Abstract
Background
This study aims to examine the longitudinal effects of a small-scale nursing home model on the change rates of psychological outcomes by comparing Green House (GH) and traditional nursing home residents.
Methods
A total of 242 residents (93 GH and 149 traditional home residents) who resided at the home least 6 months from admission. Four minimum dataset assessments every six months from admission were included. The main psychological outcomes were depressive mood, and social engagement. The main independent variable was the facility type that the resident resided in: a GH or traditional unit. Age, gender, ADL function, and cognitive function at admission were controlled in the model. A zero-inflated Poisson growth curve model was utilized to compare change rates of two psychological outcomes between the two groups taking into account many zero counts of two outcome measures.
Results
A rate of increase in depressive symptoms for GH home residents was higher than that of traditional home residents (β = 0.135, p-value = 0.025). GH home residents had a lower rate of increase of the probability of “not being socially engaged” over time compared to traditional home residents (β = −0.274, p-value = 0.010).
Conclusion
The GH nursing home model had a longitudinal effect on increasing the probability of residents’ social engagement over time, but also increasing the recognition of depressive symptoms compared to traditional nursing homes.
Keywords: person-centered care, culture change, Green House nursing home, depression, social engagement, behaviors, nursing home
INTRODUCTION
With increasing concern over quality of life for older adults in nursing homes, many traditional nursing homes have attempted to transform themselves from a model driven by clinical concerns and hospital-like environments toward emphasizing more person-centered care within homelike environments. Representative of these transformations are the various small-scale nursing home models that have been introduced in many countries using diverse labels: Green House (GH) nursing homes in the U.S., group living care in Sweden and the Netherlands, and group homes in Japan and South Korea (Seok, 2010; Verbeek et al., 2009). Although there are some cross-national variations, small-scale nursing homes have several common characteristics: (1) architecture that reflects a family home (a private room, living room and dining room), (2) care delivery that incorporates significant values of person-centered care to be more homelike (autonomy, choice and self-care), and (3) individual and socio-cultural continuity (Rabig, 2009). These small-scale nursing home models have an implicit assumption that homelike environments will improve well-being and quality of life for older adults (Molony et al., 2011).
The GH nursing home model was developed by several pioneer providers in the United States in the early 1990s emphasizing a homelike environment and organizational changes to enhance quality of life for nursing home residents (Rabig et al., 2006). GH homes are skilled nursing facilities working within the current regulations and reimbursement system by the Center for Medicare and Medicaid Services. Some of the characteristics of GH homes in the United States are that they are not dementia-specific settings, whereas small-scale nursing homes in European countries are dementia-specific, long-term care facilities. A GH model for nursing home is also not restricted to ownership type (i.e., for-profit or not-for-profit).
The GH model is an innovative program in its approach to radically redesign nursing home buildings and environments. Most GH homes are in clusters of two or three, situated on a campus with a larger, traditional nursing home (Bowers and Nolet, 2014). Extensive training and consultations are provided for new GH homes such as general principles, architecture, and roles of staff by the National Green House organization since the GH model is standardized (Bowers and Nolet, 2014). Usually 10 residents reside in each home. Each resident has a private bedroom and bathroom and shared common spaces including a large living room and dining room where residents can gather like a family. GH homes encourage and support residents’ choices and autonomy and residents are provided with individualized care (Eliopoulos, 2010). To be more homelike, hospital-like components of traditional nursing homes are avoided in GH homes including no nurse stations, medication carts, or paging systems. A special feature of the GH model is certified nurse aides (CNAs), called Shahbazim, who are highly empowered and self-managed given greater autonomy in daily activities along with greater responsibilities. Unlike traditional CNAs, they integrate diverse roles including meals, shopping, housekeeping, activities, and direct care (Eliopoulos, 2010; Ragsdale and McDougall, 2008).
