Abstract
Exposures to ultrafine particles (<100 nm, estimated as particle number concentration, PNC) differ from ambient concentrations because of the spatial and temporal variability of both PNC and people. Our goal was to evaluate the influence of time-activity adjustment on exposure assignment and associations with blood biomarkers for a near-highway population. A regression model based on mobile monitoring and spatial and temporal variables was used to generate hourly ambient residential PNC for a full year for a subset of participants (n=140) in the Community Assessment of Freeway Exposure and Health study. We modified the ambient estimates for each hour using personal estimates of hourly time spent in five micro-environments (inside home, outside home, at work, commuting, other) as well as particle infiltration. Time-activity adjusted (TAA)-PNC values differed from residential ambient annual average (RAA)-PNC, with lower exposures predicted for participants who spent more time away from home. Employment status and distance to highway had a differential effect on TAA-PNC. We found associations of RAA-PNC with high sensitivity C-reactive protein and Interleukin-6, although exposure-response functions were non-monotonic. TAA-PNC associations had larger effect estimates and linear exposure-response functions. Our findings suggest that time-activity adjustment improves exposure assessment for air pollutants that vary greatly in space and time.
Keywords: C-reactive protein, exposure misclassification, micro-environment, particle number concentration, time activity, ultrafine particles
INTRODUCTION
Residential proximity to highways, major roads, and high traffic density has been associated with increased risk for adverse cardiovascular health.1, 2, 3, 4, 5 Proximity to traffic has also been associated with higher biomarkers of systemic inflammation such as high sensitivity C-reactive protein (hsCRP) and Interleukin-6 (IL-6).6, 7, 8, 9 Cardiovascular effects in near-roadway populations are hypothesized to be partly attributable to traffic-related air pollutants (TRAPs), including ultrafine particles (<100 nm, UFP, estimated as particle number concentration, PNC) which are elevated next to high traffic roadways.10 The patterns of association of roadway proximity with health outcomes are similar to gradients of UFP; thus, there is a need for studies that directly test association of chronic UFP exposure with cardiovascular disease risk.4, 9
To our knowledge, no studies have reported relationships between chronic exposure to UFP and measures of cardiovascular health risk or health outcomes. The evidence to date for an association between UFP and adverse cardiovascular effects has instead come from animal studies,11, 12, 13 acute controlled human exposure studies,14, 15 and panel (acute) studies.16, 17, 18, 19, 20 These studies show biological plausibility that UFPs may be associated with increased inflammatory biomarkers such as hsCRP and IL-6 and cardiovascular outcomes.
UFP concentrations have been shown to vary greatly over both space and time,10, 21, 22, 23 which requires novel approaches to reduce exposure misclassification.24, 25, 26 Accurate geolocation of residences and fine-scale temporal estimates of air pollution are essential to properly characterize exposure.9, 27, 28 Since people do not spend all their time at home, let alone immediately outside their residence where ambient levels are often assessed, exposure estimates for TRAPs (such as UFP) also need to account for personal time-activity patterns and infiltration into buildings.27, 28, 29, 30, 31
The Community Assessment of Freeway Exposure and Health (CAFEH) study is a cross-sectional, community-based participatory research study of the relationship between TRAP exposures and measures of cardiovascular health risk.32 Here, we compare models of association of residential ambient annual average (RAA) PNC and time-activity adjusted (TAA)-PNC with the blood biomarkers hsCRP and IL-6 in a subset of the CAFEH study population. Our goal was to test the value of time-activity adjustment for improving exposure assessment for environmental epidemiology of UFP, a pollutant with high spatial and temporal variability.
METHODS
CAFEH Study Population
Details on the CAFEH study methods and approach are reported elsewhere,32 and a summary of the study population has been provided in Appendix 1. The CAFEH subsample analyzed here (n=204) was restricted to individuals ≥40 years of age living in neighborhoods within Somerville, Massachusetts, USA. Other studies of the effects of air pollution, including ultrafine particles, on inflammation have usually been restricted to older adults, because greater effects are expected in older adults than in young adults or children.17, 18, 19 An hourly PNC model for the Somerville study area for the year in which the participants were recruited has been published.23
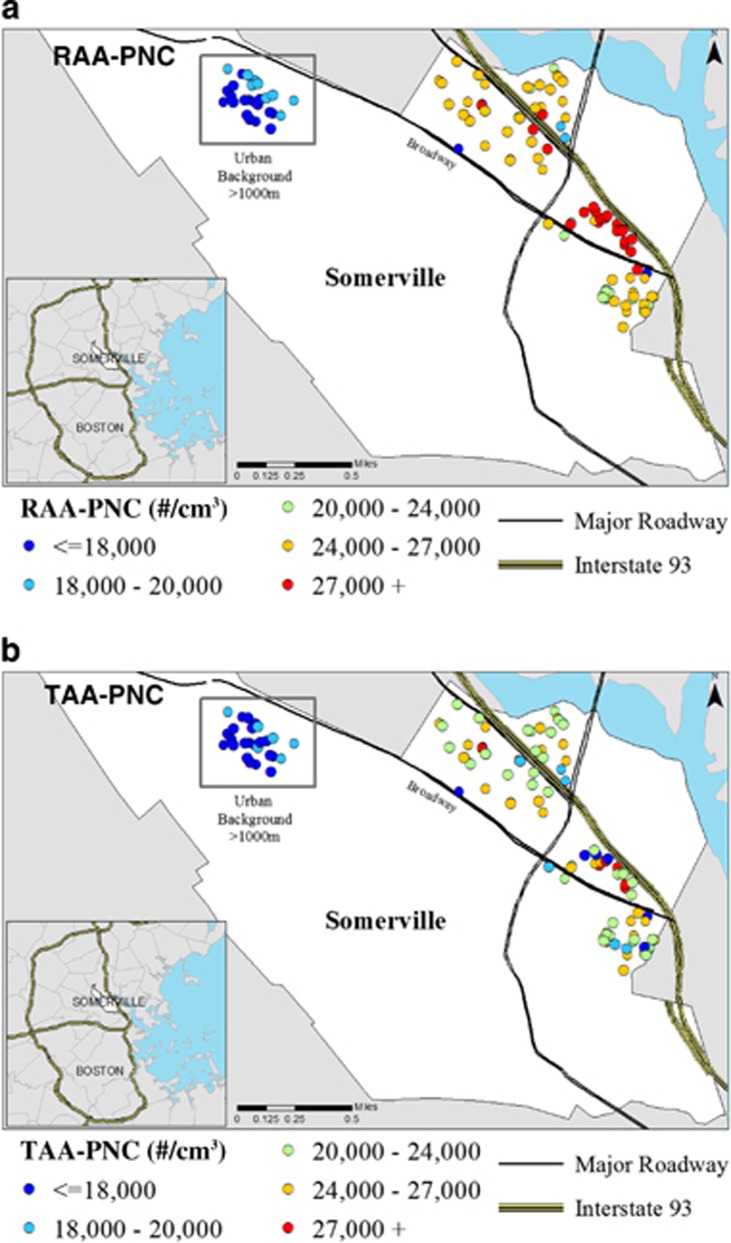
The majority of participants in this analysis (n=140) were randomly recruited from geographically-weighted areas ≤500 m from Intersate-93 (I-93) and from an urban background area that was ≥1,000 m from I-93 (Figure 1). Recruitment was between July 2009 and September 2010. We also included a convenience sample (n=65) of participants who resided in two housing complexes for elderly residents. A subset of participants attended our field clinic at least once where blood was collected for biomarker analysis (n=140) and height and weight were recorded (n=133). Blood samples were collected from August 2009 to June 2010, with an unequal seasonal distribution (fall n=26; winter n=38; spring n=70; summer n=6).
Figure 1.
Comparison of residential ambient annual average PNC and time-activity adjusted PNC (n=140 participants).
Participants completed a survey that included questions regarding demographics, window opening, air conditioning use, and time activity. The time-activity information was used to assign time spent inside or outside home, at work/school, and at other locations (including non-highway travel) for each hour of the day as well as time on highways in 15-min increments. Depending on employment status, participants were asked to characterize time activity for the most recent workday and non-workday (employed participants) or weekday and weekend day (non-employed participants). We pooled workday/weekday and non-workday/weekend time-activity data except when stratifying by employment status. Other studies have shown time-activity patterns to be stable over time.33 Similarly, analysis of data from CAFEH-study participants who completed a second time-activity questionnaire (n=127) showed little variability between surveys, supporting the use of a single survey to characterize time activity throughout the study period.28 Participants provided weekly window opening information (never, <2 times, 2–5 times, 6–7 times per week) from December to February (winter) and June to August (summer). Participants also reported air conditioner (AC) type (window or central) and usage (yes/no).
