Abstract
Aim:
To investigate the effects of calcium and vitamin D supplementation on bone turnover marker levels, muscle strength and quality of life in postmenopausal Chinese women.
Methods:
A total of 485 healthy postmenopausal Chinese women (63.44±5.04 years) were enrolled in this open-label, 2-year, prospective, community-based trial. The participants were divided into group A, B, C, which were treated with calcium (600 mg/d) alone, calcium (600 mg/d) and cholecalciferol (800 IU/d) or calcium (600 mg/d) and calcitriol (0.25 μg/d), respectively, for 2 years. Serum levels of 25-hydroxyvitamin D, parathyroid hormone, β-CTX and P1NP were measured, and the muscle strength and quality of life were assessed at baseline and at 12- and 24-month follow-ups.
Results:
Four hundred and sixty one participants completed this study. Serum levels of 25-hydroxyvitamin D were significantly increased in group C, but not changed in groups A and B at 24-month follow-up. Serum levels of parathyroid hormone, bone turnover marker β-CTX and bone formation marker P1NP were significantly decreased in group C, while serum levels of β-CTX were increased in group A at 24-month follow-up. The participants in group C maintained the grip strength, while those in groups A and B exhibited decreased grip strength at 24-month follow-up. The quality of life for the participants in groups B and C remained consistent, but that in group A was deteriorated at 24-month follow-up.
Conclusion:
Supplementation with calcitriol and calcium modifies the bone turnover marker levels, and maintains muscle strength and quality of life in postmenopausal Chinese women, whereas supplementation with cholecalciferol and calcium prevents aging-mediated deterioration in quality of life.
Keywords: postmenopausal women, cholecalciferol, calcitriol, 25-hydroxyvitamin D, parathyroid hormone, β-CTX, P1NP, bone turnover, muscle strength, quality of life
Introduction
Aging in elderly people, especially in postmenopausal women, is accompanied by reductions in muscle strength, physical performance and quality of life. Several studies have demonstrated that low serum 25(OH)D levels correlate to poor physical performance and decreased physical activity1,2,3,4,5. Although inconsistently, previous studies have suggested that vitamin D supplementation results in less severe functional limitations, fewer falls and fractures and enhanced mental health6,7,8,9,10,11. Huang et al demonstrated that vitamin D supplementation [1200 IU daily if serum 25(OH)D levels are insufficient (from 20 to 29 ng/mL) or 50 000 IU weekly if serum 25(OH)D levels are deficient (<20 ng/mL)] improved quality of life, pain and sleep in individuals with chronic pain12. The positive effects of vitamin D supplementation on muscle strength, physical performance and quality of life have been attributed to the influence of vitamin D on myocyte and neuron metabolism and function13,14,15,16. To the best of our knowledge, relatively few studies have focused on the effects of vitamin D and calcium supplementation on the physical performance and quality of life in Asian populations, especially in the Chinese population. The primary objective of this 2-year prospective trial was to evaluate the effects of calcium supplementation in combination with either cholecalciferol or calcitriol on bone turnover marker levels, muscle strength, physical performance and quality of life in postmenopausal Chinese women in Shanghai.
Subjects and methods
Study subjects
The study design was a 2-year, prospective, open-label clinical trial that was aimed at investigating the effect of calcium (600 mg/d) supplementation in combination with either cholecalciferol (800 IU/d) or calcitriol (0.25 μg/d) on bone turnover marker levels, muscle strength, physical performance and quality of life in postmenopausal Chinese women.
Community-dwelling postmenopausal women were recruited from communities in the Xuhui region of Shanghai. Potentially eligible participants were called by telephone and were persuaded to visit the hospitals in their corresponding districts to be screened based on the inclusion and exclusion criteria. Women who met the following primary inclusion criteria were considered: 1) ambulatory, community-dwelling and postmenopausal; 2) capable of independently completing the tests involved in the study; and 3) normal blood counts, normal results on liver and kidney function tests and normal serum levels of calcium, phosphorus, alkaline phosphatase (ALP), and parathyroid hormone (PTH). The exclusion criteria were as follows: 1) the presence of a disease deemed to affect vitamin D metabolism, such as cancer, hyperthyroidism, diabetes mellitus, primary hyperparathyroidism or pituitary, adrenal or rheumatic disease; 2) vitamin D and/or calcium supplementation within the prior 3 months; and 3) administration of medications that increase or decrease bone, muscle or vitamin D metabolism, including bisphosphonate, raloxifene, calcitonin, parathyroid hormone, hormone replacement drugs, thiazolidinedione, antiepileptics, aromatase inhibitors, and glucocorticoids. A total of 485 healthy postmenopausal Chinese females of Han ethnicity with a mean age of 63.44±5.04 years met the inclusion and exclusion criteria and were enrolled in this study. This study was approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People's Hospital. All of the participants signed informed consent forms prior to entering the study.
Anthropometry
Both at baseline and after 12 and 24 months of treatment, the body weight and height of each participant were measured while they were wearing a light gown and no shoes using a SK-CK Ultrasonic Body Scale. Body mass index (BMI) was calculated as body weight in kg divided by height in m2.
Groups and treatment
The participants were separated into 3 groups: A) supplementation with calcium only, B) supplementation with calcium and cholecalciferol, and C) supplementation with calcium and calcitriol. For 2 years, cholecalciferol (Cholecalciferol, Xingsha Pharmaceuticals Co, Xiamen, China) was administered at 800 IU/d, and calcitriol (Calcitriol Soft Capsules, CP Haier Pharmaceuticals Co, Qingdao, China) was administered at 0.25 μg/d. Each of the subjects received 1 pill/day of Caltrate D (containing 600 mg of calcium and 125 IU of vitamin D3, Wyeth Pharmaceuticals, Suzhou, China) for elemental calcium supplementation. Because Caltrate D contained 125 IU of vitamin D3, group B received 925 IU/d of cholecalciferol in total. All of the subjects were instructed to take the drugs and to perform physical training daily during the 24-month study period.
