Abstract
Objectives
To characterize outcomes of patients experiencing a fall and subsequent hip fracture while in a nursing home (NH) receiving skilled nursing facility (SNF) services.
Design
Observational study.
Participants
Short-stay fee-for-service Medicare beneficiaries who experienced their first hip fracture during a SNF stay.
Measurements
Outcomes measured in the 90 days after the hip fracture hospitalization included community discharge (with a stay in the community < 30 days), successful community discharge (in the community ≥30 days), death, and institutionalization.
Results
Between 1999 and 2007, 27,305 hip fractures occurred among short-stay nursing home patients receiving SNF care. After surgical repair of the hip fracture, 83.9% of these patients were discharged from the hospital back to a SNF, with most (99%) returning to the facility where the hip fracture occurred. In the first 90 days after hospitalization, 24.1% of patients died, 7.3% were discharged to the community but remained less than 30 days, 14.0% achieved successful community discharge, and 54.6% were still in a health care institution with almost 46.4% having transitioned to long-term care.
Conclusion
SNF care aims to maximize the short-stay patient’s independence and facilitate a safe community transition. However, experiencing a fall and hip fracture during the SNF stay was a sentinel event that limited the achievement of this goal. There is an urgent need to ensure the integration of fall prevention into the patient’s plan of care. Further, falls among SNF patients may serve as indicator of quality, which consumers and payers can use to make informed healthcare decisions.
Keywords: skilled nursing facilities, accidental falls, hip fracture, community discharge
Introduction
Patients are increasingly receiving post-acute care (PAC) in nursing homes under the Medicare skilled nursing facility (SNF) benefit as Federal policies have emphasized the shift of care from hospitals to lower cost care settings.1 In 1982, legislation was passed to mandate a per episode payment approach through the implementation of a hospital prospective payment system.2,3 The execution of this episode-based payment resulted in shorter hospital stays and an increase in hospital discharges to post-acute care.3,4 The patients that are transitioned to a subsequent site of care have continued functional and medical care needs that require skilled care from an interdisciplinary team, including physicians, nurses, occupational therapists, physical therapists, and pharmacists.5 Such patients enter the nursing home for PAC as short-stay patients with the goal of enhancing functional abilities in order to safely return to the community.6
This growth of PAC in nursing homes is requiring facilities to develop and enhance care delivery skills for a patient population that has care objectives different from that of the traditional long-term care residents.7 Short-stay PAC patients are admitted for a temporary stay with a care plan focused on medical recovery and maximizing independence in order to safely return to the community, thereby avoiding long-term institutionalization. On the other hand, the traditional long-term care residents live in nursing homes permanently, and thus their care is focused on maintaining current functional abilities and medical status.
Adverse events among nursing home residents, such as dehydration, catheter associated urinary tract infections, pressure ulcers, and accidental falls have been attributed to poor care.8,9 Twenty-two percent of Medicare beneficiaries experience such an event during a PAC stay, of which more than half (59%) are preventable.9 For short-stay patients, such an event often leads to a rehospitalization,9–11 which may limit their ability to achieve their goal of returning to the community; however, no study has systematically looked at the achievement of this rehabilitation outcome.
Addressing adverse events, such as accidental falls, among short-stay patients can be challenging for nursing homes.6,7 These patients differs from long-term care residents because they are in a new environment, are not well known by the staff, and their care is focused on increasing independence.6,12 In the area of fall prevention, research has demonstrated that the initial transition to the nursing home is when short-stay patients are at greatest risk for falls and subsequent fractures.12 It is estimated that 20% of short-stay patients fall in the first 30 days after nursing home admission and 4.7% of all short-stay patients will experience a hip fracture due to a fall in the nursing home.6,13 Although falls occurring in nursing homes among short-stay patients are common, costly, and can result in a rehospitalization,9 little is known about their outcomes after the subsequent hip fracture hospitalization.
Poor outcomes due to falls and fractures among long-term care residents have been well documented and include morbidity, mortality, and hospitalizations.14–24 However, the different treatment objectives and dissimilar desired outcomes limit the ability to generalize long-term care resident outcomes to short-stay patients. Further, the current mandated public reporting of accidental falls in the United States is limited to long-stay residents and does not include short-stay patients.25 Nursing homes are held accountable when such adverse events occur among long-stay residents, but no such publicly reported data is currently available for short-stay patients.
Therefore, there is a need to understand the impact of falls and fractures in the nursing home on the outcomes of short-stay patients with respect to their treatment priorities—safely returning to the community. Further, identifying whether short-stay patients who experience a hip fracture during a PAC stay are able to return to the community and avoid long-term nursing home placement will provide insight into the long-term outcomes of a nursing home adverse event. Consequently, the objective of this study is to examine the 90-day outcomes of short-stay patients who experience an accidental fall and resulting first hip fracture while in the nursing home and identify the proportion of patients who achieve their PAC rehabilitation goal of returning to the community.
METHODS
The cohort for this study was defined using the 100% Medicare Provider Analysis and Review (MEDPAR) inpatient Medicare Part A claims. Additional data utilized in this study included the US nursing home Minimum Data Set (MDS) 2.0 and the Centers for Medicare and Medicaid (CMS) standard analytic files for Medicare Part A claims, which consisted of inpatient, SNF, hospice, and home health services—plus their Medicare outpatient claims. The inpatient file contained claims on short-term acute hospitalizations, long-term acute care hospitalizations (LTCH), and inpatient rehabilitation hospitalizations, all with their admission and discharge dates. This study was approved by the Institutional Review Boards at Brown University and the University of Southern California
Using a five-year look back period, the cohort included all fee-for-service Medicare beneficiaries 75 years of age and older admitted to a hospital for their first hip fracture between 1999 and 2007 (n=1,386,310). In order to integrate the Medicare administrative data and the MDS 2.0, a longitudinal person-level record of daily Medicare utilization and residential status (i.e. community versus institutionalized in acute care hospital, long term care hospital, psychiatric hospital, inpatient rehabilitation facility, SNF or a non-SNF nursing home) was created using the residential history file methodology to identify the location, healthcare utilization, and date of death.26. Because this longitudinal person-level record relied on Medicare administrative data and MDS 2.0, community was defined as non-institutional Medicare utilization, including home with home healthcare or home with no institutional Medicare service use. The person-level record was used to isolate those patients in a nursing home using their SNF benefit at the time of the fracture and to define the 90-day outcomes of this study occurring after the acute care hip fracture hospitalization. Individuals experiencing their hip fracture while residing in the community (n=1,155,484), on hospice (n=16,101), in a nursing home as a long-term care resident (n=175,275), or in another healthcare institution (n=2,088) were excluded from the study. The remaining 37,362 individuals were short-stay patients in nursing homes utilizing their SNF benefit when the hip fracture occurred.
