Abstract
Objective
Pericardial adipose tissue (PAT) is associated with adverse cardiometabolic risk factors and cardiovascular disease (CVD). However, the relative implications of PAT, abdominal visceral and subcutaneous adipose tissue on vascular inflammation have not been explored.
Method and Results
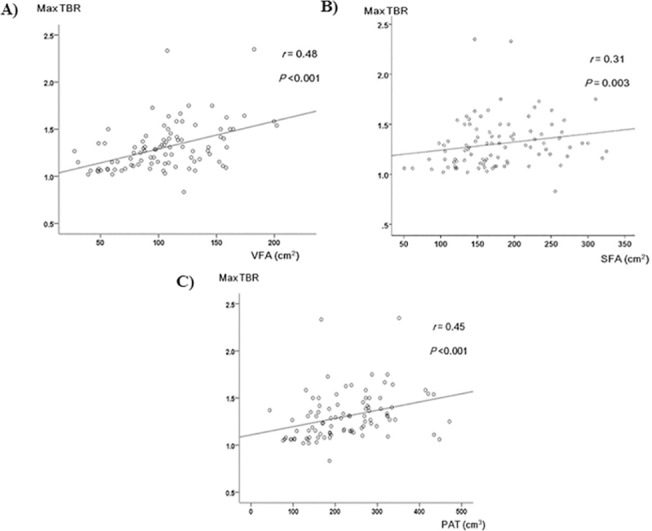
We compared the association of PAT, abdominal visceral fat area (VFA), and subcutaneous fat area (SFA) with vascular inflammation, represented as the target-to-background ratio (TBR), the blood-normalized standardized uptake value measured using 18F-Fluorodeoxyglucose Positron Emission Tomography (18FDG-PET) in 93 men and women without diabetes or CVD. Age- and sex-adjusted correlation analysis showed that PAT, VFA, and SFA were positively associated with most cardiometabolic risk factors, including systolic blood pressure, LDL-cholesterol, triglycerides, glucose, insulin resistance and high sensitive C-reactive proteins (hsCRP), whereas they were negatively associated with HDL-cholesterol. In particular, the maximum TBR (maxTBR) values were positively correlated with PAT and VFA (r = 0.48 and r = 0.45, respectively; both P <0.001), whereas SFA showed a relatively weak positive relationship with maxTBR level (r = 0.31, P = 0.003).
Conclusion
This study demonstrated that both PAT and VFA are significantly and similarly associated with vascular inflammation and various cardiometabolic risk profiles.
Introduction
Obesity is closely related to glucose and lipid metabolism, and is a well-established risk factor for atherosclerosis and cardiovascular disease (CVD) [1]. Adipose depots in different locations may confer different metabolic risk and cardio-metabolic burdens for the development of CVD. For example, abdominal visceral adipose tissue (VAT) is more closely associated with metabolic syndrome and cardiovascular mortality than subcutaneous adipose tissue (SAT) [2]. Even more, several studies suggest that SAT may serve as a buffer that protects other tissues from ectopic lipotoxic effects [3].
The heart has its own visceral fat depots between the myocardium and the visceral pericardium [epicardial adipose tissue (EAT)] and around the paracardial area (paracardial adipose tissue) [4]. Recently, pericardial adipose tissue (PAT) [EAT plus paracardial adipose tissue] has been recognized as a novel risk factor for coronary artery disease (CAD). In the Framingham Heart Study, Rosito et al. [5] found that pericardial fat was associated with coronary artery calcification (CAC) after multivariable analysis and visceral fat area (VFA) adjustment. In the Multi-ethnic Study of Atherosclerosis (MESA), PAT was associated with increased carotid stiffness, independent of traditional CVD risk factors and obesity [6]. Miao et al. [7] reported that PAT correlated significantly with the degree of coronary artery eccentricity an index of plaque burden, as measured using magnetic resonance (MR) imaging in 183 participants from the MESA study. Furthermore, Greif et al. [8] also reported that increased PAT is associated with coronary atherosclerosis, hypoadiponectinemia, and systemic inflammatory markers. Patients who had only non-calcified plaques had significantly increased PAT, indicating that PAT quantification may be useful to identify patients with CAD, even in the absence of coronary calcification.
Chronic low-grade inflammation is associated with chronic metabolic disorders, and atherosclerosis is now recognized as an inflammatory disorder [9]. Vascular culprit lesions for acute coronary syndrome or myocardial infarction are associated with a high degree of plaque inflammation [10]. Positron Emission Tomography with 18F-Fluorodeoxyglucose (18FDG-PET) is a novel imaging technique to identify vascular inflammation, and indicates macrophage infiltration in vasculature [11]. In our previous studies, 18FDG-PET revealed that patients with impaired glucose metabolism or elevated high sensitive C-reactive protein (hsCRP) had significantly higher maximum target-to-background ratio (TBR) values, which indicates vascular inflammation, than their control groups [12, 13]. In contrast, TBR values showed a negative relationship with serum adiponectin, which is an anti-inflammatory and anti-atherogenic adipokine [14].
PAT/EAT affect the cardiovascular system by secreting pro- and anti-inflammatory adipokines in paracrine or vasocrine manners [4]. The role of PAT in the development of CAD may be due to its close anatomical proximity to the myocardium and vasculature [15]. PAT/EAT may have different metabolic features from other visceral fat depots, especially with respect to adipocyte size and free fatty acid metabolism [16]. However, no previous studies have explored the association of PAT or VFA with vascular inflammation, which may reflect plaque vulnerability. Moreover, few studies investigate the importance of PAT as a cardiovascular risk factor compared to other adipose tissue depots, such as the abdominal VFA or the subcutaneous fat area (SFA).
