Abstract
Background: Breakfast omission is known to be associated with lower 24-h energy intake. However, little is known about downstream eating behaviors subsequent to skipping breakfast in free-living individuals.
Objective: We replicated the traditional crossover design of nutrition studies in a naturalistic setting to compare within-person differences in self-reported eating behaviors, energy intake, and other dietary characteristics of individuals on a day that included breakfast with a day that omitted breakfast.
Design: We used cross-sectional dietary data for 2132 adult respondents who reported breakfast in only one of 2 dietary recalls in the NHANES 2005–2010. Dietary outcomes examined included meal- and snack-eating behaviors, clock time of eating episodes, and intakes of energy, macronutrients, and food groups. Regression methods accounted for replicate diet measurements, covariates, and survey-design characteristics.
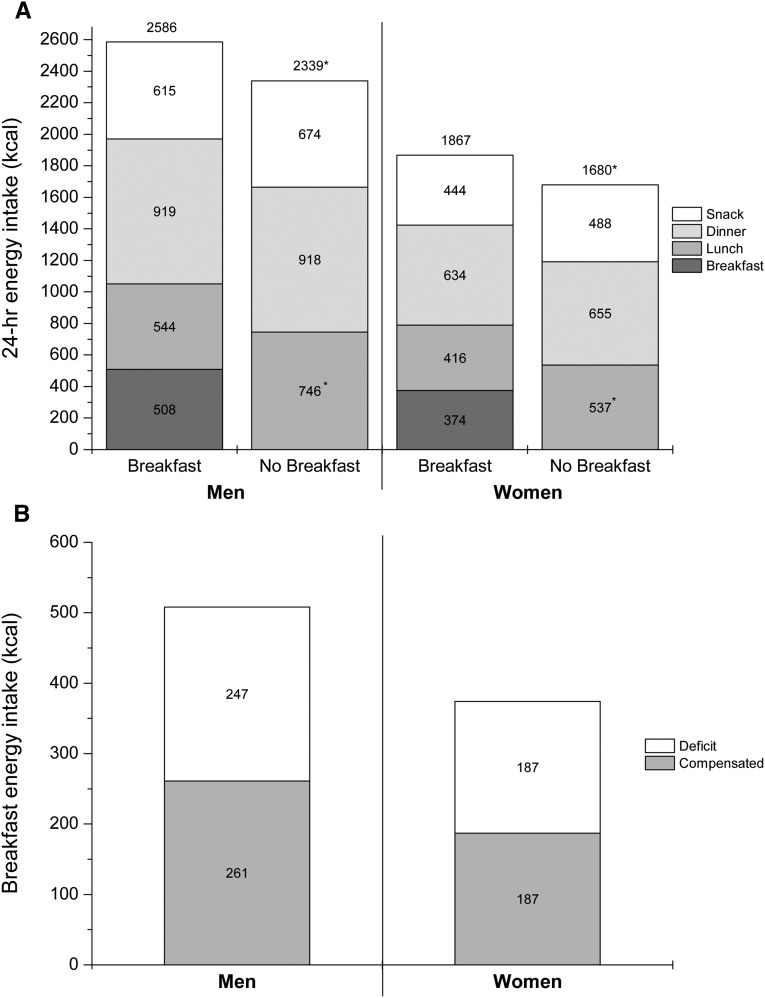
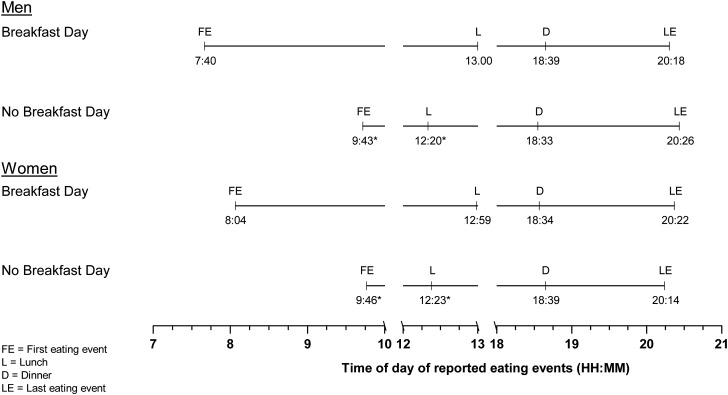
Results: The breakfast meal provided a mean of 508 kcal in men and 374 kcal in women, but differences in 24-h energy intakes between the breakfast and no-breakfast day were 247 and 187 kcal, respectively. Energy intakes at the lunch meal were higher on the no-breakfast day (202 kcal in men and 121 kcal in women), and the reported time of lunch was ∼35 min earlier. The energy contribution of dinner or its reported time did not differ. A higher number of energy-adjusted servings of fruit and whole grains were reported on the breakfast day, but the energy and macronutrient density of reported foods were not different.
Conclusions: In free-living American adults, the eating time for lunch was earlier, and the lunch meal provided more energy on the no-breakfast day than on the breakfast day. Although the quality of dietary selections reflected in the energy and macronutrient density of a day’s intake did not differ between the breakfast and the no-breakfast day, breakfast skippers may need encouragement to consume fruit and whole grains at other eating episodes.
Keywords: breakfast, chrononutrition, eating behaviors, eating frequency, energy density, food pattern equivalents, main meals, NHANES, obesity, time of eating
See corresponding editorial on page 531.
INTRODUCTION
Breakfast skippers have been reported to have lower energy intakes in both cross-sectional (1–5) and short-term crossover studies (6–9) of breakfast manipulation; however, breakfast consumption is generally held to be advantageous for weight management (10). A possible rationale for this belief includes higher rebound energy intake after omission of breakfast as a contributor to weight gain (11). However, recent randomized controlled trials of breakfast manipulation showed that body weights after 6 or 16 wk of breakfast and no-breakfast groups were not different (12, 13). Thus, Levitsky (11) and other authors (14) suggested that lower energy intake because of the omission of breakfast remains mostly uncompensated and may potentially be an adjunct to weight loss (14).
The published literature on the extent of compensatory changes in downstream eating after the omission of breakfast is limited. Observational studies addressed breakfast-related questions about eating behaviors by comparing reporters of breakfast with those of nonreporters (1–5). The commonly used analytic strategy to statistically adjust for individual demographic, lifestyle, and health characteristics leaves the potential for considerable residual confounding in making valid comparisons. For example, possible individual differences in chronotype (15–18) or individual food preferences, selections, and habituation were not considered in analyses of observational data that compared nutritional outcomes in reporters and nonreporters of breakfast.
Short-term, laboratory-based crossover studies of the comparison of downstream energy compensation after the breakfast and no-breakfast test conditions included controls on the amounts or types of foods or the times of their consumption (6–9). Longer-term trials in which subjects self-selected foods in free-living conditions also included constraints on the timing of the first meal (12, 13) and the amount consumed (13). Such constraints on when, what, and how much to consume are unlikely to approximate eating behaviors of free-living individuals functioning in their typical food, work, and leisure environments. For example, free-living subjects who do not report breakfast may consume snacks before their lunch meal with a possible association with the quality of dietary selections, or the time of initiation of the downstream eating events may change on a no-breakfast day. In fact, little is known about the temporal distribution of eating events in relation to breakfast consumption or omission in free-living individuals. This information may allow a more-nuanced understanding of eating behaviors when breakfast is not consumed.