Despite widespread adoption of small-scale nursing home models in many countries, little research evidence is currently available concerning the effects of these models. Furthermore, previous studies have suffered from methodological limitations: the use of cross-sectional design (Lindessay et al., 1991; Smit et al., 2012), short follow-up time with a quasi-experimental design (Molony et al., 2011), small sample sizes (Annerstedt, 1993; Dean et al., 1993; Molony et al., 2011), or lack of comparison groups (Dean et al., 1993; Smit et al., 2012). Recently, quasi-experimental studies have examined the effects of small-scale nursing homes: two studies in Europe (de Rooij et al., 2012; Verbeek et al., 2010, 2014), and one in the United States (Kane et al., 2007). However, research findings are mixed. GH home residents reported better quality of life than traditional home residents in the US (Kane et al., 2007), but no significant effects were found for quality of life, depression, neuropsychiatric symptoms, and agitation for residents with dementia in the Netherlands and Belgium (de Rooij et al., 2012; Verbeek et al., 2010).
The direction of nursing home care has changed towards small-scale homelike environments to meet the needs of older adults and family members, but policy makers and nursing homes face the high cost of facility conversions and ongoing questions about economies of scale. Scientific research studies on the effects of small-scale nursing homes are necessary to support evidence-based decision making. The current study examines the longitudinal effects of the GH nursing home model. Specifically, we compared the change rates in reports of two psychological outcomes (depressive symptoms, and social engagement) over time between residents in GH homes and those in a matched set of traditional nursing homes, taking into account many zero counts of outcome measures using a zero-inflated Poisson (ZIP) model.
METHODS
Study Sample
This study was a secondary analysis using minimum data set (MDS) 2.0 data from a parent study: the Study of Changes in ADL Assistant Levels in Traditional Nursing Homes and The Green House Project sties (International Severity Information Systems/Institute for Clinical Outcomes Research and Health Management Strategies, 2010). MDS data were retrospectively collected from nine GH homes and four traditional homes that had agreed to participate in the parent study. A total of 242 residents’ MDS data (93 GH home residents from nine GH homes and 149 traditional home residents from four traditional homes who had resided in the homes for at least six months) were included in the study. Exclusion criteria were residents who had been admitted for short-term rehab or hospice at the start of their stay. MDS data were retrospectively collected from admission to 18 months, which ranged from 2005 to 2009. Four MDS assessments every six months from admission (i.e., admission, 6 months, 12 months, and 18 months) were included in this study to conduct longitudinal analysis. The number of residents by group at each time point is shown in Table 1. This study was approved as exempt by the Health Science IRB of the University of Wisconsin-Madison.
Table 1.
Number of residents at each time point
| Admission | 6 months | 12 months | 18 months | |
|---|---|---|---|---|
| GH homes | 93 (100%) | 93 (100%) | 64 (69%) | 37 (40%) |
| Traditional homes | 149 (100%) | 149 (100%) | 117 (79%) | 55 (37%) |
| Total | 242 (100%) | 242 (100%) | 181 (75%) | 92 (38%) |
Note. Numbers in parenthesis indicate the residents who resided at the home at each time point.
Measures
Outcome variables
Depressive symptoms were measured using the Mood Scale Score (MSS). The MSS is a depression measure used in the MDS, which assesses the presence of eight depressive conditions using ten MDS items. The MSS ranges from 0 to 8 with higher values indicating a more depressed mood. Level of social engagement was measured using the Index of Social Engagement (ISE). The ISE is intended to capture each resident’s sense of initiative and involvement in social activities. The ISE score is computed by adding six dichotomous items in the MDS. The ISE scores range from 0 to 6 with higher values representing greater social engagement. The ISE has been shown to have good internal consistency and inter-rater reliability (Mor et al., 1995).
Independent variable
The main independent variable was the facility type, GH or traditional home.
Covariates
Age, gender, ADL and cognitive functions at baseline (i.e., admission) were controlled in the model. ADL function was measured using the ADL long-form scale, which is the sum of seven items ranging from 0 (complete independence) to 28 (total dependence). It is considered to be a good measure for detecting meaningful changes in ADL function over time (Morris et al., 1999). Cognitive function was measured using the cognitive performance scale (CPS) ranging from 0 (intact) to 6 (very severe impairment). The CPS has been used widely in nursing home studies and has good psychometric properties (Morris et al., 1994).
