Abstract
Background
The cause of death in patients with chronic kidney disease (CKD) varies with CKD severity, but variation has not been quantified.
Study Design
Retrospective analysis of prospective randomized clinical trial.
Setting & Participants
We analyzed 4,038 individuals with anemia and diabetic CKD from TREAT, a randomized trial comparing darbepoetin alfa and placebo.
Predictors
Baseline estimated glomerular filtration rate (eGFR) and protein-creatinine ratio (PCR).
Outcomes
Cause of death as adjudicated by a blinded committee.
Results
Median eGFR and PCR ranged from 20.6 mL/min/1.73 m2 and 4.1 g/g in quartile 1 (Q1) to 47.0 mL/min/1.73 m2 and 0.1 g/g in Q4 (P < 0.01). Of 806 deaths, 441, 298, and 67 were due to cardiovascular (CV), non-CV, and unknown causes, respectively. Cumulative CV mortality at 3 years was higher with lower eGFR (Q1, 15.5%; Q2, 11.1%; Q3, 11.2%; Q4, 10.3%; P < 0.001) or higher PCR (Q1, 15.2%; Q2, 12.3%; Q3, 11.7%; Q4, 9.0%; P < 0.001). Similarly, non-CV mortality was higher with lower eGFR (Q1, 12.7%; Q2, 8.4%; Q3, 6.7%; Q4, 6.1%; P < 0.001) or higher PCR (Q1, 10.3%; Q2, 7.9%; Q3, 9.4%; Q4, 6.4%; P < 0.01). Sudden death was 1.7-fold higher with lower eGFR (P < 0.04) and 2.1-fold higher with higher PCR (P < 0.001). Infection-related mortality was 3.3-fold higher in the lowest eGFR quartile (P < 0.001) and 2.8-fold higher in the highest PCR quartile (P < 0.02). The overall proportion of CV and non-CV deaths was not significantly different across eGFR or PCR quartiles.
Limitations
Results may not be generalizable to nondiabetic CKD or diabetic CKD in the absence of anemia. Measured GFR was not available.
Conclusions
In diabetic CKD, both lower baseline GFR and higher PCR are associated with higher CV and non-CV mortality rates, particularly from sudden death and infection. Efforts to improve outcomes should focus on CV disease and early diagnosis and treatment of infection.
Keywords: Chronic kidney disease (CKD), mortality, cardiovascular (CV) disease, estimated glomerular filtration rate (eGFR), renal function, protein-creatinine ratio (PCR), proteinuria, sudden death, infection, diabetic CKD, anemia, Trial to Reduce Cardiovascular Events With Aranesp Therapy (TREAT).
Chronic kidney disease (CKD) is associated with a high incidence of cardiovascular (CV) mortality and morbidity,1-3 and strong associations between kidney function and all-cause mortality have been widely reported.3-6 Although several studies have analyzed associations of kidney function with overall rates of CV and non-CV mortality or between estimated glomerular filtration rate (eGFR) and specific types of mortality,7-9 information on the variation in cause-specific mortality with eGFR is sparse. Moreover, there are few data relating the severity of proteinuria, another marker of CKD severity, with cause of death. As a result, the relative contributions of specific causes of CV and non-CV mortality to the high overall mortality in CKD remain uncertain.
Better knowledge of how causes of death change as CKD advances may help tailor treatment approaches to CKD. We hypothesized that the incidence rate of CV mortality would increase at lower eGFRs and higher baseline proteinuria and that the proportion of deaths due to CV causes, particularly those from sudden death, stroke, and myocardial infarction (MI), would increase with increasing CKD severity. To test our hypothesis and better understand how specific causes of mortality differ with kidney function, we analyzed the relationship between eGFR, proteinuria, and the adjudicated cause of death in individuals with type 2 diabetes mellitus and CKD enrolled in the Trial to Reduce Cardiovascular Events With Aranesp Therapy (TREAT),10 a randomized trial in which treatment with darbepoetin had no significant effect on either all-cause or CV mortality compared to placebo therapy in patients with anemia, diabetes, and CKD.
METHODS
Trial Design and Cohort
We analyzed 4,038 individuals enrolled in TREAT (trial registration: www.ClinicalTrials.gov; study number: NCT00093015), a randomized controlled trial comparing darbepoetin alfa and placebo in patients with anemia, diabetes, and CKD. The design and main outcomes of this trial have been reported previously.10 Enrollment required type 2 diabetes, eGFR of 20 to 60 mL/min/1.73 m2 according to the 4-variable MDRD (Modification of Diet in Renal Disease) Study equation,11 hemoglobin level ≤ 11.0 g/dL, and transferrin saturation ≥ 15%.
GFR and Proteinuria
eGFR was calculated from the baseline serum creatinine level using the 2009 CKD-EPI (CKD Epidemiology Collaboration) creatinine equation, a more accurate formula than the 4-variable MDRD Study equation.12 Although trial entry criteria resulted in most individuals having CKD stages 3 to 4,13 a minority had CKD stage 2 or 5. In order to efficiently include the entire cohort, our primary analysis divided eGFR into quartiles. Secondary analyses examined eGFRMDRD, with individuals classified as having CKD stages 4 to 5 (eGFR <, 30 mL/ min/1.73 m2), 3b (eGFR of 30-<45 mL/min/1.73 m2), and 2 to 3a (eGFR of 45-<90 mL/min/1.73 m2). In addition, we also analyzed causes of death according to whether end-stage renal disease (ESRD) was present at the time of death. Protein excretion was measured as the ratio of urinary protein to urinary creatinine concentrations (in grams per gram) and analyzed in quartiles.
Assessment of Cause of Death
A clinical end points committee blinded to both treatment arm and hemoglobin levels centrally adjudicated deaths. CV causes of death were subclassified as MI, pump failure, sudden death, presumed sudden death, presumed CV death, fatal stroke, CV procedural (related to surgical or percutaneous cardiac procedures), pulmonary embolism, other CV causes, or unknown. Non-CV causes of death were subclassified as pulmonary, malignant, infectious, hepatobiliary, gastrointestinal, renal, non-CV procedural, accidental, suicide, and other (Item S1, available as online supplementary material). Compared to placebo, darbepoetin had no effect on the risk of all-cause or CV mortality.10
Statistical Analysis
Baseline characteristics were stratified by CKD quartile, with differences across quartiles assessed by trend tests. Because mortality from any single cause precludes the possibility of death from all other causes, competing-risk methods were used to calculate the cumulative incidence of cause-specific mortality in our primary analysis and raw incidence rates were examined in sensitivity analyses. Trends in cumulative incidence rates across quartiles were assessed using competing-risk regression models according to the methods of Fine and Gray,14 and the observed cumulative incidence function at 3 years postrandomization is reported. Trends in the percentage of deaths attributable to specific causes across categories of GFR were tested using univariate logistic regression. For all trend tests, we assessed for a linear relationship between the 4-level quartile variable (coded 1/2/3/4) and outcome. Adjusted analyses were conducted using competing-risk survival models. Sensitivity analyses examining differences in incidence rates were analyzed using Poisson regression, whereas those incorporating time-updated estimates of kidney function according to the last available measurement were conducted using Cox proportional hazards regression models. All analyses were conducted using STATA, version 13 (StataCorp LP). P < 0.05 was considered to be significant.
RESULTS
Baseline Characteristics According to eGFR
eGFRs ranged from a median of 20.6 mL/min/1.73 m2 in quartile 1 (Q1) to 47.0 mL/min/1.73 m2 in Q4 (Table 1). Most individuals had eGFRs < 60 mL/min/1.73 m2 (Fig S1a). Sex and race were similarly distributed across quartiles of eGFR. Although age was significantly older in those with more severely reduced eGFR, differences were marginal. In contrast, those with lower eGFRs were characterized by significantly longer durations of diabetes and higher frequencies of retinopathy and insulin use. They were also significantly more likely to have baseline CV disease or heart failure. Low-density lipoprotein cholesterol and triglyceride levels were higher in individuals with lower eGFRs, whereas high-density lipoprotein cholesterol and albumin levels were lower. Median protein-creatinine ratio (PCR) was higher in individuals with lower eGFRs (Q1, 1.0 g/g; Q2, 0.5 g/g; Q3, 0.3 g/g; Q4, 0.2 g/g; P < 0.001). Prior intravenous iron and erythropoiesis-stimulating agent use were similarly distributed across categories of eGFR.