Serum collection and measurement
Fasting blood samples were collected at baseline and at the 12-month and 24-month follow-ups to measure serum levels of calcium, phosphate, albumin, cholesterol, triglycerides (TG), blood urea nitrogen (BUN), creatinine (Cr), alanine aminotransferase (ALT), aspartate transaminase (AST), γ-glutamyl transpeptidase (γ-GT), ALP, intact PTH (iPTH), beta C-terminal cross-linked telopeptides of type I collagen (β-CTX), amino-terminal propeptide of type I collagen (P1NP), osteocalcin (OC) and 25(OH)D. The serum levels of 25(OH)D, PTH, β-CTX, OC and P1NP were measured using an automated Roche electro-chemiluminescence system (E170, Roche Diagnostic GmbH, Mannheim, Germany). All of the biochemical markers were measured in one batch at the same time point using a single lot of reagents according to both the manufacturer's instructions and specialized laboratory-quality assay procedures. The intra-assay coefficients of variation (CVs) for 25(OH)D were 5.7% at a level of 25.2 ng/mL, 5.7% at a level of 39.9 ng/mL and 5.4% at a level of 65.6 ng/mL. The inter-assay CVs for 25(OH)D were 9.9% at a level of 25.2 ng/mL, 7.3% at a level of 39.9 ng/mL and 6.9% at a level of 65.6 ng/mL. The lower limit of detection of 25(OH)D was 4 ng/mL (10 mmol/L)17. The intra- and inter-assay CVs were 1.4% and 2.9% for PTH, 2.5% and 3.5% for β-CTX, 2.9% and 4.0% for OC, and 2.3% and 2.8% for P1NP, respectively18.
Muscle strength and physical performance measurements
Muscle strength and physical performance were assessed at baseline and at the 12-month and 24-month follow-ups. Handgrip strength was calculated using a Jamar Hand dynamometer (5030 J1, Sammons Preston, Inc, Bolingbrook, IL, USA). Three measurements were recorded from each hand, and the average values of the right and left hands were used for analysis. A chair-rising test was performed as follows: the participants were asked to stand up from a chair with folded arms five times as quickly as possible, and the time required to stand was recorded.
Quality of life assessment
To assess changes in health-related quality of life, a Short Form 36 Health Survey (SF-36) questionnaire was used after being translated into Chinese19. All of the participants were asked to respond to 36 questions, 35 of which are compressed into eight multi-item scales: physical functioning (PF), role-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE) and mental health (MH). The study participants completed the questionnaires both at baseline and after 12 and 24 months of intervention.
Statistical analysis
Statistical analyses were performed using the statistical package SPSS version 19.0 (SPSS, Inc, Chicago, IL, USA). The data were assessed for normality, and data transformation was applied whenever appropriate. Continuous variables are presented as the mean±SD. Data that were not normally distributed are presented as medians and inter-quartile ranges. ANOVA, chi-square tests and appropriate nonparametric tests were used to detect differences in demographic and lifestyle characteristics, health conditions, physical performance, and biochemical marker levels between the groups. These tests were also used to examine differences in absolute changes in physical performance and in biochemical marker levels between baseline and the 12- or 24-month follow-ups. P<0.05 was considered significant.
Results
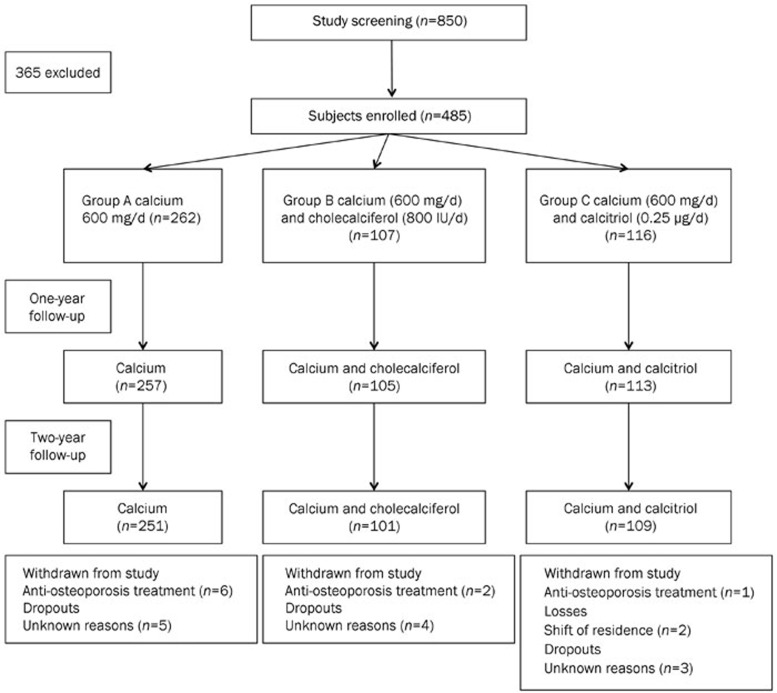
Figure 1 presents a flowchart describing the study. A total of 485 postmenopausal women who presented normal indicators of liver and kidney function and blood calcium and phosphorus levels were included in the study and were separated into three groups. Nine subjects withdrew from the study to receive anti-osteoporosis treatment. Two subjects were lost to follow-up because they changed their addresses. Twelve subjects failed to complete the study for unknown reasons. Ultimately, 461 participants completed the study. At the 12-month and 24-month follow-ups, the serum concentrations of calcium, phosphorous, and PTH and the results of liver and kidney function in the three groups all remained within normal ranges. No obvious adverse events were reported over the course of the study.
Figure 1.
Flowchart describing the study.
Baseline characteristics
The baseline characteristics of the subjects in the three groups are summarized in Table 1. No significant differences were detected in the mean ages of the three groups (63.22±4.90 years, 64.34±4.93 years and 63.35±5.99 years in groups A, B and C, respectively). No significant differences in any of the baseline characteristics were detected between the three groups, except for serum concentrations of calcium, β-CTX, and 25(OH)D, handgrip strength, time to complete the chair rising test and SF-36 questionnaire scores (Table 1). The subjects in group A exhibited higher handgrip strength and SF-36 scores than those in the other two groups. The median serum 25(OH)D level in group C was 20.90 (17.83–27.88) and was higher than that of the other groups, which was 20.03 (16.01–24.15) in group A and 20.63 (16.39–24.45) in group B.