Analysis
To examine the longitudinal impact of the GH model on reports of two psychological outcomes, a latent growth curve zero-inflated Poisson (ZIP) model was applied. The growth curve model is a longitudinal analytic method estimating the latent variables: the average level of baseline scores (intercept) and the linear rate of change over time (slope). The growth curve model is a person-centered approach measuring not only the average rate of change but also providing an estimation of variation (Muthén and Muthén, 2000). Latent variables (intercept and slope) can be regressed on covariates to determine the relationship of a particular variable with each latent variable. This study examined the impact of the GH model on the change rates (slope) of two psychological outcomes as reported by nurses at four time points. The ZIP distribution is a mixture of a Poisson distribution of count data with an excess of zero counts. The ZIP model is increasingly used in health service research today to prevent biased estimation of parameters due to extra zeros in the count data (Lee et al., 2006). Vuong’s tests were performed for each outcome measure, which demonstrated that a ZIP model is superior to a regular count model for two outcome models. In this study, within the growth curve model framework, a ZIP model was employed to simultaneously estimate a binary model (e.g., probability of not reporting depressive symptoms [reference: reporting depressive symptoms]) and count model (e.g., number [level] of depressive symptoms among those who reported depressive symptoms) of the psychological outcome trajectories. We built two separate ZIP growth curve models (depressive symptoms, and social engagement) using four time points of data (admission, 6 months, 12 months, and 18 months.) Given that the design effect of depressive symptoms by a GH home unit was 3.08 (Muthén and Satorra, 1995), a multilevel analysis (random intercept model) was applied in all analyses to take into account the nested data structure within nursing homes. Descriptive analyses were conducted using SAS 9.4, and Mplus 7 was used for growth curve ZIP models.
RESULTS
Table 1 shows the number of residents at each time point by group. There were dropouts over time, about 25% at 12 months from admission and 62% at 18 months from admission. Table 2 provides the demographic characteristics of the study sample at admission by group. The average age of the residents was more than 85 years old, and the proportion of females was 73% in both settings. About half of the residents were diagnosed with dementia at admission. ADL, cognitive functions, depressive symptoms, and social engagement were not different between the two groups at admission.
Table 2.
Demographic characteristics of the study sample at admission (N=242)
| Variable | GH (n=93) M (SD)/n (%) |
Trad (n=149) M (SD)/n (%) |
Group difference (t/X2 value) | p-value |
|---|---|---|---|---|
| Age | 87.2 (7.2) | 85.8 (9.7) | −1.27 | 0.206 |
| Female | 68 (73.1%) | 110 (73.9%) | 0.02 | 0.903 |
| ADL function (ADLLF, 0 – 28) | 14.5 (6.7) | 14.5 (7.4) | 0.01 | 0.989 |
| Cognitive function (CPS, 0 – 6) | 2.5 (1.0) | 2.2 (1.2) | −1.51 | 0.132 |
| Depressive symptoms (MMS, 0 – 8) | 1.2 (1.9) | 0.8 (1.5) | −1.63 | 0.104 |
| Social engagement(ISE, 0 – 6) | 1.0 (1.5) | 0.8 (1.5) | −1.33 | 0.184 |
Note. GH = Green House home residents; Trad = Traditional home residents; M = mean; SD = standard deviation; ADLLF = activities of daily living long form; CPS = cognitive performance scale; MSS = mood scale score; ISE = index of social engagement; Higher scores of ADL, CPS, and MSS indicate worse status, but higher scores of ISE indicate better engagement status.
