Supplemental Digital Content is available in the text.
Keywords: anticoagulants, atrial fibrillation, hemorrhage, stroke
Background and Purpose—
The use of vitamin K antagonists (VKAs), the cornerstone treatment for stroke prevention in patients with atrial fibrillation, is limited by the perceived risk of serious bleeding in Asia. Non-VKA oral anticoagulants (NOACs) are safer alternatives. Here, we evaluate performance differences of NOACs between Asians and non-Asians.
Methods—
We compared efficacy and safety of NOACs between patients enrolled in Asian and non-Asian countries using aggregative data from phase III clinical trials. The odds ratios (ORs [95% confidence interval]) were calculated by a random effects model.
Results—
Comparing with VKAs, standard-dose NOACs reduced stroke or systemic embolism (OR=0.65 [0.52–0.83] versus 0.85 [0.77–0.93], P interaction= 0.045) more in Asians than in non-Asians and were safer in Asians than in non-Asians about major bleeding (OR=0.57 [0.44–0.74] versus 0.89 [0.76–1.04], P interaction=0.004), hemorrhagic stroke (OR=0.32 [0.19–0.52] versus 0.56 [0.44–0.70], P interaction=0.046) in particular, whereas gastrointestinal bleeding was significantly increased in non-Asians (OR=0.79 [0.48–1.32] versus 1.44 [1.12–1.85], P interaction=0.041). Generally, low-dose NOACs were safer than VKAs without heterogeneity in efficacy and safety between Asians and non-Asians, except for ischemic stroke, major, and gastrointestinal bleeding.
Conclusions—
Our findings suggest that standard-dose NOACs were more effective and safer in Asians than in non-Asians, whereas low-dose NOACs performed similarly in both populations.
Stroke prevention with vitamin K antagonists (VKAs) is essential in the management of atrial fibrillation (AF).1 However, it has been generally perceived that Asian patients are naturally more sensitive to VKAs and have unacceptably higher rates of intracranial hemorrhage (ICH) even when international normalized ratio is ideally maintained.2 Consequently, VKAs have been largely underused or underdosed in Asian patients.3 Despite the average time in therapeutic range with VKAs was lower in Asian patients than that in non-Asian patients in clinical trials,4,5 the rates of major bleeding (ICH in particular) were significantly higher in Asian patients.4,6
The development of non-VKA oral anticoagulants (NOACs) has changed the landscape of stroke prevention in patients with AF, with 4 agents available namely dabigatran, rivaroxaban, apixaban, and edoxaban being tested in large phase III clinical trials.7–10 The availability of NOACs is of paramount importance to Asian patients who are prone to bleeding, including devastating ICH with or without VKAs.2,11 The observations from the Japanese Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared With Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (J-ROCKET AF) might even imply that different dosing strategies should be applied according to ethnicities, weight, and renal function.12 Several prior observations suggest that NOACs were more preferentially indicated for stroke prevention in Asian patients with AF than VKAs.4,6,13
Although each trial was powered to address primary efficacy and safety outcomes of the overall patients who have been enrolled, the benefit and risk profiles of NOACs in Asian patients need proper description given the fact that the burden of AF and its associated complications is substantially higher in Asia than in the rest of the world because Asia is the most populated region and has fast-growing aging societies.14,15 Since nonwhite ethnicities, particularly Asians, are a major factor attributable to ICH in anticoagulated patients,16–18 more Asian patients would have been deemed ineligible for treatment because of higher risk of bleeding.19 However, prior analyses of the individual approved NOACs were underpowered to show quantitative differences in various outcomes between Asian and non-Asian patients.20–23
In this meta-analysis, we aimed to assess the differences in efficacy and safety outcomes of NOACs in Asian patients compared with non-Asian patients that have not been addressed in previously published meta-analyses.24–27 Thus, these data are new and important for patients, physicians, and other healthcare professionals in this region.
Methods
Data Sources and Searches
We searched PubMed database (from January 2009 to July 2014), clinical trial registries, and relevant conference proceedings using the terms AF, warfarin, apixaban, dabigatran, edoxaban, rivaroxaban, and stroke. Ximelagatran was excluded from the search because it has been withdrawn from the market. No language restriction was imposed. The reference lists of published meta-analyses were also reviewed.
We consider randomized controlled trials comparing NOACs with VKAs in patients with nonvalvular AF. Trials were eligible for inclusion if they (1) involved >500 patients with nonvalvular AF; (2) reported both long-term efficacy and safety outcomes in Asian patients; and (3) had follow-up ≥1 year.
