Abstract
Background
Falling in the elderly results in a significant number of admissions to hospitals and long-term care facilities, especially among patients with lower extremity osteoarthritis (OA).
Objective
The aim of the study was to assess the risk of falling in adults older than 60 years with OA using timed up and go (TUG) test.
Materials and methods
A total of 187 patients (aged >60 years) were enrolled in the study. The assessment included: basic activities of daily living (ADLs), lower extremity strength with the use of the 30-second chair stand test (30 CST), and assessment of the risk of falling (TUG test). Pain intensity was evaluated with the numeric rating scale (NRS).
Results
The TUG test results were significantly better in younger OA patients (aged 60–69 years), as compared with their older peers (aged 70–79 years; P<0.01) and the oldest group (aged >80 years; P<0.001). Also, the 30 CST results were significantly higher in younger OA patients (P<0.05). Subjects older than 80 years had a significantly worse ADL score (P<0.05 and P<0.001). Pain complaints were reported significantly more frequently by women than men (P<0.05). A correlation between age and the TUG test score (r=0.412; P<0.0004) as well as between the TUG test and the 30 CST scores (r=0.7368; P=0.000) was detected. In the group with the TUG test score of <13.5 seconds, the 30 CST (P<0.0001) and ADL (P<0.003) results were significantly better. A comparison of fallers vs nonfallers revealed that the number of falls was significantly higher in the group of subjects who scored ≥13.5 when compared to <13.5 (P=0.003). Fallers significantly more often reported pain (P<0.0001), whereas nonfallers had significantly better 30 CST results (P=0.0003).
Conclusion
Elderly population with OA is at an elevated risk of falling, which increases with progressing age, pain, and muscle weakness. It seems prudent to identify individuals at a high risk of falling and to propose an adequate treatment for them.
Keywords: elderly, osteoarthritis, risk of falling
Introduction
The aging of the joints results in degenerative changes that lead to osteoarthritis (OA), which is diagnosed in ~60% of the population older than 60 years. Out of them, approximately 80% will suffer from significantly reduced joint mobility, but only 25% will be disabled.1 Radiological studies from the USA detected OA in approximately 80% of people older than 75 years.2 It usually affects the hip and knee, lumbar and cervical parts of the spine, as well as interphalangeal joints of hand. Mechanical pain, accompanied by loss of function and disability, is the main clinical manifestation of degenerative changes.1,2 Recent studies demonstrated that pain is independently correlated with the falls in the elderly inhabitants of community dwellings3 and is a vital issue as over 50% of that population experiences pain.4 A meta-analysis by Stubbs et al5 including over 17,000 elderly patients has shown that older patients with pain are at a higher risk of one or more falls in the course of the last 12 months. Prospective studies also demonstrated that the odds of falling are significantly higher in individuals with pain, especially with chronic pain.5 Also, pain in the elderly has been shown to be correlated with reduced mobility, as well as impaired gait and balance, in other words with internal risk factors for falls.6
Falls in individuals older than 65 years constitute one of the main threats of losing dexterity, mobility, and independence.7 Worldwide studies indicate that 20%–30% of the elderly fall at least once a year.8 In Poland, the problem is estimated to affect approximately 20% of the elderly population.9 Falls may lead to injuries, and women are more frequently at risk of fall-related injuries.10 The most common among them are lacerations.11 Serious injuries are the consequence of 10%–15% of all falls, including 5% of fractures (1%–2% fractures of the proximal femur). Research conducted by the Centers for Disease Control and Prevention in the USA demonstrated that every third faller required medical intervention or experienced activity limitation for at least 1 day.12
Due to various fall-related threats, the analysis of the risk of falling should constitute an inseparable element of dexterity evaluation in the elderly, particularly those with lower extremity OA. As numerous falls result from impaired balance and gait, their evaluation might constitute the basis for the analysis. In community settings, the timed up and go (TUG) test has been recommended as a simple screening tool, primarily to identify people who need more detailed assessment of gait and balance. The TUG test is recommended as a routine screening tool for risk of falls by the American Geriatric Society and British Geriatric Society.13 The National Institute of Clinical Evidence (NICE) recommends this test for gain and balance evaluation in fall prevention among the elderly.14 On the other hand, Schoene et al15 suggest that TUG test is not useful in differentiating between fallers and nonfallers among healthy elderly patients without functioning problems, while being extremely applicable when evaluating the elderly subjects with health, functioning, and basic activities of daily living (ADLs) problems.15 TUG test measures (in seconds) the time a person needs to rise from a chair with armrests, to walk the distance of 3 m with usual assistive devices, if necessary, turn, return to the chair, and sit down. TUG test is a composite measure of functional mobility. It includes transfer tasks (standing up and sitting down), walking, and turning, thus incorporating neuromuscular components such as power, agility, and balance.16 Faster test completion signals better dexterity and functional state, whereas the score of ≥13.5 is used as a cut-off point to identify the elderly individuals who are at risk for falls in community dwelling.17 The literature reports various threshold values to determine the risk of falls, from 10 to 33 seconds in the older studies,18 to up to 8.1–16 seconds according to the most recent findings.19
The aim of the study was to evaluate the risk of falling using the TUG test in people older than 60 years with diagnosed lower extremity OA. Additionally, we analyzed the effect of lower extremity strength and disease-related pain, as well as problems with basic ADLs, on the risk of falls in that group. To the best of our knowledge, the number of studies on that disease among those particular age groups of Central and Eastern Europe is limited at best.