Table 1.
Baseline Characteristics According to Baseline eGFR
| Variable | Q1: 0.9-24.2 (n = 1,008) | Q2: 24.3-31.6 (n = 1,014) | Q3: 31.7-40.2 (n = 1,007) | Q4: 40.3-119.8 (n = 1,006) | P |
|---|---|---|---|---|---|
| eGFR (mL/min/1.73 m2) | 20.6 [18.4-22.5] | 27.9 [26.0-29.7] | 35.5 [33.6-37.8] | 47.0 [43.1-52.5] | — |
| Demographics | |||||
| Age (y) | 68 [60-75] | 68 [61-76] | 69 [61-76] | 67 [58-73] | <0.001 |
| Female sex | 554 (55) | 615 (61) | 586 (58) | 554 (55) | 0.8 |
| Race | 0.04 | ||||
| White | 625 (62) | 640 (63) | 672 (67) | 660 (63) | |
| African American | 218 (22) | 184 (18) | 185 (18) | 228 (23) | |
| Hispanic or Latino | 139 (14) | 153 (15) | 124 (12) | 122 (12) | |
| Other | 26 (3) | 37 (4) | 26 (3) | 26 (3) | |
| Physical examination | |||||
| Systolic BP (mm Hg) | 136 [124-150] | 138 [124-150] | 135 [121-148] | 135 [122-148] | 0.4 |
| Diastolic BP (mm Hg) | 70 [64-80] | 71 [64-80] | 70 [64-80] | 72 [66-80] | 0.1 |
| Body mass index (kg/m2) | 30.4 [26.4-35.2] | 30.2 [26.1-34.9] | 30.2 [26.3-35.4] | 30.4 [26.3-35.2] | 0.9 |
| Medical history | |||||
| Diabetes duration (y) | 16.4 [10.1-22.5] | 15.5 [8.7-21.6] | 15.0 [7.7-21.7] | 14.2 [7.5-21.4] | <0.001 |
| Retinopathy | 507 (51) | 491 (50) | 437 (45) | 426 (44) | <0.001 |
| Cardiovascular disease | 688 (68) | 668 (66) | 653 (65) | 631 (63) | 0.01 |
| Coronary disease | 449 (45) | 459 (45) | 465 (46) | 416 (41) | 0.2 |
| Heart failure | 371 (37) | 364 (36) | 313 (31) | 297 (30) | <0.001 |
| Myocardial infarction | 185 (18) | 186 (18) | 195 (19) | 174 (17) | 0.7 |
| Stroke | 111 (11) | 113 (11) | 112 (11) | 111 (11) | 0.9 |
| PVD | 224 (22) | 203 (20) | 217 (22) | 203 (20) | 0.4 |
| AICD | 10 (1) | 16 (2) | 18 (2) | 13 (1) | 0.5 |
| Atrial fibrillation | 114 (11) | 102 (10) | 116 (12) | 91 (9) | 0.2 |
| Current smoker | 67 (7) | 38 (4) | 52 (5) | 47 (5) | 0.1 |
| Medications | |||||
| Insulin | 519 (51) | 511 (50) | 491 (49) | 467 (46) | 0.02 |
| ACE inhibitor or ARB | 750 (74) | 820 (81) | 823 (82) | 829 (82) | <0.001 |
| β-Blocker | 507 (50) | 516 (51) | 501 (50) | 463 (46) | 0.05 |
| Aldosterone blocker | 56 (6) | 40 (4) | 59 (6) | 54 (5) | 0.7 |
| Statin | 573 (57) | 608 (60) | 610 (61) | 570 (57) | 0.9 |
| Oral antiplatelet agents | 494 (49) | 490 (48) | 487 (48) | 476 (47) | 0.5 |
| Vitamin K antagonist | 69 (7) | 71 (7) | 72 (7) | 64 (6) | 0.7 |
| Intravenous iron | 17 (2) | 14 (1) | 18 (2) | 13 (1) | 0.7 |
| Prior ESA use | 139 (14) | 109 (11) | 82 (8) | 55 (5) | <0.001 |
| Laboratory values | |||||
| Creatinine (mg/dL) | 2.7 [2.4-3.1] | 2.1 [1.8-2.3] | 1.7 [1.5-1.9] | 1.3 [1.2-1.5] | <0.001 |
| Urinary PCR (g/g) | 1.0 [0.2-3.1] | 0.5 [0.2-1.9] | 0.3 [0.1-1.1] | 0.2 [0.1-1.2] | <0.001 |
| CRP (mg/L) | 3.3 [3.0-7.2] | 3.0 [3.0-6.2] | 3.0 [3.0-6.3] | 3.0 [3.0-7.1] | 0.05 |
| Albumin (g/dL) | 3.9 [3.6-4.2] | 4.0 [3.7-4.3] | 4.0 [3.8-4.3] | 4.0 [3.8-4.3] | <0.001 |
| Hemoglobin A1c (%) | 6.9 [6.2-7.9] | 6.9 [6.2-7.9] | 7.0 [6.3-8.0] | 7.0 [6.3-8.1] | 0.2 |
| Hemoglobin (g/dL) | 10.2 [9.6-10.8] | 10.4 [9.7-10.9] | 10.5 [9.9-11.0] | 10.6 [10.1-11.0] | <0.001 |
| Serum ferritin (μg/L) | 158 [84-300] | 139 [74-263] | 120 [61-240] | 117 [55-228] | <0.001 |
| LDL cholesterol (mg/dL) | 87 [65-118] | 84 [63-111] | 85 [63-109] | 83 [63-109] | 0.02 |
| HDL cholesterol (mg/dL) | 45 [38-54] | 46 [38-55] | 46 [38-57] | 47 [39-58] | <0.001 |
| Triglycerides (mg/dL) | 163 [115-237] | 160 [112-237] | 156 [111-231] | 141 [103-210] | 0.001 |
Note: eGFR quartiles expressed in mL/min/1.73 m2. Values for categorical variables are given as number (percentage); values for continuous variables are given as median [interquartile range]. P values for categorical variables, using Mantel-Haenszel χ2; P values for continuous variables, using analysis of variance. Conversion factors for units: serum creatinine in mg/dL to μmol/L, ×88.4; urea nitrogen in mg/dL to mmol/L, ×0.357; cholesterol in mg/dL to mmol/L ×0.02586.
Abbreviations: ACE, angiotensin-converting enzyme; AICD, automated implantable cardiac defibrillator; ARB, angiotensin receptor blocker; BP, blood pressure; CRP, C-reactive protein; eGFR, estimated glomerular filtration rate; ESA, erythropoiesis-stimulating agent; HDL, high-density lipoprotein; LDL, low-density lipoprotein; PCR, protein-creatinine ratio; PVD, peripheral vascular disease; Q, quartile.
Baseline Characteristics According to Proteinuria
PCR ranged from a median of 4.08 g/g in Q1 to 0.09 g/g in Q4 (Table 2). In all, 50.4% of individuals had PCR ≤ 0.4 g/g, while 83% were <3.0 g/g (Fig S1b). Individuals with high PCRs were younger, less likely to be female, and more likely to be of nonwhite race and ethnicity (Table 2). Although duration of diabetes was longer in individuals with more severe proteinuria, fewer individuals with more severe proteinuria had established CV disease at baseline. Low and high-density lipoprotein cholesterol and triglyceride levels were all higher in individuals with higher PCRs, whereas albumin concentrations were lower. Last, median eGFR was lower in individuals with higher PCRs (for Q1, Q2, Q3, and Q4, values were 27.7, 30.2, 32.9, and 35.0 mL/min/1.73 m2, respectively; P < 0.001).
Table 2.