Geocoding of Study Participants
Residential location was determined using a multi-stage process that included parcel and street network geocoding accompanied by manual correction via orthophotos and apartment/multi-unit floor plans to reduce positional error.9, 23 We used ESRI ArcGIS v10.1 (ESRI, Redlands, California, USA) software for all geographic information system (GIS) processes. Individual geocoded locations are slightly jittered on published maps to protect participants' identity. Distances to I-93, Mystic Avenue/RT 38 (a state highway adjacent to the west side of I-93; Figure 1), and other major roads were calculated in ArcGIS using the Near tool. Additionally, participants employed full or part time (n=92) who worked in a single location and provided a work address (n=42) had their employment location geocoded and distance calculated to the nearest interstate highway. None of the work addresses were ≤500 m from I-93 or any other interstate highway, but nine participants did work within 200 m of a major roadway (that is, >20,000 vehicles per day).
PNC Measurement and Regression Modeling
PNC was measured in the neighborhoods where the participants lived with a condensation particle counter (TSI Model 3775) in the Tufts Mobile Air Pollution Laboratory (TAPL).22 The TAPL was driven over the same route 2–6 times per day on 43 days (234 total hours at different times of the day, on all days of the week, and in all seasons) between September 2009 and August 2010, the year in which participants filled out surveys and provided blood samples. Comparing the clinic date with exposure dates, on average there were 180 days (SD=72 days) of exposure that occurred post clinic visit.
A regression model to predict hourly ambient PNC across the study area was built and validated.23 The model utilized both spatial (side of and distance to I-93, distance to nearest major road) and temporal (wind speed, wind direction, temperature, day of week, I-93 traffic volume, and speed) variables to predict PNC across the study area (R2=0.43; cross-validated R2=0.38–0.47). Residential coordinates were used in the model to calculate ambient residential PNC for every hour of the year for each study participant.
Time-Activity Adjustment of PNC
We averaged the ambient PNC values that were predicted by the model for all hours of the year (n=8760 h) to calculate an RAA-PNC for each residence. To derive TAA-PNC, we used hourly questionnaire data for five micro-environments (inside home, outside home, at work, on highway, and other) and we accounted separately for PNC infiltration into the home. To test the importance of each step in the time-activity adjustment, we sequentially adjusted PNC exposure for every hour of the year for each micro-environment for individual study participants. We began with the micro-environments in which the participants spent the greatest percentage of time on average, and added micro-environments in descending order. Adjustments for residential AC use were performed by two separate exposure models. The first adjusted RAA for inside home AC and did not include any TAA. The second model adjusted for inside home AC use after TAA of all micro-environments. This approach to inside home AC use allowed for evaluation of the effects of particle infiltration into homes separately from adjustment for time activity. Hourly exposure in each micro-environment was assigned as follows (Supplementary Figure 1):
Inside home
We assigned the RAA-PNC value to all hours spent inside the home, assuming 100% particle infiltration. This assumption was based upon previously published analyses of homes in our study population that showed a 0.95 median indoor–outdoor ratio (I/O).34 Because of this there is no difference between RAA-PNC and TAA-PNC inside the home. We do not consider a separate adjustment for outside home.
At work
We classified participants who were employed full or part time as having jobs with TRAP exposure (n=7; for example, bus driver, crossing-guard, and parking ticket officer) or without TRAP exposure (n=85; for example, nurse, administrator, and school teacher). For those with work-based TRAP exposure, we approximated exposures by using the average hourly RAA-PNC of all participants residing ≤50 m of I-93 for the hours they were at work. This was based on our assumption that levels of PNC exposure would be higher for these participants during hours at work. For participants without TRAP exposure at work, we approximated their work PNC exposures using the average hourly RAA-PNC of all participants residing in the urban background area, assuming that work environments with no obvious TRAP exposure were likely to have levels similar to urban background.
Other
For time spent in all other micro-environments, we also assigned the hourly residential average of all participants residing in the urban background area based on the assumption that urban background was the most likely exposure for any micro-environment in the metropolitan area.
Highway
For hours spent on highways, we used estimates of PNC on Rt 38 from the PNC model developed by Patton et al.23 We did not have information on participant vehicle type or in-vehicle behaviors such as opening windows, closing vents, or AC usage; therefore, we assumed 100% particle infiltration into vehicles.
Air conditioning adjustment
Finally, we adjusted the inside home micro-environment to account for reduction of PNC infiltration by AC use applying adjustment factors separately in both the RAA and TAA models. We had information on whether participants used AC seasonally in their homes, but we did not have hourly or daily records of use. Accordingly, we assumed that AC use occurred when ambient temperatures exceeded 21 °C (70 °F), with either a 25% or 28% reduction (window and central AC, respectively) of infiltration during those hours. These values were based on sampling at a subset of CAFEH homes in which we found PNC I/O ratios of 75% in homes using window-based units and 72% in homes using central AC.34 Given our assumption of 100% particle infiltration, we did not make an additional adjustment for window opening.
At each step of time-activity adjustment, we built on the previously adjusted PNC values for hours and micro-environments that had not been adjusted at the previous stage in the model. Equations have been included in Supplementary Table 1 to provide greater detail on the hourly adjustment methods used to derive TAA-PNC.
Statistical Analysis
Statistical analyses were performed using SAS v9.12 (Statistical Analysis Software, Cary, North Carolina, USA) and R v3.1.35 Bivariate analyses were conducted using t-tests, and analysis of variance (ANOVA) to test for differences in means. Chi-square analysis was used to compare differences in proportions. All statistical tests reporting a P-value were two-sided; a P-value of <0.05 was considered as statistically significant. For our core exploratory models, we used linear models to test the association of the natural log (LN) of PNC with LN hsCRP and LN IL-6, constructing both unadjusted models and models adjusted for age, gender, BMI, and smoking status. Sample size limited our ability to simultaneously adjust for more covariates in models. Therefore, separate models were run to examine the effect of socio-economic status (SES) on the PNC—biomarker relationship by removing smoking status. Identical unadjusted and adjusted models were constructed for each stage of the TAA-PNC exposure adjustment process. Log-transformed regression β-estimates with 95% CIs were reported as measures of elasticity (% change). We explored which parts of the exposure response function changed by comparing RAA-PNC and TAA-PNC generalized additive models (GAMs) with a locally-weighted scatterplot smoothing (LOESS) using the GAM R-cran package.36 All GAMs were adjusted for the same covariates in the linear model.
Comparison of PNC percent contributions for each micro-environment and sequential TAA for distance to highway strata were conducted on the full sample (n=204) to retain the largest sample size and potential for variation in exposures. Analyses for association between PNC and biomarkers of systemic inflammation were restricted to only those participants with viable blood samples (n=140).
Sensitivity Analysis
While we had I/O PNC data from homes in our study population,34 there are published infiltration factors that are significantly lower than ours. For example, studies have reported that ambient UFP penetration into homes can range from 7% to 100% depending on factors such as window size and openness, fan usage, air exchange rate, ambient concentrations, and meteorological conditions, with lower UFP penetration occurring in studies of unoccupied and/or tightly sealed buildings.37, 38, 39, 40, 41 Similarly, studies have found that infiltration into vehicles can range from 8% to 100%, depending on AC usage, recirculation of air, window opening, age of vehicle, make and type of vehicle and speed.42, 43, 44, 45 We therefore performed sensitivity analyses to examine the influence of infiltration factors on our findings. We applied 25%, 50%, and 75% particle reductions for both time spent inside home and traveling on highways. We ran separate regression models for associations of these exposure estimates with hsCRP and IL-6 to compare effects on the β-estimates and strength of association.
RESULTS
Characteristics of the Study Population
The mean age of study participants was 59.1 years. The majority were female (66%), white (70%), had completed high school (74%), and had incomes below $75,000 (67%) (Table 1). Demographic variables were divided into three strata based on Euclidean distance from I-93: ≤50 m, 51–500 m, and ≥1,000 m. Compared with participants residing in the urban background area, participants living ≤50 m from I-93 were significantly younger, had higher BMI, were more likely to be non-white and male, had lower income and education, were more likely to be employed full or part time, and to have never smoked. Window opening was 88% in the summer, with no significant differences by distance to I-93, and 54% in winter, with a significantly lower percentage (40%) in the urban background area. The majority of participants had either window or central air conditioning units, with little difference by proximity to I-93.
