Abstract
Study Objectives:
To estimate the health utility score and quality-adjusted life-years (QALY) index of obstructive sleep apnea syndrome (OSAS) in patients over 1 y of continuous positive airway pressure (CPAP) treatment.
Design:
Longitudinal interventional study.
Setting:
The study was carried out in Sao Paulo Sleep Institute, Brazil.
Patients and participants:
Ninety-five patients with OSAS and with apnea-hypopnea index (AHI) > 20 of either sex, body mass index < 40 kg/m2, and no previous contact with CPAP were included.
Interventions:
The participants underwent baseline and titration polysomnographies, clinical evaluation, and ambulatory blood pressure (BP) measurement, completed Short-Form 6 Dimension Health Survey (SF-6D) and Epworth Sleepiness Scale (ESS) questionnaires, and implementation of CPAP. The patients were followed for 1 y.
Measurements and Results:
The mean AHI and age were 57.6 ± 29.2 events/h and 53.3 ± 9.3 y, respectively. One year of CPAP treatment increased the health utility score from 0.611 ± 0.112 to 0.710 ± 0.121 (P < 0.01). Therefore, CPAP resulted in a mean gain of 0.092 QALY/patient. The improvements in utility scores were associated with decreases in the ESS after 1 mo, in systolic BP after 1 y, and in diastolic BP at 6 mo. BP normalization group (≤ 130/85 mmHg) showed higher QALY than that of the non-normalization group (0.10 ± 0.09 versus 0.05 ± 0.10; P = 0.03). One-year ESS score (P = 0.03), diastolic BP reduction P = 0.01) and baseline utility scores (P < 0.01) were significantly associated with QALY gain.
Conclusion:
This study showed a significant quality-adjusted life-years (QALY)/patient gain after 1 y of regular CPAP use. In addition, blood pressure normalization was associated with higher QALY gain. Thus, utility studies can provide more complete analyses of the total benefits of CPAP treatment in patients with obstructive sleep apnea syndrome and should be encouraged.
Citation:
Rizzi CF, Ferraz MB, Poyares D, Tufik S. Quality-adjusted life-years gain and health status in patients with OSAS after one year of continuous positive airway pressure use. SLEEP 2014;37(12):1963-1968.
Keywords: CPAP, obstructive sleep apnea (OSA), quality-adjusted life-years (QALY), utility
INTRODUCTION
Obstructive sleep apnea syndrome (OSAS) is an important health issue and is associated with comorbidities such as cardiovascular disease,1 traffic accidents,2 depression,3 and worsening of quality of life (QOL).4,5 The long-term treatment with continuous positive airway pressure (CPAP), especially in patients with severe disease and symptomatic patients, brought the possibility of improvements in both health and psychosocial status.1,6,7 Nevertheless, literature reporting the outcomes of CPAP treatment for OSAS in terms of quality-adjusted life-years (QALY) and health utility scores is scant.
Researchers have shown that patients with OSAS use high amounts of health care resources.8,9 Therefore, authorities encourage the execution of economic studies to establish the usefulness of OSAS treatment.9 Over the past decades, the measurement of utility has been used to obtain the weight of QOL for many diseases. Utility is a parameter that was developed by economists, and it refers to the subjective satisfaction that people derive from consuming goods and services. This parameter is used to refer to the subjective status of well-being in different states of health.10 The QALY combines both the increase in life expectancy and the improvement in health status.11 Both instruments (utility and QALY) allow the assessment of health-related QOL, supporting cost-effectiveness and cost-utility studies.
Some studies have demonstrated that CPAP is cost-effective,12,13 from the third-payer or societal perspectives in the USA12 and Canada.13 In another study from Spain, CPAP represented an incremental cost < 6.000 euros/QALY, which in a disaggregated analysis, 84% of the incremental effectiveness was attributed to the improved quality of life.14
Our hypothesis is that CPAP treatment is associated with health and QOL improvements that can be measured as utility and QALY gains. In addition, we believe that the use of utility measurement is a useful tool to assess gains after CPAP therapy. Therefore, the aims of this study are to estimate the health utility score associated with 1 y of CPAP treatment and to introduce the concept and method of the utility measurement to the sleep medicine field.
METHODS
Study Population
One hundred one consecutive patients with moderate to severe OSAS were recruited from the Sleep Clinic of Sao Paulo, Brazil. They were all administered CPAP, regardless of clinical symptoms. The inclusion criteria were both sexes, age between 30 and 65 y, and apnea-hypopnea index (AHI) > 20 events/h with comorbidities corrected with CPAP. We excluded individuals who were pregnant, had a body mass index > 40 kg/m2, those with a diagnosis of pulmonary or neuromuscular diseases, and those who had previous contact with CPAP. The study was approved by the Universidade Federal de Sao Paulo's Ethics Committee (number 0895/10) and registered at clinicaltrials.gov under number NCT01590420. All of the subjects signed an informed consent form.
