Abstract
Influenza A virus (IAV) has its natural reservoir in wild waterfowl, and new human IAVs often contain gene segments originating from avian IAVs. Treatment options for severe human influenza are principally restricted to neuraminidase inhibitors (NAIs), among which oseltamivir is stockpiled in preparedness for influenza pandemics. There is evolutionary pressure in the environment for resistance development to oseltamivir in avian IAVs, as the active metabolite oseltamivir carboxylate (OC) passes largely undegraded through sewage treatment to river water where waterfowl reside. In an in vivo mallard (Anas platyrhynchos) model, we tested if low-pathogenic avian influenza A(H7N9) virus might become resistant if the host was exposed to low levels of OC. Ducks were experimentally infected, and OC was added to their water, after which infection and transmission were maintained by successive introductions of uninfected birds. Daily fecal samples were tested for IAV excretion, genotype, and phenotype. Following mallard exposure to 2.5 μg/liter OC, the resistance-related neuraminidase (NA) I222T substitution, was detected within 2 days during the first passage and was found in all viruses sequenced from subsequently introduced ducks. The substitution generated 8-fold and 2.4-fold increases in the 50% inhibitory concentration (IC50) for OC (P < 0.001) and zanamivir (P = 0.016), respectively. We conclude that OC exposure of IAV hosts, in the same concentration magnitude as found in the environment, may result in amino acid substitutions, leading to changed antiviral sensitivity in an IAV subtype that can be highly pathogenic to humans. Prudent use of oseltamivir and resistance surveillance of IAVs in wild birds are warranted.
INTRODUCTION
Migratory waterfowl have a central role in the emergence of new human influenza A viruses (IAVs), as they are the reservoir hosts of IAV in the environment and as novel human-pathogenic IAVs often contain genetic material that originates from avian IAVs (1). In wild waterfowl, the IAV infection is intestinal with limited clinical signs (2, 3). Viruses are genetically diverse due to rapid rates of mutations and continuous reassortment of genetic segments (4) and are diffused along migratory routes (5). New human-pathogenic IAVs can evolve through reassortment of genetic segments from a human-adapted virus with segments from a virus originating from avian or other host species, a feature of all pandemic viruses of the last century (6). Avian IAVs can also infect humans by direct transmission following infection in poultry, which have both mammalian- and avian-type hemagglutinin receptors, and adaptations that enable viral crossing of the species barrier (7, 8). In March 2013, this type of transmission initiated an outbreak in China, resulting in severe human infection caused by a multiple reassortant avian A(H7N9) virus (9), with gene segments acquired from low-pathogenic avian influenza (LPAI) viruses of wild migratory birds and domesticated poultry (7, 10). Fortunately, to date no sustained human-to-human transmission of the virus has been seen (11), although it has become enzootic in China with establishment of multiple distinct regional lineages (12), and new human cases are being reported (13).
There are limited means to prevent and treat severe human IAV infections, particularly when a virus strain is novel and antigenically different from the circulating seasonal viruses, as little or no immunity exists in the population and vaccines are unavailable (14). New IAV drugs targeting different steps in the viral replication cycle and vaccines with broad immunogenicity might improve responses (15), but currently neuraminidase inhibitors (NAIs) are the best available initial means when in the face of a new human-pathogenic IAV (14). Therefore, global pandemic preparedness plans rely almost entirely on oseltamivir (Tamiflu; Roche) for the early-phase pandemic response, with large national stockpiles (16, 17). Indeed, NAIs are the primary treatment choice in the current Chinese A(H7N9) outbreak (18), and NAI resistance is associated with severe outcomes (19).
Resistant IAVs can arise in NAI-treated patients but might also be already inherent when a virus crosses the avian-human species barrier (20). Several lines of evidence suggest that wild waterfowl may be exposed to oseltamivir in their natural environment and that the IAVs infecting them might develop NAI resistance. The active metabolite, oseltamivir carboxylate (OC), is excreted by patients and is not removed during traditional sewage treatment (21, 22) or degraded by daylight exposure (23), thus ending up in sewage effluents and in river water where avian IAV hosts, such as different species of waterfowl, reside. OC measurements from river water have primarily been done in Japan, with collections from more than 40 river sample sites from the main river systems, where concentrations of up to 0.86 μg/liter have been detected (24–27). In Europe (Germany from 12 sites [28], Spain from 11 sites [29], and England from 21 sites [30]), OC concentrations in river water of approximately 0.05 μg/liter have been detected during the influenza season. The effect of environmental OC on IAV in the intestinal tract of wild birds is unknown. In vivo mallard experiments have demonstrated that IAVs of both the N1 and N2 subtypes (representing both phylogenetic neuraminidase [NA] groups N1 and N2) can develop NAI resistance when infected birds are exposed to OC concentrations ranging from 0.95 to 12 μg/liter in their water (31–33). Additionally, it was demonstrated that an acquired resistance mutation in an avian IAV can persist without drug pressure, with maintained viral fitness (34). If an avian IAV acquires and retains NAI resistance, a novel pandemic virus may be resistant already when it crosses the species barrier. Stockpiles of oseltamivir would then lose their role in the response to a pandemic, and if the virus is virulent, the public health consequences would be dramatic with limited treatment options.
From this perspective, it is important to evaluate the propensity for different NA variants to acquire and maintain NAI resistance. Here, we investigated an LPAI A(H7N9) virus in an in vivo mallard (Anas platyrhynchos) model, in which infected birds were exposed to OC in drinking and swimming water.
MATERIALS AND METHODS
Virus.
The influenza A/mallard/Sweden/1621/2002(H7N9) virus used in this study was isolated, as part of IAV surveillance, from a wild mallard in southern Sweden in December 2002, as described in reference 35.The virus was isolated in 11-day-old specific-pathogen-free (SPF) embryonated chicken eggs (ECE); the virus was inoculated in the allantoic cavity, harvested after 2 days, and detected by hemagglutination with turkey erythrocytes. A second passage in SPF ECE was done if the hemagglutination assay was negative. The positive samples were hemagglutinin (HA) subtyped by a hemagglutination inhibition assay with turkey erythrocytes and hyperimmune rabbit antisera against all HA subtypes (36). NA was subtyped by reverse transcriptase (RT)-PCR and sequencing with universal primers as described by Hoffman et al. (37). Whole-genome sequencing was done through the Influenza Virus Genome Sequencing Project (GenBank accession numbers for all segments are AHZ41929 to AHZ41940).
