Abstract
Objectives
The goals of this study were to assess syndesmotic reductions utilizing computerized tomography (CT) scans, and to determine if malreductions were associated with certain injury types or reduction forceps.
Design
Prospective cohort
Setting
Urban Level 1 Trauma center
Patients
Twenty-seven patients with operatively treated syndesmotic injuries were recruited prospectively.
Intervention
Patients underwent postoperative bilateral CT scans of the ankle and hindfoot to assess syndesmotic reduction. The uninjured extremity was used as a control.
Main outcome measurement
Side-to-side differences of fibula position within the tibial incisura were measured at several anatomic points and analyzed based on injury type, the presence of posterior malleolar injury, level of fracture, and type of reduction forceps used.
Results
On average, operatively treated syndesmotic injuries were over-compressed (fibular medialization) by 1mm (p < .001) and externally rotated by 5° (p = .002) when compared to the uninjured extremity. The absence of a posterior malleolar injury and Weber B (OTA 44-B) fractures seemed to have a protective effect against malrotation, but not against over-compression. There was no difference in malreduction based on type of clamp used.
Conclusions
It is possible, and highly likely based on these data, to over-compress the syndesmosis when using a reduction forceps. Care should be taken to avoid over-compression, as this may affect ankle motion and functional outcome. This is the first in vivo series of syndesmotic over-compression to our knowledge.
Introduction
Ankle fractures are a relatively common injury, accounting for approximately 9% of all fractures(1). The distal tibiofibular syndesmosis is thought to be injured in 20% of all operatively treated ankle fractures(2), but syndesmotic injury has been reported to be as high as 45% in some series(3). Proper reduction of the syndesmosis using internal fixation is widely recommended to avoid early ankle arthrosis and poor subjective and functional outcomes(2, 4–14).
Intraoperative evaluation of the syndesmotic reduction is notoriously difficult. Using standard two-dimensional fluoroscopy, the tibiofibular clear space (TFCS) has been suggested as a measure of proper syndesmotic reduction(15, 16). However, the appearance of the TFCS has been shown to be heavily dependent on rotation of the limb(16, 17), and moreover, is increasingly thought to be a poor method to assess the syndesmotic reduction(9, 18–24). The contralateral “true talar dome lateral”, as suggested by Summers et al. has been popularized as a method to reduce sagittal plane malreductions(25).
There has been a movement towards using postoperative computerized tomography (CT) to evaluate the syndesmotic reduction(20, 21, 26). In one case series, the rate of malreduced syndesmoses was 52%(27). More recently, the reported rates of syndesmotic malreduction have been lower, and have ranged from 11–38% in recent series (28–30).
Of the possible malreduction planes of the syndesmosis, excessive medialization of the fibula within the tibial incisura (“over-compression”) has not been studied clinically, although cadaver data has variably reported whether this phenomenon is possible(31–33). An isolated case report demonstrated over-compression(34), but this has not been shown in a cohort of patients to our knowledge. Over-compression may compromise ankle motion and affect functional outcomes. Our hypothesis was that over-compression is common using standard reduction forceps and techniques in treating syndesmotic injuries. We also sought to determine any patient or injury factors that predispose to over-compression.
Patients and Methods
Patients and Injuries
At a single Level 1 trauma center, three orthopaedic traumatologists prospectively identified patients that underwent operative treatment of unilateral ankle fractures that had persistent intraoperative syndesmotic displacement or instability after fixation of the malleolar fractures. Patients with a history of any prior ankle fracture were excluded.
Twenty-seven patients were included in the analysis. The patients’ age range was 18–72, with only a single patient greater than 60 years of age. Fourteen of twenty-seven (51.9%) had injuries to the posterior malleolus, although only three of those fourteen (21%) posterior malleolar injuries were addressed directly with reduction and fixation. Eight of the injuries (30%) were Weber B (OTA 44-B) injuries. The remaining 19 patients were grouped together as “suprasyndesmotic lesions”. This group included 5 Maisonneuve-type injuries with a proximal tibiofibular injury that was not independently surgically addressed.
