, Kaneki T, et al. Pharmacokinetic evaluation of amphotericin B in lung tissue: lung lymph distribution after intravenous injection and airspace distribution after aerosolization and inhalation of amphotericin B. Antimicrob Agents Chemother. 1998;42(7):1597–600. doi: 10.1128/aac.42.7.1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Corcoran TE, Venkataramanan R, Mihelc KM, et al. Aerosol deposition of lipid complex amphotericin-B (Abelcet) in lung transplant recipients. Am J Transplant. 2006;6(11):2765–73. doi: 10.1111/j.1600-6143.2006.01529.x. [DOI] [PubMed] [Google Scholar]
- 151.Drew RH, Dodds Ashley E, Benjamin DK, Jr, et al. Comparative safety of amphotericin B lipid complex and amphotericin B deoxycholate as aerosolized antifungal prophylaxis in lung-transplant recipients. Transplantation. 2004;77(2):232–7. doi: 10.1097/01.TP.0000101516.08327.A9. [DOI] [PubMed] [Google Scholar]
- 152.Montoya JG, Giraldo LF, Efron B, et al. Infectious complications among 620 consecutive heart transplant patients at stanford university medical center. Clin Infect Dis. 2001;33(5):629–40. doi: 10.1086/322733. [DOI] [PubMed] [Google Scholar]
- 153.Palmer SM, Drew RH, Whitehouse JD, et al. Safety of aerosolized amphotericin B lipid complex in lung transplant recipients. Transplantation. 2001;72(3):545–8. doi: 10.1097/00007890-200108150-00036. [DOI] [PubMed] [Google Scholar]
- 154.Boots RJ, Paterson DL, Allworth AM, et al. Successful treatment of post-influenza pseudomembranous necrotising bronchial aspergillosis with liposomal amphotericin, inhaled amphotericin B, gamma interferon and GM-CSF. Thorax. 1999;54(11):1047–9. doi: 10.1136/thx.54.11.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Safdar A, O’Brien S, Kouri IF. Efficacy and feasibility of aerosolized amphotericin B lipid complex therapy in caspofungin breakthrough pulmonary zygomycosis. Bone Marrow Transplant. 2004;34(5):467–8. doi: 10.1038/sj.bmt.1704552. [DOI] [PubMed] [Google Scholar]
- 156.Dhand R, Guntur VP. How best to deliver aerosol medications to mechanically ventilated patients. Clin Chest Med. 2008;29(2):277–96. vi. doi: 10.1016/j.ccm.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 157.MacIntyre NR, Silver RM, Miller CV, et al. Aerosol delivery in intubated, mechanically ventilated patients. Crit Care Med. 1985;13(2):81–4. doi: 10.1097/00003246-198502000-00005. [DOI] [PubMed] [Google Scholar]
- 158.Aerosol consensus statement-1991. American Association for Respiratory Care. Respir Care. 1991;36(9):916–21. [PubMed] [Google Scholar]
- 159.Dhand R, Sohal H. Pulmonary drug delivery system for inhalation therapy in mechanically ventilated patients. Expert Rev Med Devices. 2008;5(1):9–18. doi: 10.1586/17434440.5.1.9. [DOI] [PubMed] [Google Scholar]
- 160.Blanchard JDCD, et al. Lung deposition of interferon gamma – 1b following inhalation via AERx System vs. Respirgard II™ nebulizer. Am J Respir Crit Care Med. 2003;167:A373. [Meeting Abstract] [Google Scholar]
- 161.Watts AB, McConville JT, Williams RO. Current therapies and technological advances in aqueous aerosol drug delivery. Drug Dev Ind Pharm. 2008;34(9):913–22. doi: 10.1080/03639040802144211. [DOI] [PubMed] [Google Scholar]