In the present study, we compared vascular inflammation measured by 18FDG-PET/CT between PAT, VFA, and SFA and investigated their relationships with conventional and novel cardiometabolic risk parameters in individuals without a history of CAD or diabetes.
Materials and Methods
Study design and participants
We recruited patients who were self-referred for a routine health check-up at the Health Promotion Center of Korea, University Guro Hospital, between June 2008 and March 2009. Subjects were excluded from this study if they met any of the following criteria: history of CVD (myocardial infarction, unstable angina, stroke, or cardiovascular revascularization); diabetes; stage 2 hypertension (resting blood pressure ≥160/100 mmHg); any lipid-lowering therapies or postmenopausal hormone replacement therapy during the 6-month period before enrollment; history of inflammatory conditions such as aortitis and vasculitis; any medications that might affect inflammatory status, including steroid and non-steroidal anti-inflammatory drug within 6 months of the study; malignant disease; or severe renal or hepatic disease. After excluding ineligible subjects, we analyzed on 93 participants (53 men and 40 women). All participants provided written informed consent, and the Korea University Institutional Review Board approved this study protocol, in accordance with the Declaration of Helsinki of the World Medical Association.
Anthropometric and laboratory measurements
Body mass index (BMI) was calculated as the weight/height2 (kg/m2), and waist circumference was measured at the midpoint between the lower border of the rib cage and the iliac crest. All blood samples were obtained in the morning after a 12-hour overnight fast and were immediately stored at –80°C. Serum triglycerides and high-density lipoprotein cholesterol (HDL-C) were measured enzymatically using a chemistry analyzer (Hitachi 747; Hitachi Inc.). The low-density lipoprotein cholesterol (LDL-C) concentration was estimated using the Friedewald formula [17]. A glucose oxidase method was used to measure plasma glucose. hsCRP levels were measured by Latex-enhanced Turbidimetric Immunoassay (HiSens hsCRP LTIA; HBI Co., Ltd.), with an interassay coefficient of variation of 7.2%.
18F-FDG PET/CT
PET/CT was performed using the Gemini TF 16-slice PET/CT scanner (Philips). The TF scanner is a new high-performance, time-of-flight–capable, fully 3-dimensional PET scanner using lutetium yttrium oxyorthosilicate crystals [18]. After the patients had fasted for at least 12-hours, 18F-FDG (5.19 MBq/kg) was injected intravenously, and patients rested in a quiet room for 60 minutes. Whole-body PET images (from below the cerebellum to the inguinal region) were acquired for 10 minutes (1 minute per bed position) and the resulting images were analyzed on a dedicated workstation (Extended Brilliance Workspace 3.5 with PET/CT viewer for automated image registration; Philips). The right carotid 18F-FDG uptake was measured along the length of the right carotid vessel, starting at the bifurcation and extending inferiorly and superiorly every 4 mm, for a total 10 consecutive PET/CT images for each subject. Arterial 18F-FDG uptake was quantified by a region of interest (ROI) around each artery on every slice of the coregistered transaxial PET/CT images. The ROI was fitted to the artery wall on each axial slice, and coronal and sagittal views were used to ensure that the 18F-FDG uptake was from the artery. The standardized uptake value (SUV) is the decay-corrected tissue concentration of 18F-FDG (in kBq/mL) divided by the injected dose per body weight (kBq/g). On each image slice, the mean and maximum SUVs of the ROI were measured as the mean and maximum pixel activity. The SUVs for all 10 slices within the right carotid artery were averaged to calculate the mean and maximum SUVs for each participant. Next, the arterial SUV was divided by the blood-pool SUV measured from the jugular vein for normalization; thereby, a mean and maximum TBR value was acquired for each subject by an experienced radiologist in the Department of Nuclear Medicine (S.K.) [19].
Measurement of PAT, VFA, and SFA
The VFA, SFA and PAT volumes were measured on non-contrast enhanced CT scans using volume analysis software of the workstation (Extended Brilliance Workspace 3.5, with PET/CT viewer; Philips). The vertical PAT ranged from the bifurcation of the pulmonary artery superiorly, to the cardiac apex over the diaphragm inferiorly. The anterior border was defined by the posterior aspect of sternum and the posterior border was defined by the esophagus and the descending aorta. The ROI containing the heart and the surrounding adipose tissue was assessed by manually tracing axial slices. PAT images ranged from –190 to –30 Hounsfield units (HU) to isolate the adipose tissue containing voxels. The adipose tissue voxels were then summed to obtain PAT volume. The VFA and total abdominal fat area were calculated using the CT slice scan image at the umbilicus level. VFA was quantified by manual tracing of the intra-abdominal cavity from the internal aspect of the abdominal and oblique muscle walls and the posterior aspect of the vertebral body. The subcutaneous fat area was calculated by subtracting the VFA from the total abdominal fat area. A threshold of –190 to –30 HU was also applied to isolate fat-containing voxels.