Methods
Ethical approval
This study was approved by the Ethics Committee of Poznan University of Medical Sciences (No 838/13).
Study population
Out of 187 people aged >60 years with diagnosed lower extremity OA, 117 subjects (94 hip and 23 knee OA cases) were included in the further analysis. The inclusion criteria were age, degenerative diseases of the lower extremity, no signs of dementia, and patient consent. All participants were recruited among patients of various rehabilitation wards in Poznań. The characteristics of the patients are presented in Table 1.
Table 1.
Patient characteristics
| Parameter | Entire group | Women | Men | P-value |
|---|---|---|---|---|
| Sex | n=117 | n=96; 82.1% | n=21; 17.9% | n/s |
| Age (years) | ||||
| Mean ± SD | 73.1±6.5 | 73.9±6.0 | 69.5±7.4 | P<0.01 |
| Median; range | 73.0; 60–87 | 74.0; 63–87 | 65.0; 60–84 | |
| Weight (kg) | ||||
| Mean ± SD | 73.9±12.5 | 72.8±11.5 | 79.0±15.6 | P=0.0738 |
| Median; range | 74.0; 45–115 | 72.0; 45–100 | 78.0; 50–115 | |
| Height (cm) | ||||
| Mean ± SD | 164.0±7.0 | 161.0±5.0 | 174.0±7.0 | P<0.001 |
| Median; range | 163.0; 150–189 | 161.0; 150–176 | 174.0; 150–189 | |
| BMI | ||||
| Mean ± SD | 27.6±4.5 | 28.0±4.5 | 25.9±4.3 | P<0.05 |
| Median; range | 27.1; 16.1–41.6 | 27.5; 16.1–41.6 | 25.1; 20.8–35.5 | |
| Education | ||||
| Primary | n=23; 19.7% | n=20; 20.8% | n=3; 14.3% | P<0.01 |
| VET | n=23; 19.7% | n=14; 14.6% | n=9; 42.9% | |
| Secondary | n=52; 44.4% | n=49; 51.0% | n=3; 14.3% | |
| Higher | n=19; 16.2% | n=13; 13.5% | n=6; 28.6% | |
| MMSE | ||||
| Mean ± SD | 27.4±2.5 | 27.4±2.5 | 27.5±2.8 | n/s |
| Median; range | 28.0; 17–30 | 28.0; 17–30 | 29.0; 21–30 | |
| GDS | ||||
| Mean ± SD | 1.4±1.6 | 1.6±1.7 | 0.6±1.0 | P<0.05 |
| Median; range | 1.0; 0–5 | 1.0; 0–5 | 0.0; 0–3 | |
Abbreviations: BMI, body mass index; n/s, not specified; SD, standard deviation; MMSE, mini-mental state examination; GDS, geriatric depression scale; VET, Vocational Education and Training.
The study group included people who required no walking aid – 75 (64.1), one crutch – 14 (12%), two crutches – 26 (22.2%), and a walker – 2 (1.7%).
Procedure
Evaluation of each participant was based on selected elements of the comprehensive geriatric assessment. Mini-mental state examination (MMSE), also known as the Folstein test,20 was used as the screening test for cognitive impairment. MMSE is a screening tool that includes eleven questions in six sections, each representing a different cognitive domain or function (orientation, registration, attention and calculation, recall, language, and copying), with the maximum score of 30. A score of ≤23 points has been considered as evidence of cognitive impairment, with scores between 18 and 23 points indicating mild impairment and scores of ≤17 indicating severe impairment. We selected the cutoff for MMSE scores at ≤23 for inclusion in the study. Our reason for using this criterion was based on our clinical experience that people with very low MMSE scores have difficulties in following instructions.
The short form (15 questions) of the geriatric depression scale21 was used to identify the risk of depression. A threshold score of 5 points indicates an increased risk for depression.
Functional ability of each patient was assessed with regard to ADLs and lower extremity strength with the use of 30-second chair stand test (30 CST). The TUG test was selected to evaluate the risk of falling. All patients assessed pain intensity on the numeric rating scale (NRS) and provided information on their falls over the course of the last 12 months.
The Katz Index of Independence,22 assessing bathing, dressing, toileting, transferring, continence, and feeding, was used to measure ADLs. Patients receive 1 or 0 points for independence in each function (≤2 points – severe functional impairment in performance of ADLs, 3–4 points – moderate impairment, and 5–6 points – full function).