Data Extraction
All efficacy and safety outcomes were extracted. The efficacy outcomes include the composite of stroke or systemic embolism, ischemic stroke, myocardial infarction, and death from any cause; the safety outcomes were major bleeding, ICH, hemorrhagic stroke, and gastrointestinal bleeding. Definitions of those outcomes were the same across all trials, with the exception for major bleeding where the trial-specific definitions were adopted. In addition, gastrointestinal bleeding has not been universally reported in Asian patients. Data were used from the intention-to-treat populations for evaluating the efficacy outcomes except for J-ROCKET AF, which was primarily designed for evaluating safety outcomes. The differences in efficacy and safety outcomes of NOACs compared with VKAs among Asian and non-Asian patients were the interest of this meta-analysis.
Definition of Asian Patients
Because the individual patient-level data were not available, we could not ascertain the ethnicity of each patient enrolled in the trials. We therefore assumed that residence reported in the trials is a surrogate for ethnicity.
Data Synthesis and Analysis
Primary Analysis
Two doses of dabigatran and edoxaban were tested in the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) and the Effective Anticoagulation With Factor Xa Next Generation in Atrial Fibrillation–Thrombolysis in Myocardial Infarction 48 (ENGAGE AF-TIMI 48), respectively, and the low dose of rivaroxaban was compared with VKAs in J-ROCKET AF. Instead of combining data from different doses into one meta-analysis, which merges the therapeutic implications of different doses that might have diverse risk-benefit profiles, we conducted 2 separate meta-analyses. The meta-analysis for standard-dose NOACs included data of dabigatran 150 mg, edoxaban 60 mg, rivaroxaban 20 mg, and apixaban 5 mg. The meta-analysis for low-dose NOACs included data of dabigatran 110 mg, edoxaban 30 mg, and rivaroxaban 15 mg.
Sensitivity Analysis
Data of Asian patients have not been homogenously published in detail. In the prior subanalyses reporting efficacy/safety among Asian and non-Asian patients, there were 5, 1, and 3 Asian countries included as non-Asian countries in the Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF),21 the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE),22 and ENGAGE AF-TIMI 48,23 respectively. In addition, patients enrolled in Asian countries might not necessarily be ethnically Asian, vice versa. To mitigate the confounding of such heterogeneous data, we performed 3 sensitivity analyses by (1) examining data of 3 factor Xa inhibitors, and using (2) ethnicity-level, and (3) region-level information available from regulatory agencies. The outcome data used for sensitivity analyses were limited. Therefore, we could only investigate the composite of stroke or systemic embolism and major bleeding with respect to standard-dose NOACs compared with VKAs.
The odds ratio (OR) and associated 95% confidence interval (CI) were calculated for each outcome and trial separately and for the pooled results that were compared with DerSimonian and Laird random effects model. Heterogeneity between trials was assessed using the Cochran Q statistic and I2 test. Interaction between Asian and non-Asian patients about therapeutic outcomes of NOACs compared with VKAs was systematically tested. Statistical analysis was performed using Comprehensive Meta-Analysis software, version 2 (Biostat Inc, NJ).
Results
Of the 78 studies identified from the literature search, 73 were excluded because of reports of the trial design, subgroup analyses without data of Asian patients, short follow-up, and limited patient numbers (Figure I in the online-only Data Supplement). The characteristics of the trials and treatment included in this meta-analysis are shown in Table I in the online-only Data Supplement. The 5 included studies namely RE-LY, ROCKET AF, J-ROCKET AF, ARISTOTLE, and ENGAGE AF-TIMI 48 comprised 8928 Asian patients (5250 with NOACs and 3678 with VKAs) and 64 033 non-Asian patients (37 800 with NOACs and 26 233 with VKAs).
Standard-Dose NOACs Versus VKAs
The comparative efficacy of standard-dose NOACs and VKAs is presented in Figure 1. Standard-dose NOACs significantly reduced the composite of stroke or systemic embolism both in Asian and non-Asian patients (OR, 0.65; 95% CI, 0.52–0.83; P<0.001 for Asian patients; OR, 0.85; 95% CI, 0.77–0.93; P<0.001 for non-Asian patients). The reduction was more prominent in Asian patients than in non-Asian patients (P interaction=0.045). The effect of standard-dose NOACs on ischemic stroke and myocardial infarction was comparable with VKAs in both Asian and non-Asian patients (P interaction=0.673 and 0.977, respectively). All-cause mortality was significantly lower in both with standard-dose NOACs than with VKAs (OR, 0.80; 95% CI, 0.65–0.98; P=0.030 for Asian patients; OR, 0.91; 95% CI, 0.86–0.97; P=0.003 for non-Asian patients; P interaction=0.219).
Figure 1.