The phylogenetic placement in the context of Eurasian viruses was determined utilizing Bayesian trees. Outgroups included all Eurasian H7 (n = 531), all Eurasian N9 (n = 216), and 10 North American sequences for each H7 and N9, downloaded from the Influenza Research Database (http://www.fludb.org/). The trees were built using resources provided by the Swedish National Infrastructure for Computing (SNIC) through the Uppsala Multidisciplinary Center for Advanced Computational Science (UPPMAX).
Drugs.
OC and deuterium-labeled OC were obtained from F. Hoffmann-La Roche Ltd. (Basel, Switzerland) and zanamivir (ZA) (for use in the neuraminidase inhibition assay, as described in reference 38) was purchased locally as Relenza. The compounds were dissolved in double-distilled water, and stock solutions were stored at minus 20°C.
Mallard model.
One-day-old male mallards were purchased and bred isolated indoors at the animal facilities of the Swedish Veterinary Institute. Breeding, housing, and experimental protocols were approved by the Ethics Committee on Animal Experiments in Uppsala, Sweden (permit C63/13), and complied with guidelines of the Swedish Board of Agriculture. IAV infection prior to experiments was ruled out by blood serology (FlockCheck avian influenza virus antibody test kit; IDEXX, Hoofddorp, The Netherlands) performed at 10 weeks of age, and by real-time reverse transcriptase (RRT)-PCR of the IAV matrix gene from fecal samples (described below) taken before the ducks entered the experiment at 4 months of age.
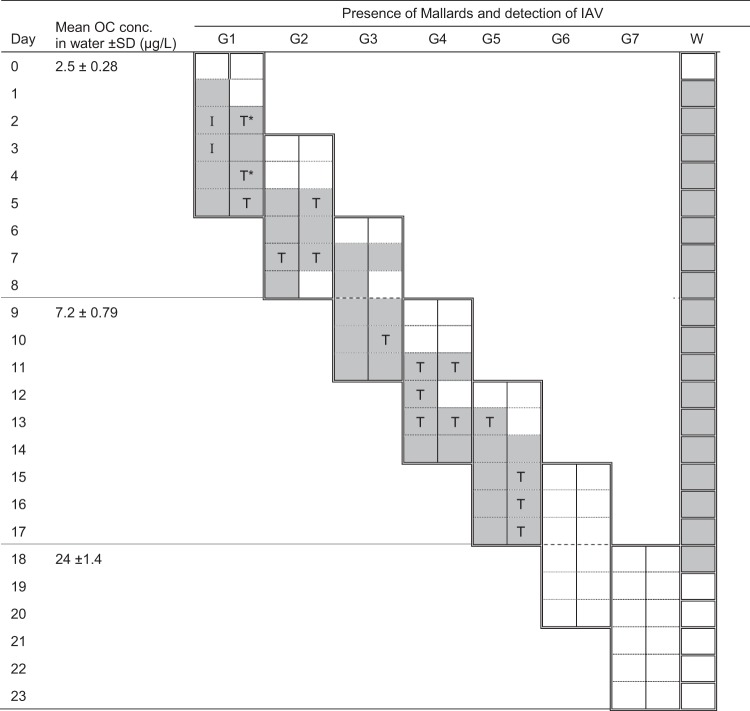
The experimental design was based on the dynamics of IAV infection in mallards, allowing continuous viral propagation by successive introduction of naive ducks to those infected and largely followed a previously described protocol (31, 32). Viral transmission between ducks is primarily by fecal excretion (1); infection and fecal shedding peak after 2 days and decrease markedly after approximately 5 to 7 days (39). At the start of the experiment, two mallards were inoculated in the esophagus with 1 ml of ECE allantoic fluid and placed in the experimental room (on day zero), which contained a single water source of 170 liters and food ad libitum. To sustain transmission with the most recently evolved viral variant, generations (two mallards) of naive ducks were introduced at day 3 postinoculation and housed together with the infected ducks during 48 h, until day 5 of the experiment, to allow transmission, after which the previous generation was euthanized (with intravenous injections of 100 mg/kg sodium pentobarbital [pentobarbital veterinary, 100 mg/ml]). On the following day (after 24 h and two changes of water), a new generation of two naive ducks was introduced and so forth, resulting in a total of seven generations of birds, each staying 5 days in the experiment, across 23 days. The water was changed daily and spiked with OC, initially to a concentration of 2.5 μg/liter, which was successively increased during the experiment, to 7.2 μg/liter of OC from day 9 and to 24 μg/liter of OC from day 18 (Fig. 1). Individual fecal samples were collected daily by swabbing fresh feces following defecation in single-use boxes. On a few occasions, cloacal swabbing replaced the fecal sampling if the birds did not defecate while in the boxes. Water samples (1 ml) were also taken daily for viral detection.
FIG 1.
Experimental mallard model with IAV shedding and NA 222 amino acid residues. The values 2.5 ± 0.28, 7.2 ± 0.79, and 24 ±1.4 μg/liter are the means ± standard deviations of 11, 9, and 7 water samples, respectively. The dashed horizontal lines indicate changes in OC concentrations. G1 represents generation one consisting of two mallards, G2 represents the second pair of mallards introduced in the experimental room, etc. Closed rectangles represent the presence of mallards in the experimental room and dotted lines indicate days. Note that birds were introduced into and removed from the experiment room in the daytime such that each bird was part of the experiment during 5 ′ 24 h, with a 24-h gap between every second generation. Shading indicates detection of IAV by RRT-PCR of the matrix gene from daily fecal samples (CT values of ≥45 were determined to be negative). I, isoleucine at NA residue 222; T*, threonine in shared proportions with isoleucine at NA residue 222; T, threonine at NA residue 222, as determined by Sanger sequencing of fecal samples; W, water from the 170-liter pool in the experimental room. Closed rectangles represent change of water and shading indicates detection of IAV by RRT-PCR of the matrix gene.
Viral detection and sequencing of NA.
Viral RNA was extracted from all fecal samples, from water, and from isolates with an automated magnetic bead method using a Magnatrix 8000 extraction robot (Magnetic Biosolutions, Stockholm, Sweden) with a Vet viral RNA kit (NorDiag ASA, Oslo, Norway). Some samples with low yields of NA PCR amplicons (see below) were reextracted from fecal samples by organic extraction with TRIzol (Life Technologies) using 900 μl reagent per 100 μl sample. Detection and quantification of IAV from fecal samples and water were done by RRT-PCR with primers and probe targeting the influenza A matrix gene (40) and an iScript one-step RT-PCR kit for probes (Bio-Rad). The reaction volumes of 25 μl with 0.5 μl enzyme mix and final concentrations of primers and probe of 400 nM and 120 nM, respectively, were run in a Corbett Research Rotor-Gene 2000 real-time thermo cycler (Corbett Research). Samples with cycle threshold (CT) values ≥45 were considered negative.