In the current study, we approximate the crossover-study design model in a realistic, unconstrained setting by comparing dietary profiles of respondents who recalled breakfast in one recall but not in a replicate recall. This approach was previously used to compare dietary intakes of drinkers on a day that included alcohol with a day that did not include alcohol (19). In the current study, we used this approach to compare a recall day that included breakfast with a recall day that omitted breakfast for within-person differences in 1) the number and type of eating episodes and their energy contribution, 2) the time of eating events, and 3) the quality of food selections.
METHODS
We used public domain cross-sectional dietary data from the continuous NHANES conducted from 2005 to 2006, 2007 to 2008, and 2009 to 2010 for this study (20, 21). The study protocol was reviewed by the City University of New York Institutional Review Board and was exempted from human subject research regulations because of the use of anonymized public domain data. The NHANES is an ongoing annual survey conducted by the National Center for Health Statistics, CDC. The public domain release includes combined data for 2 survey years. The NHANES has a complex, multistage probability sample design that includes a nationally representative sample of the US civilian, noninstitutionalized population. The survey includes both a household interview and a full medical examination conducted in a specially equipped mobile examination center (MEC)6 (21). Response rates for the MEC-examined sample in these surveys were >70% (22).
Dietary assessment
During the MEC visit, NHANES respondents were administered a 24-h dietary recall that used the automated multiple-pass method algorithm of the USDA (23). The in-person recall in the MEC was computer assisted and administered by a trained dietary interviewer by using a standardized protocol. A second recall, via telephone, was administered to all respondents 3–10 d after the first recall. A standardized set of measuring guides were used during the in-person interview to facilitate the estimation of portion sizes. Measurement tools and guides were also given to respondents to use during the telephone recall.
Analytic sample
All NHANES respondents aged ≥20 y with 2 reliable dietary recalls in each survey cycle (2005–2010) were eligible for inclusion in the study (n = 13784). We excluded pregnant and lactating women (n = 475) and individuals who reported no energy intake in either recall (n = 11), which resulted in a final analytic sample of 13,298. Within this sample, 16.8% of respondents (n = 2132) reported breakfast in one of 2 recalls that they provided and comprised the analytic sample for investigation of within-person differences in eating behaviors and dietary intake.
Exposure assessment
Each NHANES recall collects information on a name and clock time for each eating event reported (21). All recalled food or beverage items reported at one clock time are given the same eating event name. We considered respondents who recalled a day that included breakfast, desayuno, or almuerzo in the previous 24-h as breakfast reporters. A recall that did not include these eating events was considered a no-breakfast recall. This definition of breakfast is consistent with our previous work and the definition used by the USDA (24, 25). However, unlike USDA estimates, if plain water was the only item mentioned for breakfast, we did not consider it breakfast.
Dietary outcomes examined
We used the 24-h dietary recall to examine 3 types of variables as follows: meal and snack behaviors, clock time of eating events, and servings of food patterns equivalents (FPEs).
Meal and snack consumption and clock time of reported eating events
With the use of methods that we previously reported (24, 25), we considered mention of breakfast, lunch, dinner, supper, and brunch, or equivalents in the Spanish language, as main meals. All nonmain-meal eating events were considered snack events. From this information we derived the number of all reported eating events, energy from each individual main meal and all main meals combined, energy from snacks, and time of day of reports of the first and the last eating episode and of individual main meals. When plain tap or bottled water was the only reported item in a recalled eating event, it was not considered an eating event.
FPEs
We merged NHANES dietary data with the FPEs database available for the NHANES 2005–2006, 2007–2008, and 2009–2010 from the USDA website (26). For each individual, we computed the FPE servings of all fruit, whole fruit, all vegetables, all grains, whole grains, total protein, all dairy, added sugars, and discretionary fat reported in each recall.
Energy and macronutrient intake
Energy and macronutrient (grams of fat, carbohydrate, and protein), fiber, and total sugar intakes associated with each recall for each individual were available in the NHANES public domain database (21). We also computed the energy density of reported foods (excluding all beverages) as kilocalories per gram of reported foods in the recall (27).
Statistical analyses
For descriptive purposes, we examined the sociodemographic, family, and lifestyle characteristics of respondents who reported breakfast in both, one, or no recalls. The percentage of the population in each of these 3 breakfast groups was examined by categories of sex, age group, family poverty income ratio (PIR), years of education, BMI, employment status, marital status, and family size. Recall characteristics of respondents who reported breakfast in only one of 2 recalls were compared by using chi-square tests.
We compared the breakfast day and the no-breakfast day for within-individual differences in the outcomes reported by using a linear regression analysis. These models included covariates for the day of the week when breakfast was recalled as well as the recall type (i.e., in-person or telephone recall) and a separate intercept term for each individual in the study. The intercept term controlled for individual-level demographic-, lifestyle-, or health-related factors. For nutrient intakes and food pattern equivalents (FPEs), we adjusted for energy intake.
We present adjusted means (predicted margins) and their 95% CIs for each examined outcome on the recalled breakfast day or the no-breakfast day (28). Tables also include the difference between the breakfast day and no-breakfast day for each examined outcome, the 95% CI of the difference, and the associated level of significance. No adjustments were made for multiple comparisons, although, generally, results with P values ≤0.001 are highlighted in the narrative. These analyses were stratified by sex.
Descriptive analyses were conducted with SAS version 9.2 software (SAS Institute Inc.), and SAS-callable SUDAAN version 11 (29). Regression models that compared dietary intakes and eating behaviors on the breakfast day and no-breakfast day were conducted with STATA version 12.1 software (StataCorp LP). All statistical procedures accounted for the complex survey design and included 2-d diet weights (30, 31). Two-sided P values of Wald’s F test that compared the breakfast day with no-breakfast day are presented.
RESULTS
Nearly 70% of adults reported breakfast in both recalls, 16.8% of adults reported breakfast in one of 2 recalls, and 5.5% of adults did not mention breakfast in both recalls (Table 1). More subjects who reported no breakfast on one or both recalled days were younger (age: 20–39 y), were non-Hispanic black, had lower income (family PIR <130), had higher BMI, and worked night, evening, or rotating shifts. Respondents who were older (≥60 y) had higher family income (family PIR ≥350), were college educated, had a family size of 2, and were married or living as married were less likely to report no breakfast on one or both recalled days (P < 0.0001).
TABLE 1.