Table 1. Demographic and TAA variables stratified by residential distance to I-93.
| Characteristic | Total (N=204) | ≤50 m (N=32) | 51–500 m (N=129) | >1,000 m (N=43) |
|---|---|---|---|---|
| Demographic variables | ||||
| Age, mean (SD) | 59.1 (12.4) | 52.7 (10)a,b | 60.5 (11.7)b | 59.6 (14.8) |
| Female | 66% | 56%a | 66% | 72% |
| White | 70% | 58%a | 66%c | 93% |
| Smoking status | ||||
| Current | 22% | 19%a | 27%c | 7% |
| Former | 35% | 16%a,b | 36%b | 47% |
| Never | 37% | 50%b | 31%b,c | 44% |
| Missing | 6% | 16% | 6% | 2% |
| Educational attainment | ||||
| Less than high school diploma | 26% | 38%a | 26% | 16% |
| High school diploma | 31% | 31%a | 38% | 12% |
| Undergraduate school | 28% | 28% | 25% | 35% |
| Graduate school | 15% | 3%a,b | 11% | 37% |
| Annual Income | ||||
| Less than $24,999 | 19% | 12% | 12% | 14% |
| $25,000–$74,999 | 14% | 19%b | 44%b,c | 25% |
| $75,000 or more | 35% | 28% | 33% | 42% |
| Do not know/refused | 32% | 41%a,b | 11%c | 19% |
| Employment | ||||
| Working full time or part time | 45% | 66%a,b | 36%b,c | 58% |
| Retired, disabled or unemployed | 52% | 28%a,b | 62%b,c | 40% |
| Missing | 3% | 6%a,b | 2%b,c | 2% |
| Time-activity adjustment variables | ||||
| Workday/weekday (mean hours (SD)) | ||||
| Inside home | 17.14 (4.8) | 15.07 (5.4)a | 17.94 (4.2)c | 16.34 (5.4) |
| Outside home | 0.95 (2.53) | 0.48 (1.16) | 0.99 (2.14) | 1.13 (3.78) |
| Work | 3.95 (4.8) | 7.66 (5.67)a,b | 2.68 (4.07)b,c | 4.96 (4.68) |
| Other | 1.56 (2.53) | 0.52 (0.96)a | 2.02 (2.97)c | 1.02 (1.47) |
| Highway | 0.40 (0.97) | 0.27 (0.48) | 0.37 (0.71) | 0.55 (1.58) |
| Non-workday/weekend (mean hours (SD)) | ||||
| Inside home | 18.56 (4.6) | 17.24 (4.6) | 19.45 (3.5)c | 17.09 (6.2) |
| Outside home | 1.72 (3.5) | 2.88 (5.33) | 1.48 (2.72) | 1.63 (4.01) |
| Work | 1.46 (3.71) | 1.86 (2.91) | 0.63 (1.98)c | 3.33 (6.12) |
| Other | 1.89 (2.49) | 1.42 (2.24) | 2.13 (2.62) | 1.58 (2.25) |
| Highway | 0.37 (0.62) | 0.6 (0.79) | 0.32 (0.56) | 0.37 (1.76) |
| Air conditioner (AC) | ||||
| Yes | 85% | 81% | 88% | 81% |
| Open windows in winter | ||||
| Yes | 54% | 53%a | 59%c | 40% |
| Missing | <1% | 0% | <1% | 0% |
| Open windows in summer | ||||
| Yes | 88% | 88% | 87% | 93% |
| Missing | 2% | 3% | 1% | 2% |
Indicates significant (P≤0.05) mean difference between the ≤50 m and >1,000 m distance group.
Indicates significant mean difference between the ≤50 m and 51–500 m distance group.
Indicates significant (P≤0.05) mean difference between the 51–500 m and >1,000 m distance group.
The subpopulation with blood samples (n=140) had a mean BMI of 29.2, and median hsCRP and IL-6 values of 1.62 mg/l and 1.61 pg/ml, respectively (Table 2). Stratifying the inflammatory markers by season of blood sample did not result in a significant median difference in hsCRP or IL-6 (data not shown). The subset of participants who gave blood samples were similar to the full sample (Supplementary Table 2).
Table 2. Health measures stratified by distance to I-93.
| Health measure | Total (N=140) | ≤50 m (N=20) | 51–500 m (N=95) | >1,000 m (N=25) |
|---|---|---|---|---|
| BMI, mean (SD)a | 29.2 (6.9) | 32.9 (8.4)b | 29.3 (6.6) | 26.0 (5.5) |
| hsCRP mg/l, median (IQR) | 1.62 (2.8) | 1.92 (4.4) | 1.92 (2.9) | 0.94 (1.0) |
| IL-6 pg/ml, median (IQR) | 1.61 (2.3) | 1.63 (2.9) | 1.78 (2.1) | 0.97 (0.8) |
Sample size differs due to missing BMI values ≤50 m (n=19); 51–500 m (n=89); and >1,000 m (n=25).
Indicates significant (P≤0.05) difference between ≤50 m and >1,000 m distance groups.
Time Activity
Participants residing ≤50 m from I-93 spent significantly more time (31%) at work than did those in the 51–500 m (11%) and urban background (21%) areas. They also spent significantly less time (63%) inside their homes than did those living 51–500 m (75%) from I-93. While not a significant difference, the urban background participants spent more time traveling on highways than did participants residing in the other distance groups. Participants in the 51–500 m distance category spent the most time in the “other” micro-environment. During the non-workday/weekend time-activity allocation participants residing 51–500 m from I-93 spent significantly greater amounts of time inside their homes and less time at work than did participants in the urban background (Table 1).
PNC Exposure Assignments and Adjustment for Time Activity
The inside and outside home micro-environments contributed a combined 75.3% of daily time and 78.4% of daily exposure (Table 3). The work micro-environment contributed 16.5% of daily time and 13.5% of daily exposure. Time in the “other” micro-environment contributed 6.5% of daily time and 5.0% of daily exposure. The micro-environment for travel on highways contributed only 1.7% of daily time, but 3.2% of daily exposure, reflecting higher PNC levels assigned to time on highways. Stratification by employment status showed that among employed participants the work and highway micro-environments contributed more to PNC daily exposure, while the residential and “other” micro-environments contributed less as compared with the unemployed population.
Table 3. Micro-environment percent contribution to TAA-PNC annual average by employment status.
| Micro-environment | Average time (hours) | % Time (hours/24 hours) | Annual average PNC (#/cm3) | %Exposurea |
|---|---|---|---|---|
| Residential | 17.14 | 75.3 | 24,000 | 78.36 |
| Work | 3.95 | 16.5 | 18,000 | 13.54 |
| Other | 1.56 | 6.5 | 17,000 | 5.05 |
| Highway | 0.4 | 1.7 | 40,000 | 3.05 |
| Working full or part time | ||||
| Residential | 14.47 | 60.3 | 24,000 | 64.74 |
| Work | 7.55 | 31.5 | 18,000 | 25.33 |
| Other | 1.09 | 4.5 | 17,000 | 3.45 |
| Highway | 0.89 | 3.7 | 39,000 | 6.47 |
| Non-working, retired or disabled | ||||
| Residential | 20.28 | 84.5 | 25,000 | 86.54 |
| Work | 0.84 | 3.5 | 17,000 | 2.44 |
| Other | 2.23 | 9.3 | 17,000 | 6.47 |
| Highway | 0.65 | 2.7 | 41,000 | 4.55 |
Time spent in micro-environment per day multiplied by annual average PNC of micro-environment then divided by the sum annual average of all micro-environment exposures. Residential: all hours a participant indicated they were in the micro-environments inside or outside home on time-activity questionnaire. Work: All hours a person indicated they were in the work micro-environment. Other: all hours a participant indicated being in a “other” micro-environment. Highway: aggregate of 15 min intervals a person identified as traveling on the highway.
Sequential adjustment of PNC for time activity and AC reduced PNC exposures for the 0–50 m and 51–500 m subpopulations, but less so for the urban background population (Table 4). Modeled RAA-PNC was higher in near highway areas compared with the urban background area across all adjustment steps. Stratification by employment status revealed larger underlying differences in time-activity adjustment. Among employed participants in the 0–50 m distance group the work micro-environment adjustment introduced the largest downward shift in PNC (3,000 particles/cm3). Adjustment for all micro-environments for employed participants from the 0–50 m and 51–500 m groups led to downward shifts in average mean TAA-PNC relative to RAA-PNC of 4,000 particles/cm3 and 3,000 particles/cm3, respectively. The standard deviation of TAA-PNC values for employed participants tripled in the 0–50 m group and doubled in the 51–500 m group. Unemployed participants in the 0–50 m and 51–500 m distance groups had smaller shifts in mean PNC and smaller changes in standard deviation. There was no observable difference in the mean or standard deviation for the urban background subpopulation regardless of employment status. PNC adjustment models for all Somerville participants produced similar results to the participants attending clinics (Supplementary Table 3).