Table 1. Characteristics of subjects at baseline for each group. Continuous variables are presented as the means±SD. Non-normally distributed data are presented as the medians and inter-quartile ranges (in parentheses). bP<0.05 vs group A. eP<0.05 vs group B.
| Characteristic | Group A (n=262) calcium (600 mg/d) | Group B (n=107) calcium (600 mg/d) and cholecalciferol (800 IU/d) | Group C (n=116) calcium (600 mg/d) and calcitriol (0.25 μg/d) |
|---|---|---|---|
| Age (year) | 63.22±4.90 | 64.34±4.93 | 63.35±5.99 |
| Height (m) | 1.54±0.05 | 1.54±0.05 | 1.55±0.05 |
| Weight (kg) | 59.08±9.25 | 58.20±9.34 | 59.50±8.46 |
| BMI (kg/m2) | 24.75±3.36 | 24.54±3.52 | 24.69±3.32 |
| Age at menarche (year) | 15.80±1.71 | 15.40±1.82 | 15.27±1.90 |
| Age at menopause (year) | 50.53±3.29 | 50.22±3.61 | 49.82±3.25 |
| Calcium (mmol/L) | 2.43±0.10 | 2.38±0.08b | 2.40±0.09b |
| Phosphorous (mmol/L) | 1.08±0.11 | 1.11±0.12 | 1.10±1.12 |
| ALP (U/L) | 81.49±20.14 | 82.21±15.11 | 80.18±18.54 |
| BUN (mmol/L) | 4.94±1.21 | 4.81±1.19 | 5.02±1.21 |
| Cr (μmol/L) | 60.45±9.44 | 59.93±9.16 | 59.59±10.30 |
| P1NP (ng/mL) | 52.98 (41.40–66.96) | 55.93 (40.90–70.51) | 52.00 (41.50–72.31) |
| β-CTX (ng/L) | 370.00 (254.00–491.75) | 402.00 (304.00–500.00) | 451.00 (299.00–548.00)e |
| OC (ng/mL) | 17.96 (15.14–21.85) | 19.46 (15.53–22.92) | |
| PTH (pg/mL) | 32.79 (25.77–41.59) | 34.25 (25.79–40.82) | 35.61 (27.58–45.24) |
| 25(OH)D (ng/mL) | 20.03 (16.01–24.15) | 20.63 (16.39–24.45) | 20.90 (17.83–27.88)be |
| Grip strength (kg) | |||
| Left hand | 22.79±4.75 | 20.27±5.30b | 20.06±5.34b |
| Right hand | 24.34±50.2 | 21.60±5.39b | 21.25±4.77b |
| Chair rising test (s) | 7.24±1.94 | 6.18±1.29b | 6.18±1.17b |
| SF-36 | |||
| PF | 95.00 (85.00–95.00) | 80.00 (70.00–90.00)b | 90.00 (75.00–95.00)b |
| RP | 100.00 (100.00–100.00) | 100.00 (50.00–100.00)b | 100.00 (75.00–100.00)b |
| BP | 93.24 (68.82–99.90) | 79.92 (56.61–93.24)b | 81.03 (56.61–99.90)b |
| GH | 72.00 (52.00–80.00) | 60.00 (45.00–70.00)b | 65.00 (54.25–77.90)e |
| VT | 80.00 (70.00–90.00) | 65.00 (50.00–75.00)b | 70.00 (65.00–85.00)be |
| SF | 100.00 (75.00–100.00) | 62.50 (50.00–100.00)b | 87.50 (62.50–100.00)be |
| RE | 99.80 (99.80–99.80) | 99.80 (99.80–99.80)b | 99.80 (99.80–99.80)b |
| MH | 84.00 (76.00–100.00) | 76.00 (68.00–88.00)b | 76.00 (68.00–88.00)b |
PF=Physical Functioning; RP=Role-Physical; BP=Bodily pain; GH=General Health; VT=Vitality; SF=Social Functioning; RE=Role-Emotional; MH=Mental Health.
Changes in serum vitamin D and bone turnover marker levels following the different interventions
Serum levels of β-CTX significantly increased in group A, from 370.00 ng/mL (254.00–491.75) at baseline to 417.00 ng/mL (327.75–535.25) at the 24-month follow-up, whereas serum levels of PTH, P1NP and β-CTX significantly decreased in group C at the 12- and 24-month follow-ups (all P<0.05, Table 2, 4). No differences in serum levels of P1NP or β-CTX were observed between baseline and 24-month follow-up in group B. All of the levels of serum bone turnover markers that were measured were within a normal range.
Table 2. Changes in biomarker levels, physical performance and SF-36 scores in group A. Continuous variables are presented as the means±SD. Non-normally distributed data are presented as the medians and inter-quartile ranges (in parentheses). bP<0.05 vs baseline. eP<0.05 vs 12-month follow-up.
| Baseline (n=262) | 12 months (n=257) | 24 months (n=251) | |
|---|---|---|---|
| Height (m) | 1.54±0.05 | 1.54±0.05 | 1.54±0.05 |
| Weight (kg) | 59.08±9.25 | 59.49±9.85 | 60.44±9.45 |
| BMI (kg/m2) | 24.75±3.36 | 24.99±3.65 | 25.15±3.54 |
| Calcium (mmol/L) | 2.43±0.10 | 2.22±0.10b | 2.31±0.11be |
| Phosphorous (mmol/L) | 1.08±0.11 | 0.94±0.15b | 1.20±0.16be |
| ALP (U/L) | 81.49±20.14 | 75.16±17.68b | 78.89±18.18e |
| BUN (mmol/L) | 4.94±1.21 | 4.67±1.15b | 4.77±1.17 |
| Cr (μmol/L) | 60.45±9.44 | 53.06±9.81b | 58.79±10.96e |
| P1NP (ng/mL) | 52.98 (41.4–66.96) | 55.21 (44.48–67.86) | 52.87 (41.89–66.68) |
| β-CTX (ng/L) | 370.00 (254.00–491.75) | 417.00 (327.75–535.25)b | |
| OC (ng/mL) | 17.96 (15.14–21.85) | 18.81 (16.18–22.89) | |
| PTH (pg/mL) | 32.79 (25.77–41.59) | 34.59 (26.55–42.29) | |
| 25(OH)D (ng/mL) | 20.03 (16.01–24.15) | 19.56 (15.07–23.69) | |
| Grip strength (kg) | |||
| Left hand | 22.79±4.75 | 22.26±4.75 | 21.04±4.18be |
| Right hand | 24.34±5.02 | 23.45±4.98b | 23.41±4.44b |
| Chair rising test (s) | 7.24±1.94 | 7.78±1.98b | 7.82±2.19b |
| SF-36 | |||
| PF | 95.00 (85.00–95.00) | 85.00 (65.00–95.00)b | 85.00 (65.00–91.25)b |
| RP | 100.00 (100.00–100.00) | 100.00 (100.00–100.00) | 100.00 (100.00–100.00) |
| BP | 93.24 (68.82–99.90) | 82.14 (57.72–99.9) | 93.24 (57.72–99.00) |
| GH | 72.00 (52.00–80.00) | 62.00 (50.00–77.00) | 62.00 (47.00–70.00)b |
| VT | 80.00 (70.00–90.00) | 75.00 (50.00–85.00)b | 70.00 (60.00–85.00)b |
| SF | 100.00 (75.00–100.00) | 87.50 (50.00–100.00)b | 87.50 (62.50–100.00)b |
| RE | 99.80 (99.80–99.80) | 99.80 (99.80–99.80) | 99.80 (99.80–99.80) |
| MH | 84.00 (76.00–100.00) | 80.00 (68.00–91.00)b | 80.00 (68.00–88.00)b |
Abbreviations: PF=Physical Functioning; RP=Role-Physical; BP=Bodily pain; GH=General Health; VT=Vitality; SF=Social Functioning; RE=Role-Emotional; MH=Mental Health.
