Abstract
Background and Purpose
This study evaluated clustering of stroke hospitalization rates, patterns of the clustering over time, and associations with community-level characteristics.
Methods
We used Medicare hospital claims data from 1995–1996 to 2005–2006 with a principal discharge diagnosis of stroke to calculate county-level stroke hospitalization rates. We identified statistically significant clusters of high- and low-rate counties by using local indicators of spatial association, tracked cluster status over time, and assessed associations between cluster status and county-level socioeconomic and healthcare profiles.
Results
Clearly defined clusters of counties with high- and low-stroke hospitalization rates were identified in each time. Approximately 75% of counties maintained their cluster status from 1995–1996 to 2005–2006. In addition, 243 counties transitioned into high-rate clusters, and 148 transitioned out of high-rate clusters. Persistently high-rate clusters were located primarily in the Southeast, whereas persistently low-rate clusters occurred mostly in New England and in the West. In general, persistently low-rate counties had the most favorable socioeconomic and healthcare profiles, followed by counties that transitioned out of or into high-rate clusters. Persistently high-rate counties experienced the least favorable socioeconomic and healthcare profiles.
Conclusions
The persistence of clusters of high- and low-stroke hospitalization rates during a 10-year period suggests that the underlying causes of stroke in these areas have also persisted. The associations found between cluster status (persistently high, transitional, persistently low) and socioeconomic and healthcare profiles shed new light on the contributions of community-level characteristics to geographic disparities in stroke hospitalizations.
Keywords: acute stroke, epidemiology, geography, hospitalization, Medicare, risk factors
Since the first report highlighting the concentration of high stroke death rates in the Southeastern United States, many parameters of the phenomenon loosely referred to as the Stroke Belt have been documented.1 Studies have shown that the excess burden of stroke in the Southeast exists for black and white women and men of all age groups.1–6 Furthermore, the pattern is evident regardless of the geographic unit that is used (eg, county, state economic area, state) and is observed for both stroke death and hospitalization rates.7–9
Several studies monitored changes in the geographic pattern of stroke death over time ranging from 1939 to 1996.2,4,5 The results show persistence in regional patterns with important changes in subregional patterns (eg, within the Southeast, the concentration of high-rate counties shifted away from the coastal regions to the Mississippi Delta). Missing from the literature is the systematic monitoring of geographic patterns for stroke hospitalization rates at the local level over time.
In this study, we examined temporal trends in the geographic patterns of stroke hospitalization rates among Medicare beneficiaries aged ≥65, from 1995–1996 to 2005–2006. We identified statistically significant clusters of high-rate and low-rate counties in each period and tracked the counties that remained in high- or low-rate clusters over time, as well as the counties that transitioned into or out of high-rate clusters. We then compared socioeconomic and healthcare profiles of counties by their cluster status (ie, persistently high, persistently low, or transitional).
Methods
Study Population
Our study included hospital claims data for fee-for-service Medicare beneficiaries aged ≥65 for 1995, 1996, 2005, and 2006 from the Centers for Medicare and Medicaid Services’ Medicare Provider Analysis and Review file, Part A. We defined a stroke hospitalization as a short-stay hospital claim with a principal (first-listed) discharge diagnosis of cerebrovascular disease by using the International Classification of Diseases, Ninth Revision, Clinical Modification codes 430 to 434 and 436 to 438. In this study, we refer to cerebrovascular disease as stroke. Beneficiaries were determined from the Medicare Denominator Files and were excluded if they were members of a health maintenance organization, died before July 1, or were <65 years on July 1 for each of the study years.
All stroke hospitalizations and Medicare beneficiaries were assigned to the county of the patient’s residence in the Medicare claims files. The study years were combined to create 2 periods: 1995–1996 and 2005–2006. Two-year stroke hospitalization rates were calculated for each period and age-adjusted by using the 2000 US standard population weights.10 Data for independent cities in Virginia were merged with their surrounding counties. Only counties located in the 48 contiguous United States that had at least 1 neighboring county were included (n=3074). Stroke hospitalization rates were calculated by using SAS software (version 9.1.3).11 Maps were created by using ArcMap software (version 10.0).12
Spatial Clustering Analyses
We undertook a 2-step process to assess positive spatial autocorrelation, or clustering. All spatial clustering analyses were conducted by using GeoDa software (version 0.9.5-i),13 and the Empirical-Bayes standardization method was used to account for variance instability caused by small population size in the denominator of the rates. We first assessed global spatial autocorrelation across counties by using a queen contiguity matrix to calculate the Moran I coefficient.14,15 We then calculated the Local Indicators of Spatial Association (LISA)16,17 to identify the locations of statistically significant clusters of counties with either higher or lower than average rates of stroke hospitalizations at a statistical significance level of <0.01. GeoDa LISA test results identify the counties located at the center of each cluster. In our maps, clusters include the counties at the center of a cluster plus the spatial neighbors of those counties.
