Abstract
Aims
To describe the long-term natural history of a range of potential determinants of relapse from quitting smoking.
Design, setting and participants
A survey of 2502 ex-smokers of varying lengths of time quit recruited as part of the International Tobacco Control (ITC) Four Country Survey (Australia, Canada, UK, USA) across five annual waves of surveying.
Measurements
Quitters were phone interviewed at varying durations of abstinence, ranging from one to 1472 days (about 4 years) post quitting. Smoking-related beliefs and experiences (i.e., urges to smoke; outcome expectancies of smoking and quitting; and abstinence self-efficacy) were included in the survey.
Findings
Most theorised determinants of relapse changed over time in a manner theoretically associated with reduced risk of relapse, except most notably the belief that smoking controls weight, which strengthened. Change in these determinants changed at different rates: from a rapidly asymptoting log function to a less rapidly asymptoting square-root function.
Conclusions
Variation in patterns of change across time suggests that the relative importance of each factor to maintaining abstinence may similarly vary.
Keywords: smoking, tobacco, cessation, relapse
Introduction
At all ages, smoking cessation reduces the risk of premature death; after 10 to 15 years of abstinence the risk of premature death is almost equal to that of a non-smoker (1). Nevertheless, survival curves suggest that of those who quit smoking, most relapse (2–5). Although most relapse occurs within the first week or so after quitting (4), a percentage of former smokers relapse after having been abstinent for months or even years (3, 6–8). Brandon and colleagues (7) concluded from several smoking cessation studies that approximately one in eight unaided self-quitters who were abstinent at one year had relapsed by the following year.
Most smoking relapse research focuses on the early stages of quit attempts. Little is known about long-term quitting and predictors of relapse after prolonged abstinence (6). Effective prevention for late relapse is therefore limited (2, 7, 9). Research early in the cessation attempt has found that levels of potential predictors of relapse tend to change dramatically during the first few weeks of quitting, before plateauing thereafter (3, 10, 11).
This study investigates the long-term natural history of quitting among participants from the International Tobacco Control (ITC) Four Country Survey. This is a multi-country, longitudinal survey of smokers that was established to evaluate the psychosocial and behavioural impact of tobacco control policies (12). The study retains quitters, thus providing the opportunity to study predictors of relapse over time. It measures a range of theoretical mediators of smoking cessation outcomes, of which three sets of potential relapse determinants were explored: urges to smoke; outcome expectancies of smoking and quitting; and abstinence self-efficacy.
Cravings or urges to smoke are predictors of relapse (13–15). Urges are relatively sudden impulses to smoke not necessarily elicited by the physical symptoms of withdrawal (16), which are thought to arise from anticipated gratification from smoking in the presence of stimuli associated with past gratification (17). Research using multiple daily assessments on palm-top computers, found that the reported intensity of urges to smoke during the first four weeks of cessation decreased before appearing to plateau at about three weeks (10). Nevertheless, urges increased linearly in the days preceding an initial lapse in smoking and were highest during an actual lapse in smoking cessation (13). Similarly, retrospective accounts of relapse, particularly early in the quit attempt, often referred to cravings as precipitating relapse (14, 15). Urges may still be experienced even after six months of abstinence (18).
Outcome expectancies of performing a given health behaviour are predictive of that behaviour (16, 19, 20). Perceived costs of quitting (e.g., withdrawal, weight gain) and perceived benefits of smoking (e.g., anticipated relief from withdrawal or stress) are likely to heighten the likelihood of relapse (16, 21). Conversely, perceived costs of smoking (e.g., negative health consequences, money spent on cigarettes) and perceived benefits of quitting (e.g., enhanced quality of life, health benefits) should decrease the likelihood of relapse (21).
Gwaltney, Shiffman and colleagues (11) found that individual baseline differences and fluctuations in perceived benefits of smoking within quitters were both associated with lapses in smoking abstinence. After quitting, the perceived benefits of smoking decreased and then began to plateau from about two to five weeks. Dijkstra and Borland (22) found that among ex-smokers recruited at various durations of abstinence, perceived benefits of smoking predicted relapse at follow-up seven months later, but only when abstinence self-efficacy was low. Interestingly, they found that perceived benefits of smoking still appeared to be in decline years after quitting.
According to social cognitive theory (21, 23), successful quitting should result in increases in abstinence self-efficacy, reducing risk of relapse. There is good evidence for this, particularly during the early stages of quitting (3, 9, 24–26). One study revealed an initial increase in abstinence self-efficacy after quitting, which then appeared to plateau after about two weeks, but as they were only monitored for four to six weeks, the pattern of self-efficacy beyond this date was unknown. Segan, Borland, and Greenwood (3) found that in a sample of ex-smokers monitored for a year, abstinence self-efficacy was lowest for those who had quit for less than one week and highest among those who had quit for four to six months, with it plateauing after about one month. This plateau may be somewhat beneficial to maintaining abstinence. Borland and Balmford (9) found that when urges to smoke became less than daily, high self-efficacy (extremely high in this case) was associated with subsequent relapse, something they suggested may be due to overconfidence.
This paper describes how smoking related belief and experiences change as a function of duration of abstinence over a longer period than previously researched. From previous research it is clear that the rate of change is not linear; however, it is unclear if smoking related belief and experiences actually stabilize some time after quitting or if the rate of change simply slows to a rate that is more difficult to detect. If the latter, it might suggest that the change occurs as some mathematical function of time; square root and logarithmic transformations being plausible candidates. The aim of the current study was to investigate the long-term natural history of quitting smoking by exploring whether changes over time could be effectively modelled using logarithmic and square root transformations to account for the slowing of change with increasing duration of abstinence.
Method
Participants were drawn from the first five waves of the ITC-4 Survey, collected annually from 2002 through to 2007 in Australia, Canada, the UK, and the USA. They were first recruited as smokers using stratified random digit dialling and were surveyed using computer assisted telephone interview (CATI). Stratified sampling was used to try to obtain a representative sample of the smoking population in each country. Additional participants were recruited yearly to replace those lost to attrition. A detailed description of the ITC-4 Study aims and methods can be found in Thompson et. al. (27).
Participants
Participants were 2502 adults who were quit on at least one wave (see Figure 1), and reported the duration of abstinence. The ITC survey conducts the baseline interview a week or more after recruitment and, therefore, includes small numbers who quit before their initial survey. Participants who were quit at multiple waves contributed multiple response sets: 1615 participants contributed one set, 540 contributed two, 249 three, and 98 four; giving 3834 sets of responses across the five waves. Number of abstinent days quit across all five waves ranged from 1 to 1472, with a median of 180 and an interquartile range of 420 (280 participants were surveyed within a week of quitting, 483 between one week and one month, 1243 between one and six months, 669 between six and twelve months, 669 between one and two years, 347 between two and three years, and 143 after three years). As expected, mean number of days quit was higher for later waves.