Table 4. Changes in biomarker levels, physical performance and SF-36 scores in group C. Continuous variables are presented as the means±SD. Non-normally distributed data are presented as the medians and inter-quartile ranges (in parentheses). bP<0.05 vs baseline. eP<0.05 vs 12-month follow-up.
| Baseline (n=116) | 12 months (n=113) | 24 months (n=109) | |
|---|---|---|---|
| Height (m) | 1.55±0.05 | 1.56±0.05 | 1.56±0.05 |
| Weight (kg) | 59.50±8.46 | 58.79±8.74 | 58.94±8.84 |
| BMI (kg/m2) | 24.69±3.32 | 24.23±3.24 | 24.35±3.30 |
| Calcium (mmol/L) | 2.40±0.09 | 2.29±0.08b | 2.37±0.09be |
| Phosphorous (mmol/L) | 1.10±1.12 | 1.14±0.16b | 11.8±0.16b |
| ALP (U/L) | 80.18±18.54 | 71.68±21.27 | 90.75±56.53be |
| BUN (mmol/L) | 5.02±1.21 | 5.22±1.12 | 5.54±1.34b |
| Cr (μmol/L) | 59.59±10.30 | 62.94±0.53b | 60.55±13.39 |
| β-CTX (ng/L) | 451.00 (299.00–548.00) | 312.00 (210.00–458.00)b | 358.50 (274.50–476.75)b |
| P1NP (ng/mL) | 52.00 (41.50–72.31) | 41.31 (32.20–55.57)b | 47.73 (35.78–62.29)b |
| PTH (pg/mL) | 35.61 (27.58–45.24) | 29.41 (23.09–36.18)b | 28.13 (19.60–35.02)b |
| 25(OH)D (ng/mL) | 20.90 (17.83–27.88) | 23.16 (18.97–28.42) | 26.44 (21.29–32.29)be |
| Grip strength (kg) | |||
| Left hand | 20.06±5.34 | 20.93±4.52 | 19.85±4.40 |
| Right hand | 21.25±4.77 | 21.98±4.76 | 21.09±4.64 |
| Chair rising test (s) | 6.18±1.17 | 7.06±1.17b | 6.78±2.01b |
| SF-36 | |||
| PF | 90.00 (75.00–95.00) | 90.00 (80.00–95.00) | 85.00 (75.00–95.00) |
| RP | 100.00 (75.00–100.00) | 100.00 (100.00–100.00) | 100.00 (75.00–100.00) |
| BP | 81.03 (56.61–99.90) | 82.14 (57.72–99.90) | 79.92 (57.72–93.24) |
| GH | 65.00 (54.25–77.90) | 62.00 (52.00–77.00) | 60.00 (47.00–72.00) |
| VT | 70.00 (65.00–85.00) | 75.00 (55.00–90.00) | 65.00 (55.00–85.00) |
| SF | 87.50 (62.50–100.00) | 100.00 (75.00–100.00)b | 87.50 (62.50–100.00)e |
| RE | 99.80 (99.80–99.80) | 99.38 (99.80–99.80) | 66.50 (66.50–99.80) |
| MH | 76.00 (68.00–88.00) | 88.00 (76.00–96.00) | 80.00 (60.00–88.00) |
PF=Physical Functioning; RP=Role-Physical; BP=Bodily pain; GH=General Health; VT=Vitality; SF=Social Functioning; RE=Role-Emotional; MH=Mental Health.
In group C, the serum levels of 25(OH)D increased from 20.90 ng/mL (17.83–27.88) at baseline to 26.44 ng/mL (21.29–32.29) at the 24-month follow-up (P<0.05, Table 4). However, serum 25(OH)D levels were not significantly different between baseline and after the intervention in either group A or group B (P>0.05, Table 2, 3).
Table 3. Changes in biomarker levels, physical performance and SF-36 scores in group B. Continuous variables are presented as the means±SD. Non-normally distributed data are presented as the medians and inter-quartile ranges (in parentheses). bP<0.05 vs baseline. eP<0.05 vs 12-month follow-up.