Baseline Characteristics According to Baseline PCR
| Variable | Q1: 1.85-44.58 g/g (n = 1,009) | Q2: 0.39-1.85 g/g (n = 1,009) | Q3: 0.13-0.39g/g (n = 1,009) | Q4: 0.003-0.13g/g (n = 1,009) | P |
|---|---|---|---|---|---|
| Urinary PCR (g/g) | 4.08 (2.76-6.61) | 0.85 (0.39-1.85) | 0.21 (0.56-1.24) | 0.09 (0.07-0.11) | — |
| Demographics | |||||
| Age (y) | 62 [55-69] | 67 [59-74] | 71 [64-78] | 71 [64-77] | <0.001 |
| Female sex | 540 (54) | 539 (53) | 629 (62) | 603 (60) | <0.001 |
| Race | <0.001 | ||||
| White | 542 (54) | 630 (62) | 720 (71) | 676 (67) | |
| African American | 211 (21) | 194 (19) | 175 (17) | 235 (23) | |
| Hispanic or Latino | 222 (22) | 157 (16) | 86 (9) | 73 (7) | |
| Other | 34 (3) | 28 (3) | 28 (3) | 25 (2) | |
| Physical examination | |||||
| Systolic BP (mm Hg) | 142 [130-159] | 138 [126-149] | 132 [120-142] | 130 [118-140] | <0.001 |
| Diastolic BP (mm Hg) | 80 [70-84] | 72 [66-80] | 70 [62-80] | 69 [60-75] | <0.001 |
| Body mass index (kg/m2) | 29.8 [26.0-35.0] | 29.7 [25.7-34.2] | 30.4 [26.1-35.5] | 31.2 [27.3-36.2] | <0.001 |
| Medical history | |||||
| Diabetes duration (y) | 16.2 [10.3-21.3] | 16.1 [10.1-23.1] | 14.9 [8.0-22.5] | 12.2 [6.0-20.6] | <0.001 |
| Retinopathy | 605 (61) | 555 (56) | 397 (40) | 305 (31) | <0.001 |
| Cardiovascular disease | 602 (60) | 662 (66) | 688 (68) | 689 (68) | <0.001 |
| Coronary disease | 364 (36) | 438 (43) | 491 (48) | 497 (49) | <0.001 |
| Heart failure | 315 (31) | 335 (33) | 362 (36) | 334 (33) | 0.2 |
| Myocardial infarction | 118 (12) | 187 (19) | 215 (21) | 220 (22) | <0.001 |
| Stroke | 94 (9) | 133 (13) | 112 (11) | 108 (11) | 0.6 |
| PVD | 169 (17) | 240 (24) | 217 (22) | 221 (22) | 0.02 |
| AICD | 5 (1) | 12 (1) | 14 (1) | 26 (3) | 0.001 |
| Atrial fibrillation | 52 (5) | 96 (10) | 155 (15) | 122 (12) | <0.001 |
| Current smoker | 71 (7) | 61 (6) | 42 (4) | 29 (3) | <0.001 |
| Medications | |||||
| Insulin | 600 (59) | 552 (55) | 448 (44) | 388 (38) | <0.001 |
| ACE inhibitor or ARB | 816 (81) | 767 (76) | 791 (78) | 848 (84) | 0.04 |
| β-Blocker | 492 (49) | 484 (48) | 490 (49) | 522 (52) | 0.2 |
| Aldosterone blocker | 30 (3) | 42 (4) | 54 (5) | 83 (8) | <0.001 |
| Statin | 531 (53) | 558 (55) | 601 (60) | 673 (67) | <0.001 |
| Oral antiplatelet agents | 438 (43) | 467 (46) | 510 (51) | 534 (53) | <0.001 |
| Vitamin K antagonist | 39 (4) | 56 (6) | 94 (9) | 88 (9) | <0.001 |
| Intravenous iron | 14 (1) | 21 (2) | 15 (1) | 12 (1) | 0.5 |
| Prior ESA use | 87 (9) | 104 (10) | 99 (10) | 95 (9) | 0.7 |
| Laboratory values | |||||
| Creatinine (mg/dL) | 2.2 [1.7-2.7] | 2.0 [1.6-2.5] | 1.7 [1.4-2.2] | 1.7 [1.4-2.1] | <0.001 |
| eGFR (mL/min/1.73 m2) | 27.7 [21.9-37.0] | 30.2 [23.5-38.4] | 32.9 [26.2-41.4] | 35.0 [27.9-42.4] | <0.001 |
| CRP (mg/L) | 3.0 [3.0-6.5] | 3.0 [3.0-6.7] | 3.0 [3.0-6.8] | 3.0 [3.0-6.3] | 0.04 |
| Albumin (g/dL) | 3.6 [3.0-3.9] | 4.0 [3.8-4.3] | 4.1 [3.9-4.3] | 4.1 [3.9-4.4] | <0.001 |
| Hemoglobin A1c (%) | 7.4 [6.4-8.5] | 7.1 [6.3-8.2] | 6.8 [6.2-7.7] | 6.7 [6.1-7.5] | <0.001 |
| Hemoglobin (g/dL) | 10.3 [9.6-10.9] | 10.4 [9.7-10.9] | 10.5 [9.9-11.0] | 10.6 [10.1-11.0] | <0.001 |
| Serum ferritin, (mg/L) | 153 [77-273] | 140 [72-283] | 119 [58-238] | 124 [62-244] | 0.001 |
| LDL cholesterol (mg/dL) | 101 [75, 137] | 85 [63, 109] | 81 [62, 103] | 77 [58-101] | <0.001 |
| HDL cholesterol (mg/dL) | 47 [40-57] | 45 [38-55] | 45 [37-54] | 46 [38-56] | <0.001 |
| Triglycerides (mg/dL) | 174 [120-258] | 148 [108-214] | 150 [108-223] | 148 [105-215] | <0.001 |
Note: P values for categorical variables, using Mantel-Haenszel χ2; P values for continuous variables, using analysis of variance. Conversion factors for units: serum creatinine in mg/dL to μmol/L, ×88.4; urea nitrogen in mg/dL to mmol/L, ×0.357; cholesterol in mg/dL to mmol/L ×0.02586.
Abbreviations: ACE, angiotensin-converting enzyme; AICD, automated implantable cardiac defibrillator; ARB, angiotensin receptor blocker; BP, blood pressure; CRP, C-reactive protein; eGFR, estimated glomerular filtration rate; ESA, erythropoiesis-stimulating agent; HDL, high-density lipoprotein; LDL, low-density lipoprotein; PCR, protein-creatinine ratio; PVD, peripheral vascular disease; Q, quartile.
Cause of Death According to eGFR and PCR
Overall, there were 806 deaths, with 441 categorized as CV deaths; 298, as non-CV deaths; and 67, as unknown. Vital status was unknown in 7.6% of patients in the darbepoetin group and 8.1% of patients in the placebo group. As shown in Table S1, cumulative incidences of overall, CV, and non-CV mortality were significantly higher in patients with lower baseline eGFRs. Among specific causes of death, there was a doubling in the 3-year cumulative incidence of death from stroke (P = 0.03), a 1.7-fold increase in the cumulative incidence of definite or presumed sudden death (P = 0.04), and a 3.3-fold increase in death from infection from the highest to lowest quartile of eGFR (P < 0.001). The cumulative incidence of death from MI was numerically higher in those in the lowest versus highest quartile of eGFR, but differences across eGFR quartiles did not achieve significance (P = 0.06; Table 3).
Table 3.