Under the Medicare SNF benefit, long-term residents can access skilled nursing services after a qualifying acute care hospitalization. However, their care is focused on facilitating the patient’s recovery to their prior level of ability as a nursing home resident, not as a patient striving to get back to the community. Thus, in an effort to capture patients that were likely to return to the community, we excluded long-term care residents using their SNF benefit at the time of the fracture (n=3,986) as well as those that did not have surgery to repair the hip fracture (n=2,787).27,28 Additionally we excluded patients with missing or suspect MDS claims (n=2,418). To ensure complete data for the 90-day follow-up window, those patients admitted to the hospital for their hip fracture after September 30, 2007 (n=866) were also excluded. These exclusion criteria resulted in a final cohort of 27,305 short-stay patients who were in a nursing home receiving SNF level care for another medical condition when they fell and had their first hip fracture.
Outcomes
Discharge status and 90-day outcomes after hip fracture hospitalization were defined using the longitudinal person-level record of healthcare utilization and residential status, defined by the residential history file methodology.26 Acute hospital discharge status, using this methodology, characterized the subsequent location of care (i.e., SNF or a non-SNF nursing home, long term care hospital, psychiatric hospital, inpatient rehabilitation facility, or community) or indicated a hospital death. Using the 90-day window after the acute hospital discharge we determined the proportion of patients who 1) died before community re-entry, 2) were discharged to the community and remained less than 30 days, 3) returned to the community remaining at least 30 consecutive days (termed a successful community discharge), and 4) those who were not discharged to the community. For those patients who never re-entered the community, we defined the type of healthcare setting they were in at 90 days (e.g., nursing home on custodial care, acute care hospital, hospice, skilled nursing facility, other healthcare setting included psychiatric hospital or long term care hospital).
Independent Variables
Information on sociodemographic characteristics including age, race (White, Black, Hispanic, and Other race), and gender were captured from the Medicare Beneficiary Denominator File. The MDS 2.0 was used to characterize prior living status (e.g., living alone) and other patient-level characteristics associated with fall and fracture risk.6,24,29–32 The MDS.20 variables were drawn from the last SNF MDS assessment (e.g., admission assessment, 14-day assessment, 30-day assessment, 60 or 90-day SNF assessment) that was completed prior to the index hip fracture acute care hospitalization. The short-stay resident’s baseline fall risk factors included those variables drawn from the last MDS prior to the acute hip fracture hospitalization such as: a 28-point activities of daily living (ADL) score (higher score indicates greater disability), gait instability, fall history in the last 30 days, incontinence in the last seven days (e.g., bowel, urinary), number of medications, and indicators of certain types of medications received in the last seven days (antipsychotic medications, anti-anxiety medications, anti-depressant medications, and hypnotics).6 Cognition was operationalized using the cognitive performance scale (CPS) where 0=intact cognition and 6=severe cognitive impairment.30,33 Indicators of existing comorbid medical conditions (diabetes, arthritis, Parkinson’s, depression, dementia), presence of any pressure ulcer, urinary tract infection, dizziness, and syncope were also included.
Section T of the MDS 2.0 was used to describe the proportion of SNF patients receiving rehabilitation at the time of the fracture. The assessment provides the total number of days and minutes of therapy received in the last seven days for each of the three rehabilitation disciplines: occupational therapy, physical therapy, and speech therapy. Four rehabilitation variables were created to designate whether or not any rehabilitation was provided and what disciplines administered care (e.g., received any rehabilitation services, received occupational therapy, received physical therapy, received speech therapy).
Patient characteristics from the hip fracture acute hospital stay were captured using the MEDPAR and Part A claims. Variables included a count of the patient’s comorbidities as indicated on hospital discharge records using the Elixhauser comorbidity score,34,35 the type of fracture (femoral neck fracture, petrotrochanteric fracture), the occurrence of any hospital complications during initial hospitalization36 (i.e. postoperative pulmonary failure, postoperative pneumonia, postoperative myocardial infarction, postoperative deep venous thrombosis or pulmonary embolism, postoperative acute renal failure, postoperative hemorrhage, postoperative surgical site infection, postoperative gastrointestinal hemorrhage), any intensive care unit (ICU) use during the index hospitalization, the length of the hospital stay (in days), and the year of the hip fracture.
ANALYSIS
To describe the cohort, the values of continuous variables are presented as means ± standard deviations (SD) or median and intra-quartile range. Categorical variables are presented as proportions. To examine differences in patient characteristics among the four outcomes (e.g., successful community discharge, discharged to the community but remained less than 30 days, died, or still in a healthcare institution), a chi square test was used for categorical variables and ANOVA was used for continuous variables. The distribution of 90-day outcomes was examined and presented as proportions. For those still in a healthcare institution at 90 days, the proportion of patients in each care setting was identified (e.g., nursing home receiving SNF level care, nursing home as a long-term care resident, acute care hospital, hospice, and other settings). Using STATA 12.0, a logistic regression was used to predict successful community discharge, including baseline characteristics that previous research has associated with returning to the community (e.g., prior living status, functional abilities, incontinence, cognitive performance, multiple comorbidities).37–40 Patient characteristics from the hip fracture acute hospital stay were also included in the model. The Huber White correction for clustering the standard errors at the nursing home was included in the model.
RESULTS
Among the 27,305 short-stay patients who experienced their first hip fracture while receiving SNF care, the median number of days this cohort was in the SNF prior to the hip fracture hospitalization was 7 days [interquartile range 3,13]. More specifically, 96.0% of these patients had been in the facility for 30 days or less. Table 1 presents the characteristics of this short-stay patient cohort and stratifies the cohort by their 90-day post-hip fracture hospitalization outcomes. On average, the patients were 84.9 (±5.5) years of age. These individuals were predominantly female (70.8%) and white (94.0%). Twenty-one percent lived alone prior to the index SNF stay. The majority of patients (86%) were receiving rehabilitation services from at least one discipline in the seven days prior to the hip fracture hospitalization; 83.1% had received physical therapy, 74.1% were participating in occupational therapy, and 21.0% were engaging in speech therapy. More than half of these patients were identified as having unsteady gait (51.7%) and 53.4% had fallen in the past 30 days. On average, these patients took 9.7(+4.4) medications while receiving SNF care prior to the hip fracture. The average duration of the hip fracture acute care hospitalization was 6.8 (±4.7) days. Twenty percent of patients experienced an intensive care unit stay and 8.8% experienced hospital complications.
Table 1.