TUG test was used as a test for functional mobility and fall risk.16 A standard chair with armrests was used for all tests. The participant was asked to stand up, using the armrests if necessary, walk past a line 3 m away, turn around, and come back and sit down in the chair. Subjects were timed from the point when their buttocks rose from the chair to when their buttocks touched the chair when returning to the seated position. The instructions were to walk at a normal pace. Participants had one practice trial, and the second trial was timed. If a walking aid was usually used inside the home, then the walking aid was used during the test. Faster test completion indicated better functional and mobility status. The cut-off point of ≥13.5 was established as the study population was homogeneous in terms of disease type, all patients experienced problems with lower extremity functioning, and individuals with cognitive problems were excluded.17 Consecutive time ranges indicate a gradual increase in the risk for falls. TUG test score over 30 seconds suggests the need for a walking aid.16
The 30 CST is performed using a folding chair without arms, with seat height of 17 inches (43.2 cm). The participant is seated in the chair, back straight, and feet approximately shoulder width apart and placed on the floor. Arms are crossed at the wrists and held against the chest. The patient practices once or twice before completing the test. If patients must use their arms to complete the test, they are scored “0.” At the signal, the participant rises to a full stand (body erect and straight) and then returns back to the initial seated position. The participant is encouraged to complete as many full stands as possible within 30 seconds. The participant is instructed to fully sit between each stand. The score is the total number of stands within 30 seconds.23
Pain intensity, mobility, and well-being were assessed with the NRS.24 It is an 11-point scale on which patients rate functional mobility (0 – maximum disability and 10 – full ability to function), well-being (0 – worst and 10 – best mood), and pain intensity (0 – no pain, 1–3 – mild pain, 4–7 – moderate pain, and 8–10 – severe pain).
All participants supplied information about their falls over the last 12 months.
Statistical analysis
Data in interval measurement scale were present as means and standard deviations or medians and ranges in case data did not follow normal distribution. Categorical data were presented as percentages. The assumption that data follow normal distribution was checked by Shapiro–Wilk’s test. For comparison of two unpaired groups, unpaired t-test was used for data that follow normal distribution and homogeneity of variances. Homogeneity of variances was tested with Levene’s test. In case data were not normally distributed, nonparametric tests were used. Mann–Whitney U-test for comparing two groups and Kruskal–Wallis for comparison of more than two groups simultaneously. If statistically significant difference existed the Dunn’s multiple comparisons post hoc test was applied. The relationship between analyzed variables was measured with the Spearman’s rank correlation coefficient. Unpaired data for 2×2 or larger contingency tables were analyzed using the Chi-square test for independence or the Fisher–Freeman–Halton test, depending on observed frequencies. All results were considered significant at P<0.05. Statistical analysis was performed using statistical packages of STATISTICA v 10.0 (StatSoft Inc.) or StatXact v 9.0 (CytelStudio).
Results
The study group consisted of 117 people with OA, including 96 (82.1%) women and 21 (17.9%) men. Mean patient age is presented in Table 1. Women were statistically significantly older than men (73.9±6.0 years vs 69.5±7.4 years, respectively; P<0.01). Mean result of the MMSE test in the entire study group was 27.4±2.5 points and was comparable for women and men (27.4±2.5 points vs 27.5±2.8 points, respectively). Mean test result of the emotional state based on the 15-question geriatric depression scale was 1.4±1.6 points. Men achieved statistically significantly lower scores as compared to women (0.6±1.0 points vs 1.6±1.7 points, respectively; P<0.05). Regardless, despite a statistically significant difference, the results of both men and women were within the range, signifying lack of emotional disturbance. Detailed patient characteristics are presented in Table 1. Mean results of the functional tests with regard to sex and age group are presented in Tables 2 and 3.
Table 2.
Mean test results with regard to sex
| Variable | Entire roup
|
Women
|
Men
|
|---|---|---|---|
| n=117 | n=96 | n=21 | |
| TUG test (seconds) | |||
| Mean ± SD | 17.4±12.0 | 18.1±12.8 | 14.4±6.4 |
| Median; range | 14.9; 5–115 | 15.6; 5–115 | 12.9; 7–27 |
| ADL (points) | |||
| Mean ± SD | 5.7±0.6 | 5.8±0.5 | 5.7±0.7 |
| Median; range | 6.0; 3–6 | 6.0; 3–6 | 6.0; 4–6 |
| NRS (points) | |||
| Mean ± SD | 5.0±3.1 | 5.3±3.2 | 3.8±2.4 |
| Median; range | 5.0; 0–10 | 6.0; 0–10 | 5.0; 0–8 P<0.05 |
| 30 CST (points) | |||
| Mean ± SD | 5.9±5.0 | 5.7±4.9 | 7.1±5.3 |
| Median; range | 7.0; 0–14 | 7.0; 0–14 | 8.0; 0–14 |
Abbreviations: TUG, timed up and go; SD, standard deviation; ADL, activities of daily living; NRS, numeric rating scale; 30 CST, 30-second chair stand test.
Table 3.
Mean test results with regard to age
| Variable | 60–69 years
|
70–79 years
|
P-value | >80 years
|
P-value |
|---|---|---|---|---|---|
| n=38; 32.5% | n=55; 47.0% | n=24; 20.5% | |||
| TUG test (seconds) | |||||
| Mean ± SD | 12.9±5.2 | 19.4±15.3 | <0.01 vs 60–69 | 20.2±9.1 | <0.001 vs 60–69 |
| Median; range | 11.3; 7–27 | 16.1; 5–115 | 19.0; 8–43 | ||
| ADL (points) | |||||
| Mean ± SD | 6.0±0.2 | 5.7±0.6 | n/s | 5.4±0.8 | <0.001 vs 60–69 |
| Median; range | 6.0; 5–6 | 6.0; 3–6 | 6.0; 4–6 | <0.05 vs 70–79 | |
| NRS (points) | |||||
| Mean ± SD | 4.7±3.1 | 4.9±3.3 | n/s | 5.9±3.0 | n/s |
| Median; range | 5.0; 0–10 | 5.0; 0–10 | 6.0; 0–10 | ||
| 30 CST (points) | |||||
| Mean ± SD | 7.9±4.6 | 5.1±5.1 | <0.05 vs 60–69 | 4.6±4.4 | <0.05 vs 60–69 |
| Median; range | 10.0; 0–14 | 5.0; 0–14 | 5.0; 0–11 | ||
Abbreviations: n/s, not specified; TUG, timed up and go; SD, standard deviation; ADL, activities of daily living; NRS, numeric rating scale; 30 CST, 30-second chair stand test; vs, versus.