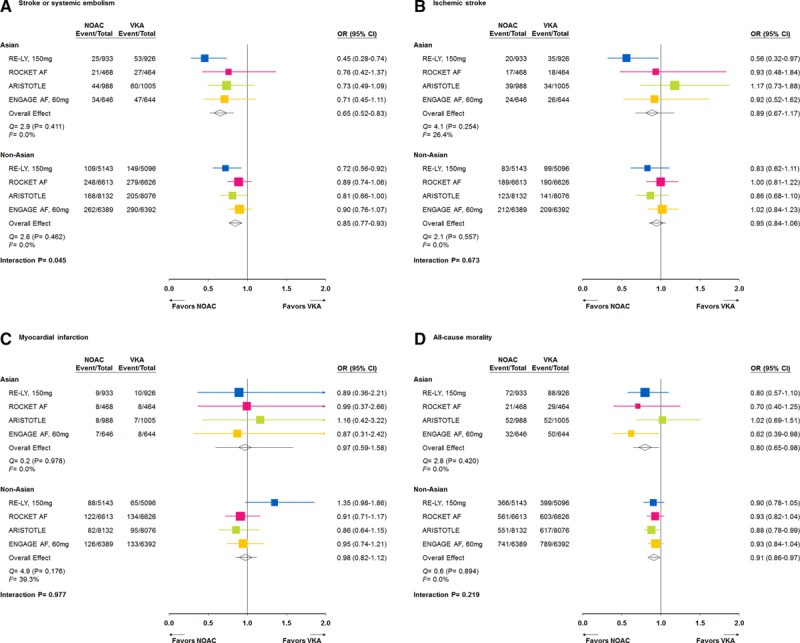
Efficacy outcomes of stroke or systemic embolism (A), ischemic stroke (B), myocardial infarction (C), and all-cause mortality (D) for the standard-dose non–vitamin K antagonist (VKA) oral anticoagulants (NOACs) vs VKAs. CI indicates confidence interval; and OR, odds ratio.
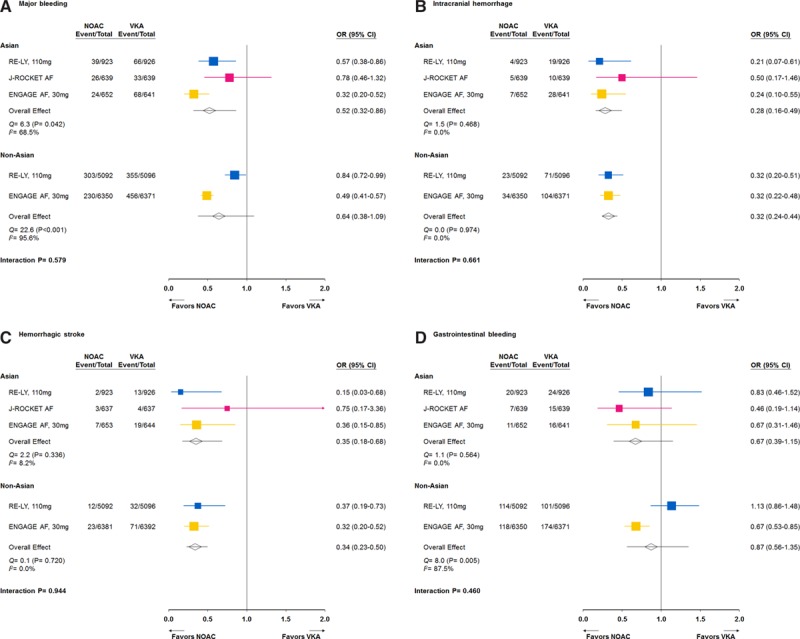
Figure 2 shows the preferential benefit of standard-dose NOACs in safety outcomes in Asian patients. Standard-dose NOACs reduced major bleeding more in Asian than in non-Asian patients (OR, 0.57; 95% CI, 0.44–0.74; P<0.001 for Asian patients; OR, 0.89; 95% CI, 0.76–1.04; P=0.143 for non-Asian patients; P interaction=0.004). ICH was significantly reduced in both with standard-dose NOACs (OR, 0.33; 95% CI, 0.22–0.50; P<0.001 for Asian patients; OR, 0.52; 95% CI, 0.42–0.64; P<0.001 for non-Asian patients; P interaction=0.059). Standard-dose NOACs had a substantial reduction in hemorrhagic stroke, which was more notable in Asian than in non-Asian patients (OR, 0.32; 95% CI, 0.19–0.52; P<0.001 for Asian patients; OR, 0.56; 95% CI, 0.44–0.70; P<0.001 for non-Asian patients; P interaction=0.046) compared with VKAs. Moreover, standard-dose NOACs increased the risk of gastrointestinal bleeding in non-Asian patients but not in Asian patients (OR, 1.44; 95% CI, 1.12–1.85; P=0.005 for non-Asian patients; OR, 0.79; 95% CI, 0.48–1.32; P=0.378 for Asian patients; P interaction=0.041).