Cohort Baseline Characteristics
| Baseline Status Stratified by 90-Day Outcome Status
|
||||||
|---|---|---|---|---|---|---|
| Cohort (n=27,305) | Successful Community Discharge (n=3,823) | Community Discharge (n=1,982) | In a Healthcare Institution (n=14,898) | Died (n=6,602) | P-Value | |
| SocioDemographics | ||||||
| Age | 84.9(5.5) | 83.9(5.2) | 84.4(5.4) | 84.8(5.5) | 85.6(5.6) | <0.001 |
| Female | 70.8% | 77.4% | 69.3% | 74.3% | 59.5% | <0.001 |
| Race/Ethnicity | ||||||
| White | 94.0% | 94.6% | 93.6% | 93.5% | 95.0% | <0.001 |
| Black | 3.9% | 3.3% | 4.3% | 4.3% | 3.3% | <0.001 |
| Hispanic | 0.8% | 1.0% | 0.8% | 0.9% | 0.6% | <0.05 |
| Other Race | 1.0% | 1.0% | 1.1% | 1.0% | 0.9% | NS |
| Lived Alone Prior to SNF Admission | 21.0% | 26.2% | 23.4% | 20.4% | 18.7% | <0.001 |
| Baseline status from MDS prior to hip fracture | ||||||
| Receipt of Rehabilitation during Index SNF stay | ||||||
| Any Rehabilitation | 86.4% | 91.2% | 89.8% | 85.9% | 83.9% | <0.001 |
| Occupational Therapy | 74.1% | 80.7% | 78.0% | 73.5% | 70.5% | <0.001 |
| Physical Therapy | 83.1% | 88.9% | 86.8% | 82.3% | 80.4% | <0.001 |
| Speech Therapy | 21.0% | 16.6% | 18.0% | 22.0% | 22.3% | <0.001 |
| Functional and Medical Status | ||||||
| ADL status (0–28 point scale) | 15.0(5.9) | 14.3(5.7) | 14.7(5.8) | 15.0(5.9) | 15.5(5.9) | <0.001 |
| Gait instability | 51.7% | 50.7% | 50.9% | 51.3% | 53.5% | <0.05 |
| History of falls in last 30 days | 53.3% | 53.3% | 52.8% | 52.8% | 54.4% | NS |
| Medical Conditions indicated on MDS | ||||||
| Diabetes | 21.4% | 19.4% | 19.9% | 22.0% | 21.8% | <0.01 |
| Arthritis | 12.8% | 14.2% | 12.5% | 13.0% | 11.5% | <0.001 |
| Cerebral Vascular Accident | 17.5% | 14.9% | 15.2% | 19.0% | 16.3% | <0.001 |
| Parkinson’s disease | 3.1% | 2.5% | 2.7% | 3.4% | 2.7% | <0.001 |
| Depression | 30.4% | 27.8% | 29.7% | 32.1% | 28.3% | <0.001 |
| Dementia | 15.5% | 10.2% | 13.3% | 16.3% | 17.1% | <0.001 |
| Urinary Tract Infection | 21.4% | 20.6% | 19.0% | 22.3% | 20.4% | <0.001 |
| Bowel Incontinence | 15.4% | 9.9% | 14.1% | 16.3% | 17.1% | <0.001 |
| Urinary Incontinence | 15.6% | 9.9% | 13.4% | 16.7% | 17.1% | <0.001 |
| Presence of a pressure ulcer | 19.7% | 17.0% | 19.9% | 18.6% | 23.5% | <0.001 |
| Medications | ||||||
| # of Medications | 9.7(4.3) | 10.0(4.5) | 10.1(4.4) | 9.5(4.3) | 9.8(4.3) | <0.001 |
| Anti-Psychotics | 19.1% | 10.7% | 16.5% | 20.5% | 21.7% | <0.001 |
| Anti-anxiety | 20.2% | 18.4% | 18.8% | 20.1% | 22.1% | <0.001 |
| Anti-depressants | 39.6% | 36.5% | 38.4% | 41.4% | 37.5% | <0.001 |
| Hypnotics | 1.5% | 2.1% | 2.0% | 1.3% | 1.6% | <0.001 |
| Symptoms in last 7 days | ||||||
| Dizziness | 1.7% | 2.4% | 2.2% | 1.6% | 1.6% | <0.01 |
| Syncope | 0.7% | 0.9% | 0.6% | 0.6% | 0.7% | NS |
| Cognitive Performance Scale (CPS) | ||||||
| Low CPS (1–2) | 51.1% | 70.0% | 59.0% | 48.2% | 44.3% | <0.001 |
| Moderate CPS (3–4) | 41.1% | 26.0% | 35.0% | 43.7% | 45.9% | <0.001 |
| High CPS (5–6) | 7.8% | 4.0% | 6.1% | 8.2% | 9.8% | <0.001 |
| Hip Fracture Hospital Stay Characteristics | ||||||
| ICU utilization | 20.1% | 16.2% | 20.4% | 17.0% | 29.1% | <0.001 |
| Elixhauser score | 2.7(1.4) | 2.6(1.4) | 2.7(1.3) | 2.6(1.3) | 2.9(1.3) | <0.001 |
| Hospital Length of Stay | 6.8(4.7) | 6.4(4.7) | 6.8(5.1) | 6.4(4.0) | 7.9(5.8) | <0.001 |
| Hospital Complications | 8.8% | 7.0% | 8.4% | 6.9% | 14.4% | <0.001 |
| Petrotrochanteric Fracture | 50.2% | 41.7% | 46.7% | 52.2% | 51.5% | <0.001 |
Note: ADL= activities of daily living with lower score indicating greater independence, ICU= intensive care unit, P-values indicated significant differences across the four outcomes for each independent variable. To examine differences in patient characteristics among the four outcomes a chi square test was used for categorical variables and ANOVA was used for continuous variables.
The short-stay patients that experienced a hip fracture and still achieved successful community discharge were higher functioning as indicated by a lower ADL score, compared to the other outcome groups. Those achieving successful community discharge also had a lower proportion of urinary tract infections, urinary incontinence, and pressure ulcers, and had higher cognitive function as indicated by a lower CPS score. Having a diagnosis of a cerebral vascular accident, depression, and dementia was more common among patients that did not achieve successful community discharge. Furthermore, once admitted to the acute care hospital for the hip fracture surgery, ICU utilization was lower among those who did achieve successful community discharge, compared to the other outcomes.
Upon hospital discharge (not presented in the table), the majority of patients were discharged from the hospital to a nursing home for SNF level care (84.0%), with 99.0% of these patients returning to the same facility where the index fall and hip fracture occurred. Of the remaining 16% of the cohort, 5.0% died in the hospital and 1.6% returned to the community with or without home health, 4.6% were discharged to an inpatient rehabilitation facility, 2.0% to a nursing home without skilled services, 1.3% transitioned to hospice, and the remaining 1.5% were discharged to another healthcare institution (i.e., long term care hospital, psychiatric hospital).