Figure 1. Number of participants quit, relapsed, and lost by wave.
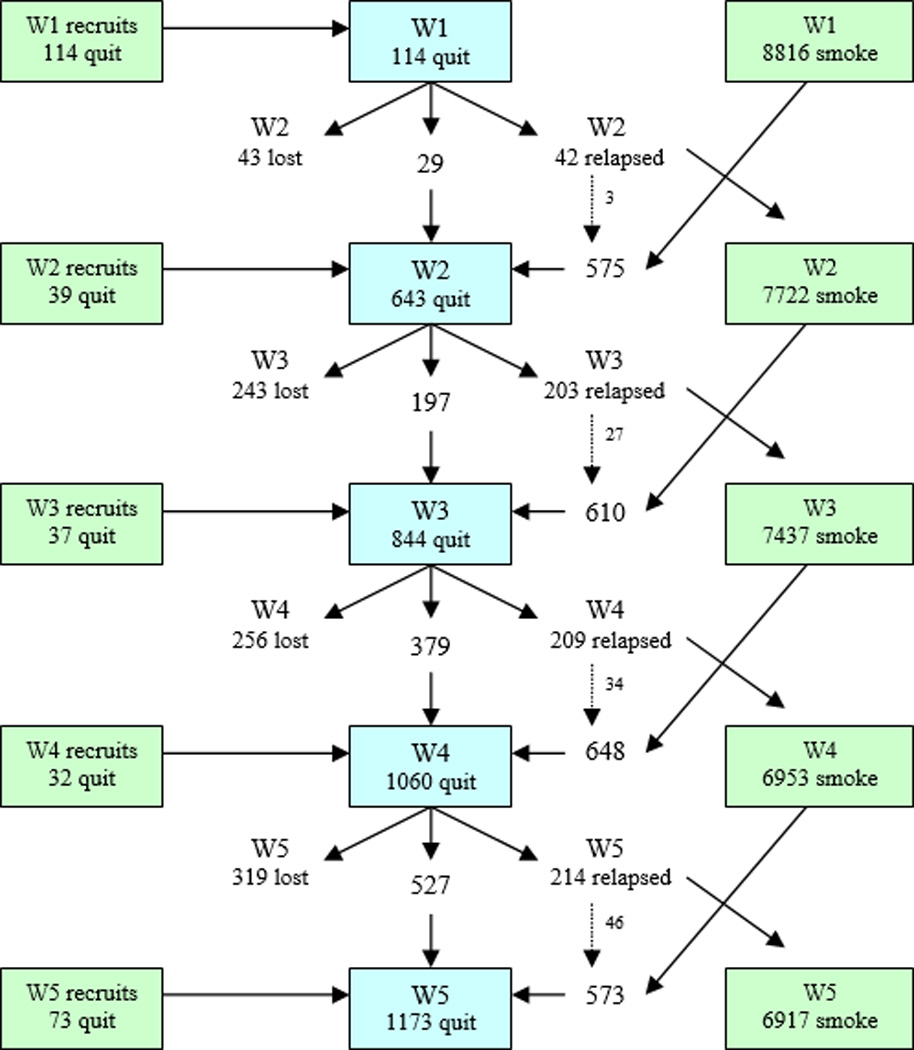
Note: The number of new recruits quit at each wave is shown in the boxes on the left. The dotted arrows indicate that some relapsers had quit again by the next wave. The number of smokers at each wave is shown in the boxes on the right; some of these smokers had quit by the subsequent wave.
Mean age of the sample was 42.6 years (SD=14.38) and 56% were female, 28% were from Australia, 27% from the UK, 24% from Canada, and the remaining 21% from the USA (see Table 1). Forty percent of participants reported smoking 1–10 cigarettes on average per day at the first survey they completed, 42% smoked 11–20, 12% smoked 21–30, and three percent smoked more than 30 cigarettes per day. The remaining participants (n=70) did not report the number of cigarettes smoked, primarily because those who had already quit smoking by their first survey were not asked.
Table 1.
Distribution of demographic variables by wave.
| Wave 1 N=114 |
Wave 2 N=643 |
Wave 3 N=844 |
Wave 4 N=1060 |
Wave 5 N=1173 |
|
|---|---|---|---|---|---|
| Sex | |||||
| Female | 50% | 57% | 54% | 57% | 57% |
| Male | 50% | 43% | 46% | 43% | 43% |
| Age group | |||||
| 18–24 yrs | 21% | 14% | 12% | 9% | 8% |
| 25–39 yrs | 35% | 36% | 34% | 30% | 29% |
| 40–54 yrs | 25% | 30% | 31% | 35% | 37% |
| 55<yrs | 19% | 19% | 24% | 26% | 26% |
| Country | |||||
| Australia | 25% | 24% | 29% | 29% | 30% |
| Canada | 20% | 29% | 25% | 24% | 24% |
| UK | 26% | 29% | 28% | 28% | 26% |
| USA | 29% | 19% | 18% | 19% | 20% |
| Median days quit (IQR) | 6 (11) | 90 (120) | 180 (300) | 297 (556) | 330 (642) |
Note: Percentages may not sum due to rounding.
May not sum to 100 due to missing responses.
Measures
Participants who had quit since the last wave were asked when they quit (in days, weeks, or months since quitting, or the specific date on which they quit). For participants who were still quit from the previous wave (without relapsing in between), duration of abstinence from the previous survey was added to the inter-survey interval. Participants who reported being quit, but then reported smoking at least once a month, were considered to be still smokers.
Survey items used to measure smoking related beliefs and experiences (Table 2) were drawn from established psychosocial models of health behaviour (refer to Fong et al (12)) and have been used in past research exploring predictors of quitting (28). Given that smokers generally endorse negative associations with smoking (e.g., negative health impact) (29–31), we measured frequency of thoughts about the costs of smoking, rather than conventional measures of strength of agreement with such attitudes. These three items were intended to be a somewhat crude measure of what Fazio and Williams (32) referred to as the accessibility or salience of a belief, rather than merely the presence or availability of such beliefs. Within this construct, the two questions measuring thoughts about the perceived harms of smoking (to self and to others) were moderately correlated (r=0.570, n=3805), so were combined into a single score. Internal consistency for the perceived benefits of quitting and the perceived benefits of smoking measures were low (α=0.38 and α=0.51, respectively); therefore, items were analysed individual.
Table 2.