Table 4. Mean and standard deviation of residential and time-activity adjusted annual average particle number concentrations (presented as 10,000 particles per cm3) from sequential model adjustment by distance to I-93 and stratified by employment status for clinic attending participants.
| PNC models | Total | ≤50 m | 51–500 | >1,000 m |
|---|---|---|---|---|
| All clinic participants | (n=140) | (n=20) | (n=95) | (n=25) |
| RAA | 2.5 (0.4) | 2.7 (0.1)a | 2.6 (0.1)b | 1.8 (0.1) |
| RAA+AC | 2.4 (0.3) | 2.7 (0.1)a | 2.6 (0.1)b | 1.8 (0.1) |
| RAA+work | 2.4(0.3) | 2.4 (0.2)a | 2.5 (0.2)b | 1.8 (0.1) |
| RAA+work+other | 2.3 (0.3) | 2.4 (0.2)a | 2.4 (0.1)b | 1.8 (0.1) |
| RAA+work+other+highway | 2.3 (0.3) | 2.4 (0.2)a | 2.4 (0.1)b | 1.8 (0.1) |
| RAA+work+other+highway+AC | 2.3 (0.3) | 2.4 (0.2)a | 2.4 (0.2)b | 1.7 (0.1) |
| Working full or part time | (n=62) | (n=14) | (n=32) | (n=16) |
| RAA | 2.4 (0.4) | 2.7 (0.1)a | 2.6 (0.1)b | 1.8 (0.1) |
| RAA+AC | 2.4 (0.4) | 2.7 (0.1)a | 2.6 (0.1)b | 1.8 (0.1) |
| RAA+work | 2.2 (0.3) | 2.4 (0.2)a | 2.4 (0.1)b | 1.8 (<0.1) |
| RAA+work+other | 2.2 (0.3) | 2.4 (0.2)a | 2.3 (0.1)b | 1.8 (<0.1) |
| RAA+work+other+highway | 2.2 (0.3) | 2.4 (0.2)a | 2.4 (0.1)b | 1.8 (0.1) |
| RAA+work+other+highway+AC | 2.2 (0.3) | 2.3 (0.3)a | 2.3 (0.2)b | 1.8 (0.1) |
| Non-working, retired or disabled | (n=78) | (n=6) | (n=63) | (n=9) |
| RAA | 2.5 (0.3) | 2.7 (0.1)a | 2.6 (0.1)b | 1.8 (0.1) |
| RAA+AC | 2.4 (0.3) | 2.7 (0.1)a | 2.5 (0.1)b | 1.7 (0.1) |
| RAA+work | 2.5 (0.3) | 2.7 (0.1)a | 2.6 (0.1)b | 1.8 (0.1) |
| RAA+work+other | 2.4 (0.3) | 2.6 (0.1)a | 2.5 (0.1)b | 1.8 (0.1) |
| RAA+work+other+highway | 2.4 (0.3) | 2.6 (0.1)a | 2.5 (0.1)b | 1.8 (0.1) |
| RAA+work+other+highway+AC | 2.3 (0.3) | 2.6 (0.1)a | 2.4 (0.2)b | 1.7 (0.1) |
Residential annual average (RAA): PNC values for all hours of the year to the participant's place of residence. Work: an average higher or lower PNC was inserted for every hour a participant indicated being in the work micro-environment and based upon TRAP exposure job categorization. Other: an urban background average was inserted for every hour a participant identified as being in the “other” micro-environment. Highway: modeled side of highway values was inserted for indicated time spent on highway. Air conditioning (AC): a % reduction when ambient hourly temperatures were above 21 °C (70 °F) was applied to PNC values for the micro-environment inside home when participants identified as having and using window or central AC.
Indicates significant mean difference between the ≤50 m and >1,000 m distance group.
Indicates significant mean difference between the 51–500 m and >1,000 m distance group. Sequential PNC adjustments are based upon each participant's individual time-activity questionnaires.
Quintiles of PNC for the entire population were used as cut points to illustrate exposure differences across the study area. The majority of participants in the urban background area were in the lowest quintile of RAA-PNC exposure (PNC≤18,000 particles/cm3), while most of the participants in the highest quintile of RAA-PNC (PNC≥27,000 particles/cm3) resided near major roadways or I-93 (Figure 1a). Adjusting for time activity had little effect on the assigned values for the urban background participants; however, time-activity adjustment resulted in lower mean exposures for participants residing close to I-93 (Figure 1b; Table 4). Additional maps that stratified by employment status (Supplementary Figure 2) illustrate the greater reduction in PNC with TAA for employed residents near I-93.
Association of PNC with Biomarkers
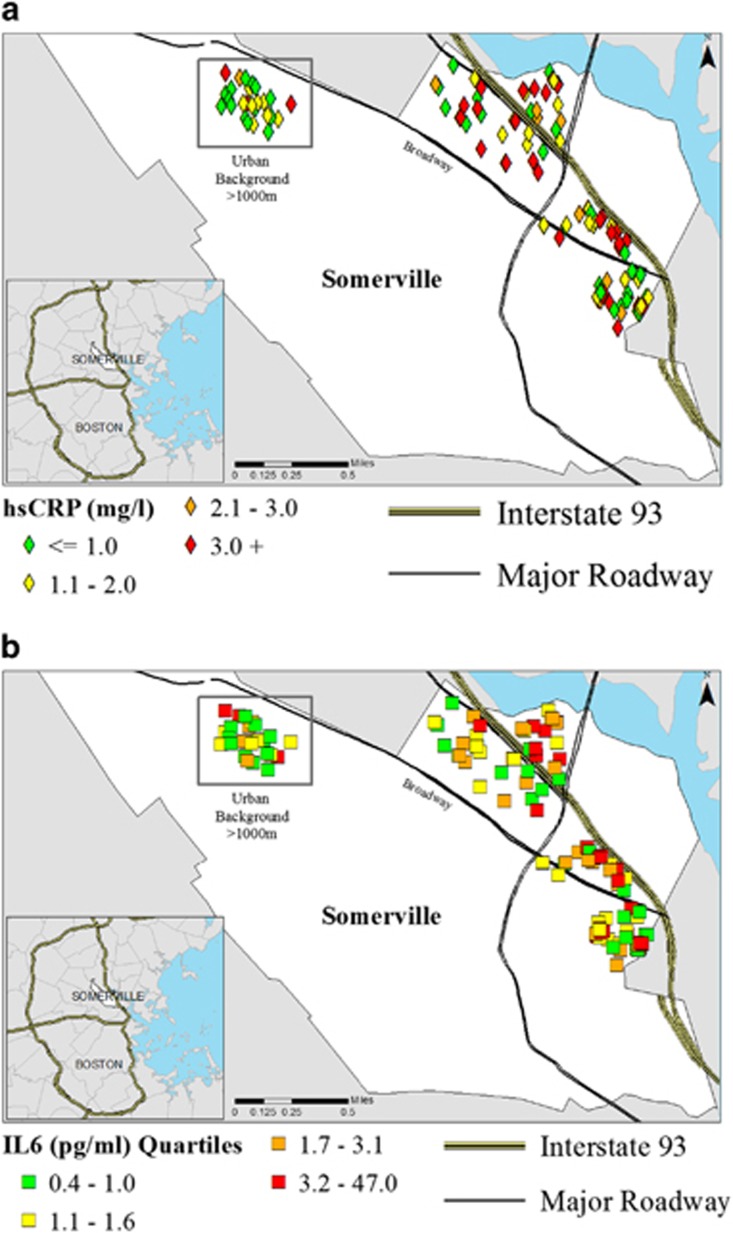
Concentrations of hsCRP and IL-6 were higher for participants living near I-93 and Broadway, a major roadway running along the near-highway study area (Figure 2 and Table 2). After controlling for key covariates (age, gender, BMI, and smoking status), multivariable regression models showed positive associations, but with reduced beta estimates that were not statistically significant (Table 5). Beta estimates tended to become larger as more TAA factors were included in the multivariate models and then declined with the addition of the AC adjustment. Additional models were tested for the effects of SES in place of smoking status to maintain adequate degrees of freedom. Income and education were significant predictors of our inflammatory markers, but did not affect the relationship with PNC by greater than 10% (data not shown).
Figure 2.
Spatial distribution of hsCRP and IL-6 across the study area.
Table 5. LN TAA-PNC models for association with LN hsCRP and LN Il-6.
| PNC exposure models |
Univariate |
Multi-variablea |
||||||
|---|---|---|---|---|---|---|---|---|
|
LN hsCRP |
LN IL-6 |
LN hsCRP |
LN IL-6 |
|||||
| β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | |
| RAA | 1.92 | (0.62, 3.22) | 1.24 | (0.35, 2.13) | 1.14 | (−0.06, 2.35) | 0.53 | (−0.28, 1.34) |
| RAA+AC | 1.81 | (0.54, 3.09) | 1.18 | (0.29, 2.08) | 0.99 | (−0.19, 2.17) | 0.54 | (−0.25, 1.33) |
| RAA+work | 2.00 | (0.27, 3.74) | 0.73 | (−0.49, 1.96) | 1.37 | (−0.24, 2.99) | 0.6 | (−0.48, 1.68) |
| RAA+work+other | 2.28 | (0.56, 3.99) | 1.14 | (−0.05, 2.35) | 1.36 | (−0.19, 2.92) | 0.54 | (−0.50, 1.58) |
| RAA+work+other+highway | 2.06 | (0.33, 3.80) | 1.07 | (−0.14, 2.27) | 1.67 | (−0.03, 3.37) | 0.76 | (−0.36, 1.88) |
| RAA+work+other+highway+AC | 1.90 | (0.47, 3.34) | 1.37 | (0.38, 2.36) | 1.26 | (−0.02, 2.75) | 0.65 | (−0.26, 1.55) |
Residential annual average (RAA): PNC values for all hours of the year to the participant's place of residence. Work: an average higher or lower PNC was inserted for every hour a participant indicated being in the work micro-environment and based upon TRAP exposure job categorization. Other: an urban background average was inserted for every hour a participant identified as being in the “other” micro-environment. Highway: modeled side of highway values was inserted for indicated time spent on highway. Air conditioning (AC): a % reduction when ambient hourly temperatures were above 21 °C (70 °F) was applied to PNC values for the micro-environment inside home when participants identified as having and using window or central AC.