90-Day Outcomes
In the first 90-days after hip fracture hospital discharge 14% achieved successful community discharge (refer to Figure 1). Of the remaining patients, 7% were discharged to the community but failed to remain in the community for 30 days and 24% died before returning to the community. The majority of patients (54.6%) were still in a healthcare setting, of which, almost half (46.4%) had transitioned to long-term care in a nursing home.
Figure 1.
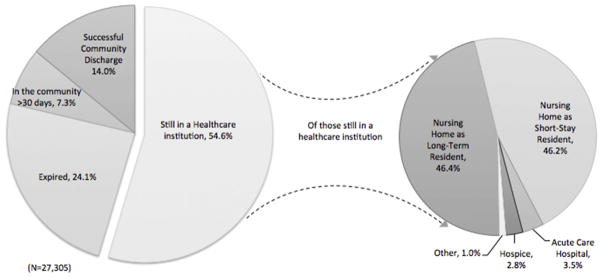
90-Day Outcomes
Note: Other= long term care hospital or psychiatric hospital
Table 2 examines the relationship between patient characteristics and successful community discharge. Younger age, being female (adjusted odds ratio (AOR) 1.40, 95% Confidence Interval (95% CI), 1.29–1.52), and Hispanic (AOR 1.57, 95% CI 1.06–12.34) had a positive association with the outcome. The presence of a pressure ulcer (AOR 0.86, 95% CI 0.78, 0.95), urinary incontinence (AOR 0.79, 95% CI 0.67,0.95), and greater cognitive impairment (AOR 0.34, 95% CI 0.29–0.41) as indicated on the MDS prior to the hip fracture hospitalization were associated with lower odds of achieving successful community discharge after experiencing a hip fracture during SNF care. A greater number of comorbid conditions, as measured by the Elixhauser comorbidity score was associated with a lower odds of achieving the outcome (AOT 0.91, 95% CI 0.89, 0.94). The occurrence of an ICU stay (AOR 0.78, 95% CI 0.71, 0.87) and hospital complications (AOR 0.84, 95% CI 0.73–0.96) were also associated with lower likelihood of achieving the desired outcome.
Table 2.
Predicting Successful Community Discharge
| Odds Ratios | 95% Confidence Interval | |
|---|---|---|
| Age | 0.93 | (0.96–0.97) |
| Female | 1.40 | (1.29–1.52) |
| Race | ||
| White | reference | |
| Black | 0.97 | (0.79–1.18) |
| Hispanic | 1.57 | (1.06–2.34) |
| Other race | 1.05 | (073–1.52) |
| Utilization in SNF prior to fracture | ||
| Any rehabilitation | 1.52 | (1.35–1.71) |
| SNF status prior to hip fracture hospitalization | ||
| Lived alone prior to SNF stay | 1.16 | (1.07–1.26) |
| ADL score (range 0–28) | 1.01 | (0.99–1.01) |
| Urinary tract infection | 0.98 | (0.90–1.07) |
| Any pressure ulcer | 0.86 | (0.78–0.95) |
| Incontinence | ||
| Urinary incontinence | 0.79 | (0.67–0.95) |
| Bowel incontinence | 0.96 | (0.80–1.14) |
| Cognitive performance score | ||
| 0–1 (Low cognitive impairment) | reference | |
| 2–4 (Moderate cognitive impairment) | 0.43 | (0.39–0.46) |
| 5–6 (High cognitive impairment) | 0.34 | (0.29–0.41) |
| Hip fracture hospitalization | ||
| ICU utilization | 0.78 | (0.71–0.87) |
| Elixhauser co-morbidity score | 0.91 | (0.89–0.94) |
| Hospital length of stay | 0.98 | (0.97–0.99) |
| Any hospital complications | 0.84 | (0.73–0.96) |
| Petrochanteric fracture | 0.69 | (0.64–0.74) |
N=27,305; R2=0.056
Note: controlling for year, ADL= activities of daily living, ICU= intensive care unit
DISCUSSION
This study found poor outcomes in a previously unstudied population—short-stay nursing home patients. Due to federal policies that have led to shorter hospital stays and increased transitions to lower cost PAC sites such as a nursing home, short-stay nursing home patients have grown in service use in the United States. 2–4 These patients entered the nursing home for PAC with the goal of returning to the community. Yet, after experiencing a fall and subsequent hip fracture during the SNF stay, only 14.0% of these patients achieved successful community discharge (meaning they remained in the community at least thirty days) after the hip fracture hospitalization. This finding emphasizes the devastating sequelae of a fall among short-stay patients.
To our knowledge, this is the first study that has characterized 90-day outcomes among short-stay nursing home patients in the US who fracture their hip during a SNF stay in which their index nursing home admission is for another diagnosis. With one in seven short-stay nursing home patients returning to the community, this rate of community re-entry is significantly lower (43%) than the community re-entry rate for older adults who experience their first hip fracture while residing in the community, which we identified in a prior study originating from the same data source.41 Further, the proportion of undesirable outcomes (e.g., death and long-term institutionalization) for the short-stay nursing home patients were also higher, when compared to older adults that experienced their first hip fracture while residing in the community.41 Thus, these poor outcomes further emphasize the negative impact falls and fractures have on short-stay nursing home patients whose care is aimed at facilitating a successful community discharge.
The focus of rehabilitation is to maximize functional independence and to facilitate a safe transition back to the community, which includes identifying fall risk factors and implementing preventative strategies in order to limit risk of future falls and re-entry into the healthcare system.42,43 The delivery of high quality PAC relies on an interdisciplinary team of nurses, physicians, pharmacists, and rehabilitation providers (e.g., occupational therapy practitioners, physical therapy practitioners, and speech language pathologists) to work in collaboration to address the medical and functional needs of the patients.5 The patients in this cohort reflected the common fall risk factors, including the presence of chronic conditions, polypharmacy, functional impairment, gait instability, cognitive impairment, and incontinence.45–47 While chronic conditions such as a diagnosis of Dementia or having a history of a CVA cannot be altered, the recognition by the interdisciplinary team that a patient with such diagnoses fits the fall risk profile can facilitate early identification, screening, and implementation of preventative strategies within the care team. To address polypharmacy, the nurses can work collaboratively with the physician and pharmacist to reconcile medications and minimize fall risk.46 Similarly, depression was common among this cohort and is a diagnosis that can be addressed within the PAC setting by the interdisciplinary team through early recognition of signs and symptoms, screening, and treating as appropriate.38,48 Regrettably, among this cohort, the majority (86.4%) of patients were in fact receiving PAC rehabilitation when they fractured their hip, yet the fall and resulting hip fracture occurred. Addressing fall risk factors, such as functional impairment, gait instability, and developing compensatory strategies for managing incontinence and other chronic conditions are within the scope and objective of PAC rehabilitation.48,49 These findings highlight the need for future research that examines how the interdisciplinary team collaborates in PAC to deliver high quality care and prevent adverse events among short-stay patients.