Survey items.
| Construct | Questionnaire Item | Scale |
|---|---|---|
| Urges to smoke | How often do you get strong urges to smoke? | 1 = ‘Never’ to 5 = ‘Hourly or more often’ |
| Frequency of thoughts about perceived benefits of smoking | In the last month, how often, if at all, did you think about how much you enjoyed smoking? | 1 = ‘Never’ to 5 = ‘Very often’ |
| Perceived benefits of smoking | You enjoy smoking too much to give it up for good? (R) | 1 = ‘Strongly disagree’ to 5 = ‘Strongly agree’ |
| Smoking is an important part of your life? (R) | 1 = ‘Strongly disagree’ to 5 = ‘Strongly agree’ | |
| Smoking calms you down when you are stressed or upset? (R) | 1 = ‘Strongly disagree’ to 5 = ‘Strongly agree’ | |
| Smoking helps you control your weight? (R) | 1 = ‘Strongly disagree’ to 5 = ‘Strongly agree’ | |
| Frequency of thoughts about the perceived costs of smoking | In the last month, how often, if at all, did you think about the harm your smoking might have been doing to you if you were still smoking? | 1 = ‘Never’ to 5 = ‘Very often’ |
| In the last month, how often, if at all, did you think about the harm your smoking might have been doing to other people if you were still smoking? | 1 = ‘Never’ to 5 = ‘Very often’ | |
| In the last month, how often, if at all, did you think about the money you used to spend on smoking? | 1 = ‘Never’ to 5 = ‘Very often’ | |
| Perceived benefits of quitting | How much do you think you would benefit from health and other gains if you were to continue not to smoke in the next 6 months? | 1 = ‘Not at all’ to 5 = ‘Extremely’ |
| How would you compare your chance of getting heart disease in the future to the chance of a non-smoker? | 1 = ‘Much more likely’ to 4 = ‘Just as likely’ | |
| Now that you have quit, taking all things into account, is your overall quality of life: (insert options) than it was when you were smoking? (R) | 1 = ‘A lot worse’ to 5 = ‘A lot better’ | |
| Abstinence self-efficacy | How sure are you that you will succeed in quitting smoking for good at this attempt? | 1 = ‘Not at all sure’ to 5 = ‘Extremely sure’ |
R=Reversed scored prior to analysis to make graphs more intuitive to read.
Participants in wave 5 were excluded for the item ‘Smoking is an important part of your life’ as the wording of this item was altered for this wave.
Participants in waves 1 and 5 were not asked the item ‘How would you compare your chance of getting heart disease in the future to the chance of a non-smoker?’
Participants in waves 1 were not asked the items ‘How often do you get strong urges to smoke?’ and ‘Now that you have quit, taking all things into account, is your overall quality of life: (insert options) than it was when you were smoking?’
Statistical analysis
All analyses were performed using STATA 10. In order to explore the natural history of quitting according to a logarithmic representation of time, reported number of days abstinent was transformed by log base 10. Other bases were not explored, as they yield the same results (33). A square root transformation of days abstinent was used to explore a square root representation of time. The rate of change for logarithmic and square root functions decreases over time: a logarithmic function begins to plateau much sooner than a square root function, meaning that change is more drawn out for the latter.
Hierarchical linear regression analysis and generalised estimating equation models (GEE) (34) were independently fitted. GEE models control for the fact that respondents could provide up to four data points. An unstructured within-subject correlation structure was used, as this allowed for unequal spacings between observations. For GEE analyses, participants’ responses were only included up until relapse; if a participant had been quit at a given wave, but then subsequently relapsed before quitting again at a later wave, then only responses from the initial quit attempt were included for analysis. This was to ensure that duration of abstinence (i.e., number of days quit) for within-subject repeated measures remained sequential. Both methods were used separately to examine the relationships between transformed duration of abstinence and the dependent variables of interest (i.e., urges to smoke, outcome expectancies of smoking and quitting, and abstinence self-efficacy), after adjusting for demographic measures (i.e., sex, age, and country, all dummy coded). We explored log and square-root transformations of duration of abstinence. A significant linear relationship between duration of abstinence and a dependent measure indicated that the dependent variable changed over time according to the transformed function. To investigate potential deviations from this form of linearity, quadratic relationships between duration of abstinence and the dependent variables were explored by entering a squared duration of abstinence term to each model in the final step.
Due to the missing data for cigarette consumption per day at recruitment, we conducted analyses with and without this variable. Given that cigarette consumption did not alter the pattern of results, we report results in which this variable was not adjusted for in analyses. Graphs of the predicted linear and quadratic relationships between duration of abstinence and the dependent variables were generated using two-way linear and quadratic prediction plots from linear regressions in STATA. Reported trend coefficients are unstandardized.
Results
We first explored demographic differences in length of abstinence. ANOVAs revealed that the mean number of log days quit increased with age, F(3, 3830) = 14.83, p < 0.001 and varied according to country, F(3, 3830) = 3.94, p < 0.01. Mean number of days quit was lower for participants from the USA (log10[days quit] = 2.06) than for participants from the UK, Australia, and Canada (log10[days quit] = 2.16, 2.13, and 2.16, respectively). There was no significant difference in duration of abstinence by sex.
We considered if the observed demographic variations in duration of abstinence were due to different rates of drop out or relapse for certain demographics. Earlier drop-out or higher rates of relapse would result in overall shorter durations of abstinence for certain demographics. Results showed that a higher proportion of younger than older participants either dropped out of the study or relapsed between the four wave-to-wave transitions (Χ2(3)=51.84, p<0.001), but there was no significant effect by country (Χ2(3)=4.77, p=0.19). These results suggest that mean number of days quit was lower for younger participants, at least in part due to higher dropout rates, but potentially also to increased relapse.
As can be seen in Table 3, smoking related beliefs and experiences did not change in the same way over time, with changes varying from logarithmic to square root. These results are discussed in detail below.
Table 3.
Results from multiple regression analyses showing the relationships between duration of abstinence and beliefs about smoking.
