Abstract
Introduction. Sleep disturbances are commonly found in patients in the postoperative period. Sleep disturbances may give rise to several complications including cardiopulmonary instability, transient cognitive dysfunction and prolonged convalescence. Many factors including host inflammatory responses are believed to cause postoperative sleep disturbances, as inflammatory responses can alter sleep architecture through cytokine-brain interactions. Our aim was to investigate alteration of sleep architecture during acute infection and its relationships to inflammation and clinical symptoms.
Materials & Methods. In this observational study, we included patients with acute uncomplicated diverticulitis as a model to investigate the isolated effects of inflammatory responses on sleep. Eleven patients completed the study. Patients were admitted and treated with antibiotics for two nights, during which study endpoints were measured by polysomnography recordings, self-reported discomfort scores and blood samples of cytokines. One month later, the patients, who now were in complete remission, were readmitted and the endpoints were re-measured (the baseline values).
Results. Total sleep time was reduced 4% and 7% the first (p = 0.006) and second (p = 0.014) nights of diverticulitis, compared to baseline, respectively. The rapid eye movement sleep was reduced 33% the first night (p = 0.016), compared to baseline. Moreover, plasma IL-6 levels were correlated to non-rapid eye movement sleep, rapid eye movement sleep and fatigue.
Conclusion. Total sleep time and rapid eye movement sleep were reduced during nights with active diverticulitis and correlated with markers of inflammation.
Keywords: Rapid eye movement, Polysomnography, Diverticulitis, Cytokines, Infection, Inflammation, Sleep
Introduction
Subjective and objective sleep disturbances are commonly found after major surgery (Gogenur et al., 2009; Kain & Caldwell-Andrews, 2003; Madsen, Rosenberg & Gogenur, 2013; Rosenberg, 2001). Several studies have demonstrated reduction or abolishment of slow-wave sleep (SWS) and rapid eye movement (REM) sleep during the first nights of sleep after surgery (Gogenur, Wildschiotz & Rosenberg, 2008; Hansen et al., 2013; Krenk, Jennum & Kehlet, 2012; Rosenberg et al., 1994). Sleep disturbances may give rise to several complications including cardiopulmonary instability, cardiac morbidity, transient cognitive dysfunction, inflammation, prolonged convalescence, fatigue, and hyperalgesia (Chouchou et al., 2014; Cremeans-Smith et al., 2006; Krenk, Rasmussen & Kehlet, 2010; Mullington et al., 2009; Rosenberg, 2001).
Many factors may influence postoperative sleep: discomfort including pain, use of drugs including opioids, nursing environments, psychological factors, effects of general anesthesia, and the surgical trauma itself (Chouchou et al., 2014; Rosenberg, 2001). Surgical trauma may lead to activations of metabolic, endocrine and inflammatory responses (Rosenberg-Adamsen et al., 1996), the surgical stress response. Sleep architecture can be altered by certain cytokines (IL-1β, TNF-α and IL-6) that are key mediators in the host inflammatory response (Pollmacher et al., 2000). This same universal host inflammatory response is also occurring during infections and after surgical trauma (Rosenberg-Adamsen et al., 1996). However, the isolated effect of this inflammatory response on sleep in a clinical population without surgery and general anesthesia has never before been investigated.
Our hypothesis was therefore that sleep architecture is altered during acute inflammation (diverticulitis), and the changes would correlate to level of circulating inflammatory cytokines. The aim of the present study was to report the sleep architecture in the course of acute uncomplicated colonic diverticulitis and investigate the relationship between acute inflammation, sleep disturbances, and subjective discomfort.
Materials & Methods
All patients were enrolled after giving written informed consent and the study was approved by the Ethics Committee of Capital Region of Denmark (ref: H-1-2012-155) and the Danish Data Protection Agency. The study was registered on www.clinicaltrials.gov (ref: NCT01840852).
We included patients between the age of 18 and 75 years, with The American Society of Anesthesiologists (ASA) Physical Status Classification I–III, and with a CT-scan confirming acute uncomplicated diverticulitis (Hansen and Stock stage I) (Klarenbeek et al., 2012). The onset of lower abdominal pain and fever had to be within 72 h prior to admission. The exclusion criteria were patients with diverticulitis requiring surgical intervention, complicated diverticular disease (fistula or abscess), onset of symptoms more than 3 days from inclusion, recent history (up to 3 months) of surgical intervention, myocardial infarction or arrhythmia, autoimmune diseases (Inflammatory bowel disease, lupus, multiple sclerosis), sleep disorders including obstructive sleep apnea, night shift professions, daily use of opioids, psychoactive drugs, or hypnotics, psychiatry disorders, daily consumption of more than 50 g of alcohol, diabetes mellitus, predicted poor compliance (language difficulties, etc.), pregnancy or nursing, urinary or fecal incontinence, severe kidney disease, or current cancer. Furthermore, sleep quality was screened with the Pittsburgh Sleep Quality Index (PSQI) to exclude any poor sleepers (PSQI > 5) (Buysse et al., 1989).
The study was composed of three nights of sleep monitoring in total, all from 2300 h (h) (lights out) to 0700 h (lights on) in a private room. After two successive nights of sleep monitoring, named study night 1 (S1) and study night 2 (S2), patients continued their treatment according to standard treatment guidelines for the department. Patients were re-admitted at 30 days after study night 1 to attend the last study night 3 (S3). In cases of relapse or failure of treatment during these periods, the patient was excluded. Patients were prohibited from intake of stimulating beverages or alcohol during the day of the study nights. Prior to lights out, light intensity in the room with all light sources off was measured with a luxmeter (Elma 1335 Luxmeter, Elma, Greve, Denmark), and only a level below 10 lux was acceptable. The blood samples were collected at 2230 h followed by administration of self-reported discomfort scales.