Study Design
This was a longitudinal study in which a sample of 101 patients with OSAS was evaluated and 95 completed the protocol. Two patients dropped out within the first week and four patients at the first month. The initial evaluation was composed of baseline and titration polysomnography (PSG), clinical assessment, Epworth Sleepiness Scale (ESS), and noninvasive blood pressure (BP) assessment using the auscultatory method15; the QOL questionnaire was also used to evaluate the utility. The clinical assessment included general health information (such as associated diseases, medications usage, and pain prevalence), education, work status, and medical intercurrences. CPAP was prescribed by the sleep specialist and administered to all patients whose AHI was higher than 20 events/h of sleep, by a trained respiratory therapist.
Subsequently, clinical evaluation and CPAP compliance were checked at the first, sixth, and 12th mo of treatment. Noninvasive BP was checked at baseline (B), 6 mo (6M) and 1 y (1Y) after the initiation of CPAP. In addition, CPAP usage was also checked monthly by telephone contact with all patients. Compliance was considered a minimal usage of 4 h per night for at least 70% of the period, as determined by the card reader.
Polysomnography
Polysomnography (PSG) was conducted in all of the patients using the EMBLA® system (17 channels, Medicare Medical Devices Natus Neurology, Ontario, Canada). The following variables were monitored: electroencephalogram (four channels), electrooculogram (two channels), electromyogram (submentonian and anterior tibial muscles), electrocardiography (ECG, modified DII channel), snoring, and body position. Nasal flow was monitored using a pressure transducer, and respiratory effort was monitored using abdominal and thoracic sensors. Arterial oxygen saturation was recorded with a pulse oximeter (Ohmeda 3700, GE Healthcare, Finland). All of the PSGs were scored following the guidelines of the American Academy of Sleep Medicine for sleep studies.16
A second full PSG recording was performed for CPAP titration purposes. The CPAP titration PSG was considered satisfactory if the respiratory disturbance index (apnea, hypopneas and flow limitation events) was ≤ 5 events/h of sleep.17
Short-Form 6 Dimension
The Short-Form 6 Dimension (SF-6D) was constructed with questions from the Short-Form 36 (SF-36) questionnaire and measured by the standard gamble and visual analogue scale. The SF-36 questionnaire was reduced by combining two domains (physical role and emotional role).11 The final questionnaire involved a six-dimension descriptive system, each with multiple answers: (1) physical functioning, (2) role limitation, (3) social functioning, (4) pain, (5) mental health, and (6) vitality. The classification system consists of four to six levels on each of the six attributes, giving a total of 18,000 health states.18 The SF-6D was translated to Brazilian Portuguese and culturally adapted,19 and preference weights and algorithm for the calculation of utility scores were analyzed using the value set for the Brazilian population.20 The questionnaire was conducted in all patients by a trained and experienced interviewer, who was blinded to all CPAP evaluation.
The utility score was measured by the SF-6D. A utility is a metric used in health economic evaluations to capture QOL and is used as a basis of cost-utility analysis, one of the most common type of health economic evaluation used in health technology assessment.18 This instrument captures health benefits alongside broader benefits, which are not solely health-related, and can facilitate economic evaluations. The score of the utility measurement ranges from 0 to 1.0, in which 1.0 indicates full health and 0 is regarded as equivalent to death.21
The QALY was derived from the health state utility scale. It uses QALY to measure health outcomes by combining survival and health-related QOL into a single index.22 Thus, the gained QALY was calculated from the difference between the 1-y and baseline utilities, multiplied by 1 y. The advantage of using the QALY index is that it allows researchers to simultaneously capture gains with the reduction of morbidity (quality) and with the reduction of mortality (quantity), in a single score.19
Statistical Analysis
The subjects' characteristics are presented as the means and standard deviations. Shapiro-Wilk normality tests were performed for all variables. One-way analyses of variance (ANOVAs) were performed to evaluate differences between groups (i.e, compliant and noncompliant; hypertensive and nonhypertensive; BP normalization and non-BP normalization; diabetic and nondiabetic; sleepiness normalization and non-sleepiness normalization). Repeated-measures ANOVA and Bonferroni post hoc tests were used to evaluate the differences at all follow-up times and between subgroups. Two regression models were built in which QALY index was the dependent variable. In model 1, classic variables were considered, such as age, AHI, body mass index (BMI), and CPAP compliance as categorical variable. Model 2 included CPAP compliance as a continuous variable, along with baseline utility score, 1-y ESS score, 1 y minus baseline systolic and diastolic BP. P values of 0.05 or less were considered significant. The statistical analyses were performed using Statistic 9.0 software (Statsoft, Tulsa, OK, USA).