Profile of adults reporting breakfast in both, one, or no recall, NHANES 2005–20101
| Reported breakfast in both recalls (n = 10,461; 77.7%) | Reported breakfast in one recall (n = 2132; 16.8%) | Reported breakfast in no recalls (n = 705; 5.5%) | P | |
| Sex | <0.0001 | |||
| Men | 46.9 (45.8, 48.0) | 49.9 (46.4, 53.3) | 60.0 (54.4, 65.3) | |
| Women | 53.1 (52.0, 54.2) | 50.1 (46.7, 53.6) | 40.0 (34.7, 45.7) | |
| Age group, y | <0.0001 | |||
| 20–39 | 31.0 (29.2, 32.9) | 51.1 (47.9, 54.3) | 61.8 (56.1, 67.1) | |
| 40–59 | 40.1 (38.8, 42.2) | 41.2 (37.5, 45.0) | 40.9 (34.9, 47.2) | |
| ≥60 | 28.8 (26.9, 30.9) | 12.3 (11.0, 13.9) | 7.0 (5.3, 9.3) | |
| Race-ethnicity | <0.0001 | |||
| Non-Hispanic white | 73.0 (68.9, 76.8) | 64.6 (60.2, 68.8) | 63.2 (56.6, 69.4) | |
| Non-Hispanic black | 9.2 (7.6, 11.0) | 18.2 (15.1, 21.7) | 21.1 (16.7, 26.4) | |
| Mexican American | 8.0 (6.4, 10.0) | 8.5 (6.6, 11.0) | 6.7 (4.6, 9.7) | |
| Other | 9.8 (7.9, 12.1) | 8.7 (7.0, 10.7) | 8.9 (6.4, 12.3) | |
| Family poverty income ratio, % | <0.0001 | |||
| <130 | 16.4 (14.9, 18.1) | 24.7 (22.1, 27.5) | 28.9 (22.8, 35.5) | |
| 130–349 | 33.6 (31.6, 35.7) | 34.4 (30.6, 38.5) | 35.6 (29.7, 41.7) | |
| ≥350 | 43.9 (41.2, 46.6) | 34.9 (30.9, 39.1) | 31.3 (25.9, 37.2) | |
| Missing (983) | 6.0 (5.3, 6.8) | 5.9 (4.8, 7.3) | 4.5 (3.0, 6.6) | |
| Education | <0.0001 | |||
| <12 y | 17.4 (16.0, 19.0) | 20.1 (17.5, 22.9) | 20.0 (16.1, 24.5) | |
| 12 y | 23.3 (21.9, 24.8) | 25.9 (23.5, 28.7) | 32.6 (27.0, 38.8) | |
| Some college | 29.7 (28.3, 31.2) | 34.1 (30.9, 37.5) | 32.3 (26.4, 38.8) | |
| College or more | 29.5 (27.1, 32.1) | 19.9 (17.5, 22.5) | 15.1 (10.9, 20.6) | |
| Month of first recall | 0.004 | |||
| November to April | 39.2 (32.5, 46.3) | 45.7 (37.8, 53.8) | 37.6 (29.3, 46.7) | |
| May to October | 60.8 (53.6, 67.5) | 54.3 (46.2, 62.1) | 62.4 (53.3, 70.7) | |
| Day of week of first recall | 0.7 | |||
| Monday to Thursday | 57.4 (55.7, 59.1) | 56.3 (53.5, 59.0) | 56.1 (51.8, 60.3) | |
| Friday to Sunday | 42.6 (40.9, 44.3) | 43.7 (41.0, 46.5) | 43.9 (39.7, 48.2) | |
| Day of week of second recall | 0.9 | |||
| Monday to Thursday | 59.5 (57.8, 61.2) | 58.8 (55.0, 62.5) | 59.1 (52.8, 65.1) | |
| Friday to Sunday | 40.5 (38.8, 42.2) | 41.2 (37.5, 45.0) | 40.9 (34.9, 47.2) | |
| BMI, kg/m2 | 0.01 | |||
| <25 | 30.2 (28.3, 32.1) | 33.7 (30.9, 36.6) | 31.4 (26.0, 37.5) | |
| 25–30 | 34.4 (32.9, 36.0) | 29.4 (26.3, 32.7) | 26.4 (22.0, 31.2) | |
| ≥30 | 34.4 (32.8, 36.0) | 36.0 (33.0, 39.1) | 41.3 (36.0, 46.9) | |
| Missing (n = 162) | ||||
| Employment status | <0.0001 | |||
| None | 38.0 (36.2, 39.9) | 34.5 (31.5, 37.6) | 36.5 (30.9, 42.6) | |
| Regular day | 53.2 (51.4, 54.9) | 48.5 (45.0, 52.0) | 44.0 (38.3, 49.8) | |
| Night/evening/rotating | 8.8 (8.0, 9.7) | 17.0 (14.4, 20.0) | 19.5 (15.4, 24.3) | |
| Family size, n | <0.0001 | |||
| 1 | 20.9 (19.4, 22.4) | 23.2 (20.7, 25.9) | 27.7 (23.0, 32.9) | |
| 2 | 32.9 (30.5, 35.4) | 25.7 (23.1, 28.5) | 19.4 (15.1, 24.5) | |
| 3 or 4 | 32.1 (30.5, 33.6) | 33.9 (30.6, 37.3) | 37.1 (32.4, 42.1) | |
| ≥5 | 14.1 (12.5, 15.9) | 17.2 (14.6, 20.2) | 15.8 (12.7, 19.6) | |
| Marital status | <0.0001 | |||
| Married or living as married | 66.3 (64.4, 68.2) | 54.4 (51.4, 57.3) | 50.1 (45.0, 55.3) | |
| All others | 33.7 (31.8, 35.6) | 45.6 (42.7, 48.6) | 49.8 (44.7, 55.0) |
All values are weighted percentages; 95% CIs in parentheses. P values were determined by using the chi-square test of independence.
In subjects who reported breakfast in one of 2 recalls, a higher percentage of in-person recalls (first recall) omitted breakfast (P ≤ 0.001), but the weekday of recalled intake was not different (Table 2). Lunch meal was mentioned by >80% of subjects on the no-breakfast day relative to 68% of subjects on the breakfast day (P < 0.001). The percentage of subjects who reported dinner on the breakfast or the no-breakfast day was not different.
TABLE 2.
Recall characteristics of adults reporting breakfast in any one of 2 dietary recalls, NHANES 2005–20101
| Men |
Women |
|||
| Breakfast day (n = 1095) | No-breakfast day (n = 1095) | Breakfast day (n = 1037) | No-breakfast day (n = 1037) | |
| Type of 24-h recall | ||||
| In-person recall | 40.7 (36.3, 45.3) | 59.2 (54.7, 63.7) | 42.1 (37.9, 46.5) | 57.9 (53.5, 62.1) |
| Telephone recall | 59.2 (54.7, 63.7) | 40.7 (36.3, 45.3) | 57.9 (53.5, 62.1) | 42.1 (37.9, 46.5) |
| P | <0.001 | <0.001 | ||
| Day of recalled intake | ||||
| Monday to Thursday | 56.9 (52.0, 61.7) | 56.1 (51.6, 60.6) | 61.3 (57.3, 65.1) | 55.9 (51.2, 60.4) |
| Friday to Sunday | 43.1 (38.3, 48.0) | 43.9 (39.4, 48.4) | 38.7 (34.9, 42.7) | 44.1 (39.6, 48.8) |
| P | 0.8 | 0.1 | ||
| Ate lunch on recalled day? | ||||
| Yes | 68.5 (64.5, 72.3) | 80.2 (76.7, 83.3) | 71.7 (67.7, 75.3) | 82.1 (78.8, 84.8) |
| No | 31.5 (27.7, 35.5) | 19.8 (16.7, 23.2) | 28.3 (24.6, 32.3) | 18.0 (15.1, 21.2) |
| P | <0.001 | <0.001 | ||
| Ate dinner on recalled day? | ||||
| Yes | 88.9 (85.9, 91.3) | 88.8 (86.2, 91.0) | 90.1 (87.2, 92.4) | 91.9 (89.4, 93.9) |
| No | 11.1 (8.7, 14.1) | 11.2 (9.0, 13.8) | 9.9 (7.6, 12.8) | 8.1 (6.1, 10.6) |
| P | 0.9 | 0.1 | ||
All values are weighted percentages; 95% CIs in parentheses. P values were determined by using the chi-square test of independence.
