Abstract
Background
This study investigates whether a recovery management intervention (RMI) can improve the utilization of community drug treatment and wraparound services among heroin users in China and subsequently lead to positive recovery outcomes.
Methods
Secondary analysis was conducted drawing data from a randomized controlled trial; 100 heroin users with no severe mental health problems were recruited in two Shanghai districts (Hongkou and Yangpu) upon their release from compulsory rehabilitation facilities. A latent variable modeling approach was utilized to test whether the RMI influences heroin users' perceived motivation and readiness for treatment, enhances treatment and wraparound service participation, and, in turn, predicts better recovery outcomes.
Results
Enrollment in drug treatment and other social service utilization increased significantly as a result of RMI rather than an individual drug user's motivation and readiness for treatment. Increased service utilization thus led to more positive individual recovery outcomes. In addition to this mediation effect through service utilization, the RMI also improved participants' community recovery directly.
Conclusions
Findings suggest that better drug treatment enrollment, community service utilization and recovery outcomes can be potentially achieved among heroin users in China with carefully designed case management interventions.
Keywords: health services
Background
China's health burden has changed dramatically in the past two decades. Among the new health challenges (e.g. poor food quality and air pollution) the country had never encountered until the 1990s, HIV/AIDS and substance abuse are two leading causes of years of life lost and years lived with disability.1
The 2012 estimate of cumulative HIV-positive cases in China was 780 000, including 154 000 AIDS cases and 28 000 AIDS-related deaths.2 Although national HIV prevalence is low (0.058%), the number of annual new infections has been alarmingly high (∼50 000 cases per year) since 2007. Although sexual transmission recently replaced injection drug use (IDU) to become the largest contributor to annual new HIV infections in China, IDU still accounts for a considerable portion of those infections (18% in 2011). Moreover, the HIV infection rate remains high among injection drug users (>50%).2 The number of drug users registered with the police in China was 1.5 million by the end of 2010.3 But the total number of drug users is estimated to be >3.5 million.3 Among the drug users who were registered with the police in 2011, ∼1 million (70%) were heroin users.3 In addition, 50–70% of the heroin users in China inject the drug.4
China used to address heroin addiction with a punitive approach, sentencing drug users to compulsory rehabilitation facilities. These police-run programs usually entail drug detoxification and labor work,5 and the relapse rate after rehabilitation was reported to be >80% within a year.4 In June 2008, ‘The Law against Drug Abuse and Illicit Drug Trafficking’ came into effect in China, wherein the country officially adopted community-based drug treatment and recovery in addition to compulsory rehabilitation.6,7
China started testing harm reduction programs in 2004 to prevent heroin use and HIV/AIDS8,9 because previous empirical evidence had demonstrated positive associations between community treatment utilization and drug users' recovery.10–12 By the end of 2011, 738 methadone maintenance treatment (MMT) clinics had been established nationwide, serving cumulatively 344 000 heroin users and 140 100 current patients.2 Current MMT patients only account for ∼15% of all registered drug users. In addition, recent evaluation studies indicated a drop-out rate of 50–70% at 3 months after MMT enrollment.13,14 Low rates of enrollment and high rates of drop out suggest that barriers may exist in patients accessing and remaining in community drug treatment in China.4
Parallel to the establishment of MMT, China has also scaled up social work services to assist drug users with their recovery.15 The planned social services for drug users include: counseling, behavioral intervention, social support, family therapy, social networking and community resources such as MMT clinics, social security funds, employment services and general health services.16 Those who work with drug users in community recovery were among the earliest social work workforces established in China.17 However, hardly any research has documented this latest development in China.
Empirical evidence in the USA has shown that case management can facilitate drug offenders' admission to community drug treatment and other services18 and subsequently address problems of substance abuse,12 employment19 and criminality.10 Previous research concluded that attitudinal factors such as drug users' treatment readiness and motivations are closely associated with their treatment/service engagement.20 To address the issue of community treatment underutilization and improve recovery outcomes among Chinese heroin users, Hser et al.21 adapted the Strengths-Based Case Management Model18 into a recovery management intervention (RMI) to implement in Shanghai, China. In that study, the RMI was reported to improve utilization of MMT and enhance recovery outcomes, as seen in higher employment rates and lower criminal activities. However, the mechanisms between the RMI, drug users' attitudes toward treatment and services, their MMT and wraparound service utilization and their recovery outcomes remain unclear.