Intra-operative Assessment of Syndesmotic Instability
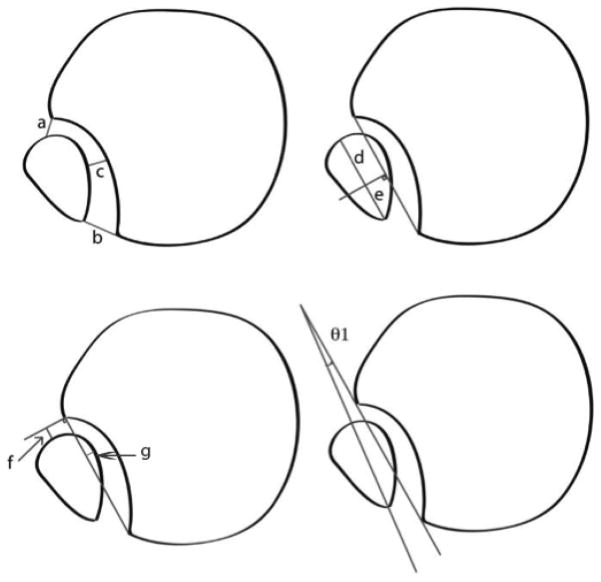
If fluoroscopic static images were within the normal range, injury to the syndesmosis was assessed using a lateral stress(35) (an adaptation of the Cotton test) which has been suggested to be the most sensitive intra-operative maneuver for detecting syndesmotic injury(36). The syndesmosis was indirectly reduced using either a pointed reduction clamp (Weber clamp) or a ball point pelvic reduction forceps, depending on surgeon preference, with the ankle in neutral dorsiflexion position. The clamp was placed approximately 1 cm proximal to the level of the mortise, just distal to the level of the fixation. Reduction force used was not quantified, but was based on subjective surgeon tactile feel and the tibio-fibular clear space reduction on the fluoroscopic mortise view. Syndesmotic fixation was achieved with one or two 3.5 mm trans-syndesmotic quadricortical position screws. Reduction was judged subjectively by comparing standard mortise and true lateral views of the injured and uninjured sides based on the method described by Summers et al.(25). Post-operatively, the patients underwent CT scans of bilateral ankles to assess operative reduction of the syndesmosis compared to the uninjured extremity, as suggested by Franke et al.(30). The position and rotation of the fibula relative to the tibial incisura for both the operative and uninjured extremities was determined using a combination of measurements described by Nault and Phisitkul (34, 40) (Figures 1,2; Table, Supplemental Digital Content 1).
Figure 1.
Illustration of an axial view of a normal syndesmosis proximal to the tibial plafond with measures a to g and angle 1. Adapted from Nault et al.(46) with permission.
Figure 2.
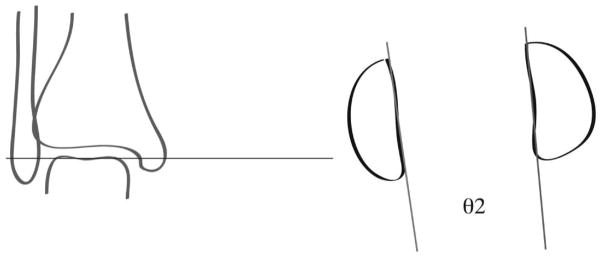
Illustration of an axial view of the 2 malleoli at the talar dome level representing angle 2. Adapted from Nault et al. (46) with permission
Statistical Analysis
Statistical analysis using Student’s t-test was performed using SPSS (IBM SPSS Statistics for Windows, Version 21.0, Armonk, NY) to compare side-to-side differences in the uninjured and operative ankles. The measurements included in the primary statistical analysis were made by a single author not involved in the treatment of the patients (SMC). A subset of 8 patients were measured by a second author (JAH). These measurements were repeated one month after the first set of measurements by both raters to allow for assessment of both inter- and intra-rater reliability.
Results
When comparing side-to-side measurements, our cohort was notable for significant over-compression (fibular medialization, Figures 3 and 4), as noted by measurements B, C and G (Table 1). Twelve of twenty seven patients (44%) had medialization of the fibula greater than 1 mm compared to the contralateral side. The mean side-to-side over-compression (measurement G) was 1.0 mm (95% CI: −1.5 to −0.5 mm, p < .001).