Research has documented significant gaps in the delivery and documentation of effective fall prevention care processes among high fall risk long-term nursing home residents.50,51 While there is a strong and growing evidence-base of PAC interventions that decrease fall and fracture risk,52–60 the extent to which such interventions are integrated into the PAC plan of care by the interdisciplinary care team is unclear. The findings of this study underscore the long-term impact of falls among short-stay patients and the urgent need to ensure the delivery of high quality fall prevention strategies. However, the ability to examine the delivery of such care processes at the population-level is in its infancy. The Medicare Administrative data used in this study does not capture whether or not such interventions were delivered as part of the PAC plan of care. Nor, does the current data provide information about the collaborations of the interdisciplinary team. Data sources that capture this level of detail, such as electronic health records and clinical registries, are in the nascent stages, particularly for PAC and long-term care.
Therefore, in order to improve the quality of PAC care and prevent adverse events, the next logical step is to build the research in this area including, the development of care process measures to assess which rehabilitation practices are associated with positive outcomes, particularly in the context of the broader interdisciplinary team. Such measures would provide the foundation for quantifying the degree to which fall prevention is integrated into the plan of care, which disciplines are involved, and how care varied by region.51 PAC providers can use these measures to engage in targeted quality improvement initiatives aimed at preventing falls and achieving optimal patient outcomes, thereby aligning with the priorities of healthcare reform.61 Finally, research efforts in the area of fall prevention for short-stay residents can lay the foundation for examining interdisciplinary team collaborations, defining care processes, and evaluating prevention efforts for other adverse events.
Limitations
As with any secondary data analysis utilizing administrative data, there are limitations to this study. Information detailing the SNF stay prior to the hip fracture hospitalization was restricted to the data available in the MDS assessments. As a result, there was no variable indicating the primary admitting diagnosis for the index SNF stay during which time the hip fracture occurred. There is also the possibility of inaccurate collection of the data represented in the MDS. Past studies have raised concerns regarding the accuracy and completeness of the MDS.62–64 For example, the diagnosis section of the MDS directs the assessor to only select the diseases relevant to the current MDS assessment. This may lead to under reporting of chronic conditions a patient may have. Therefore, because this study relied on the MDS for baseline patient characteristics, it is possible that there was underreporting of independent variables. Yet, despite these data limitations, the approach used in this study provided an opportunity to examine short-stay SNF patients’ outcomes after the subsequent acute hospitalization. Future research will require either primary data collection or other data sources to ensure the accurate and complete collection of relevant data in the examination of patient outcomes.
This study was not able to capture information regarding the healthcare providers’ clinical decision-making regarding which patients received PAC rehabilitation in the nursing home and those that did not at the time of the hip fracture. We were also unable to capture the types of interventions that were provided by members of the interdisciplinary team and consequently, we could not determine whether or not fall prevention was integrated into the plan of care. Moreover, the data did not capture the circumstances of the fall events that resulted in the hip fracture or information detailing the nursing home environment (e.g., wet floors) that may have contributed to the fall event. Our data was part of a larger study and as a result was limited to those individuals 75 years of age and older and thus may not be generalizable to those younger individuals that experience a fall and hip fracture during a PAC stay in a nursing home. Additionally, the longitudinal person-level record of healthcare utilization and residential status used to operationalize the outcomes after the index hip fracture hospitalization was limited to MEDPAR files and MDS assessments for those returning to a nursing home. Therefore, we are unable to capture information about non-Medicare services received in the community or distinguish between discharges to assisted living facilities or a private residence. Even with these limitations, to our knowledge this is the first study to describe the outcomes of short-stay patients who fall and experience their first hip fracture during a SNF stay in the US.
CONCLUSION
Only 14.6% of short-stay nursing home patients achieved successful community discharge, this emphasizes the devastating impact of a fall with injury during a SNF stay. Substantial evidence has documented the high risk of falling upon admission to a nursing home6,13 and the interventions that mitigate that risk.14–24 Unfortunately, it is not clear to what extent these preventative interventions are provided during a PAC stay in a nursing home. The poor outcomes identified in this study underscore the need to enhance the delivery of fall prevention efforts and ensure evidence-based approaches are an integral part of the short-stay patients’ plan of care. Currently, nursing homes are only mandated to report on accidental falls among long-stay residents. However, the recent passage of the Improving Medicare Post-Acute Care Transformation (IMPACT) Act of 2014 has included major falls with injury as a potential quality measure, thus SNFs and other post-acute care settings may be required to begin publicly reporting falls among their post-acute care patients.65 As the emphasis on provider accountability for patient outcomes expands throughout the healthcare system, nursing home providers must strive to deliver high quality care to short-stay patients. Thus, to achieve desired short-stay patient outcomes, fall prevention interventions will need to be a fundamental part of skilled care in nursing homes.
Acknowledgments
Funding Acknowledgements: This research was supported by the Shaping Long Term Care in America Project funded by the National Institute on Aging (1P01AG027296), the Agency for Healthcare Research and Quality (AHRQ) National Research Services Awards (NRSA) (5T32HS000011-24), and The Rehabilitation Research Career Development (RRDC) Program, National Center for Medical Rehabilitation Research (NICHD), National Institutes of Health (K12 HD055929).
Biographies
Dr. Mor is affiliated with the Warren Alpert School of Medicine at Brown University. He is also an active member of the Board of Directors of PointRight (formerly LTCQ, Inc.) an information services company in the long term care industry that markets long term care providers’ quality ranking information with the mission of improving quality of care in the overall industry. Customers include individual nursing homes and nursing facility chains, liability insurers, state governments and law firms. Since the 2nd quarter of 2003 DR. Mor has been compensated for attending quarterly board meetings.
Dr. Mor was one of 4 original founders of LTCQ and continue to be a stockholder in the company. At its inception, the company licensed intellectual property from Brown and an agreement between LTCQ and Brown was negotiated and continues to be in effect such that LTCQ provides Brown a percentage of annual earnings.