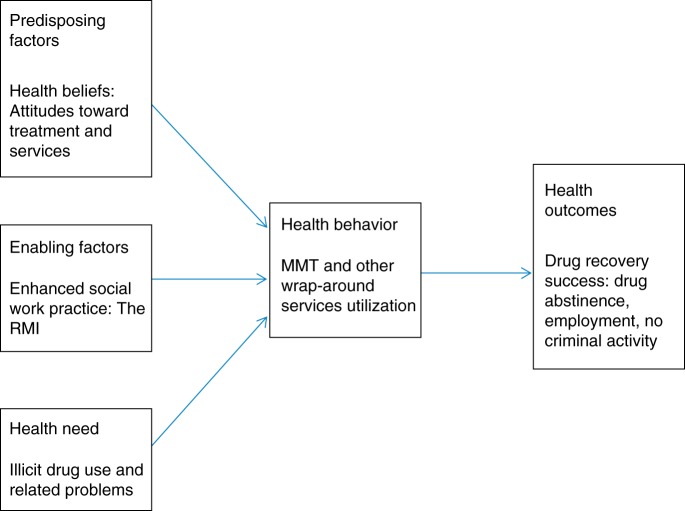
The purpose of this study is to apply the Andersen's Behavioral Model of Access to Care22,23 to investigate the relationships between drug users' attitudes toward service, service use and recovery. Figure 1 summarizes the basic concepts of the theoretical framework and our study hypotheses derived from it. Andersen's Model suggests that service utilization and health outcomes are determined by three dynamics: predisposing factors (demographic characteristics such as age, gender, ethnicity, education, health knowledge and beliefs), enabling factors (personal and community resources such as income, health insurance, social support, available services, provider-to-client ratio, etc.) and health needs (individual's evaluated health status such as diagnoses, stage, severity and symptoms of illnesses). Our study hypothesizes that an enabling factor (the RMI) will improve drug users' health outcomes (recovery indicators such as employment, drug use and criminal activities) through the mediation effect of enhanced predisposing characteristics (attitudes toward treatment and services) and health service use (community-based MMT and wraparound service utilization) among heroin users are released from compulsory rehabilitation in China.
Fig. 1.
Andersen's Behavioral Model of Access to Care and study hypotheses.
Methods
Secondary analyses were conducted with data from an intervention study entitled ‘Reducing HIV/AIDS and Drug Abuse among Heroin Addicts Released from Compulsory Rehabilitation in China’. During 2009–10, 100 Shanghai heroin users who met the DSM-IV criteria of heroin dependence, had no severe mental health illness and were willing to enroll in MMT upon release from compulsory rehabilitation, participated in the intervention study. A computer-generated randomization sheet was used to randomly assign participants to either a Standard Care condition (n = 50) or an RMI condition (n = 50). The RMI features intense social work contacts with drug users and their family, weekly assessment of their strengths and objectives, frequent urine testing and expedited referrals to MMT and other community services (Appendix I). The RMI lasted 12 weeks and was implemented by the Shanghai Zi-Qiang Social Services in two Shanghai districts, Yangpu and Hongkou. These two districts represent urban regions with high and low resources, respectively. Yangpu has the highest incomes and therefore a better community service infrastructure. Hongkou is among the districts with low incomes and community resources. Participants were surveyed at baseline and at 3 months; service records from their social workers throughout the study period were also collected. The intervention study and the secondary data analysis received approval from the Institutional Review Board at the University of California, Los Angeles.
Study measures
Group is a binary variable representing participants' study condition assignment.
Three likert (1–5) subscales were extracted from the Client Evaluation of Self and Treatment20 to reflect participants' treatment readiness and motivation: (i) desire for help, (ii) treatment readiness and (iii) pressure for treatment from family and others.
Service utilization was extracted from social worker service records and captured by three variables: (i) number of assessments, (ii) number of referrals and (iii) number of services/treatments utilized.