The NA gene was amplified from the RNA of fecal samples that were positive for IAV in the RRT-PCR by a one-step RT-PCR using specifically designed primers (see Table S1 in supplemental material) and a SuperScript III one-step RT-PCR system with Platinum Taq high fidelity polymerase (Life Technologies). Reaction volumes of 25 μl contained 0.25 μl enzyme mix, one forward and one reverse primer at a final concentration of 400 nM and 5 μl (1 pg to 1 μg) RNA sample. Thermocycling conditions were 30 min at 55°C, 5 min at 94°C, followed by 35 cycles of 1 min at 94°C, 1 min at 57°C, and 4 min at 68°C. PCR products were confirmed by gel electrophoresis and purified by enzymatic treatment with ExoSAP-IT (Affymetrix Inc., CA, USA), using 2 μl reagent to treat 24 μl sample. PCR products were Sanger sequenced at Macrogen Inc. (The Netherlands) with four sequencing primers (see Table S1 in the supplemental material). The sequence results were analyzed in SeqScape v2.7 software (Applied Biosystems) with the original A/mallard/Sweden/1621/2002(H7N9) NA sequence as a reference. A sequence result was considered reliable if there were at least two high-quality electropherogram sequences at any given nucleotide position. The genotype was determined as “mixed” if two peaks representing different nucleotides were visible at a single position in the electropherograms.
Neuraminidase inhibition by OC and ZA.
Prior to phenotypic NAI sensitivity testing, fecal samples were propagated in SPF ECE (Valo, Germany), as described above, to obtain a sufficient viral titer for the assay, followed by NA sequencing (as described above) to verify the genotype. Ten NA I222T isolates and three wild-type isolates were tested. Inhibition of NA by OC and ZA was determined on duplicate samples in a fluorogenic NA substrate assay using 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA) (Sigma) (41) with 10-step dilution series (4,000 to 0.0015 nM) of OC and ZA in black 96-well flat-bottom plates, according to the protocol of the European Vigilance Network for the Management of Antiviral Drug Resistance (VIRGIL-CLINVIR) (42). Virus and drugs were preincubated in 37°C for 30 min followed by a 60-min incubation with MUNANA substrate. Fluorescent products were measured in an Infinite M1000 PRO (Tecan) microplate reader, and 50% inhibitory concentrations (IC50s) were determined from the best-fit dose-response curves using Prism 6 software (GraphPad).
Detection and quantification of OC in water.
Water samples (∼40 ml) from the experimental water pool were collected daily, both before and after the water was changed (post- and preexposure samples, respectively). On the first and last days of each concentration level, triplicate samples were taken for evaluation of the method's variation. Ten milliliters of each water sample was prefiltered (0.45 μm) and acidified (0.1% formic acid). Analysis for detection of OC was done on 1 ml of the filtrate using an on-line solid-phase extraction/liquid chromatography-tandem mass spectrometry (SPE/LC-MS/MS) method, as previously described (43). Results were quantified using deuterium-labeled OC as an internal standard, with three calibration points. For evaluation of OC degradation during 24 h, preexposure samples were compared to postexposure samples from the first and last days of the experiment.
Screening of the NCBI Influenza Virus Resource database.
All avian N9 sequences available from the NCBI Influenza Virus Resource database (44) (http://www.ncbi.nlm.nih.gov/genomes/FLU/FLU.html) were downloaded on 15 February 2015 and aligned with BioEdit v7.2.5 software. Screening was done for amino acid 222 variant sequences.
Statistical analysis.
The hypothesis of no difference in mean IC50s of OC and ZA between wild-type virus and NA-I222T mutated virus was tested with a two-sample t test for independent samples with calculations of 95% confidence intervals (95% CI) for differences in means using Statistica v12 software (StatSoft).
RESULTS
Evolutionary relationships of H7 and N9 segments.
The LPAI A(H7N9) virus used in this study was phylogenetically nested in a clade with European wild bird viruses with regard to the H7 segment, which was also reflected by placement of the N9 segment. This virus was distantly related to poultry H7 sequences, including the Chinese A(H7N9) 2013 outbreak strain (45) (see Fig. S1 in the supplemental material).
Analysis of OC concentrations in water.
The analysis had a limit of quantification (LOQ) of 2.5 ng/liter and linearity (R2) of 0.9999. The relative standard deviations (RSD) between triplicate samples were 0 to 11%. The average daily OC concentrations (samples taken after 24 h of experiment before the change of water) were 2.5 μg/liter (n = 11, SD, 0.28 μg/liter), 7.2 μg/liter (n = 9; SD, 0.79 μg/liter), and 24 μg/liter (n = 7; SD, 1.44 μg/liter) (Fig. 1). OC concentrations were stable within 24 h, as the measured increments of 5% and 8% are within the variation of the analytical method.
IAV infection and NA amino acid substitution.
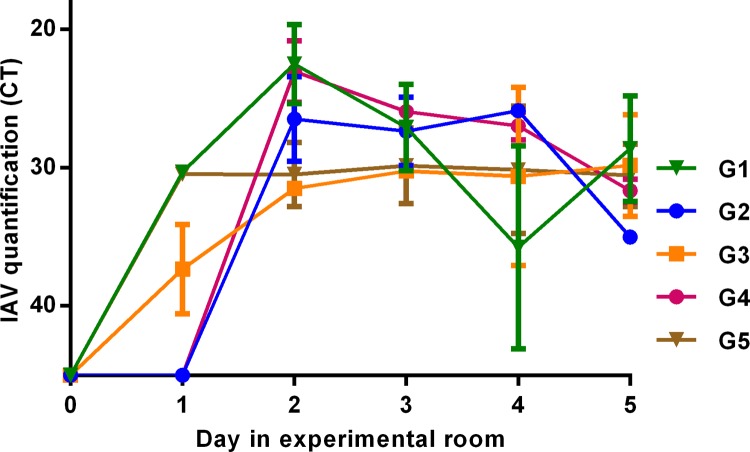
IAV infection was established and perpetuated in the first five of seven generations of mallards (across 17 days), when OC exposure was 2.5 μg/liter (8.8 nM) and 7.2 μg/liter (25 nM), as seen by fecal excretion from day 1 or 2 postinoculation or introduction to the experimental room, through day 5 (Fig. 2). During generations six and seven, when OC exposure was increased to 24 μg/liter (84 nM), no viral shedding was detected (Fig. 1). In water samples, IAV was detected during the first 18 days but not the last 5 days of the experiment, consistent with the negative fecal samples. Sequencing of NA demonstrated the amino acid substitution I222T (ATA for isoleucine changed to ACA for threonine) in a small proportion of virus from one mallard in generation one 2 days postinoculation, while OC exposure was 2.5 μg/liter. The proportion of the I222T variant increased over 3 days, and from day 5 all subsequently sequenced viruses had the I222T variant until the end of IAV transmission (Fig. 1; see also Fig. S2 in the supplemental material). No other amino acid substitutions were found in NA during the experiment.