Meal and snack contributions to energy intake on days with and without breakfast
The number of all reported eating episodes was higher on the breakfast day than on the no-breakfast day in both men and women (Table 3) (P < 0.001). The number of snack episodes reported was lower on the breakfast day than on the no-breakfast day (P ≤ 0.02). Energy intake from breakfast on the breakfast day was 508 kcal in men and 374 kcal in women (Figure 1). In men, the 24-h energy intake on the breakfast day and no-breakfast day was 2586 and 2339 kcal, respectively (difference: 247 kcal) (P < 0.001) (Figure 1A). In women, 24-h energy intake on the breakfast day was 1867 kcal compared with 1680 kcal on the no-breakfast day (difference: 187 kcal) (P < 0.001) (Figure 1B). Energy intake from lunch was ∼30% lower on the breakfast day than on the no-breakfast day in both sexes (−202 kcal in men and −121 kcal in women) (P < 0.001). Energy consumed at dinner or as snacks was not different between the breakfast day and no-breakfast day in both sexes. However, the relative energy contribution of meals (as the percentage of 24-h energy) was higher, but that from snacks was lower on the breakfast day than on the no-breakfast day (P < 0.001). The number of reported eating events at or after 2000 did not differ between the breakfast day and no-breakfast day.
TABLE 3.
Within-person differences in meal and snack behaviors between the 24-h recall that included a breakfast meal compared with the recall without breakfast in adults aged ≥20 y, NHANES 2005–20101
| Men (n = 2190) |
Women (n = 2074) |
|||||||
| Dependent variable | Breakfast day | No-breakfast day | Difference (breakfast day – no-breakfast day) | P | Breakfast day | No-breakfast day | Difference (breakfast day – no-breakfast day) | P |
| Eating episodes, n | 4.7 (4.5, 4.9) | 4.1 (3.9, 4.2) | 0.61 (0.43, 0.78) | <0.001 | 4.8 (4.7, 5.0) | 4.1 (4.0, 4.3) | 0.68 (0.52, 0.85) | <0.001 |
| Snack episodes, n | 1.97 (1.81, 2.13) | 2.28 (1.14, 2.42) | −0.31 (−0.47, −0.14) | <0.001 | 2.12 (2.17, 2.49) | 2.33 (1.96, 2.27) | −0.21 (−0.38, −0.04) | 0.02 |
| Eating episodes at or after 2000, n | 0.85 (0.77, 0.93) | 0.92 (0.85, 0.98) | −0.07 (−0.15, 0.02) | 0.1 | 0.86 (0.79, 0.92) | 0.83 (0.76, 0.89) | 0.03 (−0.05, 0.11) | 0.1 |
| Total energy, kcal | 2586 (2481, 2692) | 2339 (2225, 2454) | 247 (121, 373) | <0.001 | 1867 (1801, 1934) | 1680 (1612, 1749) | 187 (121, 253) | <0.001 |
| Breakfast energy, kcal | 508 (477, 539) | — | 374 (343, 404) | – | ||||
| Snack energy before lunch (men: n = 1554; women: n = 1538), kcal | 141 (99, 191) | 179 (143, 216) | −39 (−89, 12) | 0.1 | 87 (64, 109) | 129 (104, 155) | −42 (−79, −6) | 0.02 |
| Lunch energy, kcal | 544 (492, 595) | 746 (695, 798) | −202 (−270, −134) | <0.001 | 416 (379, 453) | 537 (501, 573) | −121 (−170, −71) | <0.001 |
| Dinner energy, kcal | 919 (860, 979) | 918 (857, 977) | 2.4 (−71, 76) | 0.9 | 634 (601, 670) | 655 (611, 697) | −18 (−60, 23) | 0.4 |
| Main meal energy,2 kcal | 1971 (1886, 2057) | 1665 (1580, 1749) | 306 (209, 404) | <0.001 | 1423 (1357, 1489) | 1192 (1133, 1251) | 231 (162, 300) | <0.001 |
| 24-h energy from main meals, % | 78 (76, 79) | 73 (71, 74) | 4.86 (2.62, 7.09) | <0.001 | 77 (76, 79) | 72 (70, 74) | 5.6 (3.94, 8.0) | <0.001 |
| Snack energy, kcal | 615 (555, 675) | 674 (612, 737) | −60 (−131, 12.3) | 0.1 | 444 (407, 481) | 488 (443, 534) | −44 (−100, 11) | 0.1 |
| 24-h energy from snacks, % | 22 (20, 24) | 27 (26, 29) | −4.86 (−7.09, −2.62) | <0.001 | 22 (21, 24) | 28 (26, 30) | −5.5 (−7.9, −3.2) | <0.001 |
| 24-h energy from eating episodes reported at or after 2000, % | 17.7 (15.9, 19.5) | 20.1 (18.3, 22.0) | −2.4 (−4.8, −0.03) | 0.05 | 16.9 (15.4, 18.5) | 18.6 (16.9, 20.2) | −1.6 (−3.5, 0.2) | 0.1 |
All values are adjusted means; 95% CIs in parentheses. Differences were determined by using linear regression models that included each dependent variable as a continuous outcome and the mention or omission of breakfast, day of the week of recall (Monday to Thursday and Friday to Sunday), and recall type (i.e., in-person or telephone recall) as independent variables along with a separate intercept term for each individual in the study. P values were determined by using Wald’s F test.
Breakfast, lunch, dinner, or supper and their equivalents in the Spanish language were considered main meals.
FIGURE 1.
Within-person differences in distribution of 24-h energy intake into named eating episodes on the breakfast day and no-breakfast day reported by adults in the NHANES 2005–2010. (A) Total, breakfast, lunch, dinner, and snack energy intakes reported in the 24-h recall of a breakfast day and no-breakfast day. Estimates are predicted margins from linear regression models that included each dependent variable as a continuous outcome and the mention or omission of breakfast, day of the week of recall (Monday to Thursday and Friday to Sunday), and recall type (i.e., in-person or telephone recall) as independent variables along with a separate intercept term for each individual in the study. (Men, n = 1095 on the breakfast day and n = 1095 on the no-breakfast day; women, n = 1037 on the breakfast day and n = 1037 on the no-breakfast day.) *Significantly different from that reported on the breakfast day within each sex, P < 0.001. (B) Compensated and uncompensated breakfast energy intake on the no-breakfast day in men and women. Estimates are predicted margins from linear regression models that included each dependent variable as a continuous outcome and the mention or omission of breakfast, day of the week of recall (Monday to Thursday and Friday to Sunday), and recall type (i.e., in-person or telephone recall) as independent variables along with a separate intercept term for each individual in the study.
Reported times of eating events on days with and without breakfast
Not surprisingly, the clock time of the first eating episode of the recall day that included breakfast was earlier than that on the no-breakfast day (difference: −123 min in men and −101 min in women) (P < 0.001) (Figure 2; Supplemental Table 1). Relative to on the no-breakfast day, the clock time of lunch was 39 min later in men and 36 min later in women on the breakfast day (P < 0.001). However, reported times of dinner or the last recalled eating event were not different between the breakfast day and no-breakfast day. On the breakfast day, the interval between the first and the last eating episodes of the day was longer in both men and women (P < 0.001), but intermeal intervals were longer only in women (P < 0.001) (Supplemental Table 1).