| Dependent measures | Survey items | Fn | Days quit (fn) | Days quit (fn) squared | ||||
|---|---|---|---|---|---|---|---|---|
| Coef. | 95% CI | p value | Coef. | 95% CI | p value | |||
| Urges to smoke | Frequency of strong urges to smoke | Log | −0.85 | −0.90– −0.81 | <0.001 | |||
| Reasons for relapse | ||||||||
| Perceived benefits of smoking | Smoking calms you down when you are stressed | Log | −0.21 | −0.26– −0.16 | <0.001 | |||
| Enjoy smoking too much to give it up for good | Log | −0.26 | −0.30– −0.22 | <0.001 | ||||
| Smoking is an important part of your life | Log | −0.24 | −0.29– −0.19 | <0.001 | ||||
| Smoking helps control weight | Log | 0.14 | 0.08–0.19 | <0.001 | ||||
| Sq Root | 0.01 | 0.007–0.015 | <0.001 | |||||
| Thoughts about the enjoyment of smoking | Log | 0.18 | −0.05–0.41 | 0.12 | −0.21 | −0.27– −0.15 | <0.001 | |
| Sq Root | −0.08 | −0.09– −0.06 | <0.001 | 0.0008 | 0.0004–0.0013 | <0.001 | ||
| Reasons for staying quit | ||||||||
| Perceived costs of smoking | Thoughts about the harm of smoking (to you and to others)** | Log | −0.09 | −0.33–0.15 | 0.47 | −0.07 | −0.13– −0.01 | <0.05 |
| Thoughts about the money spent on smoking* | Log | 0.26 | −0.01–0.53 | 0.06 | −0.16 | −0.23– −0.08 | <0.001 | |
| Sq Root | −0.026 | −0.030– −0.021 | 0.001 | |||||
| Perceived benefits of quitting | Chance of getting heart disease in the future vs. a non-smoker? | Log | 0.28 | 0.21–0.35 | <0.001 | |||
| Quality of life compared to when smoking | Log | 0.26 | 0.22–0.31 | <0.001 | ||||
| Benefits of continuing not to smoke | Log | 0.003 | −0.05–0.05 | 0.92 | ||||
| Abstinence self-efficacy | How sure are you that you will succeed in quitting?** | Log | 0.16 | −0.03–0.36 | 0.10 | 0.08 | 0.03–0.13 | <0.01 |
Notes: Models adjusted for age, sex, and country. For each dependent variable, results from one of two models are presented: models with a duration of abstinence term or models including both a duration of abstinence term and a squared duration of abstinence term. Results from quadratic models were only reported if the squared duration of abstinence coefficient was significant. P-values for non-significant quadratic models ranged from 0.093 to 0.805.
Only the linear trend was significant when duration of abstinence was expressed on a square root scale.
GEE analysis found a significant linear trend, but not a significant quadratic trend.
Frequency of urges to smoke
Figure 2A shows the observed relationship between mean frequency of urges to smoke and duration of abstinence (plotted as a log function). Although urges declined over time, 13% of participants who had been quit for longer than six months still experienced strong urges to smoke at least daily; this compares to 79% of participants who had been quit for less than a week. The graph in Figure 2B shows the smoothed regression function of urges to smoke onto the logarithm of duration of abstinence (95% confidence intervals are shaded).
Figure 2. Duration of abstinence by frequency of urges to smoke: mean urges over time and best fit linear regression line with 95% confidence intervals.
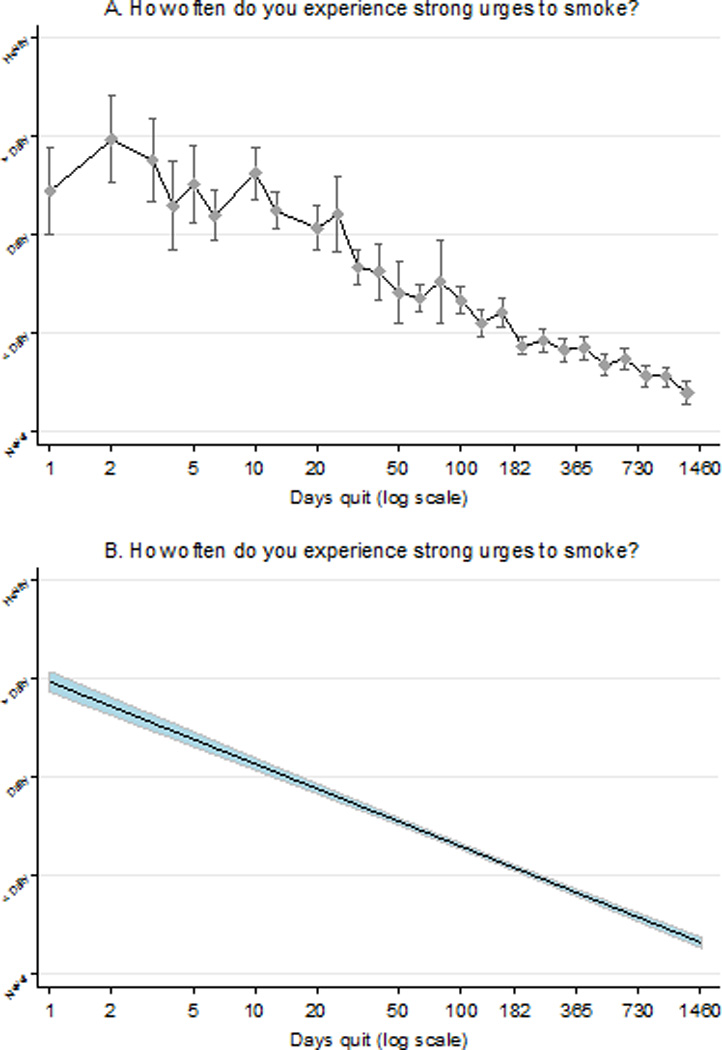
Note: To ensure a sufficient number of participants at each data point in the later stages of quitting for the first graph, the transformed number of days quit variable was rounded to one decimal place. Three data points (days quit [log10] 0.9, 1.2, & 3.1) had fewer than 20 participants and, therefore, for the purposes of this graph only, were recoded into the category below.
Perceived benefits of smoking
Four of the five perceived benefits of smoking changed over time in a log-linear way. For example, Figure 3A shows the significant log-linear relationship between duration of abstinence and “smoking calms you down when stressed”. Similar relationships were found for “smoking is too enjoyable to give up for good”, and “smoking is an important part of life”. This suggests that the rate of decline for these beliefs asymptotes over time. Despite noticeable decreases in agreement, more than half (58%) of the participants who had been quit for longer than one year still agreed or strongly agreed with the belief that smoking calms you down when stressed. By contrast, after one year of being quit, only 6% of participants believed that smoking was too enjoyable to give up for good and 9% believed that smoking was an important part of life.
Figure 3. Duration of abstinence by perceived benefits of smoking: best fit regression lines with 95% confidence intervals.