Statistical analyses
Data are expressed as mean ± standard deviation, median and interquartile range (25%-75%), or percentage. Differences between groups were tested using the Student’s t-test or the Mann-Whitney U-test, and the χ2-test was used to test for differences in the distribution of categorical variables. Each variable was examined for normal distribution by using the Shapiro-Wilk normality test. An age and sex-adjusted Spearman partial correlation analysis of VFA, SFA and PAT with other metabolic variables was conducted. We further divided the study subjects into 3 groups according to the tertile of maximum TBR (maxTBR). We then compared the cardio-metabolic risk parameters of these 3 groups to estimate the significance of any statistical associations between tertiles of maxTBR by using the analysis of variance (ANOVA) or the Kruskal-Wallis test and the χ2-test as appropriate. For multiple comparisons, we used the Tukey-Kramer test for variables with normal distribution and the Mann-Whitney test for those without normal distribution, respectively. Also, we adjusted the P-values of the Mann-Whitney U-test by using the Bonferoni correction in multiple comparisons. After adjusting for age and sex, we compared the cardio-metabolic risk parameters by using the analysis of covariance (ANCOVA) for variables with normal distribution. For non-normal continuous variables, ANCOVA was conducted after log-transformation. And, a logistic regression analysis was used for categorical variables. A P-value <0.05 was considered statistically significant in all analyses. All statistical results were based on two-sided tests. Data were analyzed using SAS for Windows (version 9.20, SAS Institute Inc., Cary, NC, USA).
Results
Characteristics of study participants
The characteristics of all study subjects are presented in Table 1. The mean age of men and women was 48.8 ± 8.9 years and 53.2 ± 9.9 years, respectively. PAT was slightly larger in men than in women (238.4 [171.2, 287.0] cm3 vs. 186.0 [144.4, 267.4] cm3, P = 0.022). In addition, VFA was larger in men than in women (113.9 ± 39.1 cm2 vs. 93.3 ± 33.4 cm2, P = 0.009), whereas SFA was greater in women than in men (157.7 ± 49.4 cm2 vs. 205.5 ± 61.3 cm2, P <0.001). On the other hand, hsCRP and HOMA-IR of study subjects were not significantly different between men and women.
Table 1. Clinical Characteristics of Study Participants.
| Male (n = 53) | Female (n = 40) | P | |
|---|---|---|---|
| Age (years) | 48.8 ± 8.9 | 53.2 ± 9.9 | 0.026 |
| BMI (kg/m2) | 24.8 ± 2.9 | 23.3 ± 3.0 | 0.017 |
| Waist circumference (cm) | 87.4 ± 6.3 | 79.2 ± 7.6 | <0.001 |
| SBP (mmHg) | 125.0 (118.5, 131.0) | 122.0 (113.5, 136.5) | 0.456 |
| DBP (mmHg) | 85.1 ± 10.4 | 80.2 ± 11.5 | 0.036 |
| Triglyceride (mmol/L) | 1.4 (0.9, 2.2) | 0.9 (0.6, 1.6) | 0.006 |
| HDL-C (mmol/L) | 1.2 (1.1, 1.5) | 1.2 (1.0, 1.4) | 0.576 |
| LDL-C (mmol/L) | 3.5 ± 0.9 | 3.1 ± 1.2 | 0.103 |
| Glucose (mmol/L) | 5.3 ± 0.7 | 4.6 ± 1.0 | 0.001 |
| hsCRP (mg/L) | 2.2 (0.5, 3.5) | 0.8 (0.4, 2.9) | 0.141 |
| HOMA-IR | 0.7 (0.3, 1.2) | 0.5 (0.3, 0.9) | 0.167 |
| Current smoker | 24 (45.3) | 3 (7.5) | <0.001 |
| Maximum TBR | 1.3 (1.2, 1.5) | 1.2 (1.1, 1.4) | 0.037 |
| VFA (cm2) | 113.9 ± 39.1 | 93.3 ± 33.4 | 0.009 |
| SFA (cm2) | 157.7 ± 49.4 | 205.5 ± 61.3 | <0.001 |
| PAT (cm3) | 238.4 (171.2, 287.0) | 186.0 (144.4, 267.4) | 0.022 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; hsCRP, high sensitivity C-reactive protein; HOMA-IR, homeostasis model assessment insulin resistance; TBR, target-to-background ratio; VFA, (abdominal) visceral fat area; SFA, (abdominal) subcutaneous fat area; PAT, pericardial adipose tissue.
Data with a normal distribution are shown as “mean ± SD”, and those without a normal distribution are shown as “median (interquartile range)”.
Only current smoker is expressed in N (%).
Correlation of VFA, SFA and PAT with cardiometabolic risk factors
Table 2 shows the correlation analysis of VFA, SFA and PAT with other major metabolic variables. After adjusting for age and sex, VFA, SFA, and PAT were positively correlated with most cardiometabolic risk factors, including obesity parameters, hypertension, dyslipidemia, hyperglycemia, HOMA-IR, and hsCRP. On the other hand, HDL-C was negatively correlated with all adipose depots. PAT showed a significant relationship with both VFA (r = 0.69, P <0.001) and SFA (r = 0.56, P <0.001). In particular, the maxTBR value was strongly and positively correlated with VFA and PAT (r = 0.48 and 0.45, respectively; both P <0.001), but SFA showed a relatively weak relationship with maxTBR levels (r = 0.31, P = 0.003) (Table 2, Fig 1), despite its close relationships with VFA (r = 0.52, P <0.001) and PAT.