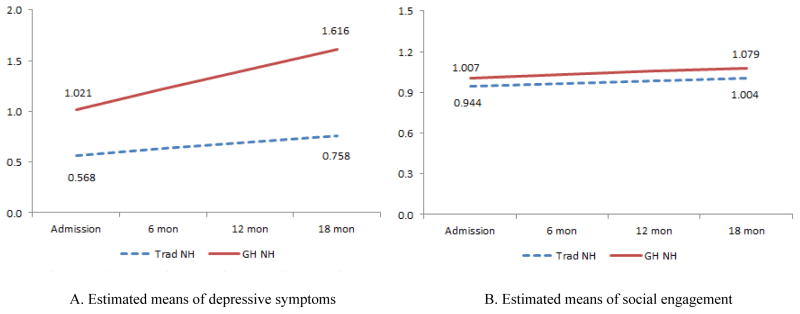
Before analyzing the longitudinal data, we examined the impact of dropouts and missingness using a pattern-mixture model (Hedeker and Gibbons, 1997), which demonstrated that it was possible to ignore missing patterns including whether residents in this study 1) dropped out before 18 months and 2) had missing values during the stay. As major study findings, Table 3 indicates that a rate of increase in depressive symptoms for GH home residents was higher than that of traditional home residents (β = 0.135, p-value = 0.025), but there was no significant difference in the change rates of the probability of “zero depressive symptoms” over time between the two groups (β = −1.020, p-value = 0.066). Given the small p-value and odds ratio (OR = 0.361), this non-significant result might be due to the insufficient power of these data. Regarding social engagement, GH home residents had less increase in the probability of “not being socially engaged” over time (β = −0.274, p-value = 0.010); however, it was not associated with the rate of increase of the social engagement level in the Poisson part (β = −0.010, p-value = 0.913). In the Poisson part, a small incidence rate ratio (IRR = 0.990) in addition to the non-significant p-value (0.913) might indicate no actual clinical difference between the two groups. To help visualize the data, Figure 1 displays the growth trajectories of the Poisson parts for depressive symptoms and social engagement for residents after the four covariates (age, gender, ADL, and cognitive function) were controlled with their means. Figure 1A shows a group difference in depressive symptoms of 0.453 units at admission (GH = 1.021, Traditional = 0.568) and 0.858 units at 18 months (GH = 1.616, Traditional = 0.758) indicating a significant difference in the rate of change. However, Figure 1B demonstrates a trivial group difference in social engagement of 0.063 (GH = 1.007, Traditional = 0.944) and 0.075 units (GH = 1.079, Traditional = 1.004) at 18 months.
Table 3.
Results of multilevel ZIP regression to examine the impact of the GH model on the change rate of psychological outcomes (N=241)
| Variable | Depressive symptoms | Social engagement | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Zero inflated part(zero vs. non-zero) | Poisson part(level of symptoms) | Zero inflated part(zero vs. non-zero) | Poisson part(level of engagement) | |||||
| Estimate (SE) | p | Estimate (SE) | p | Estimate (SE) | p | Estimate (SE) | p | |
| Age | −0.018 (0.017) | 0.270 | 0.005 (0.003) | 0.061 | −0.009 (0.005) | 0.079 | −0.001 (0.002) | 0.607 |
| Female# | −0.045 (0.553) | 0.935 | 0.008 (0.072) | 0.916 | −0.034 (0.177) | 0.847 | 0.142 (0.047) | 0.002 |
| ADL function | −0.015 (0.026) | 0.568 | 0.000 (0.005) | 0.954 | 0.004 (0.012) | 0.767 | −0.004 (0.003) | 0.250 |
| Cognitive function | 0.187 (0.217) | 0.389 | −0.042 (0.038) | 0.369 | 0.015 (0.076) | 0.842 | 0.002 (0.016) | 0.898 |
| Green House# | −1.020 (0.554) | 0.066 | 0.135 (0.060) | 0.025 | −0.274 (0.106) | 0.010 | −0.010 (0.093) | 0.913 |
|
OR (95% CI) 0.361 (0.122, 1.069) |
IRR (95% CI) 1.145 (1.017, 1.288) |
OR (95% CI) 0.760 (0.618, 0.936) |
IRR (95% CI) 0.990 (0.824, 1.189) |
|||||
Note.
Reference group: male and traditional nursing home residents, respectively; Higher scores of depressive symptoms indicate worse status, but higher scores of social engagement indicate better engagement status; SE = standard error; p = p-value; OR = odds ratio; CI = confidence interval; IRR = incidence rate ratio; The zero-inflated part provides information that variable “A” is associated with a higher (or lower) rate of increase in the probability of “zero” to “non-zero,” and the Poisson part provides information that variable “A” is related to a higher (or lower) rate of increase in the “level of symptoms.”
Figure 1.
Mean trajectories of Poisson parts of depressive symptoms and social engagement
Note. Trad NH = traditional nursing home residents; GH NH = Green House nursing home residents; All these trajectories are the estimated mean trajectories in the Poisson part with the means of four covariates (age, gender, ADL function, and cognitive function).
DISCUSSION
This study examined the longitudinal effects of the GH nursing home model on psychological outcomes. Residents in GH homes had a higher rate of increase of depressive symptoms over time, but they had a lower increase in the probability of not being socially engaged compared to traditional home residents.