Polysomnography was performed with a portable recording unit (Embla titanium, Natus Medical Incorporated, San Carlos, California, USA). Continuous recording from 2300 h to 0700 h was made by using four-channel bipolar electroencephalography, EEG, (C4-M1, C3-M2, O2-M1, O1-M2), two-channel electrooculography, EOG, and two-channel electromyography (submental). Reusable 10 mm gold cup electrodes (Natus Medical Incorporated, San Carlos, California, USA) were applied for EEG, and single use self-adhesive electrodes were applied for EOG and EMG (Ambu® Neuroline 720, Ballerup, Copenhagen, Denmark). All electrodes were placed in accordance to The American Academy of Sleep Medicine (AASM) Manual for the Scoring of Sleep and Associated Events 2007 and the skin was prepared with light abrasion and alcohol swaps before electrode fixation. Sleep staging was performed in accordance to The AASM Manual for the Scoring of Sleep and Associated Events 2007. Staging was performed by one experienced, trained scorer blinded to study nights using the software Remlogic 3.2 (Natus Medical Incorporated, San Carlos, California, USA). Sleep recordings were staged in epochs of 30 s as either N1 (stage 1 sleep), N2 (stage 2 sleep), N3 (stage 3 sleep), REM (REM sleep) or W (awake). All other sleep parameters were calculated on the basis of these sleep stages. Total sleep time (TST) summed up the time spent across all sleep stages, while sleep onset (SO) summed up the time spent in wake stage before the first sleep stage. Wake after sleep onset (WASO) summed up the time spent awake after sleep onset and before final awakening. Lastly, number of awakening (NOA) showed the number awakening from any sleep stages.
Subjective measures concerning discomfort were administered 10 min before lights out, including 100-mm visual analogue scale (VAS) of pain at rest and pain during movements (0 mm = no pain and 100 mm = worst pain imaginable), a 9-point Karolinska Sleepiness Scale (KSS) ranging from extremely alert (= score 1) to fighting sleep (= score 9) (Akerstedt & Gillberg, 1990). Fatigue and malaise were measured in VAS of overall fatigue (0 mm = no sense of fatigue and 100 = worst fatigue imaginable) and general well-being (0 mm = extremely well and 100 = extreme malaise), respectively. Lastly, a 100-mm VAS of poor sleep quality (0 mm = best sleep and 100 mm = worst sleep imaginable) was also administered in the following morning to assess self-reported sleep quality.
At 2230 h blood samples were taken. The plasma was extracted and then stored at −80 degree Celsius until analysis. Tumor necrosis factor alpha (TNF-α), interleukin-1 beta (IL-1β), interleukin-2 (IL-2), interleukin-6 (IL-6), and interleukin-10 (IL-10) were measured in a Luminex 100 IS analyzer (Luminex Corporation, Austin, TX, USA) using appropriate multiplex antibody bead kits purchased from Invitrogen (Invitrogen Corporation, Carlsbad, CA, USA). Data were analyzed using StarStation version 2.0 software (Applied Cytometry Systems, Sheffield, UK). The lower levels of detection were as followed (in picogram/milliliter): TNF-α: 0.7, IL-1β: 0.4, IL-2: 2.8 IL-6: 0.2, IL-10: 0.4.
REM sleep time was the primary endpoint of this study, while the secondary endpoints included other sleep data, scores of self-reported discomfort and levels of circulating cytokines. We assumed that REM sleep duration was approximately 70 min for healthy subjects between the ages of 40 to 50 with a standard deviation of 30 min (Ohayon et al., 2004). A 25% reduction of REM sleep between study nights 1 and 3 was considered as of clinical importance. It was estimated that 11 patients were needed, when a two-sided significance level of 5% and a power of 0.90 were applied. Wilcoxon’s signed-rank test was used for all data (sleep data, self-reported discomfort scores and cytokine levels) as paired analyses between S1 and S3, and S2 and S3. Spearman’s correlation was used to analyze the correlations between changes in sleep stages (as per cent of total sleep time) and changes in cytokine levels from S1 to S3 and from S2 to S3. The correlations estimated were the differences, rather than the absolute values, between these measurements. The correlations were also calculated between changes in self-reported discomfort scores and changes in sleep stages, as well as changes in cytokine levels and changes in self-reported discomfort scores. All data were presented as medians and ranges or quartiles. IBM SPSS Statistics for Windows, Version 20.0 (Armonk, NY: IBM Corp.) was used to carry out the calculations. The level of statistical significance was set to 0.05.
Results
Thirteen patients were enrolled, 11 completed the study, and two were excluded, one due to recurrence of diverticulitis, and one due to technical failure of the PSG recordings. Characteristics of patients, diverticular disease and analgesics consumption are presented in Table 1. All 11 patients were treated with oral or intravenous antibiotics according to standard routines and oral paracetamol, if required also ibuprofen, during their admission.