Table 2. Spearman Partial Correlation Analysis of Abdominal Visceral Fat Area (VFA), Abdominal Subcutaneous Fat Area (SFA), and Pericardial Adipose Tissue Volume (PAT) With Cardiometabolic Parameters, after Adjusting for Age and Sex.
| VFA | SFA | PAT | ||||
|---|---|---|---|---|---|---|
| r | P | r | P | r | P | |
| BMI | 0.58 | <0.001 | 0.74 | <0.001 | 0.60 | <0.001 |
| Waist circumference | 0.67 | <0.001 | 0.67 | <0.001 | 0.62 | <0.001 |
| SBP | 0.25 | 0.017 | 0.22 | 0.038 | 0.28 | 0.008 |
| DBP | 0.31 | 0.003 | 0.16 | 0.124 | 0.18 | 0.091 |
| LDL-C | 0.37 | <0.001 | 0.34 | 0.001 | 0.29 | 0.006 |
| HDL-C | −0.35 | 0.001 | −0.25 | 0.019 | −0.35 | 0.001 |
| Triglyceride | 0.45 | <0.001 | 0.38 | <0.001 | 0.52 | <0.001 |
| Glucose | 0.39 | <0.001 | 0.35 | 0.001 | 0.31 | 0.003 |
| hsCRP | 0.45 | <0.001 | 0.33 | 0.001 | 0.35 | 0.001 |
| HOMA-IR | 0.53 | <0.001 | 0.50 | <0.001 | 0.41 | <0.001 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; hsCRP, high sensitivity C-reactive protein; HOMA-IR, homeostasis model assessment insulin resistance; TBR, target-to-background ratio.
Fig 1. Scatterplot of maximum TBR values with A) abdominal visceral fat area (VFA), B) abdominal subcutaneous fat area (SFA), and C) pericardial adipose tissue volume (PAT).
Cardiovascular risk factors stratified by tertile of maximum TBR value
BMI, waist circumference, SBP, DBP, triglyceride, LDL-C, hsCRP, HOMA-IR and maxTBR values were increased with maxTBR tertiles. And, these trends did not change even after adjusting for age and sex (Table 3). Interestingly, VFA, SFA and PAT showed a stepwise increase with increasing maxTBR tertiles (P <0.001, P = 0.001 and P <0.001, respectively).
Table 3. Anthropometric, Metabolic and Cardiovascular Risk Parameters of Study Subjects by Tertiles of Maximum Target-to-Background Ratio (maxTBR) value.
| MaxTBR T1 (0.83–1.15) | MaxTBR T2 (1.16–1.35) | MaxTBR T3 (1.36–2.35) | P | P’ | |
|---|---|---|---|---|---|
| Sex, male (%) | 16 (50.0) | 16 (53.3) | 21 (67.7) | 0.322 | |
| Age (years) | 50.8 ± 8.6 | 49.0 ± 10.0 | 52.1 ± 10.2 | 0.461 | |
| BMI (kg/m2) | 22.3 (19.2, 24.2)a | 25.0 (23.7, 26.8)b | 25.4 (23.7, 26.9)b | <0.001 | <0.001 |
| Waist circumference (cm) | 79.1 ± 8.0a | 85.2 ± 7.0b | 87.5 ± 6.5b | <0.001 | <0.001 |
| SBP (mmHg) | 120.0 (111.0, 125.0)a | 126.0 (118.0, 133.0)ab | 127.0 (118.0, 143.0)b | 0.018 | 0.005 |
| DBP (mmHg) | 78.4 ± 8.8a | 82.6 ± 10.5ab | 87.8 ± 11.9b | 0.003 | 0.009 |
| Triglycerides (mmol/L) | 0.8 (0.6, 1.0)a | 1.6 (1.0, 2.3)b | 1.4 (1.2, 2.2)b | <0.001 | <0.001 |
| HDL-C (mmol/L) | 1.3 ± 0.4 | 1.2 ± 0.3 | 1.2 ± 0.3 | 0.516 | 0.489 |
| LDL-C (mmol/L) | 2.6 (2.0, 3.8)a | 2.9 (2.4, 4.3)ab | 3.8 (3.4, 4.3)b | <0.001 | <0.001 |
| Glucose (mmol/L) | 4.5 ± 0.9a | 5.0 ± 0.8b | 5.5 ± 0.7b | <0.001 | <0.001 |
| hsCRP (mg/L) | 0.4 (0.2, 0.8)a | 1.5 (0.5, 3.1)b | 3.2 (2.6, 4.8)c | <0.001 | <0.001 |
| HOMA-IR | 0.3 (0.2, 0.7)a | 0.8 (0.5, 1.2)b | 1.0 (0.5, 1.6)b | <0.001 | <0.001 |
| Current smoker (%) | 10 (31.2) | 8 (26.7) | 9 (29.0) | 0.924 | 0.688 |
| VFA (cm2) | 84.8 ± 35.9a | 101.7 ± 30.0a | 129.2 ± 34.2b | <0.001 | <0.001 |
| SFA (cm2) | 146.4 ± 48.4a | 197.0 ± 67.2b | 193.0 ± 49.0b | 0.001 | <0.001 |
| PAT (cm3) | 157.4 (116.3, 205.1)a | 233.6 (171.2, 285.1)b | 272.6 (185.5, 317.5)b | <0.001 | <0.001 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; hsCRP, high sensitivity C-reactive protein; HOMA-IR, homeostasis model assessment insulin resistance; VFA, (abdominal) visceral fat area; SFA, (abdominal) subcutaneous fat area; PAT, pericardial adipose tissue.
Data are mean ± SD, median (interquartile range), or N (%).
Means or medians with the different letter are significantly different.
The variables expressed as medians (interquartile range) were assessed by the the Mann-Withney test in multiple comparisons, and the P-values were adjusted by the Bonferoni correction (P <0.017 was considered statistically significant).
P’ values were calculated after adjusting for age and sex by using the analysis of covariance (ANCOVA) for continuous variables and a logistic regression analysis for categorical variables.