Figure 2.

Safety outcomes of major bleeding (A), intracranial hemorrhage (B), hemorrhagic stroke (C), and gastrointestinal bleeding (D) for the standard-dose non–vitamin K antagonist (VKA) oral anticoagulants (NOACs) vs VKAs. CI indicates confidence interval; and OR, odds ratio.
Low-Dose NOACs Versus VKAs
The comparative efficacy of low-dose NOACs and VKAs with regard to the various efficacy outcomes is presented in Figure 3. Low-dose NOACs had similar efficacy to VKAs on stroke or systemic embolism and ischemic stroke both in Asian and non-Asian patients (P interaction=0.353 and 0.504, respectively). With regard to myocardial infarction, non-Asian patients had more events with low-dose NOACs than with VKAs (OR, 1.28; 95% CI, 1.06–1.55; P=0.010), whereas the effect of low-dose NOACs seemed to be similar to VKAs in Asian patients (OR, 0.92; 95% CI, 0.48–1.79; P=0.816); however, there was no statistic heterogeneity (P interaction=0.352). Low-dose NOACs were associated with a significant reduction in all-cause mortality in non-Asian patients and a trend for a reduction in Asian patients (P interaction=0.934).
Figure 3.
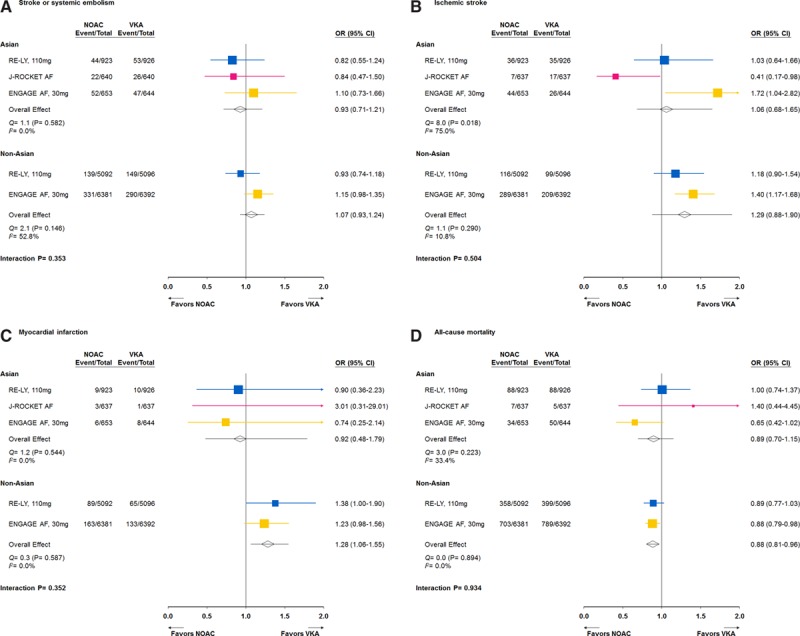
Efficacy outcomes of stroke or systemic embolism (A), ischemic stroke (B), myocardial infarction (C), and all-cause mortality (D) for the low-dose non–vitamin K antagonist (VKA) oral anticoagulants (NOACs) vs VKAs. CI indicates confidence interval; and OR, odds ratio.
The safety outcomes of low-dose NOACs are presented in Figure 4. Low-dose NOACs reduced major bleeding, ICH, and hemorrhagic stroke in both Asian and non-Asian patients (P interaction=0.579, 0.661, and 0.944, respectively). There was no difference in gastrointestinal bleeding in Asians and non-Asians (P interaction=0.460).
Figure 4.
Safety outcomes of major bleeding (A), intracranial hemorrhage (B), hemorrhagic stroke (C), and gastrointestinal bleeding (D) for the low-dose non–vitamin K antagonist (VKA) oral anticoagulants (NOACs) vs VKAs. CI indicates confidence interval; and OR, odds ratio.
Sensitivity Analysis
The sensitivity analysis undertaken using factor Xa inhibitor trials showed parallel results to the primary analyses except for stroke or systemic embolism (Table II in the online-only Data Supplement). Additional analyses using data available from the regulatory agency indicated the qualitatively similar results to our primary analyses that standard-dose NOACs significantly reduced stroke or systemic embolism and major bleeding to a greater degree in Asian than in non-Asian patients (Figures II and III in the online-only Data Supplement).