Table 1. Characteristics of patients with acute diverticulitis and their analgesics consumption.
| Subject characteristics | ||
| Sex (male/female), n | 5/6 | |
| Age (years), median | 52 | (20–74) |
| ASA (I/II/III), n | 11/0/0 | |
| Body Mass Index (BMI), median | 28 | (20–39) |
| Pittsburgh Sleep Quality Index (PSQI), median | 4 | (2–5) |
| Smokers, n | 2 | |
| Nicotine replacement therapy, n | 0 | |
| Disease characteristics | ||
| Pain debut (hours), median | 48 | (24–72) |
| Temperature at admission (°C), median | 37.8 | (36.9–39.1) |
| Hansen and Stock stagea (0/I/II/III), n | 0/11/0/0 | |
| Cancer found with endoscopy 30 days after admission, n | 0 | |
| C-reactive protein level at admission (mg/l), median | 94 | (33–190) |
| Analgesics administered | ||
| Paracetamol, n | 11 | |
| Ibuprofen, n | 2 | |
| Morphine, n | 0 |
Notes.
Values are median and range. Stages I to III refer to increasing severity of diverticulitis. Stage I refers to acute uncomplicated diverticulitis, stage II refers to acute complicated diverticulitis and stage III refers to chronic recurrent diverticulitis. ASA, American Society of Anesthesiologists.
Hansen and Stock staging of diverticulitis is a clinical classification that also accounts for asymptomatic diverticulosis (stage 0) (Klarenbeek et al., 2012).
All sleep data are presented in Table 2. TST values were significantly reduced from 391 min (median value) at S3 to 361 min and 374 min at S1 and S2, respectively. REM sleep was significantly diminished from 90 at S1 to 60 at S3. No changes in other sleep stages (N1, N2 or N3) were statistically significant. Wake time was, in contrast, significantly increased from 89 min at S1 to 119 min and 106 min, at S1 and S2, respectively. Wake time after sleep onset (WASO) was also extended from 50 min at S1 to 78 min and 86 min at S1 and S2, respectively. There was no statistical difference in number of awakenings between the study nights. Due to the risk of first night effect, post hoc paired analysis of TST, wake time and WASO between S1 and S2 were performed and showed no differences (W: p = 0.859, TST: p = 0.859, WASO: p = 0.533).
Table 2. Sleep parameters of patients with acute diverticulitis both during nights of the disease and during remission night.
Values are medians and interquartile ranges in the brackets. P-values for Wilcoxon’s signed rank test for study nights during diverticulitis compared to remission night (study night 3).
| Study night 1 | Study night 2 | Study night 3 | |||
|---|---|---|---|---|---|
| Median | p-value | Median | p-value | Median | |
| N1 (min) | 28 (24–40) | 0.169 | 39 (32–51) | 0.722 | 40 (32–52) |
| N2 (min) | 185 (122–199) | 0.477 | 147 (138–161) | 0.424 | 165 (146–191) |
| N3 (min) | 88 (73–102) | 0.423 | 83 (50–103) | 0.477 | 87 (74–101) |
| Non REM (min) | 285 (242–317) | 0.091 | 284 (264–290) | 0.062 | 293 (286–323) |
| REM (min) | 60 (42–84) | 0.016 | 73 (47–92) | 0.068 | 90 (76–112) |
| W (min) | 119 (92–184) | 0.006 | 106 (94–155) | 0.014 | 89 (61–109) |
| Sleep onset (min) | 39 (26–47) | 0.248 | 26 (19–34) | 0.594 | 29 (15–52) |
| WASO (min) | 78 (55–142) | 0.005 | 86 (68–120) | 0.003 | 50 (28–68) |
| Awakening (number) | 19 (17–27) | 0.266 | 24 (23–29) | 0.305 | 26 (19–31) |
| TST (min) | 361 (297–388) | 0.006 | 374 (326–386) | 0.014 | 391 (371–419) |
| N1 of TST (%) | 9.9 (6.0–12.5) | 0.858 | 11.5 (8.5–14.1) | 0.514 | 9.3 (7.7–14.5) |
| N2 of TST (%) | 47.4 (39.5–54.1) | 0.398 | 45.3 (37.1–52.8) | 0.449 | 42.8 (38.8–45.5) |
| N3 of TST (%) | 22.1 (19.5–27.5) | 0.929 | 23.8 (18.5–26.8) | 0.610 | 21.9 (19.5–26.1) |
| NREM of TST (%) | 82.5 (76.5–87.5) | 0.032 | 80.6 (75.5–86.5) | 0.139 | 75.5 (72.5–78.0) |
| REM of TST (%) | 17.5 (12.5–23.5) | 0.036 | 19.4 (13.5–24.5) | 0.139 | 24.5 (22.0–27.6) |
Notes.