The TUG test was used to evaluate the risk of falling. Almost a half of the participants (n=62; 53.0%) scored ≥13.5 seconds, which signified the risk of falling.
Mean TUG test scores with regard to sex and age group are presented in Tables 2 and 3. Mean result was statistically significantly better in the group of younger patients (aged 60–69 years; n=38, 32.5%), as compared to their older peers (aged 70–79 years; n=55, 47.0%) and the oldest age group (>80 years; n=24, 20.5%), P<0.01 and P<0.001, respectively (Table 3). Similarly, younger patients (aged 60–69 years) scored ≥13.5 seconds statistically significantly more often (73.7%), as compared to their older peers (aged 70–79 years; 41.8%) and the oldest age group (>80 years; 25.0%). Also, a correlation between age and the TUG test score was found r=0.412 (P<0.0004).
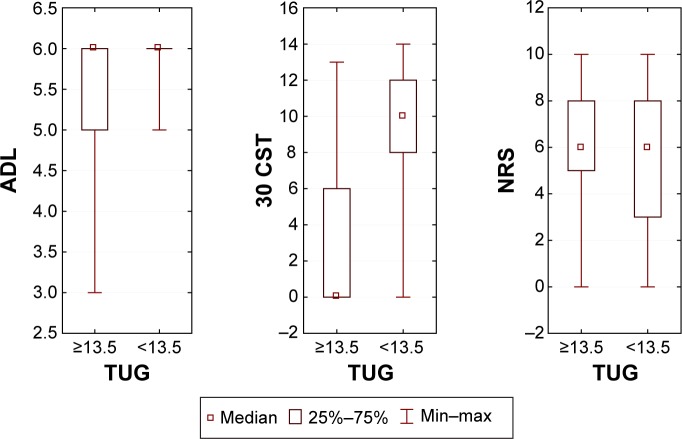
Figure 1 presents relationships between the investigated parameters and the TUG test score. Significantly better 30 CST (P<0.0001) and ADL (P<0.003) results were observed in the group with the score of <13.5 seconds, but no differences in experiencing pain were detected (P=0.441).
Figure 1.
Comparison of the TUG test score with 30 CST, NRS, and ADL results.
Abbreviations: TUG, timed up and go; 30 CST, 30-second chair stand test; NRS, numeric rating scale; ADL, activities of daily living.
The 30 CST was used to determine the number of stands a person completes when rising from a chair. Mean test result was 5.9±5.0 repetitions for the entire group. No statistically significant differences were found with regard to sex (Table 2). Mean result was statistically significantly better in the group of younger patients (aged 60–69 years), as compared to their older peers (aged 70–79 years) and the oldest (>80 years) age group, P<0.05 (Table 3). Every third participant was not able to complete the task and scored “0,” including 34.4% women (n=33) and 23.8% men (n=5). In terms of age, the task could not be performed by every sixth (n=6, 15.8%) person aged between 60 and 69 years, 40% (n=22) of patients aged 70–79 years, and 41.7% (n=10) of patients aged >80 years. A correlation between age and the 30 CST test was found (r=0.27955; P=0.002).
Mean ADL score was 5.7±0.6 points (Table 2). As far as basic ADLs are concerned, people older than 80 years scored statistically significantly worse than patients aged 60–69 years (P<0.001) and 70–79 years (P<0.05; Table 3). The vast majority of our respondents (n=93; 79.5%) obtained the maximum score of 6 points. The result was comparable in terms of sex: women (n=77; 80.2%) and men (n=16; 76.2%). Taking into account the maximum score and age, almost the entire group (n=37; 97.4%) of patients aged 60–69 years was fully functional as far as ADLs are concerned. Also, 43 subjects (78.2%) aged 70–79 years and 13 (54.2%) older than 80 years achieved the maximum result. A correlation between age and the ADL score was demonstrated (r=0.3928; P=0.0001).
Mean NRS score of self-reported pain intensity was 5.0±3.1 points. Women statistically significantly more often reported higher pain intensity as compared to men (P<0.05; Table 2). Mean result of pain intensity was comparable among all age groups (Table 3). Almost every sixth person declared no pain complaints (n=18; 15.4% [13 women: 13.5% and five men: 23.8%]). The highest-intensity pain (10 points) was reported only by women (n=10; 10.4%).