Discussion
Our study is the first meta-analysis of large phase III clinical trials that compared NOACs with VKAs in Asian and non-Asian patients with regard to both efficacy and safety outcomes. This analysis included >8000 Asian patients; the responses to NOACs were qualitatively similar between Asian and non-Asian patients with quantitatively greater benefits in Asian patients. Our data suggest that both standard-dose and low-dose NOACs are preferentially indicated in Asian patients for the prevention of AF-associated stroke rather than VKAs.
Previous meta-analyses consistently showed that standard-dose NOACs were more effective than VKAs on the reduction of stroke or systemic embolism.24–27 In our analysis, standard-dose NOACs were more effective than VKAs in both Asian and non-Asian patients, but NOACs fared even better in Asian patients. In addition, standard-dose NOACs were more effective on the reduction of hemorrhagic stroke in Asian than in non-Asian patients, which is most likely attributed to a higher bleeding risk with VKAs in Asian patients.
The major criticism of standard-dose NOACs, which has been consistently shown in previous meta-analyses, was that they were less effective on the reduction of major bleeding.25–27 In our analysis, however, standard-dose NOACs were still effective in Asian patients, compared with VKAs. In non-Asian patients, the beneficial effect on major bleeding was marginal. It is possible that NOACs are more effective in Asian patients than in non-Asian patients because the risk of major bleeding in Asian with VKAs is generally higher than in non-Asian patients even though more Asian patients had international normalized ratio <2.0 and less Asian patients had international normalized ratio >3.0.4 The absolute risk of major bleeding with NOACs was numerically lower in Asian than in non-Asian patients (the annual risk was 2.17% versus 3.52%, 3.44% versus 3.60%, and 2.02% versus 2.15%, with dabigatran 150 mg, rivaroxaban 20 mg, and apixaban 5 mg, respectively). Therefore, the absolute risk reduction in major bleeding by standard-dose NOACs was generally greater in Asian than in non-Asian patients.20–23
Another important criticism of standard-dose NOACs is an increase in risk of gastrointestinal bleeding.25–28 We found that the increased risk of gastrointestinal bleeding was only significant in non-Asian patients. Indeed, the numbers for gastrointestinal bleeding in Asian patients were not reported either in ROCKET AF or in ARISTOTLE, but the risk of gastrointestinal bleeding was numerically higher in overall patients with rivaroxaban than with VKAs (3.15% versus 2.16%) in ROCKET AF.8 The risk of digestive tract bleeding was numerically similar in overall patients with apixaban versus VKAs (0.78% versus 0.88%).29 Unlike other bleeding events, gastrointestinal bleeding with VKAs was similar in Asian and in non-Asian patients (1.41% versus 1.01% and 1.11% versus 1.24% for Asian patients versus non-Asian patients in RE-LY and ENGAGE AF-TIMI 48, respectively). Concomitant antiplatelet therapy is an independent predictor for gastrointestinal bleeding.28,30,31 In RE-LY, the concomitant use of aspirin was more common and the use of proton pump inhibitors was less common in Asian than in non-Asian patients, but gastrointestinal bleeding was not increased by dabigatran 150 mg.20 Our findings may suggest that standard-dose NOACs should not be avoided in Asian patients simply on the basis of the risk of gastrointestinal bleeding.
Low-dose NOACs are similarly effective as VKAs in prevention against stroke or systemic embolism for both Asian and non-Asian patients but might not be as effective for protection against ischemic stroke. They are safer than VKAs with respect to hemorrhagic stroke, and no difference could be found between Asian and non-Asian patients. Our analysis suggests that low-dose NOACs were effective on the reduction of major bleeding and ICH in both Asian and non-Asian patients, compared with VKAs. Again, no signal of increased gastrointestinal bleeding was observed. Based on our analysis, low-dose NOACs can be effective and safe alternatives to VKAs in Asian patients and should be considered in patients with higher bleeding risk.
Finally, the general mechanisms involved with the differential effects of NOACs compared with VKAs between Asian and non-Asian patients are yet to be determined. Genetically, Asian patients are more likely to be VKA sensitive or highly sensitive responders, who seem prone to excessive bleeding.32 Except for the variations in distributions of genetic polymorphisms for VKA metabolism,33,34 Asian patients tended to have lower body weight, smaller proportions of prior myocardial infarction, VKA experiences, and the concomitant use of gastric antacid drugs, and greater proportions of impair renal function, prior stroke, nonparoxysmal AF, and the use of antiplatelet medications.20–23 Those demographic differences might be clinically relevant factors for anticoagulant treatment other than ethnic per se.