Cause-Specific Cumulative Incidence of Mortality According to Baseline eGFR
| Type of Death (N = 806) | Q1: 0.9-24.2 (n = 1,008) | Q2: 24.3-31.6 (n = 1,014) | Q3: 31.7-40.2 (n = 1,007) | Q4: 40.3-119.8 (n = 1,006) | P Value |
|---|---|---|---|---|---|
| Overall | 30.6% (27.3%-34.0%) | 21.1% (18.3%-24.0%) | 18.9% (16.2%-21.8%) | 18.2% (15.4%-21.1%) | <0.001 |
| CV death | 15.4% (12.9%-18.0%) | 11.1% (9.1%-13.4%) | 11.2% (9.0%-13.6%) | 10.3% (8.2%-12.7%) | <0.001 |
| Fatal MI | 2.1% (1.3%-3.2%) | 1.9% (1.1%-3.2%) | 0.8% (0.4%-1.6%) | 1.1% (0.6%-2.0%) | 0.06 |
| Fatal stroke | 1.3% (0.7%-2.3%) | 1.5% (0.8%-2.4%) | 1.0% (0.5%-1.9%) | 0.6% (0.2%-1.4%) | 0.03 |
| Presumed CV death | 1.9% (1.1%-3.1%) | 1.4% (0.8%-2.5%) | 1.7% (0.9%-2.9%) | 1.3% (0.7%-2.3%) | 0.3 |
| Pump failure | 2.4% (1.5%-3.7%) | 1.7% (1.0%-2.7%) | 1.3% (0.7%-2.3%) | 2.3% (1.3%-3.7%) | 0.5 |
| CV other | 0.5% (0.2%-1.3%) | 1.0% (0.5%-1.9%) | 0.6% (0.2%-1.4%) | 0.8% (0.3%-1.5%) | 0.7 |
| Presumed sudden death | 1.4% (0.7%-2.4%) | 0.7% (0.3%-1.4%) | 1.5% (0.8%-2.7%) | 0.4% (0.1%-1.1%) | 0.3 |
| Definite sudden death | 5.7% (4.2%-7.6%) | 2.9% (1.9%-4.2%) | 4.2% (2.9%-5.8%) | 3.8% (2.6%-5.4%) | 0.07 |
| Definite or presumed sudden death | 7.1% (5.4%-9.1%) | 3.6% (2.5%-5.0%) | 5.7% (4.2%-7.6%) | 4.2% (2.9%-5.9%) | 0.04 |
| Non-CV death | 12.7% (10.4%-15.2%) | 8.4% (6.5%-10.5%) | 6.7% (5.1%-8.6%) | 6.1% (4.5%-8.0%) | <0.001 |
| Infection | 4.9% (3.5%-6.6%) | 2.7% (1.7%-3.9%) | 2.0% (1.2%-3.2%) | 1.5% (0.8%-2.7%) | <0.001 |
| Malignancy | 1.9% (1.1%-3.1%) | 2.2% (1.3%-3.4%) | 1.4% (0.8%-2.4%) | 1.8% (1.0%-3.0%) | 0.5 |
| Other | 4.0% (2.8%-5.5%) | 2.6% (1.6%-4.0%) | 2.4% (1.6%-3.7%) | 2.3% (1.4%-3.5%) | 0.03 |
| Renal | 1.9% (1.0-3.2) | 0.9% (0.4-1.8) | 0.8% (0.4-1.7) | 0.5% (0.1-1.5) | 0.01 |
| Unknown | 2.5% (1.6-3.9) | 1.6% (0.8-2.7) | 1.0% (0.5-2.0) | 1.7% (0.9-2.8) | 0.2 |
Note: eGFR quartiles expressed in mL/min/1.73 m2. Values are given as estimated cumulative incidence rate at 3 years (95% confidence interval). P value for trend test refers to risk of death across all patient follow-up for each cause of death across eGFR quartiles. Renal deaths defined as refusal of dialysis therapy or death in the setting of acute kidney injury or from direct complications of uremia, dialysis, or renal procedure. Other deaths include suicide and deaths from pulmonary, hepatobiliary, gastrointestinal, procedural, and accidental causes.
Abbreviations: CV, cardiovascular; eGFR, estimated glomerular filtration rate; MI, myocardial infarction; Q, quartile.
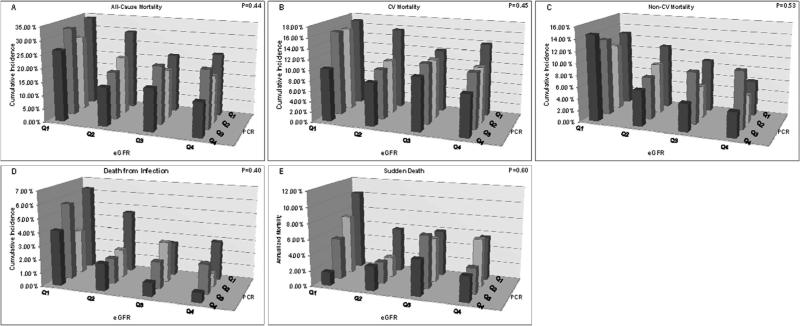
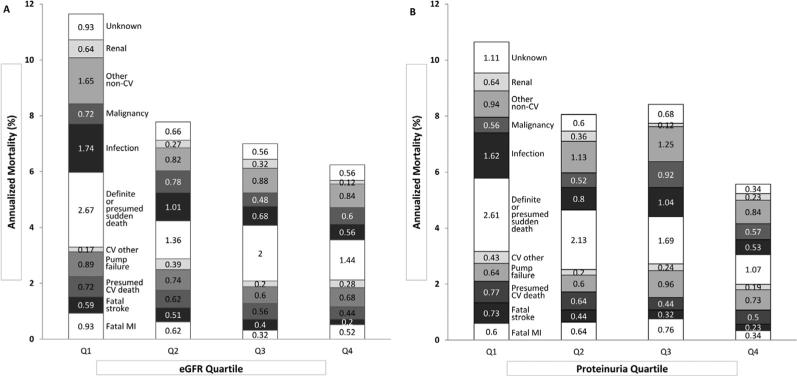
Annualized overall CV and non-CV mortality were also significantly higher with greater levels of baseline proteinuria (Fig 1; Table 4). The 3-year cumulative incidence of death from MI was not significantly associated with baseline proteinuria (Q1, 1.2%; Q4, 0.9%; P = 0.4), but the rate of stroke death increased 4.2-fold from the lowest to highest levels of protein excretion (P = 0.01). Sudden death was 2.1-fold more frequent (P < 0.001), and death from infection increased 2.8-fold (P = 0.002). Death from kidney disease was uncommon; the maximum cumulative incidence at 3 years was 1.9% in quartiles (Q1) with the lowest eGFR or highest protein excretion. However, the incidence of kidney death was significantly higher with more severe proteinuria or lower baseline eGFR (P = 0.01). Non–competing-risk analyses of incidence rate associations were qualitatively similar for eGFR and PCR as in the competing-risk estimates (Fig 2).
Figure 1.
Cumulative mortality according to estimated glomerular filtration rate (eGFR) and proteinuria at baseline. Event rates according to baseline protein-creatinine ratio (PCR) and eGFR. Median PCR values are 4.08 g/g in quartile 1 (Q1), 0.85 g/g in Q2, 0.21 g/g in Q3, and 0.09 g/g in Q4. Median eGFRs are 20.6 mL/min/1.73 m2 in Q1, 27.9 mL/min/1.73 m2 in Q2, 35.5 mL/min/ 1.73 m2 in Q3 and 47.0 mL/min/1.73 m2 in Q4. Abbreviations: CV, cardiovascular; MI, myocardial infarction.
Table 4.