| Baseline (n=107) | 12 months (n=105) | 24 months (n=101) | |
|---|---|---|---|
| Height (m) | 1.54±0.05 | 1.54±0.06 | 1.54±0.07 |
| Weight (kg) | 58.20±9.34 | 58.7±98.1 | 59.14±9.86 |
| BMI (kg/m2) | 24.54±3.52 | 24.57±3.60 | 24.81±3.56 |
| Calcium (mmol/L) | 2.38±0.08 | 2.32±0.09b | 2.35±0.11b |
| Phosphorus (mmol/L) | 1.11±0.12 | 1.14±0.15 | 1.31±0.20be |
| ALP (U/L) | 82.21±15.11 | 74.96±19.27b | 79.27±21.49 |
| BUN (mmol/L) | 4.81±1.19 | 5.08±1.11 | 5.79±1.29be |
| Cr (μmol/L) | 59.93±9.16 | 62.36±10.56 | 62.51±10.60 |
| P1NP (ng/mL) | 55.93 (40.90–70.51) | 53.53 (38.84–66.44) | 55.25 (37.61–72.99) |
| β-CTX (ng/L) | 402.00 (304.00–500.00) | 379.00 (268.25–498.00) | |
| OC (ng/mL) | 19.46 (15.53–22.92) | 18.78 (14.99–24.15) | |
| PTH (pg/mL) | 34.25 (25.79–40.82) | 31.76 (26.06–40.70) | |
| 25(OH)D (ng/mL) | 20.63 (16.39–24.45) | 20.43 (16.04–25.15) | |
| Grip strength (kg) | |||
| Left hand | 20.27±5.30 | 20.45±5.32 | 18.97±5.37e |
| Right hand | 21.60±5.39 | 21.92±4.99 | 19.87±5.52be |
| Chair rising test (s) | 6.18±1.29 | 6.50±1.91 | 6.82±2.54b |
| SF-36 | |||
| PF | 80.00 (70.00–90.00) | 90.00 (80.00–95.00)b | 85.00 (68.75–95.00)e |
| RP | 100.00 (50.00–100.00) | 100.00 (81.25–100.00) | 100.00 (75.00–100.00) |
| BP | 79.92 (56.61–93.24) | 78.81 (56.61–99.9) | 79.92 (45.51–93.24) |
| GH | 60.00 (45.00–70.00) | 61.00 (50.00–75.00) | 55.00 (45.00–65.00)e |
| VT | 65.00 (50.00–75.00) | 75.00 (60.00–85.00)b | 62.50 (50.00–75.00)e |
| SF | 62.50 (50.00–100.00) | 87.50 (75.00–100.00)b | 87.50 (75.00–100.00)b |
| RE | 99.80 (99.80–99.80) | 99.80 (99.80–99.80) | 99.80 (99.80–99.80) |
| MH | 76.00 (68.00–88.00) | 84.00 (72.00–92.00)b | 80.00 (64.00–92.00)e |
PF=Physical Functioning; RP=Role-Physical; BP=Bodily pain; GH=General Health; VT=Vitality; SF=Social Functioning; RE=Role-Emotional; MH=Mental Health.
Changes in muscle strength and physical performance
Muscle strength and physical performance were significantly decreased at the 12- and 24-month follow-ups only in group A, as demonstrated by reduced grip strength in both hands and longer time of completion on the chair rising test. The grip strength of the left hand was 22.79±4.75 kg at baseline and 21.04±4.18 kg after 24 months (P<0.05). The grip strength of the right hand was 24.34±5.02 kg at baseline and 23.45±4.98 kg and 23.41±4.44 kg after 12 and 24 months, respectively (P<0.05). The time of completion on the chair rising test was 7.24±1.94 s at baseline and 7.78±1.98 s and 7.82±2.19 s after 12 and 24 months, respectively (Table 2). The participants in group B exhibited no significant changes in muscle strength or physical performance after 12 months, as measurements of mean handgrip strength and completion times on the chair rising test were comparable with those that were taken at baseline (P>0.05). However, handgrip strength strikingly decreased, and the time of completion on the chair rising test significantly increased from 6.18±1.29 s at baseline to 6.82±2.54 s (P<0.05) at the 24-month follow-up (Table 3). The subjects in group C exhibited no significant changes in handgrip strength, although the completion time on the chair rising test was significantly increased (baseline: 6.18±1.17 s; 12 months: 7.06± 1.17 s; 24 months: 7.78±2.01 s; P<0.05) at both the 12-month and 24-month follow-ups (Table 4).
Changes in quality of life
In the current study, the subjects completed the SF-36 questionnaire to assess changes in health-related quality of life according to eight scales: PF, RP, BP, GH, VT, SF, RE and MH. In group A, the PF, VT, SF and MH scores were significantly decreased after 12 months, and the scores of all of the scales, except for RP, BP, and RE, were significantly reduced after 24 months compared to baseline (all P<0.05, Table 2). The mean PF, VT, SF, and MH scores of the participants in group B were significantly increased after 12 months (P<0.05). The mean PF, GH, VT and MH scores were lower after 24 months than after 12 months (all P<0.05) and were comparable with those at baseline (P>0.05, Table 3). In group C, none of the scores on any of the scales were significantly different after 12 or 24 months compared with baseline (all P>0.05), except for the SF score, which increased from 87.50 (62.50–100.00) at baseline to 100.00 (75.00–100.00) after 12 months (P<0.05, Table 4).
Discussion
Vitamin D deficiency has been recognized as a major public health concern worldwide. Circulating vitamin D3 (cholecalciferol) is predominately synthesized in the skin from a cholesterol derivative, 7-dehydroxycholesterol, under the effect of sunlight and its UV radiation. It is then metabolised in the liver by the enzyme 25-hydroxylase and then in the kidneys by 1-alpha-hydroxylase. Oral administration of vitamin D3, cholecalciferol and its analogues alphacholecalciferol and calcitriol are used for the treatment of vatamin D deficiency. The average serum 25(OH)D level in the current study was 21.86±6.82 ng/mL, which is defined as vitamin D insufficient. It is well known that low serum levels of 25(OH)D are associated with a significant decrease in the absorption of intestinal calcium and may induce secondary hyperparathyroidism, which could potentially stimulate the transformation of pre-osteoclasts into mature osteoclasts and lead to osteoporosis and a consequent increase in the risk of fractures20. Kuwabara et al21 demonstrated that daily supplementation of 200 mg calcium and 800 IU vitamin D3 for one month significantly reduced serum PTH levels compared to daily supplementation of only 200 mg calcium in an institutionalized, elderly Japanese population. Our results indicated that serum PTH levels significantly decreased after supplementation with 0.25 μg/d calcitriol and 600 mg/d calcium for 12 and 24 months. However, the responses of serum PTH levels to cholecalciferol supplementation appear to vary20,22,23. In the present study, no changes were detected in serum PTH levels in subjects who were treated with 600 mg/d elemental calcium and 800 IU/d cholecalciferol. Patel et al24 examined the effect of cholecalciferol on bone metabolism in healthy adult women who ranged in age from 23 to 70 years (mean age 45.3 years). The results revealed that supplementation with 800 IU/d cholecalciferol for 12 months increased serum 25(OH)D levels, whereas no effects on serum PTH or bone turnover marker levels were detected. Serum levels of PTH are also influenced by dietary calcium intake, and the optimal dose of cholecalciferol supplementation is influenced by calcium intake; thus, this interdependence must be taken into account. With respect to bone resorption, high serum concentrations of β-CTX indicate increased bone resorption, bone fragility and fracture risk25. Our results showed that serum levels of β-CTX significantly decreased after supplementation with 0.25 μg/d calcitriol and 600 mg/d calcium for 12 and 24 months. These results indicate that supplementation with 0.25 μg/d calcitriol effectively reduced bone resorption. Furthermore, the results of the current study revealed that serum levels of P1NP, a metabolic marker of bone formation, were significantly decreased after treatment with calcium and calcitriol for 24 months. Hurst et al26 found that women who were deficient in vitamin D and who were administered 4000 IU of cholecalciferol daily for 6 months exhibited a suppression of age-induced bone turnover and bone resorption. However, our results did not indicate that cholecalciferol supplementation had any effect on the levels of bone turnover markers, which is consistent with data from previous studies21,27. These results might have occurred because the participants in our study received inadequate doses of vitamin D supplementation.