- Nx
- stage x sleep
- REM
- rapid eye movement sleep
- W
- wake time
- WASO
- wake after sleep onset
- TST
- total sleep time
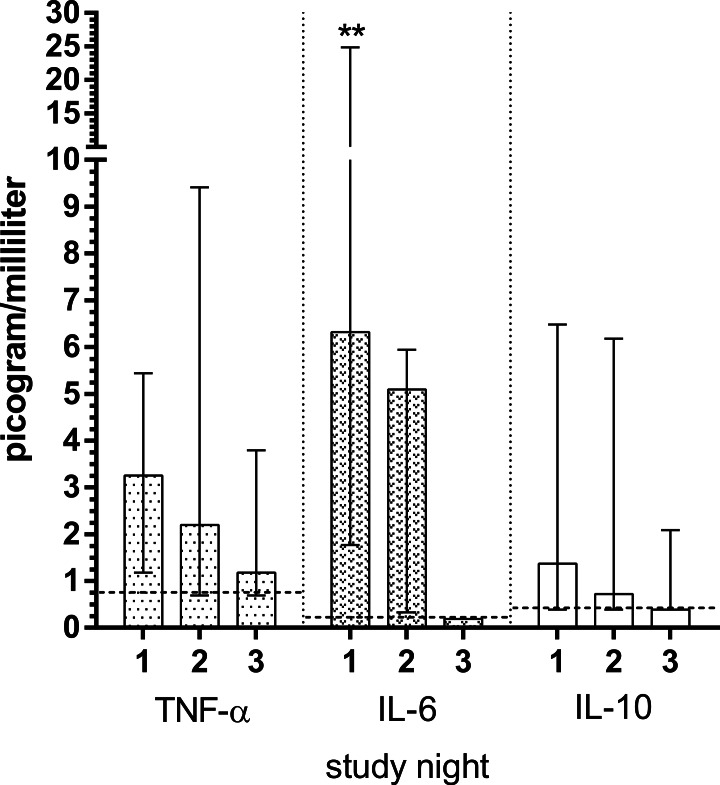
Cytokine levels are depicted in Fig. 1. Vast majority of IL-1β and IL-2 measurements were found below the detection thresholds, therefore they were excluded from further analysis. IL-6 levels were significantly decreased from 6.3 picogram/milliliter (median) at S1 to 5.1 picogram / milliliter at S2 (p = 0.008). IL-6 levels was reduced to 0.2 (p = 0.051) at S3, but without statistical significance. IL-10 (p = 0.128 for both nights versus S3) and TNF-α (p = 0.103 for S1, p = 0.314 for S2) levels were decreased over study nights, however, without statistical significance.
Figure 1. Plasma concentrations of cytokines in patients with acute diverticulitis both during nights of the disease and during remission night.
Significant differences between the nights of the disease and remission night were calculated using Wilcoxon’s signed rank test and are indicated with ∗p < 0.05, ∗∗p < 0.01. The horizontal broken lines indicate the detection thresholds for the individual cytokines. The whiskers depict interquartile range. The cytokines measured include: IL-10, interleukin 10; IL-6, interleukin 6; TNF-α, tumor necrosis factor alpha.
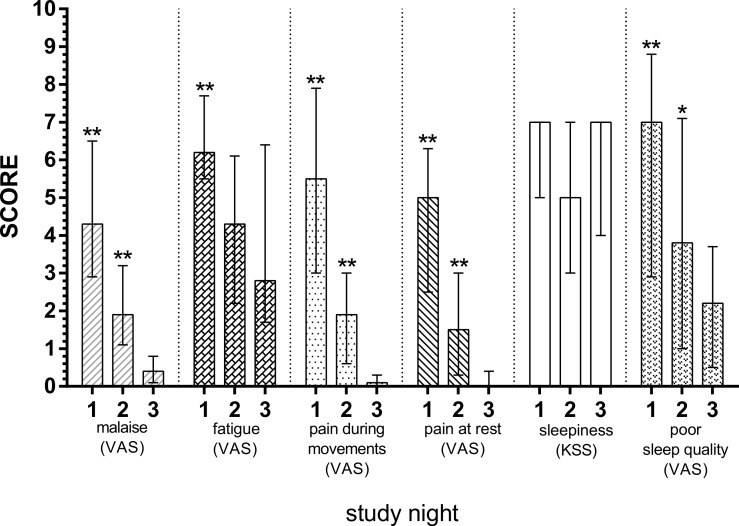
Subjective discomfort scores are depicted in Fig. 2. Malaise (p = 0.003, p = 0.005), pain during movements (p = 0.005, p = 0.005), resting pain (p = 0.003, p = 0.008) and poor sleep quality (p = 0.003, p = 0.041) were significantly diminished at S1 and S2 compared with S3. The fatigue was also diminished, however only with statistical significance from S1 to S3 (p = 0.006), but not from S2 to S3 (p = 0.374). Lastly, no significant differences were found for sleepiness for both nights (p = 0.892, p = 0.619, respectively).
Figure 2. Subjective discomfort scores in patients with acute diverticulitis both during nights of the disease and during remission night.
Significant differences between the nights of the disease and remission night were calculated using Wilcoxon’s signed rank test and are indicated with ∗p < 0.05, ∗∗p < 0.01. The whiskers depict interquartile range. Apart from sleepiness, which was measured with KSS, Karolinska Sleepiness Scale; remaining discomfort domains were measured with VAS, visual analogue scale.
Since the vast majority of IL-1β and IL-2 measurements were below the detection limits, they were excluded from correlation analyses. The correlations between cytokine levels and sleep stages are stated in Table 3. We found significant associations in changes in IL-6 levels and changes in sleep stages as percentage of TST from both S1 and S2 to S3. There were strong correlations between IL-6 and REM (S1: r = − 0.68, p = 0.02 and S2: r = − 0.67, p = 0.03) and NREM (S1: r = 0.68, p = 0.02 and S2: r = 0.67, p = 0.03). In addition, a moderate correlation between IL-6 and N2 (S1: r = 0.60, p = 0.05 and S2: r = 0.63, p = 0.04) was found. We did not find any significant correlations between changes in self-reported discomfort and changes in sleep stages; however, we did find a positive correlation between changes in fatigue and IL-6 levels from S1 to S3 (r = 0.61, p = 0.05). No other significant associations were found between changes in discomfort and changes in cytokine levels.
Table 3. Correlation cross table for changes in sleep stages and cytokine levels.