Cause-Specific Cumulative Incidence of Mortality According to Baseline PCR
| Type of Death (N = 806) | Q1: 1.85-44.58 g/g (n = 1,009) | Q2: 0.39-1.85 g/g (n = 1,009) | Q3: 0.13-0.39 g/g (n = 1,009) | Q4: 0.003-0.13g/g (n = 1,009) | P |
|---|---|---|---|---|---|
| Overall | 28.7% (25.4%-32.1%) | 21.8% (18.9%-24.9%) | 22.6% (19.7%-25.6%) | 16.2% (13.7%-18.9%) | <0.001 |
| CV death | 15.2% (12.7%-17.9%) | 12.3% (10.1%-14.9%) | 11.7% (9.6%-14.0%) | 9.0% (7.1%-11.2%) | <0.001 |
| Fatal MI | 1.2% (0.6%-2.2%) | 2.1% (1.2%-3.4%) | 1.9% (1.1%-2.9%) | 0.9% (0.5%-1.7%) | 0.4 |
| Fatal stroke | 2.1% (1.2%-3.3%) | 1.1% (0.6%-1.9%) | 0.8% (0.4%-1.6%) | 0.5% (0.2%-1.2%) | 0.01 |
| Presumed CV death | 1.8% (1.0%-3.0%) | 1.9% (1.1%-3.1%) | 1.1% (0.6%-2.0%) | 1.5% (0.8%-2.6%) | 0.2 |
| Pump failure | 1.6% (0.9%-2.7%) | 1.4% (0.7%-2.5%) | 2.8% (1.8%-4.1%) | 2.0% (1.2%-3.2%) | 0.3 |
| CV other | 1.1% (0.5%-2.1%) | 0.4% (0.1%-1.0%) | 0.7% (0.3%-1.4%) | 0.7% (0.3%-1.6%) | 0.2 |
| Presumed sudden death | 1.4% (0.8%-2.5%) | 1.1% (0.5%-2.1%) | 0.5% (0.2%-1.2%) | 0.9% (0.4%-1.9%) | 0.1 |
| Definite sudden death | 5.9% (4.4%-7.8%) | 4.4% (3.1%-6.1%) | 3.9% (2.7%-5.4%) | 2.5% (1.5%-3.7%) | <0.001 |
| Definite or presumed sudden death | 7.3% (5.6%-9.4%) | 5.5% (4.0%-7.3%) | 4.4% (3.1%-6.1%) | 3.4% (2.3%-4.9%) | <0.001 |
| Non-CV death | 10.3% (8.3%-12.7%) | 7.9% (6.1%-10.0%) | 9.4% (7.5%-11.6%) | 6.4% (4.9%-8.3%) | 0.01 |
| Infection | 4.5% (3.2%-6.2%) | 2.4% (1.5%-3.7%) | 2.7% (1.7%-4.0%) | 1.6% (0.9%-2.6%) | 0.002 |
| Malignancy | 1.5% (0.8%-2.6%) | 1.6% (0.9%-2.8%) | 2.7% (1.7%-4.1%) | 1.5% (0.9%-2.4%) | 0.4 |
| Other | 2.3% (1.5%-3.5%) | 3.0% (1.9%-4.3%) | 3.5% (2.4%-5.0%) | 2.5% (1.6%-3.8%) | 0.9 |
| Renal | 1.9% (1.1%-3.2%) | 0.9% (0.4%-1.7%) | 0.5% (0.1%-1.4%) | 0.9% (0.4%-1.9%) | 0.01 |
| Unknown | 3.2% (2.0%-4.7%) | 1.5% (0.9%-2.6%) | 1.5% (0.8%-2.6%) | 0.7% (0.3%-1.6%) | 0.004 |
Note: Values are given as estimated cumulative incidence rate at 3 years (95% confidence interval). P value for trend test refers to risk of death across all patient follow-up for each cause of death across PCR quartiles. Renal deaths defined as refusal of dialysis therapy or death in the setting of acute kidney injury or from direct complications of uremia, dialysis, or renal procedure. Other deaths include suicide and deaths from pulmonary, hepatobiliary, gastrointestinal, procedural, and accidental causes.
Abbreviations: CV, cardiovascular; MI, myocardial infarction; PCR, protein-creatinine ratio; Q, quartile.
Figure 2.
Annualized cause-specific mortality (non–competing risk) according to baseline (A) estimated glomerular filtration rate (eGFR) or (B) proteinuria. Abbreviation: CV, cardiovascular.
In multivariable competing-risk models adjusting for randomized therapy, age, race, sex, duration of diabetes, systolic and diastolic blood pressures, and history of CV disease, lower eGFR, and higher PCR were independently associated with increased relative risks of overall, CV, and non-CV death (Tables 5 and 6; P < 0.001 for trend across quartiles). Lower baseline eGFR or higher PCR was also independently associated with even greater increases in risk of fatal stroke, death from infection, and renal death (minimum hazard ratio for Q1 vs Q4, ≥2.7). In addition, PCR quartile was associated with risk of definite or presumed sudden death (P < 0.001), but the association with eGFR quartile was not significant (P = 0.06).
Table 5.
Multivariable Adjusted Competing Risks of Cause-Specific Mortality According to Baseline eGFR
| Type of Death | Q1: 0.9-24.2 (n = 1,008) | Q2: 24.3-31.6 (n = 1,014) | Q3: 31.7-40.2 (n = 1,007) | P |
|---|---|---|---|---|
| Overall | 1.83 (1.50-2.23) | 1.23 (0.99-1.51) | 1.08 (0.87-1.34) | <0.001 |
| CV death | 1.53 (1.17-1.99) | 1.16 (0.88-1.54) | 1.11 (0.84-1.48) | 0.002 |
| Fatal MI | 1.55 (0.79-3.05) | 1.15 (0.55-2.42) | 0.60 (0.25-1.43) | 0.09 |
| Fatal stroke | 2.71 (0.97-7.57) | 2.60 (0.92-7.35) | 1.96 (0.66-5.80) | 0.04 |
| Presumed CV death | 1.42 (0.67-3.04) | 1.29 (0.61-2.74) | 1.16 (0.52-2.59) | 0.3 |
| Pump failure | 1.17 (0.62-2.22) | 1.04 (0.54-2.01) | 0.81 (0.41-1.62) | 0.5 |
| CV other | 0.52 (0.15-1.78) | 1.40 (0.51-3.82) | 0.73 (0.23-2.30) | 0.6 |
| Presumed sudden death | 1.99 (0.75-5.27) | 0.96 (0.32-2.91) | 1.86 (0.70-4.95) | 0.4 |
| Definite sudden death | 1.62 (1.03-2.54) | 0.91 (0.54-1.53) | 1.28 (0.79-2.07) | 0.1 |
| Definite or presumed sudden death | 1.69 (1.12-2.54) | 0.92 (0.58-1.47) | 1.38 (0.90-2.12) | 0.06 |
| Non-CV death | 2.11 (1.52-2.93) | 1.31 (0.92-1.86) | 1.04 (0.71-1.51) | <0.001 |
| Infection | 2.74 (1.50-5.02) | 1.74 (0.90-3.34) | 1.16 (0.56-2.37) | <0.001 |
| Malignancy | 1.16 (0.56-2.37) | 1.30 (0.66-2.55) | 0.73 (0.34-1.57) | 0.4 |
| Other | 1.81 (1.06-3.09) | 0.93 (0.50-1.71) | 0.97 (0.54-1.77) | 0.04 |
| Renal | 4.57 (1.33-15.74) | 2.00 (0.52-7.64) | 2.35 (0.62-8.85) | 0.01 |
| Unknown | 1.52 (0.77-3.00) | 1.18 (0.58-2.41) | 0.99 (0.47-2.10) | 0.2 |
Note: Values are given as hazard ratio (95% confidence interval). eGFR quartiles expressed in mL/min/1.73 m2; Q4 (40.3-119.8 mL/min/1.73 m2) is reference group (n = 1,006). Multivariable competing-risks models for specific causes of death. All models adjusted for for treatment, age, race, sex, diabetes, duration of diabetes, systolic and diastolic blood pressure, and history of CV disease.
Abbreviations: CV, cardiovascular; eGFR, estimated glomerular filtration rate; MI, myocardial infarction; Q, quartile.
Table 6.
Multivariable-Adjusted Competing Risks of Cause-Specific Mortality According to Baseline PCR
| Type of Death | Q1: 1.85-44.58 g/g (n = 1,009) | Q2: 0.39-1.85 g/g (n = 1,009) | Q3: 0.13-0.39g/g (n = 1,009) | P |
|---|---|---|---|---|
| Overall | 2.89 (2.32-3.60) | 1.70 (1.37-2.10) | 1.52 (1.22-1.88) | <0.001 |
| CV death | 2.42 (1.80-3.27) | 1.64 (1.23-2.19) | 1.38 (1.03-1.85) | <0.001 |
| Fatal MI | 1.98 (0.89-4.42) | 1.84 (0.82-4.10) | 1.92 (0.88-4.21) | 0.1 |
| Fatal stroke | 3.94 (1.46-10.6) | 2.10 (0.74-6.00) | 1.33 (0.47-3.82) | 0.004 |
| Presumed CV death | 1.81 (0.87-3.78) | 1.33 (0.63-2.82) | 0.75 (0.33-1.69) | 0.07 |
| Pump failure | 1.59 (0.77-3.27) | 1.04 (0.52-2.07) | 1.36 (0.75-2.07) | 0.4 |
| CV other | 3.10 (0.93-10.5) | 1.09 (0.30-3.93) | 1.17 (0.34-4.01) | 0.1 |
| Presumed sudden death | 1.57 (0.56-4.38) | 1.48 (0.57-3.83) | 0.71 (0.22-2.29) | 0.2 |
| Definite sudden death | 2.99 (1.68-5.30) | 2.20 (1.29-3.75) | 1.80 (1.05-3.08) | <0.001 |
| Definite or presumed sudden death | 2.64 (1.59-4.36) | 2.03 (1.27-3.23) | 1.53 (0.94-2.47) | <0.001 |
| Non-CV death | 2.63 (1.86-3.74) | 1.54 (1.07-2.19) | 1.50 (1.06-2.10) | <0.001 |
| Infection | 4.05 (2.13-7.73) | 1.61 (0.80-3.25) | 1.79 (0.93-3.46) | <0.001 |
| Malignancy | 1.67 (0.76-3.67) | 1.24 (0.57-2.72) | 1.75 (0.90-3.40) | 0.3 |
| Other | 1.62 (0.89-2.96) | 1.56 (0.90-2.71) | 1.46 (0.85-2.53) | 0.09 |
| Renal | 4.24 (1.59-11.3) | 1.82 (0.60-5.54) | 0.46 (0.11-1.87) | 0.002 |
| Unknown | 4.64 (2.09-10.31 | 2.08 (0.88-4.90) | 2.09 (0.93-4.69) | <0.001 |
Note: Values are given as hazard ratio (95% confidence interval). Q4 (0.003-0.13 g/g) is reference group (n = 1,009). Multivariable competing-risks models for specific causes of death. All models adjusted for for treatment, age, race, sex, diabetes, duration of diabetes, systolic and diastolic blood pressure, and history of CV disease.