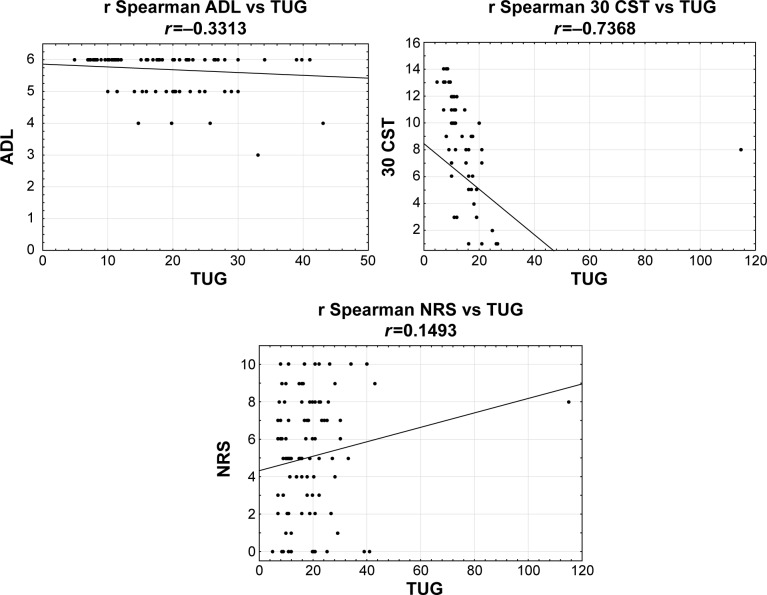
The correlation coefficient was calculated in order to investigate a possible correlation between the following variables: TUG test, 30 CST, ADLs, and NRS. The strongest correlation was found between TUG test and 30 CST results (r=0.7368; Figure 2). Moderate positive correlation was detected between TUG test vs ADLs (r=0.3313) and ADLs vs 30 CST (r=0.3735).
Figure 2.
The correlation between TUG test, 30 CST, and NRS.
Abbreviations: TUG, timed up and go; 30 CST, 30-second chair stand test; NRS, numeric rating scale; ADL, activities of daily living.
Analysis of the falls from the last 12 months revealed that 53 of 117 subjects took a fall. A correlation between a fall in the last year and TUG test time was found. The number of falls in the group of patients with the score of ≥13.5 seconds (58.06%) was statistically significantly different as compared to <13.5 seconds (30.91%; P=0.003).
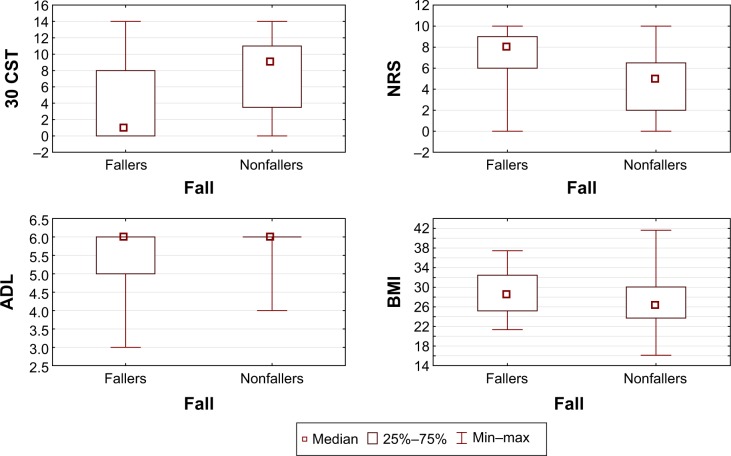
An analysis of lower extremity strength, pain, and functional ability in fallers vs nonfallers was performed. Statistically significantly greater pain complaints (NRS; P<0.00001) were reported by patients who had experienced a fall over the last 12 months. As far as lower extremity strength was concerned, nonfallers had significantly better results (P=0.0003). No differences were found in the realization of daily activities (P=0.053) between the groups. Also, the study population differed in terms of body mass index (BMI), which was significantly higher in the group of fallers (P<0.019). The results are presented in Figure 3.
Figure 3.
Test results in the groups of fallers and nonfallers.
Abbreviations: 30 CST, 30-second chair stand test; NRS, numeric rating scale; ADL, activities of daily living; BMI, body mass index.
The test results of fallers and nonfallers depending on the TUG test score (≥13.5 and <13.5) were analyzed. The results are presented in Table 4. Subjects with the TUG test score of ≥13.5 seconds who had experienced a fall over the last 12 months has significantly different pain scores (P<0.0002) as compared to nonfallers. Differences in lower extremity strength between the groups almost reached statistical significance (P=0.083). In the group with the score of <13.5 seconds, the only difference between fallers and nonfallers concerned pain complaints (P<0.0001).
Table 4.
Test results of fallers and nonfallers in the groups with TUG test scores of ≥13.5 and <13.5 seconds
| Variable | TUG ≥13.5; n=62
|
TUG <13.5; n=55
|
||||
|---|---|---|---|---|---|---|
| Fallers n=36 | Nonfallers n=26 | P-value | Fallers n=36 | Nonfallers n=26 | P-value | |
| 30 CST | ||||||
| Median | 0 | 2.5 | 0.083 | 10 | 10 | 0.214 |
| Range | 0–13 | 0–11 | 0–14 | 0–15 | ||
| ADL | ||||||
| Median | 6 | 6 | 0.183 | 6 | 6 | 0.849 |
| Range | 3–6 | 4–6 | 5–6 | 5–6 | ||
| NRS | ||||||
| Median | 7.5 | 5 | 0.0002 | 8 | 5 | 0.0001 |
| Range | 0–10 | 0–10 | 3–10 | 0–9 | ||
Abbreviations: TUG, timed up and go; 30 CST, 30-second chair stand test; ADL, activities of daily living; NRS, numeric rating scale.