The changes for study night 1 were defined as values of study night 1 minus study night 3 (remission night), and for study night 2 it was values of study night 2 minus study night 3. Significant correlations are presented in bold. Values are correlation coefficients and the corresponding p-values.
| ↑ Non REM | ↑ REM | ↑ N1 | ↑ N2 | ↑ N3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Night 1 | Night 2 | Night 1 | Night 2 | Night 1 | Night 2 | Night 1 | Night 2 | Night 1 | Night 2 | ||
| ↑ IL-6 | Correlation | 0.68 | 0.67 | −0.68 | −0.67 | −0.18 | −0.48 | 0.60 | 0.63 | −0.24 | −0.18 |
| p-value | 0.02 | 0.03 | 0.02 | 0.03 | 0.60 | 0.14 | 0.05 | 0.04 | 0.47 | 0.61 | |
| ↑ IL-10 | Correlation | 0.04 | 0.36 | −0.04 | −0.36 | 0.24 | 0.17 | −0.21 | 0.12 | 0.22 | −0.03 |
| p-value | 0.91 | 0.28 | 0.91 | 0.28 | 0.48 | 0.62 | 0.53 | 0.72 | 0.51 | 0.93 | |
| ↑ TNF-α | Correlation | −0.26 | 0.13 | 0.26 | −0.13 | −0.04 | 0.40 | −0.18 | 0.03 | 0.30 | −0.08 |
| p-value | 0.43 | 0.71 | 0.43 | 0.71 | 0.90 | 0.22 | 0.59 | 0.93 | 0.38 | 0.83 | |
Notes.
- REM
- rapid eye movement sleep
- Nx
- stage x sleep
- IL-x
- interleukinx
- TNF
- tumor necrosis factor
Discussion
We used acute uncomplicated diverticulitis as a model to investigate the effects of inflammatory responses on sleep and found that TST was consistently reduced at both study nights with diverticulitis (S1 and S2) due to increased W and WASO, and that REM sleep was decreased at S1. We also found that subjective discomfort scores were increased except sleepiness at both diverticulitis nights. Lastly, we found a significant increase in IL-6 levels during the study nights during which the patients had diverticulitis, and this increase was correlated to changes in NREM sleep (including N2 sleep), REM sleep, and fatigue scores.
Suppression of REM sleep and promotion of WASO and NREM sleep found in this study are similar to findings observed in clinical polysomnography studies of patients with infections such as early stage HIV infection and acute rhinovirus infection (Opp, 2009). In addition, sleep studies using endotoxin have been performed in healthy humans (Pollmacher et al., 2000), showing increased wake time, NREM sleep and decreased REM sleep after endotoxin administration (Mullington et al., 2000; Trachsel et al., 1994). In addition, the endotoxin-induced IL-6 elevation was positively correlated with REM latency, N2 sleep and wake time, and negatively correlated with REM sleep (Pollmacher et al., 1993). The reducing effect of REM sleep on IL-6 levels has also been demonstrated in another study (Spath-Schwalbe et al., 1998). One cross-sectional study has shown that levels of circulating IL-6 within normal ranges are significantly correlated to sleep architecture (increase of REM latency and WASO) when demographical variations were controlled (Hong et al., 2005). These findings are consistent with the associations we found in the present study, and further support the growing evidences of the sleep regulating roles of pro-inflammatory cytokines (Bryant, Trinder & Curtis, 2004). So far, evidence suggests that IL-6 can act directly on the central nervous system (Imeri & Opp, 2009), including activation of the hypothalamic-pituitary-adrenal axis (HPA-axis), to exert its effect on sleep regulation (Gomez-Gonzalez et al., 2012). Furthermore, studies have shown that inhibition of the IL-6 receptor by tocilizumab can alleviate sleep disturbances and fatigue in patients with rheumatoid arthritis (Rohleder, Aringer & Boentert, 2012; Thomas et al., 2011).
The elevated levels of plasma IL-6 found in the current study are coherent with findings in recent clinical studies investigating IL-6 levels during the course of acute diverticulitis and other abdominal infections (Elsing, Ernst & Stremmel, 2012; Rivera-Chavez et al., 2003). However, IL-1β and IL-2 levels were not elevated or detectable at all. This discrepancy has previously been observed in patients with acute pancreatitis and appendicitis (Brivet, Emilie & Galanaud, 1999; Rivera-Chavez et al., 2003). It is possible in the current study that levels of IL-1β and IL-2 may have peaked before the blood sampling, and the cytokines were already bound by high level of endogenous soluble receptors (Brivet, Emilie & Galanaud, 1999).
Compared to postoperative sleep disturbances (Rosenberg, 2001), REM sleep suppression found in our study was less prominent (33%). SWS and REM sleep are most often absent (100% reduction) during the first nights after major non-cardiac surgery (Rosenberg, 2001). In the postoperative period, pain and disturbing hospital environment (noise and staffs) are likely to cause awakenings during the night (Rosenberg, 2001), while opioids for pain relief can reduce SWS and REM sleep (Shaw et al., 2005). In recent years, more major surgeries have been performed with fast track regimes, in which perioperative care has been optimized with multimodal opioid-sparing analgesia and early hospital discharge (home environment) (Kehlet, 2008). Despite these efforts, REM sleep in the first postoperative night is still greatly reduced (62–92%) (Dette et al., 2013; Hansen et al., 2013; Krenk, Jennum & Kehlet, 2012). One randomized trial also demonstrated that even when opioids were avoided and pain was well managed, REM sleep was still abolished after major surgery (Cronin et al., 2001). In contrast, minor or less invasive surgery, such as laparoscopic surgery, only causes transient SWS reduction (46%), leaving REM sleep unaffected (Rosenberg, 2001). These findings may indicate that the magnitude of the surgical trauma, including the inflammatory response, plays a greater role in the postoperative sleep disturbances, compared to pain and opioid usage. Laparoscopic procedures cause less trauma and inflammatory response, manifested by CRP, IL-6, and TNF-α compared to major surgery (Akhtar et al., 1998; Braga et al., 2002), and therefore only causing a transient shift from SWS sleep to shallow NREM sleep.