FIGURE 2.
Reported time of day for eating events on the breakfast day and no-breakfast day in adult men and women, NHANES 2005–2010. Estimates are predicted margins from linear regression models that included each dependent variable as a continuous outcome and the mention or omission of breakfast, day of the week of recall (Monday to Thursday and Friday to Sunday), and recall type (i.e., in-person or telephone recall) as independent variables along with a separate intercept term for each individual in the study. (Men, n = 1095 on the breakfast day and n = 1095 on the no-breakfast day; women, n = 1037 on the breakfast day and n = 1037 on the no-breakfast day.) *Significantly different from that reported on the breakfast day within each sex, P < 0.001. HH:MM, hours:minutes.
Energy density and FPEs on days with and without breakfast
Total amounts of reported foods and beverages were higher on the breakfast day (P < 0.001); however, the energy density (kcal/g) of all foods (no beverages) or the percentage of 24-h energy from beverages was not different between the breakfast day and no-breakfast day (Table 4).
TABLE 4.
Within-person differences in FPEs in the 24-h recall that included a breakfast meal compared with the recall without breakfast in adults aged ≥20 y, NHANES 2005–20101
| Men (n = 2190) |
Women (n = 2074) |
|||||||
| Dependent variable | Breakfast day | No-breakfast day | Difference (breakfast day – no-breakfast day) | P | Breakfast day | No-breakfast day | Difference (breakfast day – no-breakfast day) | P |
| Amount of all foods and beverages, g | 2954 (2802, 3106) | 2690 (2555, 2824) | 264 (114, 413) | 0.001 | 2136 (2022, 2250) | 1960 (1854, 2066) | 176 (85, 268) | <0.001 |
| Energy density of foods only, kcal/g | 2.06 (2.01, 2.11) | 2.06 (2.02, 2.11) | −0.0009 (−0.06, 0.06) | 1.0 | 1.99 (1.94, 2.04) | 1.99 (1.94, 2.04) | −0.002 (−0.06, 0.06) | 0.9 |
| Energy from beverages, % | 23.0 (21.6, 24.5) | 22.0 (20.8, 23.3) | 1.01 (−0.38, 2.41) | 0.1 | 18.7 (17.1, 20.2) | 19.4 (17.8, 20.9) | −0.72 (−2.40, 0.96) | 0.4 |
| Total fruit servings, cup equivalents | 0.88 (0.75, 1.01) | 0.66 (0.54, 0.77) | 0.23 (0.09, 0.36) | 0.002 | 0.85 (0.75, 0.94) | 0.60 (0.52, 0.68) | 0.25 (0.12, 0.37) | <0.001 |
| Energy-intake–adjusted total fruit servings, cup equivalents | 0.86 (0.74, 0.99) | 0.68 (0.56, 0.79) | 0.19 (0.06, 0.31) | 0.005 | 0.82 (0.73, 0.91) | 0.62 (0.54, 0.70) | 0.20 (0.08, 0.32) | 0.002 |
| Total whole fruit servings, cup equivalents | 0.48 (0.39, 0.57) | 0.38 (0.30, 0.46) | 0.10 (0.03, 0.18) | 0.008 | 0.58 (0.50, 0.65) | 0.40 (0.33, 0.46) | 0.18 (0.10, 0.27) | <0.001 |
| Energy-intake–adjusted whole fruit servings, cup equivalents | 0.48 (0.39, 0.57) | 0.38 (0.30, 0.46) | 0.10 (0.03, 0.18) | 0.009 | 0.57 (0.49, 0.64) | 0.40 (0.34, 0.47) | 0.16 (0.08, 0.25) | <0.001 |
| Total vegetable servings, cup equivalents | 1.64 (1.51, 1.76) | 1.59 (1.45, 1.73) | 0.04 (−0.14, 0.24) | 0.6 | 1.47 (1.34, 1.59) | 1.29 (1.18, 1.40) | 0.17 (0.05, 0.30) | 0.006 |
| Energy-intake–adjusted total vegetable servings, cup equivalents | 1.57 (1.46, 1.69) | 1.66 (1.53, 1.78) | −0.08 (−0.23, 0.07) | 0.3 | 1.43 (1.30, 1.55) | 1.33 (1.22, 1.44) | 0.09 (−0.03, 0.22) | 0.1 |
| Total grain servings, oz equivalents | 7.65 (7.13, 8.18) | 6.85 (6.37, 7.34) | 0.80 (0.28, 1.33) | 0.003 | 5.64 (5.28, 5.99) | 5.08 (4.67, 5.49) | 0.55 (0.05, 1.05) | 0.03 |
| Energy-intake–adjusted total grain servings, oz equivalents | 7.28 (6.84, 7.72) | 7.22 (6.73, 7.71) | 0.07 (−0.30, 0.43) | 0.7 | 5.37 (5.03, 5.72) | 5.34 (4.95, 5.74) | 0.03 (−0.42, 0.49) | 0.1 |
| Whole grain servings, oz equivalents | 0.71 (0.52, 0.89) | 0.39 (0.31, 0.48) | 0.32 (0.14, 0.49) | 0.001 | 0.58 (0.47, 0.69) | 0.39 (0.26, 0.51) | 0.19 (0.09, 0.30) | 0.001 |
| Energy-intake–adjusted whole grain servings, oz equivalents | 0.68 (0.51, 0.96) | 0.41 (0.33, 0.50) | 0.27 (0.12, 0.42) | 0.001 | 0.56 (0.45, 0.68) | 0.40 (0.27, 0.53) | 0.16 (0.05, 0.27) | 0.005 |
| Protein servings, oz equivalents | 7.74 (7.36, 8.12) | 7.11 (6.64, 7.59) | 0.63 (0.04, 1.21) | 0.04 | 4.97 (4.54, 5.40) | 4.59 (4.28, 4.91) | 0.38 (−0.12, 0.88) | 0.1 |
| Energy-intake–adjusted protein servings, oz equivalents | 7.47 (7.10, 7.85) | 7.38 (6.93, 7.82) | 0.09 (−0.43, 0.62) | 0.7 | 4.76 (4.36, 5.16) | 4.81 (4.48, 5.14) | −0.05 (−0.52, 0.42) | 0.8 |
| Total dairy servings, cup equivalents | 1.82 (1.64, 2.00) | 1.59 (1.40, 1.78) | 0.23 (0.03, 0.44) | 0.02 | 1.51 (1.37, 1.67) | 1.20 (1.07, 1.32) | 0.31 (0.16, 0.45) | <0.001 |
| Energy-intake–adjusted total dairy servings, cup equivalents | 1.71 (1.54, 1.88) | 1.70 (1.51, 1.89) | 0.01 (−0.17, 0.20) | 0.9 | 1.43 (1.30, 1.57) | 1.27 (1.15, 1.40) | 0.15 (0.06, 0.23) | 0.001 |
| Oil + solid fat, g equivalents | 73.2 (69.2, 77.3) | 66.8 (62.3, 71.3) | 6.4 (1.41, 11.4) | 0.01 | 57.3 (54.1, 60.5) | 50.1 (47.0, 53.1) | 7.2 (3.2, 11.3) | 0.001 |
| Energy-intake–adjusted oil + solid fat, g equivalents | 69.1 (65.5, 72.6) | 71.0 (67.1, 74.9) | −1.9 (−4.4, 0.06) | 0.1 | 53.9 (51.2, 56.6) | 53.5 (50.8, 56.2) | 0.4 (−2.1, 3.0) | 0.7 |
| Added sugar, tsp equivalents | 23.3 (21.4, 25.3) | 21.8 (20.3, 23.3) | 1.54 (−0.11, 3.19) | 0.07 | 17.2 (16.0, 18.3) | 17.2 (15.8, 18.6) | −0.02 (−1.50, 1.44) | 1.0 |
| Energy-intake–adjusted added sugar, tsp equivalents | 22.4 (20.5, 24.2) | 22.7 (21.2, 24.3) | −0.4 (−1.8, 1.1) | 0.6 | 16.3 (15.2, 17.3) | 18.1 (16.7, 19.4) | −1.8 (−3.1, 0.5) | 0.008 |
All values are adjusted means; 95% CIs in parentheses. Differences were determined by using linear regression models that included each dependent variable as a continuous outcome and the mention or omission of breakfast, day of the week of recall (Monday to Thursday and Friday to Sunday), and recall type (i.e., in-person or telephone recall) as independent variables along with a separate intercept term for each individual in the study. P values were determined by using Wald’s F test. FPE, food patterns equivalent; tsp, teaspoon.