RESULTS
General Results
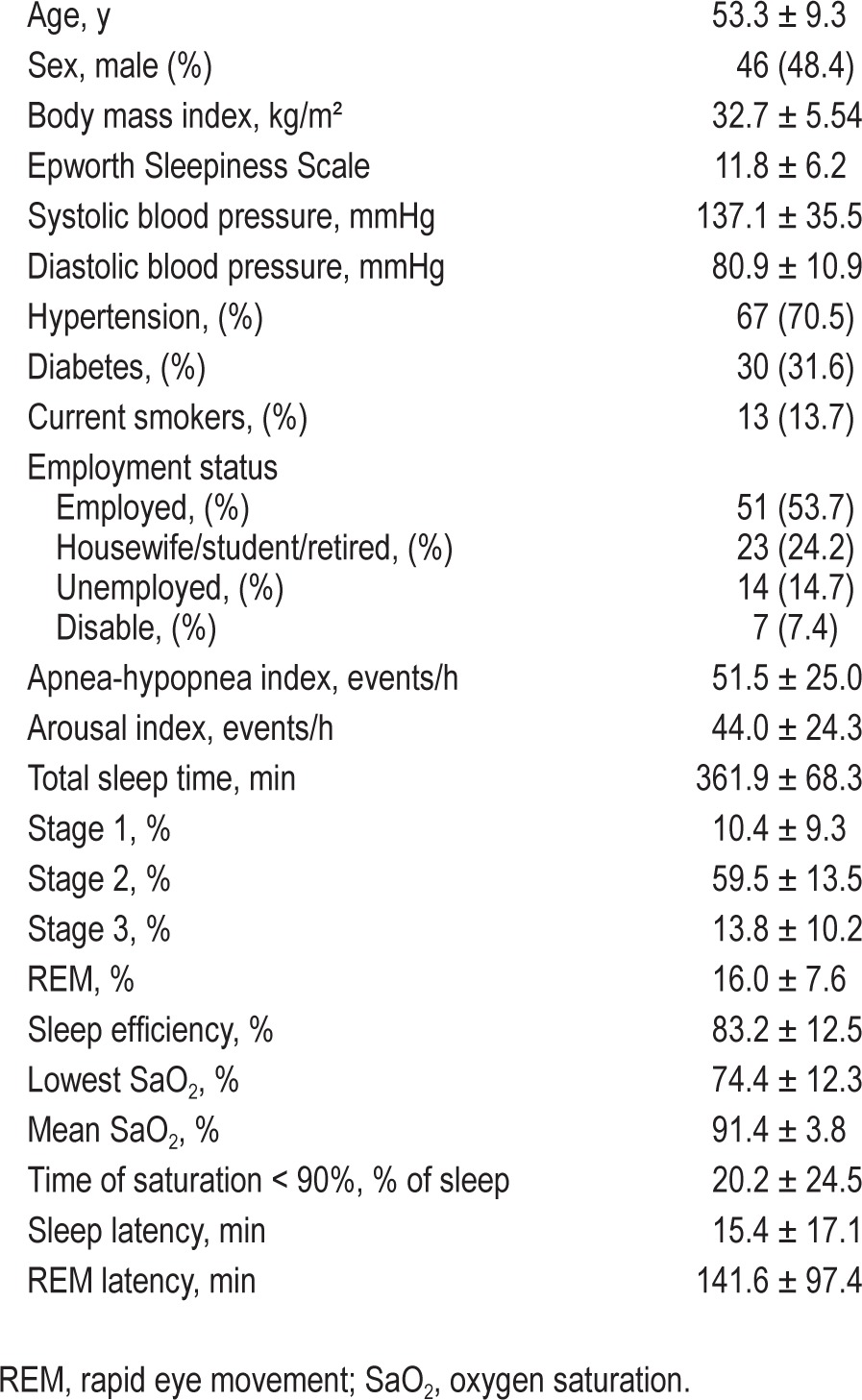
Ninety-five participants were included in the protocol between April 2010 and October 2011. The mean ages and AHI were 53.3 ± 9.3 y and 51.5 ± 25.0 events/h, respectively. Of the participants, 46 were male (48.4%). Sixty-one percent of patients were considered compliant to CPAP (mean usage of 5:18 ± 3:15 h); whereas 39% were not (mean usage of 3:59 ± 0:37), P < 0.01. The baseline characteristics of the population are presented in Table 1.
Table 1.
Baseline and polysomnography characteristics.