Recovery success of the participants was indicated by summing the three following variables from the service records into one ordinal level variable (0 = not successful, 1 = somewhat successful, 2 = successful, 3 = very successful): (i) arrest (not arrested = 1, arrested = 0); (ii) urine result (negative = 1, positive = 0); (iii) employment status (employed = 1, unemployed = 0).
Demographic information such as residential district, gender, age, education, marital status, living arrangement, employment history and drug-related problems such as arrest history, medical problem, mental health problem, age of first use, years of use, injection drug use and type of drug used were captured with the commonly used Addiction Severity Index (ASI).24
Latent variable modeling
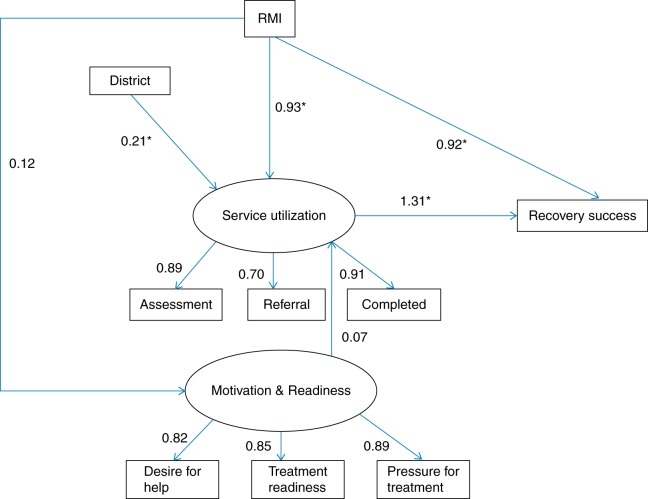
This study utilized a structural equation modeling (SEM) approach to investigate the relationships between drug users' reported motivation and readiness for treatment services, their utilization of these resources and their recovery outcomes. SEM enables us to (i) test more complicated models, such as models that involve both direct and indirect effects and (ii) conduct analyses of both observed and unobserved variables simultaneously.25 Figure 2 shows the path model representing the hypothesized relationships. EQS6.2 was used to test the model. A square represents a single observed variable and a circle represents a latent factor that is indicated by multiple observed variables. An arrow indicates the direction of the hypothesized relationship. A standard path coefficient was estimated for each path in the model: the higher the coefficient, the larger the association. Maximum likelihood methods with a robust correction (Method = ML, ROBUST)26 were used to estimate every path using P < 0.05 as the criterion. The goodness of fit of the model was evaluated with the fit indexes, including Bentler–Bonett non-normed fit index and the comparative fit index: 0.95 or higher is considered a good fit.
Fig. 2.
Effect of the RMI on drug user's service utilization and community recovery.
Results
Baseline characteristics
As reported by Hser et al.,21 the RMI and the standard care condition showed no statistically significant differences at intake in terms of demographic characteristics, including gender ratio, mean age, average years of education, marital status, living conditions after release and past employment history. This study took participants' residential district into consideration and included the variable in the path model as a covariate. Although there were equal numbers of participants in the experimental and the control groups within each participating residential district, Yangpu had almost twice as many total participants as Hongkou, suggesting differences in service capacity and infrastructure.
Participants also did not show meaningful differences in any of the seven ASI subareas, including alcohol, drug, employment, family, legal, medical and psychiatric needs.21 To look more thoroughly for potential confounders regarding participants' drug-use severity and other related problems, this study explored several representative ASI items (Table 1). The two study conditions did not show any significant difference on these items at baseline. Age of first drug use was 27.9 (SD = 7.5), average years of drug use was 10.6 (SD = 9.1) and ∼7% injected drugs within 30 days before their last arrest. Opiates are the primary drug of choice for the participants (73.7%); 9% of them indicated usage of methamphetamine within 1 month before their last arrest and methadone usage was 6%. The majority (93.7%) had past substance abuse treatment experiences. In terms of drug-related problems, 34% of the participants had been arrested in the past for reasons other than drug offenses, 13.1% reported medical problems 30 days before the baseline survey and 33% experienced mental health problems in the same period.
Table 1.