Reported fruit, vegetable (women only), grain, whole-grain, dairy, and oils plus solid-fat serving equivalents were significantly higher (P ≤ 0.03) on the breakfast day than on the no-breakfast day in both men and women (Table 4). Added sugar equivalents (teaspoon) did not differ between the breakfast day and no-breakfast day in both men and women.
In regression models with adjustment for total energy intake, reported serving equivalents of total fruit, whole fruit, and whole grain remained significantly higher on the breakfast day than on the no-breakfast day in both sexes (P ≤ 0.008) (Table 4). In women, total dairy servings were also significantly higher on the breakfast day in energy-adjusted models. Differences in servings of total grain and oils plus solid fat between the breakfast day and no-breakfast day were attenuated and no longer significant with adjustment for energy intake. However in women, energy-adjusted added sugar equivalents were higher on the no-breakfast day (P = 0.008).
Macronutrient and fiber intakes on days with and without breakfast
Grams of carbohydrate, fat, protein, fiber, and total sugars were higher on the breakfast day than on the no-breakfast day in both men and women (Table 5). However, these differences were not significant after adjustment for energy intake (P > 0.05).
TABLE 5.
Within-person differences in energy and macronutrient intake for the 24-h recall that included a breakfast meal compared with the day without breakfast in the recall in adults aged ≥20 y, NHANES 2005–20101
| Men (n = 2190) |
Women (n = 2074) |
|||||||
| Dependent variable | Breakfast day | No-breakfast day | Difference (breakfast day – no-breakfast day) | P | Breakfast day | No-breakfast day | Difference (breakfast day – no-breakfast day) | P |
| Total energy, kcal | 2586 (2481, 2692) | 2339 (2225, 2454) | 247 (121, 373) | <0.001 | 1867 (1801, 1934) | 1680 (1612, 1749) | 187 (121, 253) | <0.001 |
| Carbohydrate, g | 304 (288, 320) | 273 (260, 287) | 30.7 (14.5, 46.9) | <0.001 | 227 (219, 235) | 207 (198, 216) | 20 (11.2, 28.6) | <0.001 |
| Carbohydrate, % of energy | 48 (47, 49) | 47 (46, 48) | 0.16 (−1.1, 1.40) | 0.8 | 49.3 (48.3, 50.3) | 49.7 (48.7, 50.8) | −0.44 (−1.88, 1.0) | 0.5 |
| Fat, g | 96 (91, 100) | 87 (82, 93) | 8.6 (3.0, 14.2) | 0.003 | 73 (69, 77) | 64 (61, 68) | 9.1 (4.3, 13.9) | <0.001 |
| Fat, % of energy | 32.7 (32.0, 33.4) | 32.9 (32.1, 33.8) | −0.22 (−1.02, 0.57) | 0.6 | 34.5 (33.6, 35.5) | 33.7 (32.8, 34.5) | 0.86 (−0.43, 2.16) | 0.2 |
| Protein, g | 100 (96, 104) | 90 (86, 95) | 9.3 (4.7, 13.9) | <0.001 | 70 (67, 74) | 63 (60, 66) | 7.1 (3.5, 10.7) | <0.001 |
| Protein, % of energy | 15.9 (15.4, 16.4) | 15.9 (15.5, 16.2) | 0.03 (−0.57, 0.64) | 0.9 | 15.5 (15.1, 16.0) | 15.6 (15.0, 16.1) | −0.01 (−0.57, 0.54) | 0.9 |
| Fiber, g | 16.2 (15.2, 17.2) | 14.6 (13.5, 15.7) | 1.58 (0.53, 2.64) | 0.004 | 13.6 (12.9, 14.3) | 12.0 (11.1, 12.9) | 1.6 (1.0, 2.2) | <0.001 |
| Energy adjusted fiber intake, g | 15.6 (14.6, 16.6) | 15.2 (14.2, 16.3) | 0.34 (−0.45, 1.13) | 0.4 | 13.1 (12.4, 13.7) | 12.5 (11.7, 13.4) | 0.55 (−0.01, 1.16) | 0.06 |
| Total sugar, g | 138 (128, 148) | 123 (115, 131) | 14.6 (5.8, 23.3) | 0.002 | 106 (101, 112) | 99 (93, 105) | 7.7 (1.1, 14.4) | 0.02 |
| Energy adjusted total sugar intake, g | 132 (123, 142) | 129 (121, 136) | 3.7 (−2.7, 10.2) | 0.2 | 102 (97, 106) | 104 (98, 110) | −2.0 (−0.01, 1.2) | 0.5 |
| Alcohol, g | 18.6 (14.9, 22.2) | 16.9 (13.9, 20.0) | 1.64 (−2.1, 5.4) | 0.4 | 6.1 (4.1, 8.1) | 6.0 (4.0, 7.9) | 0.19 (−2.0, 2.5) | 0.9 |
All values are adjusted means; 95% CIs in parentheses. Differences were determined by using linear regression models that included each dependent variable as a continuous outcome and the mention or omission of breakfast, day of the week of recall (Monday to Thursday and Friday to Sunday), and recall type (i.e., in-person or telephone recall) as independent variables along with a separate intercept term for each individual in the study. P values were determined by using Wald’s F test.
DISCUSSION
The key findings of this within-person comparison of eating behaviors and dietary characteristics on the breakfast day and no-breakfast day were as follows: 1) mean 24-h energy intake was ∼10% lower on the no-breakfast day; 2) there were a higher number and percentage of energy from snacks on the no-breakfast day; 3) lunch provided higher energy and was reported earlier on the no-breakfast day; 4) there were no differences in the quality of foods selected as reflected in energy density and energy-adjusted macronutrient, fiber, and total sugars; and 5) there was a higher number of energy-adjusted servings of fruit, whole grains, and dairy (women only) on the breakfast day.
What were the differences in downstream energy intake between the breakfast day and no-breakfast day?