Limitations
Our analysis has several limitations. First, we did not have individual patient-level data from trials included for this meta-analysis. Without individual patient-level information, some of the patients enrolled in Asian countries described in our meta-analysis might not be ethnically Asian, and some of the Asian patients were included in non-Asian populations in the analyses of clinical trials.21–23 However, the majority of Asian patients would be enrolled in Asia as, for example, only 11 Asian patients were recruited at US sites in ARISTOTLE. In addition, the sensitivity analyses with the available information at ethnic and regional levels from the regulatory agency showed similar results to our primary analyses. Second, the benefit of NOACs in Asian population may be related to genetic polymorphism for VKA metabolism, and lower body weight and creatinine clearance. However, relative efficacy of NOACs is consistent across a broad range of vulnerable patients,27 and a greater reduction in bleeding risk with NOACs compared with VKAs was seen across genotypes,32 body weight,7–9 and renal function.7,8 Finally, there was some heterogeneity between included trials. Therefore, we used a random effects model to account for heterogeneity within individual trials.
Conclusions
Both standard-dose and low-dose NOACs performed equally well, or even better, with regard to efficacy and safety in Asian than in non-Asian patients. Standard-dose NOACs are preferred over VKAs in Asian patients, whereas low-dose NOACs are effective and safe alternatives to VKAs.
Sources of Funding
This work was supported, in part, by grants from the Ministry of Health and Welfare (MOHW104-TDU-B-211-113-003) and from the Ministry of Science and Technology (102-2628-B-075-004-MY3), and intramural grants from the Taipei Veterans General Hospital (V104B-026; V104C-016).
Disclosures
Dr Wang has received honoraria from Bayer and Daiichi-Sankyo. Dr Lip has served as a consultant for Bayer, Biotronik, BMS/Pfizer, Boehringer Ingelheim, Daiichi-Sankyo, Medtronic, Merck, Portola, and Sanofi and has been on the speaker bureau for Bayer, BMS/Pfizer, Boehringer Ingelheim, Daiichi-Sankyo, and Medtronic. Dr Chiang has been on the speaker bureau for Bayer, Boehringer Ingelheim, and Daiichi-Sankyo. Dr Lin reports no conflicts.
Supplementary Material
Footnotes
The online-only Data Supplement is available with this article at http://stroke.ahajournals.org/lookup/suppl/doi:10.1161/STROKEAHA.115.009947/-/DC1.
References
- 1.Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–867. doi: 10.7326/0003-4819-146-12-200706190-00007. [DOI] [PubMed] [Google Scholar]
- 2.Shen AY, Yao JF, Brar SS, Jorgensen MB, Chen W. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol. 2007;50:309–315. doi: 10.1016/j.jacc.2007.01.098. doi: 10.1016/j.jacc.2007.01.098. [DOI] [PubMed] [Google Scholar]
- 3.Gamra H, Murin J, Chiang CE, Naditch-Brûlé L, Brette S, Steg PG RealiseAF investigators. Use of antithrombotics in atrial fibrillation in Africa, Europe, Asia and South America: insights from the International RealiseAF Survey. Arch Cardiovasc Dis. 2014;107:77–87. doi: 10.1016/j.acvd.2014.01.001. doi: 10.1016/j.acvd.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 4.Chiang CE, Wang KL, Lip GY. Stroke prevention in atrial fibrillation: an Asian perspective. Thromb Haemost. 2014;111:789–797. doi: 10.1160/TH13-11-0948. doi: 10.1160/TH13-11-0948. [DOI] [PubMed] [Google Scholar]
- 5.Oldgren J, Healey JS, Ezekowitz M, Commerford P, Avezum A, Pais P, et al. RE-LY Atrial Fibrillation Registry Investigators. Variations in cause and management of atrial fibrillation in a prospective registry of 15,400 emergency department patients in 46 countries: the RE-LY Atrial Fibrillation Registry. Circulation. 2014;129:1568–1576. doi: 10.1161/CIRCULATIONAHA.113.005451. doi: 10.1161/CIRCULATIONAHA.113.005451. [DOI] [PubMed] [Google Scholar]
- 6.Yasaka M, Lip GY. Impact of non-vitamin k antagonist oral anticoagulants on intracranial bleeding in Asian patients with non-valvular atrial fibrillation. Circ J. 2014;78:2367–2372. doi: 10.1253/circj.cj-14-0720. [DOI] [PubMed] [Google Scholar]