Our study has some limitations. Patients were only mildly affected by their disease, and the magnitude of inflammation was therefore low, yet enough eliciting elevation of cytokines, C-reactive protein and body temperature. In our institution, these cases were treated with antibiotics and paracetamol, and to our knowledge, these drugs will not cause any (REM) sleep alteration. Due to the nature of the acute diverticulitis, the investigated periods (S1 and S2) of host inflammatory response were most likely not exactly synchronized amongst the patients. We did, however, only include patients with pain onset less than 72 h prior to the admission and inflammation in the diverticula proven by CT-imaging and elevated C-reactive protein. Therefore, the inflammatory response was present during the first study night, but the magnitude of this response could still vary between the patients, and so could their recovery rate due to the disease states and age differences (Ottinger et al., 2014). These uncertainties were attempted to be dealt with using paired observations, where each patient was its own control, thus allowing for differences in baseline values between the patients.
First night effect refers to reduction of TST and increase of wake time and WASO due to exposure to unfamiliar sleep environment (Toussaint et al., 1995). We did not find any significant changes in these sleep parameters between S1 and S2.
Two of the included patients were active smokers, who due to hospitalization (smoking prohibition) might have smoked lesser during the study sessions. None of the included patients reported changes in their smoking status during the entire course of the study. Epidemiological studies suggested that cigarette smoking was associated with difficulty in sleep initiation (increased sleep latency) and maintenance (Wetter & Young, 1994; Zhang et al., 2006). Therefore it is counter-intuitive that the sleep latency and awakenings after sleep onset were reducing from S1 to S3 for both patients in the current study. In addition, our main finding, approximately 30% REM-sleep reduction, cannot be explained by cigarette smoking (Zhang et al., 2006). The nature of our findings was, however, in line with an immune response mediated sleep disturbance (Spath-Schwalbe et al., 1998).
Conclusion
In conclusion, we found substantial sleep disturbances and subjective complaints in relation to acute uncomplicated diverticulitis. Inflammatory parameters correlated to sleep stages and subjective complaints.
Supplemental Information
Some sleep parameters, such as Total Sleep Time, are not included in the Raw dataset, because they are calculated from the raw sleep data. E.g. Total Sleep Time = sum of time spent in all four stages of sleep.
Funding Statement
This work was supported by grants from The Lundbeck Foundation (Denmark). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Chenxi Huang conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Mahdi Alamili and Claus Henrik Nielsen analyzed the data, contributed reagents/materials/analysis tools, reviewed drafts of the paper.
Jacob Rosenberg and Ismail Gögenur conceived and designed the experiments, analyzed the data, contributed reagents/materials/analysis tools, reviewed drafts of the paper.
Human Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
The Ethics Committee of Capital Region of Denmark, approval number: H-1-2012-155.
References
- Akerstedt & Gillberg (1990).Akerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. International Journal of Neuroscience. 1990;52:29–37. doi: 10.3109/00207459008994241. [DOI] [PubMed] [Google Scholar]
- Akhtar et al. (1998).Akhtar K, Kamalky-asl ID, Lamb WR, Laing I, Walton L, Pearson RC, Parrott NR. Metabolic and inflammatory responses after laparoscopic and open inguinal hernia repair. Annals of the Royal College of Surgeons of England. 1998;80:125–130. [PMC free article] [PubMed] [Google Scholar]
- Braga et al. (2002).Braga M, Vignali A, Zuliani W, Radaelli G, Gianotti L, Martani C, Toussoun G, Di Carlo V. Metabolic and functional results after laparoscopic colorectal surgery: a randomized, controlled trial. Diseases of the Colon and Rectum. 2002;45:1070–1077. doi: 10.1007/s10350-004-6362-2. [DOI] [PubMed] [Google Scholar]
- Brivet, Emilie & Galanaud (1999).Brivet FG, Emilie D, Galanaud P. Pro- and anti-inflammatory cytokines during acute severe pancreatitis: an early and sustained response, although unpredictable of death. Parisian study group on acute pancreatitis. Critical Care Medicine. 1999;27:749–755. doi: 10.1097/00003246-199904000-00029. [DOI] [PubMed] [Google Scholar]
- Bryant, Trinder & Curtis (2004).Bryant PA, Trinder J, Curtis N. Sick and tired: does sleep have a vital role in the immune system? Nature Reviews: Immunology. 2004;4:457–467. doi: 10.1038/nri1369. [DOI] [PubMed] [Google Scholar]