Figure 3.
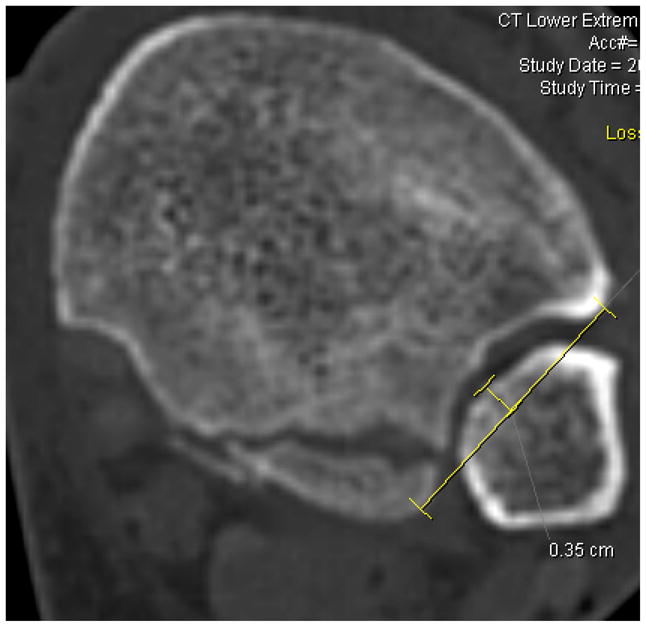
(Injured), measurement G, demonstrates over-compression of 1.5mm when compared to the uninjured side (Figure 4). Both measurements are taken 1cm proximal to the tibial plafond.
Figure 4.
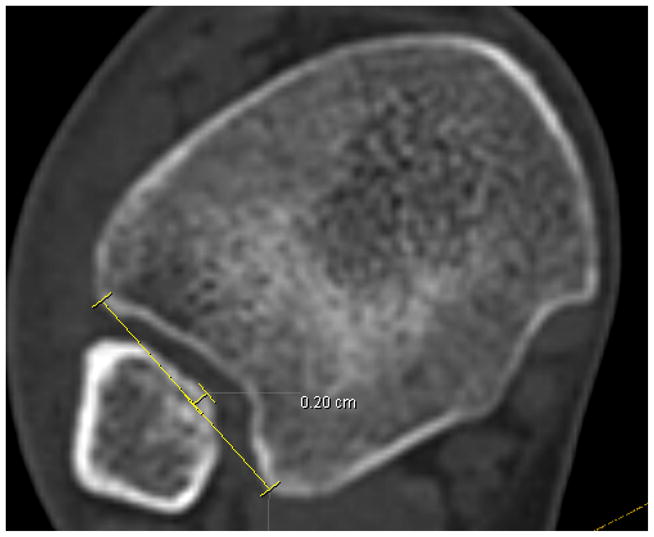
(Uninjured), measurement G.
Table 1.
All patients. Mean, SD, CI and significance calculated for each value, n=27
| Measurement (Injured-noninjured) | Mean | Std. Deviation | 95% Confidence Interval of the
|
Sig. (2-tailed) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
|
| |||||
| A (mm) | −0.01 | 0.2 | −0.6 | 0.6 | 1.0 |
| B* (mm) | −0.6 | 0.1 | −1.1 | −0.1 | 0.02* |
| C* (mm) | −0.7 | 0.1 | −1.2 | −0.3 | 0.0* |
| D (mm) | −0.8 | 0.3 | −2.0 | 0.4 | 0.2 |
| E (mm) | 0.4 | 0.2 | −0.5 | 1.3 | 0.4 |
| F (mm) | 0.1 | 0.2 | −0.5 | 0.7 | 0.6 |
| G* (mm) | −1.0 | 0.1 | −1.5 | −0.5 | 0.0* |
| Angle 1* (degrees) | 24.5 | 6.0 | 0.1 | 4.8 | 0.04* |
| Angle 2* (degrees) | 44.8 | 6.6 | 1.9 | 7.1 | 0.0* |
represents p<0.05
When analyzing the entire cohort, there were also a substantial number of malrotations of the syndesmosis. Angle 2 was statistically increased (externally rotated) (mean: 4.5°, 95% CI: 1.9 to 7.1, p = .002). This angle was increased by more than 5° compared to the uninjured side in 10/27 patients (37%). Figures, Supplemental Digital Content 2 and 3 demonstrate increased external rotation of the injured extremity as measured with Angle 2.