Sarcopenia was first defined in 1989 by Rosenberg as an age-related reduction in muscle or lean body mass28. The techniques that are used to assess sarcopenia include BIA and DXA measurements for muscle mass, handgrip strength for muscle strength, the Short Physical Performance Battery (SPPB) for typical gait speed, and the get-up-and-go test for physical performance29. The Leiden 85-plus Study examined Dutch individuals who were older than 85 years of age and found that low handgrip strength was a predictor of accelerated decline in activities of daily living (ADL) score and cognition30. Menopausal status is considered to significantly affect the maintenance of muscle mass, and a transition into menopause has been associated with a reduction in muscle mass in women31. In the participants of the present study, assessments of handgrip strength and chair rising tests were performed to measure muscle strength and physical performance, respectively. The subjects in group A exhibited significantly reduced muscle strength and physical performance over time, as demonstrated by reductions in grip strength in both hands and by increasingly long completion times on the chair rising test. These results indicated that muscle strength deteriorates and physical performance is reduced in postmenopausal women as they age. In a long-term study on healthy older men and women who exhibited serum 25(OH)D levels <30 ng/mL, daily supplementation with 800 IU vitamin D3 and 1000 mg calcium significantly improved physical performance over a 12- to 20-month period compared to supplementation with calcium alone8. In the current study, supplementation with cholecalciferol for 12 months or calcitriol for 12 or 24 months maintained baseline levels of handgrip strength. However, there were significant increases in the completion times of the chair rising test in all of the groups. The causative factor behind the lack of improvement in physical performance in the current study could be a gender-specific effect of vitamin D supplementation; an observational study of older Italians demonstrated a relationship between vitamin D status and measures of frailty in men but not in women4. Additionally, in a study that focused on the effects of cholecalciferol and calcium supplementation on skeletal muscle strength in males and females, a sex-stratified analysis revealed an improvement in handgrip strength in males but not in females32. However, a study that was conducted in Hong Kong revealed that in older Chinese men with adequate levels of vitamin D [mean serum 25(OH)D level of 77.9 nmol/L] and high levels of baseline physical function, vitamin D status may not play an important role in physical function or muscle mass based on cross-sectional or longitudinal analysis33.
To assess the effects of vitamin D supplementation on the quality of life of our participants, the subjects completed SF-36 questionnaires both before and after the intervention. The responses that are provided in the PF, RP, BP, and GH scales of the SF-36 questionnaire reflect physical health. The responses to the RE, MH, SE, and VT scales of the questionnaire reflect mental health34. In a cohort of subjects with fibromyalgia, vitamin D deficiency was reported to be associated with depression and anxiety35. Jugdeep et al36 found no significant changes in the SF-36 scores of subjects who received a single intramuscular injection of 600 000 IU ergocalciferol, whereas a different study demonstrated an improvement in seasonal affective disorder as a result of vitamin D supplementation37. In our study, there were significant decreases in PF, VT, SF, and MF scores on the SF-36 at the 12- and 24-month follow-ups, indicating that a degeneration of health status occurs, especially with respect to mental health, in postmenopausal women who are supplemented with only 600 mg/d calcium. PF, VT, SF, and MH scores significantly increased after cholecalciferol supplementation for 12 months and were identical to baseline levels after 24 months, indicating that 800 IU/d cholecalciferol improved the health status of these subjects, particularly with respect to mental health. Calcitriol supplementation at 0.25 μg/d maintained comparable physical and mental health levels based on the scores on all of the scales of the SF-36 between baseline and after 12 months and 24 months of the intervention, except for a significant increase in SF at the 12-month follow-up. The results of our study demonstrated a beneficial effect of 800 IU/d vitamin D supplementation on quality of life, especially mental health, in postmenopausal women. The underlying mechanism might involve the permeation of the blood-brain barrier and the choroid plexus by the lipophilic molecule vitamin D via both active transport and passive diffusion facilitated by vitamin D-binding protein38. In situ, vitamin D exerts its effects via vitamin D receptors, which are nuclear hormone receptors that are expressed in cerebral neurons. Importantly, vitamin D is considered a “neurosteroid hormone” due to its various neural activities in rodents, including its neurotrophic, immunoregulatory, and antioxidant effects14,15,16. Moreover, Annweiler et al39 found that serum deficiency of 25(OH)D was associated with larger lateral cerebral ventricles; these findings provide a scientific basis for vitamin D replacement in older adults.
The strengths of this study included that it was a prospectively designed study that was conducted for 2 years and that the study sample was relative large, with most of the subjects (approximately 95%) completing the 2-year follow-up. However, there were also several limitations. First, the study sample was limited to women because no data on men were available. A previous study showed that there might be a sex-specific association between serum vitamin D levels and physical performance and muscle mass40. Therefore, the effects of this supplementation on older men remain to be investigated. Second, serum levels of 25(OH)D and biochemical bone turnover markers (β-CTX) were not measured at the 12-month follow-up for groups A and B; therefore, the effects of treatment with calcium only or with calcium and cholecalciferol for 12 months on bone metabolism was not evaluated. Additionally, in this study, urinary calcium excretion was not measured in any of the groups.
Based on the results of this 2-year prospective study, we concluded that postmenopausal Chinese women exhibited significant decreases in muscle strength, physical performance and quality of life, which were accompanied by increased bone turnover marker levels, as they aged. Supplementation with 800 IU/d cholecalciferol and 600 mg/d calcium for 24 months maintained and even improved quality of life; however, this treatment exerted no significant effect on muscle strength, physical performance, bone turnover marker levels or PTH concentrations. After 24 months of intervention, supplementation with 0.25 μg/d calcitriol and 600 mg/d calcium exerted a protective effect on muscle strength, physical performance and health status, along with a suppression of bone turnover marker levels and PTH.