To examine temporal trends in the clustering of stroke hospitalization rates, we compared the LISA estimates for 1995–1996 with the estimates for 2005–2006. Counties were categorized as either persistently high (belonged to a high-rate cluster in both periods), persistently low (belonged to a low-rate cluster in both periods), transitional (transitioned into or out of a high-rate cluster), or no statistically significant clustering.
County-level variables describing the social environmental and healthcare profiles were obtained from the 2007 Area Resource File.18 The Area Resource File compiles data from numerous sources. The healthcare variables originated from the American Medical Association and the American Hospital Association. Variables describing the socioeconomic profiles originated from the US Census Bureau. The urban–rural status, persistent poverty, and retirement destination variables originated from the U S Department of Agriculture.
Results
Our study population included ≈56 million Medicare beneficiaries for 1995–1996 and ≈55 million for 2005–2006 (Table 1). The national age-adjusted stroke hospitalization rate was 18 per 1000 during 1995–1996 and decreased to 13.6 per 1000 during 2005–2006 (Supplemental I). Rates varied by age, sex, and race or ethnicity, with the highest rates in both periods observed among those aged ≥85, blacks, and men. The global Moran I statistic for 1995–1996 was 0.491 (P=0.001) and 0.506 (P=0.001) for 2005–2006, confirming that spatial clustering was present.
Table 1.
Sociodemographic Characteristics and Age-Adjusted Stroke Hospitalization Rates by Time, Medicare Beneficiaries Aged ≥65
| Stroke Hospitalizations (%)
|
Medicare Beneficiaries (%)
|
Stroke Hospitalization Rate (per 1000)
|
||||
|---|---|---|---|---|---|---|
| 1995–1996 | 2005–2006 | 1995–1996 | 2005–2006 | 1995–1996 | 2005–2006 | |
| Total | 999 377 | 770 033 | 56 339 366 | 55 331 267 | 18.0 | 13.6 |
| Age, y | ||||||
| 65–74 | 37.8 | 32.5 | 54.7 | 49.9 | 12.3* | 9.1* |
| 75–84 | 42.7 | 42.3 | 33.5 | 36.1 | 22.6* | 16.3* |
| 85+ | 19.5 | 25.2 | 11.8 | 14.0 | 29.3* | 25.2* |
| Sex | ||||||
| Women | 56.0 | 55.0 | 59.6 | 57.7 | 16.3 | 12.4 |
| Men | 44.0 | 45.0 | 40.4 | 42.3 | 20.6 | 15.3 |
| Race/ethnicity | ||||||
| Black | 9.7 | 10.4 | 7.8 | 8.0 | 22.3 | 18.3 |
| Hispanic† | 0.6 | 1.5 | 0.6 | 1.6 | 18.3 | 12.4 |
| White | 87.3 | 85.3 | 88.7 | 87.5 | 17.7 | 13.2 |
| Other | 2.4 | 2.8 | 2.9 | 3.0 | 16.2 | 13.6 |
Age group–specific rate.
Hispanic ethnicity is not coded as a mutually exclusive group in the race/ethnicity collected in the Medicare data.
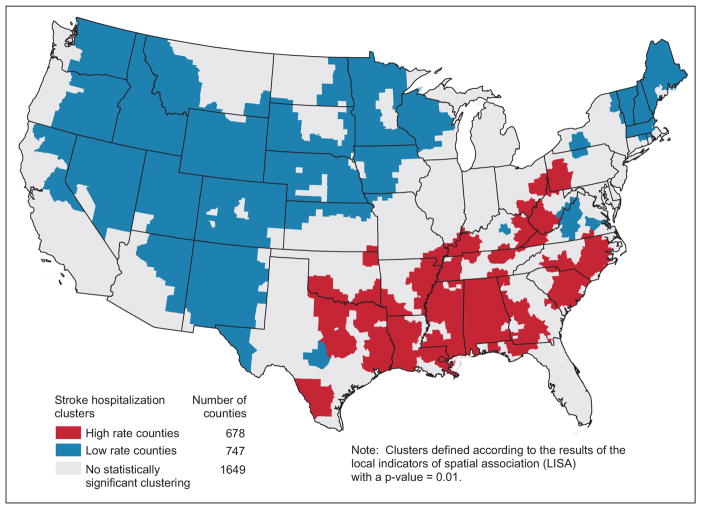
The LISA map for the total population in 2005–2006 (Figure 1) shows statistically significant clusters of both high-rate (22% of all counties) and low-rate counties (24% of all counties). The high-rate clusters were located in southern Appalachia and the Southeast, including much of Alabama, Mississippi, and Louisiana. The low-rate clusters were located in New England, the West, and the West North Central regions. Similar geographic patterns were observed for 1995–1996 (Supplemental Figures 1, 2, and 3).