Posterior Malleolar Injury
When subdivided into groups with or without posterior malleolar injury, 6 of 13 (43%) patients without posterior malleolar injury were over-compressed by at least 1 mm compared to the uninjured extremity, which was statistically significant (mean: −1.0mm, 95% CI: −1.5 to −0.6, p<.001). There was no significant malrotation in patients with an intact posterior malleolus, and only 3/13 patients had external rotation >5°. (mean: 2.3°, 95% CI: −0.6° to 5.2°, p=.11) (Table, Supplemental Digital Content 4).
In the 14 patients with injuries to the posterior malleolus, 7 were over-compressed by at least 1mm compared to the uninjured extremity (mean: −1.0mm, 95% CI: −2.0 to −0.04, p=.042). Eight of 14 were externally rotated by more than 5° (mean 6.5°, 95% CI: 2.2° to 10.8°, p=.006) (Table, Supplemental Digital Content 5).
The subset of patients that had their posterior malleolar injuries addressed with independent fixation was small (3 patients). In this subset, 1/3 were over-compressed by >1mm and 1/3 was externally rotated by >5°. This group was too small for meaningful statistical analysis.
Fibular Fracture Level
Three of the eight patients with Weber B fractures (38%) had fibular medialization >1 mm. (mean: −1.1 mm, 95% CI: −2.5 to 0.3, p=.11). Three of the eight patients with Weber B injuries were externally rotated by more than 5 degrees (mean: 2.6°, 95% CI: −0.2 to 5.5, p=.06) (Table, Supplemental Digital Content 6). There was no overlap between the patients that were over-compressed and those that were malrotated in this group.
Patients with supra-syndesmotic injury patterns had both significant over-compression (10/19 patients) (mean: −0.9 mm, 95% CI: −1.6 to −.4, p=.003) and malrotation at the talar dome (8/19 patients)(mean: 5.0°, 95% CI: 1.0 to 9.0, p=.017) (Table, Supplemental Digital Content 7). The subset of patients (n=5) with Maisonneuve-type injuries was too small for meaningful independent statistical analysis.
Type of Forceps
The type of reduction forceps used had a statistically significant effect on over-compression. Of the patients reduced with Weber pointed reduction forceps, 2/6 (33%) had over-compression of at least 1mm (mean −0.6mm, 95% CI: −1.5 to 0.4, p=.18), compared to 10/21 (48%) of patients reduced with a pelvic ball-spike reduction clamp (mean −0.8mm, 95% CI −1.5 to −0.1, p=.025). There was no significant side-to-side malrotation at the level of the talar dome in patients reduced by pointed reduction forceps. The lack of statistical significance for over-compression and malrotation in the pointed reduction forceps group is likely due to small patient numbers in this group.(See Table, Supplemental Digital Content 8).
Measurement Reliability
Cronbach alpha values for intra-rater reliability were somewhat varied, depending on measurement and experience of the rater. The rater with more experience, having measured the entire cohort, had excellent or good reliability(37) for measurements F, G, and the non-injured side for Angle 2. The agreement was good (0.865) for Angle 2 on the injured side. For the rater that was less experienced in radiographic measurement of syndesmotic reduction, having measured 8 of the 27 patients, the intra-rater reliability was also generally good-to-excellent for measurements F, G, and Angle 2. Inter-rater reliability was also good-to-excellent for measures F, G, and Angle 2 (See Tables, Supplemental Digital Content 9 and 10 for intra- and inter-rater reliability measurements, respectively.)