The breakfast meal provided a mean of 508 kcal in men and 374 kcal in women; however, corresponding differences in 24-h energy intake between the breakfast day and no-breakfast day were ∼50% lower at 247 kcal in men and 187 kcal in women. Thus, nonbreakfast eating episodes on the no-breakfast day included a higher amount of energy than on the breakfast day. These findings on the extent of difference in energy intake between the breakfast day and no-breakfast day differed from results of 2 controlled crossover studies (6, 7) and a 6-wk intervention trial (13), which reported either no difference (6) or very little difference (7, 13). The findings of previous studies may partially reflect constraints on when eating was allowed in the no-breakfast condition (6, 7, 13) and the provision of foods available for consumption (6, 7).
In men, >75% of the breakfast energy on the no-breakfast day, and in women, 65% of the breakfast energy on the no-breakfast day, was made up by higher energy intake at the lunch meal, but energy consumed at dinner or as snacks did not differ between the 2 recall days in both sexes. In cross-sectional comparisons of breakfast reporters and skippers by using NHANES 2003–2004 data, Levitsky and Pacanowski (7) reported significantly higher energy at all nonbreakfast meal and snack events. However, in the crossover study of Levitsky and Pacanowski (7) that included an ad lib breakfast, only lunch energy intake was higher in the no-breakfast test condition. We also found that energy intake from snacks consumed before lunch on the no-breakfast day was slightly higher (especially in women; P < 0.02) from that reported on the breakfast day. Overall, these findings suggest that, under free-living conditions, compensation for the omitted breakfast energy occurred in eating events proximal to the omitted meal. This finding is consistent with the higher perceived hunger in the late morning in the no-breakfast condition in a crossover study of adolescents (8).
Did the time of reported downstream eating events differ on breakfast and no-breakfast recall days?
On the no-breakfast day, the reported time of lunch was >30 min earlier than on the breakfast day. However, despite the earlier lunch, the reported dinner time or time of the last eating episode did not differ between the breakfast day and no-breakfast day. It has been suggested that the peak of biologic hunger tends to occur in the evening and is generally not responsive to eating events occurring earlier in the day (32). In a recent analysis of secular trends in eating behaviors in the US population, we reported that, although reported breakfast and lunchtime have changed over the past 40 y (they are ∼30 min later), the time of day when dinner was reported has not changed (25).
Late-day eating may be associated with more-adverse metabolic consequences (33). If breakfast omission is associated with more late-in-the-day eating, then that could be another potential mechanism for affecting health. In the current study, there was little evidence of an extension of the eating period into evening hours on the no-breakfast day because the average time of the last reported eating event of the day did not differ between the breakfast day and no-breakfast day. We did not find any other studies in which times of eating events in relation to breakfast consumption or omission were reported.
Did the quality of dietary selections differ on breakfast and no-breakfast recall days?
In the current study, women reported slightly higher intake of energy-adjusted added sugars (but not of total sugars) on the no-breakfast day; however, the energy and macronutrient density of foods consumed did not differ between the breakfast day and no-breakfast day, which suggested a similar qualitative nature of the foods selected on both days. These results differ from findings from a 6-wk intervention trial of breakfast ≥700 kcal and no breakfast, whereby carbohydrate and sugar intakes were higher in breakfast reporters (13). However, the higher energy-adjusted servings of total and whole fruit and whole grains in both men and women and dairy in women on the breakfast day suggest the relative importance of the breakfast meal for consumption of these food groups.
Strengths and limitations
Our study was an attempt to replicate the traditional crossover study design of nutrition studies in a naturalistic setting in a large and diverse sample of the US population. Our approach of the within-person comparison of various outcomes adjusted for the residual confounding that can occur in cross-sectional studies that compare breakfast reporters and nonreporters.
Although the NHANES 24-h dietary recall is collected by using a validated automated multiple-pass algorithm, which has been reported to reduce bias (34), we acknowledge the observational nature of our study where recalls were self-reported. However, note that, even in long-term or short-term randomized intervention trials, subjects usually self-report their dietary intake. Thus, the measurement error known to be associated with self-reported dietary intake (35) may expectedly have been present in our study and in other studies (including intervention trials). Moreover, previous trials have reported an intervention-associated bias in dietary reporting in intervention trials (36–38). Although we presented no empirical evidence in our study, we speculate that the types of reporting errors within an individual are more likely to be similar than among individuals. Thus, our analytic approach of comparing the diet within individuals may have reduced the effects of person-level measurement error for our inferences. Because of our study design, we focused our analysis on the subset of individuals in NHANES who reported breakfast in only one of the two 24-h recalls.
To our knowledge, no validation studies of eating behaviors (such as meal or snack episodes or time of their occurrence) examined in our study are available, nor are we aware of any biomarkers which can be used for such a purpose. We defined eating behaviors on the basis of their characterization by respondents; results may possibly differ on the basis of other definitions.
Because of the potential that dietary behaviors may vary by an individual’s demographic characteristics, the profile of our sample (Table 1) should be considered when applying our results to other samples. It is also possible that observed differences in examined dietary outcomes between the breakfast day and no-breakfast day may have reflected transitional or unstable eating patterns.
The definition of breakfast used in the current study did not distinguish between the amount and type of foods or beverages reported for the breakfast meal. Future work that uses the current study design may want to explore whether the findings reported may be replicated in analyses stratified for qualitative and quantitative characteristics of the reported breakfast or sociodemographic profile of respondents.
In conclusion, although the eating time for lunch was earlier, and the lunch meal provided more energy intake on a no-breakfast day than on the day that included breakfast, the difference in overall 24-h energy intake between the 2 recalls did not equal the magnitude of omitted breakfast energy. The quality of dietary selections reflected in the energy and macronutrient density of a day’s intake was not different between the breakfast day and no-breakfast day, but fruit and whole grains were lower when breakfast was omitted and should be encouraged at other eating episodes on a no-breakfast day.
Acknowledgments
We thank Lisa Licitra Kahle and Fannie Zhang (IMS, Silver Spring, Maryland) for expert SAS, SUDAAN, and STATA programming support and David Check (National Cancer Institute, NIH, Bethesda, Maryland) for graphics support.
The authors’ responsibilities were as follows: AKK: conceptualized the study question, designed the research, analyzed data, wrote the manuscript, and had primary responsibility for the final content of the manuscript; and BIG: provided guidance on the study design and analytic strategy and reviewed the manuscript for important intellectual content. Neither author reported a conflict of interest related to the study.
Footnotes
Abbreviations used: FPE, food patterns equivalent; MEC, mobile examination center; PIR, poverty income ratio.