Abbreviations: CV, cardiovascular; MI, myocardial infarction; PCR, protein-creatinine ratio; Q, quartile.
As shown in Table 7, most deaths were due to CV causes regardless of baseline eGFR. The proportion of CV compared with non-CV deaths did not differ significantly with eGFR, but there was a significant increase in the proportion of deaths due to infection (Q1, 14.9%; Q2, 13.0%; Q3, 9.7%; Q4, 9.0%; P = 0.04). Similarly, CV causes were responsible for most deaths at all levels of PCR (Table 8), although heart failure accounted for a smaller proportion of deaths in individuals with more proteinuria (P = 0.01). The proportion of deaths from infection did not change significantly as PCR increased (Q1, 15.3%; Q2, 10.0%; Q3, 12.4%; Q4, 9.6%; P = 0.2), but there were significantly fewer deaths from malignancy (P = 0.02).
Table 7.
Proportions of Deaths Due to Specific Causes According eGFR
| Type of Death (N = 806) | Q1: 0.9-24.2 (n = 1,008) | Q2: 24.3-31.6 (n = 1,014) | Q3: 31.7-40.2 (n = 1,007) | Q4: 40.3-119.8 (n = 1,006) | P |
|---|---|---|---|---|---|
| Overall | 275 | 200 | 175 | 156 | |
| CV death | 141 (51.27) | 109 (54.50) | 102 (58.29) | 89 (57.05) | 0.2 |
| Fatal MI | 22 (8.00) | 16 (8.00) | 8 (4.57) | 13 (8.33) | 0.7 |
| Fatal stroke | 14 (5.09) | 13 (6.5) | 10 (5.71) | 5 (3.21) | 0.5 |
| Presumed CV death | 17 (6.18) | 16 (8.00) | 14 (8.00) | 11 (7.05) | 0.7 |
| Pump failure | 21 (7.64) | 19 (9.50) | 15 (8.57) | 17 (10.90) | 0.3 |
| CV other | 4 (1.45) | 10 (5.00) | 5 (2.86) | 7 (4.49) | 0.2 |
| Presumed sudden death | 12 (4.36) | 6 (3.00) | 11 (6.29) | 6 (3.85) | 0.8 |
| Definite sudden death | 51 (18.55) | 29 (14.50) | 39 (22.29) | 30 (19.23) | 0.5 |
| Definite or presumed sudden death | 63 (22.91) | 35 (17.50) | 50 (28.57) | 36 (23.08) | 0.4 |
| Non-CV death | 112 (40.73) | 74 (37.00) | 59 (33.71) | 53 (33.97) | 0.1 |
| Infection | 41 (14.91) | 26 (13.00) | 17 (9.71) | 14 (8.97) | 0.04 |
| Malignancy | 17 (6.18) | 20 (10.00) | 12 (6.86) | 15 (9.62) | 0.3 |
| Other | 39 (14.18) | 21 (10.50) | 22 (12.57) | 21 (13.46) | 0.8 |
| Renal | 15 (5.45) | 7 (3.50) | 8 (4.57) | 3 (1.92) | 0.1 |
| Unknown | 22 (8.00) | 17 (8.50) | 14 (8.00) | 14 (8.97) | 0.8 |
Note: Values are given as number (percentage) of deaths due to specific causes within eGFR quartiles. eGFR quartiles expressed in mL/min/1.73 m2. P values are for trend in percent of deaths attributable to each cause across eGFR quartiles. Renal deaths defined as refusal of dialysis therapy or death in the setting of acute kidney injury or from direct complications of uremia, dialysis, or renal procedure. Other deaths include suicide and deaths from pulmonary, hepatobiliary, gastrointestinal, procedural, and accidental causes.
Abbreviations: CV, cardiovascular; eGFR, estimated glomerular filtration rate; MI, myocardial infarction; Q, quartile.
Table 8.
Proportions of Deaths Due to Specific Causes According to Baseline PCR
| Type of Death (N = 806) | Q1: 1.85-44.58 g/g (n = 1,009) | Q2: 0.39-1.85 g/g (n = 1,009) | Q3: 0.13-0.39 g/g (n = 1,009) | Q4: 0.003-0.13 g/g (n = 1,009) | P |
|---|---|---|---|---|---|
| Overall | 249 | 201 | 210 | 146 | |
| CV death | 135 (54.22) | 116 (57.71) | 110 (52.38) | 80 (54.79) | 0.8 |
| Fatal MI | 14 (5.62) | 16 (7.96) | 19 (9.05) | 9 (6.16) | 0.6 |
| Fatal stroke | 17 (6.83) | 11 (5.47) | 8 (3.81) | 6 (4.11) | 0.1 |
| Presumed CV death | 18 (7.23) | 16 (7.96) | 11 (5.24) | 13 (8.90) | 0.9 |
| Pump failure | 15 (6.02) | 15 (7.46) | 24 (11.43) | 19 (13.01) | 0.01 |
| CV other | 10 (4.02) | 5 (2.49) | 6 (2.86) | 5 (3.42) | 0.7 |
| Presumed sudden death | 12 (4.82) | 11 (5.47) | 5 (2.38) | 7 (4.79) | 0.5 |
| Definite sudden death | 49 (19.68) | 42 (20.90) | 37 (17.62) | 21 (14.38) | 0.2 |
| Definite or presumed sudden death | 61 (24.50) | 53 (26.37) | 42 (20.00) | 28 (19.18) | 0.1 |
| Non-CV death | 88 (35.34) | 70 (34.83) | 83 (39.52) | 57 (39.04) | 0.3 |
| Infection | 38 (15.26) | 20 (9.95) | 26 (12.38) | 14 (9.59) | 0.2 |
| Malignancy | 13 (5.22) | 13 (6.47) | 23 (10.95) | 15 (10.27) | 0.02 |
| Other | 22 (8.84) | 28 (13.93) | 31 (14.76) | 22 (15.07) | 0.05 |
| Renal | 15 (6.02) | 9 (4.48) | 3 (1.43) | 6 (4.11) | 0.1 |
| Unknown | 26 (10.11) | 15 (7.46) | 17 (8.10) | 9 (6.16) | 0.2 |
Note: Values are given as number (percentage) of deaths due to specific causes within PCR quartiles. P values are for trend in percent of deaths attributable to each cause across quartiles. Renal deaths defined as refusal of dialysis therapy or death in the setting of acute kidney injury or from direct complications of uremia, dialysis, or renal procedure. Other deaths include suicide and deaths from pulmonary, hepatobiliary, gastrointestinal, procedural, and accidental causes.
Abbreviations: CV, cardiovascular; MI, myocardial infarction; PCR, protein-creatinine ratio; Q, quartile.
Analyses jointly incorporating both baseline eGFR and PCR demonstrated increased incidence rates for overall, CV, non-CV, and infectious mortality at lower eGFRs in each category of baseline PCR (Fig 1). Sudden death cumulative incidence increased as eGFR declined in the highest quartile of protein excretion (Q1). Conversely, in the lowest quartile of protein excretion (Q4), the incidence of sudden death decreased at lower eGFRs. Cumulative incidence rates for these end points generally increased across categories of increasing PCR at all levels of baseline eGFR, except that non-CV death at the lowest quartile of eGFR (Q1) was more frequent in those with the lowest baseline PCR (Q4) compared with those with the highest baseline PCR (Q1). Although the cumulative incidence of each type of death was markedly higher in individuals belonging to both the highest quartile of PCR (Q1) and the lowest quartile of eGFR (Q1) compared with those with the lowest PCR (Q4) and highest eGFR (Q4), tests of interaction were nonsignificant without evidence of significant effect modification (P for interaction ≥ 0.4 for all comparisons).