- 7.Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi: 10.1056/NEJMoa0905561. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 8.Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. doi: 10.1056/NEJMoa1009638. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 9.Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–992. doi: 10.1056/NEJMoa1107039. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 10.Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. ENGAGE AF-TIMI 48 Investigators. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–2104. doi: 10.1056/NEJMoa1310907. doi: 10.1056/NEJMoa1310907. [DOI] [PubMed] [Google Scholar]
- 11.van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9:167–176. doi: 10.1016/S1474-4422(09)70340-0. doi: 10.1016/S1474-4422(09)70340-0. [DOI] [PubMed] [Google Scholar]
- 12.Delgado-Fernández M. The J-ROCKET AF study: a matter of ethnicity or a matter of weight? Circ J. 2013;77:2636. doi: 10.1253/circj.cj-13-0726. [DOI] [PubMed] [Google Scholar]
- 13.Lip GY, Wang KL, Chiang CE. Non-vitamin K antagonist oral anticoagulants (NOACs) for stroke prevention in Asian patients with atrial fibrillation: time for a reappraisal. Int J Cardiol. 2015;180:246–254. doi: 10.1016/j.ijcard.2014.11.182. doi: 10.1016/j.ijcard.2014.11.182. [DOI] [PubMed] [Google Scholar]
- 14.Chiang CE, Zhang S, Tse HF, Teo WS, Omar R, Sriratanasathavorn C. Atrial fibrillation management in Asia: from the Asian expert forum on atrial fibrillation. Int J Cardiol. 2013;164:21–32. doi: 10.1016/j.ijcard.2011.12.033. doi: 10.1016/j.ijcard.2011.12.033. [DOI] [PubMed] [Google Scholar]
- 15.Tse HF, Wang YJ, Ahmed Ai-Abdullah M, Pizarro-Borromeo AB, Chiang CE, Krittayaphong R, et al. Stroke prevention in atrial fibrillation–an Asian stroke perspective. Heart Rhythm. 2013;10:1082–1088. doi: 10.1016/j.hrthm.2013.03.017. doi: 10.1016/j.hrthm.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 16.Hankey GJ, Stevens SR, Piccini JP, Lokhnygina Y, Mahaffey KW, Halperin JL, et al. ROCKET AF Steering Committee and Investigators. Intracranial hemorrhage among patients with atrial fibrillation anticoagulated with warfarin or rivaroxaban: the rivaroxaban once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation. Stroke. 2014;45:1304–1312. doi: 10.1161/STROKEAHA.113.004506. doi: 10.1161/STROKEAHA.113.004506. [DOI] [PubMed] [Google Scholar]
- 17.Hart RG, Diener HC, Yang S, Connolly SJ, Wallentin L, Reilly PA, et al. Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke. 2012;43:1511–1517. doi: 10.1161/STROKEAHA.112.650614. doi: 10.1161/STROKEAHA.112.650614. [DOI] [PubMed] [Google Scholar]
- 18.Giugliano RP, Ruff CT, Rost NS, Silverman S, Wiviott SD, Lowe C, et al. ENGAGE AF-TIMI 48 Investigators. Cerebrovascular events in 21 105 patients with atrial fibrillation randomized to edoxaban versus warfarin: Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48. Stroke. 2014;45:2372–2378. doi: 10.1161/STROKEAHA.114.006025. doi: 10.1161/STROKEAHA.114.006025. [DOI] [PubMed] [Google Scholar]
- 19.Yoon CH, Park YK, Kim SJ, Lee MJ, Ryoo S, Kim GM, et al. Eligibility and preference of new oral anticoagulants in patients with atrial fibrillation: comparison between patients with versus without stroke. Stroke. 2014;45:2983–2988. doi: 10.1161/STROKEAHA.114.005599. doi: 10.1161/STROKEAHA.114.005599. [DOI] [PubMed] [Google Scholar]
- 20.Hori M, Connolly SJ, Zhu J, Liu LS, Lau CP, Pais P, et al. RE-LY Investigators. Dabigatran versus warfarin: effects on ischemic and hemorrhagic strokes and bleeding in Asians and non-Asians with atrial fibrillation. Stroke. 2013;44:1891–1896. doi: 10.1161/STROKEAHA.113.000990. doi: 10.1161/STROKEAHA.113.000990. [DOI] [PubMed] [Google Scholar]
- 21.Wong KS, Hu DY, Oomman A, Tan RS, Patel MR, Singer DE, et al. Executive Steering Committee and the ROCKET AF Study Investigators. Rivaroxaban for stroke prevention in East Asian patients from the ROCKET AF trial. Stroke. 2014;45:1739–1747. doi: 10.1161/STROKEAHA.113.002968. doi: 10.1161/STROKEAHA.113.002968. [DOI] [PubMed] [Google Scholar]