Each PNC model in the table builds iteratively upon the previous row until all micro-environments and the adjustment for residential AC have been included.
Models adjusted for age, gender, BMI, and smoking status.
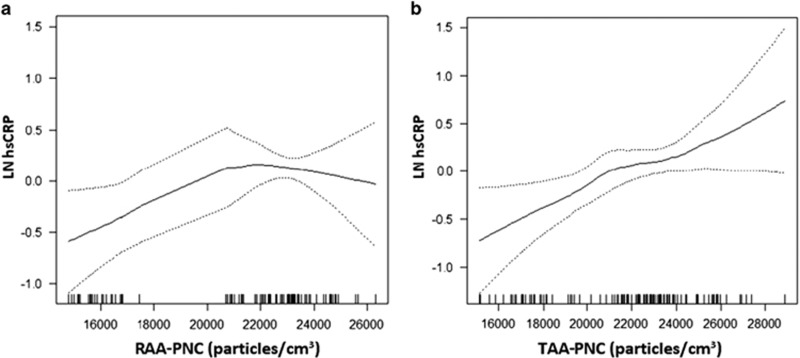
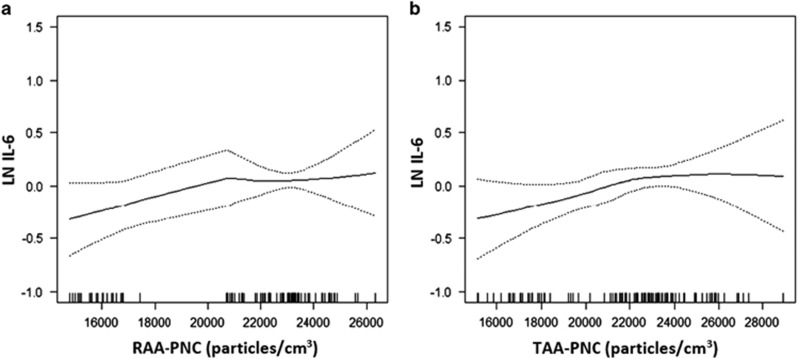
Figure 3a shows adjusted GAM plots using only residential exposure assignment. The association with hsCRP appeared non-monotonic, with confidence intervals substantially wider at higher and lower concentration tails. The shape of the curve is possibly affected by discontinuities (lack of intermediate exposures) between the near highway and urban background populations. Adjusting for time-activity patterns (Figure 3b) led to a greater continuum of exposures, with a monotonic and essentially linear association. The re-distribution of the participants' exposures can be observed in the hash marks along the X axis, which represent each individual participant's contribution to the exposure-response curve. GAMs for IL-6 did not differ substantially between RAA-PNC and TAA-PNC (Figure 4a and b).
Figure 3.
GAM model comparison of the effect of PNC exposure models on LN hsCRP.
Figure 4.
GAM model comparison of the effect of PNC exposure models on LN IL-6.
Decreasing the I/O ratio for time periods inside-home reduced exposure for the entire study population, while decreasing I/O for on-highway travel (that is, by reducing in-vehicle concentrations) led to only marginal reduction for a subset of the population (not shown). Assigning lower values for infiltration into vehicles had negligible effects on the associations with biomarkers. However, assigning reduced infiltration into homes greatly reduced effect estimates and widened confidence intervals (Supplementary Table 4). We found that decreasing the home I/O ratio by 50% or more produced null results for association with hsCRP and led to negative, but statistically insignificant, associations with IL-6.
DISCUSSION
Our goal was to test how incorporation of time-activity data could influence exposure assignment and epidemiologic findings. Our approach should better represent personal exposure to air pollutants that exhibit a high degree of spatial and temporal variation. We found that adjusting for time-activity patterns altered assigned PNC exposure levels, especially for near highway and employed participants. We also demonstrated associations, some statistically significant, of PNC exposure with hsCRP and IL-6 in unadjusted models. In adjusted models, while associations were not statistically significant, TAA increased the size of effect estimates while widening confidence intervals (Table 5). Coupled with the more biologically plausible exposure-response functions (Figures 3 and 4), these results provide evidence that adjusting PNC for time activity and air conditioning use may improve exposure assessment for UFP.
Adjustment of PNC for time activity differentially reduced assigned exposure to PNC annual averages for participants residing close to I-93 (Table 4). The downward shift in PNC for these participants was anticipated based upon our prior analysis of their hourly time-activity patterns. In that analysis, participants living ≤50 m from I-93 spent significantly less time at their residence and significantly greater amounts of time at work than participants in other distance groups.28
The uneven spatial distribution of the time-activity micro-environment adjustments resulted in differential PNC exposure assignment relative to distance to the highway (Figure 1). Consistent with our findings, one air pollutant study found large exposure differences between personal ambient PM2.5 and central monitors while another found differences in modeled NO2 before and after adjusting for time spent at work.46, 47 Studies of PNC levels in commuting scenarios and at other locations have also identified the importance of capturing micro-environment exposure.44, 48 Our results provide further support for the importance of adjusting for time-activity when assigning exposure.
The downward shift in PNC values for participants with lower hsCRP levels led to the dose response curve being monotonic, which is consistent with exposure misclassification in the RAA-PNC model partially obscuring the association (Figure 3). The gap in participants with exposures from 18,000 to 20,000 particles/cm3 in the RAA-PNC model was a byproduct of our geographically-weighted recruitment effort (Figure 3a). Our TAA classification scheme distributed exposures more evenly than RAA because many employed participants who resided in the 0–50 m and 51–500 m distance groups were assigned lower PNC exposures after adjustment for time away from home. These results suggest that taking time activity into account reduces exposure misclassification that could otherwise bias effect estimates and impede the ability to more accurately detect associations between exposure and health markers.
While we did not find a significant difference overall between the RAA-PNC and final TAA-PNC model, there were significant shifts in the mean and standard deviation within I-93 distance categories that were greater for the employed population. Comparing RAA-PNC and TAA-PNC models there was a change of 4,000 particles/cm3 for the employed residents who lived 0–50 m and of 3,000 particles/cm3 for those who lived 51–500 m from I-93 (Table 4). There was no observable shift in TAA-PNC assignment for urban background participants (>1,000 m from I-93) (Table 4). This differential effect in PNC assignment by TAA is due to: (1) near-highway participants spending significantly more time away from their homes in areas for which we assigned urban background concentrations; and (2) urban background participants having low RAA-PNC values at home as well as spending time away from home in areas assigned similarly low exposures. The variation in time-activity patterns observed between our near highway and urban background populations may not be generalizable to other populations. Additionally, there could be limited transferability of PNC models from one location to another, based on previous models of TRAP, which likely also reduces the generalizability of our results to other study areas.49, 50
Health studies often rely upon residential proximity to roadways or use models that assign ambient exposure outside at the residence to UFP and other TRAPs that actually have high spatial and temporal variability. Doing this potentially mischaracterizes effect sizes due to exposure misclassification related to time activity. Due to the spatial heterogeneity of PNC, ignoring TAA during exposure assignment biased our effect estimates toward the null and resulted in underestimating the association. Therefore adjusting for TAA could be important when studying other TRAPs with similarly high localized spatial variability such as NO and CO, but less important for more spatially homogenous air pollutants like PM2.5. Thus, epidemiologists conducting TRAP studies might benefit from considering exposure assessment models that adjust for mobility patterns in their study populations. They might also reduce misclassification by taking into consideration exposure inside homes, travel on highways, and hours working near highways. Only a small number of studies have integrated time-activity modeling into their analysis of TRAPs thus far.29, 51, 52 Studies with personal time-activity information and the ability to better characterize micro-environment concentrations could develop personal TAA models that go beyond what we did.53 Larger cohorts might need to utilize personal demographic and transport modeling software to predict population mobility trends.27, 29, 52
Strengths and Limitations
A primary limitation to our analysis is that we did not measure personal exposure of participants, so we do not have direct evidence that TAA reduced exposure misclassification. However, the main thrust of our findings is consistent with TAA reducing exposure misclassification. Another limitation was that questionnaire data were used to assess personal time activity, which could introduce reporting bias. However, the repeatability of our time-activity data was previously reported as relatively stable.28 Our time-activity questionnaire was also limited to five broad micro-environments and may contain error in responses as well as assumptions about exposures in these micro-environments. For example, our assumption that work hours with TRAP exposure should produce higher exposures than RAA-PNC should be directionally correct. However, we acknowledge that for work exposures without TRAP, using an hourly average of the urban background participants could underestimate work location exposures, particularly if participants are working in buildings at major traffic intersections. Alternatively, it could overestimate exposures if they are working within a tightly sealed building with AC or air filtration systems.