Cause of Death Before and After ESRD Onset
Onset of ESRD prior to time of death was strongly associated with cause of death (Table S1). The percent of deaths attributable to CV causes was 11.3% lower among patients who had reached ESRD prior to death than among those not reaching ESRD prior to death (P = 0.01). Conversely, the percent of deaths attributable to non-CV causes was 15.2% higher among those reaching ESRD than among those without ESRD at the time of death (P < 0.001). This was largely attributable to a significantly lower proportion of sudden deaths and a higher proportion of infectious and renal deaths.
Sensitivity and Secondary Analyses
Results were qualitatively similar when analyzed according to last eGFR (Table S2), when the 4-variable MDRD Study equation was used to estimate GFR (Table S3), in analyses incorporating time-varying estimates of kidney function (Table S4), and when incidence rates were calculated without competing-risk techniques (Tables S5 and S6). Results were also qualitatively similar when associations with cause of death were examined separately within the darbepoetin and placebo treatment groups (Tables S7 and S8). There were no significant interactions between treatment and eGFR. There was a significant quantitative interaction between PCR and treatment for the end point of fatal stroke (P = 0.03). However, similar to that observed in the overall population, the risk of stroke increased in both the darbepoetin and placebo groups as PCR increased.
We also analyzed an alternative definition of non-CV death that excluded renal deaths from the category. In competing-risk models using Q4 as the reference, the relative risk of nonrenal non-CV death remained increased as eGFR declined (hazard ratios of 1.92 [95% CI, 1.37-2.71], 1.26 [95% CI, 0.87-1.82], and 0.95 [95% CI, 0.65-1.41] for Q1, Q2, and Q3, respectively; P < 0.001) and as PCR increased (hazard ratios of 2.40 [95% CI, 1.64-3.49], 1.48 [95% CI, 1.01-2.16], and 1.63 [95% CI, 1.15-2.32] for Q1, Q2, and Q3, respectively; P < 0.001). Cumulative incidence rates were higher for individuals with lower eGFRs (Q1, 10.8%; Q2, 7.4%; Q3, 5.9%; Q4, 5.6%; P < 0.001), but not for PCR (Q1, 8.4%; Q2, 7.0%; Q3, 8.9%; Q4, 5.6%; P = 0.1).
DISCUSSION
In this study, we assessed cause-specific mortality in individuals with diabetic CKD and anemia and found that both lower eGFR and higher PCR at baseline were associated with markedly higher risks of non-CV mortality and death from infection, as well as CV mortality. With lower eGFR or higher PCR, there were significant increases in the cumulative incidence of fatal stroke, sudden death, death from infection, and renal death. Despite increasing incidence, the overall proportion of deaths from CV and non-CV causes did not differ significantly across categories of baseline eGFR and PCR. However, infection accounted for a significantly higher proportion of deaths in patients with lower baseline eGFRs.
Our analysis confirms an increase in non-CV mortality rates as diabetic CKD becomes more severe, and it newly demonstrates that the incidence of non-CV mortality continues to increase with worsening eGFRs in individuals with CKD stages 3 to 5 and diabetes, particularly at the lowest levels of eGFR. We also observed incremental increases in infectious mortality with declining eGFRs and incremental increases in renal deaths, defined as deaths due to refusal of dialysis, acute kidney injury, or complications of uremia, dialytic therapy, or renal procedures. Furthermore, the risk of these events was independently associated with baseline eGFR in adjusted models.
In contrast to prior studies, we analyzed associations of quantitative measurements of baseline proteinuria with non-CV mortality. Higher baseline PCR was associated with increased rates of both CV and non-CV mortality and incremental increases in infectious mortality and death from renal causes and was independently associated with the risk of these events in adjusted models. We also considered the combined impact of proteinuria and low eGFR on outcomes. Although non-CV mortality rates were highest in individuals with the most severe baseline abnormalities, there was no significant interaction between proteinuria and eGFR on the risk of specific causes of death. There were similar increases in risk across categories of eGFR at each level of baseline proteinuria, and risk likewise increased across categories of baseline proteinuria at each level of baseline eGFR.
Although increases in the risk of CV mortality have been reported both in individuals with reduced eGFR and those with proteinuria,1-6,15 compared with those without kidney disease, associations of these measures of kidney function with non-CV mortality or with specific causes of CV or non-CV death have been less widely analyzed. A recent study of Canadian adults, for example, demonstrated strong associations between eGFR and risk of hospitalization and death from pneumonia.7 Similarly, in an analysis of elderly individuals in the Cardiovascular Health Study, Fried et al16 found that rates of death from dementia, pulmonary disease, cancer, and infection were significantly increased in the lowest quartile of eGFR, whereas the rate of infectious death increased incrementally across quartiles of declining eGFR. Associations with proteinuria were not studied, and the number of individuals with late-stage CKD was unclear. Similarly, in a study of adults in Iceland, the presence of reduced eGFR or dipstick-positive proteinuria was associated with an increase in nonvascular mortality that appeared to be driven by noncancer deaths.8 Notably, only 77 of 16,958 individuals studied had eGFRs < 45 mL/min/1.73 m2. Furthermore, specific causes of non-CV death were not analyzed further, and associations with incremental changes in baseline proteinuria were not assessed. Finally, de Jager et al9 have reported that age-standardized rates of CV and non-CV mortality increase to a similar degree in patients initiating dialysis therapy and that there is a greater excess of non-CV than CV deaths in dialysis patients compared with the general population. Our study extends upon these findings by demonstrating associations between eGFR and proteinuria with both overall non-CV mortality, death from infection, and renal deaths in a large population of individuals with CKD, including a sizeable number with advanced CKD.
Our study also provides new data for rates of specific causes of CV death at various levels of baseline PCR and eGFR in diabetic CKD. Both eGFR and PCR were significantly associated with dramatic increases in the cumulative incidence of sudden death and stroke death. With the exception of the association of eGFR with sudden death (P = 0.06), cause of death and eGFR or PCR were independently associated after adjustment for important confounders, suggesting the possibility of causal relationships between kidney function and cause of death. In contrast, neither death from heart failure nor MI differed significantly across baseline categories of PCR or eGFR. As with non-CV death, there was no evidence of effect modification of the association of PCR and eGFR with CV death.
Finally, we analyzed the relative proportion of deaths due to individual CV and non-CV modalities of death. In contrast to our initial hypothesis, with the exception of an increased proportion of deaths due to infection as eGFR declined and a decrease in the proportion of deaths due to malignancy as PCR declined, proportions of deaths due to particular causes did not differ across categories of PCR or eGFR. Among patients reaching ESRD before dying, non-CV deaths were significantly more frequent than CV deaths. The overall proportion of CV deaths was also numerically lower at lower eGFRs, although the difference was nonsignificant. These data are consistent with the conclusion of de Jager et al9 that patients with severely decreased kidney function, that is, those initiating dialysis therapy, have a generally increased risk of death that arises equally from CV and non-CV causes.
Our findings should not diminish interest in understanding or treating CV mortality in the setting of CKD. However, further study to identify the causative mechanisms linking low eGFR and high PCR with non-CV death are also warranted and may provide an important means of improving overall outcomes in the CKD population.
The high rate of death from infection is particularly intriguing. This association may reflect an increase in oxidative stress and inflammation17 (possibly exacerbated by the use of intravenous iron to treat anemia) or defects in cellular immune function18 as eGFR declines. In contrast to many studies, we were also able to follow and compare outcomes before and after the onset of ESRD, an outcome more frequent than death in those in the first quartiles of eGFR or proteinuria but with a lower incidence in individuals with less severe abnormalities in baseline kidney function (data not shown). Our observation that 37.7% of infectious deaths occurred in patients reaching ESRD and that infection accounted for 18.1% of deaths among individuals who had reached ESRD before dying compared with only 10.1% among those not requiring renal replacement therapy is consistent with the hypothesis that a large proportion of infectious deaths in the CKD population are related to the use of catheters during the transition to dialysis therapy. Prior studies have consistently demonstrated that use of catheters as permanent access is associated with increased risks of death and infection.19,20 Controlled trials demonstrating a reduction in mortality with preferential placement of fistulas have not been performed. Our observations are preliminary, but they provide motivation for additional investigations of the impact of catheter and fistula use on the risk of infectious death in the CKD population.