FIG 2.
Shedding of A(H7N9) virus determined by RRT-PCR of the matrix gene from daily fecal samples. The x axis displays the number of days that each pair of birds had been present in the experimental room at the time of sampling. The y axis displays cycle threshold (CT) values of the RRT-PCR as a semiquantitative measure of excreted IAV. CT values of ≥45 were determined to be negative. G1 represents mallard generation one of the experiment, consisting of two mallards, G2 represents the second pair of mallards introduced in the experimental room, etc. Values in the graph indicate mean CT values from two samples, error bars indicate standard errors of the mean (SEM). For clarity, if one of the two samples of a generation from 1 day was IAV negative (CT of ≥45), only the positive sample was included in the graph, i.e., G1, day 1; G2, day 5; G3, day 2; G4, day 3; G5, day 1 (see also Fig. 1).
Sensitivity to OC and ZA.
NA inhibition by OC and ZA, tested on 10 NA I222T samples and 3 wild-type samples, showed increased IC50s of the NA I222T variant compared to those of the wild-type virus for both OC (P = 0.000011; 95% CI for difference in means, 2.5 to 4.6 nM) and ZA (P = 0.016; 95% CI for difference in means, 0.16 to 1.28 nM) (Table 1). No difference in inhibition was found between wild-type samples from the experiment and the original virus (OC: P = 0.62; 95% CI for difference in means, −0.37 to 0.48 nM; ZA: P = 0.77; 95% CI for difference in means, −1.12 to 0.96 nM) (Table 1), with IC50s in the same range as those for other avian N9, human A(H7N9), and group N2 wild-type reference viruses (18).
TABLE 1.
Neuraminidase inhibition by oseltamivir carboxylate and zanamivir
| Virus | IC50 (nM)a |
|
|---|---|---|
| Oseltamivir carboxylate | Zanamivir | |
| A/1621(H7N9)b (n = 1) | 0.45 ± 0.048 | 0.58 ± 0.010 |
| NA I222 (n = 3)c | 0.51 ± 0.12 | 0.50 ± 0.24 |
| NA I222T (n = 10)d | 4.1 ± 0.87 | 1.2 ± 0.41 |
Drug concentrations that reduced viral NA activity by 50% (IC50) in a fluorescence-based assay with the MUNANA substrate. Values are means ± SD from 1, 3, and 10 duplicate sample analyses.
Virus used for inoculation of mallards.
Virus isolated from fecal samples during the experiment, with wild-type isoleucine (I) at NA residue 222.
Virus isolated from fecal samples during the experiment, with a threonine (T) substitution at NA residue 222.
Sequence database screening.
Screening of all available 751 avian IAV N9 sequences in the NCBI Influenza Virus Resource database showed that none had threonine (T) and that all had isoleucine (I) and at amino acid residue 222.
DISCUSSION
In this OC exposure study, in which mallards were infected with an LPAI A(H7N9) that naturally circulates in wild ducks in Europe, the NA I222T substitution was detected after 2 days of 2.5 μg/liter OC exposure in the first mallard generation passage and rapidly became the dominant genotype (Fig. 1; see also Fig. S2 in the supplemental material). Although there were no unexposed control mallards and infection and transmission were inhibited when drug pressure was increased, there are compelling reasons to believe that the OC exposure generated the change in the viral genotype. Drug-induced selection of the NA I222T substitution is supported by the absence of circulating avian N9 virus with the 222T genotype (based upon IAV sequence database screening), by previously observed NA I222R and NA I222K variants in A(H7N9) virus following oseltamivir treatment of humans (46), and by in vivo induction of NA I222T in A(H3N2) by low-dose OC exposure of infected mice (47).
At OC exposure levels of 2.5 and 7.2 μg/liter, the NA I222T mutant virus replicated, was excreted, and was transmitted similarly to wild type viruses measured in previous studies in this mallard model (31, 32, 39). However, when the OC exposure level was increased to 24 μg/liter (84 nM), no viral shedding was detected, consistent with an OC concentration well above the median IC50 of 4.1 nM of the mutant. Interestingly, the 7.2 μg/liter (25 nM) OC exposure was not sufficient to prevent replication and transmission of virus to two naive duck generations, which demonstrates that OC concentrations in environmental water cannot be directly translated to an antiviral effect at the site of infection in the mallard intestinal tract. As the IAV infection in waterfowl is intestinal and virus primarily invades apical epithelial cells (39), the virus is directly exposed to the active drug without a need for systemic uptake, which may increase drug exposure compared to that for oral prodrug administration and the deposition of active OC in airway tissue required in other species.
Our experiments did not indicate reduced fitness of the NA I222T mutant as excretion and transmission of virus were similar to previous observations with wild-type viruses (31, 32, 39), nor did propagation of the fecal samples without drug exposure in embryonated chicken eggs select for wild-type virus over I222T variants (including those with a mixed genotype). However, these measures are only proxies for viral fitness. Further studies with propagation of mutated virus in mallards without drug pressure and competitive infection studies with simultaneous passage of wild-type virus and mutated virus in unexposed hosts might better conclude if fitness of the mutant is indeed retained.