Figure 1.
Clusters of age-adjusted stroke hospitalization rates among Medicare beneficiaries aged ≥65, 2005–2006—total population.
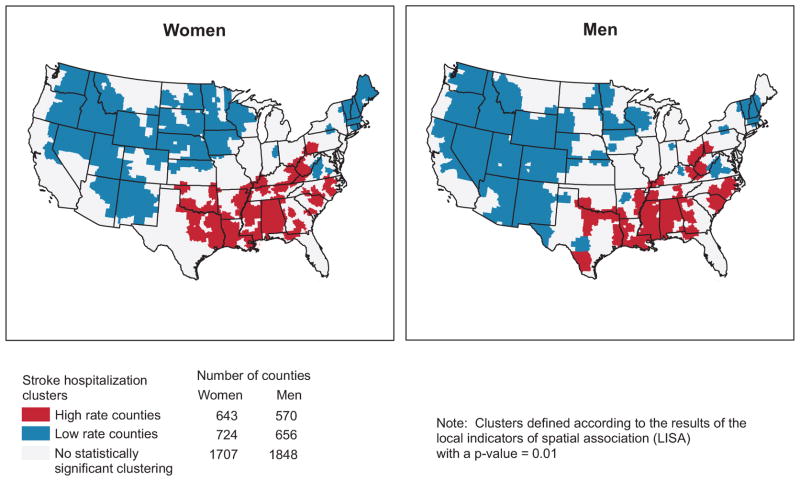
LISA maps by sex for 2005–2006 (Figure 2) show very similar patterns of geographic clustering of stroke hospitalization rates for women and men, with the overall pattern of high-rate clusters in the Southeast maintained. Slight variations in the cluster locations are found in Texas and the Midwest. In addition, we calculated cluster statistics by race; these LISA maps (Supplemental Figures 1, 2, and 3)show a very similar pattern to Figure 1, with high-rate clusters located primarily in the Southeast and Pennsylvania.
Figure 2.
Clusters of age-adjusted stroke hospitalization rates among Medicare beneficiaries aged ≥65, 2005–2006 by sex.
Comparison of LISA estimates between 1995–1996 and 2005–2006 shows that 75% of counties located in a high-rate cluster in 1995–1996 remained in a high-rate cluster for 2005–2006 (n=435). These persistently high-rate counties were found primarily in Appalachia, Alabama, Mississippi, Louisiana, and the coastal regions of North Carolina and South Carolina (Figure 3). Similarly, 76% of counties that were in a low-rate cluster during 1995–1996 remained in a low-rate cluster during 2005–2006 (n=533). These persistently low-rate counties were located primarily in the Mountain States, sections of the West North Central region, New England, and central Virginia. Approximately 25% of counties that were in a high-rate cluster during 1995–1996 (n=148) were no longer part of a high-rate cluster during 2005–2006. These transitional counties that exhibited improvement in stroke hospitalization rates were located in the coastal regions of Georgia and northern Florida, middle Tennessee, parts of the Mississippi Delta region, and near Portland, Oregon. Counties that had not been part of a high-rate cluster during 1995–1996, but became part of a high-rate cluster during 2005–2006 (n=243; 10%) were located primarily in Texas, southern Oklahoma, and western Georgia.
Figure 3.
Clusters of age-adjusted stroke hospitalization rates among Medicare beneficiaries aged ≥65: persistently high, persistently low, transitioned into high-rate cluster, transitioned out of a high-rate cluster, 1995–96 and 2005–2006.