We had very little information on where participants were when they reported being in the “other” micro-environment category, albeit this category contributed a small fraction of time and exposure. If near highway participants were spending time closer to their residences while in the “other” micro-environment our assumption would underestimate their exposures. Future studies may want to include questions about location of moderate to vigorous physical activity (respiration rate) with respect to exposure sources because it would influence dose, a factor we did not address.51
An important strength was the availability of I/O monitoring of a subset of study homes in our study population.34 Thus, the ratio we used for infiltration reflected conditions in a range of residential building types in our study area. While we did not have data from winter months when window opening is typically lower, survey responses indicated substantial window opening during winter (Table 1). Window characteristics such as use, size, and number of windows open have been shown to affect particle infiltration ratios.39 Our sensitivity analysis (Supplementary Table 4) showed the importance of accurate estimation of residential infiltration. Reducing the I/O ratio resulted in a corresponding reduction in the strength of association of TAA-PNC with hsCRP, likely due to the corresponding reduction in the range of exposure estimates (Supplementary Table 4). Had we used lower I/O ratios obtained from the literature, many of which were based on unoccupied buildings with closed windows, mechanical ventilation, or under scripted tasks,37, 38, 54 we would have found significantly smaller associations. Given the sizable effect the residential I/O had on our estimates for association, future studies should consider the potential interaction between temperature, window openness, and PNC.
We also did not include a particle infiltration factor for time in vehicles or work locations which could bias exposures and effect estimates. We also did not collect data on stove type in our study. Residential exposure to second-hand smoke was reported by 16% of the population indicating that it could affect a small part of our study population.
Field data supported our estimate that air conditioning reduced infiltration by 25%.34 However, a limitation of our assumptions for AC adjustment stems from our decision to use a single temperature cutoff of 21.1 °C, above which we assumed AC was in use. Actual AC use is also dependent upon cost and personal comfort with higher temperatures or dislike of AC. Therefore, our adjustment may over or underestimate the amount air conditioning use.
Due to our relatively small sample size, a limited set of known cardiovascular risk factors were included in the models for association with biomarkers. This restricted our ability to test for multiple categorical variables simultaneously. Additionally, other potential differences in observed effects that might be seen with stratification by covariates were not possible to explore.
A particular strength of our analysis was the availability of a spatial-temporal hourly PNC regression model,23 which when combined with the time-activity data allowed for each hour of the year to be adjusted for each individual study participant. To our knowledge, this is the first time such a model has been used for exposure assessment in an epidemiological study. The cross-validated R2 values obtained for the CAFEH Somerville model (0.38–0.47) were similar to those for other models with spatial and temporal constraints (0.23–0.51).55, 56, 57, 58 The CAFEH PNC regression model was developed via a mobile monitoring effort that included monitoring near the homes of all study participants, and therefore should have captured the range of ambient PNC to which they were exposed.
Utilization of an hourly PNC regression model permitted adjustment of time activity to be applied for each hour of the year rather than after calculating an annual average. This allows for hourly variability in PNC throughout the year, so that both diurnal and seasonal PNC levels are integrated into the annual average TAA-PNC value.59, 60 The hourly resolved PNC regression model, as would be expected, had a lower R2 than land use regression models with greater averaging times,23, 57, 58 but the ability to capture diurnal variations in development of annual average exposure estimates may lead to reduced uncertainty. We accepted lower R2 to have greater temporal resolution in the model to address the rapid temporal changes in PNC levels.23 That said, given the R2 of our PNC regression model and the small sample size of our study, exposure prediction without incorporating corresponding uncertainties could bias our effect estimates. Future work will be needed to develop models that reduce exposure misclassification further by explaining more of the variability in PNC, perhaps through use of mechanistic models or machine learning algorithms.61, 62 Additionally, part of exposure to UFPs was assigned post blood draw which may have introduced error in PNC assignment if there were large differences in exposure from year to year. However, recent studies have reported TRAP LUR models developed as much as 10–12 years apart to be stable.63, 64
CONCLUSIONS
We identified significant differences in exposure assignment between RAA-PNC and TAA-PNC. Further, TAA-PNC models increased the estimate of effect for associations with hsCRP and IL-6 leading to more biologically plausible exposure-response functions, consistent with multiple reports in the literature of toxicity and association with health effects in humans and animals.13, 14, 15, 16, 17, 18, 19, 65 These results improve our knowledge of possible association of UFP with CVD, because they provide some evidence that TAA may reduce exposure misclassification and improve the interpretability of epidemiological studies. Our approach is feasible and can be applied in health studies that have both hourly exposure models for TRAPs (such as UFP) and personal time-activity data. Our findings contribute to evidence that there is value to considering personal time activity in epidemiological analysis of pollutants with high spatial and temporal variability.
Acknowledgments
We are grateful to the CAFEH Steering Committee including Ellin Reisner, Baolian Kuang, Michelle Liang, Christina Hemphill Fuller, Lydia Lowe, Edna Carrasco, M Barton Laws, and Mario Davila. We also acknowledge the great help from our community partner the Somerville Transportation Equity Partnership (STEP). We thank our project manager Don Meglio and his field team—Kevin Stone, Marie Manis, Consuelo Perez, Marjorie Alexander, Maria Crispin, Reva Levin, Helene Sroat, Carmen Rodriguez, Migdalia Tracy, Sidia Escobar, and Betsy Rodman—for their dedication and hard work. We received analytical advice from David Arond, Sharon Sagiv, and Junenette Peters; as well as database support of Deena Wang. Luz Padró-Martínez, Jeffrey Trull, Eric Wilburn, Piers MacNaughton, Tim McAuley, Samantha Weaver, Caitlin Collins, and Jessica Perkins contributed to the mobile monitoring and PNC modeling effort. Funding for CAFEH was provided by the National Institute of Environmental Health Sciences (NIEHS) (Grant No. ES015462). Support for CAFEH was also provided by the Jonathan M. Tisch College of Citizenship and Public Service and the Tufts Community Research Center. Predoctoral support for KJL and APP was provided by the Environmental Protection Agency (EPA) Science to Achieve Results graduate fellowship program (Grant Nos.: FP-917349 and FP-917203). This manuscript has not been formally reviewed by the EPA. The views expressed in this manuscript are solely those of the authors, and EPA does not endorse any products or commercial services mentioned in this manuscript.
Author Contributions
KJL was the lead writer and analyst. JIL and MKS contributed to the writing and meaningful intellectual ideas that affected the activity adjusted interpretation and analysis of our data. AP contributed to the literature review, conducted the PNC regression modeling and provided intellectual ideas to the time-activity analysis. JLD oversaw the development of the PNC model and contributed to the writing and development of tables and figures for the PNC data. WZ helped design the analysis and contributed to the literature reviews and to its interpretation. MM oversaw the statistical analysis and assisted in the writing of that section of the paper. DB directed the study, provided primary oversight to the analysis and contributed to the writing. All authors read the manuscript multiple times, provided input and approved the version as submitted.
Appendix 1
Appendix 1 CAFEH Study Cohort Summary
CAFEH is a community-based participatory research (CBPR) study of traffic-related air pollution (TRAP) and cardiovascular health in individuals 40+ years of age living in close proximity to the major highways interstate 93 and/or Interstate 90 (NIEHS ES015462; PI Brugge). The subpopulation for the analysis reported here is from the City of Somerville, MA, which is a densely populated suburb located roughly 3 miles north from the center of Boston, MA. Somerville has a large number of multi-family dwellings, and public and elderly housing facilities located within close proximity to an eight lane interstate highway (I-93) that runs north-south through the city. Somerville is the first exit before Boston along I-93, resulting in consistent traffic congestion throughout the morning and evening commuter periods each weekday. The Somerville-based study population (N=204) was established via a geographically-weighted randomly-selected address recruitment effort from July 2009 through July 2010. The random sample (n=139) was supplemented by a convenience sample (n=65) of residents in two senior housing developments. All participants willing to participate in the CAFEH study completed a consent form certified by Tufts University School of Medicine and questionnaire at their place of residence that provided demographic information (age, gender, income, education, race, etc.) and information on a variety of other topics related to our exposure and health outcomes of interest (time activity, diet, physical activity, stress, medications, diagnosed illnesses, etc.). A subset of CAFEH participants attended a study clinic at least once (n=140) and submitted a viable peripheral blood sample for analysis of inflammatory biomarkers. The populations recruited to the CAFEH cohort lived in both a near-highway (NH; ≤500 m from highway) and urban background (UB;≥1000 m from highway) location from which participants were recruited.