Author contribution
Li-hong GAO conducted statistical analysis and drafted the manuscript. Zhen-lin ZHANG and Ling XU conceived and designed the study and revised the manuscript. Wen-jun ZHU, Yu-juan LIU and Jie-mei GU performed the study. Ou WANG and Xiao-ping XING gave valuable suggestions on the performance of the study. All of the authors read and approved the final manuscript.
Acknowledgments
We thank all the participants of this study and their family members for their invaluable cooperation. This work was supported by the Ministry of Science and Technology of the People's Republic of China (National Key Technology R&D Program 2006BAI03B03), the National Basic Research Program of China (2014CB942903) and Academic Leaders in Health Sciences in Shanghai (XBR2011014) to Zhen-lin ZHANG.
References
- Bischoff-Ferrari HA, Dietrich T, Orav EJ, Hu FB, Zhang Y, Karlson EW, et al. Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged≥ 60 y. Am J Clin Nutr. 2004;80:752–8. doi: 10.1093/ajcn/80.3.752. [DOI] [PubMed] [Google Scholar]
- Gerdhem P, Ringsberg K, Obrant K, Akesson K. Association between 25-hydroxy vitamin D levels, physical activity, muscle strength and fractures in the prospective population-based OPRA Study of Elderly Women. Osteoporos Int. 2005;16:1425–31. doi: 10.1007/s00198-005-1860-1. [DOI] [PubMed] [Google Scholar]
- Wicherts IS, van Schoor NM, Boeke AJP, Visser M, Deeg DJ, Smit J, et al. Vitamin D status predicts physical performance and its decline in older persons. J Clin Endocrinol Metab. 2007;92:2058–65. doi: 10.1210/jc.2006-1525. [DOI] [PubMed] [Google Scholar]
- Shardell M, Hicks GE, Miller RR, Kritchevsky S, Andersen D, Bandinelli S, et al. Association of low vitamin D levels with the frailty syndrome in men and women. J Gerontol A Biol Sci Med Sci. 2009;64:69–75. doi: 10.1093/gerona/gln007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki T, Kwon J, Kim H, Shimada H, Yoshida Y, Iwasa H, et al. Low serum 25-hydroxyvitamin D levels associated with falls among Japanese community-dwelling elderly. J Bone and Miner Re. 2008;23:1309–17. doi: 10.1359/jbmr.080328. [DOI] [PubMed] [Google Scholar]
- Pfeifer M, Begerow B, Minne HW, Abrams C, Nachtigall D, Hansen C. Effects of a short-term vitamin D and calcium supplementation on body sway and secondary hyperparathyroidism in elderly women. J Bone Miner Res. 2000;15:1113–8. doi: 10.1359/jbmr.2000.15.6.1113. [DOI] [PubMed] [Google Scholar]
- Bischoff HA, Stähelin HB, Dick W, Akos R, Knecht M, Salis C, et al. Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Miner Re. 2003;18:343–51. doi: 10.1359/jbmr.2003.18.2.343. [DOI] [PubMed] [Google Scholar]
- Pfeifer M, Begerow B, Minne H, Suppan K, Fahrleitner-Pammer A, Dobnig H. Effects of a long-term vitamin D and calcium supplementation on falls and parameters of muscle function in community-dwelling older individuals. Osteoporos Int. 2009;20:315–22. doi: 10.1007/s00198-008-0662-7. [DOI] [PubMed] [Google Scholar]
- Anglin RE, Samaan Z, Walter SD, McDonald SD. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. Br J Psychiatry. 2013;202:100–7. doi: 10.1192/bjp.bp.111.106666. [DOI] [PubMed] [Google Scholar]
- Barnard K, Colon-Emeric C. Extraskeletal effects of vitamin D in older adults: cardiovascular disease, mortality, mood, and cognition. Am J Geriatr Pharmacother. 2010;8:4–33. doi: 10.1016/j.amjopharm.2010.02.004. [DOI] [PubMed] [Google Scholar]
- Ju SY, Lee YJ, Jeong SN. Serum 25-hydroxyvitamin D levels and the risk of depression: a systematic review and meta-analysis. J Nutr Health Aging. 2013;17:447–55. doi: 10.1007/s12603-012-0418-0. [DOI] [PubMed] [Google Scholar]
- Huang W, Shah S, Long Q, Crankshaw AK, Tangpricha V. Improvement of pain, sleep, and quality of life in chronic pain patients with vitamin D supplementation. Clin J Pain. 2013;29:341–7. doi: 10.1097/AJP.0b013e318255655d. [DOI] [PubMed] [Google Scholar]
- Polly P, Tan TC.The role of vitamin D in skeletal and cardiac muscle function Front Physiol 2014. doi: 10.3389/fphys.2014.00145 [DOI] [PMC free article] [PubMed]
- Kalueff AV, Tuohimaa P. Neurosteroid hormone vitamin D and its utility in clinical nutrition. Curr Opin Clin Nutr Metab Care. 2007;10:12–9. doi: 10.1097/MCO.0b013e328010ca18. [DOI] [PubMed] [Google Scholar]
- Annweiler C, Schott AM, Berrut G, Chauviré V, Le Gall D, Inzitari M, et al. Vitamin D and ageing: neurological issues. Neuropsychobiology. 2010;62:139–50. doi: 10.1159/000318570. [DOI] [PubMed] [Google Scholar]
- Dickens AP, Lang IA, Langa KM, Kos K, Llewellyn DJ. Vitamin D, cognitive dysfunction and dementia in older adults. CNS drugs. 2011;25:629–39. doi: 10.2165/11593080-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, He JW, Fu WZ, Zhang CQ, Zhang ZL. An analysis of the association between the vitamin D pathway and serum 25-hydroxyvitamin D levels in a healthy Chinese population. J Bone Miner Res. 2013;28:1784–92. doi: 10.1002/jbmr.1926. [DOI] [PubMed] [Google Scholar]
- Hu WW, Zhang Z, He JW, Fu WZ, Wang C, Zhang H, et al. Establishing reference intervals for bone turnover markers in the healthy shanghai population and the relationship with bone mineral density in postmenopausal women Int J Endocrinol 20132013513925doi: 10.1155/2013/513925 [DOI] [PMC free article] [PubMed]
- McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- Heaney RP, Dowell MS, Hale CA, Bendich A. Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D. J Am Coll Nutr. 2003;22:142–6. doi: 10.1080/07315724.2003.10719287. [DOI] [PubMed] [Google Scholar]
- Kuwabara A, Tsugawa N, Tanaka K, Fujii M, Kawai N, Mukae S, et al. Improvement of vitamin D status in Japanese institutionalized elderly by supplementation with 800 IU of vitamin D (3) J Nutr Sci Vitaminol (Tokyo) 2009;55:453–8. doi: 10.3177/jnsv.55.453. [DOI] [PubMed] [Google Scholar]
- Seamans KM, Cashman KD. Existing and potentially novel functional markers of vitamin D status: a systematic review. Am J Clin Nutr. 2009;89:1997s–2008s. doi: 10.3945/ajcn.2009.27230D. [DOI] [PubMed] [Google Scholar]
- Harris SS, Dawson-Hughes B. Plasma vitamin D and 25OHD responses of young and old men to supplementation with vitamin D3. J Am Coll Nutr. 2002;21:357–62. doi: 10.1080/07315724.2002.10719235. [DOI] [PubMed] [Google Scholar]
- Patel R, Collins D, Bullock S, Swaminathan R, Blake GM, Fogelman I. The effect of season and vitamin D supplementation on bone mineral density in healthy women: a double-masked crossover study. Osteoporos Int. 2001;12:319–25. doi: 10.1007/s001980170122. [DOI] [PubMed] [Google Scholar]
- Eastell R, Hannon RA. Biomarkers of bone health and osteoporosis risk. Proc Nutr Soc. 2008;67:157–62. doi: 10.1017/S002966510800699X. [DOI] [PubMed] [Google Scholar]
- Von Hurst P, Stonehouse W, Kruger M, Coad J. Vitamin D supplementation suppresses age-induced bone turnover in older women who are vitamin D deficient. J Steroid Biochem Mol Biol. 2010;121:293–6. doi: 10.1016/j.jsbmb.2010.03.054. [DOI] [PubMed] [Google Scholar]
- Seamans KM, Hill TR, Wallace JM, Horigan G, Lucey AJ, Barnes MS, et al. Cholecalciferol supplementation throughout winter does not affect markers of bone turnover in healthy young and elderly adults. J Nutr. 2010;140:454–60. doi: 10.3945/jn.109.113480. [DOI] [PubMed] [Google Scholar]
- Rosenberg IH. Summary comments: epidemiological and methodological problems in determining nutritional status of older persons. Am J Clin Nutr. 1989;50:1231–3. [Google Scholar]
- Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–23. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taekema DG, Gussekloo J, Maier AB, Westendorp RG, de Craen AJ. Handgrip strength as a predictor of functional, psychological and social health. A prospective population-based study among the oldest old. Age Ageing. 2010;39:331–7. doi: 10.1093/ageing/afq022. [DOI] [PubMed] [Google Scholar]
- Sirola J, Kroger H.Similarities in acquired factors related to postmenopausal osteoporosis and sarcopenia J Osteoporos 20112011536735doi: 10.4061/2011/536735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta R, Sharma U, Gupta N, Kalaivani M, Singh U, Guleria R, et al. Effect of cholecalciferol and calcium supplementation on muscle strength and energy metabolism in vitamin D-deficient Asian Indians: a randomized, controlled trial. Clin Endocrinol (Oxf) 2010;73:445–51. doi: 10.1111/j.1365-2265.2010.03816.x. [DOI] [PubMed] [Google Scholar]
- Chan R, Chan D, Woo J, Ohlsson C, Mellström D, Kwok T, et al. Not all elderly people benefit from vitamin D supplementation with respect to physical function: results from the osteoporotic fractures in men study, Hong Kong. J Am Geriatr Soc. 2012;60:290–5. doi: 10.1111/j.1532-5415.2011.03789.x. [DOI] [PubMed] [Google Scholar]
- Goswami R, Vatsa M, Sreenivas V, Singh U, Gupta N, Lakshmy R, et al. Skeletal muscle strength in young Asian Indian females after vitamin D and calcium supplementation: a double-blind randomized controlled clinical trial. J Clin Endocrinol Metab. 2012;97:4709–16. doi: 10.1210/jc.2012-2340. [DOI] [PubMed] [Google Scholar]
- Armstrong D, Meenagh G, Bickle I, Lee A, Curran ES, Finch M. Vitamin D deficiency is associated with anxiety and depression in fibromyalgia. Clin Rheumatol. 2007;26:551–4. doi: 10.1007/s10067-006-0348-5. [DOI] [PubMed] [Google Scholar]
- Dhesi JK, Jackson SH, Bearne LM, Moniz C, Hurley MV, Swift CG, et al. Vitamin D supplementation improves neuromuscular function in older people who fall. Age Ageing. 2004;33:589–95. doi: 10.1093/ageing/afh209. [DOI] [PubMed] [Google Scholar]
- Gloth 3rd F, Alam W, Hollis B. Vitamin D vs broad spectrum phototherapy in the treatment of seasonal affective disorder. J Nutr Health Aging. 1999;3:5–7. [PubMed] [Google Scholar]
- Holmøy T, Moen SM, Gundersen TA, Holick MF, Fainardi E, Castellazzi M, et al. 25-Hydroxyvitamin D in cerebrospinal fluid during relapse and remission of multiple sclerosis. Mult Scler. 2009;15:1280–5. doi: 10.1177/1352458509107008. [DOI] [PubMed] [Google Scholar]
- Annweiler C, Montero-Odasso M, Hachinski V, Seshadri S, Bartha R, Beauchet O. Vitamin D concentration and lateral cerebral ventricle volume in older adults. Mol Nutr Food Res. 2013;57:267–76. doi: 10.1002/mnfr.201200418. [DOI] [PubMed] [Google Scholar]
- Dam TT, von Muhlen D, Barrett-Connor EL. Sex-specific association of serum vitamin D levels with physical function in older adults. Osteoporos Int. 2009;20:751–60. doi: 10.1007/s00198-008-0749-1. [DOI] [PMC free article] [PubMed] [Google Scholar]