Drug use severity and other related issues at intake, by group
| Experiment (n = 50) | Control (n = 50) | Total (n = 100) | |
|---|---|---|---|
| Arrest history (other than drug offense), % | 32 | 36 | 34 |
| Medical problems, past 30 days, % | 10 | 16.3 | 13.1 |
| Mental health problems, past 30 days, % | 40 | 26 | 33 |
| Drug use history | |||
| Age of first use (SD) | 28 (8.1) | 27.8 (7.0) | 27.9 (7.5) |
| Years of use (SD) | 10.5 (8.6) | 10.7 (9.7) | 10.6 (9.1) |
| Injection in past 30 days, % | 8.3 | 6 | 7.1 |
| Drug use, past 30 days, % | |||
| Heroin/opiates | 72 | 75.5 | 73.7 |
| Methadone | 6 | 6 | 6 |
| Methamphetamine | 10 | 8 | 9 |
| Sedatives | 0 | 4 | 2 |
| Other | 4 | 4 | 4 |
| Ever had alcohol/drug treatment, % | 93.6 | 93.8 | 93.7 |
Treatment readiness and motivation
The RMI group showed slight increases over 3 months in all three subscales of the treatment motivation and readiness scale extracted from the Client Evaluation of Self and Treatment21 assessment: desire for help (25.7–26.2), treatment readiness (30.5–30.9) and pressure for treatment (30.9–31.5). At the same time, their standard care group counterparts' desire for help declined (25.4–25.2) as did pressure for treatment (31.5–30.7) over the same period. None of the changes were statistically significant (Table 2).
Table 2.
Client attitudes toward treatment and services at intake and 3-month follow-up, by group
|
Baseline (n = 100) |
3-month FU (n = 94) |
|||
|---|---|---|---|---|
| Experiment (n = 50) | Control (n = 50) | Experiment (n = 48) | Control (n = 46) | |
| Treatment motivation and readiness (10–50) | ||||
| Desire for help, mean (SD) | 25.7 (5.5) | 25.4 (4.3) | 26.2 (5.4) | 25.2 (5.2) |
| Treatment readiness, mean (SD) | 30.5 (4.2) | 29.4 (4.5) | 30.9 (4.5) | 30.0 (5.2) |
| Pressure for treatment, mean (SD) | 30.9 (5.2) | 31.5 (4.5) | 31.5 (6.9) | 30.7 (6.3) |
Service utilization and recovery success
As seen in Table 3, on average, participants in the RMI group received a significantly higher number of assessment services from their social workers regarding employment needs (3.6 versus 0.1), employment skills (2.1 versus 0), financial needs (2.8 versus 1.2), housing needs (0.5 versus 0.1), health needs (2.0 versus 0.5), MMT needs (1.6 versus 0.1) and family and friends relationship needs (4.3 versus 0.5). However, few referrals, less than an average of one referral in most areas, were made to community resources that could meet participants' needs in the listed areas. The only statistical difference was found in referrals made to employment opportunities (0.4 versus 0.2). The RMI group also did not differ significantly from the control group in their actual utilization of financial, medical, housing and settlement resources in the community, but showed a marginal difference in enrollment in the community MMT programs (8% versus 0, P = 0.06). The RMI participants showed a better average score on the composite recovery success variable than participants in standard care (2.2 versus 1.8, P < 0.01).
Table 3.