Comparisons of socioeconomic and healthcare variables in persistently high-rate counties compared with persistently low-rate counties (Table 2) demonstrate that persistently high-rate counties had lower median income ($32 475 vs $40 698), higher proportions of people without a high school diploma (30.5% vs 17.2%), and higher proportions of people living in poverty (21.1% vs 12.9%). Furthermore, persistently high-rate counties had higher percentages of counties that were categorized as persistently poor (35.2% vs 4.7%), were more likely to be metropolitan (8.1% vs 5.1%), and were less likely to be designated as retirement destinations (6.7% vs 15.6%). In addition, persistently high-rate counties had fewer hospitals per 10 000 population than persistently low-rate counties (3.9 vs 8.0), but had a higher number of hospital admissions (10 146 vs 7009) and emergency room visits (43 836 vs 31 754) per 100 000, and fewer office-based general medicine physicians per 100 000 (23.3 vs 36.4).
Table 2.
Stroke Hospitalization Rates: Comparison of Persistently High-Rate Counties With Persistently Low-Rate Counties, Counties That Transitioned out of a High-Rate Cluster, and Counties That Transitioned Into a High-Rate Cluster, Medicare Beneficiaries, ≥65 Years
| Persistent Counties
|
Transitional Counties
|
||||||
|---|---|---|---|---|---|---|---|
| Column A
|
Column B
|
Column C
|
Column D
|
||||
| Persistently High-Rate Cluster*
|
Persistently Low-Rate Cluster†
|
Transitioned out of High-Rate Cluster‡
|
Transitioned Into High-Rate Cluster§
|
||||
| Value | Value | P Value|| | Value | P Value|| | Value | P Value|| | |
| Number of counties | 435 | 533 | 148 | 243 | |||
| Mean age-adjusted stroke hospitalization rate per 1000, 1995–1996 | 23.69 | 13.08 | <0.001 | 23.17 | 0.177 | 19.70 | <0.001 |
| Mean age-adjusted stroke hospitalization rate per 1000, 2005–2006 | 18.09 | 9.41 | <0.001 | 15.23 | <0.001 | 17.48 | 0.011 |
| Economic resources | |||||||
| Median household income, 2005,¶ $ | 32 475 | 40 698 | <0.001 | 36 057 | <0.001 | 35 019 | <0.001 |
| Median household income, 1995,¶ $ | 25 760 | 31 311 | <0.001 | 28 835 | <0.001 | 27 027 | 0.016 |
| Population in poverty, 2005,¶ % | 21.1 | 12.9 | <0.001 | 18.9 | <0.001 | 19.0 | <0.001 |
| Population without a high school diploma, 2000,# % | 30.5 | 17.2 | <0.001 | 28.9 | 0.116 | 28.1 | <0.001 |
| Counties in persistent poverty, 2004,** % | 35.2 | 4.7 | <0.001 | 27.0 | 0.069 | 25.1 | 0.007 |
| Health care | |||||||
| Short-term general hospitals per 100 000 population, 2005,¶ n | 3.9 | 8.0 | <0.001 | 3.5 | 0.243 | 3.4 | 0.003 |
| Short-term hospital beds per 100 000 population, 2005,¶ n | 301.7 | 367.1 | 0.392 | 261.1 | 0.032 | 235.5 | <0.001 |
| Short-term hospital admissions per 100 000 population, 2005,¶ n | 10 146 | 7009 | <0.001 | 8274 | 0.020 | 8480 | 0.050 |
| Emergency room visits per 100 000 population, 2005,¶ n | 43 836 | 31 754 | <0.001 | 39 317 | 0.150 | 38 624 | 0.037 |
| Office-based general practice MDs per 100 000 population, 2005,¶ n | 23.3 | 36.4 | <0.001 | 24.2 | 0.420 | 22.7 | 0.513 |
| Office-based general practice MDs per 100 000 population, 1995,¶ n | 22.6 | 31.9 | <0.001 | 22.7 | 0.976 | 21.1 | 0.071 |
| Urban/rural, 2003†† | |||||||
| Large metro, % | 8.1 | 5.1 | <0.001 | 18.9 | 0.002 | 11.1 | 0.283 |
| Small metro/micro, % | 47.8 | 39.2 | 37.8 | 49.4 | |||
| Noncore adjacent, % | 39.8 | 37.2 | 39.9 | 33.7 | |||
| Noncore nonadjacent, % | 4.4 | 18.6 | 3.4 | 5.8 | |||
| Migration | |||||||
| Population growth, 1995–2005, % | 5.3 | 7.5 | 0.141 | 16.3 | <0.001 | 11.6 | <0.001 |
| Retirement destinations, 2004,‡‡ % | 6.7 | 15.6 | <0.001 | 21.6 | <0.001 | 14.8 | <0.001 |
Counties located in a cluster of low rates in both 1995–1996 and 2005–2006.