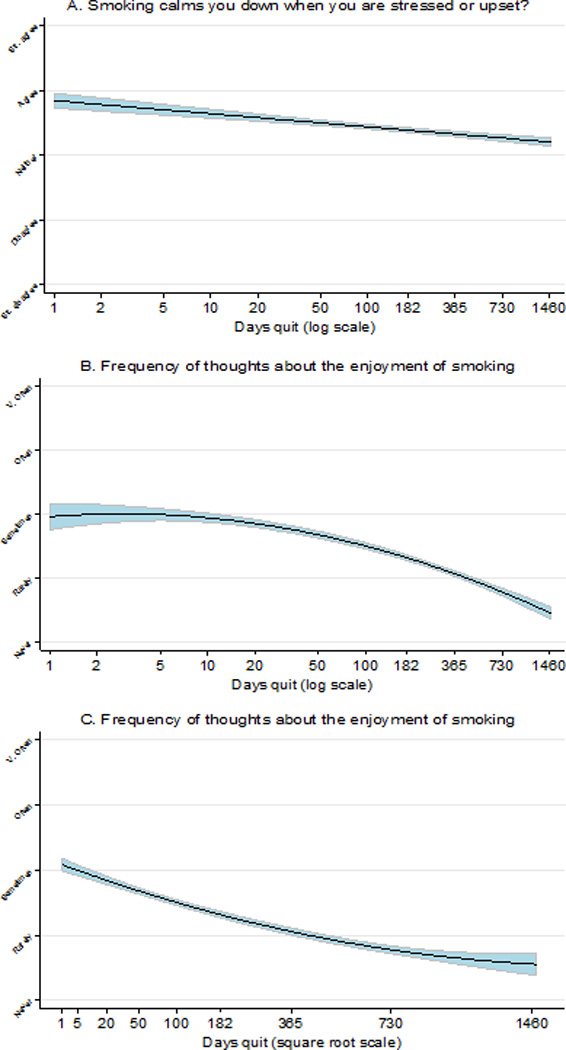
There were significant positive log-linear and square-root-linear relationships between duration of abstinence and the belief that smoking helps control weight. The two transforms accounted for a similar amount of variance and both trends were almost identical when graphed, because of the slow rate of change. Mean level of agreement increased over time from slight disagreement to slight agreement.
Frequency of thoughts about the enjoyment of smoking changed in a more complex way; there were similar sized significant negative log-quadratic and square-root-quadratic relationships between frequency of thoughts and duration of abstinence. For the log-quadratic model (Figure 3B), rate of change accelerated with increasing duration of abstinence, whereas for the square-root-quadratic model (Figure 3C), rate of change decelerated over time, suggesting some intermediate rate of change.
Perceived costs of smoking
Frequency of thoughts about the harms of smoking decreased according to a log-quadratic function in the regression analysis, but according to a log-linear function in the GEE analysis (linear estimate = −0.32, 95% CI = −0.38 – −0.26, p < 0.001) although the quadratic term was trending towards significance (quadratic estimate = −0.06, 95% CI = −0.12 – 0.01, P=0.07). By contrast, thoughts about the money spent on smoking decreased linearly with the square root transformation of time quit.
Perceived benefits of quitting
Two of the three perceived benefits of quitting changed over time according to a log-linear trend. With increasing duration of abstinence, participants were less likely to think that they had a significantly increased chance of getting heart disease in the future compared to a non-smoker. Nevertheless, almost a third (30%) of participants who had been quit for longer than a year still considered themselves to be much more likely or somewhat more likely than a smoker to get heart disease in the future. Participants’ perceived quality of life compared to when smoking increased over time since quitting, but 24% of participants still reported it as similar (22%) or reduced (2%) after a year or more of abstinence. Perceived benefits of continuing not to smoke did not change significantly over time, perhaps because there was already a high level of agreement with this belief at the start of the quit attempt (81% during the first week reported that they would benefit ‘very much’ or ‘extremely’).
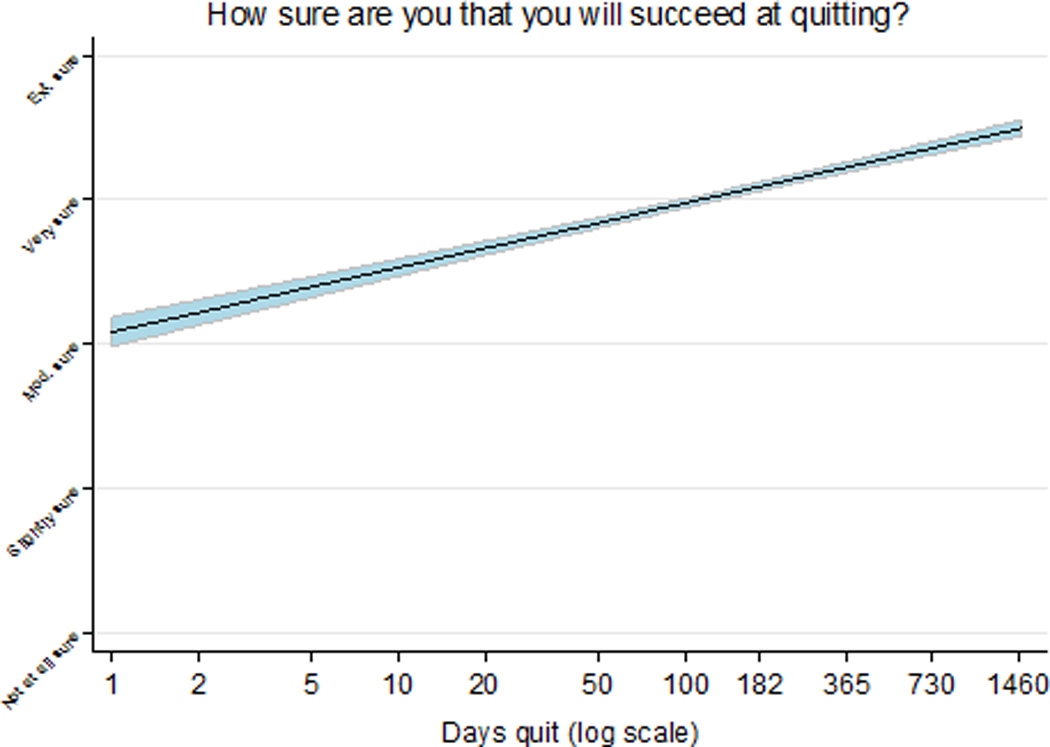
Abstinence self-efficacy
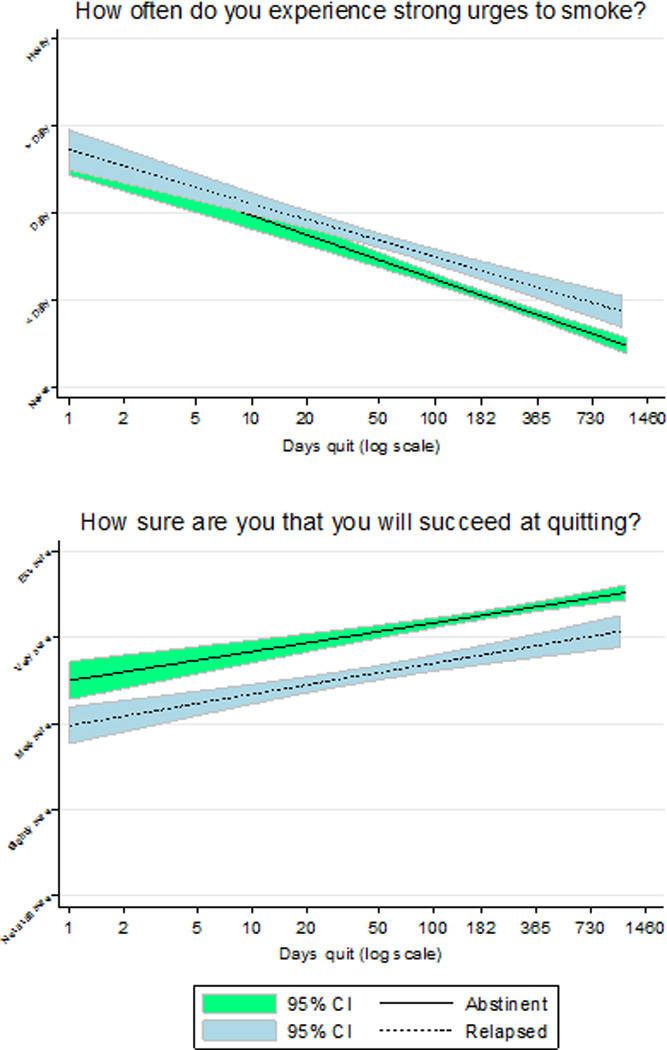
There was a significant log-quadratic trend in abstinence self-efficacy by duration of abstinence in the regression analysis; however, the GEE analysis suggested only the linear component was real (linear estimate = 0.42, 95% CI = 0.37 – 0.47, P<0.001; quadratic estimate = 0.04, 95% CI = −0.02 – 0.09, P=0.17). The smoothed log-linear regression line modelling the relationship between self-efficacy and duration of abstinence is presented in Figure 4.