In summary, the CAFEH analysis is a cross-sectional study of monitored and modeled UFP measured as particle number concentration (PNC) and that collected the corresponding human data, including time-activity data and biomarkers of systemic inflammation from near-highway and urban background populations.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Journal of Exposure Science and Environmental Epidemiology website (http://www.nature.com/jes)
Supplementary Material
References
- Hoffmann B, Moebus S, Stang A, Beck EM, Dragano N, Möhlenkamp S, et al. Residence close to high traffic and prevalence of coronary heart disease. Eur Heart J. 2006;27:2696–2702. doi: 10.1093/eurheartj/ehl278. [DOI] [PubMed] [Google Scholar]
- Hoffmann B, Moebus S, Möhlenkamp S, Stang A, Lehmann N, Dragano N, et al. Residential Exposure to Traffic Is Associated With Coronary Atherosclerosis. Circulation. 2007;116:489–496. doi: 10.1161/CIRCULATIONAHA.107.693622. [DOI] [PubMed] [Google Scholar]
- Tonne C, Melly S, Mittleman M, Coull B, Goldberg R, Schwartz J. A case–control analysis of exposure to traffic and acute myocardial infarction. Environ Health Perspect. 2007;115:53–57. doi: 10.1289/ehp.9587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugge D, Durant JL, Rioux C. Near-highway pollutants in motor vehicle exhaust: a review of epidemiologic evidence of cardiac and pulmonary health risks. Environ Health. 2007;6:23. doi: 10.1186/1476-069X-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan WQ, Tamburic L, Davies HW, Demers PA, Koehoorn M, Brauer M. Changes in residential proximity to road traffic and the risk of death from coronary heart disease. Epidemiology. 2010;21:642–649. doi: 10.1097/EDE.0b013e3181e89f19. [DOI] [PubMed] [Google Scholar]
- Hoffmann B, Moebus S, Dragano N, Stang A, Möhlenkamp S, Schmermund A, et al. Chronic residential exposure to particulate matter air pollution and systemic inflammatory markers. Environ Health Perspect. 2009;117:1302–1308. doi: 10.1289/ehp.0800362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LA, Ulrich CM, Larson T, Wener MH, Wood B, Campbell P, et al. Proximity to traffic, inflammation, and immune function among women in the Seattle, Washington, area. Environ Health Perspect. 2009;117:374–378. doi: 10.1289/ehp.11580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rioux CL, Tucker KL, Mwamburi M, Gute DM, Cohen SA, Brugge D. Residential traffic exposure, pulse pressure, and C-reactive protein: consistency and contrast among exposure characterization methods. Environ Health Perspect. 2010;118:803–811. doi: 10.1289/ehp.0901182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugge D, Lane K, Padró-Martínez LT, Stewart A, Hoesterey K, Weiss D, et al. Highway proximity associated with cardiovascular disease risk: the influence of individual-level confounders and exposure misclassification. Environ Health. 2013;12:84. doi: 10.1186/1476-069X-12-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karner AA, Eisinger DS, Niemeier DA. Near-roadway air quality: synthesizing the findings from real-world data. Environ Sci Technol. 2010;44:5334–5344. doi: 10.1021/es100008x. [DOI] [PubMed] [Google Scholar]
- Geiser M, Rothen-Rutishauser B, Kapp N, Schürch S, Kreyling W, Schulz H, et al. Ultrafine particles cross cellular membranes by nonphagocytic mechanisms in lungs and in cultured cells. Environ Health Perspect. 2005;113:1555–1560. doi: 10.1289/ehp.8006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araujo JA, Barajas B, Kleinman M, Wang X, Bennett BJ, Gong KW, et al. Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circ Res. 2008;102:589–596. doi: 10.1161/CIRCRESAHA.107.164970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araujo JA, Nel AE. Particulate matter and atherosclerosis: role of particle size, composition and oxidative stress. Part Fibre Toxicol. 2009;6:24. doi: 10.1186/1743-8977-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemmar A, Hoet PH, Vanquickenborne B, Dinsdale D, Thomeer M, Hoylaerts MF, et al. Passage of inhaled particles into the blood circulation in humans. Circulation. 2002;105:411–414. doi: 10.1161/hc0402.104118. [DOI] [PubMed] [Google Scholar]
- Samet JM, Rappold A, Graff D, Cascio WE, Berntsen JH, Huang YC, et al. Concentrated ambient ultrafine particle exposure induces cardiac changes in young healthy volunteers. Am J Respir Crit Care Med. 2009;179:1034–1042. doi: 10.1164/rccm.200807-1043OC. [DOI] [PubMed] [Google Scholar]
- Delfino RJ, Staimer N, Tjoa T, Polidori A, Arhami M, Gillen DL, et al. Circulating biomarkers of inflammation, antioxidant activity, and platelet activation are associated with primary combustion aerosols in subjects with coronary artery disease. Environ Health Perspect. 2008;116:898–906. doi: 10.1289/ehp.11189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino RJ, Staimer N, Tjoa T, Gillen DL, Polidori A, Arhami M, et al. Air pollution exposures and circulating biomarkers of effect in a susceptible population: clues to potential causal component mixtures and mechanisms. Environ Health Perspect. 2009;117:1232–1238. doi: 10.1289/ehp.0800194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertel S, Viehmann A, Moebus S, Mann K, Bröcker-Preuss M, Möhlenkamp S, Nonnemacher M, Erbel R, Jakobs H, Memmesheimer M, Jöckel KH, Hoffmann B. Influence of short-term exposure to ultrafine and fine particles on systemic inflammation. Eur J Epidemiol. 2010;25:581–592. doi: 10.1007/s10654-010-9477-x. [DOI] [PubMed] [Google Scholar]
- Delfino RJ, Staimer N, Tjoa T, Arhami M, Polidori A, Gillen DL, et al. Association of biomarkers of systemic inflammation with organic components and source tracers in quasi-ultrafine particles. Environ Health Perspect. 2010;118:756–762. doi: 10.1289/ehp.0901407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitner S, Liu L, Cyrys J, Brüske I, Franck U, Schlink U, et al. Sub-micrometer particulate air pollution and cardiovascular mortality in Beijing, China. Sci Total Environ. 2011;409:5196–5204. doi: 10.1016/j.scitotenv.2011.08.023. [DOI] [PubMed] [Google Scholar]
- Durant JL, Ash CA, Wood EC, Herndon SC, Jayne JT, Knighton WB, et al. Short-term variation in near-highway air pollutant gradients on a winter morning. Atmos Chem Phys. 2010;10:8341–8352. doi: 10.5194/acpd-10-5599-2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padró-Martínez LT, Patton AP, Trull JB, Zamore W, Brugge D, Durant JL. Mobile monitoring of particle number concentration and other traffic-related air pollutants in a near-highway neighborhood over the course of a year. Atmos Environ. 2012;61:253–264. doi: 10.1016/j.atmosenv.2012.06.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton AP, Collins C, Naumova EN, Zamore W, Brugge D, Durant JL. An hourly regression model for ultrafine particles in a near-highway urban area. Environ Sci Technol. 2014;48:3272–3280. doi: 10.1021/es404838k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino RJ, Sioutas C, Malik S. Potential role of ultrafine particles in associations between airborne particle mass and cardiovascular health. Environ Health Perspect. 2005;113:934–946. doi: 10.1289/ehp.7938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sioutas C, Delfino RJ, Singh M. Exposure assessment for atmospheric ultrafine particles (UFPs) and implications in epidemiologic research. Environ Health Perspect. 2005;113:947–955. doi: 10.1289/ehp.7939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Effects Institute Understanding the health effects of ambient ultrafine particles. Perspectives. 2013;3:1–108. [Google Scholar]
- Panis L. New Directions: Air pollution epidemiology can benefit from activity-based models. Atmos Environ. 2010;44:1003–1004. [Google Scholar]
- Lane KJ, Kangsen Scammell M, Levy JI, Fuller CH, Parambi R, Zamore W, et al. Positional error and time-activity patterns in near-highway proximity studies: an exposure misclassification analysis. Environ Health. 2013;12:75. doi: 10.1186/1476-069X-12-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckx C, Panis L, Arentze T, Janssens D, Torfs R, Broekx S, et al. A dynamic activity-based population modeling approach to evaluate exposure to air pollution: methods and application to a Dutch urban area. Environ Impact Assess Rev. 2009;29:179–185. [Google Scholar]
- Dons E, Int Panis L, Poppel MV, Theunis J, Willems H, Torfs R, et al. Impact of time activity patterns on personal exposure to black carbon. Atmos Environ. 2011;45:3594–3602. [Google Scholar]
- Buonanno G, Stabile L, Morawska L. Personal exposure to ultrafine particles: the influence of time-activity patterns. Sci Total Environ. 2014;468-469:903–907. doi: 10.1016/j.scitotenv.2013.09.016. [DOI] [PubMed] [Google Scholar]
- Fuller CH, Patton AP, Lane K, Laws MB, Marden A, Carrasco E, et al. A community participatory study of cardiovascular health and exposure to near-highway air pollution: study design and methods. Rev Environ Health. 2013;28:21–35. doi: 10.1515/reveh-2012-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song C, Qu Z, Blumm N, Barabasi A. Limits of predictability in human mobility. Science. 2010;327:1018–1021. doi: 10.1126/science.1177170. [DOI] [PubMed] [Google Scholar]
- Fuller CH, Brugge D, Williams PL, Mittleman MA, Lane K, Durant JL, et al. Indoor and outdoor measurements of particle number concentration in near-highway homes. J Expos Sci Environ Epidemiol. 2013;23:506–512. doi: 10.1038/jes.2012.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team R: A Language and Environment for Statistical Computing R Foundation for Statistical Computing: Vienna, Austria; 2014. URL http://www.R-project.org/ ]. [Google Scholar]
- Hastie Trevor.2013. Generalized Additive Models. R Package version 1.09.1.