Counties located in a cluster of high rates in both 1995–1996 and 2005–2006.
Counties located in a cluster of high rates in 1995–1996 but not in 2005–2006.
Counties not located in a cluster of rates in 1995–1996 but located in a cluster of high rates in 2005–2006.
Results of a statistical comparison between values in this column and values among counties located in persistently high-rate cluster (Column A).
Data from the Area Resource File (ARF).
US Census data from the ARF.
US Department of Agriculture (USDA) County Typology Codes from the ARF. Twenty percent or more of residents in poverty as measured in 1970, 1980, 1990, and 2000.
USDA Urban Influence Codes from the ARF.
USDA County Typology Codes from the ARF. Counties in which the number of residents 60 years or older grew by 15% or more during 1990–2000.
In general, socioeconomic and healthcare profiles of counties that transitioned out of high-rate clusters were better than corresponding profiles for persistently high-rate counties (Table 2). When compared with persistently high-rate counties, counties that transitioned out of high-rate clusters had higher median incomes ($36 057 vs $32 475), lower proportions of people living in poverty (18.9% vs 21.1%), fewer short-term hospital admissions per 100 000 population (8274 vs 10 146), higher population growth (16.3% vs 5.3%), greater percentage of counties designated as retirement destinations (21.6% vs 6.7%), and were more likely to be located in a large metropolitan area (18.9% vs 8.1%). The profiles for counties that transitioned into high-rate clusters during 2005–2006 were similar to those that transitioned out, with socioeconomic conditions that were worse than the counties in persistently low-rate clusters, but better than counties in persistently high-rate clusters. The urban/rural characteristics of these counties more closely matched those of the high-rate cluster counties with more counties located in small metropolitan areas.
Discussion
In this study, we found that clusters of counties with high- and low-stroke hospitalization rates remained largely intact from 1995–1996 to 2005–2006. Clusters of persistently high-rate counties were located predominantly in the Southeast and Appalachia. In contrast, clusters of persistently low-rate counties were located predominantly in New England and the West. However, changes in cluster status also occurred; 243 counties transitioned into high-rate clusters and 148 counties transitioned out of high-rate clusters. In general, socioeconomic and healthcare profiles were most favorable for persistently low-rate counties, followed by counties that transitioned into or out of high-rate clusters, and least favorable for persistently high-rate counties.
The observed geographic patterns of stroke hospitalization rates among Medicare beneficiaries are consistent with previously observed patterns of stroke incidence,9,19 prevalence,20 and death.1–6 The consistency of these geographic patterns supports the hypothesis that place-based characteristics play an important role in the occurrence of stroke and its risk factors.21–25 We examined 2 sets of place-based characteristics: socioeconomic resources and healthcare resources.
Our finding that counties with persistently high rates of stroke hospitalizations had the least favorable socioeconomic resources is consistent with other community-level studies of socioeconomic resources and stroke.26,27 In France, neighborhoods with the least favorable socioeconomic resources (eg, higher levels of unemployment, percentage renting main residence, percentage without a car, income inequality) had the highest levels of stroke incidence.27 A New Zealand study found community socioeconomic status (measured by average household income) to be inversely associated with the incidence of stroke, even after adjusting for individual income and individual-level risk factors for stroke.26 In the United States, the Brain Attack Surveillance in Corpus Christi Project reported an inverse association between neighborhood-level socioeconomic status and risk for stroke. The association was reduced when individual-level socioeconomic status was included; however, individual-level socioeconomic status was not available for ≈50% of the stroke cases.28 Many other studies have documented the association between community-level socioeconomic resources and other cardiovascular conditions, including coronary heart disease,21 atherosclerosis,22,25 hypertension,23,24 and cardiovascular disease death.29,30 Socioeconomic resources at the community level are widely understood to influence opportunities for residents to engage in healthy lifestyles that influence their risk for stroke (eg, diet and exercise,31 low stress levels,32 access to health care33).