The finding that GH nursing home residents reported a greater increase in the rate of depressive symptoms over time seems at odds with Kane’s previous quasi-experimental study that reported better quality of life in GH residents (Kane et al., 2007). However, this longitudinal study’s finding of increasing reports of depressive symptoms over time may provide important practical considerations. An accurate assessment or early recognition of residents’ change, particularly in the subjective and psychological aspects (pain, mood), is highly dependent upon the subjects’ and assessors’ characteristics (Mor et al., 2003), and familiarity between assessors and subjects (Power, 2014). GH homes usually consist of 10 residents and a few staff who spend more time together and across a range of activities than is the case in traditional homes. Staff assignments are consistent, and close relationships between staff and residents in small-scale homes enable staff to more easily recognize and monitor changes in residents’ moods. Thus, staff are more likely to report these changes in the MDS and provide timely treatment. Residents may be more comfortable expressing their feelings or emotions to close staff within these home-like care environments. This unique atmosphere of closeness in small-scale nursing homes might lead to a significant increase in the recognition and reporting of residents’ depressive symptoms over time compared to traditional nursing home residents.
It is, however, possible that GH residents experience increasing depressive symptoms over time, for other reasons. One study reported a concern that the GH model provides fewer organized formal group activities and could lead to lower resident stimulation (Zimmerman and Cohen, 2010), and that the consequences of emphasizing privacy and individual preferences may prevent residents from developing meaningful social relationships. However, the current study revealed less increase in the probability of not being socially engaged in GH homes. This partially positive effect of the GH model on social engagement is consistent with recent Dutch and Belgium studies indicating that small-scale nursing home residents reported higher levels of engagement (de Rooij et al., 2012; Verbeek et al., 2010, 2014). Considering that more intensive contact between residents and staff as well as environmental stimuli (especially related to real-world tasks and activities that residents were used to doing) can significantly influence residents’ social engagement (Cohen-Mansfield et al., 2010; de Rooij et al., 2012), encouraging residents to be involved in activities in the GH model seemed to be effective in improving the probability of social engagement. Nevertheless, change rates in the level of social engagement were not significantly different between the two groups as determined by the Poisson part. This indicates that the GH model is effective in increasing the probability of residents being socially engaged, but it is possible that the frequency of activities is insufficient over time.
One of the limitations of this study was that the control group (traditional nursing homes) and GH homes were under the same organization. A GH organization usually has one traditional building and more than one GH home. The traditional building and GH homes are physically separate on the same campus, but the overall organizational vision and policies are likely to be shared by both types of homes under the same organization. This may be a source of contamination of the effects of the GH model compared to the control groups. Although the two psychological outcomes (depressive mood and social engagement) are inter-related (Cohen-Mansfield et al., 2012), we built two separate models in this study due to the insufficient sample size to build one integrated model. Lastly, this study used MDS data. The MDS has been widely used in research studies and practice, but concerns about data accuracy and potential errors have been raised (Mor et al., 2003).
There are several implications for future research that will enhance the findings of this study. First, to improve the quality of health outcome research in this area, more studies are needed to capture the accurate status of residents. Outcome measurements, especially for the psychological aspects are highly influenced by measurement errors. Particularly for residents who are not cognitively intact, it is more difficult to capture the psychological aspects sensitively. Thus, different measurement strategies regarding psychological aspects depending on the cognitive function of residents are needed for future studies. The new MDS 3.0 version includes new tools to measure residents’ mood (PHQ-9), which is a well-established and standardized instrument including interviews and observational versions (Saliba et al., 2012). Second, further studies to examine care processes are necessary. It is important to provide practical information concerning concrete strategies of care processes to nursing homes to improve residents’ health outcomes. Despite limited data sources, the MDS can be the first place to investigate the significant processes that have varying influences on resident health outcomes in GH nursing homes. However, currently all nursing home care provided to residents cannot be documented in the structured MDS data set, so a time-and-motion observation study is necessary to examine more comprehensive care processes in terms of types of care and quantity of care. In addition, different work environments including communication, teamwork, and leadership may influence nursing staff`s care-giving processes differently (Temkin-Greener et al., 2009), so qualitative studies to explore these aspects are needed.