Service utilization and recovery success at 3 months, by group
| Experiment (n = 48) | Control (n = 46) | Total (n = 94) | |
|---|---|---|---|
| Needs assessment, average # (SD) | |||
| Employment needsa | 3.6 (3.2) | 0.1 (0.2) | 1.9 (2.9) |
| Employment skillsa | 2.1 (2.4) | 0 (0.2) | 1.1 (2.0) |
| Financial needsa | 2.8 (1.9) | 1.2 (0.4) | 2.0 (1.6) |
| Relationship needsa | 4.3 (2.4) | 0.5 (1.0) | 2.4 (2.7) |
| Housing needsb | 0.5 (0.8) | 0.1 (0.2) | 0.3 (0.6) |
| Health needsa | 2.0 (1.9) | 0.5 (0.5) | 1.3 (1.6) |
| Settlement needs | 0.7 (0.7) | 0.5 (0.5) | 0.6 (0.6) |
| MMT needsa | 1.6 (1.9) | 0.1 (0.3) | 0.9 (1.5) |
| Referrals made to, average # (SD) | |||
| Employment opportunitiesc | 0.4 (0.7) | 0.2 (0.4) | 0.3 (0.6) |
| Employment skills training | 0.1 (0.3) | 0 (0) | 0 (0.3) |
| Social security services | 1.1 (0.8) | 0.8 (0.8) | 1.0 (0.8) |
| Housing services | 0.1 (0.3) | 0.1 (0.3) | 0.1 (0.3) |
| Health services | 0.6 (0.5) | 0.5 (0.5) | 0.6 (0.5) |
| Settlement services | 0.5 (0.5) | 0.5 (0.5) | 0.6 (0.5) |
| MMT services | 0.2 (0.6) | 0 (0) | 0.1 (0.4) |
| Services successfully completed, % | |||
| Social security | 81.3 | 80.4 | 80.9 |
| Housing | 10.4 | 6.5 | 8.5 |
| Medical | 43.8 | 50 | 46.8 |
| Settlement | 45.8 | 52.2 | 48.9 |
| MMT | 8.3 | 0 | 4.3 |
| Recovery success, # (SD)b | 2.2 (0.7) | 1.8 (0.6) | 2.0 (0.7) |
aSignificant main effect of group (P < 0.001).
bSignificant main effect of group (P < 0.01).
cSignificant main effect of group (P < 0.05).
Path model
As shown in Figure 2, the RMI did not show significant impact on participants' changes over time in motivation and readiness to participate in treatment/services. This attitudinal factor was also not related to clients' actual treatment and service utilization. Participants' residential district, on the other hand, was found to be strongly associated with their treatment and wraparound service utilization (standardized path coefficient = 0.21, P < 0.05). Controlling for the effect of residential district, the RMI still showed a strong effect on participants' service utilization (standardized path coefficient = 0.93, P < 0.05). More service and treatment utilization then led to significantly better recovery success in the RMI group (standardized path coefficient = 1.31, P < 0.05). In addition to this mediated process, the RMI also showed a direct effect on participants' recovery success (standardized path coefficient = 0.92, P < 0.05). The goodness-of-fit indexes are satisfactory (CFI = 0.96 and the Bentler–Bonett non-normed fit index = 0.94, as our analyses detected data non-normality).27
Conclusions
Main findings of this study
The RMI was able to increase drug users' service utilization (i.e. MMT and other wraparound services) in the community, and then subsequently led to greater recovery success (i.e. participants were less likely to be arrested, less likely to relapse and more likely to be employed). The RMI was also found to directly improve drug users' recovery. The intervention did not improve participants' attitudes toward treatment and services.
What is already known on this topic
According to Andersen's Behavioral Model of Access to Care,22,23 an enabling factor in the community will increase clients' access to care, and therefore improve their health outcomes. Past empirical research shows that clients' self-rated attitudes toward treatment and service serve as proxies of their actual engagement in treatment and services and changes during recovery and recovery outcomes.20 Previous evidence also demonstrates that strengths-based case management is effective in improving clients' treatment and wraparound service utilization.18 Employment status, drug use and involvement in criminal activities are recovery outcomes often found to be positively associated with intense case management and enhanced service utilization.10,12,19
What this study adds
Key findings from the path analysis were in accordance with the Andersen's Behavioral Model of Access to Care and empirical research about the effect of case management on access to care and health outcomes, but did not support the association between clients' attitudes toward treatment services and their actual usage. One interesting finding is that the RMI had a direct effect on participants' recovery success. We speculate that intense social work contacts, including frequent urine testing, would have served as a strong deterrent to illicit drug use and other criminal activities. Frequent communications also might have increased social workers' understanding of clients' recovery needs and clients' exposures to available services and resources.
For example, we found a marginal effect of the RMI on MMT enrollment. The most important criterion for MMT referral is the detection of relapse to drugs. Approximately 8% of the participants from both study conditions relapsed at 3 months, but only the RMI participants were enrolled in MMT. Significant effects of the RMI were found in seven out of eight needs assessment areas (all except settlement needs). We also found a significant difference across groups in referrals made to employment opportunities and participants' employment rates at 3 months, which had been identified as the most important milestone in drug users' recovery.21 Future endeavors are needed to confirm what components of the intervention caused this direct effect on drug users in recovery so that we can strengthen these components and add them to routine social work practice in China.