Utility and QALY Results
The SF-6D questionnaire showed that 1 y of CPAP treatment increased the health utility score from 0.611 ± 0.112 to 0.710 ± 0.121 (P < 0.01). Therefore, the treatment resulted in a mean net gain of 0.0929 QALY/patient. The gained QALY was accompanied by decreases in the ESS (from 11.8 ± 6.2 to 6.7 ± 4.8; P < 0.001), in systolic BP after 1 y (B: 138.6 ± 36.9, 6M: 130.9 ± 14.9, 1Y: 129.8 ± 13.6 mmHg; P = 0.02), and in diastolic BP after 6 mo (B: 81.7 ± 10.2, 6M: 77.1 ± 11.6, 1Y: 75.3 ± 9.7 mmHg; P < 0.001). The utility values and clinical outcomes are presented in Figure 1.
Figure 1.
Utility score and clinical outcomes after 1 y of CPAP. Repeated measures analysis of variance, P ≤ 0.05. (A) utility score, (B) Epworth Sleepiness Scale score, (C) systolic blood pressure, (D) diastolic blood pressure. * Differ from baseline.
There were no differences in utility scores between all subgroups (Table 2). The QALY were similar between compliant and noncompliant (0.08 ± 0.16 versus 0.09 ± 0.15, respectively; P = 0.8), hypertensive and nonhypertensive (0.07 ± 0.10 versus 0.11 ± 0.12, respectively; P = 0.1), diabetic and nondiabetic (0.07 ± 0.08 versus 0.09 ± 0.12, respectively; P = 0.4), and sleepiness normalization and nonsleepiness normalization (0.10 ± 0.16 versus 0.07 ± 0.16; P = 0.4). Nevertheless, BP normalization subgroup (≤ 130/85 mmHg) presented higher QALY/patient than nonnormalization group (0.10 ± 0.09 versus 0.05 ± 0.10; P = 0.03) (Figure 2).
Table 2.
Utility scores for subgroups.
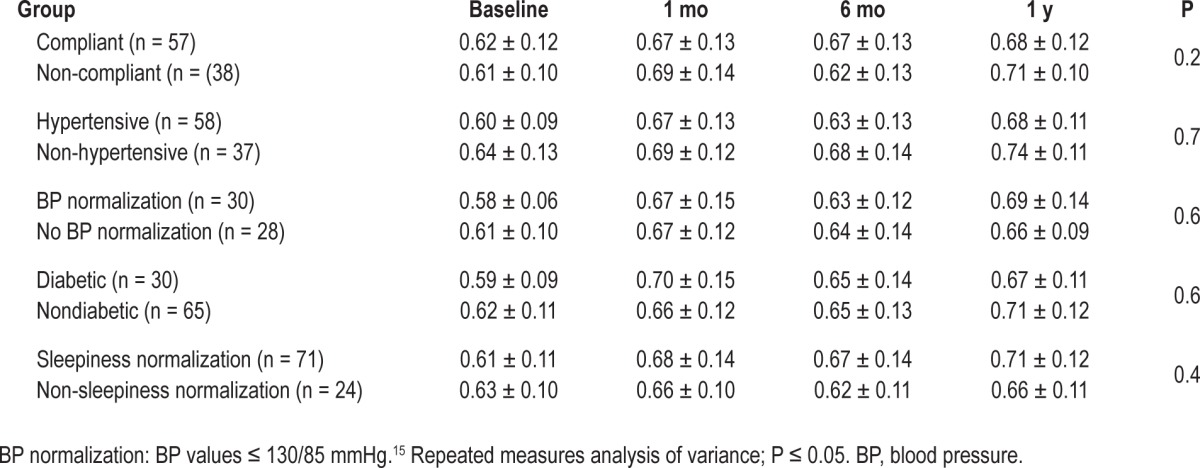
Figure 2.
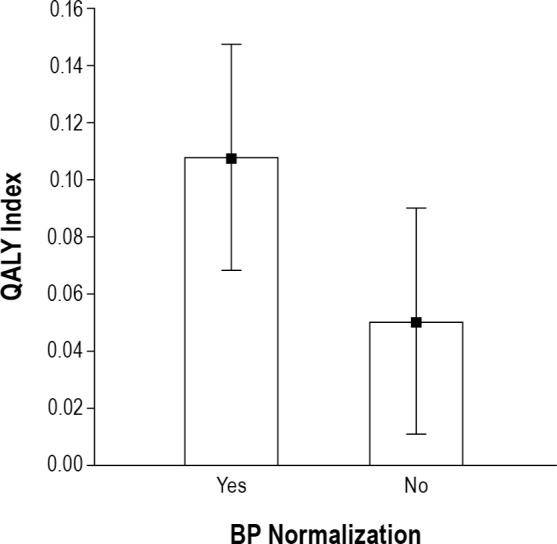
Quality-adjusted life-years (QALY) index and blood pressure (BP) normalization. One-way analysis of variance, P ≤ 0.05. Black squares represent the mean, whiskers represent 95% confidence intervals.