Footnotes
Conflicts of Interest: Drs. Gozalo and Teno, are affiliated with the Warren Alpert School of Medicine at Brown University none of these relationships pose a conflict of interest or potential conflict of interest. Dr. Bynum is affiliated with Dartmouth Medical School & Dartmouth Institute for Health Policy and Clinical Practice neither of these relationships pose a conflict of interest or potential conflict of interest. Dr. Leland was affiliated with the Warren Alpert School of Medicine at Brown University at the time of the study and is now affiliated with the Division of Occupational Science and Occupational Therapy in the Herman Ostrow School of Dentistry & Davis School of Gerontology at University of Southern California, none of these relationships pose a conflict of interest or potential conflict of interest. Dr. Christian was affiliated with Brown University at the time of this study and now is employed by Abt Associates, neither of these relationships pose a conflict of interest.
Financial Disclosures: No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated.
The potential scientific conflict of interest between his role at PointRight and his externally funded and unfunded research as a Brown Professor revolves around the fact that his own research and publication includes the creation, testing and validation of various measures related to the quality of care provided in long term care facilities. Dr. Mor’s NIA grants incorporate such measures in testing the effect of states’ policies on the quality of care facilities provide. It might be perceived that my publications and reports regarding approaches to measuring long term care quality could be influenced by his financial interest in PointRight. However, the company does not support any current or ongoing research in which Dr. Mor is engaged. In the past, whenever there has been the possibility of a joint effort with PointRight, Dr. Mor has played no role in negotiating the contractual relationship, leaving this to senior staff at the Center for Gerontology and Health Care Research. Dr. Mor anticipates that this “arms length” arrangement will continue in the future. Furthermore, all research Dr. Mor has done that is related to the development of new measures of long term care quality are published in some form with the code and definitions of these measures totally available in the public domain or consistent with the terms of the research contract under which the research was produced.
PointRight does not support any students or research staff who are under my administrative control under any form of contract (the annual proceeds from the licensing arrangement between PointRight and Brown does devolve to the Gerontology Center which is free to use those funds for various purposes and Dr. Mor has no control over those funds). There are no plans for PointRight to support students or fellows at Brown. Indeed, they have developed their own research team which periodically attends open research meetings we have at Brown to which other area researchers are also invited to discuss research in long term care.
NaviHealth
NaviHealth is a new company that was founded by principals in the private equity firm, Welsh, Carson, Anderson and Stowe. Before NaviHealth was founded, Dr. Mor advised a senior member of Welsh, Carson about the workings of the post-acute sector in the US, the volume of the sector and the various actors in it and particularly what types of services were most needed by the major players in the health care field, the managed care companies and the hospitals. Once NaviHealth was founded, Dr. Mor was asked to serve as the Chair of a Scientific Advisory Committee to advise the company about the way in which they are bringing together organizational assets, clinical services and technology to improve patient quality and reduce post-acute costs. As part of the contract, which went into effect August 1, 2012, Dr. Mor is compensated for his role as the Chair of the Scientific Advisory Committee as well as for his separate consultation to the CEO and Chief Medical Officer. In return for his engagement with the company in these roles, he was awarded a contingent equity position in the company amounting to approximately .1% of the outstanding shares. At present this has no value, but it could have value, depending upon the performance of the company.
This activity is not in conflict with my research, although it could be perceived by the scientific community that his research on the nursing home and post-acute industry could be biased by his relationship with NaviHealth. I will declare this potential conflict in all relevant research manuscripts and to the NIH upon submission of grant proposals related to long term care and the post-acute care system.
NaviHealth does not provide funding or support for my Brown based research program. There are no funds made available to support graduate students or post-doctoral fellows. He has and continues to provide the annual disclosure to his students and fellows the fact that he is consulting with NaviHealth.
HCRManorcare
For the past 2 years Dr. Mor has been serving as the Chair of the Independent Quality Committee to this 280 facility proprietary nursing home chain. On a quarterly basis Dr. Mor and two of his colleagues meet with senior leaders of the firm and review their efforts to improve their quality review systems, personnel training in quality issues and how the company measures their performance with respect to the quality of care provided the patients they serve. The company gets the benefit of Dr. Mor’s extensive knowledge of long term care quality and its measurement and his advice on where to place their priorities. He is compensated for serving this role and devotes 6 days a year to the effort.
To date, this relationship has not had any relationship with his research program, although there may be instances in which HCRManorcare clinical staff and leadership will assist with his research colleagues at Brown in recruiting their facilities and/or staff to participate in funded research projects.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Medicare Payment Advisory Commission (MEDPAC) Report to the Congress: Medicare Payment Policy. Washington, DC: Mar, 2012. p. 443. [Google Scholar]
- 2.Office of the Inspector General. Medicare hospital prospective payment system: How DRG rates are calculated and updated. Aug, 2001. OEI-09-00-00200. [Google Scholar]
- 3.Liu KGB, Harvell J, Stevenson D, Brennan N. Medicare’s post-acute care benefit: Background, trends, and issues to be faced. Office of the Assistant Secretary for Planning and Evaluation U.S. Department of Health and Human Services; 1999. [Google Scholar]