Discussion
Based on an oft-cited cadaveric study, it had generally been accepted that over-compression of the tibiofibular syndesmosis was not possible(32). Phistikul et al. demonstrated in a cadaveric injury model that using reduction forceps, over-compression occurred on post-reduction CT scans, but the functional application of this finding has been limited (31). Additionally, Miller et al. have demonstrated that iatrogenic malreductions are influenced by the angle at which the clamp is placed(33). At our institution, we use post-operative CT scans to assess syndesmotic reduction, and our data has shown that it is possible to over-compress the syndesmosis in vivo, and was quite common in this series.
Regarding the surgical technique to obtain intra-operative reduction, further analysis is needed to determine if the type of clamp has a significant effect on over-compression. Our series suggests that pointed reduction forceps may be less likely to cause over-compression, although the sample size is small. Furthermore, our analysis suggests that fibular fractures at the level of the syndesmosis (Weber B) are less likely to be over-compressed and malreduced, but the significance of this finding was also limited by small sample size.
The presence of a posterior malleolar injury led to both over-compression and malrotation in the majority of cases, whereas the presence of an intact posterior malleolus seems have less predisposition for malrotation. Direct reduction of the posterior malleolus may not protect against over-compression and malrotation, although, again this subset in our study is small. A previous study has suggested that posterior malleolar fixation may help obtain a more anatomic syndesmotic reduction(38). Further work is needed to determine if the additional morbidity of a posterior approach is offset by improved syndesmotic reduction.
Radiographic evaluation of the syndesmosis has been notoriously difficult, and only recently have normal values been established for the population. There is a lack of literature that evaluates side-to-side anatomic differences in uninjured controls. An area for future study would be to establish normal side-to-side differences in uninjured controls. This would be a reasonable starting point to assess whether a syndesmotic reduction is considered anatomically “acceptable”.
In a gender-blind normative study, Mukhopadhyay et al. found that 12/19 patients (63%) had side-to-side differences in diastasis >2mm between patients’ uninjured syndesmoses using a measurement that was not utilized in our study(39). This study forces us to critically evaluate the previous literature. Gardner et al. judged syndesmoses to be malreduced with a greater than 2mm difference between the anterior and posterior tibiofibular distance(27), although this study included only unilateral CT scans postoperatively. Wikerøy et al. showed a non-significant trend toward worse functional outcomes with post-operative diastasis of 1.5mm(40). In a retrospective review, Sagi et al. found 40% of their cohort had a subjective malreduction based on bilateral postoperative CT scans. The criteria for judging acceptable reduction were not defined in the study. These patients tended toward worse functional scores(12). There is a need for future studies to compare objective measures of malreduction and functional scores to help determine which patients would benefit most from revision syndesmotic fixation. In order to reduce the incidence of malreduction, there has been increased use of intraoperative three-dimensional imaging during reduction of ankle fractures with syndesmotic injury, although malreduction rates remain relatively high even with use of this technology (29, 30, 41–43).
Regarding the inter- and intra-rater reliability of our measurements, we found that the measures, particularly for measures F, G, and Angle 2, were mostly excellent, while some were rated “good”. Our measurements were at least as reliable as previously suggested by Nault et al(44). As might be expected, there is a small, and likely non-significant increase in the intra-rater reliability in a rater with more experience, however our inter-rater analysis suggest that a novice rater would be acceptable when compared to a more experienced rater.
The slightly lower reliability for measures A, B, and C are likely because these measurements are inherently less precise when taken first, as these measurements require the rater to pinpoint the exact anterior and posterior points of the incisura, and in some individuals, the incisura borders are relatively curved. Measurement G might be more reliable to determine first, since to find this distance, one starts by laying a line of best fit over the most prominent “points” of the incisura. In the future, our group will likely make measurement G first, then proceed through the remainder of the measurements in hopes on increasing accuracy of measures A–C. The lack of reliability in Angle 1 is likely related to the difficulty in determining the sagittal plane axis of the fibula at a level one centimeter proximal to the plafond. The shape of the fibula at this level is widely varied, and in our hands, somewhat difficult and unreliable to determine.
We did not find a significant sagittal plane (anteroposterior) malreduction in our cohort. This may have been due to our technique of using a true talar dome lateral comparison view, which greatly minimizes the risk of sagittal plane malreduction(25). As described by Sagi et al.(12), based on the anatomic variation of incisura shapes (Type A: flat, Type B: concave), further analysis needs to be taken to assess if incisura shape predisposes to over-compression or sagittal plane malreductions. In addition, it may be beneficial to objectively define the anatomic categories rather than on based on subjective analysis.