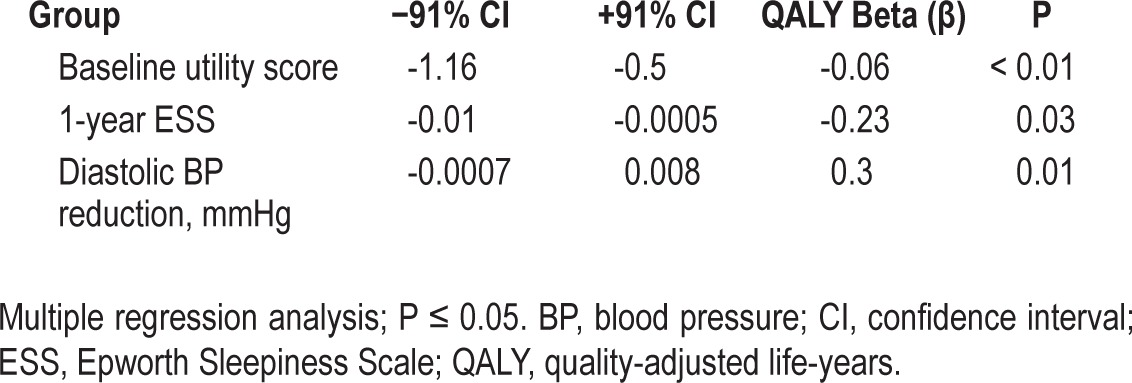
Regression Results
Age, AHI, BMI, and CPAP compliance did not show significant association with QALY index in our population of patients with OSA (P > 0.05, all) (Table 3). However, 1-y ESS score (P = 0.03), diastolic BP reduction (P = 0.01) and baseline utility scores (P < 0.01) were significantly associated with QALY gain (Table 4).
Table 3.
Multiple regression model, dependent variable: QALY index - Model 1
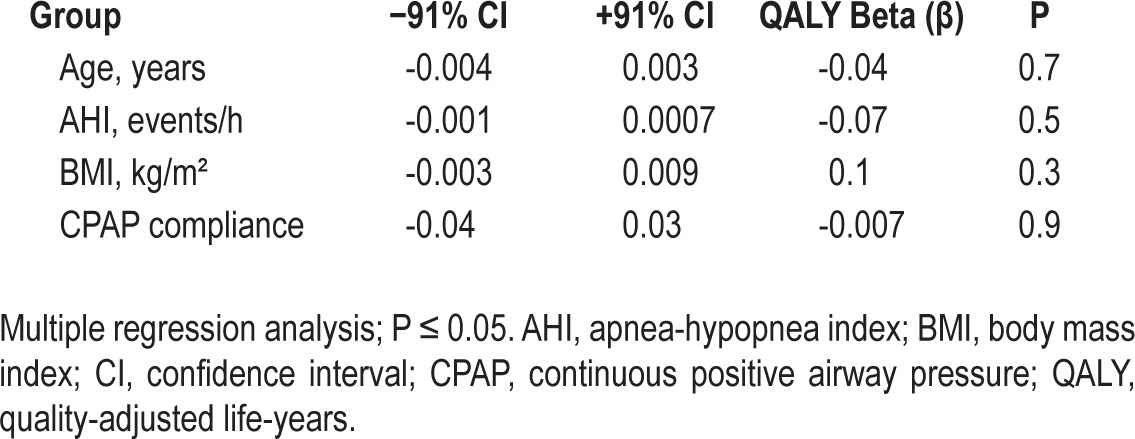
Table 4.
Multiple regression model, dependent variable: QALY index - Model 2
DISCUSSION
To our knowledge, this is the first longitudinal study to evaluate the utility score and QALY after treatment with CPAP in patients with OSAS. Our analysis revealed that the gain in utility scores occurs within 1 mo of therapy and remains throughout the first year with close assistance by the staff. Moreover, in those patients whose BP achieved values below 130/85 mmHg, QALY values after 1 y of CPAP was higher. Our study differs from previous ones because they were retrospective and used an analytical model to measure this relationship.12–14,23,24 One previous study compared various instruments to obtain the utility indices. The authors found that SF-6D utility index and Euro-thermometer visual analog scale seemed better suited to reflect the disease state of patients with OSA, and to track treatment-induced changes.23 For instance, previous studies used probability analysis and decision trees, based on projecting results. Tan et al.13 used a Markov decision analytical model to evaluate the utility values in a 5-y time horizon for a specific population of drivers. Similarly, Ayas NT et al.12 used a decision model and utility values from published studies to analyze the costs and QOL improvements with CPAP therapy, accounting for the gains from reduced vehicle accidents. The Markov model and decision tree model was also used in previous studies from Spain14 and USA,24 taking into account utility values from evidences already published to construct their economic evaluations. We followed and evaluated all patients for 1 y to accurately analyze health improvements data, compliance, and utility values.