The active substrate binding site of NA is composed of 9 amino acids, supported by 10 framework residues, including I222 (48). NA I222T variants are described in human seasonal influenza B (49, 50), A(H3N2) (51), and A(H1N1)/pdm2009 (52) viruses, as well as in A(H5N1) virus (53), where the substitution was demonstrated to change the binding kinetics (loss of slow OC binding) (54). NA I222T and several other amino acid substitutions at the 222 NA residue generate reduced sensitivity to NAIs, either as independent resistance substitutions (55) or, perhaps of more concern, by enhancing resistance induced by H274Y in N1 virus (56, 57) or by E119V in N2 virus (58). Several substitutions also seem to restore reduced fitness: I222T/V/R combined with H274Y in N1 virus (56, 57) and I222V combined with E119V in N2 virus (59). Sequential evolution of permissive amino acids in a viral population over time, including at the NA 222 position, appears to facilitate acquisition and harboring of new resistance mutations, illustrated by the OC-resistant human seasonal A(H1N1)/H274Y virus that circulated in 2007 to 2009 (60).
Changes in inhibition by NAIs caused by NA I222T in our study, 8-fold and 2.4-fold increases in IC50s by OC and ZA, respectively (Table 1), are similar to previously described levels for the substitution in other viral subtypes (49, 50, 52, 54, 61, 62). The level of change in IC50 does not meet the criteria for reduced inhibition according to the WHO phenotype criteria for resistance surveillance (>10-fold increase in IC50 compared to that for reference strains) (63). However, the results demonstrate that an OC-exposed avian N9 virus, in its natural host, can acquire a mutation that influences NAI sensitivity and that can modulate NAI-resistant viruses (53, 56). Environmental OC concentrations of 0.86 μg/liter detected to date (25) are below the experimental concentrations at which resistance has evolved in IAVs in mallards, both in previous studies (31–33) and in this one. However, the concentrations are on the same order of magnitude, environmental levels may occasionally be higher than thus far detected, particularly during an epidemic or pandemic peak, and different avian IAVs acquire resistance mutations at different exposure levels. Additionally, in the present study, as 2.5 μg/liter was the lowest level of OC exposure, we cannot exclude the possibility that the I222T substitution could have been acquired at a lower OC concentration. Taking our results together, we believe there are good reasons not to ignore environmental OC as a risk factor for resistance development in avian IAVs of wild birds. Indeed, there are no indications that NAI resistance per se contributes to viral crossing of the avian to human species barriers. Rather, the reason for concern regarding NAI resistance in wild bird IAVs is the great genetic variability, which provides potential for a genetic context allowing emergence and persistence of resistance mutations, possibly also through a species-crossing evolutionary process, should such occur, to a novel human-pathogenic virus. Compared to NAI resistance evolving in treated humans, where the clinical outcome of individuals may be affected, a novel inherently resistant human IAV would change a pandemic scenario entirely and disarm preparedness plans.
In conclusion, the acquisition of I222T in a European wild duck LPAI A(H7N9) virus demonstrates that N9 viruses can harbor I222T substitutions and confirms the levels of reduced NAI sensitivity in other NA subtypes. Retained transmission and replication of the I222T mutant virus in our mallard model indicates that it might be sustained in wild migratory waterfowl. Although the LPAI A(H7N9) we used in our study is not related to the Chinese A(H7N9) outbreak strains, our findings demonstrate that a mutation which influences NAI sensitivity and can compensate for reduced fitness caused by other resistance mutations can occur among wild bird hosts in an IAV subtype that is potentially human pathogenic. To better understand the emergence and persistence of resistant IAVs, it is important to further study possible transmission of avian IAVs containing resistance-related mutations from wild birds to poultry, humans, and other mammals. As resistance mutation(s) in an A(H7N9) virus or in another novel human-pathogenic IAV with pandemic potential poses a public health threat, our results stress the need for prudent antiviral use and better sewage treatment as preventive measures, as well as resistance surveillance of IAVs in wild birds.
Supplementary Material
ACKNOWLEDGMENTS
We acknowledge the Swedish Research Council FORMAS (grant 211-2013-1320), the Swedish Research Council (Vetenskapsrådet), and the Family Olinder-Nielsen's Foundation for financial support. We also acknowledge the National Institute of Allergy and Infectious Diseases-NIH Centers of Excellence for Influenza Research and Surveillance contract HHSN266200700010C for full virus genome sequencing of the A(H7N9) isolate.
Susanne Bloemberg and the rest of the staff at the animal facility of the National Veterinary Institute, Uppsala, are gratefully acknowledged for excellent animal care.
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/AAC.00886-15.
REFERENCES
- 1.Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y. 1992. Evolution and ecology of influenza A viruses. Microbiol Rev 56:152–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jourdain E, Gunnarsson G, Wahlgren J, Latorre-Margalef N, Bröjer C, Sahlin S, Svensson L, Waldenström J, LundkvistÅ Olsen B. 2010. Influenza virus in a natural host, the mallard: experimental infection data. PLoS One 5:e8935. doi: 10.1371/journal.pone.0008935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Latorre-Margalef N, Gunnarsson G, Munster VJ, Fouchier RA, Osterhaus AD, Elmberg J, Olsen B, Wallensten A, Haemig PD, Fransson T, Brudin L, Waldenström J. 2009. Effects of influenza A virus infection on migrating mallard ducks. Proc Biol Sci 276:1029–1036. doi: 10.1098/rspb.2008.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dugan VG, Chen R, Spiro DJ, Sengamalay N, Zaborsky J, Ghedin E, Nolting J, Swayne DE, Runstadler JA, Happ GM, Senne DA, Wang R, Slemons RD, Holmes EC, Taubenberger JK. 2008. The evolutionary genetics and emergence of avian influenza viruses in wild birds. PLoS Pathog 4:e1000076. doi: 10.1371/journal.ppat.1000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olsen B, Munster VJ, Wallensten A, Waldenström J, Osterhaus AD, Fouchier RA. 2006. Global patterns of influenza A virus in wild birds. Science 312:384–388. doi: 10.1126/science.1122438. [DOI] [PubMed] [Google Scholar]