Discussion
The terminology distinguishing different fat depots around heart is somewhat confusing [3]. In general, EAT has been defined as the intra-epicardial fat depot between the myocardium and the visceral pericardium. PAT, also known as extra-pericardial adipose tissue, has been defined to include both EAT and the fat depot outside the visceral pericardium [20]. Post mortem studies have shown that EAT covers 80% of the heart’s surface and constitutes up to 20% of the total ventricular weight of the human heart [21]. Greif et al. [8] reported an excellent correlation between EAT and PAT (r = 0.97), although PAT had better reproducibility (interobserver variability 8%) than EAT (15%). PAT/EAT can generate various bioactive molecules that may affect cardiovascular health [3]. Previous studies have shown the association between PAT/EAT and early-stage atherosclerosis and plaque formation. The accumulation of pericardial fat is associated with impairment in left ventricular function, independent of other factors such as hypertension or diabetes [22]. In a study using multi-detector computed tomography (MDCT), increased pericardial fat volume was an independent risk factor for coronary artery stenosis, even after adjusting for confounding factors [23]. Moreover, Schlett et al. [24] found that patients with high-risk coronary lesions have nearly twice the PAT as those without CAD, independent of clinical characteristics and general obesity. In a nested case-control study including asymptomatic patients without CAD, individuals experiencing major adverse cardiovascular events (MACE) had a significantly higher pericardial fat burden compared with event-free control subjects even with similar cardiovascular risk profiles [25]. Based on their 5.4-year cohort study in 145 patients with stable CAD, Greif et al. [15] suggested that PAT measurement increases the predictive power of CAC for the development of cardiovascular events. In the present study, we first showed the significant implications of PAT and VFA with FDG uptake values measured using 18FDG-PET/CT, which indicates macrophage infiltration within carotid vasculature.
Several pathogenic mechanisms that may mediate the relationship between PAT and atherosclerosis have been suggested. In individuals without CAD or diabetes, PAT was associated with insulin resistance, independent of BMI and waist circumference [26]. This is in agreement with our observation that both PAT and VFA were significantly associated with insulin resistance. Additionally, both PAT and VFA showed close relationships with several components of metabolic syndrome, such as hypertension, hyperglycemia and dyslipidemia, which is consistent with previous studies [3, 8]. Pericardial fat, which has greater lipolytic activity than subcutaneous fat, releases excessive free fatty acids to promote atherosclerosis. Furthermore, recent studies support visceral adipose tissue in obesity as an important source of inflammation, which is characterized by increased infiltration of macrophages, lymphocytes, and mast cells [27]. Pericardial fat produces more pro-inflammatory adipokines, such as tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and monocyte chemotactic protein-1 (MCP-1), than subcutaneous fat [28]. Konishi et al. [29] examined the association between CAD and inflammation in pericardial fat measured by immunohistochemical stain in 39 autopsy cases. They found that pericardial fat inflammation was significantly associated with the presence of CAD, independent of risk factors such as hypertension, dyslipidemia, and diabetes. Vela et al. [30] have shown that macrophage infiltration in the peri-adventitial fat of rupture-prone vulnerable lipid-rich plaques is higher than in fibrocalcific plaques. In the Framingham Offspring Study, multiple markers of inflammation, such as CRP, IL-6, and oxidative stress, were correlated with PAT [31]. Mazurek et al. [32, 33] reported that inflammation of PAT increases the risk of plaque instability in the patients with acute coronary syndrome (ACS), and has a close relationship with the occurrence of atrial fibrillation. These studies indicate that inflammation of PAT is associated with cardiac electrical disturbance as well as coronary atherosclerosis. Moreover, Mazzoccoli et al. [34, 35] also reported that EAT might have a relationship with venous thromboembolism beyond arterial atherosclerosis. In this study, we confirmed the association between PAT and hsCRP, a systemic subclinical inflammatory marker. Subclinical inflammation has been established as a pivotal underlying pathogenic mechanism in the initiation, progression and rupture of atherosclerotic plaques. In contrast, adiponectin, an anti-inflammatory and anti-atherogenic adipokine, decreases with increased PAT [8]. Considering the close relationship between hsCRP, adiponectin and FDG uptake as measured by FDG-PET/CT in our previous and present results, local and systemic inflammation may link PAT with cardiovascular disorders associated with obesity [13, 14]. Lately, Alexopoulos et al. [36] reported that statin administration induced regression of EAT in hyperlipidemic post-menopausal women, and found that intensive therapy was more effective than moderate-intensity therapy. They concluded that this effect is not linked to LDL lowering and may be secondary to pleiotropic actions of statins, such as anti-inflammatory effects.
In this study, we also compared the association of vascular inflammation and traditional and novel cardiometabolic risk factors with PAT compared to other adiposity measures such as VFA and SFA. Interestingly, the magnitude of the association between PAT, vascular inflammation, and various cardiometabolic risk parameters was similar to VFA, whereas SFA had a relatively weak relationship with vascular inflammation. Considering the data showing that women have a higher SFA than men, these results might reveal an important underlying mechanism that mediates the relatively better cardiovascular outcomes in women. Our data are consistent with previous results indicating that PAT is correlated with echocardiographic measures of cardiac abnormalities, but the association is not stronger than that of other obesity indices such as waist circumference [37]. Fox et al. [38] also reported that pericardial fat is correlated with cardiovascular magnetic resonance measures, but the association was not independent or stronger than measures of visceral obesity. Moreover, Cheng et al. [39] showed that tissue levels of TNF-α, IL-6, leptin and visfatin from abdominal fat depots were significantly higher compared to those from epicardial fat in patients with CAD. Therefore, they concluded that abdominal adiposity may play a more significant role in the pathogenesis of coronary atherosclerosis than epicardial fat [39]. However, Konish et al. [40] demonstrated that pericardial fat accumulation, but not waist circumference, was significantly associated with the presence of any coronary plaques detected by coronary angiography. The exact reason for this discrepancy is not clear, our study used abdominal CT for the measurement of visceral fat, which is more accurate. Interestingly, despite the previous suggestion of protective role of SAT in cardiometabolic disorders [41, 42], the present study demonstrated that SAT had a positive association with vascular inflammation and cardiometabolic risk parameters. However, these relationships were relatively weak compared to those of PAT or VFA.