Economic studies have found that nontreated patients with OSAS consume significantly more health resources and present with decreased work performance,8,25,26 which creates deficits that extend beyond health resources, affecting other areas of economic functioning. CPAP treatment has the potential to decrease these costs and the direct costs with health; however, previous studies have not quantified the gain in QALY associated with health benefits. Our data demonstrated that 1 y of CPAP was effective in significantly reducing blood pressure levels and diurnal excessive sleepiness. In addition, CPAP resulted in a mean gain of 0.0929 QALY/patient in an OSAS population with other comorbidities such as hypertension and diabetes. A common problem found in the literature is the lack of consensus of what is the ideal CPAP compliance. It may depend on the outcome evaluated. CPAP usage higher than 4 h for at least 70% of time would be associated with better cardiovascular outcome.27 However, for improving sleepiness higher compliance has been suggested.28 We used the former compliance criteria, and found that CPAP benefits both groups, compliant and less compliant. A potential explanation is that a mean usage of 3.59 h in the less compliant group might have been sufficient to improve QALY. It may suggest that different compliance criteria might be required for achieving different outcomes.
Utility assessment has been used for chronic diseases with public health relevance. In recurrent major depressive disorder, 2 y of venlafaxine was associated with a QALY of 0.055.29 In 151 diabetic subjects with moderate to high risk of cardiovascular disease, a 3-y program of lifestyle modifications composed of physical activity plus dietary changes resulted in a gain of 0.07 QALY, when it was measured using the SF-6D.30 In addition, in patients with primary insomnia, eszopiclone compared to placebo led to a QALY of 0.006831 after 6 mo of follow-up.31 Data from other diseases, such as from patients with chronic obstructive pulmonary disease, showed that treatment with indacaterol32 and tiotropium33 resulted in QALY gains values of 0.0026/y and 0.012/y, respectively. Furthermore, smoking cessation was associated with a QALY increase of 0.009.34
However, it appears that the treatment of hypertension brings better results in the utility gained. In hypertensive and smoker subjects, the treatment was associated with a QALY of 0.54/patient in opposition to a gain of 0.5/patient in those who did not receive any treatment for hypertension.35 Our study showed similar results. In those patients in whom BP normalized, QALY/patient value was higher than in those whose BP did not normalize. Indeed, we found that diastolic BP reduction was significantly associated with 1-y QALY gain. This finding suggests that BP reduction, or at least diastolic BP reduction, may be an important CPAP treatment outcome. Diastolic BP reduction has already been reported in previous studies after CPAP treatment.36 ESS score after 1 y of CPAP treatment was also significantly associated with QALY gain. Excessive daytime sleepiness is usually the most commonly reported variable showing improvement after CPAP treatment in patients with OSA.28 Our study reinforced the concept that sleepiness is also an important clinical outcome to be monitored in CPAP-treated patients. Probably, QALY index is significantly associated with improvements in health (such as decreases in BP and sleepiness) in a sample from a patient with OSA.
In our study, long-term CPAP treatment resulted in a QALY similar to other chronic disorders, such as depression, diabetes, and insomnia. Nevertheless, one factor that may have negatively affected the utility score in our study was the high prevalence of pain complaints in our population (82%) that may have impaired daily activities. Nevertheless, pain complaints were reported both at baseline and during the follow-up time. Perhaps pain is a comorbid unrelated health problem that should be taken into account in future studies. The lack of a control group of untreated patients with OSA and the absence of measuring the utility score 1 y prior to the initiation of CPAP are potential limitations of this study.
The SF-6D questionnaire is an easy and accessible tool that allows for the evaluation of the long-term effectiveness of CPAP, and the current analysis showed improvements in health status with the CPAP for OSAS. CPAP effectiveness evaluated by utility and the QALY index provides a measure that can be universally useful, even for different economies and countries.
Potential limitations of this study are the single-center data collection, and the relatively small number of patients.
In conclusion, this longitudinal study showed a significant QALY/patient gain after 1 y of regular CPAP use, and higher QALY index in those patients whose BP normalized. Consequently, utility scores can provide more complete analyses of the total benefits of CPAP treatment in patients with OSAS. Utility and economic studies should be encouraged to support decision making in the health care system.