- Buysse et al. (1989).Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Chouchou et al. (2014).Chouchou F, Khoury S, Chauny JM, Denis R, Lavigne GJ. Postoperative sleep disruptions: a potential catalyst of acute pain? Sleep Medicine Reviews. 2014;18:253–262. doi: 10.1016/j.smrv.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Cremeans-Smith et al. (2006).Cremeans-Smith JK, Millington K, Sledjeski E, Greene K, Delahanty DL. Sleep disruptions mediate the relationship between early postoperative pain and later functioning following total knee replacement surgery. Journal of Behavioral Medicine. 2006;29:215–222. doi: 10.1007/s10865-005-9045-0. [DOI] [PubMed] [Google Scholar]
- Cronin et al. (2001).Cronin AJ, Keifer JC, Davies MF, King TS, Bixler EO. Postoperative sleep disturbance: influences of opioids and pain in humans. Sleep. 2001;24:39–44. doi: 10.1093/sleep/24.1.39. [DOI] [PubMed] [Google Scholar]
- Dette et al. (2013).Dette F, Cassel W, Urban F, Zoremba M, Koehler U, Wulf H, Graf J, Steinfeldt T. Occurrence of rapid eye movement sleep deprivation after surgery under regional anesthesia. Anesthesia and Analgesia. 2013;116:939–943. doi: 10.1213/ANE.0b013e3182860e58. [DOI] [PubMed] [Google Scholar]
- Elsing, Ernst & Stremmel (2012).Elsing C, Ernst S, Stremmel W. Value of lipopolysaccharide binding protein, interleukin-6 and C-reactive protein as biomarkers of severity in acute diverticulitis: a prospective study. Clínica y Laboratorio. 2012;58:145–151. [PubMed] [Google Scholar]
- Gogenur et al. (2009).Gogenur I, Bisgaard T, Burgdorf S, Van Someren E, Rosenberg J. Disturbances in the circadian pattern of activity and sleep after laparoscopic versus open abdominal surgery. Surgical Endoscopy. 2009;23:1026–1031. doi: 10.1007/s00464-008-0112-9. [DOI] [PubMed] [Google Scholar]
- Gogenur, Wildschiotz & Rosenberg (2008).Gogenur I, Wildschiotz G, Rosenberg J. Circadian distribution of sleep phases after major abdominal surgery. British Journal of Anaesthesia. 2008;100:45–49. doi: 10.1093/bja/aem340. [DOI] [PubMed] [Google Scholar]
- Gomez-Gonzalez et al. (2012).Gomez-Gonzalez B, Dominguez-Salazar E, Hurtado-Alvarado G, Esqueda-Leon E, Santana-Miranda R, Rojas-Zamorano JA, Velazquez-Moctezuma J. Role of sleep in the regulation of the immune system and the pituitary hormones. Annals of the New York Academy of Sciences. 2012;1261:97–106. doi: 10.1111/j.1749-6632.2012.06616.x. [DOI] [PubMed] [Google Scholar]
- Hansen et al. (2013).Hansen MV, Madsen MT, Wildschiodtz G, Rosenberg J, Gogenur I. Sleep disturbances and changes in urinary 6-sulphatoxymelatonin levels in patients with breast cancer undergoing lumpectomy. Acta Anaesthesiologica Scandinavica. 2013;57:1146–1153. doi: 10.1111/aas.12157. [DOI] [PubMed] [Google Scholar]
- Hong et al. (2005).Hong S, Mills PJ, Loredo JS, Adler KA, Dimsdale JE. The association between interleukin-6, sleep, and demographic characteristics. Brain, Behavior, and Immunity. 2005;19:165–172. doi: 10.1016/j.bbi.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Imeri & Opp (2009).Imeri L, Opp MR. How (and why) the immune system makes us sleep. Nature Reviews: Neuroscience. 2009;10:199–210. doi: 10.1038/nrn2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kain & Caldwell-Andrews (2003).Kain ZN, Caldwell-Andrews AA. Sleeping characteristics of adults undergoing outpatient elective surgery: a cohort study. Journal of Clinical Anesthesia. 2003;15:505–509. doi: 10.1016/j.jclinane.2003.02.002. [DOI] [PubMed] [Google Scholar]
- Kehlet (2008).Kehlet H. Fast-track colorectal surgery. Lancet. 2008;371:791–793. doi: 10.1016/S0140-6736(08)60357-8. [DOI] [PubMed] [Google Scholar]
- Klarenbeek et al. (2012).Klarenbeek BR, De Korte N, Van der Peet DL, Cuesta MA. Review of current classifications for diverticular disease and a translation into clinical practice. International Journal of Colorectal Disease. 2012;27:207–214. doi: 10.1007/s00384-011-1314-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krenk, Jennum & Kehlet (2012).Krenk L, Jennum P, Kehlet H. Sleep disturbances after fast-track hip and knee arthroplasty. British Journal of Anaesthesia. 2012;109:769–775. doi: 10.1093/bja/aes252. [DOI] [PubMed] [Google Scholar]
- Krenk, Rasmussen & Kehlet (2010).Krenk L, Rasmussen LS, Kehlet H. New insights into the pathophysiology of postoperative cognitive dysfunction. Acta Anaesthesiologica Scandinavica. 2010;54:951–956. doi: 10.1111/j.1399-6576.2010.02268.x. [DOI] [PubMed] [Google Scholar]
- Madsen, Rosenberg & Gogenur (2013).Madsen MT, Rosenberg J, Gogenur I. Actigraphy for measurement of sleep and sleep-wake rhythms in relation to surgery. Journal of Clinical Sleep Medicine. 2013;9:387–394. doi: 10.5664/jcsm.2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullington et al. (2000).Mullington J, Korth C, Hermann DM, Orth A, Galanos C, Holsboer F, Pollmacher T. Dose-dependent effects of endotoxin on human sleep. American Journal of Physiology: Regulatory, Integrative and Comparative Physiology. 2000;278:R947–R955. doi: 10.1152/ajpregu.2000.278.4.R947. [DOI] [PubMed] [Google Scholar]