Discussion
Our study revealed that people older than 60 years with confirmed diagnosis of hip and knee OA are at an increased risk of falling based on the prolonged TUG test time, which strongly correlated with weak muscle strength of the lower extremities, evaluated using 30 CST. Our study showed statistically significant differences between fallers and nonfallers in the group with the scores of <13.5 and ≥13.5 seconds (P<0.003), as well as between the fall and lower extremity strength (P=0.0003), pain complaints (P=0.0001), and BMI (P=0.019). Reports that a cut-off point should not be determined to identify individuals at higher risk for falls, who are independent and live in community dwelling have been published.19 Barry et al19 investigated elderly populations who lived in community dwellings. In our study, we included patients with lower extremity OA and established that, even if the cut-off point is not determined, the risk of falls increases with higher TUG test score.
In Poland, the problem of falling concerns ~20% of people older than 65 years and significantly increases with age. According to the POLSenior data, published in 2012, 12% of all individuals aged 65–69 years, and as many as 36% in the age group 90 years or older, fall.9 Although the falls are reported more frequently in females than males, the differences disappear after the age of 90.25 Most falls among the elderly take place during basic ADLs, such as walking (~40%), or getting in and out of bed (~25%).25
Our study demonstrated that hip and knee OA belong to the group of diseases that significantly increase the risk of falling assessed with TUG test. A study by Sturnieks et al revealed that elderly people with lower limb arthritis are at increased risk for falling due to deficits in the neuromuscular systems. These authors emphasized the need for targeted fall prevention interventions among this population, aiming to improve muscle strength of the lower limbs and proprioceptive acuity, resulting in better balance and reduced risk of falling.26
The findings of Sturnieks et al confirmed the results of our study in patients with hip and knee OA, indicating a correlation between the risk for falling (TUG test) and decreased muscle strength of the lower limbs (30 CST). Therefore, interventions suggested by these authors might be equally beneficial in case of OA patients.
Kerrigan et al27 indicated that loss of hip extension range and strength may be a biomechanical contributor to the risk for falling, whereas Arnold et al pointed to the activities directly contributing to falls, ie, reaching and getting up from a chair or bed. Those activities might also be directly associated with hip OA-related impairments due to the fact that they require weight shifting on one lower extremity to reach and adequate strength in hip musculature to move from the sitting to standing position.18
A study in older adults conducted by Niino et al28 detected that ~50% of all reported falls occurred during ambulation activities. While walking, patients need to bear 80% of their body weight on one limb for 60% of the gait cycle; in other words, the loading force through the hip greater is equal to two-times their body weight. People suffering from hip pain and/or muscle weakness surrounding the hip often tend to compensate for the decreased ability to support load on one limb by shifting the center of the body mass over the support limb, thus increasing the efficiency of the abductor muscles. As a result, an abnormal gait with a displacement of the center of gravity toward the side of the painful hip occurs.29
Varela-Burstein and Miller30 found that the presence of any arthritis or joint pain to be a risk factor for falls. In our study, only every sixth subject reported no pain complaints, what indirectly signals a risk of falling in that group of patients. We also demonstrated a strong correlation among pain intensity, TUG test, and 30 CST scores. Cecchi et al proved that hip or knee OA patients are at a higher risk of falling. Also, the future risk is significantly elevated if their condition is accompanied by joint pain and if they have a history of falling.31 In our study, patients with pain complaints fell significantly more often during the last 12 months, regardless of their TUG test scores. A similar correlation was observed by Stubbs et al5 whose comprehensive meta-analysis revealed that elderly patients with pain fell significantly more frequently during the last 12 months and were at risk of another fall in the future.
Another study reported an increased risk for falling in patients with hip joint pain.32 Therefore, pain is an important prognostic factor and its evaluation should always be included when assessing the risk for falling. A meta-analysis by Stubbs et al5 has shown, among numerous risk-promoting factors, a strong correlation with foot pain (n=691; OR=2.38; 95% CI =1.62–3.4) and chronic pain (OR=1.80; 95% CI =1.56–2.09; I2=0%). In yet another meta-analysis, Stubbs et al5 concluded that elderly patients with pain are also at risk of recurrent falling.
Pavol et al suggest that the biomechanical ability to prevent a fall depends on where the center of gravity is located while moving. An anterior shift of the center of gravity due to flexed posturing or loss of hip extension is associated with falling when a trip is induced. Buckling of a limb, which may occur due to pain or muscle weakness, greatly increases the risk of falling. The accumulation of gait adaptations due to OA-related hip pain, combined with aging, might increase the risk of falling during locomotion in that group of patients.33
Our study revealed a correlation between TUG test scores and ADLs performance. Viccaro et al34 during their 1-year observation of 500 veterans, also found that worse TUG test scores, apart from risk of falls, predispose to health decline and ADLs performance problems in formerly fit people. Regardless, Huang et al35 noticed that worse TUG test scores upon enrolment to the study predisposed to ADL disability within 6 months, but not within 12 and 18 months. In our study, a correlation was found between both, TUG test results and the scores obtained for ADLs, as well as between TUG test and self-reported well-being and mobility. Another study, conducted by Janssen et al confirmed that poor TUG test performance has been associated with poor muscle strength, poor balance, slow gait speed, fear of falling, physical inactivity, and impairments relating to basic and instrumental ADLs.36
Additionally, Arnold et al showed that ~45% among elderly (≥65) individuals with hip OA fell at least once in the course of the last 12 months, ie, more than the reported score of their healthy age peers (30%). The majority of these falls occurred during ambulation or while navigating steps and stairs, what often reflects OA-related gait impairment.18
Functional disability is a common consequence of falls. A study by Sekaran et al based on the Health and Retirement Study conducted on a representative group of USA inhabitants aged 51 years or older, estimated the 2-year risk of losing the ability to perform basic ADLs, eg, feeding or getting dressed, to be 80% and 30% for subjects after a fall with or without accompanying injury, respectively. The risk rises dramatically in the event of multiple falls, amounting to 275% and 140% after falls with or without injury.37
A study by Chu et al conducted in Hong Kong, observed the risk of losing the ability to perform basic and complex ADLs among fallers to increase threefold and fourfold, respectively, annually.38 Noteworthy, OA particularly disturbs the functioning of the lower extremities. Thus, it seems justifiable to use a testing tool that evaluates change of position gait and turn. All of the abovementioned activities are necessary for independent functioning as far as basic ADLs are concerned, in other words independence, what was confirmed by a correlation between the TUG test and ADL scores (r=0.2745; P=0.0280). It seems advisable for medical personnel who provide care to elderly OA patients to conduct routine evaluation of the risk for falls and pain, as it may have significant impact on later functioning of the affected individuals.