CONCLUSION
This study examined the effects of the GH model on two psychological outcomes. Major findings were that GH residents had a higher rate of increase of depressive symptoms, and a lower rate of increase in the probability of not being socially engaged over time relative to those in traditional nursing homes. Despite somewhat mixed findings, the fundamental philosophy of the GH model is innovative and may be associated with an increase in nursing home residents’ quality of life. Given that the GH model is continuously evolving with updated and revised educational and support programs (Bowers and Nolet, 2014), further studies are necessary to examine the effects of the GH model and the mechanism to create differences between the two settings that influence residents’ psychological outcomes.
Acknowledgments
This research was partially supported by a grant from the Robert Wood Johnson Foundation (Grant 66360; PI: SDH) and the Clinical and Translational Science Award Program, through the NIH National Center for Advancing Translational Sciences (grant UL1TR000427; BJB). The funding agency had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of this manuscript. The content is solely the responsibility of the authors and does not necessarily represent the views of the sponsors.
Footnotes
Conflict of Interest
None.
Description of Authors’ Roles
Study concept and design: JY Yoon, RL Brown, BJ Bowers, SS Sharkey, and SD Horn. Acquisition of data: SS Sharkey and SD Horn. Analysis and interpretation of data: JY Yoon, RL Brown, BJ Bowers, and SD Horn. Drafting or revising manuscript for important intellectual content: JY Yoon, RL Brown, BJ Bowers, SS Sharkey, and SD Horn.
References
- Annerstedt L. Development and consequences of group living in Sweden. A new mode of care for the demented elderly. Social Science and Medicine. 1993;37:1529–1538. doi: 10.1016/0277-9536(93)90187-9. [DOI] [PubMed] [Google Scholar]
- Bowers BJ, Nolet K. Developing the green house nursing care team: variations on development and implementation. The Gerontologist. 2014;54:S53–64. doi: 10.1093/geront/gnt109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Dakheel-Ali M, Jensen B, Marx MS, Thein K. An analysis of the relationships among engagement, agitated behavior, and affect in nursing home residents with dementia. International Psychogeriatrics. 2012;24:742–52. doi: 10.1017/S1041610211002535. [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Marx MS, Thein K, Dakheel-Ali M. The impact of past and present preferences on stimulus engagement in nursing home residents with dementia. Aging and Mental Health. 2010;14:67–73. doi: 10.1080/13607860902845574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean R, Proundfoot R, Lindesay J. The quality of interactions schedule (quis): development, reliability and use in the evaluation of two domus units. International Journal of Geriatric Psychiatry. 1993;8:819–826. [Google Scholar]
- De Rooij AHPM, Luijkx KG, Schaafsma J, Declercq AG, Emmerink PMJ, Schols JMGA. Quality of life of residents with dementia in traditional versus small-scale long-term care settings: A quasi-experimental study. International Journal of Nursing Studies. 2012;49:931–940. doi: 10.1016/j.ijnurstu.2012.02.007. [DOI] [PubMed] [Google Scholar]
- Eliopoulos C. Guest Editorial: Cultural transformation in nursing homes. International Journal of Older People Nursing. 2010;5:1–2. doi: 10.1111/j.1748-3743.2009.00202.x. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods. 1997;2:64–78. [Google Scholar]
- Kane RA, Lum TY, Cutler LJ, Degenholtz HB, Yu TC. Resident outcomes in small-house nursing homes: a longitudinal evaluation of the initial Green House program. Journal of the American Geriatrics Society. 2007;55:832–839. doi: 10.1111/j.1532-5415.2007.01169.x. [DOI] [PubMed] [Google Scholar]
- Lee AH, Wang K, Scott JA, Yau KKW, McLachlan GJ. Multi-level zero-inflated poisson regression modelling of correlated count data with excess zeros. Statistical methods in medical research. 2006;15:47–61. doi: 10.1191/0962280206sm429oa. [DOI] [PubMed] [Google Scholar]