- 4.Cotterill Pg, Gage BJ. Overview: Medicare post-acute care since the Balanced Budget Act of 1997. Health Care Financing Review. 2002;24(2):1–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Whyte J. Rehabilitation Systems of Care: Promoting Research that Addresses Quality Outcomes. American Journal of Physical Medicine & Rehabilitation. 2014;93(10):917–919. doi: 10.1097/PHM.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 6.Leland NE, Gozalo P, Teno J, Mor V. Falls in newly admitted nursing home residents: A national study. JAGS. 2012;60(5):939–945. doi: 10.1111/j.1532-5415.2012.03931.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keeler EB, Kane RL, Solomon DH. Short- and long-term residents of nursing homes. Med Care. 1981;19(3):363–370. doi: 10.1097/00005650-198103000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Morley JE. Adverse Events in Post-Acute Care: The Office of the Inspector General’s Report. J Am Med Dir Assoc. 2014;15(5):305–306. doi: 10.1016/j.jamda.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 9.Office of the Inspector General. Adverse events in skilled nursing facilities: National incidence among Medicare beneficiaries. Feb, 2014. OEI-06-11-00370. [Google Scholar]
- 10.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood) 2010;29(1):57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Unruh MA, Trivedi AN, Grabowski DC, Mor V. Does reducing length of stay increase rehospitalization of medicare fee-for-service beneficiaries discharged to skilled nursing facilities? J Am Geriatr Soc. 2013;61(9):1443–1448. doi: 10.1111/jgs.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rapp K, Lamb SE, Klenk J, et al. Fractures after nursing home admission: incidence and potential consequences. Osteoporos Inst. 2009;20:1775–1783. doi: 10.1007/s00198-009-0852-y. [DOI] [PubMed] [Google Scholar]
- 13.Colon-Emeric CS, Biggs DP, Schenck AP, Lyles KW. Risk factors for hip fracture in skilled nursing facilities: who should be evaluated? Osteoporos Inst. 2002;14:484–489. doi: 10.1007/s00198-003-1384-5. [DOI] [PubMed] [Google Scholar]
- 14.Berry SD, Samelson EJ, Bordes M, Broe K, Kiel DP. Survival or aged nursing home residents with hip fracture. Journal of Gerontology. 2009;64A(7):771–777. doi: 10.1093/gerona/glp019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neuman MD, Silber JH, Magaziner JS, Passarella MA, Mehta S, Werner RM. Survival and functional outcomes after hip fracture among nursing home residents. JAMA internal medicine. 2014;174(8):1273–1280. doi: 10.1001/jamainternmed.2014.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carroll NV, Delafuente JC, Cox FM, Narayanan S. Fall-related hospitalization and facility costs among residents of institutions providing long-term care. The Gerontologist. 2008;48(2):213–222. doi: 10.1093/geront/48.2.213. [DOI] [PubMed] [Google Scholar]
- 17.Beaupre LA, Cinats JG, Jones CA, et al. Does functional recovery in elderly hip fracture patients differ between patients admitted from long-term care and the community? Journal of Gerontology. 2007;62A(10):1127–1133. doi: 10.1093/gerona/62.10.1127. [DOI] [PubMed] [Google Scholar]
- 18.Hoverman C, Shugarman LR, Saliba D, Buntin MB. Use of postacute care by nursing home residents hospitalized for stroke or hip fracture: how prevalent and to what end? J Am Geriatr Soc. 2008;56(8):1490–1496. doi: 10.1111/j.1532-5415.2008.01824.x. [DOI] [PubMed] [Google Scholar]
- 19.Quigley P, Campbell RR, Bulat T, Olney RL, Buerhaus P, Needleman J. Incidence and cost of serious fall-related injuries in nursing homes. Clin Nurs Res. 2012;21(1):10–23. doi: 10.1177/1054773811414180. [DOI] [PubMed] [Google Scholar]
- 20.Eastwood EA, Magaziner J, Wang J, et al. Patients with hip fracture: subgroups and their outcomes. J Am Geriatr Soc. 2002;50:1240–1249. doi: 10.1046/j.1532-5415.2002.50311.x. [DOI] [PubMed] [Google Scholar]
- 21.Hannan EL. Mortality and Locomotion 6 Months After Hospitalization for Hip Fracture: Risk Factors and Risk-Adjusted Hospital Outcomes. JAMA: The Journal of the American Medical Association. 2001;285(21):2736–2742. doi: 10.1001/jama.285.21.2736. [DOI] [PubMed] [Google Scholar]
- 22.Dharmarajan TS, Tankala H, Patel B, Sipalay M, Norkus EP. Outcome in ambulatory status immediately following hip fracture surgery in the acute setting: A comparison of nursing home residents and community older adults. J Am Med Dir Assoc. 2001;2:115–119. [PubMed] [Google Scholar]
- 23.Heinrich S, Rapp K, Rissmann U, Becker C, Konig HH. Service use and costs of incident femoral fractures in nursing home residents in Germany: The Bavarian Fall and Fracture Prevention Project (BF2P2) J Am Med Dir Assoc. 2011;12:459–466. doi: 10.1016/j.jamda.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 24.Chen JS, Simpson JM, March LM, et al. Risk factors for fracture following a fall among older people in residential care facilities in Australia. J Am Geriatr Soc. 2008;56(11):2020–2026. doi: 10.1111/j.1532-5415.2008.01954.x. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Medicare & Medicaid Services (CMS) [Accessed August 29, 2014];Nursing Home Compare. http://www.medicare.gov/nursinghomecompare/search.html.
- 26.Intrator O, Hiris J, Berg K, Miller SC, Mor V. The residential history file: studying nursing home residents’ long-term care histories. Health Services Research. 2010:1–18. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leland NE, Teno JM, Gozalo P, Bynum J, Mor V. Decision making and outcomes of a hospice patient hospitalized with a hip fracture. Journal of Pain and Symptom Management. 2012;44(3):458–465. doi: 10.1016/j.jpainsymman.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neuman MD, Fleisher LA, Even-Shoshan O, Mi L, Silber JH. Nonoperative care for hip fracture in the elderly: the influence of race, income, and comorbidities. Med Care. 2010;48(4):314–320. doi: 10.1097/mlr.0b013e3181ca4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rubenstein LZ, Josephson KR, Robbins AS. Falls in the nursing home. Ann Intern Med. 1994;121(6):442–451. doi: 10.7326/0003-4819-121-6-199409150-00009. [DOI] [PubMed] [Google Scholar]
- 30.Kiely DK, Kiel DP, Burrows AB, Lipsitz LA. Identifying nursing home residents at risk for falling. Journal of the American Geriatrics Society. 1998;46(5):551–554. doi: 10.1111/j.1532-5415.1998.tb01069.x. [DOI] [PubMed] [Google Scholar]
- 31.French DD, Werner DC, Campbell RR, et al. A multivariate fall risk assessment model for VHA nursing homes using the Minimum Data Set. J Am Med Dir Assoc. 2007;8:115–122. doi: 10.1016/j.jamda.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Kearns WD, Fozard JL, Becker M, et al. Path Tortuosity in Everyday Movements of Elderly Persons Increases Fall Prediction Beyond Knowledge of Fall History, Medication Use, and Standardized Gait and Balance Assessments. J Am Med Dir Assoc. 2012;13(7) doi: 10.1016/j.jamda.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 33.Morris JN, Fries BE, Mehr DR, et al. MDS Cognitive Performance Scale. J Gerontol. 1994;49(4):M174–182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 34.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical Care. 1998;31(6):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 35.HCUP. Elixhauser Comorbidity Software. 3.4. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ); 2009. SAS code to calculate Elixhauser’s Comorbidity Index. [Google Scholar]