DISCLOSURE STATEMENT
This was not an industry supported study. This study was supported by Fundacao Fundo de Amparo a Pesquisa do Estado de Sao Paulo (FAPESP) e Associacao Fundo de Incentivo a Pesquisa (AFIP). Dr. Poyares and Dr. Tufik are recipients of CNPQ grants, Brazil. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Author contributions: Dr. Rizzi was responsible for study design, acquisition of data, analysis and interpretation of data, and writing the manuscript. Dr. Ferraz was responsible for study design, analysis and interpretation of data, and writing the manuscript. Dr. Poyares was responsible for study design, interpretation of data, and writing the manuscript. Dr. Tufik was responsible for study design and interpretation of data.
Footnotes
A commentary on this article appears in this issue on page 1885.
REFERENCES
- 1.Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52:686–717. doi: 10.1016/j.jacc.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Ellen RL, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M. Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med. 2006;2:193–200. [PubMed] [Google Scholar]
- 3.Aloia MS, Arnedt JT, Smith L, Skrekas J, Stanchina M, Millman RP. Examining the construct of depression in obstructive sleep apnea syndrome. Sleep Med. 2005;6:115–21. doi: 10.1016/j.sleep.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Bano K, Kryger MH. Sleep apnea: clinical investigations in humans. Sleep Med. 2007;8:400–26. doi: 10.1016/j.sleep.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Chervin RD. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest. 2000;118:372–9. doi: 10.1378/chest.118.2.372. [DOI] [PubMed] [Google Scholar]
- 6.Siccoli MM, Pepperell JC, Kohler M, Craig SE, Davies RJ, Stradling JR. Effects of continuous positive airway pressure on quality of life in patients with moderate to severe obstructive sleep apnea: data from a randomized controlled trial. Sleep. 2008;31:1551–8. doi: 10.1093/sleep/31.11.1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sánchez AI, Martínez P, Miró E, Bardwell WA, Buela-Casal G. CPAP and behavioral therapies in patients with obstructive sleep apnea: effects on daytime sleepiness, mood, and cognitive function. Sleep Med Rev. 2009;13:223–33. doi: 10.1016/j.smrv.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Albarrak M, Banno K, Sabbagh AA, et al. Utilization of healthcare resources in obstructive sleep apnea syndrome: a 5-year follow-up study in men using CPAP. Sleep. 2005;28:1306–11. doi: 10.1093/sleep/28.10.1306. [DOI] [PubMed] [Google Scholar]
- 9.Leger D, Bayon V, Laaban JP, Philip P. Impact of sleep apnea on economics. Sleep Med Rev. 2012;16:455–62. doi: 10.1016/j.smrv.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Robinson R. Economic evaluation and health care. What does it mean? BMJ. 1993;307:670–3. doi: 10.1136/bmj.307.6905.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brazier J, Usherwood T, Harper R, Thomas K. Deriving a preference-based single index from the UK SF-36 Health Survey. J Clin Epidemiol. 1998;51:1115–28. doi: 10.1016/s0895-4356(98)00103-6. [DOI] [PubMed] [Google Scholar]
- 12.Ayas NT, FitzGerald JM, Fleetham JA, et al. Cost-effectiveness of continuous positive airway pressure therapy for moderate to severe obstructive sleep apnea/hypopnea. Arch Intern Med. 2006;166:977–84. doi: 10.1001/archinte.166.9.977. [DOI] [PubMed] [Google Scholar]
- 13.Tan MC, Ayas NT, Mulgrew A, et al. Cost-effectiveness of continuous positive airway pressure therapy in patients with obstructive sleep apneahypopnea in British Columbia. Can Respir J. 2008;15:159–65. doi: 10.1155/2008/719231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mar J, Rueda JR, Durán-Cantolla J, Schechter C, Chilcott J. The cost-effectiveness of nCPAP treatment in patients with moderate-to-severe obstructive sleep apnoea. Eur Respir J. 2003;21:515–22. doi: 10.1183/09031936.03.00040903. [DOI] [PubMed] [Google Scholar]
- 15.Chobanian AV, Bakris GL, Black WR, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 16.Iber C, Ancoli-Israel S, Chesson A, Quan S for the American Academy of Sleep Medicine. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, 1st ed. [Google Scholar]
- 17.Kushida CA, Littner MR, Morgenthaler T, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28:499–521. doi: 10.1093/sleep/28.4.499. [DOI] [PubMed] [Google Scholar]