Our findings that counties with persistently high-stroke hospitalization rates also had less access to primary health-care services (eg, fewer general practice physicians and more emergency room visits) are consistent with other studies that found higher rates of stroke death in communities with lower ratios of primary care physicians to the population.34,35 Stroke is preventable. Access to quality preventive care is particularly important for stroke prevention because the main risk factors for stroke (ie, hypertension, high cholesterol, diabetes mellitus) are preventable, modifiable, and should be assessed in the primary care setting.36,37
The observation that persistently high-rate counties had the fewest hospitals per population suggests that additional secondary treatment resources are needed in those counties. Increasingly, efforts are being made to provide telemedicine resources at hospitals located in rural areas to meet the need for specialized stroke treatment.37
The finding that, in general, counties transitioning into and out of high-rate clusters for stroke hospitalizations had socioeconomic and healthcare profiles that were more favorable than counties in persistently high-rate clusters, but not as favorable as counties in low-rate clusters, supports the hypothesis that improvements in socioeconomic and health-care resources can reduce the burden of stroke hospitalizations. Additional spatiotemporal studies are needed that address the effect of changing community-level resources on the burden of stroke.
The limitations in this study are restricted primarily to those inherent in using administrative databases for surveillance studies. The Centers for Medicare and Medicaid Services’ Medicare Provider Analysis and Review file does not include detailed nonbilling information and is subject to variation in coding practices. However, studies have found that International Classification of Diseases codes in administrative databases do accurately identify strokes.38–40 Our study population, traditional fee-for-service Medicare beneficiaries aged ≥65, represents ≈85% of the Medicare population. Although 70% of all stroke hospitalizations occur among people aged ≥65, blacks tend to have strokes at younger ages than whites;41,42 therefore, our rates for blacks may be underestimates. In addition, Hispanic ethnicity is not coded as a mutually exclusive group in the race/ethnicity collected in the Medicare data, and Hispanics also tend to have strokes at younger ages than whites, leading to underestimates in those rates.42,43 Last, Centers for Medicare and Medicaid Services’ Medicare Provider Analysis and Review Part A files do not distinguish between repeat hospitalizations and first-time hospitalizations; therefore, our data may include multiple hospitalizations for the same patient. Past studies have found a 1-year recurrence rate for stroke of <14%.44–46
The strengths of our study include the use of spatial statistics to identify and monitor county clusters of stroke hospitalization rates, the identification of transitional counties in addition to persistently high- and persistently low-rate clusters, and the inclusion of community-level healthcare profiles and socioeconomic profiles. The use of Medicare data enabled nationwide analysis of geographic patterns in stroke hospitalizations.
Summary
Age-adjusted stroke hospitalization rates among Medicare beneficiaries exhibited statistically significant and persistent spatial clustering in the United States. High-rate clusters were located predominantly in the Southeast and had the least favorable socioeconomic and healthcare profiles. In general, counties transitioning into and out of high-rate clusters for stroke hospitalizations had socioeconomic and healthcare profiles that were more favorable than counties in persistently high-rate clusters, but not as favorable as counties in low-rate clusters. These findings add a new dimension to understanding the role that social determinants play on geographic disparities and the burden of stroke.
Supplementary Material
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The online-only Data Supplement is available with this article at http://stroke.ahajournals.org/lookup/suppl/doi:10.1161/STROKEAHA.112.669705/-/DC1.
Disclosures
None.
References
- 1.Borhani NO. Changes and geographic distribution of mortality from cerebrovascular disease. Am J Public Health Nations Health. 1965;55:673–681. doi: 10.2105/ajph.55.5.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Casper M, Anda RF, Knowles M, Pollard RA, Wing S. The shifting stroke belt: changes in the geographic pattern of stroke mortality in the United States, 1962 to 1988. Stroke. 1995;26:755–760. doi: 10.1161/01.str.26.5.755. [DOI] [PubMed] [Google Scholar]