- 6.Guan Y, Vijaykrishna D, Bahl J, Zhu H, Wang J, Smith GJ. 2010. The emergence of pandemic influenza viruses. Protein Cell 1:9–13. doi: 10.1007/s13238-010-0008-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu D, Shi W, Shi Y, Wang D, Xiao H, Li W, Bi Y, Wu Y, Li X, Yan J, Liu W, Zhao G, Yang W, Wang Y, Ma J, Shu Y, Lei F, Gao GF. 2013. Origin and diversity of novel avian influenza A H7N9 viruses causing human infection: phylogenetic, structural, and coalescent analyses. Lancet 381:1926–1932. doi: 10.1016/S0140-6736(13)60938-1. [DOI] [PubMed] [Google Scholar]
- 8.Forrest HL, Webster RG. 2010. Perspectives on influenza evolution and the role of research. Anim Health Res Rev 11:3–18. doi: 10.1017/S1466252310000071. [DOI] [PubMed] [Google Scholar]
- 9.Jernigan DB, Cox NJ. 2015. H7N9: preparing for the unexpected in influenza. Annu Rev Med 66:361–371. doi: 10.1146/annurev-med-010714-112311. [DOI] [PubMed] [Google Scholar]
- 10.Lam TT, Wang J, Shen Y, Zhou B, Duan L, Cheung CL, Ma C, Lycett SJ, Leung CY, Chen X, Li L, Hong W, Chai Y, Zhou L, Liang H, Ou Z, Liu Y, Farooqui A, Kelvin DJ, Poon LL, Smith DK, Pybus OG, Leung GM, Shu Y, Webster RG, Webby RJ, Peiris JS, Rambaut A, Zhu H, Guan Y. 2013. The genesis and source of the H7N9 influenza viruses causing human infections in China. Nature 502:241–244. doi: 10.1038/nature12515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watanabe T, Kiso M, Fukuyama S, Nakajima N, Imai M, Yamada S, Murakami S, Yamayoshi S, Iwatsuki-Horimoto K, Sakoda Y, Takashita E, McBride R, Noda T, Hatta M, Imai H, Zhao D, Kishida N, Shirakura M, de Vries RP, Shichinohe S, Okamatsu M, Tamura T, Tomita Y, Fujimoto N, Goto K, Katsura H, Kawakami E, Ishikawa I, Watanabe S, Ito M, Sakai-Tagawa Y, Sugita Y, Uraki R, Yamaji R, Eisfeld AJ, Zhong G, Fan S, Ping J, Maher EA, Hanson A, Uchida Y, Saito T, Ozawa M, Neumann G, Kida H, Odagiri T, Paulson JC, Hasegawa H, Tashiro M, Kawaoka Y. 2013. Characterization of H7N9 influenza A viruses isolated from humans. Nature 501:551–555. doi: 10.1038/nature12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lam TT, Zhou B, Wang J, Chai Y, Shen Y, Chen X, Ma C, Hong W, Chen Y, Zhang Y, Duan L, Chen P, Jiang J, Zhang Y, Li L, Poon LL, Webby RJ, Smith DK, Leung GM, Peiris JS, Holmes EC, Guan Y, Zhu H. 2015. Dissemination, divergence and establishment of H7N9 influenza viruses in China. Nature 522:102−105. doi: 10.1038/nature14348. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. 2015. Human infection with avian influenza A(H7N9) virus—China. Disease outbreak news 11 March 2015. http://www.who.int/csr/don/11-march-2015-avian-influenza-china/en/. [Google Scholar]
- 14.Nguyen-Van-Tam JS, Openshaw PJ, Nicholson KG. 2014. Antivirals for influenza: where now for clinical practice and pandemic preparedness? Lancet 384:386–387. doi: 10.1016/S0140-6736(14)60726-1. [DOI] [PubMed] [Google Scholar]
- 15.Webster RG, Govorkova EA. 2014. Continuing challenges in influenza. Ann N Y Acad Sci 1323:115–139. doi: 10.1111/nyas.12462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel A, Gorman SE. 2009. Stockpiling antiviral drugs for the next influenza pandemic. Clin Pharmacol Ther 86:241–243. doi: 10.1038/clpt.2009.142. [DOI] [PubMed] [Google Scholar]
- 17.Wan Po AL, Farndon P, Palmer N. 2009. Maximizing the value of drug stockpiles for pandemic influenza. Emerg Infect Dis 15:1686–1687. doi: 10.3201/eid1510.090844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baranovich T, Burnham AJ, Marathe BM, Armstrong J, Guan Y, Shu Y, Peiris JM, Webby RJ, Webster RG, Govorkova EA. 2014. The neuraminidase inhibitor oseltamivir is effective against A/Anhui/1/2013 (H7N9) influenza virus in a mouse model of acute respiratory distress syndrome. J Infect Dis 209:1343–1353. doi: 10.1093/infdis/jit554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hu Y, Lu S, Song Z, Wang W, Hao P, Li J, Zhang X, Yen HL, Shi B, Li T, Guan W, Xu L, Liu Y, Wang S, Zhang X, Tian D, Zhu Z, He J, Huang K, Chen H, Zheng L, Li X, Ping J, Kang B, Xi X, Zha L, Li Y, Zhang Z, Peiris M, Yuan Z. 2013. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet 381:2273–2279. doi: 10.1016/S0140-6736(13)61125-3. [DOI] [PubMed] [Google Scholar]
- 20.Järhult JD. 2012. Oseltamivir (Tamiflu) in the environment, resistance development in influenza A viruses of dabbling ducks and the risk of transmission of an oseltamivir-resistant virus to humans—a review. Infect Ecol Epidemiol 2. doi: 10.3402/iee.v2i0.18385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fick J, Lindberg RH, Tysklind M, Haemig PD, Waldenström J, Wallensten A, Olsen B. 2007. Antiviral oseltamivir is not removed or degraded in normal sewage water treatment: implications for development of resistance by influenza A virus. PLoS One 2:e986. doi: 10.1371/journal.pone.0000986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ghosh GC, Nakada N, Yamashita N, Tanaka H. 2010. Occurrence and fate of oseltamivir carboxylate (Tamiflu) and amantadine in sewage treatment plants. Chemosphere 81:13–17. doi: 10.1016/j.chemosphere.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 23.Bartels P, von Tumpling W Jr. 2008. The environmental fate of the antiviral drug oseltamivir carboxylate in different waters. Sci Total Environ 405:215–225. doi: 10.1016/j.scitotenv.2008.06.032. [DOI] [PubMed] [Google Scholar]