- 18.Obradovic M, Lal A, Liedgens H. Validity and responsiveness of EuroQol-5 dimension (EQ-5D) versus Short Form-6 dimension (SF-6D) questionnaire in chronic pain. Health Qual Life Outcomes. 2013;11:110. doi: 10.1186/1477-7525-11-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Campolina AG, Bortoluzzo AB, Ferraz MB, Ciconelli RM. Validation of the Brazilian version of the generic six-dimensional short form quality of life questionnaire (SF-6D Brazil) Cien Saude Colet. 2011;16:3103–10. doi: 10.1590/s1413-81232011000800010. [DOI] [PubMed] [Google Scholar]
- 20.Cruz LN, Camey SA, Hoffmann JF, et al. Estimating the SF-6D value set for a population-based sample of Brazilians. Value Health. 2011;14:S108–14. doi: 10.1016/j.jval.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21:271–92. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- 22.Teckle P, McTaggart-Cowan H, Van der Hoek K, et al. Mapping the FACT-G cancer-specific quality of life instrument to the EQ-5D and SF-6D. Health Qual Life Outcomes. 2013;11:203. doi: 10.1186/1477-7525-11-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidlin M, Fritsch K, Matthews F, Thurnheer R, Senn O, Bloch KE. Utility indices in patients with the obstructive sleep apnea syndrome. Respiration. 2010;79:200–8. doi: 10.1159/000222094. [DOI] [PubMed] [Google Scholar]
- 24.Billings ME, Kapur VK. Medicare long-term CPAP coverage policy: a cost-utility analysis. J Clin Sleep Med. 2013;9:1023–9. doi: 10.5664/jcsm.3074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27:453–8. doi: 10.1093/sleep/27.3.453. [DOI] [PubMed] [Google Scholar]
- 26.Hoffman B, Wingenbach DD, Kagey AN, Schaneman JL, Kasper D. The long-term health plan and disability cost benefit of obstructive sleep apnea treatment in a commercial motor vehicle driver population. J Occup Environ Med. 2010;52:473–7. doi: 10.1097/JOM.0b013e3181dbc8ab. [DOI] [PubMed] [Google Scholar]
- 27.Montesi SB, Edwards BA, Malhotra A, Bakker JP. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med. 2012;8:587–96. doi: 10.5664/jcsm.2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weaver TE, Maislin G, Dinges DF, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30:711–9. doi: 10.1093/sleep/30.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sobocki P, Ekman M, Ovanfors A, Khandker R, Jönsson B. The cost-utility of maintenance treatment with venlafaxine in patients with recurrent major depressive disorder. Int J Clin Pract. 2008;62:623–32. doi: 10.1111/j.1742-1241.2008.01711.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eriksson MK, Hagberg L, Lindholm L, Malmgren-Olsson EB, Osterlind J, Eliasson M. Quality of life and cost-effectiveness of a 3-year trial of lifestyle intervention in primary health care. Arch Intern Med. 2010;170:1470–9. doi: 10.1001/archinternmed.2010.301. [DOI] [PubMed] [Google Scholar]
- 31.Botteman MF, Ozminkowski RJ, Wang S, Pashos CL, Schaefer K, Foley DJ. Cost effectiveness of long-term treatment with eszoplicone for primary insomnia: a decision analytical model. CNS Drugs. 2007;21:319–34. doi: 10.2165/00023210-200721040-00005. [DOI] [PubMed] [Google Scholar]
- 32.Price D, Asukai Y, Ananthapavan J, Malcolm B, Radwan A, Keyzor I. A UK-based cost-utility analysis of indacaterol, a once-daily maintenance bronchodilator for patients with COPD, using real world evidence on resource use. Appl Health Econ Health Policy. 2013;11:259–74. doi: 10.1007/s40258-013-0021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hettle R, Wouters H, Ayres J, et al. Cost-utility analysis of tiotropium versus usual care in patients with COPD in the UK and Belgium. Respir Med. 2012;106:1722–33. doi: 10.1016/j.rmed.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 34.Menn P, Leidl R, Holle R. A lifetime Markov model for the economic evaluation of chronic obstructive pulmonary disease. Pharmacoeconomics. 2012;30:825–40. doi: 10.2165/11591340-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 35.Athanasakis K, Souliotis K, Tountas Y, Kyriopoulos J, Hatzakis A. A cost-utility analysis of hypertension treatment in Greece: assessing the impact of age, sex, smoking status, on outcomes. J Hypertens. 2012;30:227–34. doi: 10.1097/HJH.0b013e32834d9f18. [DOI] [PubMed] [Google Scholar]
- 36.Barbé F, Durán-Cantolla J, Capote F, et al. Long-term effect of continuous positive airway pressure in hypertensive patients with sleep apnea. Am J Respir Crit Care Med. 2010;181:718–26. doi: 10.1164/rccm.200901-0050OC. [DOI] [PubMed] [Google Scholar]