Figure 4. Duration of abstinence by perceived abstinence self-efficacy: best fit linear regression line with 95% confidence intervals.
Cumulative relapse and change over time
It is possible that the observed trends might simply be a consequence of cumulative relapse over time, as it likely that the characteristics of the sample as a whole gradually changed as relapsers were dropped from the sample. Therefore, we explored separate regression lines for each dependent variable according to whether participants were abstinent or had relapsed at the subsequent wave of measurement. Although graphs for some dependent variables differed according to follow-up smoking status (e.g., frequency of urges to smoke, abstinence self-efficacy), on the whole, changes over time were not a consequence of cumulative relapse.
Discussion
Results showed that changes in smoking related beliefs and experiences asymptote quite quickly over time, but not all at the same rate. A log-function was the most common pattern of change; however, some beliefs asymptoted more slowly. The slowest or most prolonged change was for frequency of thoughts about the money spent on smoking, which changed according to a square-root function. In interpreting the results, it is important to understand the implications of the different time-related functions. For a log linear function, the amount of change in the first 10 days after quitting will be around one quarter of that which occurs in the next 10,000 days - around 27 years (assuming they stay quit), the next quarter takes around three months, the next 2.4 years and the last approximately 24 years. Square-root-linear models change considerably slower; only about 3% of the change in 27 years occurs during the first 10 days and another 7% during the next three months, giving only 10% in the first 100 days. A significant log-quadratic model accelerating over time in conjunction with a significant square-root-quadratic model decelerating over time (as was the case for frequency of thoughts about the enjoyment of smoking) is indicative of a function that is somewhere between the above two trends. The one noticeable difference between the GEE and regression results was for abstinence self-efficacy; it increased log-linearly according to the GEE model, but more slowly according to the regression model. This discrepancy may have been due to the exclusion of secondary quit attempts after relapse from the GEE analysis, but not the regression analysis. If so, this would suggest that for relapsers, self-efficacy increases more slowly (we explore this in the companion paper (35)).
The main limitation of the study is that we have limited longitudinal data that is restricted by gaps of around one year between surveys. To the extent that we have explored it, the trends reported did not markedly change when we removed cases that relapsed before the next assessment, suggesting that the trends cannot be attributed to differential dropout. The trends come from a broadly-based population sample, and we found no clear differences as a function of the demographic and smoking-related variables we studied. It is possible that changes in attitudes within individuals are more dramatic than gradual, and that the observed mean trends simply give the appearance of gradual change. It is hard to assess this given the long inter-survey interval. Furthermore, it is also possible that trends over time for some individuals do not map simply onto the lawful functions observed overall. However, in analyses not reported here, when we plotted the within-subjects graphs (i.e., changes within individuals) we found very similar patterns to those reported here. More work is required to establish the generality of these findings across other populations especially from countries with different cultures or where there is less social pressure to quit.
In line with previous research (10, 11), we found that decreases in smoking urges and increases in abstinence self-efficacy asymptote rapidly (logarithmic trajectory). Extrapolating from our findings, and assuming that the predictor variables are truly log-linear, frequency of urges to smoke would cease between 13 and 14 years post quitting and self-efficacy would reach its maximum somewhat later. It is putting too much weight on the accuracy of our estimates to treat these forecasts as strong predictions; rather they are indicative of the likely slow rates at which even the faster changing beliefs or experiences are likely to disappear (or reach trivial levels). The results also show that some beliefs are never likely to disappear, perhaps helping to explain why relapse can occur even after years of successful abstinence.
Four of the five perceived benefits of smoking measured decreased over time. Agreement with the belief that smoking calms you down when stressed decreased early on, but asymptoted soon after quitting (logarithmic trajectory) at quite a high level, showing that many ex-smokers continue to hold onto this belief long after quitting. Although smokers often cite stress relief as a reason for smoking (13, 36–38) and also use smoking to attempt to reduce stress (39, 40), research suggests that smoking is actually related to an increase in stress. (41–43). This inconsistency may exist because smoking appears to reduce stress in nicotine dependent smokers, and this is more salient than the longer-term increases in smoking induced stressed. The effectiveness of relapse reduction interventions might be enhanced by convincing ex-smokers that relief from nicotine withdrawal merely gives the impression of reduced stress.
The perception that smoking helps control weight was the only perceived benefit of smoking that became more positive with increasing duration of abstinence. It is likely that for at least some participants this belief was confirmed by the experience of weight gain, something that is frequently reported to be a consequence of quitting (44–49), but not assessed in the current study.
Frequency of thoughts about the costs of smoking decreased over time more slowly than most. This continuing decline is consistent with such thoughts becoming less relevant the longer the duration of smoking abstinence. In contrast, perceived benefits of quitting increased log-linearly. It is surprising that there was a rapid increase in these beliefs during a time when withdrawal is strongest. It is not clear whether the increase reflects a genuine change in perception or simply an attempt to boost motivation (i.e., wanting to believe it) in the context of the challenges being faced.
We are not clear about the significance of the different rates of change of these potential predictors of relapse, but one consequence is that their relative strengths will change over time, and this could affect either or both the probability of relapse or the conditions most likely to precipitate it. As a result, it is important to control for these patterns of change over time when exploring potential determinants of relapse (as we do in our companion paper (35)).