Limitations
The investigated population was relatively small because our study included patients with OA who participated in physiotherapeutic classes at rehabilitation wards and suffered from moderate to severe disease. Lower extremities OA was analyzed without distinguishing the type of joint deformity. The study population was predominantly female, what is proof of feminization among the elderly.
Conclusion
Based on our results, it seems safe to conclude that people with hip or knee OA are at a higher risk of falling due to prolonged time they required to complete the TUG test. Moreover, the future risk is further elevated in case of accompanying joint pain and muscle weakness. The results indicate that TUG test may be a useful tool for screening elderly populations with OA to predict mobility loss and frequency of falls. Thus, it seems prudent to identify older OA patients at a higher risk of falling and encourage them to engage in appropriate treatment strategies, indicating the need for fall prevention interventions in this age group.
Acknowledgments
We wish to offer our sincere thanks to patients who helped with the development of this work.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Górska-Zimmermann I. Osteoarthritis – a new look? Pol Arch Med Wewn. 2008;74-B:118–121. [Google Scholar]
- 2.Arden N, Nevitt MC. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol. 2006;20(1):3–25. doi: 10.1016/j.berh.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Muraki S, Akune T, Ishimoto Y, et al. Risk factors for falls in a longitudinal population-based cohort study of Japanese men and women: the ROAD study. Bone. 2013;52(1):516–523. doi: 10.1016/j.bone.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 4.Abdulla A, Adams N, Bone M, et al. British Geriatric Society Guidance on the management of pain in older people. Age Ageing. 2013;42(1):1–57. doi: 10.1093/ageing/afs200. [DOI] [PubMed] [Google Scholar]
- 5.Stubbs B, Binnekade T, Eggermont L, Sepehry AA, Patchay S, Schofield P. Pain and the risk for falls in community-dwelling older adults: systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95(1):175–187. doi: 10.1016/j.apmr.2013.08.241. [DOI] [PubMed] [Google Scholar]
- 6.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faulkner KA, Redfern MS, Cauley JA, et al. Health, Aging, and Body Composition Study Multitasking: association between poorer performance and a history of recurrent falls. J Am Geriatr Soc. 2007;55(4):570–576. doi: 10.1111/j.1532-5415.2007.01147.x. [DOI] [PubMed] [Google Scholar]
- 8.Milat AJ, Watson WL, Monger C, Barr M, Giffin M, Reid M. Prevalence, circumstances and consequences of falls among community-dwelling older people: results of the 2009 NSW Falls Prevention Baseline Survey. N S W Public Health Bull. 2011;22(3–4):43–48. doi: 10.1071/NB10065. [DOI] [PubMed] [Google Scholar]
- 9.Skalska A, Wizner B, Piotrowicz K, et al. The prevalence of falls and their relation to visual and hearing impairments among a nation-wide cohort of older Poles. Exp Gerontol. 2013;48(2):140–146. doi: 10.1016/j.exger.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Tinetti ME, Doucette J, Claus E, Marottoli R. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc. 1995;43(11):1214–1221. doi: 10.1111/j.1532-5415.1995.tb07396.x. [DOI] [PubMed] [Google Scholar]
- 11.Stevens JA. Self-reported falls and fall-related injuries among persons aged > or =65 years United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57(v):225–229. [PubMed] [Google Scholar]
- 12.Berry S, Miller R. Falls: epidemiology, pathophysiology, and relationship to fracture. Curr Osteoporos Rep. 2008;6(4):149–154. doi: 10.1007/s11914-008-0026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Panel on Prevention of Falls in Older Persons; American Geriatrics Society and British Geriatrics Society Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 14.NICE. The Assessment and Prevention of Falls in Older People. National Institute for Health and Care Excellence Manchester; 2013. Available from: http://www.nice.org.uk/CG161. [PubMed] [Google Scholar]
- 15.Schoene D, Wu SM, Mikolaizak AS, et al. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc. 2013;61(2):202–208. doi: 10.1111/jgs.12106. [DOI] [PubMed] [Google Scholar]
- 16.Podsiadlo D, Richardson S. The timed “up and go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 17.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed “up and go” test. Phys Ther. 2000;80(9):896–903. [PubMed] [Google Scholar]