- 36.Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Annals of surgery. 2009;250(6):1029–1034. doi: 10.1097/sla.0b013e3181bef697. [DOI] [PubMed] [Google Scholar]
- 37.Wang CY, Graham JE, Karmarkar AM, Reistetter TA, Protas EJ, Ottenbacher KJ. FIM motor scores for classifying community discharge following inpatient rehabilitation for hip fracture. PM R. 2013 doi: 10.1016/j.pmrj.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Givens JL, Sanft TB, Marcantonio ER. Functional recovery after hip fracture: the combined effects of depressive symptoms, cognitive impairment, and delirium. J Am Geriatr Soc. 2008;56(6):1075–1079. doi: 10.1111/j.1532-5415.2008.01711.x. [DOI] [PubMed] [Google Scholar]
- 39.Deutsch A, Granger CV, Fiedler RC, et al. Outcomes and reimbursement of inpatient rehabilitation facilities and subacute rehabilitation programs for Medicare beneficiaries with hip fracture. Med Care. 2005;43(9):892–901. doi: 10.1097/01.mlr.0000173591.23310.d5. [DOI] [PubMed] [Google Scholar]
- 40.Landi F, Bernabei R, Russo A, et al. Predictors of rehabilitation outcomes in frail patients treated in a geriatric hospital. J Am Geriatr Soc. 2002;50(4):679–684. doi: 10.1046/j.1532-5415.2002.50162.x. [DOI] [PubMed] [Google Scholar]
- 41.Leland N, Gozalo P, Christian TJ, Teno J, Mor V. Getting home and staying home after hip fracture post-acute care. Gerontologist. 2013;53:553. [Google Scholar]
- 42.Mackintosh S, Hill K, Dodd KJ, Goldie P, Culham E. Falls and injury prevention should be part of every stroke rehabilitation plan. Clinical Rehabilitation. 2005;19:441–445. doi: 10.1191/0269215505cr796oa. [DOI] [PubMed] [Google Scholar]
- 43.Johnston K, Barras S, Grimmer-Somers K. Relationship between pre-discharge occupational therapy home assessment and prevalence of post-discharge falls. J Eval Clin Pract. 2010;16(6):1333–1339. doi: 10.1111/j.1365-2753.2009.01339.x. [DOI] [PubMed] [Google Scholar]
- 44.Rochat S, Monod S, Seematter-Bagnoud L, Lenoble-Hoskovec C, Büla CJ. Fallers in Postacute Rehabilitation Have Worse Functional Recovery and Increased Health Services Use. Journal of the American Medical Directors Association. 2013;14(11):832–836. doi: 10.1016/j.jamda.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 45.Cashin R, Yang M. Medication prescribed and occurence of falls in general medicine inpatients. The Canadian journal of hospital pharmacy. 2011;64(5):321–326. doi: 10.4212/cjhp.v64i5.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guideline for the Prevention of Falls in Older Persons. Special Series: Clinical Practice: American Geriatrics Society (AGS), British Geriatrics Society, and American Academy of Orthopedic Surgeons Panel on Falls Prevention. Journal of American Geriatrics Society. 2001;49(5):664–672. [PubMed] [Google Scholar]
- 47.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. 2012;9 doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Neyens JC, van Haastregt JC, Dijcks BP, et al. Effectiveness and Implementation Aspects of Interventions for Preventing Falls in Elderly People in Long-Term Care Facilities: A Systematic Review of RCTs. Journal of the American Medical Directors Association. 2011;12(6):410–425. doi: 10.1016/j.jamda.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 49.Berggren M, Stenvall M, Olofsson B, Gustafson Y. Evaluation of a fall-prevention program in older people after femoral neck fracture: a one-year follow-up. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2008;19(6):801–809. doi: 10.1007/s00198-007-0507-9. [DOI] [PubMed] [Google Scholar]
- 50.Gama ZAS, Medina-Mirapeix F, Saturno PJ. Ensuring Evidence-Based Practices for Falls Prevention in a Nursing Home Setting. Journal of the American Medical Directors Association. 2011;12(6):398–402. doi: 10.1016/j.jamda.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 51.Wagner LM, Dionne JC, Zive JR, Rochon PA. Fall Risk Care Processes in Nursing Home Facilities. Journal of the American Medical Directors Association. 2011;12(6):426–430. doi: 10.1016/j.jamda.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 52.Taylor JA. The Vanderbilt fall prevention program for long-term care: Eight years of field experience with nursing home staff. JAMDA. 2002;3(3):180–185. [PubMed] [Google Scholar]
- 53.Taylor JA, Parmelee PA, Brown H, Ouslander JG. The falls management program: A quality improvement initiative for nursing facilities. Agency for Healthcare Research and Quality (AHRQ); 2005. [Google Scholar]
- 54.Taylor SL, Saliba D. Improving patient safety in long-term care facilities. Module 3: Falls prevention and management. Student workbook. Rockville, MD: AHRQ Publications; 2012. [Google Scholar]
- 55.Sawka AM, Ismaila N, Cranney A, et al. A scoping review of strategies for the prevention of hip fracture in elderly nursing home residents. PLoS ONE. 2010;5(3):10. doi: 10.1371/journal.pone.0009515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rask K, Parmelee PA, Taylor JA, et al. Implementation and evaluation of a nursing home fall management program. J Am Geriatr Soc. 2007;55(3):342–349. doi: 10.1111/j.1532-5415.2007.01083.x. [DOI] [PubMed] [Google Scholar]
- 57.Neyens JC, Dijcks BP, Twisk J, et al. A multifactorial intervention for the prevention of falls in psychogeriatric nursing home patients, a randomised controlled trial (RCT) Age and Ageing. 2009;38:194–199. doi: 10.1093/ageing/afn297. [DOI] [PubMed] [Google Scholar]
- 58.Neyens JC, Van Haastregt JCM, Dijcks B, et al. Effectiveness and implementation aspects of interventions for preventing falls in elderly people in long-term care facilities: a systematic review of RCTs. JAMDA. 2011;12:410–425. doi: 10.1016/j.jamda.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 59.Choi M, Hector M. Effectiveness of intervention programs in preventing falls: A systematic review of recent 10 years and meta-analysis. JAMDA. 2012;13:188.e113–188e.121. doi: 10.1016/j.jamda.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 60.Taylor JA, Parmelee P, Brown H, Strothers HS, Capezuti E, Ouslander JG. A model quality improvement program for the management of falls in nursing homes. J Am Med Dir Assoc. 2007;8(3):S26–S36. doi: 10.1016/j.jamda.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 61.Berwick DM, Nolan TW, Whittington J. The triple aim: Care, health, and cost. Health Affairs. 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 62.Bates-Jensen BM, Simmons SF, Schnelle JF, Alessi C. Evaluating the accuracy of minimum data set bed-mobility ratings against independent performance assessments: systematic error and directions for improvement. Gerontologist. 2005;45(6):731–738. doi: 10.1093/geront/45.6.731. [DOI] [PubMed] [Google Scholar]
- 63.Mor V, Angelelli J, Jones R, Roy J, Moore T, Morris J. Inter-rater reliability of nursing home quality indicators in the U.S. BMC Health Serv Res. 2003;3(1):20. doi: 10.1186/1472-6963-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Office of the Inspector General. Nursing home resident assessment quality of care. Jan, 2001. OEI-02-99-00040. [Google Scholar]
- 65.Improving Medicare Post-Acute Care Transformation Act of 2014 H.R. 4994.