REFERENCES
- 1.Nicklas TA, Myers L, Reger C, Beech B, Berenson GS. Impact of breakfast consumption on nutritional adequacy of the diets of young adults in Bogalusa, Louisiana: ethnic and gender contrasts. J Am Diet Assoc 1998;98:1432–8. [DOI] [PubMed] [Google Scholar]
- 2.Cho S, Dietrich M, Brown CJ, Clark CA, Block G. The effect of breakfast type on total daily energy intake and body mass index: results from the Third National Health and Nutrition Examination Survey (NHANES III). J Am Coll Nutr 2003;22:296–302. [DOI] [PubMed] [Google Scholar]
- 3.Song WO, Chun OK, Obayashi S, Cho S, Chung CE. Is consumption of breakfast associated with body mass index in US adults? J Am Diet Assoc 2005;105:1373–82. [DOI] [PubMed] [Google Scholar]
- 4.Kant AK, Andon MB, Angelopoulos TJ, Rippe JM. Association of breakfast energy density with diet quality and body mass index in American adults: National Health and Nutrition Examination Surveys, 1999-2004. Am J Clin Nutr 2008;88:1396–404. [DOI] [PubMed] [Google Scholar]
- 5.O’Neil CE, Nicklas TA, Fulgoni VL 3rd. Nutrient intake, diet quality, and weight/adiposity parameters in breakfast patterns compared with no breakfast in adults: National Health and Nutrition Examination Survey 2001-2008. J Acad Nutr Diet 2014;114(12 Suppl):S27–43. [DOI] [PubMed] [Google Scholar]
- 6.Kral TV, Whiteford LM, Heo M, Faith MS. Effects of eating breakfast compared with skipping breakfast on ratings of appetite and intake at subsequent meals in 8- to 10-y-old children. Am J Clin Nutr 2011;93:284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levitsky DA, Pacanowski CR. Effect of skipping breakfast on subsequent energy intake. Physiol Behav 2013;119:9–16. [DOI] [PubMed] [Google Scholar]
- 8.Leidy HJ, Ortinau LC, Douglas SM, Hoertel HA. Beneficial effects of a higher-protein breakfast on the appetitive, hormonal, and neural signals controlling energy intake regulation in overweight/obese, “breakfast-skipping,” late-adolescent girls. Am J Clin Nutr 2013;97:677–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gonzalez JT, Veasey RC, Rumbold PL, Stevenson J. Breakfast and exercise contingently affect post- prandial metabolism and energy balance in physically active males. Br J Nutr 2013;110:721–32. [DOI] [PubMed] [Google Scholar]
- 10.Dietary Guidelines Advisory Committee. 2010. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2010, to the Secretary of Agriculture and the Secretary of Health and Human Services. U.S. Department of Agriculture, Agricultural Research Service, Washington (DC).
- 11.Levitsky DA. Next will be apple pie. Am J Clin Nutr 2014;100:503–4. [DOI] [PubMed] [Google Scholar]
- 12.Dhurandhar EJ, Dawson J, Alcorn A, Larsen LH, Thomas EA, Cardel M, Bourland AC, Astrup A, St-Onge MP, Hill JO, et al. The effectiveness of breakfast recommendations on weight loss: a randomized controlled trial. Am J Clin Nutr 2014;100:507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr 2014;100:539–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zilberter T, Zilberter EY. Breakfast: to skip or not to skip? Front Public Health 2014;2:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fleig D, Randler C. Association between chronotype and diet in adolescents based on food logs. Eat Behav 2009;10:115–8. [DOI] [PubMed] [Google Scholar]
- 16.Sato-Mito N, Shibata S, Sasaki S, Sato K. Dietary intake is associated with human chronotype as assessed by both morningness-eveningness score and preferred midpoint of sleep in young Japanese women. Int J Food Sci Nutr 2011;62:525–32. [DOI] [PubMed] [Google Scholar]
- 17.Kanerva N, Kronholm E, Partonen T, Ovaskainen ML, Kaartinen NE, Konttinen H, Broms U, Männistö S. Tendency toward eveningness is associated with unhealthy dietary habits. Chronobiol Int 2012;29:920–7. [DOI] [PubMed] [Google Scholar]
- 18.Reutrakul S, Hood MM, Crowley SJ, Morgan MK, Teodori M, Knutson KL. The relationship between breakfast skipping, chronotype, and glycemic control in type 2 diabetes. Chronobiol Int 2014;31:64–71. [DOI] [PubMed] [Google Scholar]
- 19.Breslow RA, Chen CM, Graubard BI, Jacobovits T, Kant AK. Diets of drinkers on drinking and nondrinking days: NHANES 2003-2008. Am J Clin Nutr 2013;97:1068–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data [Internet]. Hyattsville (MD): US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005–2006, 2007–2008, 2009–2010 [cited 2014 Jul 21]. Available from: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 21.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire and Examination protocol [Internet]. Hyattsville (MD): US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005–2006, 2007–2008, 2009–2010 [cited 2014 Jul 21]. Available from: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 22.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey. Response rates and survey totals [Internet]. Hyattsville (MD): US Department of Health and Human Services, Centers for Disease Control and Prevention; c2013 [cited 2014 Jul 21]. Available from: http://www.cdc.gov/nchs/nhanes/response_rates_cps.htm.
- 23.Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr 2006;136:2594–9. [DOI] [PubMed] [Google Scholar]
- 24.Kant AK, Graubard BI. Family income and education were related with 30-year time trends in dietary and meal behaviors of American children and adolescents. J Nutr 2013;143:690–700. Erratum in: J Nutr 2013;143:1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kant AK, Graubard BI. 40-Year Trends in Meal and Snack Eating Behaviors of American Adults. J Acad Nutr Diet. J Acad Nutr Diet 2015;115:50–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.United States Department of Agriculture, Agricultural Research Service. Food patterns equivalents database [Internet]. c2013 [cited 2014 Jul 14]. Available from: http://www.ars.usda.gov/Services/docs.htm?docid=23869.
- 27.Kant AK, Graubard BI. Secular trends in patterns of self-reported food consumption of adult Americans: NHANES 1971-1975 to NHANES 1999-2002. Am J Clin Nutr 2006;84:1215–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics 1999;55:652–9. [DOI] [PubMed] [Google Scholar]
- 29. RTI International. SUDAAN. Version 11.0. Research Triangle Park (NC): RTI International. 2012.
- 30.Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LRl. National health and nutrition examination survey: Analytic guidelines, 1999–2010. National Center for Health Statistics. Vital Health Stat 2(161). 2013. [PubMed]
- 31.Korn EL, Graubard BI. Analysis of health surveys. New York: John Wiley and Sons; 1999. [Google Scholar]
- 32.Scheer FA, Morris CJ, Shea SA. The internal circadian clock increases hunger and appetite in the evening independent of food intake and other behaviors. Obesity (Silver Spring) 2013;21:421–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boseck JJ, Engel SG, Allison KC, Crosby RD, Mitchell JE, deZwaan M. The application ofeco- logical momentary assessment to thes tudy of nighteating. Int J Eat Disord 2007;40:271–6. [DOI] [PubMed] [Google Scholar]
- 34.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88:324–32. [DOI] [PubMed] [Google Scholar]
- 35.Thompson FE, Subar AF. Dietary assessment methodology. In: Coulston AM, Boushey CJ, editors. Nutrition in the Prevention and Treatment of Disease (2). San Diego (CA): Academic Press; 2008.
- 36.Byers T. On the hazards of seeing the world through intervention-colored glasses. Am J Clin Nutr 2003;78:904–5. [DOI] [PubMed] [Google Scholar]
- 37.Harnack L, Himes JH, Anliker J, Clay T, Gittelsohn J, Jobe JB, Ring K, Snyder P, Thompson J, Weber JL. Intervention-related bias in reporting of food intake by fifth-grade children participating in an obesity prevention study. Am J Epidemiol 2004;160:1117–21. [DOI] [PubMed] [Google Scholar]
- 38.Natarajan L, Pu M, Fan J, Levine RA, Patterson RE, Thomson CA, Rock CL, Pierce JP. Measurement error of dietary self-report in intervention trials. Am J Epidemiol 2010;172:819–27. [DOI] [PMC free article] [PubMed] [Google Scholar]