- 3.Casper ML, Barnett E, Williams GJ, Halverson J, Braham V, Greenlund K. Atlas of Stroke Mortality: Racial, Ethnic, and Geographic Disparities in the United States. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 4.Howard G, Howard VJ, Katholi C, Oli MK, Huston S. Decline in US stroke mortality: an analysis of temporal patterns by sex, race, and geographic region. Stroke. 2001;32:2213–2220. doi: 10.1161/hs1001.096047. [DOI] [PubMed] [Google Scholar]
- 5.Lanska DJ. Geographic distribution of stroke mortality in the United States: 1939–1941 to 1979–1981. Neurology. 1993;43:1839–1851. doi: 10.1212/wnl.43.9.1839. [DOI] [PubMed] [Google Scholar]
- 6.Pickle LW, Mungiole M, Gillum RF. Geographic variation in stroke mortality in blacks and whites in the United States. Stroke. 1997;28:1639–1647. doi: 10.1161/01.str.28.8.1639. [DOI] [PubMed] [Google Scholar]
- 7.Casper M, Nwaise I, Croft J, Nilasena D. Atlas of Stroke Hospitalizations Among Medicare Beneficiaries. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 8.Lanska DJ, Kryscio R. Geographic distribution of hospitalization rates, case fatality, and mortality from stroke in the United States. Neurology. 1994;44:1541–1550. doi: 10.1212/wnl.44.8.1541. [DOI] [PubMed] [Google Scholar]
- 9.Rich DQ, Gaziano JM, Kurth T. Geographic patterns in overall and specific cardiovascular disease incidence in apparently healthy men in the United States. Stroke. 2007;38:2221–2227. doi: 10.1161/STROKEAHA.107.483719. [DOI] [PubMed] [Google Scholar]
- 10.Klein RJ, Schoenborn CA. Age-Adjustment Using the 2000 Projected U.S. Population. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2001. [PubMed] [Google Scholar]
- 11.SAS Institute Inc. SAS 9.1.3 (computer program) Cary, NC: SAS Institute Inc; 2005. [Google Scholar]
- 12.ESRI. ArcMap 10.0 (computer program) Redlands, CA: ESRI; 2010. [Google Scholar]
- 13.Anselin L. GeoDa: An introduction to spatial data analysis. Geogr Anal. 2006;38:5–22. [Google Scholar]
- 14.Assunção RM, Reis EA. A new proposal to adjust Moran’s I for population density. Stat Med. 1999;18:2147–2162. doi: 10.1002/(sici)1097-0258(19990830)18:16<2147::aid-sim179>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 15.Moran PA. Notes on continuous stochastic phenomena. Biometrika. 1950;37:17–23. [PubMed] [Google Scholar]
- 16.Anselin L. Local Indicators of Spatial Association—LISA. Geogr Anal. 1995;27:93–115. [Google Scholar]
- 17.Baller RD, Anselin L, Messner SF, Deane G, Hawkins DF. Structural covariates of US county homicide rates: Incorporating spatial effects. Criminology. 2001;39:561–590. [Google Scholar]
- 18.US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions. Area Resource File (ARF) Rockville, MD: US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions; 2007. [Google Scholar]
- 19.El-Saed A, Kuller LH, Newman AB, Lopez O, Costantino J, McTigue K, et al. Geographic variations in stroke incidence and mortality among older populations in four US communities. Stroke. 2006;37:1975–1979. doi: 10.1161/01.STR.0000231453.98473.67. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) Prevalence of stroke—United States, 2005. MMWR Morb Mortal Wkly Rep. 2007;56:469–474. [PubMed] [Google Scholar]
- 21.Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 22.Kim D, Diez Roux AV, Kiefe CI, Kawachi I, Liu K. Do neighborhood socioeconomic deprivation and low social cohesion predict coronary calcification?: the CARDIA study. Am J Epidemiol. 2010;172:288–298. doi: 10.1093/aje/kwq098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Soc Sci Med. 2007;65:1853–1866. doi: 10.1016/j.socscimed.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008;19:590–598. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- 25.Murray ET, Diez Roux AV, Carnethon M, Lutsey PL, Ni H, O’Meara ES. Trajectories of neighborhood poverty and associations with subclinical atherosclerosis and associated risk factors: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2010;171:1099–1108. doi: 10.1093/aje/kwq044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brown P, Guy M, Broad J. Individual socio-economic status, community socio-economic status and stroke in New Zealand: a case control study. Soc Sci Med. 2005;61:1174–1188. doi: 10.1016/j.socscimed.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Grimaud O, Béjot Y, Heritage Z, Vallée J, Durier J, Cadot E, et al. Incidence of stroke and socioeconomic neighborhood characteristics: an ecological analysis of Dijon stroke registry. Stroke. 2011;42:1201–1206. doi: 10.1161/STROKEAHA.110.596429. [DOI] [PubMed] [Google Scholar]