We believe that the strength of this study is that we are able to demonstrate consistent over-compression at the syndesmosis using previously established measurements. We have confirmed that Nault et al.’s measurements are reliable and reproducible. The variety of injury types evaluated in this study is also a strength, and determined that over-compression is common and not limited only to certain injury patterns.
A notable weakness of this study is that the functional consequences of syndesmotic over-compression are currently unknown, and was not addressed with this study. Although the findings of over-compression on CT are statistically significant, we are in the process of following these patients’ long-term functional outcomes to determine if there are radiographic thresholds for “acceptable” reduction of the syndesmosis.
Conclusion
Statistically significant over-compression and malrotation of syndesmotic injuries occurred in this series. This is the first study to our knowledge to identify intra-operative over-compression compared to contralateral uninjured ankles. The functional consequences of these findings have not yet been elucidated and are a target for future study.
Supplementary Material
Footnotes
Presented in part at the Annual Meeting of the American Academy of Orthopaedic Surgeons, New Orleans, LA, 2014.
Ricci: Consultancy: Smith & Nephew, Biomet, Stryker, Wright Medical
Royalties: Smith & Nephew, Wright Medical, Lippincott
Research Support: Smith & Nephew
Gardner: Consultancy: DePuy Synthes, Stryker, DGIMed, BoneSupport AB, Pacira PHarma
Royalties: Lippincott
Research Support: DePuy Synthes
References
- 1.Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures--an increasing problem? Acta Orthop Scand. 1998;69:43–47. doi: 10.3109/17453679809002355. [DOI] [PubMed] [Google Scholar]
- 2.Pettrone FA, Gail M, Pee D, et al. Quantitative criteria for prediction of the results after displaced fracture of the ankle. J Bone Joint Surg Am. 1983;65:667–677. [PubMed] [Google Scholar]
- 3.Tornetta P, 3rd, Axelrad TW, Sibai TA, et al. Treatment of the Stress Positive Ligamentous SE4 Ankle Fracture: Incidence of Syndesmotic Injury and Clinical Decision Making. J Orthop Trauma. 26:659–661. doi: 10.1097/BOT.0b013e31825cf39c. [DOI] [PubMed] [Google Scholar]
- 4.Leeds HC, Ehrlich MG. Instability of the distal tibiofibular syndesmosis after bimalleolar and trimalleolar ankle fractures. J Bone Joint Surg Am. 1984;66:490–503. [PubMed] [Google Scholar]
- 5.Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am. 1976;58:356–357. [PubMed] [Google Scholar]
- 6.Burns WC, 2nd, Prakash K, Adelaar R, et al. Tibiotalar joint dynamics: indications for the syndesmotic screw--a cadaver study. Foot Ankle. 1993;14:153–158. doi: 10.1177/107110079301400308. [DOI] [PubMed] [Google Scholar]
- 7.Mont MA, Sedlin ED, Weiner LS, et al. Postoperative radiographs as predictors of clinical outcome in unstable ankle fractures. J Orthop Trauma. 1992;6:352–357. doi: 10.1097/00005131-199209000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Tunturi T, Kemppainen K, Patiala H, et al. Importance of anatomical reduction for subjective recovery after ankle fracture. Acta Orthop Scand. 1983;54:641–647. doi: 10.3109/17453678308992903. [DOI] [PubMed] [Google Scholar]
- 9.Jenkinson RJ, Sanders DW, Macleod MD, et al. Intraoperative diagnosis of syndesmosis injuries in external rotation ankle fractures. J Orthop Trauma. 2005;19:604–609. doi: 10.1097/01.bot.0000177114.13263.12. [DOI] [PubMed] [Google Scholar]