- Lindessay J, Briggs K, Lawes M, MacDonald A, Herzberg J. The domus philosophy: a comparative evaluation of a new approach to residential care for the demented elderly. International Journal of Geriatric Psychiatry. 1991;6:727–736. [Google Scholar]
- Molony SL, Evans LK, Jeon S, Rabig J, Straka LA. Trajectories of at-homeness and health in usual care and small house nursing homes. The Gerontologist. 2011;51:504–515. doi: 10.1093/geront/gnr022. [DOI] [PubMed] [Google Scholar]
- Mor V, Berg K, Angelelli J, Gifford D, Morris J, Moore T. The quality of quality measurement in U.S. nursing homes. The Gerontologist. 2003;43:37–46. doi: 10.1093/geront/43.suppl_2.37. [DOI] [PubMed] [Google Scholar]
- Mor V, Branco K, Fleishman J, Hawes C, Phillips C, Morris J, Fries B. The structure of social engagement among nursing home residents. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1995;50:P1–P8. doi: 10.1093/geronb/50b.1.p1. [DOI] [PubMed] [Google Scholar]
- Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V, Lipsitz LA. MDS Cognitive Performance Scale. Journal of Gerontology. 1994;49:M174–M182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 1999;54:M546–M553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcoholism, clinical and experimental research. 2000;24:882–891. [PubMed] [Google Scholar]
- Muthén B, Satorra A. Complex sample data in structural equation modeling. Sociological Methodology. 1995;25:267–316. [Google Scholar]
- Power GA. Optimal staffing to prevent nursing home hospitalizations. Medical Care. 2014;52:93. doi: 10.1097/MLR.0b013e3182a98371. [DOI] [PubMed] [Google Scholar]
- Rabig J. Home again: small houses for individuals with cognitive impairment. Journal of Gerontological Nursing. 2009;35:10–15. doi: 10.3928/00989134-20090706-04. [DOI] [PubMed] [Google Scholar]
- Rabig J, Thomas W, Kane RA, Cutler LJ, McAlilly S. Radical redesign of nursing homes: applying the green house concept in Tupelo, Mississippi. The Gerontologist. 2006;46:533–539. doi: 10.1093/geront/46.4.533. [DOI] [PubMed] [Google Scholar]
- Ragsdale V, McDougall GJ. The changing face of long-term care: looking at the past decade. Issues in Mental Health Nursing. 2008;29:992–1001. doi: 10.1080/01612840802274818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saliba D, Difilippo S, Edelen MO, Kroenke K, Buchanan J, Steim J. Testing the PHQ-9 Interview and Observational Versions (PHQ-9 OV) for MDS 3.0. Journal of the American Medical Directors Association. 2012;13:618–625. doi: 10.1016/j.jamda.2012.06.003. [DOI] [PubMed] [Google Scholar]
- Seok JE. Public long-term care insurance for the elderly in Korea: design, characteristics, and tasks. Social Work in Public Health. 2010;25:185–209. doi: 10.1080/19371910903547033. [DOI] [PubMed] [Google Scholar]
- Smit D, de Lange J, Willemse B, Pot AM. The relationship between small-scale care and activity involvement of residents with dementia. International Psychogeriatrics. 2012:1–11. doi: 10.1017/S1041610211002377. [DOI] [PubMed] [Google Scholar]
- Temkin-Greener H, Zheng N, Katz P, Zhao H, Mukamel DB. Measuring work environment and performance in nursing homes. Medical Care. 2009;47:482–491. doi: 10.1097/mlr.0b013e318190cfd3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbeek H, Zwakhalen SMG, van Rossum E, Ambergen T, Kempen GIJM, Hamers JPH. Dementia care redesigned: Effects of small-scale living facilities on residents, their family caregivers, and staff. Journal of the American Medical Directors Association. 2010;11:662–670. doi: 10.1016/j.jamda.2010.08.001. [DOI] [PubMed] [Google Scholar]
- Verbeek H, Zwakhalen SMG, van Rossum E, Ambergen T, Kempen GIJM, Hamers JPH. Effects of small-scale, home-like facilities in dementia care on residents’ behavior, and use of physical restraints and psychotropic drugs: a quasi-experimental study. International psychogeriatrics. 2014:1–12. doi: 10.1017/S1041610213002512. [DOI] [PubMed] [Google Scholar]
- Zimmerman S, Cohen LW. Evidence behind The Green House and similar models of nursing home care. Aging Health. 2010;6:717–737. [Google Scholar]