Mahabadi et al. [43] suggested that PAT is predominantly associated with coronary heart disease (CHD), whereas VFA is associated with stroke. Carotid plaque inflammation measured using 18FDG-PET has been reported to be related with the risk of stroke and cerebral micro-embolism [44, 45]. The present study using 18FDG-PET/CT examined FDG uptake that reflects vascular inflammation in carotid vasculature. Further research might be needed to explore the relative impact of PAT on regional atherosclerosis and CVD compared to other fat depots such as VAT or SAT.
Some limitations of this study need to be considered. First, the cross-sectional nature of this study did not allow us to identify causal relationships. Second, our study was comprised of Asian men and women without a history of CAD and diabetes, which limits our ability to generalize our study results to other populations with different ethnicities and characteristics.
In conclusion, the present study clearly showed that both PAT and VFA had significant associations with maxTBR values, which indicate vascular inflammation, and with other cardiometabolic risk factors as well. In addition, the magnitude of the relationship with vascular inflammation, along with the unfavorable CV risk factor profile, was similar between PAT and VFA in Korean men and women without CAD or diabetes.
Data Availability
Korean Personal Information Protection Law prohibits providing personal data to 3rd party personnel without permission. IRB in Korea University Guro Hospital recommended that the data upon request might be provided only after specific permission of IRB. Contact information to which requests for the data: medica7@gmail.com.
Funding Statement
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea. (HI14C0133) (KMC). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Ouchi N, Parker JL, Lugus JJ, Walsh K. Adipokines in inflammation and metabolic disease. Nature reviews Immunology. 2011;11(2):85–97. 10.1038/nri2921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2010;11(1):11–8. 10.1111/j.1467-789X.2009.00623.x . [DOI] [PubMed] [Google Scholar]
- 3. Cherian S, Lopaschuk GD, Carvalho E. Cellular cross-talk between epicardial adipose tissue and myocardium in relation to the pathogenesis of cardiovascular disease. American journal of physiology Endocrinology and metabolism. 2012;303(8):E937–49. 10.1152/ajpendo.00061.2012 . [DOI] [PubMed] [Google Scholar]
- 4. Sacks HS, Fain JN. Human epicardial adipose tissue: a review. American heart journal. 2007;153(6):907–17. 10.1016/j.ahj.2007.03.019 . [DOI] [PubMed] [Google Scholar]
- 5. Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008;117(5):605–13. 10.1161/CIRCULATIONAHA.107.743062 . [DOI] [PubMed] [Google Scholar]
- 6. Brinkley TE, Hsu FC, Carr JJ, Hundley WG, Bluemke DA, Polak JF, et al. Pericardial fat is associated with carotid stiffness in the Multi-Ethnic Study of Atherosclerosis. Nutrition, metabolism, and cardiovascular diseases: NMCD. 2011;21(5):332–8. 10.1016/j.numecd.2009.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Miao C, Chen S, Ding J, Liu K, Li D, Macedo R, et al. The association of pericardial fat with coronary artery plaque index at MR imaging: The Multi-Ethnic Study of Atherosclerosis (MESA). Radiology. 2011;261(1):109–15. 10.1148/radiol.11110346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Greif M, Becker A, von Ziegler F, Lebherz C, Lehrke M, Broedl UC, et al. Pericardial adipose tissue determined by dual source CT is a risk factor for coronary atherosclerosis. Arteriosclerosis, thrombosis, and vascular biology. 2009;29(5):781–6. 10.1161/ATVBAHA.108.180653 . [DOI] [PubMed] [Google Scholar]
- 9. Handschin C, Spiegelman BM. The role of exercise and PGC1alpha in inflammation and chronic disease. Nature. 2008;454(7203):463–9. 10.1038/nature07206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rudd JH, Fayad ZA. Imaging atherosclerotic plaque inflammation. Nature clinical practice Cardiovascular medicine. 2008;5 Suppl 2:S11–7. 10.1038/ncpcardio1160 . [DOI] [PubMed] [Google Scholar]
- 11. Chen W, Bural GG, Torigian DA, Rader DJ, Alavi A. Emerging role of FDG-PET/CT in assessing atherosclerosis in large arteries. European journal of nuclear medicine and molecular imaging. 2009;36(1):144–51. 10.1007/s00259-008-0947-2 . [DOI] [PubMed] [Google Scholar]
- 12. Kim TN, Kim S, Yang SJ, Yoo HJ, Seo JA, Kim SG, et al. Vascular inflammation in patients with impaired glucose tolerance and type 2 diabetes: analysis with 18F-fluorodeoxyglucose positron emission tomography. Circulation Cardiovascular imaging. 2010;3(2):142–8. 10.1161/CIRCIMAGING.109.888909 . [DOI] [PubMed] [Google Scholar]
- 13. Yoo HJ, Kim S, Park MS, Yang SJ, Kim TN, Seo JA, et al. Vascular inflammation stratified by C-reactive protein and low-density lipoprotein cholesterol levels: analysis with 18F-FDG PET. Journal of nuclear medicine: official publication, Society of Nuclear Medicine. 2011;52(1):10–7. 10.2967/jnumed.110.080838 . [DOI] [PubMed] [Google Scholar]