Our results document more precisely the fact that the days and weeks after quitting is a time of large-scale changes in experiences and beliefs and that the rate of change declines with time, sometimes quite rapidly. This confirms that the influence of time since quitting is relative to the beginning of the quit attempt, rather than constant. We should routinely be controlling for length of time quit in analyses of predictors of relapse, something that might be especially important in the early weeks of a quit attempt. The greater frequency of log-linear trends in the current study suggests that duration of abstinence expressed as a log function may be an optimal means by which to view time in smoking cessation research. However, it is also possible that the different rates of change influence the relationships between the variables and relapse. The next steps in analysing the processes that happen post-quitting is to determine to what extent the levels of, and changes in, factors we have studied actually predict cessation outcomes, and whether the thresholds predicting relapse vary systematically with time quit (35). According to the self-regulatory function of locomotion (50), motivation to stay quit might be impaired if the rate of change in smoking related attitudes and experiences falls below an expected rate of improvement. Research has shown that temporal comparisons that compare a present state to a past smoking state predict relapse (51); however, there has been no research exploring if the rate at which these comparisons form and change over time predicts relapse. Individual profiles of the natural history of quitting would need to be explored to determine if a slowing down of progress over time increases the likelihood of relapse.
Finally, given the increased stability of potential determinants of relapse with time, we think it that extending studies of predictors of relapse beyond the four years of this study is unlikely to provide additional insights into the quitting process, even though there is little doubt that some of those still quit at this point will eventually relapse.
Figure 5. Urges to smoke and perceived abstinence self-efficacy by duration of abstinence according to follow-up smoking status: best fit linear regression line with 95% confidence intervals.
Acknowledgements
We wish to thank Ann McNeill for her comments on an earlier draft of this paper. The first author was supported by an Australian Postgraduate Award. This research was funded by grants from the National Cancer Institute of the United States (R01 CA 100362), the Roswell Park Transdisciplinary Tobacco Use Research Center (P50 CA111236), Robert Wood Johnson Foundation (045734), Canadian Institutes of Health Research (57897 and 79551), National Health and Medical Research Council of Australia (265903 and 450110), Cancer Research UK (C312/A3726), and Canadian Tobacco Control Research Initiative (014578), with additional support from the Centre for Behavioural Research and Program Evaluation, National Cancer Institute of Canada/ Canadian Cancer Society.
Footnotes
Conflict of interest declaration: None
References
- 1.U.S. Department of Health and Human Services. The Health Benefits of Smoking Cessation. A Report of the Surgeon General. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1990. DHHS Publication No. (CDC) 90-8416. [Google Scholar]
- 2.Piasecki TM, Fiore MC, McCarthy DE, Baker TB. Have we lost our way? The need for dynamic formulations of smoking relapse proneness. Addiction. 2002;97:1093–1108. doi: 10.1046/j.1360-0443.2002.00216.x. [DOI] [PubMed] [Google Scholar]
- 3.Segan CJ, Borland R, Greenwood KM. Can transtheoretical model measures predict relapse from the action stage of change among ex-smokers who quit after calling a quitline? Addictive Behaviors. 2006;31:414–428. doi: 10.1016/j.addbeh.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 4.Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99:29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- 5.Marlatt GA, Curry S, Gordon JR. A longitudinal analysis of unaided smoking cessation. Journal of Consulting and Clinical Psychology. 1988;56:715–720. doi: 10.1037//0022-006x.56.5.715. [DOI] [PubMed] [Google Scholar]
- 6.Wetter DW, Cofta-Gunn L, Fouladi RT, Cinciripini PM, Sui D, Gritz ER. Late relapse/ sustained abstinence among former smokers: a longitudinal study. Preventive Medicine. 2004;39:1156–1163. doi: 10.1016/j.ypmed.2004.04.028. [DOI] [PubMed] [Google Scholar]
- 7.Brandon TH, Lazev AB, Juliano LM. Very delayed smoking relapse warrants research attention. Psychological Reports. 1998;83:72–74. doi: 10.2466/pr0.1998.83.1.72. [DOI] [PubMed] [Google Scholar]
- 8.Blondal T, Gudmundsson LJ, Olafsdottir I, Gustavsson G, Westin A. Nicotine nasal spray with nicotine patch for smoking cessation: randomised trial with six year follow up. British Medical Journal. 1999;318:285–289. doi: 10.1136/bmj.318.7179.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Borland R, Balmford J. Perspectives on relapse prevention: An exploratory study. Psychology and Health. 2005;20:661–671. [Google Scholar]
- 10.Shiffman S, Engberg JB, Paty JA, Perz WG, Gnys M, Kassel JD, et al. A day at a time: predicting smoking lapse from daily urge. Journal of Abnormal Psychology. 1997;106:104–116. doi: 10.1037//0021-843x.106.1.104. [DOI] [PubMed] [Google Scholar]
- 11.Gwaltney CJ, Shiffman S, Balabanis MH, Paty JA. Dynamic self-efficacy and outcome expectancies: prediction of smoking lapse and relapse. Journal of Abnormal Psychology. 2005;114:661–675. doi: 10.1037/0021-843X.114.4.661. [DOI] [PubMed] [Google Scholar]
- 12.Fong GT, Cummings KM, Borland R, Hastings G, Hyland A, Giovino GA, et al. The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tobacco Control. 2006;15:iii3–iii11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: within-subjects analysis of real-time reports. Journal of Consulting and Clinical Psychology. 1996;64:366–379. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- 14.Cummings KM, Jaen CR, Giovino G. Circumstances Surrounding Relapse in a Group of Recent Ex-smokers. Preventive Medicine. 1985;14:195–202. doi: 10.1016/0091-7435(85)90035-0. [DOI] [PubMed] [Google Scholar]
- 15.Norregaard J, Tonnesen P, Petersen L. Predictors and reasons for relapse in smoking cessation with nicotine and placebo patches. Preventive Medicine. 1993;22:261–271. doi: 10.1006/pmed.1993.1021. [DOI] [PubMed] [Google Scholar]
- 16.Marlatt GA, Gordon JR, editors. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviours. New York: Guilford Press; 1985. [Google Scholar]
- 17.Larimer ME, Palmer RS, Marlatt GA. Relapse prevention: an overview of Marlatt's cognitive-behavioural model. Alcohol Research and Health. 1999;23:151–160. [PMC free article] [PubMed] [Google Scholar]