Our study has several limitations. The combination of diabetes, CKD, and anemia was required for enrollment in TREAT. Thus, our results may not be generalizable to nondiabetic CKD or to diabetic CKD in the absence of anemia. This may be particularly important because diabetes is strongly associated with CV events and mortality in CKD.5 We were also unable to measure GFR and relied on eGFR, which is an imperfect tool. However, any misclassification would be expected to be random, and associations with eGFR were qualitatively similar when it was estimated using the 4-variable MDRD Study equation (data not shown). The number of events for individual modes of death was small and limited the power to detect differences in the rates of some events across quartiles of eGFR and PCR. Conversely, the large number of analyses performed may have increased the likelihood of false-positive findings. Finally, ascertaining cause of death can be challenging, particularly when only limited clinical data could be obtained, although use of standard definitions and blinding of adjudicators should limit misattribution and ensure consistency. Finally, the relatively small number of events for individual causes of death limited our ability to build stable multivariable models with simultaneous adjustment for more than a few confounding factors. For each of these reasons, larger studies enrolling a broader CKD population are warranted to confirm our findings.
In conclusion, we studied a large population of individuals with diabetes, anemia, and CKD. CV deaths accounted for most deaths, and the overall proportion of deaths due to specific causes was similar at all levels of protein excretion or baseline eGFR. In addition, there were marked increases in non-CV mortality rates with lower baseline eGFR or higher baseline PCR. Changes in the rate of death due to infection were particularly notable and suggest that prophylaxis and early treatment of infection in moderate to advanced CKD may represent an important therapeutic target for improving mortality in this population.
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank Hongshu Guan for assistance with statistical analysis.
Support: Dr Charytan was partially supported by the Carl Gottschalk Award of the American Society of Nephrology and National Institute of Diabetes and Digestive and Kidney Diseases grants R21DK089368, R21DK100772, 1U01DK096189, and R01HL118314.
Footnotes
Because an author of this article is an editor for AJKD, the peer-review and decision-making processes were handled entirely by an Associate Editor (Martin Zeier, MD) who served as Acting Editor-in-Chief. Details of the journal's procedures for potential editor conflicts are given in the Information for Authors & Editorial Policies.
This work was presented in abstract form at the November 2013 meeting of the American Society of Nephrology.
Financial Disclosure: TREAT was funded by Amgen. This analysis was conducted independently by the authors and used the data set held at the Brigham & Women's Hospital; the authors designed and conducted all analyses described herein and were solely responsible for the drafting and editing of this manuscript. Dr Charytan reports consulting fees from Keryx, Tengion, and Boehringer Ingeleheim, as well as fees for serving on a clinical events committee for PLC Medical. Dr Pfeffer reports research support from Amgen, Novartis, and Sanofi and indirect consulting fees from Bristol-Myers Squibb, GlaxoSmithKline, Hamilton Health Sciences, Merck, Karo Bio, NicOx, Novartis, Roche, Sanofi, and University of Oxford. Dr McMurray has received travel expenses and reports that his employer has been paid for his work on the steering committees of TREAT and the RED-HF (Reduction of Events With Darbepoetin Alfa in Heart Failure) trial. Dr Singh reports consulting fees and travel expenses from Amgen and consulting to IHS Dialysis, Sandoz, Rockwell, and Concert. Dr Toto reports research support, consulting fees, and travel from Amgen and board membership at Boehringer Ingelheim. Dr Ivanovich reports travel and other fees from Amgen for work on a data and safety monitoring board and fees for serving on data and safety monitoring boards for Reata and Applied Clinical Intelligence and is a member of the medical advisory board of Physician Software Systems LLC. Dr Lewis reports research support from Amgen, Novartis, and Sanofi. Dr Solomon reports research support and consulting fees from Amgen. Dr Levey reports funding from Tufts Medical Center for research and contracts with the National Institutes of Health, National Kidney Foundation, Amgen, Pharmalink AB, and Gilead Sciences. Dr Weinrauch reports receiving travel expenses from Amgen and fees related to service on clinical events committees from Amgen, Sanofi, and Novartis and as site principal investigator for Roche, Wyeth, and Boehringer Ingelheim Pharmaceuticals. Dr Desai reports funding from Amgen to support travel to publication committee meetings for the RED-HF trial. The other authors declare that they have no other relevant financial interests.
REFERENCES
- 1.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 2.Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295. doi: 10.1056/NEJMoa041365. [DOI] [PubMed] [Google Scholar]
- 3.Astor BC, Matsushita K, Gansevoort RT, et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with mortality and end-stage renal disease. A collaborative meta-analysis of kidney disease population cohorts. Kidney Int. 2011;79:1331–1340. doi: 10.1038/ki.2010.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clase CM, Gao P, Tobe SW, et al. Estimated glomerular filtration rate and albuminuria as predictors of outcomes in patients with high cardiovascular risk: a cohort study. Ann Intern Med. 2011;154:310–318. doi: 10.7326/0003-4819-154-5-201103010-00005. [DOI] [PubMed] [Google Scholar]
- 5.Fox CS, Matsushita K, Woodward M, et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet. 2012;380:1662–1673. doi: 10.1016/S0140-6736(12)61350-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsushita K, van der Velde M, Astor BC, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073–2081. doi: 10.1016/S0140-6736(10)60674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.James MT, Quan H, Tonelli M, et al. CKD and risk of hospitalization and death with pneumonia. Am J Kidney Dis. 2009;54:24–32. doi: 10.1053/j.ajkd.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Di Angelantonio E, Chowdhury R, Sarwar N, Aspelund T, Danesh J, Gudnason V. Chronic kidney disease and risk of major cardiovascular disease and non-vascular mortality: prospective population based cohort study. BMJ. 2010;341:c4986. doi: 10.1136/bmj.c4986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Jager DJ, Grootendorst DC, Jager KJ, et al. Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA. 2009;302:1782–1789. doi: 10.1001/jama.2009.1488. [DOI] [PubMed] [Google Scholar]
- 10.Pfeffer MA, Burdmann EA, Chen CY, et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med. 2009;361:2019–2032. doi: 10.1056/NEJMoa0907845. [DOI] [PubMed] [Google Scholar]
- 11.Levey AS, Greene T, Kusek J, Beck G. A simplified equation to predict glomerular filtration rate from serum creatinine [abstract]. J Am Soc Nephrol. 2000;11:155A. [Google Scholar]
- 12.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139:137–147. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 14.Fine J, Gray RJ. A proportional hazards model for the sub-distribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 15.van der Velde M, Matsushita K, Coresh J, et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int. 2011;79:1341–1352. doi: 10.1038/ki.2010.536. [DOI] [PubMed] [Google Scholar]
- 16.Fried LF, Katz R, Sarnak MJ, et al. Kidney function as a predictor of noncardiovascular mortality. J Am Soc Nephrol. 2005;16:3728–3735. doi: 10.1681/ASN.2005040384. [DOI] [PubMed] [Google Scholar]
- 17.Himmelfarb J, Stenvinkel P, Ikizler TA, Hakim RM. The elephant in uremia: oxidant stress as a unifying concept of cardiovascular disease in uremia. Kidney Int. 2002;62:1524–1538. doi: 10.1046/j.1523-1755.2002.00600.x. [DOI] [PubMed] [Google Scholar]
- 18.Mahajan S, Kalra OP, Asit KT, Ahuja G, Kalra V. Phagocytic polymorphonuclear function in patients with progressive uremia and the effect of acute hemodialysis. Ren Fail. 2005;27:357–360. [PubMed] [Google Scholar]
- 19.Collins AJ, Foley RN, Herzog C, et al. US Renal Data System 2010 annual data report. Am J Kidney Dis. 2011;57(suppl 1):e1–e526. doi: 10.1053/j.ajkd.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Ravani P, Palmer SC, Oliver MJ, et al. Associations between hemodialysis access type and clinical outcomes: a systematic review. J Am Soc Nephrol. 2013;24:465–473. doi: 10.1681/ASN.2012070643. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.