- 18.Arnold CM, Faulkner RA. The history of falls and the association of the timed up and go test to falls and near-falls in older adults with hip osteoarthritis. BMC Geriatr. 2007;7:17. doi: 10.1186/1471-2318-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barry E, Galvin R, Keogh C, Horgan F, Fahey T. Is the timed up and go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr. 2014;1(14):14. doi: 10.1186/1471-2318-14-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bravo G, Hébert R. Age- and education-specific reference values for the mini-mental and modified mini-mental state examinations derived from a non-demented elderly population. Int J Geriatr Psychiatry. 1997;12(10):1008–1018. doi: 10.1002/(sici)1099-1166(199710)12:10<1008::aid-gps676>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 21.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 22.Katz S, Down TD, Cash HR, Grotz RC. Progress in the development of the index of ADL. Gerontologist. 1970;10(1):20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 23.Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1990;70(2):113. doi: 10.1080/02701367.1999.10608028. [DOI] [PubMed] [Google Scholar]
- 24.Moskovitz BL, Benson CJ, Patel AA, et al. Analgesic treatment for moderate-to-severe acute pain in the United States: patients’ perspectives in the physicians partnering against pain (P3) survey. J Opioid Manag. 2011;7(4):277–286. doi: 10.5055/jom.2011.0069. [DOI] [PubMed] [Google Scholar]
- 25.Mossakowska M, Więcek A, Błędowski P. Medical aspects, psychological, sociological and economic aging people in Poland. Polsenior Termedia Poznań. 2012:275–294. [Google Scholar]
- 26.Sturnieks DL, Tiedemann A, Chapman K, Munro B, Murray SM, Lord SR. Physiological risk factors for falls in older people with lower limb arthritis. J Rheumatol. 2004;31:2272–2279. [PubMed] [Google Scholar]
- 27.Kerrigan DC, Lee LW, Collins JJ, Riley PO, Lipsitz LA. Reduced hip extension during walking: healthy elderly and fallers versus young adults. Arch Phys Med Rehabil. 2001;82(1):26–30. doi: 10.1053/apmr.2001.18584. [DOI] [PubMed] [Google Scholar]
- 28.Niino N, Tsuzuku S, Ando F, Shimokata H. Frequencies and circumstances of falls in the National Institute for Longevity Sciences, Longitudinal Study of Aging (NILS-LSA) J Epidemiol. 2000;10(1):90–94. doi: 10.2188/jea.10.1sup_90. [DOI] [PubMed] [Google Scholar]
- 29.Barak Y, Wagenaar RC, Holt KG. Gait characteristics of elderly people with a history of falls: a dynamic approach. Phys Ther. 2006;86:1501–1510. doi: 10.2522/ptj.20050387. [DOI] [PubMed] [Google Scholar]
- 30.Varela-Burstein E, Miller PA. Is chronic pain a risk factor for falls among community dwelling elders? Top Geriatr Rehabil. 2003;19(2):145–159. [Google Scholar]
- 31.Cecchi F, Molino-Lova R, Di Iorio A, et al. Measures of physical performance capture the excess disability associated with hip pain or knee pain in older persons. J Gerontol A Biol Sci Med Sci. 2009;64(12):1316–1324. doi: 10.1093/gerona/glp125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muraki S, Akune T, Oka H, et al. Prevalence of falls and the association with knee osteoarthritis and lumbar spondylosis as well as knee and lower back pain in Japanese men and women. Arthritis Care Res (Hoboken) 2011;63:1425–1431. doi: 10.1002/acr.20562. [DOI] [PubMed] [Google Scholar]
- 33.Pavol MJ, Owings TM, Foley KT, Grabiner MD. Influence of Lower extremity strength of healthy older adults on the outcome of an induced trip. J Am Geriatr Soc. 2002;50:256–262. doi: 10.1046/j.1532-5415.2002.50056.x. [DOI] [PubMed] [Google Scholar]
- 34.Viccaro LJ, Perera S, Studenski SA. Is timed up and go better than gait speed in predicting health, function, and falls in older adults? J Am Geriatr Soc. 2011;59(5):887–892. doi: 10.1111/j.1532-5415.2011.03336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang WN, Perera S, VanSwearingen J, Studenski S. Performance measures predict onset of activity of daily living difficulty in community-dwelling older adults. J Am Geriatr Soc. 2010;58(5):844–852. doi: 10.1111/j.1532-5415.2010.02820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Janssen HC, Samson MM, Meeuwsen IB, Duursma SA, Verhaar HJ. Strength, mobility and falling in women referred to a geriatric outpatient clinic. Aging Clin Exp Res. 2004;16:122–125. doi: 10.1007/BF03324540. [DOI] [PubMed] [Google Scholar]
- 37.Sekaran NK, Choi H, Hayward RA, Langa KM. Fall-associated difficulty with activities of daily living in functionally independent individuals aged 65 to 69 in the United States: a cohort study. J Am Geriatr Soc. 2013;61:96–100. doi: 10.1111/jgs.12071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chu LW, Chiu AY, Chi I. Impact of falls on the balance, gait, and activities of daily living functioning in community-dwelling Chinese older adults. J Gerontol Med Sci. 2006;61(4):399–404. doi: 10.1093/gerona/61.4.399. [DOI] [PubMed] [Google Scholar]