- Zhu Y, Hinds WC, Krudysz M, Kuhn T, Froines JR, Sioutas C. Penetration of freeway ultrafine particles into indoor environments. J Aerosol Sci. 2004;36:303–322. [Google Scholar]
- McAuley TR, Fisher R, Zhou X, Jaques PA, Ferro AR. Relationships of outdoor and indoor ultrafine particles at residences downwind of a major international border crossing in Buffalo, NY. Indoor Air. 2010;20:298–308. doi: 10.1111/j.1600-0668.2010.00654.x. [DOI] [PubMed] [Google Scholar]
- Bhangar S, Mullen NA, Hering SV, Kreisberg NM, Nazaroff WW. Ultrafine particle concentrations and exposures in seven residences in northern California. Indoor Air. 2010;21:132–144. doi: 10.1111/j.1600-0668.2010.00689.x. [DOI] [PubMed] [Google Scholar]
- Rim D, Wallace LA, Persily AK. Indoor ultrafine particles of outdoor origin: importance of window opening area and fan operation condition. Environ Sci Technol. 2013;47:1922–1929. doi: 10.1021/es303613e. [DOI] [PubMed] [Google Scholar]
- Kearney J, Wallace L, MacNeill M, Héroux ME, Kindzierski W, Wheeler A. Residential infiltration of fine and ultrafine particles in Edmonton. Atmos Environ. 2014;94:793–805. [Google Scholar]
- Zhu Y, Eiguren-Fernandez A, Hinds WC, Miguel AH. In-cabin commuter exposure to ultrafine particles on Los Angeles Freeways. Environ Sci Technol. 2007;41:2138–2145. doi: 10.1021/es0618797. [DOI] [PubMed] [Google Scholar]
- Knibbs LD, de Dear RJ, Morawska L. Effect of cabin ventilation rate on ultrafine particle exposure inside automobiles. Environ Sci Technol. 2010;44:3546–3551. doi: 10.1021/es9038209. [DOI] [PubMed] [Google Scholar]
- Hudda N, Kostenidou E, Sioutas C, Delfino RJ, Fruin SA. Vehicle and driving characteristics that influence in-cabin particle number concentrations. Environ Sci Technol. 2011;45:8691–8697. doi: 10.1021/es202025m. [DOI] [PubMed] [Google Scholar]
- Hudda N, Eckel SP, Knibbs LD, Sioutas C, Delfino RJ, Fruin SA. Linking in-vehicle ultrafine particle exposures to on-road concentrations. Atmos Environ. 2012;59:578–586. doi: 10.1016/j.atmosenv.2012.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setton EM, Keller CP, Cloutier-Fisher D, Hystad PW. Spatial variations in estimated chronic exposure to traffic-related air pollution in working populations: a simulation. Int J Health Geogr. 2008;7:39. doi: 10.1186/1476-072X-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kioumourtzoglou MA, Spiegelman D, Szpiro AA, Sheppard L, Kaufman JD, Yanosky JD, et al. Exposure measurement error in PM2.5 health effects studies: a pooled analysis of eight personal exposure validation studies. Environ Health. 2014;13:2. doi: 10.1186/1476-069X-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace L, Ott W. Personal exposure to ultrafine particles. J Expo Sci Environ Epidemiol. 2010;21:20–30. doi: 10.1038/jes.2009.59. [DOI] [PubMed] [Google Scholar]
- Wang M, Beelen R, Bellander T, Birk M, Cesaroni G, Cirach M, et al. Performance of multi-city land use regression models for nitrogen dioxide and fine particles. Environ Health Perspect. 2014;122:843–849. doi: 10.1289/ehp.1307271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Tsai MY, Keidel D, Gemperli A, Ineichen A, Hazenkamp-von Arx M, Bayer Oglesby L, Rochat T, Künzli N, Ackermann-Liebrich U, Straehl P, Schwartz J, Schindler C. Long term exposure models for traffic related NO2 across geographically diverse areas over separate years. Atmos Environ. 2012;46:460–471. [Google Scholar]
- Blangiardo M, Hansell A, Richardson S. A Bayesian model of time activity data to investigate health effect of air pollution in time series studies. Atmos Environ. 2011;45:379–386. [Google Scholar]
- Dons E, Van Poppel M, Kochan B, Wets G, Panis LI. Implementation and validation of a modeling framework to assess personal exposure to black carbon. Environ Int. 2014;62:64–71. doi: 10.1016/j.envint.2013.10.003. [DOI] [PubMed] [Google Scholar]
- Panis LI, De Geus Bas, Vandenbulcke G, Willems H, Degraeuwe B, Bleux N, et al. Exposure to particulate matter in traffic: a comparison of cyclists and car passengers. Atmos Environ. 2010;44:2263–2270. [Google Scholar]
- Cyrys J, Pitz M, Bischof W, Wichmann HE, Heinrich J. Relationship between indoor and outdoor levels of fine particle mass, particle number concentrations and black smoke under different ventilation conditions. J Expos Anal Environ Epidemiol. 2004;14:275–283. doi: 10.1038/sj.jea.7500317. [DOI] [PubMed] [Google Scholar]
- Zwack LM, Paciorek CJ, Spengler JD, Levy JI. Modeling spatial patterns of traffic-related air pollutants in complex urban terrain. Environ Health Perspect. 2011;119:852–859. doi: 10.1289/ehp.1002519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera M, Basagaña X, Aguilera I, Agis D, Bouso L, Foraster M, et al. Spatial distribution of ultrafine particles in urban settings: A land use regression model. Atmos Environ. 2012;54:657–666. [Google Scholar]
- Li L, Wu J, Hudda N, Sioutas C, Fruin S, Delfino RJ. Modeling the concentrations of on-road air pollutants in southern California. Environ Sci Technol. 2013;47:9291–9299. doi: 10.1021/es401281r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller CH, Brugge D, Williams P, Mittleman M, Durant JL, Spengler JD. Estimation of ultrafine particle concentrations at near-highway residences using data from local and central monitors. Atmos Environ. 2012;57:257–265. doi: 10.1016/j.atmosenv.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoek G, Beelen R, Kos G, Dijkema M, van der Zee SC, Fischer PH, Brunekreef B. Land use regression model for ultrafine particles in Amsterdam. Environ Sci Technol. 2011;45:622–628. doi: 10.1021/es1023042. [DOI] [PubMed] [Google Scholar]
- Hoek G, Kos G, Harrison R, de Hartog J, Meliefste K, ten Brink H, et al. Indoor–outdoor relationships of particle number and mass in four European cities. Atmos Environ. 2008;42:156–169. [Google Scholar]
- Holmes S, Morawska L. A review of dispersion modelling and its application to the dispersion of particles: an overview of different dispersion models available. Atmos Environ. 2006;40:5902–5928. [Google Scholar]
- Singh KP, Gupta S, Rai P. Identifying pollution sources and predicting urban air quality using ensemble learning methods. Atmos Environ. 2013;80:426–437. [Google Scholar]
- Eeftens M, Beelen R, Fischer P, Brunekreef B, Meliefste K, Hoek G. Stability of measured and modelled spatial contrasts in NO2 over time. Occup Environ Med. 2011;68:765–770. doi: 10.1136/oem.2010.061135. [DOI] [PubMed] [Google Scholar]
- Wang R, Henderson SB, Sbihi H, Allen RW, Brauer M. Temporal stability of land use regression models for traffic-related air pollution. Atmos Environ. 2013;64:312–319. [Google Scholar]
- Araujo JA, Barajas B, Kleinman M, Wang X, Bennett BJ, Gong KW, Navab M, Harkema J, Sioutas C, Lusis AJ, Nel AE. Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circ Res. 2008;102:589–596. doi: 10.1161/CIRCRESAHA.107.164970. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.