- 28.Lisabeth LD, Diez Roux AV, Escobar JD, Smith MA, Morgenstern LB. Neighborhood environment and risk of ischemic stroke: the brain attack surveillance in Corpus Christi (BASIC) Project. Am J Epidemiol. 2007;165:279–287. doi: 10.1093/aje/kwk005. [DOI] [PubMed] [Google Scholar]
- 29.Diez Roux AV, Borrell LN, Haan M, Jackson SA, Schultz R. Neighbourhood environments and mortality in an elderly cohort: results from the cardiovascular health study. J Epidemiol Community Health. 2004;58:917–923. doi: 10.1136/jech.2003.019596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Waitzman NJ, Smith KR. Phantom of the area: poverty-area residence and mortality in the United States. Am J Public Health. 1998;88:973–976. doi: 10.2105/ajph.88.6.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chow CK, Lock K, Teo K, Subramanian SV, McKee M, Yusuf S. Environmental and societal influences acting on cardiovascular risk factors and disease at a population level: a review. Int J Epidemiol. 2009;38:1580–1594. doi: 10.1093/ije/dyn258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Finch BK, Phuong Do D, Heron M, Bird C, Seeman T, Lurie N. Neighborhood effects on health: Concentrated advantage and disadvantage. Health Place. 2010;16:1058–1060. doi: 10.1016/j.healthplace.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kirby JB, Kaneda T. Neighborhood socioeconomic disadvantage and access to health care. J Health Soc Behav. 2005;46:15–31. doi: 10.1177/002214650504600103. [DOI] [PubMed] [Google Scholar]
- 34.Shi L, Macinko J, Starfield B, Xu J, Politzer R. Primary care, income inequality, and stroke mortality in the United States: a longitudinal analysis, 1985–1995. Stroke. 2003;34:1958–1964. doi: 10.1161/01.STR.0000082380.80444.A9. [DOI] [PubMed] [Google Scholar]
- 35.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council for High Blood Pressure Research, Council on Peripheral Vascular Disease, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 37.Schwamm LH, Audebert HJ, Amarenco P, Chumbler NR, Frankel MR, George MG, et al. American Heart Association Stroke Council; Council on Epidemiology and Prevention; Interdisciplinary Council on Peripheral Vascular Disease; Council on Cardiovascular Radiology and Intervention. Recommendations for the implementation of telemedicine within stroke systems of care: a policy statement from the American Heart Association. Stroke. 2009;40:2635–2660. doi: 10.1161/STROKEAHA.109.192361. [DOI] [PubMed] [Google Scholar]
- 38.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43:480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
- 39.Fisher ES, Whaley FS, Krushat WM, Malenka DJ, Fleming C, Baron JA, et al. The accuracy of Medicare’s hospital claims data: progress has been made, but problems remain. Am J Public Health. 1992;82:243–248. doi: 10.2105/ajph.82.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tirschwell DL, Longstreth WT., Jr Validating administrative data in stroke research. Stroke. 2002;33:2465–2470. doi: 10.1161/01.str.0000032240.28636.bd. [DOI] [PubMed] [Google Scholar]
- 41.Sacco RL, Hauser WA, Mohr JP. Hospitalized stroke in blacks and Hispanics in northern Manhattan. Stroke. 1991;22:1491–1496. doi: 10.1161/01.str.22.12.1491. [DOI] [PubMed] [Google Scholar]
- 42.Sacco RL, Boden-Albala B, Gan R, Chen X, Kargman DE, Shea S, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke Study. Am J Epidemiol. 1998;147:259–268. doi: 10.1093/oxfordjournals.aje.a009445. [DOI] [PubMed] [Google Scholar]
- 43.Morgenstern LB, Smith MA, Lisabeth LD, Risser JM, Uchino K, Garcia N, et al. Excess stroke in Mexican Americans compared with non-Hispanic Whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004;160:376–383. doi: 10.1093/aje/kwh225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Allen NB, Holford TR, Bracken MB, Goldstein LB, Howard G, Wang Y, et al. Trends in one-year recurrent ischemic stroke among the elderly in the USA: 1994–2002. Cerebrovasc Dis. 2010;30:525–532. doi: 10.1159/000319028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brown DL, Lisabeth LD, Roychoudhury C, Ye Y, Morgenstern LB. Recurrent stroke risk is higher than cardiac event risk after initial stroke/transient ischemic attack. Stroke. 2005;36:1285–1287. doi: 10.1161/01.STR.0000165926.74213.e3. [DOI] [PubMed] [Google Scholar]
- 46.Dhamoon MS, Sciacca RR, Rundek T, Sacco RL, Elkind MS. Recurrent stroke and cardiac risks after first ischemic stroke: the Northern Manhattan Study. Neurology. 2006;66:641–646. doi: 10.1212/01.wnl.0000201253.93811.f6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.