Possible explanations for the non-significant difference in MMT enrollment is that the urine positive rate was still low at 3 months for most drug users in recovery and the limited sample size did not have enough power to detect the real difference. The current routine with drug users is to provide settlement services that are standardized for all drug users returning from compulsory rehabilitation; this includes standard filing procedures in the community to obtain regular resident IDs, employment IDs and basic welfare.28 This may explain why >80% of the participants received social security assistance in both study conditions. The reason why increased needs assessment did not translate to more referrals and service use may lie in the lack of relevant resources in the community.
For example, there were no referrals made to services that could help with participants' relationship needs simply because there were no such services available. Since social work and drug users' community recovery are both new in China, there may not be many community-based resources that social workers can access. There could also be a lack of coordination between social work agencies and other community sectors. More research is needed to investigate how to make more community resources available to drug users and how to improve current referral and follow-up mechanisms to enable better access to community resources.
The significant impact of residential district on participants' treatment and service utilization suggested regional differences. Besides the differences in economies, infrastructures and community resources, differences may lie in the two districts' social work workforce professionalism, such as the training background of social workers and the ratio of participants to social workers. Since social work is a fairly new field in China, future research will inevitably need to include explorations of regional differences as well as how the social work workforce develops regionally.
Limitations and implications
The sample size was 100, rendering small-to-medium power in the context of multivariate modeling. Some of the scales were being used for the first time in China and had not been validated with the Chinese drug-using population. Some measurement errors may exist. A 3-month follow-up period was relatively short for monitoring recovery outcomes. Regional variation in China is large, and this study focused only on Shanghai. Therefore, results may lack generalizability and transferability to other localities.
Despite these limitations, this study provides evidence that well-designed case management models such as the RMI have the potential to improve utilization of community drug treatment and other wraparound services, and increase drug recovery success among opiate-dependent individuals in China or other countries that are facing the same challenge of moving from the outdated punitive approach to a community recovery orientation.
Funding
This work was supported by Grant # R21DA025385 (PI: Hser) from the National Institute on Drug Abuse (NIDA). NIDA played no direct role in the design or conduct of the study or in the collection, management, analysis and interpretation of the data and did not review or approve this manuscript. Dr Hser has full access to all of the data in this study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Acknowledgements
The authors thank the Shanghai Zi-Qiang social workers for their support and the clients in China for their participation.
Appendix I
RMI intervention procedures
Besides the Zi-Qiang standard procedures (i.e. monthly contacts, urine tests every 2 months and brief planning sessions after release) with drug users in community recovery, the RMI participants received the following additional procedures:
Case conferences were organized by the social worker staff, involving participants and their family members (if any), immediately after release from rehabilitation. Participants and their family laid out the blueprint for their community recovery goals based on a ‘strengths assessment’ that social workers conducted.
Social workers contacted the RMI participants weekly for 12 weeks and conducted follow-up assessments on their strengths and objectives.
At each contact, a urine sample was collected from the RMI participants on-site to test for opiates. If positive, social worker staff immediately provided referrals to MMT.
Social workers were provided with a list of available community resources to promptly refer clients to relevant wraparound services based on their weekly review of the RMI clients' strengths and objectives.
References
- 1.Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 2013;381:1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ministry of Health of China, Joint United Nations Programme on HIV/AIDS, & World Health Organization. Estimates for the HIV/AIDS Epidemic in China. Beijing, China, 2011. [Google Scholar]
- 3.Narcotics Control Bureau of the Chinese Ministry of Public Security. Drug report on China. Beijing, China, 2011. [Google Scholar]
- 4.Hser YI, Li JH, Jiang HF, et al. Effects of a randomized contingency management intervention on opiate abstinence and retention in methadone maintenance treatment in China. Addiction 2011;106:1801–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin CQ, Wu ZY, Rou KM, et al. Structural-level factors affecting implementation of the methadone maintenance therapy program in China. J Subst Abuse Treat 2010;38:119–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li L, Huang W. A comparison of the existing drug abuse treatment models in China. J Henan Judicial Police Vocational Coll 2008;6(2):81–3. [Google Scholar]
- 7.Yao JL. The new drug legislation and reconstruction of China's drug treatment system. J Chin Police Acad 2008;132:39–44. [Google Scholar]
- 8.Sullivan SG, Wu Z. Rapid scale up of harm reduction in China. Int J Drug Policy 2007;18(2):118–28. [DOI] [PubMed] [Google Scholar]
- 9.State Council AIDS Working Committee Office & UN Theme Group on AIDS in China. A joint assessment of HIV/AIDS prevention, treatment and care in China, 2007.