- 24.Söderström H, Järhult JD, Olsen B, Lindberg RH, Tanaka H, Fick J. 2009. Detection of the antiviral drug oseltamivir in aquatic environments. PLoS One 4:e6064. doi: 10.1371/journal.pone.0006064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Takanami R, Ozaki H, Giri RR, Taniguchi S, Hayashi S. 2010. Detection of antiviral drugs oseltamivir phosphate and oseltamivir carboxylate in Neya River, Osaka Japan. J Water Environ Technol 8:363–372. doi: 10.2965/jwet.2010.363. [DOI] [Google Scholar]
- 26.Azuma T, Nakada N, Yamashita N, Tanaka H. 2012. Synchronous dynamics of observed and predicted values of anti-influenza drugs in environmental waters during a seasonal influenza outbreak. Environ Sci Technol 46:12873–12881. doi: 10.1021/es303203c. [DOI] [PubMed] [Google Scholar]
- 27.Ghosh GC, Nakada N, Yamashita N, Tanaka H. 2010. Oseltamivir carboxylate, the active metabolite of oseltamivir phosphate (Tamiflu), detected in sewage discharge and river water in Japan. Environ Health Perspect 118:103–107. doi: 10.1289/ehp.0900930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prasse C, Schlusener MP, Schulz R, Ternes TA. 2010. Antiviral drugs in wastewater and surface waters: a new pharmaceutical class of environmental relevance? Environ Sci Technol 44:1728–1735. doi: 10.1021/es903216p. [DOI] [PubMed] [Google Scholar]
- 29.Gonçalves C, Perez S, Osorio V, Petrovic M, Alpendurada MF, Barcelo D. 2011. Photofate of oseltamivir (Tamiflu) and oseltamivir carboxylate under natural and simulated solar irradiation: kinetics, identification of the transformation products, and environmental occurrence. Environ Sci Technol 45:4307–4314. doi: 10.1021/es1032629. [DOI] [PubMed] [Google Scholar]
- 30.Singer AC, Järhult JD, Grabic R, Khan GA, Lindberg RH, Fedorova G, Fick J, Bowes MJ, Olsen B, Söderstrom H. 2014. Intra- and inter-pandemic variations of antiviral, antibiotics and decongestants in wastewater treatment plants and receiving rivers. PLoS One 9:e108621. doi: 10.1371/journal.pone.0108621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gillman A, Muradrasoli S, Söderstrom H, Nordh J, Bröjer C, Lindberg RH, Latorre-Margalef N, Waldenström J, Olsen B, Järhult JD. 2013. Resistance mutation R292K is induced in influenza A(H6N2) virus by exposure of infected mallards to low levels of oseltamivir. PLoS One 8:e71230. doi: 10.1371/journal.pone.0071230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Järhult JD, Muradrasoli S, Wahlgren J, Söderstrom H, Orozovic G, Gunnarsson G, Bröjer C, Latorre-Margalef N, Fick J, Grabic R, Lennerstrand J, Waldenström J, LundkvistÅ Olsen B. 2011. Environmental levels of the antiviral oseltamivir induce development of resistance mutation H274Y in influenza A/H1N1 virus in mallards. PLoS One 6:e24742. doi: 10.1371/journal.pone.0024742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Achenbach JE, Bowen RA. 2013. Effect of oseltamivir carboxylate consumption on emergence of drug-resistant H5N2 avian influenza virus in mallard ducks. Antimicrob Agents Chemother 57:2171–2181. doi: 10.1128/AAC.02126-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gillman A, Muradrasoli S, Söderstrom H, Holmberg F, Latorre-Margalef N, Tolf C, Waldenström J, Gunnarsson G, Olsen B, Järhult JD. 2015. Oseltamivir-resistant influenza A (H1N1) virus strain with an H274Y mutation in neuraminidase persists without drug pressure in infected mallards. Appl Environ Microbiol 81:2378–2383. doi: 10.1128/AEM.04034-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wallensten A, Munster VJ, Latorre-Margalef N, Brytting M, Elmberg J, Fouchier RA, Fransson T, Haemig PD, Karlsson M, Lundkvist Å Osterhaus AD, Stervander M, Waldenström J, Olsen B. 2007. Surveillance of influenza A virus in migratory waterfowl in northern Europe. Emerg Infect Dis 13:404–411. doi: 10.3201/eid1303.061130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fouchier RAM, Munster V, Wallensten A, Bestebroer TM, Herfst S, Smith D, Rimmelzwaan GF, Olsen B, Osterhaus ADME. 2005. Characterization of a novel influenza a virus hemagglutinin subtype (H16) obtained from black-headed gulls. J Virol 79:2814–2822. doi: 10.1128/JVI.79.5.2814-2822.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch Virol 146:2275–2289. doi: 10.1007/s007050170002. [DOI] [PubMed] [Google Scholar]
- 38.Hurt A. 2007. Standard operating procedure WHO-025: Fluorometric neuraminidase inhibition assay. Official copy. World Health Organization Collaborating Centre for Reference & Research on Influenza Australia. http://www.nisn.org/documents/A.Hurt_Protocol_for_NA_fluorescence.pdf. [Google Scholar]
- 39.Bröjer C, Järhult JD, Muradrasoli S, Söderstrom H, Olsen B, Gavier-Widen D. 2013. Pathobiology and virus shedding of low-pathogenic avian influenza virus (A/H1N1) infection in mallards exposed to oseltamivir. J Wildl Dis 49:103–113. doi: 10.7589/2011-11-335. [DOI] [PubMed] [Google Scholar]
- 40.Spackman E, Suarez DL. 2008. Type A influenza virus detection and quantitation by real-time RT-PCR. Methods Mol Biol 436:19–26. doi: 10.1007/978-1-59745-279-3_4. [DOI] [PubMed] [Google Scholar]
- 41.Potier M, Mameli L, Belisle M, Dallaire L, Melancon SB. 1979. Fluorometric assay of neuraminidase with a sodium (4-methylumbelliferyl-alpha-d-N-acetylneuraminate) substrate. Anal Biochem 94:287–296. doi: 10.1016/0003-2697(79)90362-2. [DOI] [PubMed] [Google Scholar]
- 42.Lackenby A. 24 May 2008. Determination of influenza virus susceptibility to neuraminidase inhibitors using a fluorescent substrate, p 1–15. Neuraminidase Inhibitor Surveillance Network. http://www.nisn.org/documents/Zambon_-_VIRGIL_IC50_SOP.pdf. [Google Scholar]