- 14. Choi HY, Kim S, Yang SJ, Yoo HJ, Seo JA, Kim SG, et al. Association of adiponectin, resistin, and vascular inflammation: analysis with 18F-fluorodeoxyglucose positron emission tomography. Arteriosclerosis, thrombosis, and vascular biology. 2011;31(4):944–9. 10.1161/ATVBAHA.110.220673 . [DOI] [PubMed] [Google Scholar]
- 15. Greif M, Leber AW, Saam T, Uebleis C, von Ziegler F, Rummler J, et al. Determination of Pericardial Adipose Tissue Increases the Prognostic Accuracy of Coronary Artery Calcification for Future Cardiovascular Events. Cardiology. 2012;121(4):220–7. 10.1159/000337083 . [DOI] [PubMed] [Google Scholar]
- 16. Iacobellis G, Bianco AC. Epicardial adipose tissue: emerging physiological, pathophysiological and clinical features. Trends in endocrinology and metabolism: TEM. 2011;22(11):450–7. 10.1016/j.tem.2011.07.003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry. 1972;18(6):499–502. . [PubMed] [Google Scholar]
- 18. Surti S, Kuhn A, Werner ME, Perkins AE, Kolthammer J, Karp JS. Performance of Philips Gemini TF PET/CT scanner with special consideration for its time-of-flight imaging capabilities. Journal of nuclear medicine: official publication, Society of Nuclear Medicine. 2007;48(3):471–80. . [PubMed] [Google Scholar]
- 19. Rudd JH, Myers KS, Bansilal S, Machac J, Pinto CA, Tong C, et al. Atherosclerosis inflammation imaging with 18F-FDG PET: carotid, iliac, and femoral uptake reproducibility, quantification methods, and recommendations. Journal of nuclear medicine: official publication, Society of Nuclear Medicine. 2008;49(6):871–8. 10.2967/jnumed.107.050294 . [DOI] [PubMed] [Google Scholar]
- 20. Clement K, Basdevant A, Dutour A. Weight of pericardial fat on coronaropathy. Arteriosclerosis, thrombosis, and vascular biology. 2009;29(5):615–6. 10.1161/ATVBAHA.108.182907 . [DOI] [PubMed] [Google Scholar]
- 21. Corradi D, Maestri R, Callegari S, Pastori P, Goldoni M, Luong TV, et al. The ventricular epicardial fat is related to the myocardial mass in normal, ischemic and hypertrophic hearts. Cardiovascular pathology: the official journal of the Society for Cardiovascular Pathology. 2004;13(6):313–6. 10.1016/j.carpath.2004.08.005 . [DOI] [PubMed] [Google Scholar]
- 22. Konishi M, Sugiyama S, Sugamura K, Nozaki T, Matsubara J, Akiyama E, et al. Accumulation of pericardial fat correlates with left ventricular diastolic dysfunction in patients with normal ejection fraction. Journal of cardiology. 2012;59(3):344–51. 10.1016/j.jjcc.2012.01.006 . [DOI] [PubMed] [Google Scholar]
- 23. Kim TH, Yu SH, Choi SH, Yoon JW, Kang SM, Chun EJ, et al. Pericardial fat amount is an independent risk factor of coronary artery stenosis assessed by multidetector-row computed tomography: the Korean Atherosclerosis Study 2. Obesity. 2011;19(5):1028–34. 10.1038/oby.2010.246 . [DOI] [PubMed] [Google Scholar]
- 24. Schlett CL, Ferencik M, Kriegel MF, Bamberg F, Ghoshhajra BB, Joshi SB, et al. Association of pericardial fat and coronary high-risk lesions as determined by cardiac CT. Atherosclerosis. 2012;222(1):129–34. 10.1016/j.atherosclerosis.2012.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cheng VY, Dey D, Tamarappoo B, Nakazato R, Gransar H, Miranda-Peats R, et al. Pericardial fat burden on ECG-gated noncontrast CT in asymptomatic patients who subsequently experience adverse cardiovascular events. JACC Cardiovascular imaging. 2010;3(4):352–60. 10.1016/j.jcmg.2009.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McAuley PA, Hsu FC, Loman KK, Carr JJ, Budoff MJ, Szklo M, et al. Liver attenuation, pericardial adipose tissue, obesity, and insulin resistance: the Multi-Ethnic Study of Atherosclerosis (MESA). Obesity. 2011;19(9):1855–60. 10.1038/oby.2011.191 . [DOI] [PubMed] [Google Scholar]
- 27. Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. The Journal of clinical investigation. 2003;112(12):1796–808. 10.1172/JCI19246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108(20):2460–6. 10.1161/01.CIR.0000099542.57313.C5 . [DOI] [PubMed] [Google Scholar]
- 29. Konishi M, Sugiyama S, Sato Y, Oshima S, Sugamura K, Nozaki T, et al. Pericardial fat inflammation correlates with coronary artery disease. Atherosclerosis. 2010;213(2):649–55. 10.1016/j.atherosclerosis.2010.10.007 . [DOI] [PubMed] [Google Scholar]
- 30. Vela D, Buja LM, Madjid M, Burke A, Naghavi M, Willerson JT, et al. The role of periadventitial fat in atherosclerosis. Archives of pathology & laboratory medicine. 2007;131(3):481–7. 10.1043/1543-2165(2007)131[481:TROPFI]2.0.CO;2 . [DOI] [PubMed] [Google Scholar]