- 10.Siegal H, Li L, Rapp R. Case management as a therapeutic enhancement: impact on post-treatment criminality. J Addict Dis 2002;21(4):37–47. [DOI] [PubMed] [Google Scholar]
- 11.Vaughan-Sarrazin MS, Hall JA, Rick GS. Impact of case management on use of health services by rural clients in substance abuse treatment. J Drug Issues 2000;30(2):435–63. [Google Scholar]
- 12.Siegal H, Fisher J, Rapp R, et al. Enhancing substance abuse treatment with case management: its impact on employment. J Subst Abuse Treat 1996;13(2):93–8. [DOI] [PubMed] [Google Scholar]
- 13.He HX, Bao YG, Chen LF, et al. Effectiveness of methadone maintenance treatment in preventing HIV/AIDS. Chin J AIDS STDS 2008;14(2):124–6. [Google Scholar]
- 14.Feng WD, Wei QH, Wei L, et al. Effectiveness of methadone maintenance treatment for 556 drug users in Liuzhou. J Public Health Prev Med China 2007;18(4):31–3. [Google Scholar]
- 15.Fan ML, Xu YC. The localization and professionalization of social welfare policy and practice in China. Society 2007;27:119–34. [Google Scholar]
- 16.Zhang Y. Developing social work for drug users recovering in the community. Drug Abuse Stud 2008;62(6):60–5. [Google Scholar]
- 17.Sha W, Wong YC, Lou VW, et al. Career preferences of social work students in Beijing and Shanghai. Soc Work Educ Int J 2012;31(1):4–21. [Google Scholar]
- 18.Hesse M, Vanderplasschen W, Rapp R, et al. Case management for persons with substance use disorders. Cochrane Database Syst Rev 2007;17(4):CD006265. [DOI] [PubMed] [Google Scholar]
- 19.Martin S, Inciardi J. Case management approaches for the criminal justice client. In: Inciardi J. (ed.). Drug Treatment and Criminal Justice. Thousand Oaks, CA: Sage Publications, 1993,84–6. [Google Scholar]
- 20.Joe GW, Broome KM, Rowan-Szal GA, et al. Measuring patient attributes and engagement in treatment. J Subst Abuse Treat 2002;22(4):183–96. [DOI] [PubMed] [Google Scholar]
- 21.Hser YI, Fu LM, Wu F, et al. Pilot trial of a recovery management intervention for heroin addicts released from compulsory rehabilitation in China. J Subst Abuse Treat 2013;44(1):78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersen RM. Behavioral Model of Families Use of Health Services. Research Series No. 25 Chicago, IL: Center for Health Administration Studies, University of Chicago, 1968. [Google Scholar]
- 23.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995;36:1–10. [PubMed] [Google Scholar]
- 24.McLellan AT, Alterman AI, Cacciola J, et al. A new measure of substance abuse treatment. Initial studies of the treatment services review. J Nerv Ment Dis 1992;180(2):101–10. [DOI] [PubMed] [Google Scholar]
- 25.Kim K, Bentler PM. Data modeling: structural equation modeling. In: Green JL, Camilli G, Elmore PB, Skukauskaitie A, Grace E. (eds). Handbook of Complimentary Methods in Education Research. Mahwah, NJ: Lawrence Erlbaum, 2006, 161–75. [Google Scholar]
- 26.Chou CP, Bentler PM. Estimates and tests in structural equation modeling. In: Hoyle RH. (ed.). Structural Equation Modeling: Concepts, Issues and Applications. Thousand Oaks, CA: Sage, 1995,37–55. [Google Scholar]
- 27.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999;6(1):1–55. [Google Scholar]
- 28.Shanghai Zi-Qiang Social Services. Current drug abuse community recovery in Shanghai. In: Presentation at the World Day against Drug Abuse Shanghai, China, 2009. [Google Scholar]