- 43.Khan GA, Lindberg R, Grabic R, Fick J. 2012. The development and application of a system for simultaneously determining anti-infectives and nasal decongestants using on-line solid-phase extraction and liquid chromatography-tandem mass spectrometry. J Pharm Biomed Anal 66:24–32. doi: 10.1016/j.jpba.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 44.Bao Y, Bolotov P, Dernovoy D, Kiryutin B, Zaslavsky L, Tatusova T, Ostell J, Lipman D. 2008. The influenza virus resource at the National Center for Biotechnology Information. J Virol 82:596–601. doi: 10.1128/JVI.02005-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lebarbenchon C, Brown JD, Stallknecht DE. 2013. Evolution of influenza A virus H7 and N9 subtypes, Eastern Asia. Emerg Infect Dis 19:1635–1638. doi: 10.3201/eid1910.130609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marjuki H, Mishin VP, Chesnokov AP, Jones J, De La Cruz JA, Sleeman K, Tamura D, Nguyen HT, Wu HS, Chang FY, Liu MT, Fry AM, Cox NJ, Villanueva JM, Davis CT, Gubareva LV. 2015. Characterization of drug-resistant influenza A(H7N9) variants isolated from an oseltamivir-treated patient in Taiwan. J Infect Dis 211:249–257. doi: 10.1093/infdis/jiu447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pizzorno A, Abed Y, Plante PL, Carbonneau J, Baz M, Hamelin ME, Corbeil J, Boivin G. 2014. Evolution of oseltamivir resistance mutations in influenza A(H1N1) and A(H3N2) viruses during selection in experimentally infected mice. Antimicrob Agents Chemother 58:6398–6405. doi: 10.1128/AAC.02956-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Varghese JN, McKimm-Breschkin JL, Caldwell JB, Kortt AA, Colman PM. 1992. The structure of the complex between influenza virus neuraminidase and sialic acid, the viral receptor. Proteins 14:327–332. doi: 10.1002/prot.340140302. [DOI] [PubMed] [Google Scholar]
- 49.Sheu TG, Deyde VM, Okomo-Adhiambo M, Garten RJ, Xu X, Bright RA, Butler EN, Wallis TR, Klimov AI, Gubareva LV. 2008. Surveillance for neuraminidase inhibitor resistance among human influenza A and B viruses circulating worldwide from 2004 to 2008. Antimicrob Agents Chemother 52:3284–3292. doi: 10.1128/AAC.00555-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hatakeyama S, Sugaya N, Ito M, Yamazaki M, Ichikawa M, Kimura K, Kiso M, Shimizu H, Kawakami C, Koike K, Mitamura K, Kawaoka Y. 2007. Emergence of influenza B viruses with reduced sensitivity to neuraminidase inhibitors. JAMA 297:1435–1442. [DOI] [PubMed] [Google Scholar]
- 51.Lee HK, Tang JW, Loh TP, Hurt AC, Oon LL, Koay ES. 2015. Molecular surveillance of antiviral drug resistance of influenza A/H3N2 virus in Singapore, 2009-2013. PLoS One 10:e0117822. doi: 10.1371/journal.pone.0117822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dapat C, Kondo H, Dapat IC, Baranovich T, Suzuki Y, Shobugawa Y, Saito K, Saito R, Suzuki H. 2013. Neuraminidase inhibitor susceptibility profile of pandemic and seasonal influenza viruses during the 2009-2010 and 2010-2011 influenza seasons in Japan. Antiviral Res 99:261–269. doi: 10.1016/j.antiviral.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 53.McKimm-Breschkin JL. 2012. Influenza neuraminidase inhibitors: antiviral action and mechanisms of resistance. Influenza Other Respir Viruses 7(Suppl 1):25–36. doi: 10.1111/irv.12047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McKimm-Breschkin JL, Barrett S, Pudjiatmoko Azhar M, Wong FY, Selleck P, Mohr PG, McGrane J, Kim M. 2013. I222 neuraminidase mutations further reduce oseltamivir susceptibility of Indonesian clade 2.1 highly pathogenic avian influenza A(H5N1) viruses. PLoS One 8:e66105. doi: 10.1371/journal.pone.0066105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van der Vries E, Collins PJ, Vachieri SG, Xiong X, Liu J, Walker PA, Haire LF, Hay AJ, Schutten M, Osterhaus AD, Martin SR, Boucher CA, Skehel JJ, Gamblin SJ. 2012. H1N1 2009 pandemic influenza virus: resistance of the I223R neuraminidase mutant explained by kinetic and structural analysis. PLoS Pathog 8:e1002914. doi: 10.1371/journal.ppat.1002914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Huang L, Cao Y, Zhou J, Qin K, Zhu W, Zhu Y, Yang L, Wang D, Wei H, Shu Y. 2014. A conformational restriction in the influenza A virus neuraminidase binding site by R152 results in a combinational effect of I222T and H274Y on oseltamivir resistance. Antimicrob Agents Chemother 58:1639–1645. doi: 10.1128/AAC.01848-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pizzorno A, Abed Y, Bouhy X, Beaulieu E, Mallett C, Russell R, Boivin G. 2012. Impact of mutations at residue I223 of the neuraminidase protein on the resistance profile, replication level, and virulence of the 2009 pandemic influenza virus. Antimicrob Agents Chemother 56:1208–1214. doi: 10.1128/AAC.05994-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Baz M, Abed Y, McDonald J, Boivin G. 2006. Characterization of multidrug-resistant influenza A/H3N2 viruses shed during 1 year by an immunocompromised child. Clin Infect Dis 43:1555–1561. doi: 10.1086/508777. [DOI] [PubMed] [Google Scholar]
- 59.Simon P, Holder BP, Bouhy X, Abed Y, Beauchemin CA, Boivin G. 2011. The I222V neuraminidase mutation has a compensatory role in replication of an oseltamivir-resistant influenza virus A/H3N2 E119V mutant. J Clin Microbiol 49:715–717. doi: 10.1128/JCM.01732-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Duan S, Govorkova EA, Bahl J, Zaraket H, Baranovich T, Seiler P, Prevost K, Webster RG, Webby RJ. 2014. Epistatic interactions between neuraminidase mutations facilitated the emergence of the oseltamivir-resistant H1N1 influenza viruses. Nat Commun 5:5029. doi: 10.1038/ncomms6029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Burnham AJ, Armstrong J, Lowen AC, Webster RG, Govorkova EA. 2015. Competitive fitness of influenza B viruses with neuraminidase inhibitor-resistant substitutions in a co-infection model of the human airway epithelium. J Virol 89:4575−4587. doi: 10.1128/JVI.02473-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Burnham AJ, Baranovich T, Marathe BM, Armstrong J, Webster RG, Govorkova EA. 2014. Fitness costs for influenza B viruses carrying neuraminidase inhibitor-resistant substitutions: underscoring the importance of E119A and H274Y. Antimicrob Agents Chemother 58:2718–2730. doi: 10.1128/AAC.02628-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.World Health Organization. 2012. Meetings of the WHO working group on surveillance of influenza antiviral susceptibility—Geneva, November 2011 and June 2012. Wkly Epidemiol Rec 87:369–374. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.