- 18.Hughes JR. Tobacco withdrawal in self-quitters. Journal of Consulting and Clinical Psychology. 1992;60:689–697. doi: 10.1037//0022-006x.60.5.689. [DOI] [PubMed] [Google Scholar]
- 19.Brandon TH, Wetter DW, Baker TB. Affect, expectancies, urges, and smoking: do they conform to models of drug motivation and relapse? Experimental and Clinical Psychopharmacology. 1996;4:29–36. [Google Scholar]
- 20.Beck AT, Wright FD, Newman CF, Liese BS. Cognitive Therapy of Substance Abuse. New York: The Guilford Press; 1993. [PubMed] [Google Scholar]
- 21.Bandura A. Social cognitive theory: An agentic perspective. Annual Review of Psychology. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 22.Dijkstra A, Borland R. Residual outcome expectations and relapse in ex-smokers. Health Psychology. 2003;22:340–346. doi: 10.1037/0278-6133.22.4.340. [DOI] [PubMed] [Google Scholar]
- 23.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 24.Condiotte MM, Lichtenstein E. Self-efficacy and relapse in smoking cessation programs. Journal of Consulting and Clinical Psychology. 1981;49:648–658. doi: 10.1037//0022-006x.49.5.648. [DOI] [PubMed] [Google Scholar]
- 25.Stuart K, Borland R, McMurray N. Self-efficacy, health locus of control, and smoking cessation. Addictive Behaviours. 1994;19:1–12. doi: 10.1016/0306-4603(94)90046-9. [DOI] [PubMed] [Google Scholar]
- 26.Shiffman S, Balabanis MH, Paty JA, Engberg J, Gwaltney CJ, Liu KS, et al. Dynamic effects of self-efficacy on smoking lapse and relapse. Health Psychology. 2000;19:315–323. doi: 10.1037//0278-6133.19.4.315. [DOI] [PubMed] [Google Scholar]
- 27.Thompson ME, Fong GT, Hammond D, Boudreau C, Driezen P, Hyland A, et al. Methods of the International Tobacco Control (ITC) Four Country Survey. Tobacco Control. 2006;15:12–18. doi: 10.1136/tc.2005.013870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hyland A, Borland R, Li Q, Yong H-H, McNeill A, Fong GT, et al. Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tobacco Control. 2006;15(Suppl III):iii83–iii94. doi: 10.1136/tc.2005.013516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huijding J, Jong PJd, Wiers WR, Verkooijen K. Implicit and explicit attitudes toward smoking in a smoking and a nonsmoking setting. Addictive Behaviors. 2005;30:949–961. doi: 10.1016/j.addbeh.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 30.Litz BT, Payne TJ, Colletti G. Schematic processing of smoking information by smokers and never-smokers. Cognitive Therapy and Research. 1987;11:301–313. [Google Scholar]
- 31.Leung KS, McCusker CG. Accessibility and availability of smoking-related associations in smokers. Addiction Research. 1999;7:213–226. [Google Scholar]
- 32.Fazio RH, Williams CJ. Attitude accessibility as a moderator of the attitude-perception and attitude-behavior relations: an investigation of the 1984 presidential election. Journal of Personality and Social Psychology. 1986;51:505–514. doi: 10.1037//0022-3514.51.3.505. [DOI] [PubMed] [Google Scholar]
- 33.Howell DC. Statistical methods of psychology. Belmont, CA: Wadsworth Publishing Company; 1997. [Google Scholar]
- 34.Liang K, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 35.Herd N, Borland R, Hyland A. Predictors of relapse by duration of abstinence: findings from the International Tobacco Control (ITC) Four Country Survey. Addiction. doi: 10.1111/j.1360-0443.2009.02732.x. Submitted; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baer JS, Lichtenstein E. Classification and prediction of smoking relapse episodes: an exploration of individual differences. Journal of Consulting and Clinical Psychology. 1988;56:104–110. doi: 10.1037//0022-006x.56.1.104. [DOI] [PubMed] [Google Scholar]
- 37.Shiffman S. Relapse following smoking cessation: a situational analysis. Journal of Consulting and Clinical Psychology. 1982;50:71–86. doi: 10.1037//0022-006x.50.1.71. [DOI] [PubMed] [Google Scholar]
- 38.Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychological Bulletin. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- 39.Rose JE, Ananda S, Jarvik ME. Cigarette smoking during anxiety-provoking and monotonous tasks. Addictive Behaviours. 1983;8:353–359. doi: 10.1016/0306-4603(83)90035-7. [DOI] [PubMed] [Google Scholar]
- 40.Pomerleau OF, Pomerleau CS. A biobehavioral view of substance abuse and addiction. Journal of Drug Issues. 1987;17:111–131. [Google Scholar]
- 41.Jones MEE, Parrott AC. Stress and arousal circadian rhythms in smokers and non-smokers working day and night shifts. Stress Medicine. 1997;13:91–97. [Google Scholar]
- 42.Vollrath M. Smoking, coping and health behavior among university students. Psychology and health. 1998;13:431–441. [Google Scholar]
- 43.Cohen S, Lichtenstein E. Perceived stress, quitting smoking, and smoking relapse. Health Psychology. 1990;9:466–478. doi: 10.1037//0278-6133.9.4.466. [DOI] [PubMed] [Google Scholar]
- 44.Filozof C, Pinilla MCF, Fernandez-Cruz A. Smoking cessation and weight gain. Obesity Review. 2004;5:95–103. doi: 10.1111/j.1467-789X.2004.00131.x. [DOI] [PubMed] [Google Scholar]
- 45.Klesges RC, Winders SE, Meyers AW, Eck LH, Ward KD, Hultquist CM, et al. How much weight gain occurs following smoking cessation? A comparison of weight gain using both continuous and point prevalence abstinence. Journal of Consulting and Clinical Psychology. 1997;65:286–291. doi: 10.1037//0022-006x.65.2.286. [DOI] [PubMed] [Google Scholar]
- 46.Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. The New England Journal of Medicine. 1991;324:739–745. doi: 10.1056/NEJM199103143241106. [DOI] [PubMed] [Google Scholar]
- 47.Swan GE, Carmelli D. Characteristics associated with excessive weight gain after smoking cessation in men. American Journal of Public Health. 1995;85:73–77. doi: 10.2105/ajph.85.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Borrelli B, Mermelstein R. The role of weight concern and self-efficacy in smoking cessation and weight gain among smokers in a clinic-based cessation program. Addictive Behaviors. 1998;23:609–622. doi: 10.1016/s0306-4603(98)00014-8. [DOI] [PubMed] [Google Scholar]
- 49.Pisinger C, Jorgensen T. Waist circumference and weight following smoking cessation in a general population: The Inter99 study. Preventive Medicine. 2007;44:290–295. doi: 10.1016/j.ypmed.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 50.Kruglanski AW, Higgins ET, Pierro A, Thompson EP, Atash MN, Shah JY. To "do the right thing" or to "just do it": locomotion and assessment as distinct self-regulatory imperatives. Journal of Personality and Social Psychology. 2000;79:793–815. doi: 10.1037//0022-3514.79.5.793. [DOI] [PubMed] [Google Scholar]
- 51.Dijkstra A, Borland R, Buunk BP. The motivation to stay abstinent in ex-smokers: Comparing the present with the past. Addictive Behaviors. 2007 doi: 10.1016/j.addbeh.2007.02.007. [DOI] [PubMed] [Google Scholar]