- Mullington et al. (2009).Mullington JM, Haack M, Toth M, Serrador JM, Meier-Ewert HK. Cardiovascular, inflammatory, and metabolic consequences of sleep deprivation. Progress in Cardiovascular Diseases. 2009;51:294–302. doi: 10.1016/j.pcad.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohayon et al. (2004).Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- Opp (2009).Opp MR. Sleep and psychoneuroimmunology. Immunology and Allergy Clinics of North America. 2009;29:295–307. doi: 10.1016/j.iac.2009.02.009. [DOI] [PubMed] [Google Scholar]
- Ottinger et al. (2014).Ottinger ME, Monaghan SF, Gravenstein S, Cioffi WG, Ayala A, Heffernan DS. The geriatric cytokine response to trauma: time to consider a new threshold. Surgical Infections. 2014;15:800–805. doi: 10.1089/sur.2013.235. [DOI] [PubMed] [Google Scholar]
- Pollmacher et al. (1993).Pollmacher T, Schreiber W, Gudewill S, Vedder H, Fassbender K, Wiedemann K, Trachsel L, Galanos C, Holsboer F. Influence of endotoxin on nocturnal sleep in humans. American Journal of Physiology. 1993;264:R1077–R1083. doi: 10.1152/ajpregu.1993.264.6.R1077. [DOI] [PubMed] [Google Scholar]
- Pollmacher et al. (2000).Pollmacher T, Schuld A, Kraus T, Haack M, Hinze-Selch D, Mullington J. Experimental immunomodulation, sleep, and sleepiness in humans. Annals of the New York Academy of Sciences. 2000;917:488–499. doi: 10.1111/j.1749-6632.2000.tb05413.x. [DOI] [PubMed] [Google Scholar]
- Rivera-Chavez et al. (2003).Rivera-Chavez FA, Wheeler H, Lindberg G, Munford RS, O’ GE, Keefe Regional and systemic cytokine responses to acute inflammation of the vermiform appendix. Annals of Surgery. 2003;237:408–416. doi: 10.1097/01.SLA.0000055274.56407.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohleder, Aringer & Boentert (2012).Rohleder N, Aringer M, Boentert M. Role of interleukin-6 in stress, sleep, and fatigue. Annals of the New York Academy of Sciences. 2012;1261:88–96. doi: 10.1111/j.1749-6632.2012.06634.x. [DOI] [PubMed] [Google Scholar]
- Rosenberg-Adamsen et al. (1996).Rosenberg-Adamsen S, Kehlet H, Dodds C, Rosenberg J. Postoperative sleep disturbances: mechanisms and clinical implications. British Journal of Anaesthesia. 1996;76:552–559. doi: 10.1093/bja/76.4.552. [DOI] [PubMed] [Google Scholar]
- Rosenberg (2001).Rosenberg J. Sleep disturbances after non-cardiac surgery. Sleep Medicine Reviews. 2001;5:129–137. doi: 10.1053/smrv.2000.0121. [DOI] [PubMed] [Google Scholar]
- Rosenberg et al. (1994).Rosenberg J, Wildschiodtz G, Pedersen MH, von Jessen F, Kehlet H. Late postoperative nocturnal episodic hypoxaemia and associated sleep pattern. British Journal of Anaesthesia. 1994;72:145–150. doi: 10.1093/bja/72.2.145. [DOI] [PubMed] [Google Scholar]
- Shaw et al. (2005).Shaw IR, Lavigne G, Mayer P, Choiniere M. Acute intravenous administration of morphine perturbs sleep architecture in healthy pain-free young adults: a preliminary study. Sleep. 2005;28:677–682. doi: 10.1093/sleep/28.6.677. [DOI] [PubMed] [Google Scholar]
- Spath-Schwalbe et al. (1998).Spath-Schwalbe E, Hansen K, Schmidt F, Schrezenmeier H, Marshall L, Burger K, Fehm HL, Born J. Acute effects of recombinant human interleukin-6 on endocrine and central nervous sleep functions in healthy men. Journal of Clinical Endocrinology and Metabolism. 1998;83:1573–1579. doi: 10.1210/jcem.83.5.4795. [DOI] [PubMed] [Google Scholar]
- Thomas et al. (2011).Thomas KS, Motivala S, Olmstead R, Irwin MR. Sleep depth and fatigue: role of cellular inflammatory activation. Brain, Behavior, and Immunity. 2011;25:53–58. doi: 10.1016/j.bbi.2010.07.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toussaint et al. (1995).Toussaint M, Luthringer R, Schaltenbrand N, Carelli G, Lainey E, Jacqmin A, Muzet A, Macher JP. First-night effect in normal subjects and psychiatric inpatients. Sleep. 1995;18:463–469. doi: 10.1093/sleep/18.6.463. [DOI] [PubMed] [Google Scholar]
- Trachsel et al. (1994).Trachsel L, Schreiber W, Holsboer F, Pollmacher T. Endotoxin enhances EEG alpha and beta power in human sleep. Sleep. 1994;17:132–139. doi: 10.1093/sleep/17.2.132. [DOI] [PubMed] [Google Scholar]
- Wetter & Young (1994).Wetter DW, Young TB. The relation between cigarette smoking and sleep disturbance. Preventive Medicine. 1994;23:328–334. doi: 10.1006/pmed.1994.1046. [DOI] [PubMed] [Google Scholar]
- Zhang et al. (2006).Zhang L, Samet J, Caffo B, Punjab NM. Cigarette smoking and nocturnal sleep architecture. American Journal of Epidemiology. 2006;164:529–537. doi: 10.1093/aje/kwj231. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Some sleep parameters, such as Total Sleep Time, are not included in the Raw dataset, because they are calculated from the raw sleep data. E.g. Total Sleep Time = sum of time spent in all four stages of sleep.