- 31. Tadros TM, Massaro JM, Rosito GA, Hoffmann U, Vasan RS, Larson MG, et al. Pericardial fat volume correlates with inflammatory markers: the Framingham Heart Study. Obesity. 2010;18(5):1039–45. 10.1038/oby.2009.343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mazurek T, Kochman J, Kobylecka M, Wilimski R, Filipiak KJ, Krolicki L, et al. Inflammatory activity of pericoronary adipose tissue may affect plaque composition in patients with acute coronary syndrome without persistent ST-segment elevation: preliminary results. Kardiologia polska. 2014;72(5):410–6. 10.5603/KP.a2013.0320 . [DOI] [PubMed] [Google Scholar]
- 33. Mazurek T, Kiliszek M, Kobylecka M, Skubisz-Gluchowska J, Kochman J, Filipiak K, et al. Relation of proinflammatory activity of epicardial adipose tissue to the occurrence of atrial fibrillation. The American journal of cardiology. 2014;113(9):1505–8. 10.1016/j.amjcard.2014.02.005 . [DOI] [PubMed] [Google Scholar]
- 34. Mazzoccoli G, Dagostino MP, Fontana A, Copetti M, Pellegrini F, Grilli M, et al. Concomitant evaluation of flow-mediated vasodilation and epicardial fat thickness in idiopathic deep venous thrombosis. Journal of biological regulators and homeostatic agents. 2012;26(1):81–8. . [PubMed] [Google Scholar]
- 35. Mazzoccoli G, Copetti M, Dagostino MP, Grilli M, Fontana A, Pellegrini F, et al. Epicardial adipose tissue and idiopathic deep venous thrombosis: an association study. Atherosclerosis. 2012;223(2):378–83. 10.1016/j.atherosclerosis.2012.05.033 . [DOI] [PubMed] [Google Scholar]
- 36. Alexopoulos N, Melek BH, Arepalli CD, Hartlage GR, Chen Z, Kim S, et al. Effect of intensive versus moderate lipid-lowering therapy on epicardial adipose tissue in hyperlipidemic post-menopausal women: a substudy of the BELLES trial (Beyond Endorsed Lipid Lowering with EBT Scanning). Journal of the American College of Cardiology. 2013;61(19):1956–61. 10.1016/j.jacc.2012.12.051 . [DOI] [PubMed] [Google Scholar]
- 37. Liu J, Fox CS, Hickson DA, May WL, Ding J, Carr JJ, et al. Pericardial fat and echocardiographic measures of cardiac abnormalities: the Jackson Heart Study. Diabetes care. 2011;34(2):341–6. 10.2337/dc10-1312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fox CS, Gona P, Hoffmann U, Porter SA, Salton CJ, Massaro JM, et al. Pericardial fat, intrathoracic fat, and measures of left ventricular structure and function: the Framingham Heart Study. Circulation. 2009;119(12):1586–91. 10.1161/CIRCULATIONAHA.108.828970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cheng KH, Chu CS, Lee KT, Lin TH, Hsieh CC, Chiu CC, et al. Adipocytokines and proinflammatory mediators from abdominal and epicardial adipose tissue in patients with coronary artery disease. International journal of obesity. 2008;32(2):268–74. 10.1038/sj.ijo.0803726 . [DOI] [PubMed] [Google Scholar]
- 40. Konishi M, Sugiyama S, Sugamura K, Nozaki T, Ohba K, Matsubara J, et al. Association of pericardial fat accumulation rather than abdominal obesity with coronary atherosclerotic plaque formation in patients with suspected coronary artery disease. Atherosclerosis. 2010;209(2):573–8. 10.1016/j.atherosclerosis.2009.10.008 . [DOI] [PubMed] [Google Scholar]
- 41. Narumi H, Yoshida K, Hashimoto N, Umehara I, Funabashi N, Yoshida S, et al. Increased subcutaneous fat accumulation has a protective role against subclinical atherosclerosis in asymptomatic subjects undergoing general health screening. International journal of cardiology. 2009;135(2):150–5. 10.1016/j.ijcard.2008.03.044 . [DOI] [PubMed] [Google Scholar]
- 42. Porter SA, Massaro JM, Hoffmann U, Vasan RS, O'Donnel CJ, Fox CS. Abdominal subcutaneous adipose tissue: a protective fat depot? Diabetes care. 2009;32(6):1068–75. 10.2337/dc08-2280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mahabadi AA, Massaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA, et al. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. European heart journal. 2009;30(7):850–6. 10.1093/eurheartj/ehn573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Moustafa RR, Izquierdo-Garcia D, Fryer TD, Graves MJ, Rudd JH, Gillard JH, et al. Carotid plaque inflammation is associated with cerebral microembolism in patients with recent transient ischemic attack or stroke: a pilot study. Circulation Cardiovascular imaging. 2010;3(5):536–41. 10.1161/CIRCIMAGING.110.938225 . [DOI] [PubMed] [Google Scholar]
- 45. Grandpierre S, Desandes E, Meneroux B, Djaballah W, Mandry D, Netter F, et al. Arterial foci of F-18 fluorodeoxyglucose are associated with an enhanced risk of subsequent ischemic stroke in cancer patients: a case-control pilot study. Clinical nuclear medicine. 2011;36(2):85–90. 10.1097/RLU.0b013e318203bb42 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Korean Personal Information Protection Law prohibits providing personal data to 3rd party personnel without permission. IRB in Korea University Guro Hospital recommended that the data upon request might be provided only after specific permission of IRB. Contact information to which requests for the data: medica7@gmail.com.