- 22.Goto S, Zhu J, Liu L, Oh BH, Wojdyla DM, Aylward P, et al. ARISTOTLE Investigators. Efficacy and safety of apixaban compared with warfarin for stroke prevention in patients with atrial fibrillation from East Asia: a subanalysis of the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) Trial. Am Heart J. 2014;168:303–309. doi: 10.1016/j.ahj.2014.06.005. doi: 10.1016/j.ahj.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 23.Koretsune Y, Yamashita T, Yang Y, Chen SA, Chung N, Giugliano RP, et al. Edoxaban versus warfarin in east-asian (including Japanese) patients with atrial fibrillation―an engage AF-TIMI 48 sub-analysis. Circ J. 2014;78:I–484. [Google Scholar]
- 24.Lip GY, Larsen TB, Skjøth F, Rasmussen LH. Indirect comparisons of new oral anticoagulant drugs for efficacy and safety when used for stroke prevention in atrial fibrillation. J Am Coll Cardiol. 2012;60:738–746. doi: 10.1016/j.jacc.2012.03.019. doi: 10.1016/j.jacc.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 25.Miller CS, Grandi SM, Shimony A, Filion KB, Eisenberg MJ. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol. 2012;110:453–460. doi: 10.1016/j.amjcard.2012.03.049. doi: 10.1016/j.amjcard.2012.03.049. [DOI] [PubMed] [Google Scholar]
- 26.Capodanno D, Capranzano P, Giacchi G, Calvi V, Tamburino C. Novel oral anticoagulants versus warfarin in non-valvular atrial fibrillation: a meta-analysis of 50,578 patients. Int J Cardiol. 2013;167:1237–1241. doi: 10.1016/j.ijcard.2012.03.148. doi: 10.1016/j.ijcard.2012.03.148. [DOI] [PubMed] [Google Scholar]
- 27.Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383:955–962. doi: 10.1016/S0140-6736(13)62343-0. doi: 10.1016/S0140-6736(13)62343-0. [DOI] [PubMed] [Google Scholar]
- 28.Desai J, Kolb JM, Weitz JI, Aisenberg J. Gastrointestinal bleeding with the new oral anticoagulants–defining the issues and the management strategies. Thromb Haemost. 2013;110:205–212. doi: 10.1160/TH13-02-0150. doi: 10.1160/TH13-02-0150. [DOI] [PubMed] [Google Scholar]
- 29.Hylek EM, Held C, Alexander JH, Lopes RD, De Caterina R, Wojdyla DM, et al. Major bleeding in patients with atrial fibrillation receiving apixaban or warfarin: The ARISTOTLE Trial (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation): predictors, characteristics, and clinical outcomes. J Am Coll Cardiol. 2014;63:2141–2147. doi: 10.1016/j.jacc.2014.02.549. doi: 10.1016/j.jacc.2014.02.549. [DOI] [PubMed] [Google Scholar]
- 30.Dans AL, Connolly SJ, Wallentin L, Yang S, Nakamya J, Brueckmann M, et al. Concomitant use of antiplatelet therapy with dabigatran or warfarin in the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial. Circulation. 2013;127:634–640. doi: 10.1161/CIRCULATIONAHA.112.115386. doi: 10.1161/CIRCULATIONAHA.112.115386. [DOI] [PubMed] [Google Scholar]
- 31.Alexander JH, Lopes RD, Thomas L, Alings M, Atar D, Aylward P, et al. Apixaban vs. warfarin with concomitant aspirin in patients with atrial fibrillation: insights from the ARISTOTLE trial. Eur Heart J. 2014;35:224–232. doi: 10.1093/eurheartj/eht445. doi: 10.1093/eurheartj/eht445. [DOI] [PubMed] [Google Scholar]
- 32.Mega JL, Walker JR, Ruff CT, Vandell AG, Nordio F, Deenadayalu N, et al. Genetics and the clinical response to warfarin and edoxaban: findings from the randomised, double-blind ENGAGE AF-TIMI 48 trial. Lancet. 2015;385:2280–2287. doi: 10.1016/S0140-6736(14)61994-2. doi: 10.1016/S0140-6736(14)61994-2. [DOI] [PubMed] [Google Scholar]
- 33.Takahashi H, Wilkinson GR, Nutescu EA, Morita T, Ritchie MD, Scordo MG, et al. Different contributions of polymorphisms in VKORC1 and CYP2C9 to intra- and inter-population differences in maintenance dose of warfarin in Japanese, Caucasians and African-Americans. Pharmacogenet Genomics. 2006;16:101–110. doi: 10.1097/01.fpc.0000184955.08453.a8. [DOI] [PubMed] [Google Scholar]
- 34.Gaikwad T, Ghosh K, Shetty S. VKORC1 and CYP2C9 genotype distribution in Asian countries. Thromb Res. 2014;134:537–544. doi: 10.1016/j.thromres.2014.05.028. doi: 10.1016/j.thromres.2014.05.028. [DOI] [PubMed] [Google Scholar]