- 10.Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma. 2005;19:102–108. doi: 10.1097/00005131-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 11.McKinley TO, Tochigi Y, Rudert MJ, et al. Instability-associated changes in contact stress and contact stress rates near a step-off incongruity. J Bone Joint Surg Am. 2008;90:375–383. doi: 10.2106/JBJS.G.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 26:439–443. doi: 10.1097/BOT.0b013e31822a526a. [DOI] [PubMed] [Google Scholar]
- 13.Chissell HR, Jones J. The influence of a diastasis screw on the outcome of Weber type-C ankle fractures. J Bone Joint Surg Br. 1995;77:435–438. [PubMed] [Google Scholar]
- 14.Roberts RS. Surgical treatment of displaced ankle fractures. Clin Orthop Relat Res. 1983:164–170. [PubMed] [Google Scholar]
- 15.Harper MC, Keller TS. A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle. 1989;10:156–160. doi: 10.1177/107110078901000308. [DOI] [PubMed] [Google Scholar]
- 16.Pneumaticos SG, Noble PC, Chatziioannou SN, et al. The effects of rotation on radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle Int. 2002;23:107–111. doi: 10.1177/107110070202300205. [DOI] [PubMed] [Google Scholar]
- 17.Beumer A, Swierstra BA. The influence of ankle positioning on the radiography of the distal tibial tubercles. Surg Radiol Anat. 2003;25:446–450. doi: 10.1007/s00276-003-0147-5. [DOI] [PubMed] [Google Scholar]
- 18.Beumer A, van Hemert WL, Niesing R, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004:227–234. doi: 10.1097/01.blo.0000129152.81015.ad. [DOI] [PubMed] [Google Scholar]
- 19.Nielson JH, Sallis JG, Potter HG, et al. Correlation of interosseous membrane tears to the level of the fibular fracture. J Orthop Trauma. 2004;18:68–74. doi: 10.1097/00005131-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Ebraheim NA, Elgafy H, Padanilam T. Syndesmotic disruption in low fibular fractures associated with deltoid ligament injury. Clin Orthop Relat Res. 2003:260–267. doi: 10.1097/01.blo.0000052935.71325.30. [DOI] [PubMed] [Google Scholar]
- 21.Ebraheim NA, Lu J, Yang H, et al. Radiographic and CT evaluation of tibiofibular syndesmotic diastasis: a cadaver study. Foot Ankle Int. 1997;18:693–698. doi: 10.1177/107110079701801103. [DOI] [PubMed] [Google Scholar]
- 22.Brage ME, Bennett CR, Whitehurst JB, et al. Observer reliability in ankle radiographic measurements. Foot Ankle Int. 1997;18:324–329. doi: 10.1177/107110079701800602. [DOI] [PubMed] [Google Scholar]
- 23.Oae K, Takao M, Naito K, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology. 2003;227:155–161. doi: 10.1148/radiol.2271011865. [DOI] [PubMed] [Google Scholar]
- 24.Marmor M, Hansen E, Han HK, et al. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int. 32:616–622. doi: 10.3113/FAI.2011.0616. [DOI] [PubMed] [Google Scholar]
- 25.Summers HD, Sinclair MK, Stover MD. A reliable method for intraoperative evaluation of syndesmotic reduction. J Orthop Trauma. 2013;27:196–200. doi: 10.1097/BOT.0b013e3182694766. [DOI] [PubMed] [Google Scholar]
- 26.Taser F, Shafiq Q, Ebraheim NA. Three-dimensional volume rendering of tibiofibular joint space and quantitative analysis of change in volume due to tibiofibular syndesmosis diastases. Skeletal Radiol. 2006;35:935–941. doi: 10.1007/s00256-006-0101-9. [DOI] [PubMed] [Google Scholar]
- 27.Gardner MJ, Demetrakopoulos D, Briggs SM, et al. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27:788–792. doi: 10.1177/107110070602701005. [DOI] [PubMed] [Google Scholar]
- 28.Davidovitch RI, Weil Y, Karia R, et al. Intraoperative syndesmotic reduction: three-dimensional versus standard fluoroscopic imaging. J Bone Joint Surg Am. 2013;95:1838–1843. doi: 10.2106/JBJS.L.00382. [DOI] [PubMed] [Google Scholar]
- 29.Atesok K, Finkelstein J, Khoury A, et al. The use of intraoperative three-dimensional imaging (ISO-C-3D) in fixation of intraarticular fractures. Injury. 2007;38:1163–1169. doi: 10.1016/j.injury.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 30.Franke J, von Recum J, Suda AJ, et al. Intraoperative three-dimensional imaging in the treatment of acute unstable syndesmotic injuries. J Bone Joint Surg Am. 94:1386–1390. doi: 10.2106/JBJS.K.01122. [DOI] [PubMed] [Google Scholar]
- 31.Phisitkul P, Ebinger T, Goetz J, et al. Forceps reduction of the syndesmosis in rotational ankle fractures: a cadaveric study. J Bone Joint Surg Am. 2012;94:2256–2261. doi: 10.2106/JBJS.K.01726. [DOI] [PubMed] [Google Scholar]
- 32.Tornetta P, 3rd, Spoo JE, Reynolds FA, et al. Overtightening of the ankle syndesmosis: is it really possible? J Bone Joint Surg Am. 2001;83-A:489–492. doi: 10.2106/00004623-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Miller AN, Barei DP, Iaquinto JM, et al. Iatrogenic syndesmosis malreduction via clamp and screw placement. J Orthop Trauma. 2013;27:100–106. doi: 10.1097/BOT.0b013e31825197cb. [DOI] [PubMed] [Google Scholar]
- 34.Rupp RE. Overcompression of the syndesmosis during ankle fracture fixation: a case report. American journal of orthopedics. 2008;37:259–261. [PubMed] [Google Scholar]
- 35.Lui TH, Ip K, Chow HT. Comparison of radiologic and arthroscopic diagnoses of distal tibiofibular syndesmosis disruption in acute ankle fracture. Arthroscopy. 2005;21:1370. doi: 10.1016/j.arthro.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 36.Stoffel K, Wysocki D, Baddour E, et al. Comparison of two intraoperative assessment methods for injuries to the ankle syndesmosis. A cadaveric study. J Bone Joint Surg Am. 2009;91:2646–2652. doi: 10.2106/JBJS.G.01537. [DOI] [PubMed] [Google Scholar]
- 37.George D, Mallery P. SPSS for Windows Step by Step: A Simple Guide and Reference, 11.0 Update. Allyn and Bacon; 2003. [Google Scholar]
- 38.Gardner MJ, Brodsky A, Briggs SM, et al. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res. 2006;447:165–171. doi: 10.1097/01.blo.0000203489.21206.a9. [DOI] [PubMed] [Google Scholar]
- 39.Mukhopadhyay S, Metcalfe A, Guha AR, et al. Malreduction of syndesmosis--are we considering the anatomical variation? Injury. 42:1073–1076. doi: 10.1016/j.injury.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 40.Wikeroy AK, Hoiness PR, Andreassen GS, et al. No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fractures. J Orthop Trauma. 24:17–23. doi: 10.1097/BOT.0b013e3181bedca1. [DOI] [PubMed] [Google Scholar]
- 41.Richter M, Geerling J, Zech S, et al. Intraoperative three-dimensional imaging with a motorized mobile C-arm (SIREMOBIL ISO-C-3D) in foot and ankle trauma care: a preliminary report. J Orthop Trauma. 2005;19:259–266. doi: 10.1097/01.bot.0000151822.10254.db. [DOI] [PubMed] [Google Scholar]
- 42.Richter M, Zech S. Intraoperative 3-dimensional imaging in foot and ankle trauma-experience with a second-generation device (ARCADIS–3D) J Orthop Trauma. 2009;23:213–220. doi: 10.1097/BOT.0b013e31819867f6. [DOI] [PubMed] [Google Scholar]
- 43.Kendoff D, Citak M, Gardner MJ, et al. Intraoperative 3D imaging: value and consequences in 248 cases. J Trauma. 2009;66:232–238. doi: 10.1097/TA.0b013e31815ede5d. [DOI] [PubMed] [Google Scholar]
- 44.Nault ML, Hebert-Davies J, Laflamme GY, et al. CT Scan Assessment of the Syndesmosis: A New Reproducible Method. J Orthop Trauma. 2013;27:638–641. doi: 10.1097/BOT.0b013e318284785a. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.